Abstract
AIM: To investigate the effect of curcumin on bacterial translocation and oxidative damage in an obstructive jaundice model and compare the results to glutamine, an agent known to be effective and clinically used.
METHODS: Twenty-four female Wistar-Albino rats, weighing 200-250 g, were randomly divided into three groups (8 in each group). After ligation of the common bile duct in all animals, Group I received oral normal saline, Group II received oral glutamine and Group III received oral curcumin for seven days. Blood samples via cardiac puncture, tissue samples (terminal ileum, liver and mesenteric lymph node) and peritoneal fluid were obtained from the animals at the time of death to investigate bacterial translocation and oxidative damage.
RESULTS: We observed that both glutamine and curcumin reduced bacterial translocation in blood, hepatocellular damage, plasma cytokine levels, oxidative tissue damage and apoptosis significantly compared to the control group. Additionally, glutamine showed protective effects on ileal epithelium and reduced villus atrophy.
CONCLUSION: On the basis of these findings, both curcumin and glutamine are thought to be effective in preventing or reducing bacterial translocation and oxidative damage in obstructive jaundice.
Keywords: Obstructive jaundice, Bacterial translocation, Oxidative damage, Glutamine, Curcumin
INTRODUCTION
Obstructive jaundice is characterized by a disability in the secretion of bile into the intestinal system, accumulation of toxic bile salts and bilirubin in the tissues and significant changes in systemic and hepatic functions[1]. Despite current modern diagnostic and therapeutic approaches, interventions in patients with biliary tract obstruction result in 10%-25% mortality and up to 56% major morbidity[2]. Biliary sepsis, wound infections, intra-abdominal abscess formation and renal failure are frequent complications in obstructive jaundice. Bacterial translocation and oxidative tissue damage have been emphasized as the leading causes of these complications in obstructive jaundice by numerous investigators[2-4]. Obstructive jaundice causes alterations leading to bacterial translocation both in the intestinal barrier and in the reticuloendothelial system. Some of these alterations may be listed as mucosal damage in the intestinal lumen due to lack of bile, apoptosis, bacterial overgrowth, motility disorder associated with oxidative stress and functional abnormalities in the tissue macrophages[2,5].
Glutamine, a non-essential amino acid, occupies a central role in numerous metabolic processes such as amino acid transport and nitrogen balance. It is the main energy source for rapidly proliferating cells such as enterocytes and lymphocytes. It has been reported not only to lower the rate of endotoxemia and translocation by preserving mucosal integrity but also to improve the immune system action against bacteria and endotoxins which succeed in passing the intestinal barrier[3,5-7].
Curcumin is a polyphenol derived from the herbal remedy and dietary spice turmeric. The antioxidant, anti-cancer, anti-inflammatory and cytoprotective effects of curcumin have been demonstrated by numerous experimental and clinical studies[8]. Gülçubuk et al[9] have declared that curcumin has positive effects on intestinal barrier function due to its anti-inflammatory properties and possibly can prevent bacterial translocation. We have previously shown positive effects of curcumin on oxidative damage and liver function in obstructive jaundice[10]. However, according to our knowledge, a comprehensive and comparative study regarding the effect of curcumin on bacterial translocation and oxidative damage in obstructive jaundice has not been performed yet.
The aim of this study was to compare the effects of curcumin with those of glutamine, a reliable control, on bacterial translocation and oxidative damage in an obstructive jaundice model and to evaluate the results with a review of the literature.
MATERIALS AND METHODS
Animals
Twenty-four healthy female rats weighing 200-250 g, housed in stainless steel cages under controlled temperature (22°C) and humidity and with 12-h dark/light cycles, were used in this study. Standard industrial rat feed containing 21% protein and fresh tap water were given ad libitum before and after operation. The experimental protocol was designed according to the ethical standards for animal use and approved by the local committee of animal use.
Surgical procedure and treatment
All procedures were performed under general anesthesia induced by intramuscular injections of ketamine hydrochloride 80 mg/kg (Ketalar flk; Pfizer, Istanbul, Turkey) plus 5 mg/kg xylazine (Rompun; Bayer, Istanbul, Turkey). The abdomen was shaved and soaked with Betadine solution. After a midline laparotomy of 1-2 cm, the common bile duct was identified, doubly ligated using 4/0 silk sutures and divided. Abdominal incisions were closed in two layers using 4/0 silk sutures. The animals were randomized into three groups (8 in each). Group I was treated with normal saline 1 cc orally once daily after bile duct ligation. Group II was treated with glutamine (Resource Glutamine powder 5 g; Nestle Health Care Nutrition, Germany) 200 mg/kg orally once daily after bile duct ligation. Group III was treated with curcumin (Curcumin from Curcuma longa; Sigma Aldrich, Germany) 20 mg/kg orally once daily after bile duct ligation. Animals were regularly nourished and maintained for 7 d as described above. Glutamine was dissolved in distilled water and the solution was stirred immediately before use. Curcumin was suspended in distilled water and the suspension was stirred immediately before use. The re-laparotomy was performed through the old incision on postoperative 8th day under general anesthesia and subjects were sacrificed. Systemic blood via cardiac puncture, peritoneal fluid and tissue (terminal ileum, liver and mesenteric lymph node) samples were obtained to investigate bacterial translocation and oxidative damage. All procedures were performed aseptically using sterile instruments.
Microbiological examination
Systemic blood samples obtained via cardiac puncture and peritoneal fluid samples were cultured aerobically using BacTec Peds (BioMérieux, Durham, USA). Blood cultures were continuously monitored for 7 d. Positive cultures were plated out on appropriate media and species identified by Sceptor microdilution and standard bacteriological techniques. The mesenteric lymph node, liver and terminal ileum samples were removed and placed in pre-weighed sterile glass bottles containing sterile pre-reduced brain-heart infusion. The bottles were re-weighed and tissue homogenates were prepared in 2-mL brain-heart infusions using sterile mortars and pestles. A portion (0.1 mL) of homogenates was cultured on blood agar, eosin methylene blue agar. All the plates were examined after 24 and 48 h of incubation at 37°C.
