Abstract
Using a longitudinal, prospective adoption design, this study examined the effects of the environment (adoptive parents’ depressive symptoms and responsiveness) and genetic liability of maternal depression (inferred by birth mothers’ major depressive disorder [MDD]) on the development of fussiness between 9 and 18 months of age in adopted children. The sample included 281 families linked through adoption, with each family including four individuals (i.e., adopted child, birth mother, adoptive father and mother). Results showed that adoptive mothers’ depressive symptoms at 9 months of child age were positively associated with child fussiness at 18 months of age. A significant interaction between birth mothers’ MDD and adoptive mothers’ responsiveness indicated that children of birth mothers with MDD showed higher levels of fussiness at 18 months of age when adoptive mothers had been less responsive at 9 months of child age. However, in the context of high levels of adoptive mothers’ responsiveness, children of birth mothers with MDD did not show elevated fussiness at 18 months. Findings are discussed in terms of gene-environment interactions in the intergenerational risk transmission of depression.
Keywords: maternal depression, fussiness, parental responsiveness, adoption designs, gene-environment interactions
Maternal depression has been identified as a potent familial risk factor involved in the development of internalizing and externalizing psychopathology in offspring (e.g., Downey & Coyne, 1990; Frendrich, Warner, & Weissman, 1990; Goodman & Gotlib, 1999; Zimmermann et al., 2008). Even infants and toddlers are sensitive to maternal depression; young children of depressed mothers often display their distress through fussing and crying (Campbell, Cohn, & Meyers, 1995; Cicchetti, Rogosch, & Toth, 1998; Weinberg & Tronick, 1998). While maternal depression exerts adverse impact on emotional development of offspring in some families (Hammen, 1991), not all offspring of depressed mothers develop emotional and behavioral problems. There is very little systematic evidence to explain why there is such marked variability in children’s responses to maternal depression. Given that depression is significantly genetically loaded (McGuffin & Katz, 1989), such heterogeneity may be better understood from a gene-environment interaction framework: A positive, enriched social context could prevent or at least attenuate the expression of a genetic diathesis for depression, whereas in the presence of a stressful environment, the likelihood of genetic liability might increase. In other words, the quality of children’s proximal social context should moderate the expression of genetic liability (Shannahan & Hofer, 2005). The major aim of the present study was, therefore, to investigate the interplay of genetic and environmental contributions in the transmission of maternal depression to emotional development in early childhood, using a prospective, longitudinal adoption design.
To examine whether genetic liability of depression transmitted from a mother to a child is moderated by the caregiving environment, it is necessary to partition nature and nurture effects from one another. Conventional family studies composed of depressed mothers and their biological child(ren) are less than optimal because maternal depression increases the child’s risk for depression for both environmental and genetic reasons (Goodman & Gotlib, 1999; Kim-Cohen, Moffitt, Taylor, Pawlby, & Caspi, 2005). An adoption study is one of the most powerful designs for detecting the interaction between genetic liability and environment because it allows a relatively clean separation of nature from nurture (Rutter, Pickles, Murray, & Eaves, 2001). Using data from the Early Growth and Development Study (EGDS; Leve et al., 2007), the current study approximated genetic liability for depression from birth mothers’ lifetime diagnosis of major depressive disorder (MDD), and estimated environmental influences from adoptive parents’ responsiveness to examine their joint effects on the development of child fussiness in early toddlerhood.
How genetic liability for depression is manifested in the emotional development of infants and toddlers is currently unknown. This may be due to the fact that depressive tendencies, much less depressive disorders, in toddlers are difficult to assess and likely do not emerge until later in childhood. In studying psychopathology in infants and toddlers, one approach is to examine risk factors associated with subsequent disorders (Zeanah, Boris, & Scheeringa, 1997). A likely precursor of affective problems that may be genetically influenced is young children’s fussy, emotionally negatively charged behaviors — plausible phenotypes through which infants manifest their emotional distress and difficulties. Fussy behaviors and affectively charged negative reactions in young children have been found to predict a broad spectrum of later internalizing symptomatology (Caspi, Henry, McGee, Moffitt, & Silva, 1995; Rende, 1993). For instance, a global pattern of distress during early childhood, which becomes differentiated to negative emotions such as distress and anger tendencies in later infancy and toddlerhood (e.g., Riese, 1987; Sternberg & Campos, 1990), has been linked to depression and anxiety at age 7 (Rende, 1993). Indeed, research on toddlers has documented that facial and vocal expressions charged with negative emotions at four months of age are linked to socially withdrawn behaviors at 30 months of age (Gloggler & Pauli-Pott, 2008). Infant fussiness, often studied as an index of difficult temperament, is known to be influenced by both genetic and environmental factors during the first year of life (Silberg et al., 2005).
The focus of the present study was on developmental changes in fussy, difficult behaviors from infancy to toddlerhood. With the rapid development of toddler’s emotional development and awareness of the presence and intents of others, children increasingly become capable of displaying their emotional distress through actions such as throwing temper tantrums, fussing, and crying. Such affectively charged behavior increases between the first and second year of life, although there exists marked individual differences in its developmental change (Partridge & Lerner, 2007). This study was designed to employ a gene × environmental interaction paradigm to investigate under what conditions fussiness increases.
Adoptive parents’ responsiveness was considered as a potential environmental moderator that may alter the expression of genetic liability associated with depression. Parental responsiveness during infancy is characterized by the presence of high affection, positive reinforcement, as well as sensitive and contingent responses to the child’s needs (Landry, Smith, Swank, Assel, & Vellet, 2001). Parental, particularly maternal, responsiveness has consistently been found to be a protective factor for an array of maladaptive outcomes in social, emotional, cognitive, and communicative domains (e.g., Bornstein & Tamis-LeMonda, 1989; Bradley, Caldwell, & Rock, 1988; Landry, Smith, & Swank, 2006; Wakshlag & Hans, 1999). Attachment theorists also consider early parental responsiveness the critical element for optimizing children’s development because children develop a basic trust of their environment through positive interactions with caregivers (Ainsworth, Blehar, Waters, & Walls, 1978; van den Boom, 1995).
While high levels of caregiver responsiveness play a crucial role in child development in general, the magnitude of parental responsiveness that is necessary to promote children’s optimal development appears to depend, in part, on the specific needs of individual children. If a child is easily distressed, high parental responsiveness may be particularly helpful in calming and soothing the child. Indeed, a number of studies have shown the importance of the match between the child’s needs and parenting in promoting his or her healthy development (e.g., Crockenberg & Leerkes, 2006; Feldman, Greenbaum, & Yirmiya, 1999; Kochanska, 1995; Kochanska, Aksan, & Joy, 2007; Landry, Smith, Miller-Loncar, & Swank, 1997; Landry et al., 2001). For instance, mothers’ use of gentle, non-power-asserting discipline was hypothesized to be effective in promoting the development of internalization of control in highly fearful children because such parental discipline could keep children’s levels of anxious arousal low (Kochanska, 1995). Likewise, fathers’ power assertion was counterproductive for fearful children’s internalization of rules (Kochanska et al., 2007). Furthermore, consistent maternal responsive parenting has been found to be particularly important for the development of biologically at-risk children who were born prematurely (Landry et al., 2001). It is plausible, then, that high levels of contingent attentiveness and responsiveness from parents could be effective in keeping distress low among children who are genetically predisposed for developing internalizing problems such as depression. We thus hypothesized that adopted children with a genetic liability for depression would likely benefit from high responsiveness displayed by adoptive parents more than children without a genetic liability for depression. In addition, as the majority of empirical work has solely focused on maternal responsiveness, we sought to expand the extant literature by also incorporating measurement of fathers’ responsiveness as a potential moderating factor for genetic liability for depression. Thus, the current study examined both maternal and paternal responsiveness.
No study that we are aware of has tested interactions between genetic liability for depression and parental responsiveness in relation to the development of fussiness and distress in very young children. In the literature on adolescent and adult depression, a potential moderation of genetic risk by environment has been frequently observed (e.g., Caspi et al., 2003; Eaves, Silberg, & Erkanli, 2003; Kendler et al., 1995; Rice, Harold, Shelton, & Thaper, 2006; Silberg, Rutter, Neale, & Eaves, 2001). For instance, Kendler et al. (1995) found an interaction between estimated genetic liability (indexed by the co-twin’s major depressive disorder status) and stressful life events. These investigators showed that in the absence of a severe life event, the likelihood of major depression was relatively equally distributed regardless of the individual’s genetic risk. In the presence of a severe life event, however, the risk of onset of major depression was significantly higher in individuals with higher genetic risk than in those with lower genetic risk (Kendler et al., 1995). Rice et al. (2006) also reported an interaction between genetic liability for depression and family conflict in their twin study.
