Abstract
Background: Blacks have lower average triglyceride and LDL cholesterol concentrations than do whites but higher rates of coronary heart disease. Apolipoprotein (apo) C-III in VLDL and LDL stimulates atherogenic processes in vascular cells. In blacks, the concentration of lipoproteins with apo C-III is unknown, and the response to dietary strategies that lower triglyceride and apo C-III has not been investigated
Objective: We compared the concentration of and dietary effects on apo C-III–containing lipoproteins in blacks and whites.
Design: In a randomized, 3-period feeding study [OmniHeart (Optimal Macronutrient Intake Trial to Prevent Heart Disease)], we measured lipoprotein concentrations in 89 blacks and 73 whites who consumed self-selected diets (baseline) and after 3 healthful diets emphasizing carbohydrate, unsaturated fat, or protein. Participants had prehypertension or hypertension, and 79% were overweight or obese.
Results: While consuming self-selected diets, blacks had lower apo C-III in total plasma, VLDL, and LDL than did whites. Unsaturated fat and protein diets lowered plasma apo C-III (16% and 18%, respectively) and triglyceride (12% and 21%, respectively) in whites but not in blacks, reducing racial differences. Most important, blacks had a lower concentration of atherogenic LDL with apo C-III at baseline and after study diets (34–41% lower, P < 0.02). The molar ratio of apo E to apo B was higher in blacks than in whites in total plasma and LDL at baseline and after the study diets.
Conclusions: Blacks have lower concentrations of atherogenic lipoproteins that contain apo C-III than do whites when consuming diverse diets and an attenuated dietary response of triglyceride and apo C-III. Dietary efforts to lower triglyceride and apo C-III may be more effective in whites than in blacks. The OmniHeart Trial was registered at www.clinicaltrials.gov as NCT00051350.
INTRODUCTION
Black Americans suffer a higher morbidity and mortality from coronary heart disease (CHD) than do white Americans (1–3) and are nearly twice as likely to die prematurely (1). In 2005, the age-adjusted rate for deaths from heart disease was 30% higher in black Americans than in white Americans (2). Blacks tend to have higher incidence of obesity, hypertension, and diabetes (1), diseases that are intimately tied to cardiovascular disease (CVD), diet, and plasma lipids, and elevated concentrations of inflammation markers (4, 5). Yet, many studies have reported that blacks on average have lower LDL cholesterol and plasma triglyceride than do whites (6–10), which are well-established risk factors for CHD (11–13).
Although blood lipids are associated with CHD, recent studies have found even stronger associations between CHD and plasma apolipoprotein (apo) B (14–20) and apo C-III (21–23). Apo C-III blocks the clearance of VLDL by the liver (24–26), channeling it to formation of LDL (26, 27). Recent data also show direct proinflammatory, atherogenic activity of apo C-III through activation of human endothelial cells and monocytes (28, 29). LDL particles with apo C-III, a remnant particle produced by lipolysis in plasma of VLDL with apo C-III (30), is the apo B lipoprotein type that predicts CHD most strongly in patients with type 2 diabetes (21). In contrast, plasma apo E increases the clearance rate of apo B particles through recognition and uptake by liver receptors (25, 31), reducing the concentration of atherogenic lipoprotein remnants and LDL (30). Whites have higher concentrations of triglyceride and LDL cholesterol than do blacks, but racially stratified data are scarce on apolipoprotein concentrations.
Diet has a direct effect on plasma lipids and lipoproteins. Compared with a typical high-saturated-fat diet, healthy diets that emphasize carbohydrate, protein, or unsaturated fat reduce plasma total and LDL apo B (32). Substituting protein for carbohydrate in the context of a healthy dietary pattern reduces atherogenic apo C-III–containing LDL and its precursor, apo C-III–containing VLDL (32).
For the first time, to our knowledge, we examine racial differences in lipoprotein subtypes and their response to dietary intervention, information lacking in the literature yet crucial to the understanding of the racial disparity in CHD. We hypothesize that the higher burden of CHD in blacks than in whites may be explained in part by higher concentrations in blacks of atherogenic apo B lipoproteins containing apo C-III, despite their lower overall concentration of apo C-III. The majority of apo C-III resides in non–apo B lipoproteins. As such, blacks could have lower plasma apo C-III and triglyceride but a greater concentration of apo B particles that contain apo C-III, explaining the higher burden of CHD. This hypothesis took into account the greater insulin resistance and obesity in blacks than in whites (9, 10), both of which are associated with elevated apo C-III. In addition, we compare the effects of controlled study diets in blacks and whites on these lipoprotein risk factors to assess their effectiveness in reducing CHD risk.
METHODS
The rationale and design of the Optimal Macronutrient Intake Trial to Prevent Heart Disease (OmniHeart) (33), the main lipid results (34), and the results on lipoprotein subtypes (32) have been published previously. Briefly, the OmniHeart trial is an investigator-initiated National Heart, Lung, and Blood Institute–sponsored study that used a randomized, 3-period crossover design to compare the effects of macronutrients on blood pressure and plasma lipids. Study diets were modeled on the successful Dietary Approaches to Stop Hypertension (DASH) diet and emphasized either carbohydrate (CARB), unsaturated fats (UNSAT), or protein, with emphasis on plant sources such as soy, legumes, nuts, and seeds (PROT). The DASH diet was chosen as the model for the study diets because it is effective at lowering blood pressure and LDL cholesterol. Although DASH lowered LDL cholesterol, it also lowered HDL cholesterol and did not affect triglycerides, findings attributable to its high carbohydrate content (35). In OmniHeart, we examined the effect of replacing some of the carbohydrate with unsaturated fat or protein. The study protocol was approved by the Institutional Review Boards at all affiliated institutions (Johns Hopkins University, Brigham and Women's Hospital, and the Harvard School of Public Health).
Participant recruitment and controlled feeding
Details of participant recruitment and controlled feeding have been described previously (34, 36). Briefly, participants were recruited from the population of the greater Baltimore, MD, and Boston, MA, areas. They were ≥30 y of age with blood pressure (BP) at enrollment that was above normal but less than stage 2 hypertension (systolic BP of 120–159 mm Hg or diastolic BP of 80–99 mm Hg). Participants’ fasting LDL cholesterol could not exceed 220 mg/dL, and triglycerides could not exceed 750 mg/dL. One of the primary recruitment goals was to ensure that ≈50% of enrolled participants were black due to blacks’ disproportionately high burden of CVD. This was achieved by self-identification of race on the screening questionnaire.
To assess eligibility, each participant was required to complete 3 clinical visits, which were all conducted a minimum of 7 d after the previous visit. Blood samples were drawn and processed at each of the visits, and participants completed a food-frequency questionnaire (FFQ) at screening visit 3 (Walter Willett FFQ, version 88GP; Channing Laboratory, Boston, MA). After completing the 3 visits, eligible participants then participated in a 6-d run-in period to determine ability to adhere to the diet sequences. Those who completed the run-in period successfully were randomly assigned to 1 of 6 possible sequences of the 3 diets (CARB, UNSAT, PROT). During the run-in period and all study diet periods, subjects were provided with all of their food for each day, and no nonstudy food was to be consumed. A detailed description of these 3 diets has been published previously (36, 37). Briefly, the composition of the study diets was 58:27:15 (carbohydrate:protein:fat) for CARB, 48:37:15 for PROT, and 48:27:25 for UNSAT. Adherence was monitored through daily diet diaries and at participants’ weekday visits to the study center. Participants were instructed to maintain usual levels of physical activity, and changes in weight were prevented by weight checks at food distribution and alteration of caloric intake as necessary. Blood was drawn at the end of the fourth and sixth weeks of each diet period. The 6-wk samples were used in this substudy. Participants then ate their usual diet of their own choice for a minimum of 2 wk before beginning the next diet period. Controlled feeding took place from April 2003 to June 2005. To quantify insulin resistance, the homeostasis model assessment (HOMA) index was calculated from fasting glucose and insulin concentrations as HOMA = [(fasting plasma insulin concentration in μU/mL) × (fasting plasma glucose concentration in mmol/L)]/22.5. This was calculated at baseline and after all 3 diet periods.