Biochemical examination
Systemic blood via cardiac puncture and tissue (terminal ileum) samples were obtained from rats for biochemical evaluation. Tissues were washed with physiological serum for biochemical analysis, weighed and homogenized using the method of Sier et al[11]. Serum levels of cytokines tumor necrosis factor-α (TNF-α) (pg/mL) and interleukin-6 (IL-6) (pg/mL) were measured by immunoenzymatic enzyme-linked immunosorbent assay method (Quantikine High Sensitivity Human by R&D Systems, USA) according to the manufacturer’s protocol. Minimum detectable concentrations were determined by the manufacturer to be 0.12 pg/mL and 0.03 pg/mL, respectively. Intra-assay (2.6 for TNF-α and 1.6 for IL-6) and inter-assay (14 for TNF-α and 6.4 for IL-6) precision performances of the assay were determined on 20 replicates from the quality control data of the laboratory. Malondialdehyde (MDA) was determined spectrophotometrically by the thiobarbituric acid method. Aliquots of 0.2 mL of serum were mixed thoroughly with 0.8 mL of phosphate-buffered saline (pH 7.4) and 25 μL of butylated hydroxytoluene solution. The samples were placed on ice for 2 h after addition of 0.5 mL of 30% trichloroacetic acid. Then, samples were centrifuged at 2000 g at 25°C for 15 min. After that, 1 mL of each supernatant was mixed with 0.075 mL of 0.1 mol/L ethylenediamine tetraacetic acid and 0.25 mL of 1% thiobarbituric acid in 0.05 mol/L sodium hydroxide (NaOH). Supernatant of each sample was kept in boiling water for 15 min and then cooled to room temperature. Finally, the absorbance of thiobarbituric acid reactive substances (TBARS) was measured at 532 nm. The data regarding TBARS were expressed in mDA, using a molar extinction coefficient for MDA of 1.56 × 105/cm per mol/L and the results were expressed in nmol/L (range: 0.1-2.5). Serum nitric oxide (NO) levels were measured with Griess reagent as previously described[12]. The first step is the conversion of nitrate using nitrate reductase. The second step is the addition of Griess reagent, which converts nitrite to a purple azocompound. Protein interference was avoided by treatment of the reacted samples with zinc sulphate and centrifugation for 5 min at 10 000 g; the azochromophore spectrophotometry was performed at 450 nm; sodium nitrate was used as the standard and results were expressed in mmol/L (range: 10-120 mmol/L). Myeloperoxidase (MPO) activity was measured as described previously[13]. In short, tissue homogenates were incubated with 0.5% hexadecyl-trimethylammonium bromide in 50 mol/L potassium phosphate buffer (pH 5.5), plus 0.026% ortho-dianisidine dihydrochloride substrate and 0.018% H2O2. The reaction kinetics were followed for 30 min at 450 nm in 96-well plates. The specificity of the reaction was checked with sodium azide (0.1 mmol/L). All samples were analyzed in duplicate and standardized using a homogenate of pooled human neutrophils, and MPO activity was expressed in arbitrary units (U/mg protein). The enzymatic activity of caspase-3 in tissue samples was measured as described previously[14]. Five 10 μm cryostat sections of tissues were suspended in a lysis buffer consisting of 10 mmol/L 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) (pH 7.0), 40 mmol/L β-glycerophosphate, 50 mmol/L NaCl, 2 mmol/L MgCl2 , and 5 mmol/L ethylene glycol tetraacetic acid. After 10 min on ice, the cells were disrupted by 10 s of sonification followed by four cycles of freezing and thawing and stored at -80°C. Protein concentration was determined using the method described by Bradford[15]. For measurement of caspase-3 enzymatic activity, samples containing 15 μg protein were incubated with 2.5 nmol of the enzyme substrates DEVD-AMC (7-Amino-4-methylcoumarin, N-acetyl-L-aspartyl-L-glutamyl-L-valyl-l-aspartic acid amide) in a 100 mmol/L HEPES buffer (pH 7.25) containing 10% (w/v) sucrose, 0.1% (v/v) NP40, and 10 mmol/L DL-Dithiothreitol. During incubation at 37°C, fluorescent AMC was cleaved off by active caspases, corresponding with the level of caspase activity in the sample. The fluorescent AMC was monitored at an excitation of 360 nm and emission of 460 nm using a FLUO star Optima plate reader. Calibration curves were constructed using free AMC. Caspase-3 activity was measured as pmolAMC/min per mg protein. Serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) activities were determined according to Reitman and Frankel[16], whereas alkaline phosphatase (ALP) activity was estimated by the Belfield method[17]. Total bilirubin, and γ-glutamyl transferase (GGT) were determined using Diamond Diagnostic Kit as reported[18]. The results were reported as mean and standard deviation.
Histopathological examination
Liver and a 2-cm segment of terminal ileum samples were obtained at the final laparotomy. The bowel was stripped from its mesentery and the segment was opened along its length and rinsed in a cold solution. Specimens were fixed in 10% formalin in 0.15 mol/L phosphate buffer (pH 7.2), embedded in paraffin and then sections measuring 5 μm in thickness were cut. The specimens were stained with hematoxylin-eosin and examined under the light microscope (Olympus BX50, Japan). Histopathological examination was performed by an experienced pathologist who was not aware of the sample group. Ductular proliferation in liver samples was examined according to the modified scoring system used by Sheen-Chen et al[3]. This system, assessing ductular proliferation with seven different scores, was reduced to three scores since it was more appropriate for statistical assessment and number of subjects was fewer. Grade 1 (mild): Portal area involvement less than 50%; Grade 2 (moderate): Portal area involvement more than 50% or expansion of the portal tract; Grade 3 (severe): Presence of bridging in portal tracts. Apoptosis was also assessed in liver samples and reported as present or absent. Villus structures (villus length and width), lymphatic dilatation and sub-epithelial edema were examined to investigate mucosal damage in terminal ileum sections and reported as present or absent.
