Abstract
Hepatitis C virus (HCV) infection causes significant morbidity, and efficient mouse models would greatly facilitate virus studies and the development of effective vaccines and new therapeutic agents. Entry factors, innate immunity, and host factors needed for viral replication represent the initial barriers that restrict HCV infection of mouse cells. Experiments in this paper consider early postentry steps of viral infection and investigate the roles of interferon regulatory factors (IRF-3 and IRF-9) and microRNA (miR-122) in promoting HCV replication in mouse embryo fibroblasts (MEFs) that contain viral subgenomic replicons. While wild-type murine fibroblasts are restricted for HCV RNA replication, deletion of IRF-3 alone can facilitate replicon activity in these cells. This effect is thought to be related to the inactivation of the type I interferon synthesis mediated by IRF-3. Additional deletion of IRF-9 to yield IRF-3−/− IRF-9−/− MEFs, which have blocked type I interferon signaling, did not increase HCV replication. Expression of liver-specific miR-122 in MEFs further stimulated the synthesis of HCV replicons in the rodent fibroblasts. The combined effects of miR-122 expression and deletion of IRF-3 produced a cooperative stimulation of HCV subgenome replication. miR-122 and IRF-3 are independent host factors that are capable of influencing HCV replication, and our findings could help to establish mouse models and other cell systems that support HCV growth and particle formation.
Hepatitis C virus (HCV) is a blood-borne pathogen that represents a serious public health burden and infects an estimated 170 million people, or 3% of the global population (43). This virus establishes chronic infections in about 80% of infected individuals, which may lead to severe liver complications, including cirrhosis and hepatocellular carcinoma (13). Current treatment options are suboptimal, and there are no effective vaccines on the horizon. The differences in host response between patients who spontaneously clear the virus and those whose disease worsens are also not well defined. The only other natural host for HCV, besides humans, is the chimpanzee. A human liver xenograft model in severely immunocompromised (SCID) mice has been developed (54). However, there is still an urgent need for development of an efficient immunocompetent mouse model to facilitate drug and vaccine discovery and to better understand the virus-host interactions (10).
The 9.6-kb HCV genome contains a single continuous open reading frame (ORF) flanked by a 5′ internal ribosomal entry site (IRES) and a 3′-untranslated region (3′ UTR). Translation of the viral genome yields a single polyprotein from the ORF, which is processed by host and viral proteases to yield 3 structural proteins (C, E1, and E2), 1 ion channel protein (p7), and 6 nonstructural proteins (NS2, NS3, NS4A, NS4B, NS5A, and NS5B) during the viral life cycle (55). Numerous studies modeling the HCV life cycle in vitro support the notion that viral replication is dependent upon specific cellular factors. The importance of the host is enunciated by the species and cell type restriction of HCV replication in culture and the limitation of virion production to the human hepatoma Huh-7 cell line (62), which supports the complete viral life cycle (7). Genetic defects in the innate immune system have subsequently been identified as the factors affecting the efficiency of HCV replication in this cell line and its derivatives (44). More specifically, during host cell innate immunity, pattern recognition receptors (PRRs) such as Toll-like receptor 3 (TLR3) and retinoic acid-inducible gene I (RIG-I) recognize viral RNA signatures and trigger the downstream interferon regulatory factor 3 (IRF-3) transcription activator to induce beta interferon (IFN-β) synthesis, which finally activates IFN-stimulated genes (ISGs) of the antiviral defense program (40). Huh-7 and Huh-7.5 cells, which support the replication and assembly of HCV, have been shown to be deficient in TLR3 and in TLR3 and RIG-I, respectively (9, 46, 70, 75, 81). IRF-3-deficient mice also have a poor IFN response and are more susceptible to virus infections in general (66).