Laboratory measurements
The details of laboratory measurements have been published previously (32). Briefly, samples were thawed, filtered, and incubated overnight in anti–-apo C-III immunoaffinity columns (polyclonal goat anti-human apo C-III antibody bound to Sepharose 4B Resin; Academy Biomedical Company Inc, Houston, TX) to separate apo C-III–containing and apo C-III–deficient lipoproteins. These fractions were then ultracentrifuged at 15°C and 25,000 rpm in the outermost row of a Beckman 25-Ti rotor with a Beckman L8-70M ultracentrifuge (Beckman Coulter Inc,Fullerton, CA) to produce 6 fractions for analysis: VLDL (d < 1.006 g/mL) without apo C-III, VLDL (d < 1.006 g/mL) with apo C-III, LDL (1.006 g/mL < d < 1.063 g/mL) without apo C-III, LDL (1.006 g/mL < d < 1.063 g/mL) with apo C-III, and remaining plasma proteins with and without apo C-III (d > 1.063 g/mL). Each participant's 4 samples (baseline and after each of the three 6-wk diet periods) were analyzed in the same batch in random order to reduce analytic variation. Batches consisted of samples of 5 or 9 participants, and analyses were completed within 5 d. All laboratory staff were blinded to the diet sequences of the participants.
Concentrations of apo B, apo C-III, and apo E in whole plasma and lipoprotein fractions were determined by sandwich ELISA procedures by using affinity purified antibodies (Academy Biomedical Company Inc). Triglyceride and cholesterol were determined by enzymatic assay (Thermo Scientific, Waltham, MA). Liquid transfer for 96-well plate loading and ELISA dilutions were handled robotically with a Multiprobe II (Perkin Elmer, Waltham, MA) to minimize error. Both ELISA and lipids plates were read with a BioTek ELx808iu 96-well plate reader controlled by KCJunior software (BioTek, Winooski, VT). All assays were completed in triplicate, and any sample with an intraassay CV >15% was repeated.
Statistics
The primary outcomes for this analysis were triglyceride, apo C-III, apo E, apo B, and cholesterol concentrations in whole plasma and in the lipoprotein subfractions. We also calculated the molecular ratios of apoE to apoB and apoC-III to apoB. The main comparisons in this study were between blacks and whites in the outcome variables at baseline and after each of the 3 study diets. The effect of race was calculated by using regression models that simultaneously adjusted for study site, sex, and age. Analyses were performed by using SAS version 9.1 (SAS Institute Inc, Cary, NC). In cases in which the distributions of outcome measures were at risk of violating the normality assumptions of our statistical models, testing was also performed on log-transformed outcomes. Secondarily, we examined racial differences in the changes elicited by the study diets by using similar regression models. Statistical significance was defined as P < 0.05, and we did not adjust P values for multiple comparisons because the hypotheses tested were prespecified. Many of the outcome variables under analysis are correlated and produce patterns of significance that corroborate one another.
For a study such as this with many subsamples per participant, there were randomly occurring missing values stemming from limitations in laboratory technology (eg, problems with sample aliquots, lack of sufficient sample, or liquid transfer failures). Because it is reasonable to assume that sample loss was statistically independent of participant characteristics and the value of the missing sample, no missing data were imputed for the primary analysis. Instead, the tests for each outcome were performed by using subsets of the data that exclude any subject who is missing data for that particular analyte. To ensure that bias was not introduced by the exclusion of participants without complete data sets, we performed several sensitivity analyses. First, we compared the means of the outcome variables in the subsets with those in the whole population and observed that they were not statistically different. We then performed the analyses on all available data points, allowing the n to vary for each outcome. This produced patterns of significance and results in line with the primary subset analyses with no significant discrepancies in the data. Finally, we used for secondary analysis the SAS "proc MI" (multiple imputation) procedure, which uses available observations in the data set to impute probable values for the missing data points and to estimate SEs and P values on the basis of analysis of within-imputation and between-imputation variances. Once again, this produced results highly consistent with the basic primary analysis.
RESULTS
Participants
A total of 191 participants, 104 black and 87 white, successfully completed the run-in period and were randomly assigned to 1 of the 6 diet sequences. Of these, 89 blacks and 73 whites finished ≥2 of the 3 diet periods and were eligible for inclusion in the analysis. Dropout occurrence was low, similar for both races, and distributed evenly across the 3 diets with no one diet proving more difficult to adhere to than the others. Adherence to the feeding protocol was high, with individuals reporting that on >95% of person-days all study foods were consumed and no nonstudy foods were added. On average, mean body weight decreased from baseline by 1 kg, and this change occurred equally across all 3 diets in both blacks and whites.
A summary of population characteristics is presented in Table 1. Baseline characteristics of participants did not differ according to the 6 diet sequences, but there were differences by race. A higher percentage of blacks were female, and fewer black than white women were postmenopausal. Approximately two-thirds of the black participants were from Baltimore. Lipoprotein differences between blacks and whites tended to be greater in women than in men. There was no difference detected between races in HOMA index. Body mass index (BMI) and menopausal status were not observed to be significant confounders of race-biomarker associations.
TABLE 1.
Characteristics of study population1
| All |
Female |
Male |
|||||||
| Black | White | P | Black | White | P | Black | White | P | |
| n | 89 | 73 | — | 50 | 22 | — | 39 | 51 | — |
| Percentage in study | 55 | 45 | — | 31 | 14 | — | 24 | 31 | — |
| Postmenopausal (%) | 66 | 90 | — | 66 | 90 | — | — | — | — |
| Age (y) | 52 ± 112 | 55 ± 11 | 0.13 | 53 ± 10 | 60 ± 7 | <0.01 | 51 ± 11 | 52 ± 11 | 0.5 |
| BMI (kg/m2) | 31.5 ± 6.3 | 29.0 ± 5.6 | <0.01 | 31.5 ± 6.5 | 32.1 ± 6.9 | 0.7 | 31.6 ± 6.1 | 27.6 ± 4.3 | <0.01 |
| HOMA index | 2.58 ± 1.98 | 2.27 ± 2.72 | 0.4 | 2.51 ± 1.87 | 2.76 ± 4.11 | 0.7 | 2.67 ± 2.13 | 2.05 ± 1.85 | 0.1 |
| Triglycerides (mg/dL) | 88 ± 65 | 116 ± 66 | <0.01 | 79 ± 61 | 109 ± 64 | 0.06 | 100 ± 69 | 119 ± 67 | 0.2 |
| LDL-C (mg/dL) | 125 ± 33 | 138 ± 41 | 0.03 | 128 ± 36 | 163 ± 43 | <0.01 | 121 ± 30 | 127 ± 35 | 0.1 |
| HDL-C (mg/dL) | 51.3 ± 18.0 | 48.5 ± 13.6 | 0.27 | 56.4 ± 17.1 | 56.2 ± 15.5 | 0.9 | 44.7 ± 17.2 | 45.1 ± 11.3 | 0.9 |
| Apo B (mg/dL) | 80 ± 22 | 88 ± 30 | 0.06 | 82 ± 21 | 96 ± 35 | 0.05 | 77 ± 22 | 84 ± 28 | 0.2 |
| Apo C-III (mg/dL) | 10.7 ± 5.8 | 15 ± 9.4 | <0.01 | 11.0 ± 6.4 | 16.7 ± 12.1 | 0.01 | 10.4 ± 4.8 | 14.3 ± 8.0 | <0.01 |
| Apo E (mg/dL) | 7.65 ± 2.86 | 7.03 ± 2.61 | 0.2 | 8.0 ± 3.3 | 8.1 ± 3.6 | 0.9 | 7.2 ± 2.2 | 6.6 ± 1.9 | 0.2 |
HOMA, homeostasis model assessment; LDL-C, LDL cholesterol; HDL-C, HDL cholesterol; Apo, apolipoprotein. P values were derived from Student's t test comparing blacks and whites; the race-by-sex interaction was significant for BMI only.