A limited number of studies on young children also appear to support the possibility of the interaction between genetic risk and environment in predicting emotional distress. A recent investigation on toddlers’ affective problems (such as crying, sadness) has demonstrated that risks associated with genetic variation in doparminergic function were decreased when children were exposed to sensitive mothers (Mills-Koonce et al., 2007). Furthermore, in their study of serotonin transporter gene, Barry, Kochanska, and Philibert (2008) recently reported that 15-month children with a short 5-HTT allele were likely to show insecure attachment --which included crying as one of the indices -- when mothers were unresponsive to them at 7 months. In a study of school-aged children, Kaufman et al. (2004) found that children with a short 5-HTT allele were at risk for depression if they had been exposed to maltreatment and received low social support. Although these studies have highlighted the importance of gene-environmental interplay in the etiology of depression, existing knowledge about young children’s distress still remains scant. In addition, the question of whether moderation of genetic liability by parental responsiveness has prospective significance in increases or decreases in distress over time merits further examination. The present investigation attempts to bridge the gap in the existing literature by testing genetic liability-environment interaction using data from children who were adopted at birth and then assessed at 9 and 18 months of age.
The Present Study
This study tested whether genotype and environment jointly influence the development of one aspect of emotional adjustment in very early childhood: fussiness. Our hypotheses were three-fold: (a) genetic liability for depression would be associated with increases in child fussiness from 9 to 18 months of age; (b) adoptive parents’ responsiveness would be prospectively associated with decreased levels of child fussiness; and most importantly, (c) the effect of genetic liability would be buffered by the adoptive parents’ responsiveness. Specifically, we expected child fussiness to increase from 9 to 18 months of age when children with a genetic liability for depression, as indexed by birth mother’s diagnosis of MDD, encountered less responsive parenting in their adoptive home. Conversely, in the context of high levels of adoptive parents’ responsiveness, the effect of genetic liability on child fussiness was expected to be attenuated. In testing these hypotheses, we also examined the main effect of adoptive parents’ depressive symptoms because it represents an important additional environmental stress. An examination of the main and interactive effects of birth mothers’ depression, adoptive parents’ responsiveness, and adoptive parents’ depressive symptoms on changes in child fussiness has significant potential to shed light on how genotype and family environment operate to link maternal depression and infants’ emotional adjustment.
Method
Participants
The Early Growth and Development Study (EGDS) is an ongoing, prospective multi-site study of 361 families linked through adoption. The participants from each linked family involve the child who was adopted at birth, the adoptive parents, and the birth mother. Although not a focus of this study, birth fathers also participated in approximately one-third of the families. The overarching goal of the EGDS is to examine the effects of genotype-environment interaction and correlation on socioemotional development. The EGDS drew its sample from 33 adoption agencies in 10 states in three regions in the U.S.: Northwest, Southwest, and Mid-Atlantic. These agencies reflect the full range of U.S. adoption agencies: public, private, religious, secular, those favoring open adoptions, and those favoring closed adoptions. Each agency recorded the demographic information from all clients who met the recruitment criteria (domestic adoption placement to a non-relative within 90 days of birth). Because the sample was recruited from three different geographical regions, we examined regional differences in demographic characteristics (i.e., age, income, education of birth and adoptive parents). Only two significant regional differences were found: adoptive fathers’ education was slightly higher in the Northwest site than in the Southwest site and birth mothers’ household income was slightly higher in the Mid-Atlantic site than the Southwest site.
The current investigation was based on the first two waves of data. The adopted children were approximately 9 months (M = 8.84, SD = 1.20) and 18 months (M = 17.83, SD = 1.20) of age at the Time 1 (T1) and Time 2 (T2) assessments, respectively. A total of 331 of the original 361 linked families had data on one or more of the T2 measures analyzed in the present study. The analytical sample in this report included 281 linked adoption triads (i.e., the adopted child, birth mother, and adoptive parents) who provided complete information on the crucial study variables (i.e., birth mother’s diagnosis of MDD, both adoptive mother- and father-report of the adopted child’s fussiness at the T2 assessment, and interviewer’s ratings for both adoptive mother’s and father’s responsiveness). There were no significant differences between the participants in the analytical sample and those who were not included in this report on demographic characteristics and other study variables, except that those who were excluded from the present report described their experience of adoption as more closed (M = −0.19, SD = 0.71) than participants in the current sample (M = 0.08, SD = 0.73; t(359) = 2.92, p < .01) .
The mean age of the child at the adoption placement was three days (SD = 5 days). Forty-three percent (n = 122) of the children were female. Fifty-nine percent of the children were Caucasian, 21% were mixed race, 8% were African American, and 12% were Asian or unknown. The mean ages for adoptive mothers, adoptive fathers, and birth mothers at T1 were 37.9 (SD = 5.2), 38.7 (SD = 5.9), and 24.0 (SD = 6.0), respectively. At T2, they were 38.6 (SD = 5.2), 39.3 (SD = 5.8), and 25.0 (SD = 6.0) years old, respectively. Ninety-one percent of adoptive mothers and 89% of adoptive fathers in this sample were Caucasian. These estimates for Caucasians are higher than the Census 2000 national estimates of adoptive parents’ race/ethnicity composition (71% of adoptive parents were non-Hispanic White, see Kreider, 2003 for details). The birth mother sample was more ethnically diverse: 72% were Caucasian, 9% were African American, 4% were Hispanic American, 4% were American Indian/Alaska native, 2% were Asian, 7 % were more than one racial/ethnic background, and 2% had unknown/other racial-ethnic background. Nearly half (49%) of the adoptive parents were characterized as affluent and had annual gross household incomes that exceeded $100,000. More than 70% of adoptive parents had completed college education or had advanced to graduate schools for further educational degree. Adoptive parents had been married an average of 11.54 years (SD = 5.1 years) at T1. Eighty-five percent of birth mothers had household income of less than $20,000. The majority of birth mothers (96%) did not have a college degree.
Procedure
The birth parent assessment consisted of a 2 ½ hour interview in their home or in another location convenient for them; the adoptive family assessments were 2 ½ hours long and conducted in their home. Participants were paid for volunteering their time to the study. For both the birth- and adoptive-parent assessments, interviewers asked participants computer-assisted interview questions, and each participant independently completed a set of questionnaires. Participants also answered some questions via paper-pencil prior to the interview. Assessments of birth parents and adoptive families were conducted by separate teams of interviewers; each team was completely blind to data collected by the other. Domains assessed for both adoptive and birth parents included personality, psychosocial adjustment, life events, and the adoption placement. Interviewers completed a minimum of 40 hours of training, including a two-day group session, pilot interviews, and videotaped feedback, prior to administering interviews with study participants. All interviews were audio- or video-recorded and feedback was provided by a trained evaluator for a random selection of 15% of the interviews to ensure adherence to the study’s standardized interview protocols. Additional details on the EGDS study recruitment procedures, sample, and assessment methods can be found in Leve et al. (2007).
Measures
Child fussiness at 9 and 18 months of age
At the T1 and T2 assessments, adoptive mothers and fathers separately completed seven items from the “Fussy-Difficult” factor of the Infant Characteristics Questionnaire (ICQ: Bates, Freeland, & Lounsbury, 1979). The 7-item Fussy-Difficult subscale assesses parental perception of fussiness, negative emotionality, and soothability in a child. A sample of items include: How easy or difficult is it for you to calm or soothe your baby when s/he is upset? How many times per day, on average, does your baby get fussy or irritable for either short or long periods of time? How easily does your baby get upset? How often does your baby’s mood change? Adoptive parents indicated their responses using a 7-point scale, with higher scores indicating greater child fussiness. Adoptive-mother and -father reports demonstrated adequate internal consistency for both waves, with Cronbach’s alpha coefficients of .84 and .86 for T1 and .84 and .85 for T2, respectively.