Statistical analysis
Findings obtained in the study were assessed using SPSS (Statistical Package for Social Sciences) for Windows 15.0 program. One-way Anova test was used in comparing parameters between groups and Tukey’s HDS (Honestly Significant Difference) test was used in detecting the group causing variation when comparing qualitative data. Kruskal Wallis test was used in comparing parameters displaying abnormal distribution between groups and Mann Whitney U test was used in detecting the group causing variation. For comparison of qualitative data, χ2 or Fisher exact test was used. Results were calculated as mean ± SD. P < 0.05 values were considered statistically significant.
RESULTS
Jaundice became apparent in all subjects on postoperative day 3. Two of the rats (one in Group I and one in Group II) died during the experiment. The experiment was completed with 7 rats in Group I, 7 rats in Group II and 8 rats in Group III.
Microbiological findings
Significant microbial growth was investigated in blood obtained by intracardiac puncture, samples of mesenteric lymph nodes, peritoneal fluid, and terminal ileum tissue. Escherichia coli (E. coli) was the most common bacteria detected (34%) among all positive cultures. Other detected bacteria were identified as Enterococci, Klebsiella oxytoca, Streptococcus spp and Klebsiella pneumoniae. Positive blood cultures were detected in 6 of 7 animals (85%) in Group I, in 1 of 7 animals (14%) in Group II, and in 2 of 8 animals (25%) in Group III. The rates in groups II and III were determined to be significantly less than that of group I (P = 0.029 and P = 0.041, respectively). The difference between Groups II and III was not statistically significant (P > 0.05). Positive cultures of mesenteric lymph node samples were detected in all animals (100%) in Group I, in 3 of 7 animals (42%) in Group II and in 7 of 8 animals (87%) in Group III. There was no statistically significant difference among groups although positive cultures were fewer in Group II. Positive cultures of peritoneal fluids were detected in 4 of 7 animals (57%) in Group I, none of 7 animals (0%) in Group II and in 4 of 8 animals (50%) in Group III. These results were not statistically significantly different between groups (P > 0.05). Significant pathogens in terminal ileum samples were detected in all animals (100%) in Group I, in 5 of 7 animals (71%) in Group II and in 7 of 8 animals (87%) in Group III. These results were not statistically significant either (P > 0.05).
Biochemical findings
ALT, AST, ALP, GGT, total bilirubin, IL-6 and TNF-α levels were measured in blood samples. MPO, NO, MDA levels and caspase-3 activity were measured in terminal ileum samples (Table 1). There was no significant difference in terms of serum total bilirubin values among groups and obstructive jaundice was detected in all subjects. ALT and AST levels, markers of hepatocellular damage, in Group II were found to be significantly reduced compared to Group I and Group III (P = 0.002 and P = 0.001, respectively). Furthermore, these enzyme levels were found to be significantly reduced in Group III when compared with Group I (P = 0.001). ALP and GGT levels, markers of cholestasis, were found to be significantly lower (P < 0.05) in Groups III and II than in Group I. When the results of Groups II and III were compared, ALP levels were lower in Group II; whereas, GGT was found to be lower in Group III and these results were statistically significant (P < 0.05). TNF-α levels were detected to be significantly decreased in Group II when compared with Group I and Group II (P = 0.001 and P = 0.002, respectively). TNF-α levels detected in Group III were also significantly lower than that of Group I (P = 0.002). IL-6 levels detected in Group II were significantly less than those in Group I and Group III (P = 0.002 and P = 0.001, respectively). Although the results were lower in Group III they were not statistically significant when compared with Group I (P > 0.05). MPO levels, a marker of tissue inflammation and neutrophil sequestration, were found to be significantly lower in Group II than the other groups (P = 0.002 for Group I and P = 0.001 for Group III). MPO levels detected in Group III were also lower than that of Group I, which was statistically significant (P = 0.001). NO levels, an indicator of oxidative damage and MDA, an end product of lipid peroxidation and an index of oxidative stress, were determined to be significantly lower in Group II than the other groups (P < 0.05). Additionally, values detected in Group III were lower than those of Group I and this was also statistically significant (P < 0.05). Caspase-3 activity, an apoptosis marker, was found to be significantly lower in Group II than the other groups (P = 0.002 for Group I and P = 0.001 for Group III). The value detected in Group III was lower than that of Group I and this was also statistically significant (P = 0.001).
Table 1.