Unadjusted mean ± SD (all such values).
Lipid and lipoprotein differences between blacks and whites when consuming their usual self-selected diets
When consuming their usual self-selected diets, blacks had lower total plasma triglycerides, apo C-III, and LDL cholesterol in crude analysis (P < 0.03; Table 1) and after adjustment for age, sex, and site of recruitment (all P = 0.02; Table 2). Blacks trended toward having lower apo B (P = 0.06) (Table 1). Blacks had lower apo C-III in VLDL and in LDL (31% and 24%, respectively; P < 0.03), lower concentrations of LDL with apo C-III (presented in Table 2 as apo B in LDL with apo C-III) (35%, P = 0.02), and lower cholesterol in LDL with apo C-III (33%, P = 0.02) (Table 2). Plasma total apo E concentrations were not different between the 2 races, but the average amount of apo E on LDL lipoproteins containing apo C-III as determined by the ratio of molecules of apo E to apo B was significantly higher in blacks than in whites (P = 0.01). All together, these differences signify a less atherogenic lipoprotein profile in blacks than in whites while consuming their usual, self-selected diets.
TABLE 2.
Concentrations of plasma lipids and lipoproteins with consumption of free-living and controlled study diets in blacks and whites, adjusted for age, sex, and site of recruitment1
| Baseline |
||||||||||||||
| Black |
White |
CARB |
UNSAT |
PROT |
||||||||||
| n | Values | n | Values | P | Black | White | P | Black | White | P | Black | White | P | |
| Whole plasma (mg/dL) | ||||||||||||||
| Triglycerides | 57 | 88 (7.3) | 50 | 115 (8.1) | 0.02 | 93 (7.2) | 105 (7.9) | 0.3 | 90 (7.9) | 101 (8.8)2 | 0.4 | 84 (7.4) | 96 (8.2)2 | 0.3 |
| Apo C-III | 59 | 12 (1.1) | 56 | 16 (1.1) | 0.02 | 13 (1.0) | 14 (1.0)2 | 0.4 | 12 (1.0) | 13 (1.0)2 | 0.4 | 12 (0.8) | 13 (0.9)2 | 0.7 |
| Total cholesterol | 59 | 202 (5.9) | 52 | 225 (6.3) | 0.01 | 185 (5.3)2 | 208 (5.7)2 | <0.01 | 182 (5.2)2 | 201 (5.6)2 | 0.02 | 174 (5.0)2 | 203 (5.3)2 | <0.01 |
| LDL-C | 59 | 123 (5.0) | 52 | 141 (5.4) | 0.02 | 110 (4.4)2 | 131 (4.8)2 | <0.01 | 109 (4.4)2 | 124 (4.7)2 | 0.03 | 105 (4.0)2 | 124 (4.3)2 | <0.01 |
| Apo B | 43 | 78 (4.5) | 45 | 87 (4.4) | 0.2 | 76 (3.5) | 80 (3.5)2 | 0.5 | 73 (3.6) | 80 (3.5)2 | 0.2 | 71 (3.6)2 | 78 (3.5)2 | 0.2 |
| Apo E | 75 | 7.7 (0.3) | 65 | 7.2 (0.4) | 0.3 | 7.2 (0.3)2 | 6.3 (0.3)2 | 0.05 | 7.1 (0.3)2 | 6.0 (0.3)2 | 0.01 | 7.1 (0.3)2 | 6.0 (0.3)2 | 0.03 |
| Lipoproteins without apo C-III | ||||||||||||||
| VLDL (mg/dL) | ||||||||||||||
| Triglycerides | 57 | 30 (5.5) | 50 | 37 (5.9) | 0.4 | 30 (4.8) | 36 (5.1) | 0.4 | 28 (5.3) | 32 (5.7) | 0.6 | 26 (5.5)2 | 28 (5.9) | 0.8 |
| Cholesterol | 59 | 9.3 (1.2) | 52 | 13 (1.3) | 0.09 | 9.2 (1.2) | 11.4 (1.3) | 0.2 | 8.5 (1.2) | 11 (1.3) | 0.1 | 7.4 (1.4) | 11 (1.5) | 0.2 |
| Apo B | 43 | 2.5 (0.5) | 45 | 2.9 (0.4) | 0.5 | 2.5 (0.4) | 3.3 (0.4) | 0.2 | 2.3 (0.3) | 2.9 (0.3) | 0.2 | 2.2 (0.3) | 2.6 (0.3) | 0.5 |
| Apo E | 75 | 0.20 (0.03) | 65 | 0.22 (0.03) | 0.5 | 0.22 (0.03) | 0.21 (0.03) | 0.8 | 0.19 (0.02) | 0.20 (0.03) | 0.8 | 0.21 (0.03) | 0.20 (0.03) | 0.9 |
| LDL | ||||||||||||||
| Triglycerides (mg/dL) | 57 | 25 (2.0) | 50 | 33 (2.1) | 0.02 | 25 (1.9) | 26 (2.0)2 | 0.8 | 25 (2.3) | 24 (2.5)2 | 0.6 | 25 (1.8) | 23 (2.0)2 | 0.5 |
| Cholesterol (mg/dL) | 59 | 113 (4.8) | 52 | 126 (5.1) | 0.07 | 101 (4.1)2 | 116 (4.4)2 | 0.02 | 100 (4.0)2 | 110 (4.3)2 | 0.1 | 97 (3.7)2 | 110 (4.0)2 | 0.02 |
| Apo B (mg/dL) | 43 | 69 (3.7) | 45 | 74 (3.6) | 0.4 | 66 (2.9) | 65 (2.9)2 | 0.8 | 64 (2.9) | 67 (2.9)2 | 0.5 | 63 (2.9) | 66 (2.9)2 | 0.5 |