Birth mothers’ lifetime diagnosis for major depressive disorder
At the T2 assessment, the major depressive disorder (MDD) module in the Composite International Diagnostic Interview (CIDI: Andrews & Peters, 1998; Kessler & Ustun, 2004) was used to assess birth mothers’ lifetime MDD. The CIDI is a highly structural, standardized interview that assesses 17 major diagnostic mental disorders according to the definitions and criteria of the International Classification of Disease (ICD: World Health Organization, 1992, 1993) and the fourth edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-IV: American Psychiatric Association, 1994). Interviewers asked birth mothers a series of questions about their mental health using the computer-assisted personal interview program. Data were processed by a SAS program distributed by the CIDI training group. The diagnosis of MDD was based on DSM-IV criteria. Birth mothers who were diagnosed with lifetime MDD were coded as one and those without any history of MDD as zero. By the T2 assessment, 30% (n = 85) of birth mothers met diagnosis for lifetime MDD and 70% (n = 196) did not.
Adoptive parents’ responsiveness at 9 months of child age
Upon completion of the T1 in-home interview, interviewers reported their ratings of adoptive parents’ responsiveness using the responsiveness subscale of the infant and toddler version of the Home Observation for Measurement of the Environment Inventory (Caldwell & Bradley, 1984). The HOME was designed to measure the quantity and quality of social, emotional, and cognitive support available to young children up to 3 years of age at their home (Caldwell & Bradley, 1984). Using a yes-no response format, the interviewers rated each adoptive mother and father separately on items regarding his or her emotional and verbal responsivity during the visit (α = .54 and .63 for adoptive mothers and fathers, respectively). The original parental responsiveness scale in the HOME consists of 11 items. However, in the EGDS, one item (i.e., Mother/father allows the child to engage in “messy” types of play, including playing with sand, mud, water, finger-paints, or, for young babies, food) was omitted due to the interviewers’ limited opportunities to observe such behaviors during the visit. Therefore, the parental responsiveness scale used in this study was based on the remaining 10 items. Sample items include: Mother/Father responds to the child’s vocalizations with verbal or vocal response; when speaking of or to the child, mother’s/father’s voice conveys positive feeling; and mother/father shows some positive emotional response to praise of the child offered by interviewer.
Adoptive parents’ depressive symptoms at 9 months of child age
At the T1 assessment, adoptive mothers and fathers completed the Beck Depression Inventory (BDI; Beck & Steer, 1993) to indicate their level of depressive symptoms. The BDI is a widely-used, self-report measure of depressive symptoms. Adoptive parents were asked to choose one of four statements that ranged from positive to depressive feelings in the past week, with higher scores indicating higher levels of depressive symptoms. The original BDI consists of 21 items, but an item about suicidal ideation was omitted in this study because of limited resources for making clinical referrals, resulting in 20 items. The Cronbach’s alphas were .80 for both adoptive mothers and fathers.
Covariates
For reasons that are described below, three covariates were included in the analyses: openness in adoption, birth mothers’ substance use during pregnancy, and birth mothers’ age at the assessment of MDD.
Openness in adoption was accounted for in the analyses to control for similarities between birth and adoptive families that may have resulted from post-adoption exchanges between parties. The level of openness in adoption was measured at T1 using three subscales independently reported by birth mothers, adoptive mothers, and adoptive fathers (for details, see Ge et al., 2008). Three subscales included perceived openness (a 7-point scale ranging from 1 = very closed to 7 = very open); actual contact between adoptive and birth parents (four items for birth mothers, six items for adoptive mothers and fathers on a 5-point scale ranging from 1 = never to 5 = daily); and the amount of knowledge of one another between birth mother and adoptive parents (five items on knowledge about the other party’s physical health, mental health, ethnic and cultural background, reasons for adoption, and the extended family’s health history rated on a 4-point Likert-type scale ranging from 1 = nothing to 4 = a lot). The perceived openness, contact, and knowledge subscales were then standardized and combined to create an aggregate openness score for each informant (alphas ranged from .74 – .78). Finally, the three informant ratings were standardized and combined to create the openness composite (α = .88).
Birth mothers’ substance use during pregnancy is a potential intrauterine environmental effect that can confound estimates of the genetic influences. In the analyses, we included prenatal exposure to drug and alcohol that was approximated by birth mothers’ substance use during pregnancy (for details, see Leve et al., in press). Birth mothers reported their use of ten substance classes (tobacco, alcohol, sedatives, tranquilizers, amphetamines, painkillers, inhalants, cocaine, heroin, and hallucinogens) during pregnancy using a pregnancy history calendar method developed for the study. Participants were asked to identify key events throughout the pregnancy period (e.g., birthdays, holidays, vacations) and respond to the questions about their substance use during the pregnancy period, using the calendar as a reference to facilitate recall. Life history calendar methods have been shown to be an effective and reliable means of asking about retrospective events and conditions (Caspi et al., 1996). Dichotomizing all 10 indicators (0 = no use, 1 = any use) yielded an internally consistent scale, Cronbach’s α (KR-20) = .67. The ten indicators were then aggregated to create the final scale of birth mothers’ substance use during pregnancy with a 5-point scale (0, 1, 2, 3, 4 = prenatal use of no, one, two, three, or four or more substances, respectively). Fifty-seven percent of birth mothers in the analytical sample reported at least one substance use during pregnancy (27% for one, 14% for two, 10% for three, and 5% for four or more substances).
Because we focused on lifetime diagnosis of birth mothers’ MDD, the likelihood of positive MDD diagnosis was inevitably reduced for younger mothers. Therefore, birth mothers’ age at the time of MDD diagnosis (the T2 assessment) was included as a covariate to statistically account for the differential likelihood of lifetime MDD diagnosis by birth mothers’ age.
Results
Analytical Strategy
Analyses were conducted in the following steps. First, descriptive statistics and inter-correlations among the study variables were examined. Second, a series of regression analyses were performed to test whether birth mothers’ MDD and adoptive parents’ responsiveness at 9 months of child age were associated with child fussiness at 18 months of age after controlling for baseline fussiness. In testing these effects, it is important to minimize the problems associated with shared method variance. When a predictor and a criterion share the same data source, the estimated association may be inflated simply due to the shared method of assessment (Bank, Dishion, Skinner, & Patterson, 1990). Studies of psychopathology, such as the current investigation, particularly need to be aware of this problem because, for instance, depressed individuals tend to view their environment in a more negative tone (Gotlib, 1983; Moggs, Bradley, & Williams, 1995). As a means of circumventing overestimation of genetic and environmental effects due to the problem of shared method variance, we mismatched the informants who reported the criterion variable (the adopted child’s fussiness) and the major predictors (birth mothers’ MDD, adoptive parents’ depressive symptoms and responsiveness). Specifically, when we tested the effect of adoptive mother’s responsiveness (reported by interviewer) and her depressive symptoms at T1 (self-reported by adoptive mothers), we used adoptive father’s report of the adopted child’s fussiness as a criterion variable. Conversely, adoptive mother’s report of the child’s fussiness was used as an outcome variable when we entered adoptive father’s responsiveness (reported by interviewers) and his depressive symptoms at T1 (self-reported by adoptive fathers) as predictors. Birth mother’s MDD status was reported by the birth mother. The utility of multiple informants has been advocated widely (e.g., Bank et al., 1990; Kraemer et al., 2003).
Descriptive Analyses
Table 1 presents the means, standard deviations, and bivariate correlations of the study variables. As shown in Table 1, both adoptive fathers and mothers reported that the child had become fussier from 9 to 18 months of age (for adoptive fathers, t(267) = −6.58, p < .001; for adoptive mothers, t(269) = −9.24, p < .001). Examination of within-informant stability coefficients suggested that child fussiness was moderately stable across two waves (rs = .56, .60, ps < .001, for adoptive mothers and fathers, respectively). The cross-sectional correlations between adoptive mother- and father- reports of child fussiness were .61, p < .001, for T1, and .68, p < .001, for T2, indicating relatively high convergence across informants for both waves.
Table 1.
