Abstract
The massive depletion of gastrointestinal-tract CD4 T cells is a hallmark of the acute phase of HIV infection. In contrast, the depletion of the lower-respiratory-tract mucosal CD4 T cells as measured in bronchoalveolar lavage (BAL) fluid is more moderate and similar to the depletion of CD4 T cells observed in peripheral blood (PB). To understand better the dynamics of disease pathogenesis and the potential for the reconstitution of CD4 T cells in the lung and PB following the administration of effective antiretroviral therapy, we studied cell-associated viral loads, CD4 T-cell frequencies, and phenotypic and functional profiles of antigen-specific CD4 T cells from BAL fluid and blood before and after the initiation of highly active antiretroviral therapy (HAART). The major findings to emerge were the following: (i) BAL CD4 T cells are not massively depleted or preferentially infected by HIV compared to levels for PB; (ii) BAL CD4 T cells reconstitute after the initiation of HAART, and their infection frequencies decrease; (iii) BAL CD4 T-cell reconstitution appears to occur via the local proliferation of resident BAL CD4 T cells rather than redistribution; and (iv) BAL CD4 T cells are more polyfunctional than CD4 T cells in blood, and their functional profile is relatively unchanged after the initiation of HAART. Taken together, these data suggest mechanisms for mucosal CD4 T-cell depletion and interventions that might aid in the reconstitution of mucosal CD4 T cells.
The assessment of the degree of memory CD4 T-cell depletion at mucosal sites during human immunodeficiency virus (HIV) infection is perhaps the most comprehensive way to estimate the impact of HIV on the T-cell pool. As such, the massive depletion of gastrointestinal CD4 T cells is a hallmark of HIV and simian immunodeficiency virus (SIV) infection (5, 12, 17, 19, 20, 30). This depletion occurs during the acute phase of infection and is maintained throughout the chronic phase. Mechanisms underlying this depletion have been shown to include the direct consequence of target cell infection (4, 19) and virus-induced Fas-mediated apoptosis (17). However, while it is clear that the substantial depletion of CD4 T cells occurs in the gastrointestinal (GI) tract and vaginal mucosa (31) of SIV-infected macaques and HIV-infected individuals (5, 12, 20, 30), similar depletion does not manifest at all mucosal sites, particularly the lung, in human studies (4).
Highly active antiretroviral therapy (HAART) has significantly improved the prognosis of HIV-infected individuals (15, 16). Individuals who initiate HAART before their CD4 T-cell counts in peripheral blood (PB) fall below 350 cells/μl have significantly improved survival compared to that of individuals who initiate HAART with CD4 T-cell counts less than 350 cells/μl (15). Several studies also have shown that when HAART is initiated after CD4 T-cell counts fall below 350 cells/μl, the reconstitution of CD4 T cells in the GI tract is very poor, even after years of therapy (10, 12, 21). However, HIV-infected individuals treated with HAART during the early phase of infection may reconstitute CD4 T cells in the GI tract (18, 21). In contrast to the GI tract, little is known regarding CD4 T-cell reconstitution in the lung compartment during the course of HIV treatment. Nevertheless, the timing of HAART initiation after infection appears to be an important predictor of successful mucosal T-cell reconstitution.
The massive depletion of CD4 T cells during the acute phase of infection does not occur at all mucosal sites, as CD4 T cells in bronchoalveolar lavage (BAL) are relatively spared and are slowly depleted during the chronic phase of infection (4). Despite this preservation of lung CD4 T cells, diminished BAL T-cell immune responses to certain pathogens have been reported in HIV-infected subjects (14). Given that many patients worldwide have access to and will receive antiretroviral therapy, the study of mucosal responses longitudinally during the course of treatment is likely to enhance our understanding of immune restoration. In addition, the early cellular events following HAART initiation are likely to skew the immune system toward both protective (i.e., immunosurveillance) and pathological (i.e., immune reconstitution inflammatory syndrome) responses. In this context, the study of the human pulmonary immune response remains an important aspect of HIV infection and treatment. To examine the dynamics of lung CD4 T-cell reconstitution, we studied the treatment of naïve HIV-infected individuals longitudinally during their course of HAART. We sampled peripheral blood and BAL T cells prior to, at 1 month, and after 1 year of HAART. From each subject and within each compartment, we examined the proliferative and functional capacity of stimulated CD4 and CD8 T cells.
MATERIALS AND METHODS
Subjects.
The pulmonary immune reconstitution inflammatory syndrome (IRIS) study is an ongoing, prospective observational study designed to assess protective and pathological immune responses in the lung after HAART initiation. HIV-infected subjects who planned to initiate HAART based on clinical criteria were asked to undergo bronchoscopy before initiating treatment and 1 month and 1 year after treatment initiation. Twenty HIV-infected, antiretroviral therapy-naïve subjects who were >18 years of age and free of acute respiratory tract symptoms were recruited for this study. Subjects were ineligible if they had received antiretroviral therapy in the past 12 months. Clinical details are shown in Table 1. HAART regimens were not dictated by protocol, but no patient received a CCR5 antagonist. The study was approved by local institutional review boards, and all subjects provided written informed consent. The viral load (VL) was determined using either the Roche Amplicor Monitor assay or the Roche Ultradirect assay.
TABLE 1.