The singular replication of HCV RNA in Huh-7 cells can also be attributed to another host factor, the liver-specific microRNA 122 (miR-122). MicroRNAs (miRNAs) are short (∼22 nucleotides), noncoding, evolutionarily conserved endogenous RNA species that normally regulate gene expression via mRNA cleavage or translational repression through binding to the 3′ UTR of the target mRNA (6). The miRNAs are generated by two rounds of ordered cleavages, with primary transcripts termed primary miRNAs (pri-miRNAs) being processed first to yield short stem-loop structures known as precursor miRNAs (pre-miRNAs), which are finally cropped to produce functional mature miRNAs (6). Mature miRNAs then associate with other proteins to form RNA-induced silencing complexes (RISC), and through pairing with partially complementary sites in the 3′ UTRs of mRNAs, they initiate the repression of their target mRNAs. Recent reviews have revealed that miRNAs participate in various cellular biological processes, including growth development, metabolism, cell proliferation, hematopoiesis, and apoptosis, and are functionally associated with a number of human diseases and cancers (3, 6, 67). While the effects of miRNAs are generally inhibitory, one particular miRNA, the liver-specific miR-122 (20), seems to positively promote HCV replication in the host cell and has been suggested to contribute to the liver tropism of this virus (32, 37). Further evidence supporting this notion came with the observation that miR-122 can enhance HCV replication in nonhepatic human cells, suggesting that the presence of miR-122 indeed plays an important role in sustaining the HCV life cycle in hepatic cells (19).
While many of the host-specific factors for HCV replication have been identified in the human liver, host components for viral replication in rodents are largely unexplored. In an attempt to facilitate HCV infection in small-animal models, examinations of specific intracellular determinants that support HCV infections have been initiated in several different mouse systems, including fibroblasts and hepatocytes, yielding greatly reduced replication compared to that in human hepatoma Huh-7 cells (21, 50, 52, 73, 80, 82). Although the double-stranded-RNA-binding protein kinase R (PKR) has been suggested as a potential innate immune factor regulating HCV replication in murine embryonic cells (21), the influence of other components of innate immunity remain to be tested. In order to clarify the host factors required to support HCV replication in rodent cells, we focused on the roles of innate immune transcription factors, including IRF-3 and IRF-9, and the liver-specific miR-122 in influencing subgenomic viral RNA synthesis within murine fibroblasts. We provide evidence that both IRF-3 deletion and miR-122 expression, independently or in combination, can promote increased HCV RNA and viral protein production in mouse fibroblasts. Both transient luciferase reporter and drug-resistant subgenomic replicon assays corroborated these results. These observations should provide insight into some of the postentry factors that will have to be considered in generating a mouse model for HCV replication.
MATERIALS AND METHODS
Cell culture and reagents.
Human hepatoma Huh-7 cells were kindly provided by Stanley M. Lemon (University of Texas Medical Branch, Galveston, TX) and were maintained in Dulbecco's modified Eagle's medium (Wisent, St.-Bruno, Quebec, Canada) supplemented with 10% fetal bovine serum (FBS; Wisent), 50 μg/ml gentamicin (Gibco-Invitrogen, Carlsbad, CA), and 0.5 μg/ml amphotericin B (Gibco-Invitrogen). C57BL/6 mouse embryonic fibroblasts (MEFs) from wild-type (WT), IRF-3−/− (IRF-3-deficient), and IRF-3−/− IRF-9−/− (IRF-3- and IRF-9-deficient) mice (66) (originally obtained from Tadatsugu Taniguchi, University of Tokyo, Tokyo, Japan) were grown in alpha minimal essential medium (Wisent) supplemented with 10% FBS, 50 μg/ml gentamicin, and 0.5 μg/ml amphotericin B. Cell lines carrying HCV replicons were maintained in the presence of blasticidin (Invivogen, San Diego, CA). MEFs were checked for deletion of IRF-3 and IRF-9 by standard reverse transcription-PCR (RT-PCR). Mouse liver cell homogenate was kindly provided by Brent Johnston (Dalhousie University, Halifax, Canada). miR-122 (miRIDIAN mimic hsa-mir-122; C-300591-05) and negative-control miRNA (miRIDIAN mimic negative control; CN-001000-01) were purchased from Dharmacon (Lafayette, CO).
Plasmids and replicons.
The plasmid pSGR-Luc-JFH1 and its NS5B polymerase-inactive control, pSGR-Luc-JFH1/GND (72), were a generous gift from John McLaughlin (MRC Virology Unit, Institute of Virology, Glasgow, United Kingdom). To construct pSGR-Bsd-JFH1 and pSGR-Bsd-JFH1/GND, the plasmids pSGR-Luc-JFH1 and pSGR-Luc-JFH1/GND were digested with BglII and PmeI to remove the firefly luciferase gene, and then the blasticidin S deaminase (Bsd) gene, amplified from pcDNA6/V5-HisA (Invitrogen), was inserted by use of BglII and PmeI sites at the 5′ and 3′ termini. The constructs were verified by sequencing.