| Apo E (mg/dL) | 75 | 0.41 (0.03) | 65 | 0.38 (0.03) | 0.4 | 0.41 (0.03) | 0.34 (0.03) | 0.2 | 0.37 (0.02) | 0.33 (0.02) | 0.2 | 0.39 (0.03) | 0.33 (0.03) | 0.2 |
| Apo E:apo B (mol/mol) | 42 | 0.11 (0.01) | 43 | 0.09 (0.01) | 0.1 | 0.11 (0.01) | 0.09 (0.01) | 0.2 | 0.10 (0.01) | 0.09 (0.01) | 0.1 | 0.11 (0.01) | 0.09 (0.01) | 0.1 |
| Lipoproteins with apo C-III | ||||||||||||||
| VLDL (mg/dL) | ||||||||||||||
| Triglycerides | 57 | 13 (1.9) | 50 | 16 (2.0) | 0.2 | 16 (2.3) | 22 (2.5) | 0.08 | 17 (2.9) | 23 (3.1) | 0.1 | 15 (2.4) | 20 (2.5) | 0.2 |
| Apo C-III | 59 | 1.04 (0.13) | 56 | 1.50 (0.13) | 0.02 | 1.4 (0.16) | 1.7 (0.16) | 0.2 | 1.2 (0.15) | 1.8 (0.15) | <0.01 | 1.3 (0.15) | 1.6 (0.15) | 0.2 |
| Cholesterol | 59 | 4.0 (0.6) | 52 | 5.0 (0.6) | 0.1 | 4.5 (0.6) | 6.1 (0.7) | 0.1 | 4.8 (0.7) | 5.9 (0.8) | 0.4 | 4.3 (0.7) | 6.0 (0.7) | 0.1 |
| Apo B | 43 | 0.80 (0.13) | 45 | 1.08 (0.13) | 0.2 | 1.0 (0.17) | 1.5 (0.17)2 | 0.08 | 0.89 (0.15) | 1.5 (0.14)2 | 0.01 | 0.93 (0.15) | 1.2 (0.14) | 0.2 |
| Apo E | 75 | 0.31 (0.03) | 65 | 0.31 (0.03) | 0.9 | 0.42 (0.04) | 0.46 (0.05) | 0.5 | 0.38 (0.04) | 0.46 (0.05) | 0.3 | 0.40 (0.05) | 0.41 (0.05) | 0.8 |
| LDL | ||||||||||||||
| Triglycerides (mg/dL) | 57 | 7.8 (0.8) | 50 | 9.6 (0.8) | 0.1 | 8.6 (0.8) | 11.5 (0.9) | 0.03 | 8.5 (0.8) | 11 (0.8)2 | 0.04 | 8.7 (0.7) | 10 (0.8)2 | 0.2 |
| Apo C-III (mg/dL) | 59 | 1.50 (0.14) | 56 | 1.96 (0.15) | 0.03 | 1.5 (0.14) | 2.0 (0.15) | 0.02 | 1.4 (0.13) | 2.0 (0.14) | <0.01 | 1.5 (0.13) | 1.8 (0.14) | 0.1 |
| Cholesterol (mg/dL) | 59 | 10 (1.3) | 52 | 15 (1.4) | 0.02 | 9.2 (1.4) | 15 (1.5) | <0.01 | 8.9 (1.2) | 14 (1.3) | <0.01 | 8.2 (1.2)2 | 14 (1.3) | <0.01 |
| Apo B (mg/dL) | 43 | 6.0 (1.0) | 45 | 9.2 (1.0) | 0.02 | 6.1 (1.0) | 9.8 (0.9) | <0.01 | 6.0 (0.8) | 8.8 (0.8) | 0.01 | 5.5 (0.7) | 8.1 (0.7) | 0.01 |
| Apo E (mg/dL) | 75 | 0.42 (0.03) | 65 | 0.36 (0.04) | 0.3 | 0.41 (0.03) | 0.37 (0.03) | 0.5 | 0.41 (0.03) | 0.37 (0.04) | 0.4 | 0.41 (0.03) | 0.37 (0.04) | 0.4 |
| Apo E:apo B (mol/mol) | 42 | 1.62 (0.17) | 43 | 0.97 (0.17) | 0.01 | 1.44 (0.15) | 0.96 (0.15) | 0.03 | 1.58 (0.18) | 0.92 (0.18) | 0.01 | 1.78 (0.22) | 1.04 (0.22) | 0.02 |
| HDL (mg/dL) | ||||||||||||||
| Apo C-III | 59 | 9.4 (0.9) | 56 | 12 (1.0) | 0.04 | 9.5 (0.09) | 10 (0.9) | 0.7 | 9.2 (0.9) | 9.3 (0.9) | 0.9 | 9.7 (0.8) | 9.5 (0.8) | 0.8 |
Values are presented as least-squares means; SEs in parentheses. CARB, carbohydrate diet; UNSAT, unsaturated fats diet; PROT, protein diet; Apo/apo, apolipoprotein; LDL-C, LDL cholesterol. P values for comparison of blacks and whites were derived from a generalized linear model adjusted for age, sex, and site of recruitment.
Significant change from baseline, P < 0.05 (generalized linear model adjusted for age, sex, and site of recruitment).
Because diet affects lipoprotein profile and diet was not controlled in the free-living state, we compared the self-selected diets in blacks and whites to see if this might explain the lipid and lipoprotein differences. On average, blacks reported that they consumed about half the amount of alcohol per day than was reported by whites (P < 0.01) (Table 3). The difference in these reports was confounded by site of recruitment and sex, with participants from Boston reporting consuming nearly 3 times as much as those reported in Baltimore and men consuming 6 times as much as women. The significant difference in reported alcohol intake between blacks and whites was eliminated in the model that adjusted for site of recruitment and sex.
TABLE 3.