Subject cohorta
| Subject | Age | Gender | Duration of infection(days) | Baseline CD4 | pVL | Baseline BAL % lymphocyte | Prior lung disease |
|---|---|---|---|---|---|---|---|
| 3001 | 38 | M | 4,800 | 430 | 67,583 | 17 | Pneumonia |
| 3002 | 56 | M | 50 | 37 | 85,208 | 20 | PCP |
| 3003 | 28 | M | 50 | 25 | 24,656 | 10 | |
| 3005 | 48 | M | 1,700 | 92 | 99,787 | 15 | Pneumonia |
| 3006 | 49 | M | 100 | 184 | 31,900 | 20 | |
| 3007 | 37 | M | 200 | 48 | 750,000 | 16 | |
| 3008 | 45 | M | 2,200 | 385 | 64,200 | 5 | |
| 3009 | 47 | M | 2,800 | 395 | 53,400 | 1 | Pneumonia |
| 3010 | 50 | F | 100 | 48 | 3,480 | 1 | Pneumonia |
| 3011 | 43 | F | 350 | 814 | 23,800 | 12 | |
| 3012 | 36 | M | 1,300 | 296 | 24,100 | 2 | |
| 3014 | 24 | M | 50 | 286 | 100,000 | 25 | |
| 3015 | 37 | M | 100 | 308 | 51,100 | 4 | Asthma |
| 3016 | 46 | M | 4,500 | 188 | 100,000 | 24 | |
| 3017 | 49 | M | 2,600 | 649 | 100,000 | 15 | |
| 3018 | 23 | M | 400 | 296 | 750,000 | 30 | |
| 3019 | 46 | M | 5,600 | 16 | 100,000 | 51 | |
| 3021 | 50 | F | 1,000 | 450 | 7,270 | 12 | |
| 3022 | 51 | M | 5,200 | 277 | 46,400 | 9 | Pneumonia |
| 3023 | 43 | M | 700 | 440 | 94,750 | 19 |
pVL, plasma viral load; baseline, day 0 relative to HAART; PCP, Pnuemocystis pneumonia; M, male; F, female. CD4 counts are given as cells/μl blood. HIV duration is an approximation at the baseline.
Samples.
Peripheral blood mononuclear cells were prepared from venous blood by density gradient centrifugation. BAL cells were obtained after anesthetizing the upper airways with a 4% lidocaine nebulizer and the vocal cords and proximal airways with a 1% lidocaine solution. Bronchoscopy with lavage was performed through a fiber optic bronchoscope wedged in a subsegmental bronchus of the right-middle and right-lower lobes as previously described (28). A volume of 150 ml of normal saline at room temperature was instilled in 50-ml aliquots into the medial segment of the right-middle lobe and repeated in the anterior segment of the right-lower lobe. Typically, 300 ml was instilled to obtain a return of 125 to 200 ml of BAL fluid. BAL fluid was filtered through 100-μm nylon mesh (Tetko Inc., Elmsford, NY) to remove debris and was centrifuged at 400 × g for 10 min. Recovered BAL fluid was frozen at −70°C in small aliquots. The cell pellet was washed twice and resuspended in complete medium at 106 cells/ml. Suspended cells then were shipped on wet ice overnight for T-cell analysis. Cell differentials were obtained from cytospin slides.
Flow-cytometric analysis.
Eighteen-parameter flow-cytometric analysis was performed using a FACSAria flow cytometer (Becton Dickinson, San Jose, CA). Fluorescein isothiocyanate (FITC), phycoerythrin (PE), Cy7PE, Cy5.5PE, allophycocyanin (APC), Cy7APC, Alexa700, Texas red PE (TRPE), aqua blue amine reactive dye, and Cascade blue were used as the fluorophores. At least 300,000 live lymphocytes were collected. The list-mode data files were analyzed using FlowJo (Tree Star Inc., Ashland, OR). Functional capacity was determined after Boolean gating, and subsequent analysis was performed using Simplified Presentation of Incredibly Complex Evaluations (SPICE; version 2.9, Mario Roederer, VRC, NIAID, NIH). All values used for analyzing the proportionate representation of responses are background subtracted.
Antigen-specific T-cell assay.
Stimulation was performed on fresh or frozen lymphocytes as described elsewhere (25). Freshly isolated or freshly thawed lymphocytes were resuspended at 106/ml in medium supplemented with 1 μg/ml anti-CD28 and anti-CD49d antibodies. Peptides 15 amino acids in length, overlapping by 11 amino acids and encompassing cytomegalovirus (CMV) pp65 and IE1, were used to stimulate CMV-specific CD8 T cells in the presence of brefeldin A (BFA; 1 μg/ml; Sigma) for 15 h at 37°C. A CMV whole-antigen preparation (Microbix) was used to stimulate CMV-specific CD4 T cells, and Staphylococcus enterotoxin B (SEB; 1 μg/ml; Sigma) was used to mitogenically stimulate CD4 and CD8 T cells. All cells were surface stained for phenotypic markers of interest and intracellularly stained for cytokines (intracellular cytokine staining [ICS]).
Monoclonal antibodies and T-cell phenotyping.
Monoclonal antibodies used for the phenotypic and functional characterization of T-cell subsets were anti-CD3 Alx700, anti-CD45RO TRPE, anti-CD27 Cy5PE, CCR5 PE, anti-CD4 Cy5.5PE, anti-CD8 Cascade blue, anti-gamma interferon (IFN-γ) Cy7PE, anti-Ki67 FITC, anti-tumor necrosis factor (TNF) FITC, and anti-interleukin-2 (IL-2) APC (Becton Dickinson Pharmingen, San Diego, CA). As naïve T cells do not express CCR5, and as HIV-specific T cells are not detectable in the naïve T-cell pool, we report these data as percentages of memory T cells as appropriate. We first gated for memory CD4 and CD8 T cells based upon characteristic expression patterns of CD45RO and CD27. We then determined the percentage of CD4 and CD8 T cells that express CCR5 or are producing cytokines after stimulation.
qPCR.