Descriptive Statistics of the Study Variables
| Means | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Child's fussiness at T2 (AF report) | 21.22 | 5.62 | -- | ||||||||||
| 2 Child's fussiness at T2 (AM report) | 21.39 | 5.69 | 0.61 *** | -- | |||||||||
| 3 Child's fussiness at T1 (AF report) | 19.18 | 5.58 | 0.60 *** | 0.43 *** | -- | ||||||||
| 4 Child's fussiness at T1 (AM report) | 18.38 | 5.51 | 0.45 *** | 0.56 *** | 0.68 *** | -- | |||||||
| 5 BM's lifetime MDD diagnosis | -- | -- | −0.06 | −0.01 | −0.11 | −0.02 | -- | ||||||
| 6 AM's depressive symptoms at T1 | 3.68 | 3.16 | 0.16 *** | 0.15 ** | 0.06 | 0.15 ** | 0.10 | -- | |||||
| 7 AF's depressive symptoms at T1 | 2.76 | 3.35 | 0.16 *** | 0.02 | 0.16 ** | 0.10 | −0.05 | 0.05 | -- | ||||
| 8 AM's responsiveness at T1 | 9.45 | 1.47 | −0.06 | −0.03 | −0.04 | −0.01 | −0.11 | 0.05 | −0.03 | -- | |||
| 9 AF's responsiveness at T1 | 8.91 | 1.62 | −0.08 | −0.06 | −0.09 | 0.04 | 0.02 | 0.04 | 0.02 | 0.48 *** | -- | ||
| 10 Openness in adoption | 0.08 | 0.73 | −0.06 | −0.01 | −0.06 | −0.01 | 0.05 | 0.01 | 0.01 | −0.02 | 0.02 | -- | |
| 11 BM's substance use during pregnancy | 1.04 | 1.19 | −0.05 | −0.06 | 0.08 | −0.08 | 0.22 *** | 0.03 | −0.04 | −0.06 | −0.07 | 0.01 | -- |
| 12 BM's age at T2 | 25.03 | 5.94 | 0.10 | −0.02 | −0.01 | 0.01 | 0.13 * | −0.06 | 0.03 | −0.01 | 0.01 | −0.24 *** | 0.09 |
Note. T1= Time 1 assessment when adopted children were 9 months old. T2=Time 2 assessment when adopted children were 18 months old. AF=adoptive fathers. AM=adoptive mothers. BM=birth mothers. N=281 linked families.
p <.05.
p <.01.
p <.001.
Bivariate correlations indicated that birth mothers’ MDD was not significantly associated with child fussiness at either wave. On the other hand, adoptive mothers’ depressive symptoms at T1 were prospectively and positively associated with both adopted-father and –mother reports of child fussiness at T2 (rs = .16, p < .001, and .15, p < .01, respectively). Adoptive fathers’ depressive symptoms at T1 were significantly associated with their reports of child fussiness at T2 (r = .16, p <.001), but not with fussiness reported by adoptive mothers. There was no significant correlation between adoptive parents’ responsiveness and child fussiness. Similarly, openness in adoption and birth mothers’ substance use during pregnancy were not significantly associated with child fussiness.
If the birth mothers’ MDD diagnosis was significantly associated with adoptive parents’ measures, gene-environment correlation may be implicated. However, we did not find any significant association between birth mothers’ MDD diagnosis and adoptive parents’ depressive symptoms or responsiveness.
To ensure the predictive validity of child fussiness as a correlate of later depression, we calculated the bivariate correlations between child fussiness at T1 and T2 (both adoptive mother- and father-reports) and child scores on the anxious-depressed and withdrawn subscales of the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2000) at T2. The CBCL was not used in the primary analysis because it was not administered at T1; it was not developmentally appropriate for 9-month old children. Results (not shown) suggested that fussiness at T1 and T2 were positively and significantly associated with the CBCL internalizing factor at T2 (with within-informant correlations ranging from 0.21 to 0.52, and cross-informant correlations ranging from 0.20 to 0.31, p <. 01 for all coefficients), suggesting that fussy behavior is an early correlate of toddler internalizing problems.
Primary Analysis
The major aim of this study was to examine the main and joint effects of birth mothers’ MDD and adoptive parents’ responsiveness on the development of fussiness among children adopted at birth. To accomplish this task, we performed hierarchical linear regressions. Results are presented in Table 2. All continuous scales were centered at their own means. Birth mothers’ MDD was dummy-coded (0 = no MDD history, 1 = MDD history). Model 1 examined the effects of birth mothers’ MDD and adoptive mothers’ responsiveness. Model 2 tested the effects of birth mothers’ MDD and adoptive fathers’ responsiveness. In these models, we controlled for the covariates of openness in adoption, birth mothers’ substance use during pregnancy, and birth mothers’ age.
Table 2.
The Prospective Effects of Birth and Adoptive Parents' Depression and Adoptive Parents' Responsiveness on the Adopted Child's Fussiness
| Child's fussiness at T2 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Informants | AF report | AM report | |||||||||||
| Model 1a | Model 1b | Model 2a | Model 2b | ||||||||||
| b | SE | B | b | SE | B | b | SE | B | b | SE | B | ||
| Intercept | 21.34 *** | 0.33 | 21.30 *** | 0.33 | 21.30 *** | 0.35 | 21.35 *** | 0.35 | |||||
| BM age at T2 | 0.11 * | 0.05 | 0.12 | 0.11 * | 0.05 | 0.12 | −0.02 | 0.05 | −0.02 | −0.02 | 0.05 | −0.02 | |
| Openness in adoption | BM, AM,AF | −0.19 | 0.38 | −0.03 | −0.19 | 0.38 | −0.03 | −0.41 | 0.41 | −0.05 | −0.41 | 0.41 | −0.05 |
| BM's substance use during pregnancy | BM | −0.34 | 0.23 | −0.08 | −0.37 | 0.24 | −0.08 | −0.34 | 0.25 | −0.07 | −0.42 | 0.26 | −0.09 |
| AM's depressive symptoms at T1 | AM | 0.25 *** | 0.09 | 0.14 | 0.26 *** | 0.09 | 0.15 | -- | -- | -- | -- | ||
| AF's depressive symptoms at T1 | AF | -- | -- | -- | -- | −0.06 | 0.09 | −0.04 | −0.07 | 0.09 | −0.04 | ||
| Child's fussiness at T1 | AM | -- | -- | -- | -- | 0.61 *** | 0.05 | 0.59 | 0.63 *** | 0.05 | 0.60 | ||
| AF | 0.59 *** | 0.05 | 0.59 | 0.59 *** | 0.05 | 0.59 | -- | -- | -- | -- | |||
| BM's lifetime major depressive disorder | BM | −0.44 | 0.61 | −0.04 | −0.46 | 0.62 | −0.04 | 0.36 | 0.65 | 0.03 | 0.42 | 0.65 | 0.03 |
| AM's responsiveness at T1 | Interviewer | -- | -- | 0.05 | 0.36 | 0.01 | -- | -- | -- | -- | |||
| AF's responsiveness at T1 | Interviewer | -- | -- | -- | -- | -- | -- | −0.16 | 0.23 | −0.04 | |||
| BM depression × AM responsiveness | BM, Interviewer | -- | -- | −1.07 * | 0.58 | −0.12 | -- | -- | -- | -- | |||
| BM depression × AF responsiveness | BM, Interviewer | -- | -- | -- | -- | -- | -- | −0.75 | 0.47 | −0.10 | |||
| AIC | 1544.8 | 1512.3 | 1574.2 | 1521.8 | |||||||||
Note .
p<.05.
p<.01.
p<.001.
T1=Time 1 assessment at 9 months of child age. T2= Time 2 assessment at 18 months of child age. AM=adoptive mother. AF=adoptive father. BM=birth mother. We used the informant mismatched design to conservatively test the effects of adoptive parents' depressive symptoms on child's fussiness. Model 1a and 1b include AM's self-reported depressive symptoms to predict AF-report of child fussiness. Model 2a and 2b, on the other hand, include the effect of AF self-reported depressive symptoms on AM's report on child's fussiness.
In Model 1a, we first tested the main effect of birth mothers’ MDD after controlling for child fussiness at T1, adoptive mothers’ depressive symptoms at T1, and the other covariates. Child fussiness was moderately stable across the two waves (b = .59, p < .001). Adoptive mothers’ depressive symptoms at T1 was positively associated with child fussiness at T2 (b = .25, p < .001) after statistically controlling for the stability in child fussiness. The main effect of birth mothers’ MDD on child fussiness assessed at T2 was not statistically significant.