In vitro transcription and RNA preparation.
HCV replicon RNA was transcribed in vitro by use of a MEGAscript T7 in vitro transcription kit (Ambion, Austin, TX) according to the manufacturer's instructions. For pSGR-JFH1 derivatives, plasmid DNA was digested with XbaI, followed by a single treatment with 1 unit/μg mung bean DNA nuclease (New England Biolabs, Pickering, Ontario, Canada) as previously described (38). After RNA synthesis, the DNA template was removed by three repeated digests with 0.2 unit/μl DNase I (Ambion), followed by standard phenol and chloroform purification. All RNA samples from cells were isolated using TRIzol reagent (Invitrogen), treated with DNase I (Qiagen Inc., Mississauga, Ontario, Canada) for the removal of genomic DNA, and purified by phenol-chloroform extraction according to the manufacturers' protocols.
RNA electroporation.
Cells were trypsinized, washed three times with cold phosphate-buffered saline (PBS) (Wisent), and resuspended at a concentration of 1 × 107 cells/ml in PBS. A total of 10 μg in vitro-transcribed RNA was mixed with 400 μl of 1 × 107 cells/ml in cell suspension in a 0.4-cm-gap cuvette (Bio-Rad, Hercules, CA), alone or in the presence of 50 nM miRNA (miR-122 or negative control), and immediately pulsed with a Gene Pulser Xcell instrument (Bio-Rad). The electroporation conditions used for Huh-7 cells were 270 V and 960 μF, and those for MEFs were 400 V and 250 μF.
Transient replication assay using luciferase.
The transient replication assay was based on previously described methods (41, 72). Briefly, cells were transfected by electroporation as described above, using 10 μg of luciferase replicon RNA in the presence or absence of 50 nM miRNA (miR-122 or negative control). Following dilution of the cells with 8 ml of medium, 6-well plates were seeded with 0.5-ml aliquots of the electroporated cells. At 4 h and each subsequent day postelectroporation, for up to 7 days, the cells were harvested and then assayed for luciferase activity by using a luciferase assay system (Promega, Madison, WI) and a luminometer (Promega). The luciferase levels at 4 h postelectroporation were used to correct for transfection efficiency. Values are expressed as fold changes in relative light units (RLU) with respect to the 4-h input (47). All experiments were performed independently three times, and data were plotted as means ± standard errors of the means (SEM). Remaining cells from the electroporation mixtures were also seeded into a separate dish for harvest of RNA 3 days after electroporation for detection of miRNA (see below).
Colony formation assay by drug selection.
Cells were electroporated with HCV RNA as indicated above. Electroporated cells were diluted with 10 ml of fresh medium and seeded into tissue culture dishes at various dilutions, depending on the experiment. After 24 to 48 h of recovery, and every 3 to 4 days subsequently, the culture medium was replaced with fresh medium supplemented with 5 to 10 μg/ml blasticidin until colonies were visible (about 2 to 3 weeks, depending on the cell type). Colonies were then characterized for HCV protein and genomic integration or fixed and stained with 0.1% crystal violet (Sigma) for visualization. Colonies were also counted and expressed as CFU/μg of input HCV RNA, with values presented as means ± SEM in Table 1.
TABLE 1.
Colony-forming efficiencies induced by HCV SGR-Bsd-JFH1 RNA
| Cell line | Colony-forming efficiency (CFU/μg RNA)a |
|---|---|
| Huh-7 | 6.02 × 103 ± 0.32 × 103 |
| WT MEF | 4.20 × 101 ± 1.45 × 101 |
| IRF-3 KO MEF | 3.91 × 102 ± 0.21 × 102 |
| WT MEF + miR-122 | 1.72 × 103 ± 0.34 × 103 |
| IRF-3 KO MEF + miR-122 | 4.43 × 103 ± 0.58 × 103 |
| IRF3KO-HmiR122 MEF | 4.05 × 103 ± 0.51 × 103 |
Values given are means ± SEM for three independent experiments.
Detection of HCV protein by immunohistochemical staining.
