Abstract
Objectives. We examined whether racial disparities in stage-specific colorectal cancer survival changed between 1960 and 2005.
Methods. We used US Mortality Multiple-Cause-of-Death Data Files and intercensal estimates to calculate standardized mortality rates by gender and race from 1960 to 2005. We used Surveillance, Epidemiology, and End Results (SEER) data to estimate stage-specific colorectal cancer survival. To account for SEER sampling uncertainty, we used a bootstrap resampling procedure and fit a Cox proportional hazards model.
Results. Between 1960–2005, patterns of decline in mortality rate as a result of colorectal cancer differed greatly by gender and race: 54% reduction for White women, 14% reduction for Black women, 39% reduction for White men, and 28% increase for Black men. Blacks consistently experienced worse rates of stage-specific survival and life expectancy than did Whites for both genders, across all age groups, and for localized, regional, and distant stages of the disease.
Conclusions. The rates of stage-specific colorectal cancer survival differed among Blacks when compared with Whites during the 4-decade study period. Differences in stage-specific life expectancy were the result of differences in access to care or quality of care. More attention should be given to racial disparities in colorectal cancer management.
Although colorectal cancer mortality rates have declined since 1960, these declines have been uneven,1–3 and racial disparities in mortality rates have increased. Factors contributing to increased mortality rates among Blacks include racial differences in risk factors, prevention, detection, and treatment.4 Blacks receive less colorectal screening,5 and their cancer is detected at more advanced stages.6,7 Important differences exist in how colorectal cancer is detected, but not necessarily in how it is treated once detected. Significant improvements have occurred in colorectal cancer treatment through time, yet these improvements may not be distributed equally across all racial groups. Previous research has also found Black–White differences in stage-specific colorectal cancer survival rates, suggesting disparities in the management of cancer.8–10
In this article, we assessed whether differences in stage-specific colorectal cancer survival rates reflected racial differences over 4 decades. In doing so, we adjusted for differences in incidence and screening, focusing instead on the management of tumors once they are found. Racial disparities are likely a product of a broad set of social, biological, and environmental factors. By observing changes in stage-specific mortality over time, rather than statically at a cross-sectional moment, we may develop a better understanding of how these factors have contributed to increased racial disparities.
METHODS
To estimate overall colorectal cancer mortality rates, we used death counts from Mortality Multiple-Cause-of-Death Data Files, which contain information from US death certificates transmitted to the National Center for Health Statistics between 1960 and 2005. Pertinent information includes date of death, gender, race, age, and cause of death. We identified deaths from colon cancer and rectal cancer by International Classification of Diseases versions 7, 8, 9, and 10 coding. Large-scale assessments comparing hospital medical records and death certificates have found colorectal cancer death reporting to be highly accurate.11,12 We used decennial census counts and annual intercensal estimates of the study population by age, gender, and race to estimate exposure to the risk of death.
To estimate stage-specific colorectal cancer survival, we used the National Cancer Institute Surveillance, Epidemiology and End Results (SEER) database, the most comprehensive publicly available domestic cancer registry in the United States. The SEER Registry collects stage at diagnosis, age at diagnosis, cancer type and site, gender, race, and vital status. Among deceased persons listed in the SEER Registry, death may have occurred from colorectal cancer or any other cause of death. Using the SEER Registry 1973–2006 Limited-Use cancer data (updated April 15, 2009), we analyzed all cases of colorectal cancer. We used SEER Summary Staging (localized, regional, and distant) to categorize the extent of the disease.
Mortality rates were defined as the ratio of death counts to exposure by age, gender, race, and year. For each year, we calculated the crude colorectal cancer mortality rate and then standardized it to a common age composition (arbitrarily chosen as the White male age distribution in 1990) to allow comparison across gender, race, and time.13
We used the Kaplan–Meier method to estimate survival curves in order to compare observed survival between Blacks and Whites and among stages of colorectal cancer for a given gender and decade of diagnosis.