Biochemical results
|
mean ± SD |
P |
|||||
| Group I | Group II | Group III | Group I-II | Group I-III | Group II-III | |
| T-Bil bilirubin | 7.814 ± 0.855 | 7.303 ± 1.059 | 7.456 ± 1.037 | > 0.05 | > 0.05 | > 0.05 |
| ALT | 285.714 ± 6.945 | 203.157 ± 5.777 | 230.5 ± 7.368 | 0.002 | 0.001 | 0.001 |
| AST | 277.571 ± 8.6 | 188.714 ± 5.908 | 227.25 ± 7.573 | 0.002 | 0.001 | 0.001 |
| ALP | 417.714 ± 13.865 | 373.714 ± 9.322 | 353.938 ± 141.502 | 0.002 | 0.042 | 0.015 |
| GGT | 410.429 ± 5.711 | 395.857 ± 4.337 | 402.375 ± 4.926 | 0.002 | 0.010 | 0.040 |
| IL-6 | 1.087 ± 0.117 | 0.627 ± 0.147 | 0.984 ± 0.123 | 0.002 | 0.063 | 0.001 |
| TNF-α | 1.346 ± 0.21 | 0.53 ± 0.089 | 0.869 ± 0.104 | 0.002 | 0.002 | 0.001 |
| MPO | 0.537 ± 0.01 | 0.309 ± 0.038 | 0.468 ± 0.009 | 0.002 | 0.001 | 0.001 |
| NO | 149.286 ± 9.499 | 101.171 ± 3.396 | 135.625 ± 5.181 | 0.002 | 0.009 | 0.001 |
| MDA | 2.743 ± 0.196 | 1.753 ± 0.227 | 2.3 ± 0.379 | 0.002 | 0.011 | 0.015 |
| CAS | 35.741 ± 0.848 | 22.929 ± 1.533 | 30.445 ± 1.463 | 0.002 | 0.001 | 0.001 |
ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; ALP: Alkaline phosphatase; GGT: γ-glutamyltransferase; IL-6: interleukin-6; TNF-α: Tumor necrosis factor-α; MPO: Myeloperoxidase; NO: Nitric oxide; MDA: Malondialdehyde; CAS: Caspase 3 activity.
Histopathological findings
Ductal proliferation and apoptosis rates were measured in the histopathological evaluation of liver sections (Figure 1A). Regarding the former, 14% mild, 57% moderate and 29% severe ductal proliferation was detected in Group I, 43% mild, 14% moderate and 43% severe ductal proliferation was detected in Group II and 38% mild and 62% severe ductal proliferation was detected in Group III. Rates of apoptosis were determined to be 42% in Group I and Group II and 62% in Group III. No significant difference in terms of either ductal proliferation or apoptosis was found when the results of histopathological examination of liver samples were statistically compared among groups (P > 0.05). Villus height and width, lymphatic dilatation and subepithelial edema were evaluated in terminal ileum sections. When shortening in villus height was compared among groups, shortening in Group II was significantly less than Group I (P = 0.02). Shortening observed in Group II was less than that of Group III and shortening determined in Group III was less than that of Group I but these differences were not statistically significant (P > 0.05). In the comparison of villus width, no significant difference was detected among groups, although it was found less frequently in Group II (P > 0.05). Degree of lymphatic dilatation was observed to be significantly lower in Group II than that of Group I (P = 0.02). Lymphatic dilatation observed in Group II was less than that of Group III but this was not statistically significant. Lymphatic dilatation determined in Group III was less than that of Group I, but again this was not statistically significant (P > 0.05). No significant difference among groups in terms of subepithelial edema was detected (P > 0.05).
Figure 1.
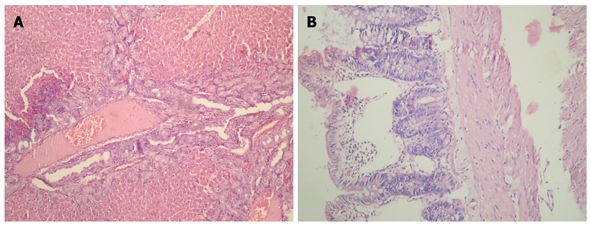
Histopathological view of liver and terminal ileum. A: Liver of a jaundiced rat, bridging of portal tracts, severe ductal proliferation, × 200; B: Terminal ileum of a jaundiced rat, shortening of villus length and severe lymphatic dilatation, × 200.
DISCUSSION
Bacterial translocation is the passage of bacteria or endotoxins from the gastrointestinal tract to extraintestinal sites, such as mesenteric lymph nodes, liver, spleen, and/or bloodstream. In a normal, healthy individual, gut-originated bacteremia and sepsis do not occur because the host has multiple defense mechanisms to prevent the bacteria and their products from crossing the mucosal barrier and spreading to systemic tissues. Under certain experimental and clinical circumstances, this intestinal barrier function becomes overwhelmed or impaired, resulting in bacterial translocation[19-21]. Current advances in the pathophysiology of intestinal failure in obstructive jaundice have shown that the breakdown of the gut barrier is multifactorial, involving disruption of immunologic, biological, mechanical, and biochemical barriers. Berg and Garlington[22] defined bacterial translocation as the passage of viable enteric bacteria through intestinal epithelial cells into the lamina propria and then to mesenteric lymph nodes, and possibly other tissues. Bacterial translocation was first defined as the passage of viable bacteria. However, at the present time either bacterial fragments or the translocation of bacterial products such as endotoxins from dead bacteria have been known to stimulate the immune system[23]. Under normal conditions, the gastrointestinal system keeps bacterial content in the intestinal lumen while absorbing nutrients. This is called “intestinal barrier function”[5]. Despite the number of bacteria present in the cecum, one cell beneath the mucosa is sterile. The intestinal barrier is both a functional and anatomical barrier to intestinal contents. The functional aspect is inherent in the modulation of tight junctional permeability and selective endocytosis of intestinal contents, while the anatomical barrier aspect is represented by the interconnected tight junctional/cell membrane system which effectively excludes large molecules and bacterial antigens. The first component of the intestinal barrier consists of intestinal microflora which have two functions, “bacterial antagonism” and “colonization resistance”[24,25]. The other components of the intestinal barrier are the physical barrier function of the mucosal epithelium, a mucus layer on the intestinal epithelium, blockade of epithelial adhesion sites by secreted IgA, and the preventive effects of intestinal peristalsis and intermittent desquamation of epithelial cells forming the mucosa. Despite these defense systems, translocated bacteria and bacterial products are neutralized in intestine-related lymphoid tissues (intraepithelial and lamina propria lymphocytes, lymphoid follicles, Peyer’s patches and complexes of mesenteric lymph nodes), and the immune system (especially the reticuloendothelial system organs, such as the liver). In various studies bacterial translocation has been reported to develop in mechanical intestinal obstruction, hemorrhagic shock, sepsis, endotoxemia, severe trauma, thermal injury, obstructive jaundice and cirrhosis[24,25]. The clinical importance of bacterial translocation was revealed in a study conducted by MacFie et al[26] in over 927 patients throughout 13 years. Bacterial translocation was detected in 130 patients (14%) in this study. Postoperative sepsis was seen more frequently (42.3% and 19.9%) in these patients. The authors reported ethical and methodological problems present in their study of bacterial translocation in humans and probably these problems are even bigger than described. According to our current knowledge, glutamine support, aggressive and targeted nutrition, adequate provision of visceral flow, appropriate use of antibiotics and selective intestinal decontamination are important objectives in restricting bacterial translocation[5].