Detection of HCV protein by immunohistochemical staining was performed as previously described (46), with some modifications. Briefly, naïve cells or HCV RNA-induced colonies were fixed and permeabilized by methanol, treated with 3% H2O2 for 30 min to inactivate endogenous enzyme activity, and then blocked for 1 h with 3% bovine serum albumin (BSA). Immunostaining for NS5A was performed using the mouse monoclonal anti-NS5A 9E10 antibody (generously provided by Charles M. Rice, Center for the Study of Hepatitis C, The Rockefeller University, New York, NY) and goat anti-mouse-alkaline phosphatase conjugate (Sigma), followed by development with 1-Step nitroblue tetrazolium chloride-5-bromo-4-chloro-3-indolyphosphate p-toluidine salt (NBT/BCIP) solution (Thermo Fisher Scientific/Pierce, Rockford, IL). Nuclei were then counterstained with hematoxylin for photography. A mouse IgG2 isotype control antibody (eBioscience, San Diego, CA) was also included in the experiments.
Innate immunity gene analysis by RT-PCR and VSV infection assay for antiviral response.
WT and IRF-3-deficient MEFs were electroporated as indicated above, using either 10 μg of luciferase replicon RNA (GND) or 10 μg of poly(I:C) (Sigma), or were mock electroporated, followed by seeding into 6-cm dishes for RNA extraction or into 12-well plates for vesicular stomatitis virus (VSV) infection.
For innate immunity gene analysis by RT-PCR, total cellular RNA was extracted from the samples, after a recovery incubation of 6 h, as described above. The purified RNA (2 μg) was then subjected to cDNA conversion by use of a first-strand cDNA synthesis kit (GE Healthcare/Amersham Biosciences, Piscataway, NJ) according to the manufacturer's protocol. Murine innate immunity genes were then PCR amplified with 10% of the resulting cDNA, using the following primers: mISG15 (432 bp) (58); mISG54 forward primer, 5′-GGAGAGCAATCTGCGACAGC-3′; mISG54 reverse primer, 5′-GCTGCCCTGAGGAGTGTATC-3′ (720 bp); mISG56 forward primer, 5′-GAGCCAGAAAACCCTGAGTA-3′; mISG56 reverse primer, 5′-CCTCAGTTGGGAGATTTGTTGC-3′ (381 bp); mIFN-β forward primer, 5′-GCGTTCCTGCTGTGCTTC-3′; mIFN-β reverse primer, 5′-CCATCCAGGCGTAGCTG-3′ (454 bp); murine IFN-inducible protein 10 (mIP-10) forward primer, 5′-ATGAACCCAAGTGCTGCCGT; mIP-10 reverse primer, 5′-CTGGGTAAAGGGGAGTGATG (379 bp); murine glyceraldehyde-3-phosphate dehydrogenase (mGAPDH) forward primer, 5′-GTGAAGGTCGGTGTGAACGG-3′; and mGAPDH reverse primer, 5′-GTGGCAGTGATGGCATGGAC-3′ (542 bp). All PCRs were carried out with standard PCR techniques.
For VSV infection assay, the electroporated cells were allowed to recover for 24 h prior to infection with a green fluorescent protein (GFP)-tagged VSV (VSV-GFP, Indiana serotype; a gift from Brian Lichty, McMaster University, Hamilton, Ontario, Canada) (69). As a control, mock-electroporated cells were also treated with 100 U/ml murine IFN-β (Sigma) for 24 h. Following recovery, the cell monolayers were infected at a multiplicity of infection (MOI) of 0.01 for 1 h before overlay with medium containing 2% fetal calf serum (FCS) and 2% methylcellulose. Pictures were taken between 24 and 48 h postinfection, at a magnification of ×100 (Leica Microsystems, Wetzlar, Germany).
Establishment of murine cells stably expressing miR-122.
IRF-3-deficient MEFs were transduced by use of a lentivirus expression system (Thermo Fisher Scientific, Waltham, MA) with a vector (pLemiR) expressing human primary miR-122 (pri-miR-122) transcripts under the control of the cytomegalovirus (CMV) promoter (Open Biosystems, Huntsville, AL). Expression of the pri-miRNA transcripts allowed interaction with the endogenous microRNA processing/regulatory pathways, which would first yield pre-miRNAs and, subsequently, mature miRNAs. The pre-miRNA was coexpressed with TurboRed fluorescent protein (TurboRFP) and a puromycin resistance selectable marker which allows monitoring of miRNA-expressing cells and generation of stable cell lines. The pLemiR pri-miR-122 vector was transfected into 293T cells by use of a Trans-Lentiviral GIPZ packaging system (Open Biosystems) to produce a VSV glycoprotein (VSV-G)-pseudotyped virus according to the manufacturer's protocol. Puromycin selection and TurboRFP marker expression were used to exclude any nontransduced cells, and the successfully established cell lines that stably expressed miR-122 were termed “IRF-3-deficient (KO)-HmiR122 MEFs.”