To account for sampling uncertainty in the SEER data, we applied the bootstrap resampling procedure. In 1000 random samples, original data were replaced to estimate confidence intervals in our outcomes of interest.14 The bootstrapped sample sizes were equal to the original sample size (NSEER = 536 277). For each bootstrapped sample, we fit a Cox proportional hazards model in which survival was a function of gender, race, age at diagnosis, stage at diagnosis, decade of diagnosis, and the statistical interaction of race and decade of diagnosis. We graphically and statistically tested the proportional hazards assumption and found no strong evidence in support of nonproportionality for the covariates specified, which suggests a Cox model as an appropriate model for these data. We used R version 2.9.2 (R Project for Statistical Computing; available at http://www.r-project.org) for all statistical analyses.
RESULTS
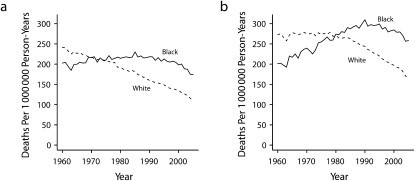
Figure 1 depicts overall colorectal cancer mortality rate trends and reveals 2 results. First, both White men and women historically experienced higher colorectal cancer mortality rates than did their Black counterparts. The racial crossover from higher to lower mortality rates occurred around 1970 for women and 1979 for men. Second, progress against overall colorectal cancer mortality in the last 45 years was not uniformly experienced by the entire population. White female colorectal cancer mortality rates steadily declined from 241 deaths per million person-years in 1960 to 111 deaths per million person-years in 2005, a 54% relative reduction. Yet, the decline for Black female colorectal cancer mortality was only 14%, from 203 deaths per million person-years in 1960 to 174 deaths per million person-years in 2005. For men, the differences were even more striking. Colorectal cancer mortality declined for White men from 273 deaths per million person-years in 1960 to 166 deaths per million person-years in 2005, a 39% relative decline. By contrast, Black male colorectal cancer mortality rates increased 28% from 201 deaths per million person-years in 1960 to 258 deaths per million person-years in 2005.
FIGURE 1.
Overall standardized colorectal cancer death rate for (a) women and (b) men: US Mortality Data Files and US intercensal estimates, 1960–2005.
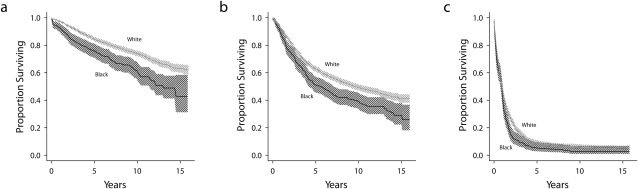
Stage-specific colorectal cancer survival rates were lower for Blacks than for Whites in each of the last 4 decades. Figure 2 shows, as an example, women aged 60–64 years who were entered into the SEER Registry during the 1990s. The survival rate of Black women who had localized and regional colorectal cancer was significantly lower compared with White women. For distant cancer, the survival rate among Blacks was significantly lower after 2 years. We found similar patterns in women and men aged 50 years and older in all 4 decades. In general, the hazard of death was greater for Blacks than for Whites for all age groups, all decades, and both genders.
FIGURE 2.
Observed stage-specific survival of women aged 60–64 years, by race, for (a) localized cancer, (b) regional cancer, and (c) distant cancer: National Cancer Institute Surveillance, Epidemiology, and End Results database, 1990–1999.
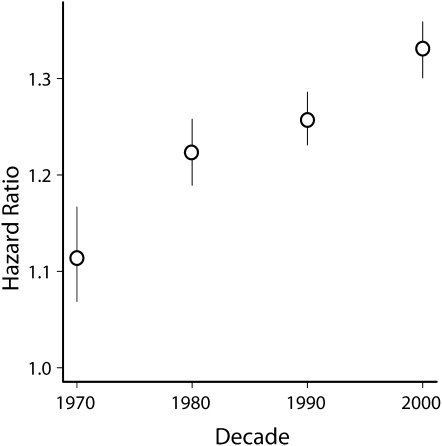
Hazard ratios (which reflect excess mortality of Blacks over Whites) increased across decades as shown in Figure 3. In other words, we found a positive interaction of race and time, which indicated worsening survival rates in stage-specific colorectal cancer for Blacks. In the 1970s, the hazard of death was 1.11 times greater (95% CI = 1.07, 1.17) for Black patients compared with White patients of the same age group, gender, and stage at diagnosis. The disparity increased consistently over the next 3 decades. The hazard of death for Black patients was 1.22 times greater (95% CI = 1.19,1.26) in the 1980s, 1.26 times greater (95% CI = 1.23, 1.29) in the 1990s, and 1.33 times greater (95% CI = 1.30, 1.36) in the 2000s compared with White patients of the same age group, gender, and stage at diagnosis. (Full model estimates and confidence intervals derived from bootstrap resampling are available in the Appendix, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 3.