Free-living diet composition for select nutrients in blacks (n = 87) compared with whites (n = 71)1
| Univariate analysis |
Multivariate analysis2 |
|||||
| Black | White | P value | Black | White | P value | |
| Calories (kcal) | 2267 (126) | 2355 (140) | 0.6 | 2298 (131) | 2317 (147) | 0.9 |
| Alcohol | ||||||
| (% kcal) | 1.2 (0.3) | 2.0 (0.3) | 0.05 | 1.6 (0.3) | 1.5 (0.3) | 0.9 |
| (g/d) | 3.2 (0.9) | 7.0 (1.0) | <0.01 | 4.4 (0.8) | 5.6 (0.9) | 0.4 |
| Carbohydrate (% kcal) | 51.5 (0.9) | 47.9 (1.0) | <0.01 | 51.1 (0.9) | 48.3 (1.0) | 0.05 |
| Protein (% kcal) | 17.5 (0.4) | 17.3 (0.5) | 0.8 | 17.2 (0.5) | 17.6 (0.5) | 0.6 |
| Animal (% kcal) | 12.7 (0.5) | 11.5 (0.5) | 0.08 | 12.5 (0.5) | 11.7 (0.5) | 0.3 |
| Other (% kcal) | 4.8 (0.2) | 5.9 (0.2) | <0.01 | 4.7 (0.2) | 5.9 (0.3) | <0.01 |
| Fat (% kcal) | 29.9 (0.7) | 32.8 (0.7) | <0.01 | 30.1 (0.7) | 32.5 (0.8) | 0.02 |
| Saturated fat (% kcal) | 10.7 (0.3) | 12.0 (0.3) | <0.01 | 10.8 (0.3) | 11.9 (0.4) | 0.05 |
| Monounsaturated fat (% kcal) | 12.6 (0.3) | 13.6 (0.4) | 0.02 | 12.7 (0.3) | 13.5 (0.4) | 0.1 |
| Polyunsaturated fat (% kcal) | 6.6 (0.2) | 7.2 (0.2) | 0.02 | 6.6 (0.2) | 7.2 (0.2) | 0.05 |
| Omega-3 fatty acids (% kcal) | 0.68 (0.02) | 0.67 (0.02) | 0.7 | 0.68 (0.02) | 0.68 (0.03) | 0.9 |
| Long-chain omega-3 fatty acids (% kcal) | 0.22 (0.02) | 0.17 (0.02) | 0.02 | 0.21 (0.02) | 0.18 (0.02) | 0.1 |
| Omega-6 fatty acids (% kcal) | 5.1 (0.2) | 5.7 (0.2) | 0.01 | 5.1 (0.2) | 5.6 (0.2) | 0.05 |
| Saturated fat (% of total fat) | 35.9 (0.5) | 26.3 (0.6) | 0.6 | 35.9 (0.6) | 36.3 (0.6) | 0.7 |
| Monounsaturated fat (% of total fat) | 41.9 (0.3) | 41.2 (0.3) | 0.1 | 41.9 (0.3) | 41.1 (0.3) | 0.07 |
| Polyunsaturated fat (% of total fat) | 22.2 (0.6) | 22.5 (0.6) | 0.8 | 22.1 (0.6) | 22.6 (0.6) | 0.6 |
| Fiber (g/1000 kcal) | 10.1 (0.5) | 11.2 (0.5) | 0.1 | 10.0 (0.5) | 11.4 (0.5) | 0.06 |
| Total folate (μg/1000 kcal) | 266 (19) | 317 (21) | 0.07 | 254 (19) | 331 (21) | 0.01 |
| Cholesterol (mg/d) | 353 (22) | 327 (25) | 0.4 | 356 (23) | 324 (26) | 0.4 |
| Vitamin E (mg/d) | 59.6 (10.0) | 59.5 (11.1) | 0.9 | 57.2 (10.4) | 62.5 (11.6) | 0.8 |
| Sodium (mg/d) | 2222 (151) | 2468 (167) | 0.3 | 2242 (158) | 2443 (177) | 0.4 |
Values are means; SEs in parentheses.
Multivariate linear regression model adjusted for site of enrollment, sex, BMI, and age. Assessed by the Walter Willett food-frequency questionnaire (version 88GP; Channing Laboratory, Boston, MA). Four of the 162 eligible participants did not have food-frequency questionnaire data available.
Blacks obtained a smaller percentage of calories from saturated and unsaturated fats than did whites and a greater percentage of their calories from carbohydrate. Percentage of calories from carbohydrate was significantly related to apo C-III and triglyceride concentrations in VLDL with apo C-III in a univariate model, but these associations lost significance when race was added to the model, suggesting that carbohydrate intake was acting as a marker of race in the model. A diet richer in carbohydrate would be expected to result in a higher plasma triglyceride and apo C-III concentration, although in our population as in others plasma triglyceride and apo C-III was lower in blacks than in whites. Blacks also obtained less of their protein from nonanimal sources than did whites. The percentage of calories from long-chain omega-3 (n–3) fatty acids was slightly higher in blacks than in whites, whereas the percentage from omega-6 fatty acids was lower. After adjustment for site of recruitment and sex, blacks consumed 12% less fiber (P = 0.06) and 23% less folate (P = 0.01) than did whites (Table 3). These differences in self-selected diets between blacks and whites do not explain the differences in lipoprotein profiles that we observed.
Lipid and lipoprotein differences comparing blacks and whites while consuming study diets
LDL with apo C-III
On each of the 3 diets, blacks maintained a 32–38% lower concentration of LDL with apo C-III (presented in Table 2 as apo B in LDL with apo C-III) as compared with whites (P < 0.02) and 36–41% lower concentrations of cholesterol in LDL with apo C-III (Table 2). Concentrations of apo C-III in LDL with apo C-III were lower in blacks compared with whites after the CARB and UNSAT diets but not after the PROT diet.
Triglycerides and apo C-III
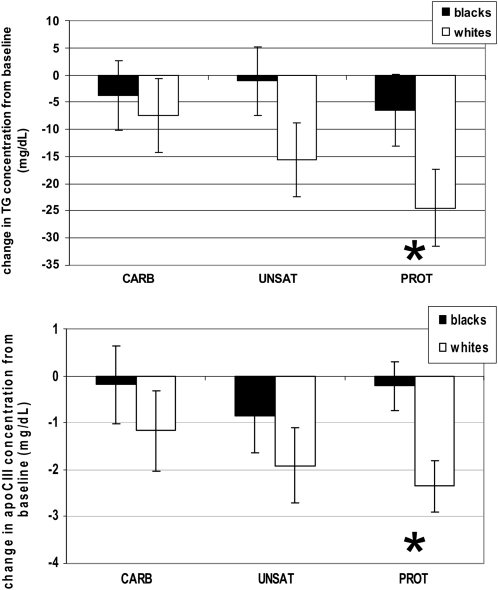
Mean plasma total triglycerides and apo C-III, although lower in blacks than in whites at baseline, were no longer significantly different after the study diets (Table 2) because the diets reduced plasma triglycerides and apoC-III in whites more than in blacks (Figure 1), bringing the means for the 2 groups closer together. Apo C-III in VLDL was significantly lower in blacks than in whites after the UNSAT diet but not after the CARB and PROT diets (Table 2).
FIGURE 1.
Mean (±SEM) changes from baseline in plasma TG and apo C-III by diet in blacks and whites. The study diets reduced plasma triglyceride (TG) (top) and apolipoprotein (apo) C-III (bottom) in whites more than in blacks, after adjustment for baseline concentrations. Plasma TG: blacks, n = 57; whites, n = 50; plasma apo C-III: blacks, n = 59; whites, n = 56. *P for race < 0.05 in the linear regression model, adjusted for baseline plasma TG, sex, age, and site of recruitment, indicating that the differences from baseline differ significantly by race. CARB, carbohydrate diet; UNSAT, unsaturated fats diet; PROT, protein diet.
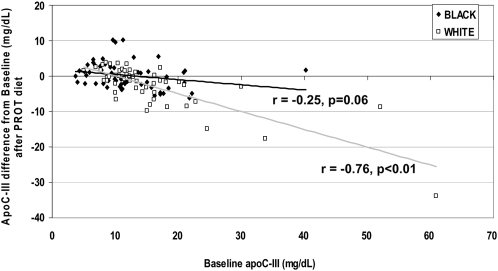
It could be argued that these differential effects of diet were due to the lower mean triglyceride and apo C-III concentrations in blacks at baseline—a "floor effect" that defines a lower limit to dietary responses. To test this, we fit 2 regression models relating change from baseline in plasma triglycerides or apo C-III to baseline plasma triglyceride or apo C-III concentration (to match the dependent variable) with control for dichotomous race, sex, age, BMI, and site of recruitment. All 3 diets showed trends toward a smaller reduction in triglycerides by the diets from baseline in blacks compared with whites, with the largest apparent difference in diet effect occurring after the PROT diet. There was a 15-mg/dL and 23-mg/dL decrease in triglycerides after the UNSAT and PROT diets in whites, respectively (P < 0.02), with no significant change in blacks. We then added an interaction term between race and baseline plasma triglycerides to the model. The interaction term was significant in all 3 diets (P < 0.02), indicating that there is a difference in how blacks’ and whites’ triglyceride concentrations respond to the diets. Race is also a significant predictor of the change from baseline in plasma apo C-III (P < 0.01 comparing races), with the largest difference between races after the PROT diet where blacks showed a nonsignificant decrease of 0.2 mg/dL compared with a significant decrease of 2.3 mg/dL in whites (Figure 2). Whites also showed a significant decrease of 1.9 mg/dL after the UNSAT diet whereas blacks showed none. The interaction term between baseline apo C-III and race was only significant after the PROT diet (P < 0.01), where the effect of diet was greatest in whites. As with triglycerides, the higher the baseline concentration of plasma apo C-III, the more the diets lowered plasma apo C-III from baseline concentrations in whites. This effect was greatly attenuated almost to the point of nonexistence in blacks. This difference was especially evident in the PROT diet, which resulted in the greatest apo C-III changes from baseline.