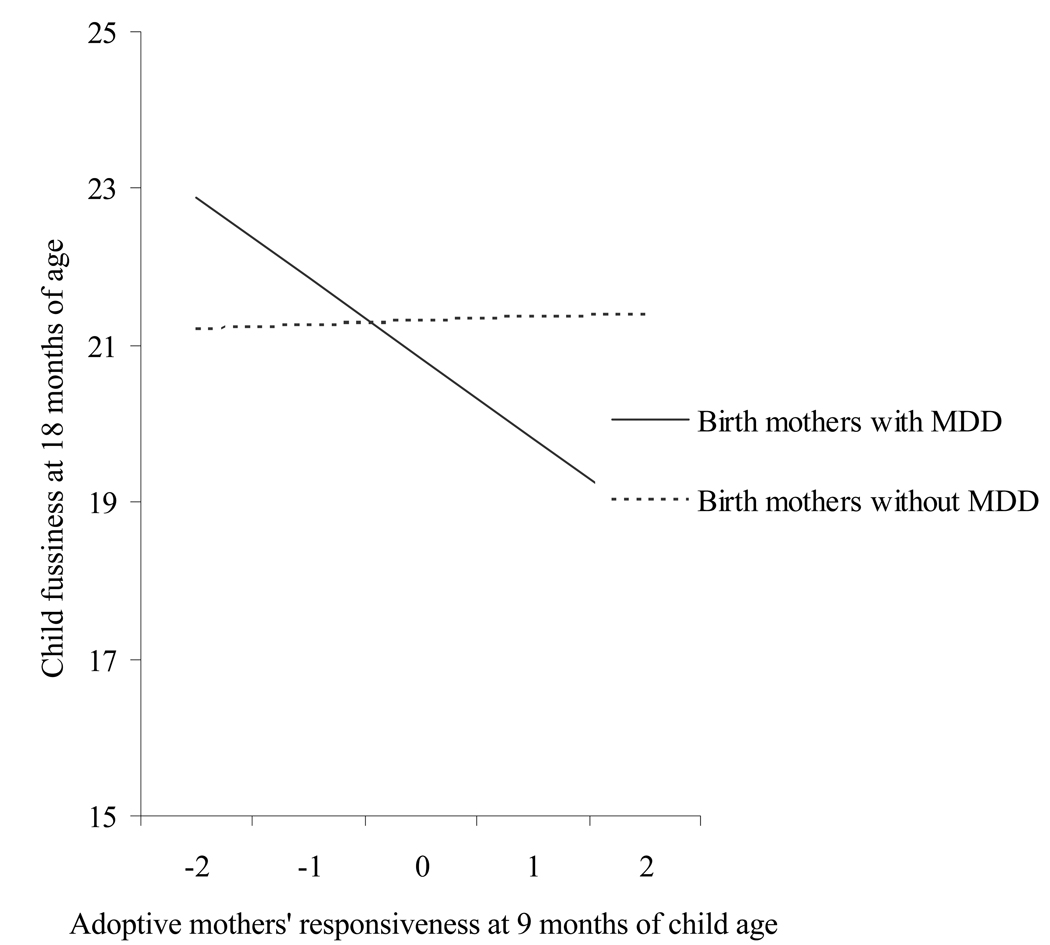
Model 1b included the main effect of adoptive mothers’ responsiveness and its interaction with birth mothers’ MDD to predict changes in adoptive father-report of child fussiness. The main effect of adoptive mothers’ responsiveness at T1 on child fussiness assessed at T2 was not statistically significant. Importantly, however, we found the interaction between birth mothers’ MDD and adoptive mothers’ responsiveness to be significant (b = −1.07, p < .05). Figure 1 illustrates this statistical interaction. As shown in Figure 1, children of birth mothers with a history of MDD exhibited higher levels of fussiness at 18 months of age when their adoptive mothers had been less responsive to them at 9 months. However, genetic liability associated with birth mothers’ MDD was mitigated when coupled with high responsiveness offered by adoptive mothers.
Figure 1.
The interaction between birth mothers’ lifetime MDD and adoptive mothers’ responsiveness at 9 months of child age in predicting child fussiness at 18 months of age.
A similar, but weaker pattern of findings emerged for adoptive fathers’ responsiveness. In Model 2a, the effect of adoptive fathers’ depressive symptoms at T1 on adoptive-mother report of child fussiness at T2 was not statistically significant after controlling for the baseline fussiness. Model 2b revealed a similar pattern of statistical interaction to that of Model 1b, although it did not reach statistical significance (b = −.75, p = .11).
Discussion
Maternal depression has long been recognized as a potent family risk factor for young children (e.g., Campbell et al., 1995; Weinberg & Tronick, 1998). While depression runs in some families, significant variability in outcomes among offspring of depressed parents has yet to be explained. The overarching goal of this study was to examine how genetic liability for depression and family environment together explain the variation in offspring’s emotional experiences in very early childhood. Capitalizing on the adoption design, we sought to clarify the interaction between genetic liability indexed by birth mothers’ MDD and adoptive parents’ responsiveness in predicting the development of fussiness during early toddlerhood.
Several important findings emerged. Central to our genotype-environment interaction hypothesis, we found a statistically significant interaction between genetic liability inferred from birth mothers’ phenotype and adoptive mothers’ responsiveness in predicting increases in children’s fussiness. While the main effects of genetic liability and adoptive mothers’ responsiveness did not attain statistical significance, their interaction was significant even after controlling for baseline levels of child fussiness. Compared to children without genetic risk for depression, children who were predisposed with genetic liability for depression were likely to develop increased levels of fussy, emotionally charged behavior when adoptive mothers provided a caregiving environment characterized by low levels of responsiveness. Children with genetic liability for depression, when provided with highly responsive caregiving at 9 months of age, demonstrated decreasing levels of fussiness at 18 months. For children without genetic risk, maternal responsiveness was not related to the development of child fussiness. A similar, but statistically nonsignificant pattern was observed for the moderation of genetic risk by adoptive fathers’ responsiveness.
The finding of the interaction between genetic liability and parental socialization is consonant with Eisenberg’s (2006) view that “one process does not fit all.” Children with different temperaments and predispositions appear to need different forms of parenting to effectively promote healthy development (Rothbart & Bates, 1998). Consistent with research conducted during infancy on disruptive problem behavior (Martin, 1981; Shaw, Keenan, & Vondra, 1994; Shaw et al., 1998), the current report suggests that maternal responsiveness is a particularly important environmental factor for preventing less optimal developmental pathways for children, and in this case specifically for children with a genetic risk for depression. Plausibly, parents’ keen awareness of the child’s needs, and prompt, warm, and positive responses may be particularly helpful to manage and soothe children who are predisposed to be easily distressed. This finding is consistent with a general proposition of the interaction between genotype and environment: A richer environment could compensate genetic liability whereas a poorer environment could trigger genetic diathesis (Moffitt, Caspi, & Rutter, 2005; Shannahan & Hofer, 2005).
We also found that adoptive mothers’ self-reported depressive symptoms were prospectively associated with fussiness of the child, as reported by the adoptive father. Our finding concurs with a voluminous body of research on maternal depression (see Goodman & Gotlib, 1999 for a review), indicating its risk for offspring’s development. However, it is worth noting that unlike traditional studies of maternal depression based on a sample of birth mothers and their offspring, the observed effect for maternal depressive symptoms in this report represents an environmental liability, not confounded by genetic interpretation. As such, the current finding extends prior research by suggesting that the presence of a depressed mother at home is an important environmental influence during early childhood. Prior analyses with the current sample indicated both main and interactive effects of adoptive mother depression/anxiety on a distinct variable—infant attention to frustration—further suggesting the centrality of maternal depression on outcomes during infancy and toddlerhood (Leve et al., in press). The environmental component of risks associated with maternal depression has also been recently reported in an adoption study of adolescents (Tully, Iacono, & McGue, 2008). Nevertheless, the mechanism through which maternal depression is environmentally transmitted to offspring’s fussiness requires further investigation. As described in previous literature, potential explanatory environmental factors include disturbed parenting, contextual adversity, and exposure to maladaptive repertoire of maternal behavior, affect, and cognition (see Downey & Coyne, 1990; Goodman & Gotlib, 1999, for reviews). Continued research is encouraged to examine environmental factors in explaining the intergenerational transmission of emotional problems.
Adoptive fathers’ depressive symptoms, unlike that of adoptive mothers, were not a significant predictor of children’s later fussiness after adjusting for shared method variance. Prior studies indicate that paternal depression is a risk factor for children’s internalizing and externalizing psychopathology (Kane & Garber, 2004; Phares & Compas, 1992). However, the little influence of paternal depression in this report echoes a recent finding in 3-year olds (Meadows, McLanahan, & Brooks-Gunn, 2007) and in adopted adolescents (Tully et al., 2008). Specifically, Meadows et al. (2007) found that paternal internalizing disorder (depression/anxiety) was not as influential as maternal psychiatric disorder in predicting emotional and behavioral problems in 3-year olds. Similarly, Tully et al. (2008) recently reported in their study of adoptive families that maternal major depression was found to be an environmental liability for children’s psychopathology, but paternal major depression was not. The question of why maternal depression, not paternal depression, exerted significant influences on children’s emotional development remains an important topic of investigation. The differential impact of maternal and paternal depression may be explained by higher negativity in parent-child interactions in families with a depressed mother in comparison to families with a depressed father (Jacob & Johnson, 1997). The finding may also reflect the differences in the amount of time mothers and fathers spend with children during early childhood. The time young children (between the ages of 0 to 2) spend with their fathers is 60% and 80% that of mothers on weekdays and weekends, respectively (Yeung, Sandberg, Davis-Kean, & Hofferth, 2001). The etiology of the differential impact of maternal and paternal depression also warrants further attention.