Excess stage-specific colorectal cancer mortality over 4 decades among Blacks: 1970–2000.
Note. The 95% bootstrap confidence interval is shown as a vertical line, and the point estimate is shown as an open circle.
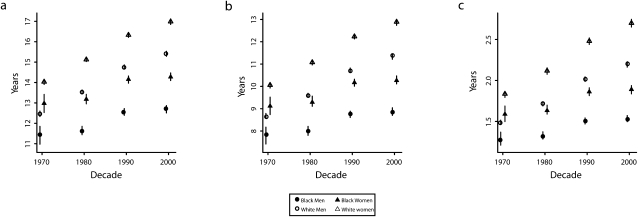
Figure 4 shows life expectancy differences for Blacks and Whites for the last 4 decades. The life expectancy for a 60-year-old, White male patient with localized colorectal cancer was 1.01 years greater (95% CI = 0.61, 1.49) than for similarly stratified Black patients in the 1970s. The gap widened to 1.91 years (95% CI = 1.68, 2.13) in the 1980s, to 2.18 years (95% CI = 2.01, 2.36) in the 1990s, and to 2.70 years (95% CI = 2.49, 2.91) in the 2000s. A similar pattern occurred for 60-year-old women. Widening Black–White disparities in life expectancy were also observed in regional and distant cases of colorectal cancer. Although the results are not shown, we found the same patterns for life expectancy starting at all other ages.
FIGURE 4.
Estimated life expectancy at age 60, by race and gender: 1970–2000.
Note. The 95% bootstrap confidence interval is shown as a vertical line. The point estimate is shown as an open circle for men and an open triangle for women. Death may occur from colorectal cancer or any other cause. The vertical scale of life expectancy differs by stage at diagnosis.
DISCUSSION
This study has 3 important findings. First, Black patients have consistently worse stage-specific colorectal cancer survival rates than White patients, an effect found for both men and women, across all age groups, and for localized, regional, and distant stages of the disease. Second, the gap between survival rates for Blacks and Whites is widening over time—an effect largely attributable to declining mortality among Whites over the past 4 decades but also to far less improvement in stage-specific survival rates for Blacks during the same period. Third, racial differences in stage-specific survival are associated with differences in life expectancy among Black and White colorectal cancer patients.
Our results are consistent with previous population-based and multiple institution-based studies that observed stage-specific racial disparities in colorectal cancer mortality for specific time periods. In their study of patients enrolled in the National Cancer Institute Black–White Cancer Survival Study, Mayberry and colleagues found the hazard of death for Blacks with colorectal cancer was 1.00–1.45 times higher than for Whites, conditional on age, gender, and cancer stage.15 In another study of the Pennsylvania tumor registry, Marcella and Miller found the hazard of death for Blacks was 1.19–1.40 times higher than for Whites, conditional on age, gender, and tumor characteristics.16 To our knowledge, our study is the first to demonstrate that the hazard of death for Blacks is growing over time, across both genders, and all disease stages.