The quantification of HIV gag DNA in sorted memory CD4 T cells was performed by quantitative PCR (qPCR) by means of the 5′ nuclease (TaqMan) assay with an ABI7700 system (Perkin Elmer, Norwalk, CT) as previously described (3, 8). To quantify cell numbers in each reaction mixture, qPCR was performed simultaneously for albumin gene copy numbers as previously described (9). Standards were constructed for the absolute quantification of gag and albumin copy numbers and were validated with sequential dilutions of 8E5 cell lysates that contain one copy of gag per cell. Duplicate reactions were run and template copies calculated using ABI7700 software.
RESULTS
CD4 T cells reconstitute after 1 year of HAART.
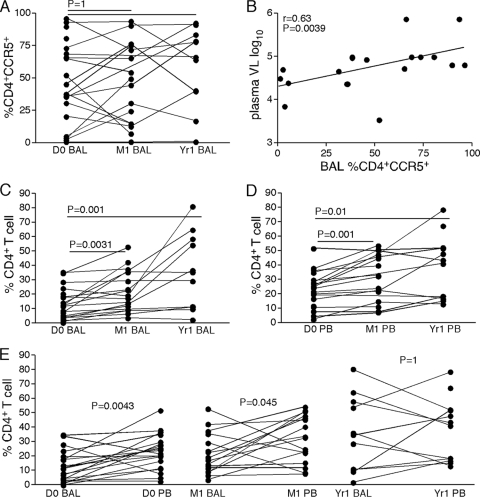
The majority of T cells within mucosal sites are CD45RO+ memory T cells that express the HIV coreceptor CCR5, and while CCR5+ CD4 T cells are preferentially depleted from the GI tract in HIV-infected individuals, CCR5+ CD4 T cells in BAL are present at frequencies similar to those of healthy volunteers in most HIV-infected individuals (4). To determine whether CCR5+ CD4 memory T cells reconstitute the lung compartment, we performed flow cytometry on BAL samples obtained before HAART, 1 month after HAART, and 1 year after HAART. Similarly to our previous cross-sectional study (7), we found comparable frequencies of CCR5+ CD4 memory T cells in BAL samples of HIV-infected and uninfected individuals regardless of HAART duration (Fig. 1 A). Moreover, there was wide variability in the frequencies of CCR5+ CD4 memory T cells in BAL, which was significantly associated with plasma viral loads (Fig. 1B). However, the overall frequencies of total CD4 T cells in BAL were significantly lower than the frequencies of total CD4 T cells in blood of HAART-naïve, HIV-infected individuals (Fig. 1D), but after 1 year of HAART the frequencies of CD4 T cells were similar in blood and BAL (Fig. 1E). These data strongly suggest that the total CD4 T-cell pool in BAL was reconstituted after the initiation of HAART. Indeed, by as early as 1 month after the initiation of HAART, frequencies of CD4 T cells in BAL were significantly higher than the frequencies of CD4 T cells in BAL prior to HAART (Fig. 1C). CD4 T-cell frequencies in BAL were further increased after 1 year of HAART (Fig. 1C). Most individuals had reconstituted CD4 T cells in BAL samples to frequencies observed in HIV-uninfected individuals (not shown). Similarly to BAL, CD4 T cells in blood increased at 1 month and 1 year after HAART (Fig. 1D). These differences between compartments are significant at 1 month but not at 1 year, suggesting it takes many months to reconstitute pulmonary mucosal CD4 T cells.
FIG. 1.
CD4 reconstitution in BAL and PB. (A) Frequencies of CD4 T cells that express CCR5 prior to, after 1 month, and after 1 year of HAART. (B) Association between frequencies of CD4 T cells that express CCR5 in BAL with plasma viral loads. (C) Percentage of CD4 T cells (of all CD3+ T cells) in BAL prior to, after 1 month, and after 1 year of HAART. (D) Percentage of CD4 T cells (of all CD3+ T cells) in PB prior to, after 1 month, and after 1 year of HAART. (E) Comparison of CD4 T-cell frequencies in PB and BAL prior to, after 1 month, and after 1 year of HAART. Wilcoxon's matched-pairs test was used to determine statistical significance.
The preferential infection and subsequent depletion of CD4 T cells at mucosal sites is associated with a lack of the reconstitution of CD4 T cells in the GI tract (21, 22). As we did not find the massive depletion of CD4 T cells in BAL and CD4 T cells appear to reconstitute the lung as early as 1 month after the initiation of HAART, we examined the infection frequencies of CD4 T cells in paired BAL and blood samples prior to, after 1 month, and after 1 year of HAART. We found that the infection frequency of PB and BAL memory CD4 T cells was decreased by 1 month after the initiation of HAART and stabilized thereafter (Fig. 2 A and B). Indeed, the infection frequency of BAL memory CD4 T cells was similar to the infection frequencies of PB memory CD4 T cells at baseline and 1 year, with a significant difference at 1 month (Fig. 2C). Thus, unlike the GI tract, BAL CD4 memory T-cell infection does not affect BAL's ability to reconstitute.
FIG. 2.
Infection frequencies of CD4 T cells in PB and BAL before and after HAART. (A) Frequencies of infected memory CD4 T cells in PB prior to, after 1 month, and after 1 year of HAART. (B) Frequencies of infected memory CD4 T cells in BAL prior to, after 1 month, and after 1 year of HAART. (C) Comparison of memory CD4 T-cell infection frequencies in PB and BAL prior to, after 1 month, and after 1 year of HAART. Wilcoxon's matched pairs test was used to determine statistical significance.
Reconstitution of BAL CD4 T cells involves local proliferation of CD4 T cells.