Another important point in the pathophysiology of obstructive jaundice is the increased oxidative stress in the tissues. When the balance between the production of free oxygen radicals and antioxidant systems is impaired, oxidative stress leading to tissue damage occurs[26,27]. Increased intestinal oxidative stress which can cause intestinal damage and endotoxin translocation has been detected in rats with obstructive jaundice. In fact, obstructive jaundice causes oxidative stress in other organs such as the liver, kidneys, brain, heart and lungs. The development of tissue injury depends directly on the bile acids or occurs via macrophages; formation of oxygen free radicals as a result of systemic endotoxemia-induced xanthine oxidase, endotoxin-mediated systemic cytokine response, neutrophil chemotaxis of jaundice, increase of superoxide anion production and reduction of plasma levels of fat-soluble vitamins, particularly vitamin E, have been blamed for oxidative stress occurring in obstructive jaundice[28].
The effect of obstructive jaundice on bacterial translocation has been investigated in numerous clinical and experimental studies. Several changes have been shown to occur both in the intestinal barrier and in the reticuloendothelial system in obstructive jaundice. Bile and bile salts in the intestinal lumen are believed to have protective effects against bacterial translocation[23]. Luminal flow of bile salts has a regulatory effect on the intestinal flora and a direct detergent effect on endotoxins[25]. Furthermore, some trophic effects of pancreaticobiliary secretions on the intestinal mucosa have been identified[28]. Ogata et al[29] showed that oral administration of bile salts reduced absorption of endotoxin in rats with jaundice. Intestinal permeability increases with mucosal damage and as a consequence of changes in the intestinal flora a convenient media for bacterial translocation is prepared. Gatt et al[5] showed that reticuloendothelial system function was impaired subsequent to biliary tract obstruction and caused an increase in bacterial translocation. Reticuloendothelial system is defined as tissue macrophages. These are found chiefly in the liver, spleen, lung and bone marrow. They are responsible for cleaning up particulate materials such as bacteria, endotoxin, immune complexes and cell debris[3]. Kupffer cells in the liver are responsible for 80%-90% of the reticuloendothelial system activity. Assimakopoulos et al[28] detected increased intestinal oxidative stress which could cause intestinal damage and increased intestinal endotoxin translocation in an experimental model of rats with jaundice. Bacterial translocation and inflammatory responses in patients with obstructive jaundice were examined in a study performed by Ljungdahl et al[30] The results of this study which had few cases are as follows: bacterial translocation could not be detected in any of the patients. Elevated levels of preoperative endotoxin, TNF-α and IL-6 were measured in patients with jaundice. In these patients, the number of macrophages and apoptosis increased while T-lymphocyte count decreased in the mesenteric lymph nodes.
Treatment modalities and agents affecting the different pathophysiological steps described above have been investigated for many years, in order to reduce mortality and morbidity seen post-treatment or during the elapsed time until the definitive treatment of obstructive jaundice. Glutamine is one of the most important products surveyed for this purpose. Glutamine is the most common free amino acid in the body and has an important role in numerous metabolic events such as amino acid transport and nitrogen balance. It is the main food source of rapidly dividing cells such as enterocytes and lymphocytes. These cells have important roles in the intestinal mucosa barrier and the immune system. Numerous studies examining the effect of glutamine on bacterial translocation have been performed[6]. Glutamine reduces translocation not only by strengthening the intestinal barrier but also by reinforcing the immune system against bacteria and endotoxins successful in passing this barrier[3,6]. White et al[6] reported that glutamine regulated intestinal permeability, reduced bacterial translocation and even reinforced the immune system in rats with obstructive jaundice. Aldemir et al[7] showed that glutamine improved mucosal integrity and reduced bacterial translocation in the same model. In an experimental study performed by Margaritis et al[31], oral glutamine replacement was reported to reduce bacterial translocation, endotoxemia and apoptosis and to improve the ileal and liver histology in obstructive jaundice. Sheen-Chen et al[3] examined liver apoptosis in the obstructive jaundice rat model and determined that although glutamine replacement reduced liver apoptosis rate and ductal proliferation on day 3 of the experiment, the same effect could not be shown on day 7. In clinical studies, glutamine treatment was determined to have beneficial effects on bacterial translocation and sepsis. These effects can be listed as reduction in mucosal atrophy, rapid improvement in radiotherapy- and chemotherapy-induced mucosal damage, strengthening of intestinal and systemic immunity and decrease in length of hospital stay and infection rates in patients in intensive care. Use of glutamine before abdominal radiation has been shown to exert a protective effect on the intestinal mucosa, to increase intestinal glutamine metabolism and to decrease morbidity and mortality subsequent to total abdominal irradiation. Glutamine also shows this effect when administered after the radiation therapy. Glutamine also plays a critical role in synthesis of glutathione, a major antioxidant, which protects tissues against free radical damage. The jejunal mucosal weight, DNA and nitrogen content increase and villus atrophy reduces significantly in glutamine-enriched total parenteral nutrition. Methotrexate-induced enterocolitis proceeds more slowly, and 5-fluorouracil-induced mucosal damage recovery occurs more rapidly, in patients fed on a glutamine-supplemented enteral diet[5,32]. In a study performed on rats by Kul et al[33] the positive effect of glutamine on oxidative stress both in a hypoxia-reoxygenation model and in healthy neonatal rats was reported. Glutamine supplementation has been suggested to prevent necrotizing enterocolitis in neonates.