The predominant and enduring trends in our analyses reveal substantial and increasing advantages in stage-specific colorectal cancer survival for Whites. Differences in stage-specific survival may result from differences in (1) accuracy of staging, (2) tumor biology, (3) competing mortality, or (4) treatment. First, if Black patients are more consistently understaged than White patients (for example, if tumors in Blacks are more likely to be classified as localized even though the tumors are in fact regional), those misclassifications could contribute to observed racial disparities in stage-specific survival. Second, if colorectal cancer among Black patients is more aggressive than among White patients, we would expect the racial differences in stage-specific survival that we observed; however, there appears to be strong evidence against such a possibility.5,17,18 Black patients are more likely than White patients to have more proximal colorectal tumors19 and to have proximal tumors present at more advanced stages,20 but these differences are generally attributed to differences in detection rather than biology. More generally, if biologic differences were to explain our findings, we would have to postulate that these biologic differences have been increasing in the last 4 decades to account for the widening disparity we observed over time. Third, competing mortality from comorbid conditions could contribute to observed differences in stage-specific survival rates. Differences in mortality rates between Blacks and Whites have generally increased through time, although there are exceptions such as deaths from influenza and pneumonia.21 We do not know whether Black colorectal cancer patients experience higher mortality from comorbid conditions as compared with that of similarly staged White patients. We observed a very small advantage in life expectancy among White patients who have distant metastatic colorectal cancer compared with similarly staged Black patients, which suggests there are not any large differences in competing mortality from comorbid conditions. A similar finding and conclusion were noted by Marcella and Miller.16 Fourth, differences in type of treatment recommended, completion of treatment, and post-treatment surveillance may be important factors contributing to rising stage-specific survival disparities.8,9,22 Survival differences may be further compounded by differences in the quality of the health care systems and providers treating Black and White patients. Hurley et al. argued that differences in access to and quality of health care for Blacks and Whites in general have increased considerably over time.23 More specific advances, such as the introduction of adjuvant chemotherapy, which gained widespread use in the early 1990s,24 may have diffused more rapidly among White populations than among Black populations.25 These lags would not explain the increasing differences before the 1990s, however. Several studies have demonstrated that Black and White patients are treated by different providers in the United States,26,27 and 1 study has extended this to differences in colorectal cancer treatment. In an analysis of patients in California who had stage 1–3 colorectal cancer, Black, Hispanic, and Asian patients and patients from neighborhoods with lower socioeconomic status were more likely to be treated in hospitals that had a record of higher mortality rates.28
Race itself may not drive the widening survival gap for stage-specific colorectal cancer. Rather, race likely serves as a confounding variable. Numerous literatures spanning sociology, economics, health policy, and medicine argue that race may be a proxy for income and wealth, educational attainment, employment, residential segregation, medical insurance, access to health care, characteristics of the hospital in which care occurs, home ownership, region of the country, and marital status. Stage-specific colorectal cancer survival may be more proximally related to these socioeconomic covariates, rather than to race. For example, Marcella and Miller found excess hazard of death among Blacks was reduced after adjusting for several socioeconomic characteristics and for stage, age, and gender.16
Racial and socioeconomic disparities in overall and stage-specific survival have also been observed in lung,29 breast,30 and cervical31 cancers. For example, Gadgeel and Kalemkerian found differences in overall lung cancer survival rates between Blacks and Whites. They argue that likely contributing factors include smaller declines in incidence for Black patients, a greater trend toward advanced stage disease, and worsening survival disparity.29 A similar pattern, driven by socioeconomic differences, is observed in cases of cervical cancer.31 The complex relationship between socioeconomic status and race and their effects on survival differs by cancer type. Hoffman and colleagues observe that although prostate cancer mortality among Blacks is much greater than among Whites, this difference attenuates considerably after adjusting for stage.32
One unexpected observation was the lower rate of colorectal cancer mortality among Blacks compared with Whites in the early years of this analysis. The reasons for this observed advantage among Blacks are unknown, yet are of great interest and warrant additional research. Miller and Cooper note a similar racial crossover pattern in lung cancer mortality rates between 1950 and 1977 for both men and women.33 Their analysis carefully considered the validity of national death data and attribution bias as possible explanations. Yet given the magnitude of the observed racial crossover, they argue that cigarette smoking, migration, and occupational patterns (especially industrial employment), as well as environmental factors, must also be leading contributing factors.
We acknowledge several limitations of our study. First, variability and biases in death certificate data, especially cause of death and age at death, may distort temporal patterns in mortality rates. Assessments that compare hospital diagnosis and cause of death listed on the death certificate have found detection and confirmation rates exceeding 93% for colorectal cancer.11,12 However, our results could be biased if the accuracy of assessments of cause of death varies by race or across decades. Second, the SEER Registry does not capture the entire US population. Our results may be biased to the extent that the SEER Registry fails to represent more general US trends. Third, because of the need to compare data from 1960 and later, we used the broader cancer stage categories of localized, regional, and distant rather than the more exact criteria of the American Joint Committee on Cancer. However, the broader categories remain clinically meaningful in predicting both treatment and outcome.