Credence of the findings in this report is enhanced by several methodological strengths of the study. Most importantly, the adoption design is useful because, unlike in traditional family study designs whereby a child and his/her biological mother are recruited from the same family, it can maximally tease apart nature and nurture aspects of familial aggregation of psychopathology; genetic liability can be inferred from birth mothers and environmental contributions from adoptive parent(s) (Rutter et al., 2001). We further sought to establish a clearer separation of nature and nurture by adopting three methodological strategies: (a) recruiting the sample of adoptees who were placed at birth, (b) including assessments of openness in adoption as a covariate to further statistically control any post-adoption contact between adoptive and birth parents, and (c) assessing birth mothers’ substance use during pregnancy to approximate and statistically account for the possible intrauterine environmental risk. In addition, the longitudinal design, although does not offer causality, yields more definitive logical basis for inferring what would likely happen later when children with differing levels of genetic liability are provided with varying levels of responsive caregiving environments. Nevertheless, because evidence of moderation of genetic liability by environment in a longitudinal behavioral genetic design is rare, replication is certainly needed. Finally, this study used the mismatched informant design to address the issue of shared method variance. We used four reporters (birth mother, adoptive mother, adoptive father, and interviewer) and created a design whereby no informant reported both the criterion and the predictor variables of substantive interest. These methodological approaches provided an opportunity to conservatively test how genotype and environment jointly constitute the underpinnings of intergenerational transmission of depression.
Limitations and Future Directions
Some caveats of the study need to be noted. First, genetic liability is inferred from the phenotype of biological mothers. The major limitation of this approach is that it is not entirely certain whether the birth mother’s genotypes that are expressed in their phenotype were in fact genetically inherited by the child. Although depression has been convincingly shown to have a heritable component (McGuffin & Katz, 1989), this estimation strategy cannot guarantee that a heritable trait from the maternal side is in fact genetically transmitted to the child. Furthermore, environmental interventions such as pharmaceutical treatments for depression may inhibit potential expression of genetic risk in birth mothers’ phenotypes. One solution would be to assess candidate genes, but the hunt for specific genes that are linked to specific phenotypes in humans appears to only account for small amount of variance in outcomes (Plomin & McGuffin, 2003). Even if a candidate gene is identified, it is not warranted that “liability” associated with the gene is passed on to offspring. Theories and studies of developmental epigenetics argue that most phenotypes appear to involve complex interactions and sequences of multiple genes, neural activities, and environments (e.g., Gottlieb, 1998, 2007; Philibert et al., 2008). In addition, genetic risk inferred in this study may well be underestimated because it was based on the diagnostics from one parent only. Although we believe that findings based on inferred genetic effect are not trivial in understanding a piece of complex interplay between genes and environment, readers are repeatedly reminded that the relationship between genetic risk for MDD and child emotional development is highly complex.
Second, presence or absence of birth mothers’ lifetime MDD was determined during the T2 assessment. However, the sample of birth mothers varied widely in their age (ranged from 16 to 44 years of age), inevitably weighting the likelihood of being diagnosed with lifetime MDD higher for older birth mothers than younger mothers. Although we included birth mothers’ age in the models to at least statistically account for this issue, readers should cautiously interpret the results. A third limitation, generic to adoption designs, involves the effects of the intrauterine environment. Although we included birth mothers’ substance use during pregnancy to approximate intrauterine exposure to substances, there are other possible intrauterine effects that may be relevant for the development of emotional distress. For instance, maternal prenatal anxiety has been linked to children’s emotional problems (O'Connor, Heron, Golding, Beveridge, & Glover, 2002) and associated physiological functioning (e.g., hypothalamus-pituitary-adrenal axis; O’Connor et al., 2005).
Fourth, this study broadly assessed components of parental responsiveness via interviewer ratings on a standardized measure after a 2 ½ hour home visit. However, parental responsiveness is a multidimensional, complex construct encompassing factors such as response contingency, emotional-affective support, scaffolding of infant attention, and language input, and each aspect is known to have related yet distinct functioning in supporting child development (Landry et al., 2006). Readers are also reminded that the alphas for the responsiveness scale were lower than optimal and that the scale was negatively skewed. Moreover, developmental consideration of parental responsiveness requires researchers’ attention to children’s changing needs as they develop. With an increasing physical, cognitive, and emotional capacity, children’s needs change rapidly in the first two years of their lives. Responsive parental behaviors that were needed at earlier points of the child’s life may no longer be appropriate as the child grows. Future studies are needed to examine how parents respond to the child’s changing needs over time.
Fifth, while distressed, emotionally charged behavior in infancy has been linked to later emotional problems (Rende, 1993), it is also associated with a variety of behavioral syndromes, including externalizing problems (Bates, Maslin, & Frankel, 1985; Sanson, Oberklaid, Pedlow, & Prior, 1991; Shaw, Owen, Vondra, Keenan, & Winslow, 1996). Therefore, infant fussiness may not necessarily be the most specific precursor of child-onset depression. Finally, it is important to note that the observed effects were small. However, dismissing small effects as trivial could be erroneous given the complexity of human behavior (Ahadi & Diener, 1989).
These limitations notwithstanding, the current investigation underscores the importance of the interplay between genetic and environmental aspects of maternal depression that affect changes in young children’s emotional experiences. Maternal depression appears to be both environmental and genetic risk factor for increases in offspring’s fussy, emotionally charged behavior, particularly when offspring is devoid of a responsive caregiving environment. However, when the caregiving context is contingently responsive to children’s needs and cues, increases in children’s levels of fussiness are likely to be reduced. Given that the current findings highlight the important role of environmental influences in maternal depression and responsiveness, the results generated from this study have broader significance to future intervention; interventions that are designed to improve maternal depression and positive parenting (e.g., parental responsiveness) may be an effective way to reduce children’s distress. This suggestion echoes a finding from a recent report showing that such an applied effort can be successful in reducing young children’s internalizing and externalizing problems (Shaw, Connell, Dishion, Wilson, & Gardner, 2009).
In summary, the findings from this report shed new light on potential mechanisms underlying the familial aggregation of emotional problems: maternal depression might affect offspring’s early development through (a) genetic liability of depression accentuated by unresponsive caregiving environment, and (b) the environmental effect of being exposed to maternal depression. Such an intricate interaction between genotype and environment appears to partially explain why emotional problems tend to cluster in some families of depressed parents but not others.
Acknowledgments
This project was supported by grant R01 HD042608, NICHD, NIDA, and the Office of the Director, NIH, U.S. PHS (PI Years 1–5: David Reiss, MD; PI Years 6–10: Leslie Leve, PhD). The writing of this manuscript was partially supported by P30 DA023920, NIDA, NIH, U.S. PHS. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health.