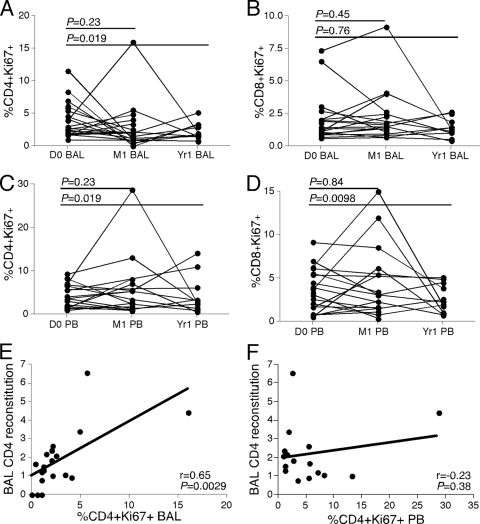
To determine a mechanism by which BAL CD4 T cells are reconstituted after the initiation of HAART, we measured the expression of Ki67 by memory T cells (Fig. 3). Ki67 is a nuclear antigen expressed by all dividing cells and has been used as a measure of immune activation and proliferation in chronically infected individuals. We found similar frequencies of memory Ki67+ CD4 and CD8 T cells in PB and BAL at baseline and 1 month after the initiation of HAART, but these frequencies tended to decrease after 1 year of HAART (Fig. 3A to D). Since local homeostatic proliferation could underlie the reconstitution of CD4 T cells, we compared CD4 T-cell reconstitution in BAL samples to the frequency of Ki67+ memory CD4 T cells at 1 month after HAART. Indeed, we found a significant positive correlation between CD4 reconstitution in BAL (based on fold change) and the proliferation of local CD4 T cells (Fig. 3E). However, there was no correlation between the frequency of Ki67+ memory CD4 T cells in PB and the reconstitution of CD4 T cells in BAL (Fig. 3F). These data suggest that local proliferation in lung or regional lymphoid tissue, rather than redistribution from the blood or distant sites, leads to the reconstitution of CD4 T cells in BAL fluid.
FIG. 3.
Proliferation of T cells in BAL and PB before and after HAART. (A) Frequencies of Ki67+ memory CD4 T cells in BAL prior to, after 1 month, and after 1 year of HAART. (B) Frequencies of Ki67+ memory CD8 T cells in BAL prior to, after 1 month, and after 1 year of HAART. (C) Frequencies of Ki67+ memory CD4 T cells in PB prior to, after 1 month, and after 1 year of HAART. (D) Frequencies of Ki67+ memory CD8 T cells in PB prior to, after 1 month, and after 1 year of HAART. (E) Association between CD4 T-cell reconstitution (fold change from day 0 to 1 month) in BAL and the frequency of memory CD4 T cells in BAL that express Ki67 at 1 month after HAART. (F) Association between CD4 T-cell reconstitution (based upon the fold increase after baseline) in BAL (fold change from day 0 to 1 month) and the frequency of memory CD4 T cells in PB that express Ki67 at 1 month after HAART. Wilcoxon's matched-pairs test or Spearman's rank correlation was used to determine statistical significance.
Functionality of T cells in PB and BAL after HAART.
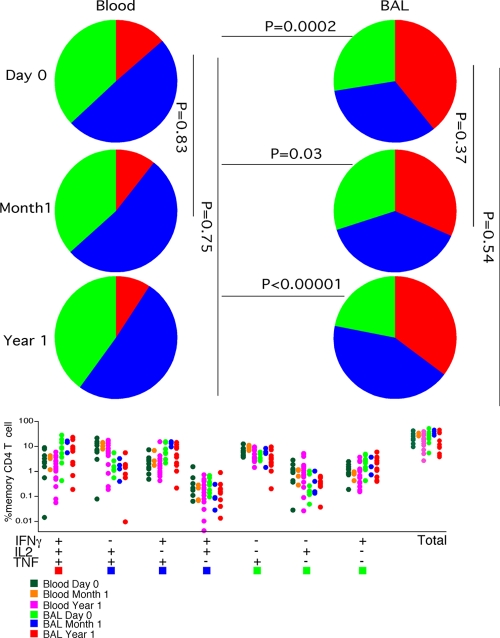
Polyfunctional T cells are capable of secreting more than one effector cytokine, confer protection in some vaccine studies (7), and are associated with a nonprogressive course of HIV disease (2). Based upon the inability to simultaneously produce effector cytokines, the dysfunction of T cells is a hallmark of the chronic phase of HIV infection (2). However, we previously noted that HIV-specific T cells in BAL of untreated HIV-infected subjects were significantly more polyfunctional than T cells in PB (4). The subsequent longitudinal analysis of HIV-specific T-cell responses was not possible, as HIV-specific responses were completely abrogated by HAART (not shown). Therefore, we examined the functionality of CD4 and CD8 T cells in PB and BAL in response to SEB and CMV prior to and after the initiation of HAART. Initially, we mitogenically stimulated T cells in PB and BAL samples with SEB to examine the overall functionality of CD4 (Fig. 4) and CD8 (Fig. 5) T cells. Consistently with the increased functionality of HIV-specific T cells in BAL compared to that of PB, mitogenically stimulated memory CD4 T cells from BAL were significantly more polyfunctional than memory CD4 T cells from PB (Fig. 4). Moreover, the functional profile of memory CD4 T cells in BAL and PB remained fairly constant longitudinally after the initiation of HAART. Indeed, at both 1 month and 1 year the functionality of memory CD4 T cells in PB and BAL were comparable to the functionality of these CD4 T cells measured prior to the initiation of HAART (Fig. 4).
FIG. 4.
Functionality of mitogenically stimulated CD4 T cells in PB and BAL before and after HAART. The frequency and functionality of mitogenically stimulated CD4 T cells in PB and BAL prior to, after 1 month, and after 1 year of HAART. P values represent the results of Mann Whitney U tests. The frequency of the total producing one (green), two (blue), or three (red) cytokines and the relative contribution to the total response were determined using SPICE as described in Materials and Methods.