Our results suggest large and growing differences in stage-specific colorectal cancer mortality rates for Blacks and Whites. Because racial disparity is unlikely to be a product of differences in the accuracy of staging, tumor biology, or competing mortality, racial disparity seems most likely to be a product of differences in access to care or the quality of that care. The existence of racial differences in colorectal cancer management demands attention, and the increase of those disparities over the past several 4 decades should make this a priority.
Acknowledgments
We thank the Robert Wood Johnson Foundation Health & Society Scholars and Robert Wood Johnson Clinical Scholars programs for their financial support.
An earlier version of this work was presented at the Robert Wood Johnson Health & Society Scholars Annual meeting on May 14, 2009.
We thank Robert Aronowitz, Valerie Lewis, and Jason Schnittker for helpful comments and suggestions.
Human Participant Protection
The University of Pennsylvania institutional review board determined that this research met eligibility criteria for review exemption.
References
- 1.American Cancer Society Cancer Facts and Figures for African Americans 2007-2008. Atlanta: American Cancer Society; 2007 [Google Scholar]
- 2.Chu KC, Tarone RE, Chow W, Hankey BF, Ries LAG. Temporal patterns in colorectal cancer incidence, survival, and mortality from 1950 through 1990. J Natl Cancer Inst. 1994;86(13):997–1006 [DOI] [PubMed] [Google Scholar]
- 3.Irby K, Anderson WF, Henson DE, Devesa SS. Emerging and widening colorectal carcinoma disparities between blacks and whites in the United States (1975-2002). Cancer Epidemiol Biomarkers Prev. 2006;15(4):792–797 [DOI] [PubMed] [Google Scholar]
- 4.Wong M, Ettner S, Boscardin W, Shapiro M. The contribution of cancer incidence, stage at diagnosis and survival to racial differences in years of life expectancy. J Gen Intern Med. 2009;24(4):475–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97(6):1528–1540 [DOI] [PubMed] [Google Scholar]
- 6.Mandelblatt J, Andrews H, Kao R, Wallace R, Kerner J. The late-stage diagnosis of colorectal cancer: demographic and socioeconomic factors. Am J Public Health. 1996;86(12):1794–1797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen VW, Fenoglio-Preiser CM, Wu XC, et al. Aggressiveness of colon carcinoma in blacks and whites. National Cancer Institute Black/White Cancer Survival Study Group. Cancer Epidemiol Biomarkers Prev. 1997;6(12):1087–1093 [PubMed] [Google Scholar]
- 8.Polite BN, Dignam JJ, Olopade OI. Colorectal cancer and race: understanding the differences in outcomes between African Americans and whites. Med Clin North Am. 2005;89(4):771–793 [DOI] [PubMed] [Google Scholar]
- 9.Polite BN, Dignam JJ, Olopade OI. Colorectal cancer model of health disparities: understanding mortality differences in minority populations. J Clin Oncol. 2006;24(14):2179–2187 [DOI] [PubMed] [Google Scholar]
- 10.Demissie K. Racial differences in the treatment of colorectal cancer: a comparison of surgical and radiation therapy between whites and blacks. Ann Epidemiol. 2004;14(3):215–221 [DOI] [PubMed] [Google Scholar]
- 11.Percy C, Stanek E, Gloeckler L. Accuracy of cancer death certificates and its effect on cancer mortality statistics. Am J Public Health. 1981;71(3):242–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Percy CL, Miller BA, Gloeckler Ries LA. Effect of changes in cancer classification and the accuracy of cancer death certificates on trends in cancer mortality. Ann N Y Acad Sci. 1990;609(November):87–97, discussion 97–99 [DOI] [PubMed] [Google Scholar]
- 13.Preston SH, Heuveline P, Guillot M. Demography: Measuring and Modeling Population Processes. Oxford: Blackwell Publishers Ltd; 2001 [Google Scholar]