TaqMan probe real-time qPCR detection of miR-122.
To detect the presence of miRNA, total cellular RNA was extracted from the different cells as well as from samples in the transient replication assays, as described above. The purified RNA (10 ng) was then subjected to cDNA conversion by use of a TaqMan microRNA reverse transcription kit (ABI, Foster City, CA) according to the manufacturer's protocol. The cDNA product was then assessed by real-time quantitative PCR (qPCR), using TaqMan microRNA assays with primers and probes specific only for the mature sequences of miR-122 and the control miRNA miR-16 (ABI). Samples were run on an ABI 7900HT sequence detection system, and results were analyzed using SDS software (ABI). All assays were done in triplicate. Data from three independent experiments were normalized against the control miRNA miR-16 and then plotted with respect to the control group as means ± SEM in bar graphs.
RESULTS
Deletion of IRF-3 supports transient and drug-selected replication of subgenomic HCV JFH1 RNA.
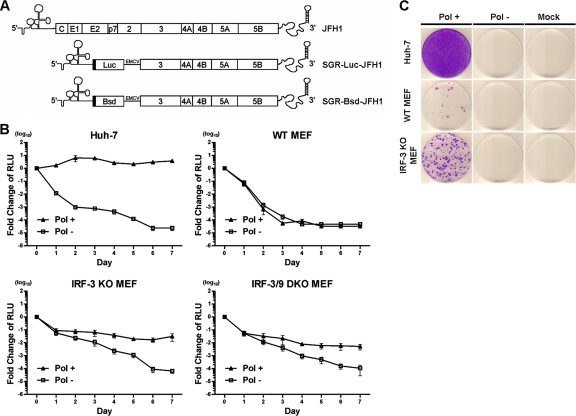
The HCV JFH1 replicon is a robust RNA that requires minimal adaptation to replicate in either liver or nonhepatic cells (38, 39, 46) and has previously been shown to multiply in some mouse cells (21, 73). We used two subgenomic constructs based on this backbone to assess HCV replication, with one engineered with the firefly luciferase reporter gene (SGR-Luc-JFH1) for transient replication assays and the other engineered with the blasticidin S deaminase gene (SGR-Bsd-JFH1), which confers resistance to blasticidin (Fig. 1 A), for drug selection and cell colony formation assays. As expected, the HCV subgenomic RNA replicated robustly in Huh-7 cells (Fig. 1B and C), with a colony formation efficiency of 6.02 × 103 ± 0.32 × 103 CFU/μg RNA (Table 1). In contrast, WT MEFs were nonpermissive for transient HCV replication, with no difference in luciferase reporter activity from either the replication-competent or mutated control replicon (Fig. 1B). Similarly, subgenomic replicons expressing the Bsd resistance gene produced limited colony formation in WT MEFs grown in the presence of blasticidin (Fig. 1C and Table 1). Importantly, IRF-3-deficient MEFs were more supportive of HCV RNA replication in transient replicon luciferase reporter assays conducted at 7 days postelectroporation (Fig. 1B). In addition, HCV replicons in IRF-3 null cells had a significantly higher replication activity (9-fold) in colony formation assays than those in WT MEFs (Fig. 1C and Table 1). These observations indicated that deletion of the innate immune factor IRF-3 in mouse fibroblasts can favor HCV RNA replication.
FIG. 1.