FIG. 5.
Functionality of mitogenically stimulated CD8 T cells in PB and BAL before and after HAART. Shown are the frequency and functionality of mitogenically stimulated CD8 T cells in PB and BAL prior to, after 1 month, and after 1 year of HAART. P values represent the results of Whitney U tests. The frequency of the total producing one, two, or three cytokines and the relative contribution to the total response were determined using SPICE as described in Materials and Methods.
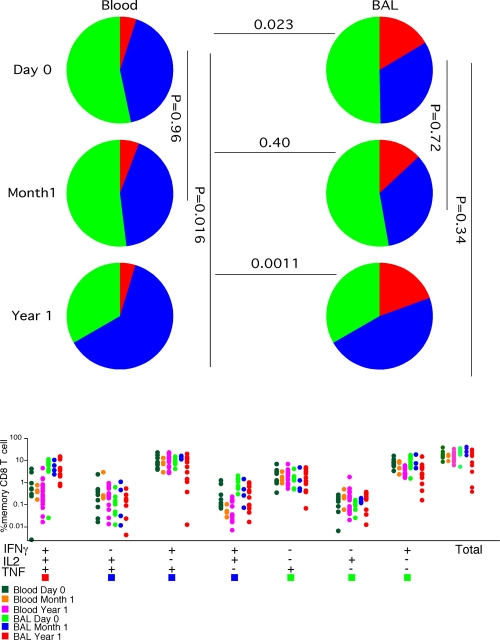
Similar data were obtained from PB and BAL memory CD8 T cells stimulated mitogenically (Fig. 5). With the exception of the 1-month time point, the memory CD8 T cells in BAL were significantly more polyfunctional than the memory CD8 T cells in PB. The lack of statistical significance at the 1-month time point likely is related to the few data points we were able to obtain from memory CD8 T cells in BAL. Moreover, while the functionality of memory CD8 T cells in BAL appeared to remain fairly constant after the initiation of HAART, memory CD8 T cells in PB were significantly more polyfunctional, with higher frequencies of memory CD8 T cells simultaneously producing a combination of TNF-α, IFN-γ, or IL-2 at 1 year after the initiation of HAART compared to those at the treatment-naïve time point. These data suggest that long-term HAART is required to confer the improved functionality of some memory T-cell subsets.
We were unable to study the functionality of HIV-specific T cells beyond the baseline, as their frequencies significantly decrease after the initiation of HAART (6). Thus, we examined the functionality of memory T cells specific for cytomegalovirus (Fig. 6 and 7). In contrast to mitogenically stimulated memory T cells, CMV-specific CD4 (Fig. 6) and CD8 (Fig. 7) T cells tended to be significantly more polyfunctional in PB than BAL regardless of HAART duration, and there was little change in the functionality of CMV-specific T cells in either BAL or PB longitudinally. These data are consistent with previous work demonstrating differences in the clonal hierarchy of antigen-specific T cells in PB and BAL (4).
FIG. 6.
Functionality of CMV-specific CD4 T cells in PB and BAL before and after HAART. Shown are the frequency and functionality of CMV-specific CD4 T cells in PB and BAL prior to, after 1 month, and after 1 year of HAART. P values represent the results of Whitney U tests. The frequency of the total producing one, two, or three cytokines and the relative contribution to the total response were determined using SPICE as described in Materials and Methods.
FIG. 7.
Functionality of CMV-specific CD8 T cells in PB and BAL before and after HAART. Shown are the frequency and functionality of CMV-specific CD8 T cells in PB and BAL prior to, after 1 month, and after 1 year of HAART. P values represent the results of Whitney U tests. The frequency of the total producing one, two, or three cytokines and the relative contribution to the total response were determined using SPICE as described in Materials and Methods.
DISCUSSION
To characterize the pulmonary immune response during the course of HIV treatment, we investigated viral infection, T-cell functionality, CD4 T-cell depletion, and CD4 T-cell reconstitution following HAART from PB and BAL. Five major points emerged: (i) BAL CD4 T cells are not massively depleted or preferentially infected by HIV compared to levels for PB; (ii) CD4 T cells reconstitute following HAART, coincidently with decreases in the frequencies of memory CD4 T cells infected by HIV in vivo; (iii) in PB and BAL, the reconstitution of CD4 T cells in BAL involves the compartmentalized proliferation of memory CD4 T cells; (iv) mitogenically stimulated T cells are more polyfunctional in BAL than in PB, and functionality can improve moderately with long-term HAART; and (v) CMV-specific T cells, on the other hand, are significantly more polyfunctional in PB than in BAL, and functionality remains fairly constant longitudinally after the administration of HAART.
There are a number of reasons for studying the pulmonary immune response during the course of HAART. In HIV-infected subjects, pulmonary infections are common and likely due to the failure of local immunity during the course of disease (14). Additionally, the ability to repeatedly access the lung compartment by BAL permits a relatively noninvasive way to monitor mucosal responses, which has been shown to have prognostic value in early HIV studies (1, 28). Lymphocytes obtained from BAL are analogous to lymphocytes obtained from other noninductive mucosal sites, such as the GI lamina propria, as they lack a naïve population (unlike PB). In pathogenic SIV infections of Asian macaques, CD4 T cells are depleted rapidly from the lung, much like the GI tract, and suggest a common theme of mucosal T-cell depletion in these animals (23, 24).