FIGURE 2.
Higher baseline apolipoprotin (apo) C-III concentrations were associated with greater reductions in plasma apo C-III from baseline in whites than in blacks (n = 115, 57 blacks and 58 whites). This effect remained with the top 5 outliers removed from both groups (not shown). r = correlation coefficient comparing baseline apo C-III and change from baseline in apo C-III after the protein (PROT) diet. P = P value for correlation coefficient; P value for race = 0.03 in the linear regression model comparing change from baseline apo C-III after the PROT diet to baseline apo C-III, adjusted for race, sex, age, and site of recruitment.
Apo B and LDL cholesterol
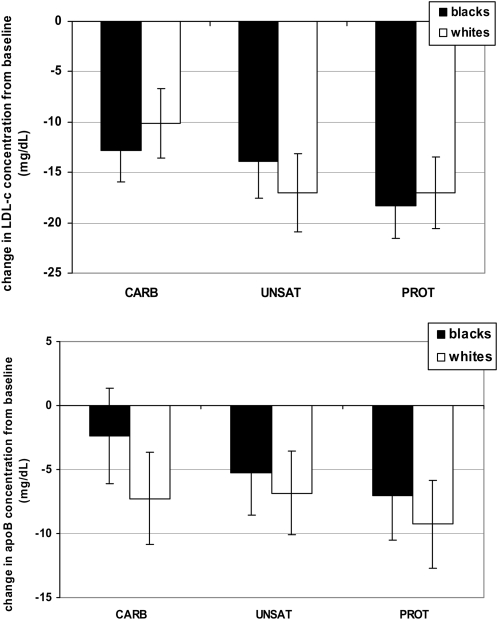
The study diet lowered plasma total apo B and LDL cholesterol similarly in blacks and whites (Figure 3). Plasma total apo B concentrations remained similar between the races after the 3 study diets (Table 2), with the UNSAT and PROT diets reducing concentrations by 6–10% in both races. LDL cholesterol was reduced by 7–15% (P < 0.03) in both blacks and whites after all 3 study diets, and LDL cholesterol in blacks remained 12–16% lower than in whites (Table 2). Cholesterol in LDL without apo C-III (the major apo B lipoprotein type) was 9–13% lower in blacks than in whites in the multivariate model after the study diets, significantly so for the PROT and CARB diets but not for the UNSAT diet. These postdiet racial differences are similar to those while consuming the baseline self-selected diets. The diet changes from baseline in LDL without apo C-III did not differ between the races.
FIGURE 3.
Mean (±SEM) changes from baseline in plasma LDL cholesterol and apolipoprotein (apo) B by diet in blacks and whites. The study diets reduced LDL cholesterol (LDL-c) (top) and apo B (bottom) equally in whites and blacks. LDL-c: blacks, n = 59; whites, n = 52; plasma apo B: blacks, n = 43; whites, n = 45. All P values for race >0.05 in the linear regression models, adjusted for race, sex, age, and site of recruitment. CARB, carbohydrate diet; UNSAT, unsaturated fats diet; PROT, protein diet.
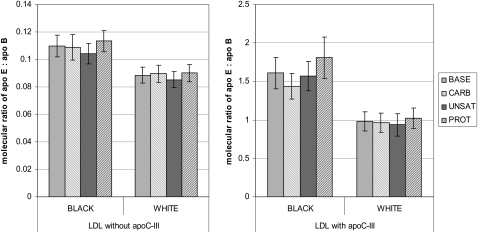
Apo E
Blacks had 14–18% higher plasma total apo E after all 3 diets compared with whites (Table 2) and a higher apo E:apo B ratio in LDL with apo C-III (Figure 4). All 3 diets reduced plasma apo E compared with the baseline diet in both blacks (6–9%) and whites (11–16%).
FIGURE 4.
Molecular ratio of apolipoprotein (apo) E to apo B in LDL lipoproteins with and without apo C-III at baseline (BASE) and after the study diets in blacks and whites. Data are presented as mean (±SEM) ratios of molecules of apo E to molecules of apo B. Blacks, n = 42; whites, n = 43. All P values for race <0.05 in the univariate regression models with race. P value for race in LDL with apo C-III remained significant after adjustment for sex, age, and site of recruitment (all P ≤ 0.03), whereas P = 0.08–0.2 for LDL without apo C-III. CARB, carbohydrate diet; UNSAT, unsaturated fats diet; PROT, protein diet.
DISCUSSION
Apo C-III can be present on apo B–containing or apo A-I–containing (ie, HDL) lipoproteins but is not integral to the basic lipoprotein particle structure; thus, particles exist both with and without apo C-III. Apo B–containing lipoproteins with apo C-III are enriched in triglycerides and cholesterol and have reduced clearance from plasma. The concentration of apo C-III in VLDL and LDL is highly and independently predictive of CHD, more so than triglycerides alone (23). Above all, LDL particles with apo C-III, remnant particles produced by partial lipolysis in plasma of VLDL with apo C-III (26), are the lipoprotein particle type most predictive for CHD in patients with type 2 diabetes (21). apo C-III inhibits direct clearance of VLDL particles from plasma, causing them to be metabolized to LDL (30). New research strengthens the association between CHD and apo C-III by showing that apo C-III increases adhesion of human monocytes to endothelial cells and activates proinflammatory molecules such as nuclear transcription factor κB in these cells (28, 29, 38).
When consuming their usual diets, blacks had a much lower concentration of atherogenic LDL lipoproteins containing apo C-III that could not be explained by differences in diet. For example, blacks reported consuming 4% more calories from carbohydrate and less fat than did whites. Increases in dietary carbohydrate increase plasma triglyceride and apo C-III. After the controlled study diets, blacks continued to have lower LDL with apo C-III, and these racial differences remained consistent even after adjustment for insulin sensitivity (HOMA index) and obesity (BMI). Blacks had a higher BMI and similar HOMA index to whites, yet had lower triglyceride and apo C-III concentrations. Given all of this, we suggest that there is some inherent racial difference in the metabolism of apo C-III–containing apo B lipoproteins that produces this more favorable lipoprotein profile in blacks. One plausible mechanism for these racial differences lies with apo E. Animal studies report that plasma apo E increases the clearance rate of apo B particles through recognition and uptake by liver receptors (31, 39). A study of the kinetics of apo B metabolism in humans showed that apo E when present with apo C-III directs flux from lipolysis toward clearance, limiting LDL formation (26). The ratio of molecules of apo E to apo B in LDL with and without apo C-III was higher in blacks than in whites, suggesting a better likelihood for clearance of these atherogenic particles. In the aforementioned kinetics study, the ratio of apo E to apo B in VLDL correlated with its fractional catabolic rate [Figure 7 in reference (26)].