In the present study, we examined the effects of glutamine and curcumin use on bacterial translocation and oxidative stress in rats with obstructive jaundice. Consistent with the literature, we detected the positive effects of glutamine use on these issues. Positive culture rates observed in the microbiological assays were less in all samples from the glutamine-treated group compared to those of the control and curcumin-treated groups. However, only the blood culture rates were statistically significant in comparison with the control group (P = 0.029). Moreover, shortening of villus height and lymphatic dilation were found to be significantly lower in the glutamine-treated group terminal ileum (P < 0.05).
Curcumin is a polyphenol derived from turmeric, which is used as a spice or herbal medicine. It is produced from the root of a plant, Curcuma longa. Dried roots of this plant have been used for thousands of years in Asian medicine[34]. Curcumin has been suggested to reduce inflammation which causes bacterial translocation by exhibiting an anti-inflammatory effect[9]. In the study performed by Shen et al[35], curcumin was shown to increase expression of antioxidant biomolecules and reduce neutrophil infiltration and reactive oxygen metabolites after ischemia-reperfusion injury in the liver. Treatment of rats with curcumin decreased total nitric oxide synthase activity after reperfusion. However, endothelial nitric oxide synthase activity was not affected. Moreover, curcumin has been shown to have positive effects on inflammatory damage and intestinal reperfusion injury in a recent experimental study by Karatepe et al[10].
In the present study, we examined the effects of curcumin on bacterial translocation and oxidative damage in an obstructive jaundice model and we compared it with glutamine, which is a reliable control and has been recently in clinical use. Microbiologically, positive culture rates were found to be less in all samples from the curcumin-treated group compared to those from the control group. However, only the rates of blood cultures were statistically significant (P = 0.041). No significant difference was observed when compared with the glutamine-treated group. All biochemical parameters (except ALP levels) of the glutamine-treated group were found to be lower in a statistically significant manner in comparison with those of the curcumin-treated group (P < 0.05). No statistically significant difference was detected in the histopathological examination of the samples obtained from the curcumin-treated group compared to the glutamine-treated and control groups (P > 0.05).
In conclusion, in the present study we detected positive effects of glutamine and curcumin on bacterial translocation and oxidative damage in rats with obstructive jaundice. Both glutamine and curcumin were observed to reduce bacterial translocation in blood, hepatocellular injury, serum cytokine levels, oxidative tissue damage and apoptosis rates significantly in comparison to the control group. However, more extensive comparative experimental and clinical studies are required before the clinical use of curcumin for this purpose and perhaps the combined use of glutamine with curcumin will be more effective.
COMMENTS
Background
Despite current modern diagnostic and therapeutic approaches, interventions in patients with biliary tract obstruction result in 10%-25% mortality and up to 56% major morbidity. Bacterial translocation and oxidative tissue damage have been emphasized as the leading cause of the complications in obstructive jaundice by numerous investigators.
Research frontiers
The antioxidant, anti-cancer, anti-inflammatory and cytoprotective effects of curcumin have been demonstrated by numerous experimental and clinical studies. Administration of glutamine has been shown to improve bacterial translocation and oxidative damage in obstructive jaundice but the exact role of curcumin in this issue is still unknown. In this study, the authors demonstrate that both curcumin and glutamine are effective in preventing or reducing bacterial translocation and oxidative damage in obstructive jaundice.
Innovations and breakthroughs
Obstructive jaundice causes alterations leading to bacterial translocation both in the intestinal barrier and in the reticuloendothelial system. Some of these alterations may be listed as mucosal damage in the intestinal lumen due to lack of bile, apoptosis, bacterial overgrowth, motility disorder associated with oxidative stress and functional abnormalities in the tissue macrophages. According to the authors’ knowledge, a comprehensive and comparative study regarding the effect of curcumin on bacterial translocation and oxidative damage in obstructive jaundice has not been performed yet. Both glutamine and curcumin were observed to reduce bacterial translocation in blood, hepatocellular injury, serum cytokine levels, oxidative tissue damage and apoptosis rates significantly in comparison to the control group.
Applications
Curcumin can be used like glutamine in order to prevent bacterial translocation and oxidative damage observed in obstructive jaundice and to reduce mortality and morbidity observed in the elapsed time until definitive treatment or after treatment.
Terminology
Glutamine, a non-essential amino acid, has been reported not only to lower the rate of endotoxemia and translocation by preserving mucosal integrity but also to improve the action of the immune system against bacteria and endotoxins which succeed in passing the intestinal barrier. Curcumin is a polyphenol derived from the herbal remedy and dietary spice turmeric. The antioxidant, anti-cancer, anti-inflammatory and cytoprotective effects of curcumin have been demonstrated by numerous experimental and clinical studies.
Peer review
This is a well conceived and implemented experimental protocol which seeks to answer the question of the relative efficacy of glutamine and curcumin in the treatment or prevention of intestinal bacterial translocation in the setting of obstructive jaundice. The experimental protocol is well carried out and can be expected to extrapolate to human clinical situations in which obstructive jaundice is present.