In contrast to SIV models of infection, our recent cross-sectional human study showed that BAL CCR5+ CD4 memory T lymphocytes, unlike lymphocytes at other mucosal sites, were maintained in HIV-infected subjects (4). This difference in the lung compartment between SIV- and HIV-mediated CD4 T-cell depletion during infection could be due to differences in the kinetics of virus replication, pulmonary host factors such as local concentrations of CCR5-binding chemokines, or the diverse nature of the cohorts enrolled in human studies. Indeed, we found a significant correlation between the frequencies of BAL CCR5+ CD4 memory T cells and plasma viral replication. These data indicate that CCR5+ CD4 memory T cells in BAL support viral replication and are a source of plasma viral load. However, after these cells are depleted, possibly by direct viral infection, plasma viral loads subsequently decrease. Regardless, these data highlight the anatomically restricted immunological occurrences of chronically HIV-infected individuals and suggest that, unlike SIV-infected rhesus macaques, BAL cannot be used as a reflection of occurrences at all mucosal sites.
Our current study suggests that both CCR5− and, to a lesser extent, CCR5+ CD4 T cells are reconstituting the BAL compartment, an event not likely to occur in the GI tract. The differential reconstitution after the initiation of HAART within the GI tract (11, 13, 18, 21) compared to that of BAL might be explained by fibrosis within lymphoid tissue (10, 26, 27). The lung has a paucity of locally organized lymphoid tissue. However, fibrosis described within peripheral lymph nodes (27) and, to a greater extent, within the GI tract (10) clearly correlates with the inability to restore CD4 T-cell pools. Indeed, this hypothesis is consistent with the requirement for the local proliferation of mucosal CD4 T cells upon immune reconstitution within BAL. On the other hand, the contraction of the virally expanded CD8 T-cell pool in BAL may be partially responsible for the increased frequencies of BAL CD4 T cells we observe after the initiation of HAART (29). Nevertheless, increases in BAL CD4 T-cell frequency in combination with proliferating Ki67+ memory CD4 T cells strongly suggests a component of local pulmonary T-cell reconstitution. However, it is possible that these cells actually were proliferating in lymph nodes and then homed to BAL, leading to reconstitution.
The presence of T cells capable of simultaneously producing several effector cytokines has been associated with better protection against HIV (2, 4) and leishmania (7). The increased functionality of memory T cells we observe within the BAL compared to that of PB may help explain the lack of pulmonary opportunistic infections within HIV-infected individuals during the long, asymptomatic chronic phase of infection. Interestingly, CMV-specific (in contrast to mitogenically stimulated and HIV-specific) CD8 and CD4 memory T cells are more polyfunctional in blood than lung, suggesting a hierarchy of antigenic responses in various compartments. Moreover, the decreased T-cell polyfunctionality observed within PB of HIV-infected individuals is maintained even after 1 year of HAART. Further studies are required to examine the impact of the early initiation of HAART on local immune reconstitution to pulmonary pathogens.
There are several confounding issues that require further study and analysis. First, half of our volunteers were smokers at the time of enrollment, which may decrease the breadth of local T-cell responses. Second, Ki67+ memory CD4 T cells frequently are increased at 1 month. It is unclear if this proliferation represents pathological proliferative responses to antigens present in the HIV-infected lung in some subjects. Third, although all subjects were on HAART, occasional increases in viral load were noted in blood throughout the 1-year course of follow-up. The impact of low-level intermittent viremia cannot be completely assessed. Finally, given the small numbers of T cells in some samples, not all analyses could be performed on all subjects at every time point. Increased numbers of samples and longitudinal analysis beyond 1 year may be useful in this regard.
In summary, while causal relationships between viral replication, T-cell functionality, CD4 T-cell reconstitution, and local immunological phenomena often are difficult to delineate, our findings show an anatomically distinct mucosal site that contains ample cellular targets for HIV infection that nevertheless remains relatively intact, is capable of compartmentalized reconstitution after HAART, and maintains polyfunctional T cells. These findings provide a mechanism underlying the differential depletion and subsequent reconstitution after HAART of mucosal CD4 T cells.
Acknowledgments
We thank Ian Robey, Suzette Chavez, Ben Turney, Tim Stump, and Patricia Smith for technical support and subject recruitment.
This project was supported by the Indiana Clinical and Translational Sciences Institute, funded in part by grant RR025761 from the National Institutes of Health, Clinical and Translational Sciences Award. K.S.K. is supported by NIH grant R01 HL083468. H.L.T. is supported by NIH grant U01 HL098960. This work was supported in part by intramural funding from NIAID, NIH.
Footnotes
Published ahead of print on 7 July 2010.