In a global test across all diets, blacks had significantly lower concentrations of apo C-III than did whites in total plasma and in their VLDL and LDL lipoproteins. Triglyceride correlates with apo C-III, and we observed that blacks also had significantly lower triglyceride in total plasma, VLDL with and without apo C-III, and LDL with apo-C-III in the global test. From a public health perspective, the differences in triglyceride are striking. In this population, 10% of blacks exhibited plasma triglyceride concentrations above the generally recognized cutoff for elevated plasma triglyceride of 150 mg/dL, whereas 23% of whites fell above the cutoff. Over half of the blacks had plasma triglycerides <70 mg/dL, whereas less than 20% of whites fit that category.
In our previous publication we noted that we were surprised to find that the UNSAT diet did not significantly lower triglycerides when it replaced carbohydrate (32), as has been observed in other studies (40). We now find that the UNSAT diet does reduce plasma triglycerides in whites but not in blacks. Thus, the lack of a significant effect in the total cohort resulted from the combination of highly responsive whites and nonresponsive blacks. Most previous studies had entirely or predominantly white populations, and our findings in the white participants agree with this literature (40).
The controlled study diets lowered plasma apo C-III and triglycerides from concentrations on the participants’ usual diets in whites but not in blacks, bringing whites closer to the low means of blacks and eliminating the large differences between the races in these atherogenic lipoprotein components. We observed that the lack of diet effects on triglycerides and apo C-III in blacks is independent of their lower baseline concentrations. The specific reasons for this cannot be ascertained from this study. Whatever the mechanism, dietary therapies to reduce atherogenic apo C-III and triglyceride that are useful in whites may not prove to be as successful in blacks. However, these diets may still be effective in reducing CHD risk in blacks through reductions in blood pressure, cholesterol, and apo B.
Strengths and limitations
The sample size was large, and the participants were demographically heterogeneous, which strengthens the application of the results to the general US population. Statistical power was high due to recruitment of nearly equal numbers of blacks and whites and the crossover design. Risk of bias was low due to similarly high rates of adherence to and completeness of follow-up in both races after all 3 of the diets. Changes in lipids and lipoproteins can be attributed to dietary factors because other important factors that might elicit these changes were successfully controlled for (ie, weight, calorie intake, and alcohol consumption patterns).
The relatively brief duration of each diet period does not allow for assessment of permanence of lipoprotein changes. However, for the conventional lipid risk factors—plasma total cholesterol and triglycerides, HDL cholesterol, and LDL cholesterol—the 4-wk results were similar to the 6-wk results, suggesting that a new baseline was reached. The controlled diet design makes it difficult to gauge the success of long-term adherence to each diet when the diet is adopted by people in a free-living, uncontrolled environment, which is essential to continued CHD risk reduction. Because the free-living diet was not controlled, examination of changes from baseline elicited by study diets, where we have observed the largest diet effects, are not as robust as comparison between study diets.
Conclusions
Based solely on lipoprotein profile, blacks would be expected to have lower risk of CHD than whites, independent of dietary intake. However, epidemiologic studies report otherwise. Thus, blacks are susceptible to CHD at lower concentrations of these lipid and lipoprotein risk factors compared with whites, possibly due to their higher rates of hypertension, diabetes, and obesity, eclipsing their atheroprotective lipoprotein profile. It will be important to determine risk curves in blacks for apo C-III and triglyceride-related lipoproteins to know if current recommendations should be race-specific for healthy concentrations for these lipids and lipoproteins. If the risk curves are similar for blacks and whites, then there must be other, very strong adverse risk factors in blacks to overcome the protective influence of their favorable lipoprotein profile. Although the study diets are useful for reduction of CHD risk by reducing apo B, LDL cholesterol, and blood pressure in both races, they did not lower plasma triglycerides and apo C-III in blacks.
Acknowledgments
The authors’ responsibilities were as follows—JDF: full access to all study data and responsible for the integrity of the data and the accuracy of the data analysis; LJA, FMS, and VJC: study concept and design; JDF, FMS, LJA, and VJC: acquisition of data; JDF, FMS, and VJC: analysis and interpretation of data; JDF, FMS, and HC: drafting of the manuscript; JDF, FMS, HC, LJA, VJC, and AES: critical revision of the manuscript for important intellectual content; JDF, FMS, VJC, and HC: statistical analysis; LJA, FMS, and VJC: obtainment of funding; JDF, FMS, LJA, VJC, and AES, administrative, technical, or material support; and JDF, FMS, LJA, and VJC: study supervision. There were no conflicts of interest to report.
REFERENCES
- 1.National Center for Health Statistics. Health, United States, 2007 with chartbook on trends in the health of Americans. Hyattsville, MD: National Center for Health Statistics, 2007 [PubMed] [Google Scholar]
- 2.Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: final data for 2005. Natl Vital Stat Rep 2008;56:1–120 [PubMed] [Google Scholar]
- 3.Pleis JR, Lethbridge-Çejku M. Summary health statistics for U.S. adults: National Health Interview Survey, 2006. National Center for Health Statistics. Vital Health Stat 2007;10 [PubMed] [Google Scholar]
- 4.Kelley-Hedgepeth A, Lloyd-Jones DM, Colvin A, et al. Ethnic differences in C-reactive protein concentrations. Clin Chem 2008;54:1027–37 [DOI] [PubMed] [Google Scholar]
- 5.Wee CC, Mukamal KJ, Huang A, Davis RB, McCarthy EP, Mittleman MA. Obesity and C-reactive protein levels among white, black, and Hispanic US adults. Obesity (Silver Spring) 2008;16:875–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cowie CC, Howard BV, Harris MI. Serum lipoproteins in African Americans and whites with non-insulin-dependent diabetes in the US population. Circulation 1994;90:1185–93 [DOI] [PubMed] [Google Scholar]
- 7.Holvoet P, Jenny NS, Schreiner PJ, Tracy RP, Jacobs DR. The relationship between oxidized LDL and other cardiovascular risk factors and subclinical CVD in different ethnic groups: the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis 2007;194:245–52 [DOI] [PubMed] [Google Scholar]
- 8.Stein E, Kushner H, Gidding S, Falkner B. Plasma lipid concentrations in nondiabetic African American adults: associations with insulin resistance and the metabolic syndrome. Metabolism 2007;56:954–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sumner AE, Cowie CC. Ethnic differences in the ability of triglyceride levels to identify insulin resistance. Atherosclerosis 2008;196:696–703 [DOI] [PubMed] [Google Scholar]