Footnotes
Peer reviewers: Jay Pravda, MD, Inflammatory Disease Research Center, Gainesville, FL 32614-2181, United States; Saúl Villa-Trevio, MD, PhD, Departamento de Biología Celular, Centro de Investigación y de Estudios Avanzados del IPN (Cinvestav), Ave. IPN No. 2508. Col. San Pedro, Zacatenco, CP 07360, México, DF, México
S- Editor Wang YR L- Editor Logan S E- Editor Lin YP
References
- 1.Crawford JM. The liver and the biliary tract. In: Cotran RS, Kumar V, Robbins SL, eds , editors. Pathologic Basis of Disease. Philadelphia: WB Saunders; 1994. pp. 838–840. [Google Scholar]
- 2.Sileri P, Morini S, Sica GS, Schena S, Rastellini C, Gaspari AL, Benedetti E, Cicalese L. Bacterial translocation and intestinal morphological findings in jaundiced rats. Dig Dis Sci. 2002;47:929–934. doi: 10.1023/a:1014733226337. [DOI] [PubMed] [Google Scholar]
- 3.Sheen-Chen SM, Hung KS, Ho HT, Chen WJ, Eng HL. Effect of glutamine and bile acid on hepatocyte apoptosis after bile duct ligation in the rat. World J Surg. 2004;28:457–460. doi: 10.1007/s00268-004-7189-7. [DOI] [PubMed] [Google Scholar]
- 4.Akin ML, Erenoglu C, Dal A, Erdemoglu A, Elbuken E, Batkin A. Hyperbaric oxygen prevents bacterial translocation in rats with obstructive jaundice. Dig Dis Sci. 2001;46:1657–1662. doi: 10.1023/a:1010641201842. [DOI] [PubMed] [Google Scholar]
- 5.Gatt M, Reddy BS, MacFie J. Review article: bacterial translocation in the critically ill--evidence and methods of prevention. Aliment Pharmacol Ther. 2007;25:741–757. doi: 10.1111/j.1365-2036.2006.03174.x. [DOI] [PubMed] [Google Scholar]
- 6.White JS, Hoper M, Parks RW, Clements WD, Diamond T. Glutamine improves intestinal barrier function in experimental biliary obstruction. Eur Surg Res. 2005;37:342–347. doi: 10.1159/000090334. [DOI] [PubMed] [Google Scholar]
- 7.Aldemir M, Geyik MF, Kökoğlu OF, Büyükbayram H, Hoşoğlu S, Yağmur Y. Effects of ursodeoxycholic acid, glutamine and polyclonal immunoglobulins on bacterial translocation in common bile duct ligated rats. ANZ J Surg. 2003;73:722–726. doi: 10.1046/j.1445-2197.2003.02749.x. [DOI] [PubMed] [Google Scholar]
- 8.Sharma RA, Gescher AJ, Steward WP. Curcumin: the story so far. Eur J Cancer. 2005;41:1955–1968. doi: 10.1016/j.ejca.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 9.Gülçubuk A, Sönmez K, Gürel A, Altunatmaz K, Gürler N, Aydin S, Oksüz L, Uzun H, Güzel O. Pathologic alterations detected in acute pancreatitis induced by sodium taurocholate in rats and therapeutic effects of curcumin, ciprofloxacin and metronidazole combination. Pancreatology. 2005;5:345–353. doi: 10.1159/000086534. [DOI] [PubMed] [Google Scholar]
- 10.Karatepe O, Gulcicek OB, Ugurlucan M, Adas G, Battal M, Kemik A, Kamali G, Altug T, Karahan S. Curcumin nutrition for the prevention of mesenteric ischemia-reperfusion injury: an experimental rodent model. Transplant Proc. 2009;41:3611–3616. doi: 10.1016/j.transproceed.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 11.Sier CF, Kubben FJ, Ganesh S, Heerding MM, Griffioen G, Hanemaaijer R, van Krieken JH, Lamers CB, Verspaget HW. Tissue levels of matrix metalloproteinases MMP-2 and MMP-9 are related to the overall survival of patients with gastric carcinoma. Br J Cancer. 1996;74:413–417. doi: 10.1038/bjc.1996.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moshage H, Kok B, Huizenga JR, Jansen PL. Nitrite and nitrate determinations in plasma: a critical evaluation. Clin Chem. 1995;41:892–896. [PubMed] [Google Scholar]
- 13.Kruidenier L, Kuiper I, Van Duijn W, Mieremet-Ooms MA, van Hogezand RA, Lamers CB, Verspaget HW. Imbalanced secondary mucosal antioxidant response in inflammatory bowel disease. J Pathol. 2003;201:17–27. doi: 10.1002/path.1408. [DOI] [PubMed] [Google Scholar]
- 14.Jonges LE, Nagelkerke JF, Ensink NG, van der Velde EA, Tollenaar RA, Fleuren GJ, van de Velde CJ, Morreau H, Kuppen PJ. Caspase-3 activity as a prognostic factor in colorectal carcinoma. Lab Invest. 2001;81:681–688. doi: 10.1038/labinvest.3780277. [DOI] [PubMed] [Google Scholar]
- 15.Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 16.Reitman S, Frankel S. A colorimetric method for the determination of serum glutamic oxalacetic and glutamic pyruvic transaminases. Am J Clin Pathol. 1957;28:56–63. doi: 10.1093/ajcp/28.1.56. [DOI] [PubMed] [Google Scholar]
- 17.Belfield A, Goldberg DM. Revised assay for serum phenyl phosphatase activity using 4-amino-antipyrine. Enzyme. 1971;12:561–573. doi: 10.1159/000459586. [DOI] [PubMed] [Google Scholar]
- 18.Henry RJ. Clinical Chemistry, Principles and Techniques. 2nd ed. New York: Harper and Row; 1974. p. 525. [Google Scholar]