We would like to thank the birth and adoptive parents who participated in this study and the adoption agencies who helped with the recruitment of study participants. Special gratitude is given to Remi Cadoret and Beverly Fagot who were centrally involved in this work prior to their deaths. In addition, we hold sincere respect and admiration for the contributions of Xiaojia Ge to this project. Dr. Ge was instrumental in the development of this study, and was an integral contributor to this manuscript.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA Prescool Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2000. [Google Scholar]
- Ahadi S, Diener E. Multiple determinants and effect size. Journal of Personality and social Psychology. 1989;56:398–406. doi: 10.1037//0022-3514.56.3.317. [DOI] [PubMed] [Google Scholar]
- Ainsworth M, Blehar M, Waters E, Walls S. Patterns of attachment: A psychological study of the Strange Situation. Hillsdale, NJ: Erlbaum; 1978. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorder (DSM-VI) 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Andrews G, Peters L. The psychometric properties of the Composite International Diagnostic Interview. Social Psychiatry Psychiatric Epidemiology. 1998;33(2):80–88. doi: 10.1007/s001270050026. [DOI] [PubMed] [Google Scholar]
- Bank L, Dishion TJ, Skinner M, Patterson GR. Method variance in structural equation modeling: Living with "glop". In: Patterson GR, editor. Aggression and depression in family interactions. Hillsdale, NJ: Erlbaum; 1990. pp. 247–280. [Google Scholar]
- Barry RA, Kochanska G, Philibert RA. GxE interaction in the organization of attachment: mothers' responsiveness as a moderator of children's genotypes. Journal of Child Psychology and Psychiatry. 2008;49:1313–1320. doi: 10.1111/j.1469-7610.2008.01935.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates JE, Freeland CB, Lounsbury ML. Measurement of infant difficulties. Child Development. 1979;50:794–803. [PubMed] [Google Scholar]
- Bates JE, Maslin C, Frankel K. Attachment security, mother-child interaction, and temperament as predictors of behavior-problem ratings at age 3 year. In: Bretherington I, Waters E, editors. Growing points of attachment theory and research. 1985. [PubMed] [Google Scholar]
- Beck A, Steer R. Beck Depression Inventory Manual. San Antonio, TX: The Psychological Corporation Barcourt Brace Jovanovich, Inc; 1993. [Google Scholar]
- Bornstein MH, Tamis-LeMonda CS. Maternal responsiveness and cognitive development in children. In: Bornstein MH, editor. Maternal responsiveness: Characteristics and consequences. San Francisco: Jossy-Bass; 1989. pp. 49–61. [DOI] [PubMed] [Google Scholar]
- Bradley RH, Caldwell BM, Rock S. Home environment and school performance: A ten year follow-up and examination of three models of environmental action. Child Development. 1988;59:852–867. doi: 10.1111/j.1467-8624.1988.tb03239.x. [DOI] [PubMed] [Google Scholar]
- Caldwell BM, Bradley RH. Administration manual, revisited edition: The Home Observation for Measurement of the Environment. Little Rock, AR: University of Arkansas; 1984. [Google Scholar]
- Campbell SB, Cohn JF, Meyers T. Depression in first-time mothers: Mother-infant interaction and depression chronicity. Developmental Psychology. 1995;31:349–357. [Google Scholar]
- Caspi A, Henry B, McGee RO, Moffitt TE, Silva PA. Temperamental origins of child and adolescent behavior problems: From age three to age fifteen. Child Development. 1995;66:55–68. doi: 10.1111/j.1467-8624.1995.tb00855.x. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Thornton A, Freedman D, Arnell JW, Harrington H, et al. The life history calendar: A research and clinical assessment method for collecting retrospective event-history data. International Journal of Methods in Psychiatric Research. 1996;6(2):101–114. [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression : Moderation by a polymorphism in the 5-HTTgene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. Maternal depressive disorder and contextual risk: Contributions to the development of attachment insecurity and behavior problems in toddlerhood. Development and Psychopathology. 1998;10:283–300. doi: 10.1017/s0954579498001618. [DOI] [PubMed] [Google Scholar]
- Crockenberg SC, Leerkes E. Infant and maternal behavior moderate reactivity to novelty to predict anxious behavior at 2.5 years. Development and Psychopathology. 2006;18:17–34. doi: 10.1017/S0954579406060020. [DOI] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Eaves LJ, Silberg J, Erkanli A. Resolving multiple epigenetic pathways to adolescent depression. Journal of Child Psychology and Psychiatry. 2003;44:1006–1014. doi: 10.1111/1469-7610.00185. [DOI] [PubMed] [Google Scholar]
- Eisenberg N. Introduction. In: Damon W, Lerner RM, editors. Handbook of child development: Social, emotional, and personality development. 6th ed. Vol. 3. New York: Wiley; 2006. pp. 1–23. [Google Scholar]
- Feldman R, Greenbaum CW, Yirmiya N. Mother-infant affect synchrony as an antecedent of the emergence of self-control. Developmental Psychology. 1999;35:223–231. doi: 10.1037//0012-1649.35.1.223. [DOI] [PubMed] [Google Scholar]
- Frendrich M, Warner V, Weissman MM. Family risk factors, parental depression, and psychopathology in offspring. Developmental Psychology. 1990;26:40–50. [Google Scholar]
- Ge X, Natsuaki MN, Martin D, Leve LD, Neiderhiser JM, Shaw DS, et al. Bridging the divide: Openness in adoption and post-adoption psychological adjustment. Journal of Family Psychology. 2008;22:52–540. doi: 10.1037/a0012817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gloggler B, Pauli-Pott U. Different fear-regulation behaviors in toddlerhood: Relations to preceding infant negative emotionality, maternal depression, and sensitivity. Merrill-Palmer Quarterly. 2008;54:86–101. [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106(3):458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Gotlib IH. Perception and recall of interpersonal feedback: Negative bias in depression. Cognitive therapy and research. 1983;7(5):399–412. [Google Scholar]
- Gottlieb G. Normally occuring environmental and behavioral influences on gene activities: From central dogma to probabilistic epigenesis. Psychological Review. 1998;105:792–802. doi: 10.1037/0033-295x.105.4.792-802. [DOI] [PubMed] [Google Scholar]
- Gottlieb G. Probablistic epigenesis. Developmental Science. 2007;10:1–11. doi: 10.1111/j.1467-7687.2007.00556.x. [DOI] [PubMed] [Google Scholar]
- Hammen C. Depression runs in families: The social context of risk and resilience in children of depressed mothers. New York: Springer-Verlag; 1991. [Google Scholar]
- Jacob T, Johnson SL. Parent-child interaction among depressed fathers and mothers: Impact on child functioning. Journal of Family Psychology. 1997;11:391–409. [PubMed] [Google Scholar]
- Kane P, Garber J. The relations among depression in fathers, children's psychopathology, and father-child conflict: A meta-analysis. Clinical Psychology Review. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Yang B, Douglas-Palumberi H, Houshyar S, Lipschitz D, Krystal JH, et al. Social supports and serotonin transporter gene moderate depression in maltreated children. Proceedings of the National Academy of Sciences of the United States of America. 2004;101:17316–17321. doi: 10.1073/pnas.0404376101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Kendler KS, Walters EE, MacLean C, Neale MC, Heath AC, et al. Stressful life events, genetic liability, and onset of an episode of major depression in women. American Journal of Psychiatry. 1995;152:833–842. doi: 10.1176/ajp.152.6.833. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) The International Journal of Methods in Psychiatric Research. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Moffitt TE, Taylor A, Pawlby SJ, Caspi A. Maternal depression and children's antisocial behavior. Archives of General Psychiatry. 2005;62:173–181. doi: 10.1001/archpsyc.62.2.173. [DOI] [PubMed] [Google Scholar]
- Kochanska G. Children's temperament, mothers' discipline, and security of attachment: Multiple pathways to emerging internalization. Child Development. 1995;66:597–615. [Google Scholar]
- Kochanska G, Aksan N, Joy ME. Children's fearfulness as a moderator of parenting in early socialization: Two longitudinal studies. Developmental Psychology. 2007;43(4):222–237. doi: 10.1037/0012-1649.43.1.222. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Measelle JR, Ablow JC, Essex MJ, Boyce WT, Kupfer DJ. A new approach to integrating data from multiple informants in psychiatric assessment and research: Mixing and matching contexts and perspectives. American Journal of Psychiatry. 2003;160:1566–1577. doi: 10.1176/appi.ajp.160.9.1566. [DOI] [PubMed] [Google Scholar]
- Landry SH, Smith KE, Miller-Loncar CL, Swank PR. Predicting cognitive-linguistic and social growth curves from early maternal behaviors in children at varying degrees of biological risk. Developmental Psychology. 1997;33:1040–1053. doi: 10.1037//0012-1649.33.6.1040. [DOI] [PubMed] [Google Scholar]