- 10.Sumner AE, Vega GL, Genovese DJ, Finley KB, Bergman RN, Boston RC. Normal triglyceride levels despite insulin resistance in African Americans: role of lipoprotein lipase. Metabolism 2005;54:902–9 [DOI] [PubMed] [Google Scholar]
- 11.Executive Summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285:2486–97 [DOI] [PubMed] [Google Scholar]
- 12.Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. J Cardiovasc Risk 1996;3:213–9 [PubMed] [Google Scholar]
- 13.Sarwar N, Danesh J, Eiriksdottir G, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation 2007;115:450–8 [DOI] [PubMed] [Google Scholar]
- 14.Chien KL, Hsu HC, Su TC, Chen MF, Lee YT, Hu FB. Apolipoprotein B and non-high density lipoprotein cholesterol and the risk of coronary heart disease in Chinese. J Lipid Res 2007;48:2499–505 [DOI] [PubMed] [Google Scholar]
- 15.Ingelsson E, Schaefer EJ, Contois JH, et al. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA 2007;298:776–85 [DOI] [PubMed] [Google Scholar]
- 16.Onat A, Ozhan H, Can G, Hergenc G, Karabulut A, Albayrak S. [Serum apolipoprotein B is superior to LDL-cholesterol level in predicting incident coronary disease among Turks.] Anadolu Kardiyol Derg 2007;7:128–33(in Turkish) [PubMed] [Google Scholar]
- 17.Pischon T, Girman CJ, Sacks FM, Rifai N, Stampfer MJ, Rimm EB. Non-high-density lipoprotein cholesterol and apolipoprotein B in the prediction of coronary heart disease in men. Circulation 2005;112:3375–83 [DOI] [PubMed] [Google Scholar]
- 18.Simon A, Chironi G, Gariepy J, Del Pino M, Levenson J. Differences between markers of atherogenic lipoproteins in predicting high cardiovascular risk and subclinical atherosclerosis in asymptomatic men. Atherosclerosis 2005;179:339–44 [DOI] [PubMed] [Google Scholar]
- 19.Talmud PJ, Hawe E, Miller GJ, Humphries SE. Nonfasting apolipoprotein B and triglyceride levels as a useful predictor of coronary heart disease risk in middle-aged UK men. Arterioscler Thromb Vasc Biol 2002;22:1918–23 [DOI] [PubMed] [Google Scholar]
- 20.Williams K, Sniderman AD, Sattar N, D'Agostino R, Jr, Wagenknecht LE, Haffner SM. Comparison of the associations of apolipoprotein B and low-density lipoprotein cholesterol with other cardiovascular risk factors in the Insulin Resistance Atherosclerosis Study (IRAS). Circulation 2003;108:2312–6 [DOI] [PubMed] [Google Scholar]
- 21.Lee SJ, Campos H, Moye LA, Sacks FM. LDL containing apolipoprotein CIII is an independent risk factor for coronary events in diabetic patients. Arterioscler Thromb Vasc Biol 2003;23:853–8 [DOI] [PubMed] [Google Scholar]
- 22.Luc G, Fievet C, Arveiler D, et al. Apolipoproteins C-III and E in apoB- and non-apoB-containing lipoproteins in two populations at contrasting risk for myocardial infarction: the ECTIM study. Etude Cas Temoins sur Infarctus du Myocarde. J Lipid Res 1996;37:508–17 [PubMed] [Google Scholar]
- 23.Sacks FM, Alaupovic P, Moye LA, et al. VLDL, apolipoproteins B, CIII, and E, and risk of recurrent coronary events in the Cholesterol and Recurrent Events (CARE) trial. Circulation 2000;102:1886–92 [DOI] [PubMed] [Google Scholar]
- 24.Aalto-Setala K, Weinstock PH, Bisgaier CL, Wu L, Smith JD, Breslow JL. Further characterization of the metabolic properties of triglyceride-rich lipoproteins from human and mouse apoC-III transgenic mice. J Lipid Res 1996;37:1802–11 [PubMed] [Google Scholar]
- 25.de Silva HV, Lauer SJ, Wang J, et al. Overexpression of human apolipoprotein C-III in transgenic mice results in an accumulation of apolipoprotein B48 remnants that is corrected by excess apolipoprotein E. J Biol Chem 1994;269:2324–35 [PubMed] [Google Scholar]
- 26.Zheng C, Khoo C, Ikewaki K, Sacks FM. Rapid turnover of apolipoprotein C-III-containing triglyceride-rich lipoproteins contributing to the formation of LDL subfractions. J Lipid Res 2007;48:1190–203 [DOI] [PubMed] [Google Scholar]
- 27.Mendivil CO, Zheng C, Furtado J, Lel J, Sacks FM. Metabolism of very-low-density lipoprotein and low-density lipoprotein containing apolipoprotein C-III and not other small apolipoproteins. Arterioscler Thromb Vasc Biol 2009;30:239–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kawakami A, Aikawa M, Alcaide P, Luscinskas FW, Libby P, Sacks FM. Apolipoprotein CIII induces expression of vascular cell adhesion molecule-1 in vascular endothelial cells and increases adhesion of monocytic cells. Circulation 2006;114:681–7 [DOI] [PubMed] [Google Scholar]
- 29.Kawakami A, Aikawa M, Nitta N, Yoshida M, Libby P, Sacks FM. Apolipoprotein CIII-induced THP-1 cell adhesion to endothelial cells involves pertussis toxin-sensitive G protein- and protein kinase C alpha-mediated nuclear factor-kappaB activation. Arterioscler Thromb Vasc Biol 2007;27:219–25 [DOI] [PubMed] [Google Scholar]
- 30.Zheng C, Khoo C, Furtado J, Sacks FM. Apolipoprotein C-III and the metabolic basis for hypertriglyceridemia and the dense low-density lipoprotein phenotype. Circulation 2010;121:1722–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahley RW, Rall SC., Jr Apolipoprotein E: far more than a lipid transport protein. Annu Rev Genomics Hum Genet 2000;1:507–37 [DOI] [PubMed] [Google Scholar]
- 32.Furtado JD, Campos H, Appel L, et al. Effect of protein, unsaturated fat, and carbohydrate intakes on plasma apolipoprotein B and VLDL and LDL containing apolipoprotein C-III: results from the OmniHeart Trial. Am J Clin Nutr 2008;87:1623–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carey VJ, Bishop L, Charleston J, et al. Rationale and design of the Optimal Macro-Nutrient Intake Heart Trial to Prevent Heart Disease (OMNI-Heart). Clin Trials 2005;2:529–37 [DOI] [PubMed] [Google Scholar]
- 34.Appel LJ, Sacks FM, Carey VJ, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA 2005;294:2455–64 [DOI] [PubMed] [Google Scholar]
- 35.Obarzanek E, Sacks FM, Vollmer WM, et al. Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) Trial. Am J Clin Nutr 2001;74:80–9 [DOI] [PubMed] [Google Scholar]
- 36.Swain JF, McCarron PB, Hamilton EF, Sacks FM, Appel LJ. Characteristics of the diet patterns tested in the Optimal Macronutrient Intake Trial to Prevent Heart Disease (OmniHeart): options for a heart-healthy diet. J Am Diet Assoc ( in press ) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Souza RJ, Swain JF, Appel LJ, Sacks FM. Alternatives for macronutrient intake and chronic disease: a comparison of the OmniHeart diets with popular diets and with dietary recommendations. Am J Clin Nutr 2008;88:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kawakami A, Aikawa M, Libby P, Alcaide P, Luscinskas FW, Sacks FM. Apolipoprotein CIII in apolipoprotein B lipoproteins enhances the adhesion of human monocytic cells to endothelial cells. Circulation 2006;113:691–700 [DOI] [PubMed] [Google Scholar]
- 39.Kashyap VS, Santamarina-Fojo S, Brown DR, et al. Apolipoprotein E deficiency in mice: gene replacement and prevention of atherosclerosis using adenovirus vectors. J Clin Invest 1995;96:1612–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr 2003;77:1146–55 [DOI] [PubMed] [Google Scholar]