- 14.Efron B, Tibshirani R. An Introduction to the Bootstrap. 1st ed Boca Raton, FL: Chapman & Hall/CRC; 1994 [Google Scholar]
- 15.Mayberry RM, Coates RJ, Hill HA, et al. Determinants of black/white differences in colon cancer survival. J Natl Cancer Inst. 1995;87(22):1686–1693 [DOI] [PubMed] [Google Scholar]
- 16.Marcella S, Miller JE. Racial differences in colorectal cancer mortality. The importance of stage and socioeconomic status. J Clin Epidemiol. 2001;54(4):359–366 [DOI] [PubMed] [Google Scholar]
- 17.Coates RJ, Greenberg RS, Liu MT, et al. Anatomic site distribution of colon cancer by race and other colon cancer risk factors. Dis Colon Rectum. 1995;38(1):42–50 [DOI] [PubMed] [Google Scholar]
- 18.Devesa SS, Chow WH. Variation in colorectal cancer incidence in the United States by subsite of origin. Cancer. 1993;71(12):3819–3826 [DOI] [PubMed] [Google Scholar]
- 19.Wu XC, Chen VW, Steele B, et al. Subsite-specific incidence rate and stage of disease in colorectal cancer by race, gender, and age group in the United States, 1992-1997. Cancer. 2001;92(10):2547–2554 [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez E, Roetzheim R, Ferrante J, Campbell R. Predictors of proximal vs. distal colorectal cancers. Dis Colon Rectum. 2001;44(2):251–258 [DOI] [PubMed] [Google Scholar]
- 21.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff. 2005;24(2):325–334 [DOI] [PubMed] [Google Scholar]
- 22.Berry J, Bumpers K, Ogunlade V, et al. Examining racial disparities in colorectal cancer care. J Psychosoc Oncol. 2009;27(1):59–83 [DOI] [PubMed] [Google Scholar]
- 23.Hurley RE, Pham HH, Claxton G. A widening rift in access and quality: growing evidence of economic disparities. Health Aff (Millwood). 2005;Suppl Web Exclusives(W5):566–576 [DOI] [PubMed] [Google Scholar]
- 24.NIH Consensus Conference Adjuvant therapy for patients with colon and rectal cancer. JAMA. 264(11):1444–1450 [PubMed] [Google Scholar]
- 25.Potosky AL, Harlan LC, Kaplan RS, Johnson KA, Lynch CF. Age, sex, and racial differences in the use of standard adjuvant therapy for colorectal cancer. J Clin Oncol. 2002;20(5):1192–1202 [DOI] [PubMed] [Google Scholar]
- 26.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351(6):575–584 [DOI] [PubMed] [Google Scholar]
- 27.Kressin NR. Separate but not equal: the consequences of segregated health care. Circulation. 2005;112(17):2582–2584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang W, Ayanian JZ, Zaslavsky AM. Patient characteristics and hospital quality for colorectal cancer surgery. Int J Qual Health Care. 2007;19(1):11–20 [DOI] [PubMed] [Google Scholar]
- 29.Gadgeel SM, Kalemkerian GP. Racial differences in lung cancer. Cancer Metastasis Rev. 2003;22(1):39–46 [DOI] [PubMed] [Google Scholar]
- 30.Randolph WM, Goodwin JS, Mahnken JD, Freeman JL. Regular mammography use is associated with elimination of age-related disparities in size and stage of breast cancer at diagnosis. Ann Intern Med. 2002;137(10):783–790 [DOI] [PubMed] [Google Scholar]
- 31.Singh GK, Miller BA, Hankey BF, Edwards BK. Persistent area socioeconomic disparities in U.S. incidence of cervical cancer, mortality, stage, and survival, 1975-2000. Cancer. 2004;101(5):1051–1057 [DOI] [PubMed] [Google Scholar]
- 32.Hoffman RM, Gilliland FD, Eley JW, et al. Racial and ethnic differences in advanced-stage prostate cancer: the prostate cancer outcomes study. J Natl Cancer Inst. 2001;93(5):388–395 [DOI] [PubMed] [Google Scholar]
- 33.Miller WJ, Cooper R. Rising lung cancer death rates among black men: the importance of occupation and social class. J Natl Med Assoc. 1982;74(3):253–258 [PMC free article] [PubMed] [Google Scholar]