REFERENCES
- 1.Agostini, C., V. Poletti, R. Zambello, L. Trentin, F. Siviero, L. Spiga, F. Gritti, and G. Semenzato. 1988. Phenotypical and functional analysis of bronchoalveolar lavage lymphocytes in patients with HIV infection. Am. Rev. Respir. Dis. 138:1609-1615. [DOI] [PubMed] [Google Scholar]
- 2.Betts, M. R., M. C. Nason, S. M. West, S. C. De Rosa, S. A. Migueles, J. Abraham, M. M. Lederman, J. M. Benito, P. A. Goepfert, M. Connors, M. Roederer, and R. A. Koup. 2006. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood 107:4781-4789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brenchley, J. M., B. J. Hill, D. R. Ambrozak, D. A. Price, F. J. Guenaga, J. P. Casazza, J. Kuruppu, J. Yazdani, S. A. Migueles, M. Connors, M. Roederer, D. C. Douek, and R. A. Koup. 2004. T-cell subsets that harbor human immunodeficiency virus (HIV) in vivo: implications for HIV pathogenesis. J. Virol. 78:1160-1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brenchley, J. M., K. K. Knox, A. I. Asher, D. A. Price, L. M. Kholi, E. Gostick, B. J. Hill, C. A. Hage, Z. Brahmi, A. Khoruts, H. L. Twigg, T. W. Schacker, and D. C. Douek. 2008. High frequencies of polyfunctional HIV-specific T cells are associated with preservation of mucosal CD4 T cells in bronchoalveolar lavage. Mucosal Immunol. 1:49-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brenchley, J. M., T. W. Schacker, L. E. Ruff, D. A. Price, J. H. Taylor, G. J. Beilman, P. L. Nguyen, A. Khoruts, M. Larson, A. T. Haase, and D. C. Douek. 2004. CD4+ T-cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract. J. Exp. Med. 200:749-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casazza, J. P., M. R. Betts, L. J. Picker, and R. A. Koup. 2001. Decay kinetics of human immunodeficiency virus-specific CD8+ T cells in peripheral blood after initiation of highly active antiretroviral therapy. J. Virol. 75:6508-6516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Darrah, P. A., D. T. Patel, P. M. De Luca, R. W. Lindsay, D. F. Davey, B. J. Flynn, S. T. Hoff, P. Andersen, S. G. Reed, S. L. Morris, M. Roederer, and R. A. Seder. 2007. Multifunctional TH1 cells define a correlate of vaccine-mediated protection against Leishmania major. Nat. Med. 13:843-850. [DOI] [PubMed] [Google Scholar]
- 8.Douek, D. C., M. R. Betts, J. M. Brenchley, B. J. Hill, D. R. Ambrozak, K. L. Ngai, N. J. Karandikar, J. P. Casazza, and R. A. Koup. 2002. A novel approach to the analysis of specificity, clonality, and frequency of HIV-specific T-cell responses reveals a potential mechanism for control of viral escape. J. Immunol. 168:3099-3104. [DOI] [PubMed] [Google Scholar]
- 9.Douek, D. C., J. M. Brenchley, M. R. Betts, D. R. Ambrozak, B. J. Hill, Y. Okamoto, J. P. Casazza, J. Kuruppu, K. Kunstman, S. Wolinsky, Z. Grossman, M. Dybul, A. Oxenius, D. A. Price, M. Connors, and R. A. Koup. 2002. HIV preferentially infects HIV-specific CD4+ T-cells. Nature 417:95-98. [DOI] [PubMed] [Google Scholar]
- 10.Estes, J., J. V. Baker, J. M. Brenchley, A. Khoruts, J. L. Barthold, A. Bantle, C. S. Reilly, G. J. Beilman, M. E. George, D. C. Douek, A. T. Haase, and T. W. Schacker. 2008. Collagen deposition limits immune reconstitution in the gut. J. Infect. Dis. 198:456-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Estes, J. D., J. M. Brenchley, J. Bathold, A. Khoruts, G. Beilman, J. V. Baker, C. Reilly, D. C. Douek, A. T. Haase, and T. Schacker. 2007. CD4 reconstitution of lymphoid tissues is dependent on earlier initiation of HAART, abstr. 67. Abstr. 14th Conf. Retrovir. Opportun. Infect.
- 12.Guadalupe, M., E. Reay, S. Sankaran, T. Prindiville, J. Flamm, A. McNeil, and S. Dandekar. 2003. Severe CD4+ T-cell depletion in gut lymphoid tissue during primary human immunodeficiency virus type 1 infection and substantial delay in restoration following highly active antiretroviral therapy. J. Virol. 77:11708-11717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guadalupe, M., S. Sankaran, M. D. George, E. Reay, D. Verhoeven, B. L. Shacklett, J. Flamm, J. Wegelin, T. Prindiville, and S. Dandekar. 2006. Viral suppression and immune restoration in the gastrointestinal mucosa of human immunodeficiency virus type 1-infected patients initiating therapy during primary or chronic infection. J. Virol. 80:8236-8247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kalsdorf, B., T. J. Scriba, K. Wood, C. L. Day, K. Dheda, R. Dawson, W. A. Hanekom, C. Lange, and R. J. Wilkinson. 2009. HIV-1 infection impairs the bronchoalveolar T-cell response to mycobacteria. Am. J. Respir. Crit. Care Med. 180:1262-1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kitahata, M. M., S. J. Gange, A. G. Abraham, B. Merriman, M. S. Saag, A. C. Justice, R. S. Hogg, S. G. Deeks, J. J. Eron, J. T. Brooks, S. B. Rourke, M. J. Gill, R. J. Bosch, J. N. Martin, M. B. Klein, L. P. Jacobson, B. Rodriguez, T. R. Sterling, G. D. Kirk, S. Napravnik, A. R. Rachlis, L. M. Calzavara, M. A. Horberg, M. J. Silverberg, K. A. Gebo, J. J. Goedert, C. A. Benson, A. C. Collier, S. E. Van Rompaey, H. M. Crane, R. G. McKaig, B. Lau, A. M. Freeman, and R. D. Moore. 2009. Effect of early versus deferred antiretroviral therapy for HIV on survival. N. Engl. J. Med. 360:1815-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuller, L. H., R. Tracy, W. Belloso, S. De Wit, F. Drummond, H. C. Lane, B. Ledergerber, J. Lundgren, J. Neuhaus, D. Nixon, N. I. Paton, and J. D. Neaton. 2008. Inflammatory and coagulation biomarkers and mortality in patients with HIV infection. PLoS Med. 5:e203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li, Q., L. Duan, J. D. Estes, Z. M. Ma, T. Rourke, Y. Wang, C. Reilly, J. Carlis, C. J. Miller, and A. T. Haase. 2005. Peak SIV replication in resting memory CD4+ T cells depletes gut lamina propria CD4+ T cells. Nature 434:1148-1152. [DOI] [PubMed] [Google Scholar]