- Landry SH, Smith KE, Swank PR. Responsive parenting: Establishing early foundations for social communication, and independent problem-solving skills. Developmental Psychology. 2006;42:627–642. doi: 10.1037/0012-1649.42.4.627. [DOI] [PubMed] [Google Scholar]
- Landry SH, Smith KE, Swank PR, Assel MA, Vellet S. Does early responsive parenting have a special importance for children's development or is consistency across early childhood necessary? Developmental Psychology. 2001;37(3):387–403. doi: 10.1037//0012-1649.37.3.387. [DOI] [PubMed] [Google Scholar]
- Leve LD, Kerr DCR, Shaw DS, Ge X, Neiderhiser JM, Scaramella LV, et al. Infant pathways to externalizing behavior: Evidence of genotype × environment interactions. Child Development. doi: 10.1111/j.1467-8624.2009.01398.x. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Neiderhiser JM, Ge X, Scaramella LV, Conger RD, Reid JB, et al. The Early Growth and Development Study: A prospective adoption design. Twin Research and Human Genetics. 2007;10:84–95. doi: 10.1375/twin.10.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin J. A longitudinal study of the consequences of early mother-infant interaction: A microanalytic approach. Monographs of the Society for Research in Child Development. 1981;46 [Google Scholar]
- McGuffin P, Katz R. The genetics of depression and manic depressive disorder. British Journal of Psychiatry. 1989;155:294–304. doi: 10.1192/bjp.155.3.294. [DOI] [PubMed] [Google Scholar]
- Meadows SO, McLanahan SS, Brooks-Gunn J. Parental depression and anxiety and early childhood behaivor problems across family types. Journal of Marriage and the Family. 2007;52:1162–1177. [Google Scholar]
- Mills-Koonce WR, Propper CB, Gariepy JL, Blair C, Garrett-Peters P, Cox MJ. Bidirectional genetic and environmental influences on mother and child behavior: The family system as the unit of analysis. Development and Psychopathology. 2007;19:1073–1087. doi: 10.1017/S0954579407000545. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Rutter M. Strategy for investigating interactions between measured genes and measured environments. Archives of General Psychiatry. 2005;62:473–481. doi: 10.1001/archpsyc.62.5.473. [DOI] [PubMed] [Google Scholar]
- Moggs K, Bradley BP, Williams R. Attentional bias in anxiety and depression: The role of awareness. British Journal of Clinical Psychology. 1995;34:17–36. doi: 10.1111/j.2044-8260.1995.tb01434.x. [DOI] [PubMed] [Google Scholar]
- O'Connor TG, Ben-Shlomo Y, Heron J, Golding J, Adams D, Glover V. Prenatal anxiety predicts individual differences in cortisol in pre-adolescent children. Biological Psychiatry. 2005;58:211–217. doi: 10.1016/j.biopsych.2005.03.032. [DOI] [PubMed] [Google Scholar]
- O'Connor TG, Heron J, Golding J, Beveridge M, Glover V. Maternal antenatal anxiety and children's behavioural/emotional problems at 4 years. British Journal of Psychiatry. 2002;180:502–508. doi: 10.1192/bjp.180.6.502. [DOI] [PubMed] [Google Scholar]
- Partridge T, Lerner JV. A latent growth-curve approach to difficult temperament. Infant and Child Development. 2007;16:255–265. [Google Scholar]
- Phares V, Compas B. The role of fathers in child and adolescent psychopathology: Make a room for daddy. Psychological Bulletin. 1992;111:387–412. doi: 10.1037/0033-2909.111.3.387. [DOI] [PubMed] [Google Scholar]
- Philibert RA, Sandhu H, Hollenbeck N, Gunter T, Adams W, Madan A. The relationship of 5Htt(SLC6A4) methylation and genotype on mRNA expression and liability to major depression and alcohol dependence in subjects from the Iowa Adoption Studies. American Journal of Medical Genetics Part B. 2008;147B:543–549. doi: 10.1002/ajmg.b.30657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plomin R, McGuffin P. Psychopathology in the postgenomic era. Annual Review of Psychology. 2003;54:205–228. doi: 10.1146/annurev.psych.54.101601.145108. [DOI] [PubMed] [Google Scholar]
- Rende RD. Longitudinal relations between temperament traits and behaivoral syndromes in middle childhood. Journal of American Academy of Child and Adolescent Psychiatry. 1993;32:287–290. doi: 10.1097/00004583-199303000-00008. [DOI] [PubMed] [Google Scholar]
- Rice F, Harold GT, Shelton KH, Thaper A. Family conflict interacts with genetic liability in predicting childhood and adolescent depression. Journal of American Academy of Child and Adolescent Psychiatry. 2006;45:841–848. doi: 10.1097/01.chi.0000219834.08602.44. [DOI] [PubMed] [Google Scholar]
- Riese ML. Temperament stability between the neonatal period and 24 months. Developmental Psychology. 1987;23:216–222. [Google Scholar]
- Rothbart MK, Bates JE. Temperament. In: Damon W, Eisenberg N, editors. Handbook of child psychology: Social, emotional, and personality development. 5th ed. Vol. 3. New York: John Wiley & Sons, Inc; 1998. pp. 105–176. [Google Scholar]
- Rutter M, Pickles A, Murray R, Eaves LJ. Testing hypotheses on specific environmental causal effects on behavior. Psychological Bulletin. 2001;127(3):291–324. doi: 10.1037/0033-2909.127.3.291. [DOI] [PubMed] [Google Scholar]
- Sanson A, Oberklaid F, Pedlow R, Prior M. Risk indicators: Assessment of infancy predictors of pre-school behavioural maladjustment. Journal of Child Psychology and Psychiatry. 1991;32:609–626. doi: 10.1111/j.1469-7610.1991.tb00338.x. [DOI] [PubMed] [Google Scholar]
- Shannahan M, Hofer SM. Social context in gene-environment interactions: Retrospect and prospect. Journals of Gerontology. 2005;60B:65–76. doi: 10.1093/geronb/60.special_issue_1.65. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, Gardner F. Improvements in maternal depression as a mediator of intervention effects on early childhood problem behaivor. Development and Psychopathology. 2009;21:417–439. doi: 10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Keenan K, Vondra JI. Developmental precursors of externalizing behavior: Ages 1 to 3. Developmental Psychology. 1994;30:355–364. [Google Scholar]
- Shaw DS, Owen EB, Vondra JI, Keenan K, Winslow EB. Early risk factors and pathways in the development of early disruptive behavior problems. Development and Psychopathology. 1996;8:679–699. [Google Scholar]
- Shaw DS, Winslow EB, Owen EB, Vondra JI, Cohn JF, Bell RQ. The development of early externalizing problems among children from low-income families: A transformational perspective. Journal of Abnormal Child Psychology. 1998;26:95–107. doi: 10.1023/a:1022665704584. [DOI] [PubMed] [Google Scholar]
- Silberg J, Febo San Miguel V, Murrelle EL, Prom E, Bates JE, Canino G, et al. Genetic and environmental influences on temperament in the first year of life: The Puerto Rico Infant Twin Study (PRINTS) Twin Research and Human Genetics. 2005;8:328–336. doi: 10.1375/1832427054936808. [DOI] [PubMed] [Google Scholar]
- Silberg J, Rutter M, Neale MC, Eaves LJ. Genetic moderation of environmental risk for depression and anxiety in adolescent girls. British Journal of Psychiatry. 2001;179:116–121. doi: 10.1192/bjp.179.2.116. [DOI] [PubMed] [Google Scholar]
- Sternberg CR, Campos JJ. The development of anger expressions in infancy. In: Stein NL, Leventhal B, Trabasso T, editors. Psychological and biological approaches to emotion. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1990. pp. 247–282. [Google Scholar]
- Tully EC, Iacono WG, McGue M. An adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. American Journal of Psychiatry. 2008;165:1148–1154. doi: 10.1176/appi.ajp.2008.07091438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Boom DC. Do first-year intervention effects endure? Follow-up during toddlerhood of a sample of Dutch irritable infants. Child Development. 1995;66:1798–1816. [PubMed] [Google Scholar]
- Wakshlag LS, Hans SL. Relation of maternal responsiveness during infancy to the development of behavioral problems in high risk youth. Developmental Psychology. 1999;31:147–169. doi: 10.1037//0012-1649.35.2.569. [DOI] [PubMed] [Google Scholar]
- Weinberg MK, Tronick E. Emotional characteristics of infants associated with maternal depression and anxiety. Pediatrics. 1998;102(5):1298–1304. [PubMed] [Google Scholar]
- World Health Organization. Geneva: World Health Organization; The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. 1992
- World Health Organization. Geneva: World Health Organization; The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. 1993
- Yeung WJ, Sandberg JF, Davis-Kean PE, Hofferth SL. Children's time with fathers in intact families. Journal of Marriage and the Family. 2001;63:136–154. [Google Scholar]
- Zeanah CH, Boris NW, Scheeringa MS. Psychopathology in infancy. Journal of Child Psychology and Psychiatry. 1997;38:81–99. doi: 10.1111/j.1469-7610.1997.tb01506.x. [DOI] [PubMed] [Google Scholar]
- Zimmermann P, Bruckl T, Lieb R, Nocon A, Ising M, Beesdo K, et al. The interplay of familial depression liability and adverse events in predicting the first onset of depression during a 10-year follow-up. Biological Psychiatry. 2008;63:406–414. doi: 10.1016/j.biopsych.2007.05.020. [DOI] [PubMed] [Google Scholar]