- 19.Wang Q, Gurusamy KS, Lin H, Xie X, Wang C. Preoperative biliary drainage for obstructive jaundice. Cochrane Database Syst Rev. 2008:CD005444. doi: 10.1002/14651858.CD005444.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Baiocchi L, Tisone G, Russo MA, Longhi C, Palmieri G, Volpe A, Almerighi C, Telesca C, Carbone M, Toti L, et al. TUDCA prevents cholestasis and canalicular damage induced by ischemia-reperfusion injury in the rat, modulating PKCalpha-ezrin pathway. Transpl Int. 2008;21:792–800. doi: 10.1111/j.1432-2277.2008.00682.x. [DOI] [PubMed] [Google Scholar]
- 21.Slott PA, Liu MH, Tavoloni N. Origin, pattern, and mechanism of bile duct proliferation following biliary obstruction in the rat. Gastroenterology. 1990;99:466–477. doi: 10.1016/0016-5085(90)91030-a. [DOI] [PubMed] [Google Scholar]
- 22.Berg RD, Garlington AW. Translocation of certain indigenous bacteria from the gastrointestinal tract to the mesenteric lymph nodes and other organs in a gnotobiotic mouse model. Infect Immun. 1979;23:403–411. doi: 10.1128/iai.23.2.403-411.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White JS, Hoper M, Parks RW, Clements WD, Diamond T. Patterns of bacterial translocation in experimental biliary obstruction. J Surg Res. 2006;132:80–84. doi: 10.1016/j.jss.2005.07.026. [DOI] [PubMed] [Google Scholar]
- 24.Albillos A, de la Hera A. Multifactorial gut barrier failure in cirrhosis and bacterial translocation: working out the role of probiotics and antioxidants. J Hepatol. 2002;37:523–526. doi: 10.1016/s0168-8278(02)00265-9. [DOI] [PubMed] [Google Scholar]
- 25.Parks RW, Clements WD, Pope C, Halliday MI, Rowlands BJ, Diamond T. Bacterial translocation and gut microflora in obstructive jaundice. J Anat. 1996;189(Pt 3):561–565. [PMC free article] [PubMed] [Google Scholar]
- 26.MacFie J, Reddy BS, Gatt M, Jain PK, Sowdi R, Mitchell CJ. Bacterial translocation studied in 927 patients over 13 years. Br J Surg. 2006;93:87–93. doi: 10.1002/bjs.5184. [DOI] [PubMed] [Google Scholar]
- 27.Gutteridge JM. Lipid peroxidation and antioxidants as biomarkers of tissue damage. Clin Chem. 1995;41:1819–1828. [PubMed] [Google Scholar]
- 28.Assimakopoulos SF, Vagianos CE, Patsoukis N, Georgiou C, Nikolopoulou V, Scopa CD. Evidence for intestinal oxidative stress in obstructive jaundice-induced gut barrier dysfunction in rats. Acta Physiol Scand. 2004;180:177–185. doi: 10.1046/j.0001-6772.2003.01229.x. [DOI] [PubMed] [Google Scholar]
- 29.Ogata Y, Nishi M, Nakayama H, Kuwahara T, Ohnishi Y, Tashiro S. Role of bile in intestinal barrier function and its inhibitory effect on bacterial translocation in obstructive jaundice in rats. J Surg Res. 2003;115:18–23. doi: 10.1016/s0022-4804(03)00308-1. [DOI] [PubMed] [Google Scholar]
- 30.Ljungdahl M, Osterberg J, Ransjö U, Engstrand L, Haglund U. Inflammatory response in patients with malignant obstructive jaundice. Scand J Gastroenterol. 2007;42:94–102. doi: 10.1080/00365520600825190. [DOI] [PubMed] [Google Scholar]
- 31.Margaritis VG, Filos KS, Michalaki MA, Scopa CD, Spiliopoulou I, Nikolopoulou VN, Vagianos CE. Effect of oral glutamine administration on bacterial tanslocation, endotoxemia, liver and ileal morphology, and apoptosis in rats with obstructive jaundice. World J Surg. 2005;29:1329–1334. doi: 10.1007/s00268-005-7721-4. [DOI] [PubMed] [Google Scholar]
- 32.Zheng YM, Li F, Zhang MM, Wu XT. Glutamine dipeptide for parenteral nutrition in abdominal surgery: a meta-analysis of randomized controlled trials. World J Gastroenterol. 2006;12:7537–7541. doi: 10.3748/wjg.v12.i46.7537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kul M, Vurucu S, Demirkaya E, Tunc T, Aydinoz S, Meral C, Kesik V, Alpay F. Enteral glutamine and/or arginine supplementation have favorable effects on oxidative stress parameters in neonatal rat intestine. J Pediatr Gastroenterol Nutr. 2009;49:85–89. doi: 10.1097/MPG.0b013e318198cd36. [DOI] [PubMed] [Google Scholar]
- 34.Weber-Mzell D, Zaupa P, Petnehazy T, Kobayashi H, Schimpl G, Feierl G, Kotanko P, Höllwarth M. The role of nuclear factor-kappa B in bacterial translocation in cholestatic rats. Pediatr Surg Int. 2006;22:43–49. doi: 10.1007/s00383-005-1599-y. [DOI] [PubMed] [Google Scholar]
- 35.Shen SQ, Zhang Y, Xiang JJ, Xiong CL. Protective effect of curcumin against liver warm ischemia/reperfusion injury in rat model is associated with regulation of heat shock protein and antioxidant enzymes. World J Gastroenterol. 2007;13:1953–1961. doi: 10.3748/wjg.v13.i13.1953. [DOI] [PMC free article] [PubMed] [Google Scholar]