- 18.Macal, M., S. Sankaran, T. W. Chun, E. Reay, J. Flamm, T. J. Prindiville, and S. Dandekar. 2008. Effective CD4+ T-cell restoration in gut-associated lymphoid tissue of HIV-infected patients is associated with enhanced Th17 cells and polyfunctional HIV-specific T-cell responses. Mucosal Immunol. 1:475-488. [DOI] [PubMed] [Google Scholar]
- 19.Mattapallil, J. J., D. C. Douek, B. Hill, Y. Nishimura, M. Martin, and M. Roederer. 2005. Massive infection and loss of memory CD4+ T cells in multiple tissues during acute SIV infection. Nature 434:1093-1097. [DOI] [PubMed] [Google Scholar]
- 20.Mehandru, S., M. A. Poles, K. Tenner-Racz, A. Horowitz, A. Hurley, C. Hogan, D. Boden, P. Racz, and M. Markowitz. 2004. Primary HIV-1 infection is associated with preferential depletion of CD4+ T lymphocytes from effector sites in the gastrointestinal tract. J. Exp. Med. 200:761-770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mehandru, S., M. A. Poles, K. Tenner-Racz, P. Jean-Pierre, V. Manuelli, P. Lopez, A. Shet, A. Low, H. Mohri, D. Boden, P. Racz, and M. Markowitz. 2006. Lack of mucosal immune reconstitution during prolonged treatment of acute and early HIV-1 infection. PLoS Med. 3:e484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mehandru, S., M. A. Poles, K. Tenner-Racz, V. Manuelli, P. Jean-Pierre, P. Lopez, A. Shet, A. Low, H. Mohri, D. Boden, P. Racz, and M. Markowitz. 2007. Mechanisms of gastrointestinal CD4+ T-cell depletion during acute and early human immunodeficiency virus type 1 infection. J. Virol. 81:599-612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Okoye, A., M. Meier-Schellersheim, J. M. Brenchley, S. I. Hagen, J. M. Walker, M. Rohankhedkar, R. Lum, J. B. Edgar, S. L. Planer, A. Legasse, A. W. Sylwester, M. Piatak, Jr., J. D. Lifson, V. C. Maino, D. L. Sodora, D. C. Douek, M. K. Axthelm, Z. Grossman, and L. J. Picker. 2007. Progressive CD4+ central memory T-cell decline results in CD4+ effector memory insufficiency and overt disease in chronic SIV infection. J. Exp. Med. 204:2171-2185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Picker, L. J., S. I. Hagen, R. Lum, E. F. Reed-Inderbitzin, L. M. Daly, A. W. Sylwester, J. M. Walker, D. C. Siess, M. Piatak, Jr., C. Wang, D. B. Allison, V. C. Maino, J. D. Lifson, T. Kodama, and M. K. Axthelm. 2004. Insufficient production and tissue delivery of CD4+ memory T cells in rapidly progressive simian immunodeficiency virus infection. J. Exp. Med. 200:1299-1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pitcher, C. J., C. Quittner, D. M. Peterson, M. Connors, R. A. Koup, V. C. Maino, and L. J. Picker. 1999. HIV-1-specific CD4+ T cells are detectable in most individuals with active HIV-1 infection, but decline with prolonged viral suppression. Nat. Med. 5:518-525. [DOI] [PubMed] [Google Scholar]
- 26.Schacker, T. W., J. M. Brenchley, G. J. Beilman, C. Reilly, S. E. Pambuccian, J. Taylor, D. Skarda, M. Larson, D. C. Douek, and A. T. Haase. 2006. Lymphatic tissue fibrosis is associated with reduced numbers of naive CD4+ T cells in human immunodeficiency virus type 1 infection. Clin. Vaccine Immunol. 13:556-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schacker, T. W., P. L. Nguyen, G. J. Beilman, S. Wolinsky, M. Larson, C. Reilly, and A. T. Haase. 2002. Collagen deposition in HIV-1 infected lymphatic tissues and T-cell homeostasis. J. Clin. Investig. 110:1133-1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Twigg, H. L., D. M. Soliman, R. B. Day, K. S. Knox, R. J. Anderson, D. S. Wilkes, and C. T. Schnizlein-Bick. 1999. Lymphocytic alveolitis, bronchoalveolar lavage viral load, and outcome in human immunodeficiency virus infection. Am. J. Respir. Crit. Care Med. 159:1439-1444. [DOI] [PubMed] [Google Scholar]
- 29.Twigg, H. L., III, M. Weiden, F. Valentine, C. T. Schnizlein-Bick, R. Bassett, L. Zheng, J. Wheat, R. B. Day, H. Rominger, R. G. Collman, L. Fox, B. Brizz, J. Dragavon, R. W. Coombs, and R. P. Bucy. 2008. Effect of highly active antiretroviral therapy on viral burden in the lungs of HIV-infected subjects. J. Infect. Dis. 197:109-116. [DOI] [PubMed] [Google Scholar]
- 30.Veazey, R. S., M. DeMaria, L. V. Chalifoux, D. E. Shvetz, D. R. Pauley, H. L. Knight, M. Rosenzweig, R. P. Johnson, R. C. Desrosiers, and A. A. Lackner. 1998. Gastrointestinal tract as a major site of CD4+ T-cell depletion and viral replication in SIV infection. Science 280:427-431. [DOI] [PubMed] [Google Scholar]
- 31.Veazey, R. S., P. A. Marx, and A. A. Lackner. 2003. Vaginal CD4+ T cells express high levels of CCR5 and are rapidly depleted in simian immunodeficiency virus infection. J. Infect. Dis. 187:769-776. [DOI] [PubMed] [Google Scholar]