IRF-3 deficiency facilitates replication of HCV replicon RNA in mouse fibroblasts. (A) Schematic representation (not to scale) of HCV JFH1 RNA genome, subgenomic luciferase reporter JFH1 construct (SGR-Luc-JFH1), and subgenomic blasticidin resistance-conferring JFH1 construct (SGR-Bsd-JFH1). EMCV, EMCV IRES; Luc, firefly luciferase gene; Bsd, blasticidin S deaminase gene conferring resistance to blasticidin. (B) Transient replication assays using the HCV SGR-Luc-JFH1 RNA in Huh-7 cells and in WT, IRF-3-deficient (KO), and IRF-3/9-deficient (DKO) MEFs. Cells were electroporated with the HCV RNA, harvested at the indicated time points, and assayed for luciferase activity. The luciferase reporter activity is indicative of HCV RNA replication. Bioluminescence is expressed on a logarithmic scale as the fold change in RLU normalized to the light emitted from input RNA at 4 h postelectroporation. Each point represents the mean value for three independent experiments, with error bars showing the SEM. Pol + (solid triangles), polymerase-active HCV RNA; Pol − (open squares), polymerase-defective (nonreplicating; GND) control. (C) Colony formation assay using HCV SGR-Bsd-JFH1 RNA in Huh-7 cells and WT and IRF-3-deficient (KO) MEFs. Cells were electroporated with the HCV RNA, seeded onto culture plates at a 1:2 dilution, and then selected with blasticidin for 2 to 3 weeks before being stained with crystal violet. Representative images from three independent experiments are shown. Pol +, polymerase-active HCV RNA; Pol −, polymerase-defective (nonreplicating; GND) control; mock, mock electroporation with buffer.
Following binding of IFN to its cell surface receptor, phosphorylated signal transducer and activator of transcription (STAT) proteins interact with IRF-9 to promote the expression of ISGs. These include IRF-7, which activates the synthesis of more type I IFN (33). To determine whether deletion of IRF-9 in the IFN signaling pathway could further contribute to HCV replication, we assayed replicon activity in murine fibroblasts doubly deficient for IRF-3 and IRF-9 (IRF-3−/− IRF-9−/− MEFs). Type I IFN production in these cells is greatly diminished, and they are highly susceptible to viral infections (66). Surprisingly, IRF-3−/− IRF-9−/− MEFs exhibited no further increase in HCV replication compared to that in IRF-3−/− cells (Fig. 1B). Thus, it appears in considering the type I IFN signaling pathway that IRF-3 deficiency alone is sufficient to promote HCV RNA replication in mouse fibroblasts. Interestingly, in both IRF-3−/− and IRF-3−/− IRF-9−/− cells, the NS5B polymerase-defective mutant usually took longer (6 to 7 days) to produce baseline luciferase values than the same replicon in WT MEFs (4 to 5 days), an observation likely due to diminished antiviral RNase L activity present in the defective type I IFN system.
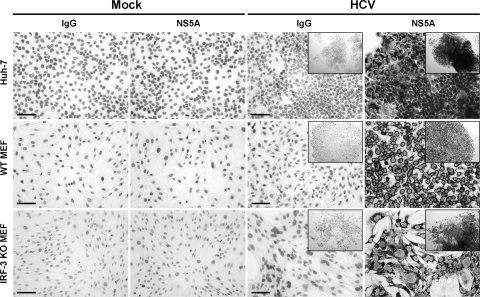
To further validate HCV replication in the cells used in the above experiments, colonies obtained in the dishes were assessed for HCV NS5A expression by immunohistochemical staining (Fig. 2). NS5A protein could be detected in the cytoplasmic and perinuclear regions of replicon cells. Mouse fibroblasts containing the HCV replicons were also stained with an IgG control antibody or compared with control cells that did not contain HCV RNA. To rule out genomic integration of cDNA from the template for the HCV replicon, PCR analysis was performed to amplify the Bsd gene and the HCV 5′ UTR, using genomic DNA from the pooled MEF colonies. None of the cells containing HCV RNA or proteins yielded PCR signals that could be attributed to genomic integration of the blasticidin resistance gene or viral cDNA, indicating that the MEFs were authentic replicon cell lines (data not shown). The immunochemical staining and PCR results provided a correlation between the colony formation assays and transient luciferase reporter assays. The preceding results further demonstrated that HCV RNA could replicate in rodent cells and that the replication efficiency was enhanced by deletion of the gene for IRF-3.
FIG. 2.
Detection of NS5A protein in HCV replicon colony formation assays. Colonies obtained by blasticidin drug selection of HCV SGR-Bsd-JFH1 RNA in Huh-7 cells and WT and IRF-3-deficient (KO) MEFs were fixed and immunostained for NS5A with anti-NS5A or IgG control primary antibody. Antibody binding was determined with a goat anti-mouse secondary antibody conjugated to alkaline phosphatase. Binding of the secondary antibody was revealed by incubating the cells with NBT/BCIP substrate, which formed a brown precipitate. Nuclei were counterstained with hematoxylin. Naïve cells (mock) of each cell type were stained as a control. Magnification, ×200 or ×50 (insets showing colonies). Bars, 100 μm. Representative images from two independent experiments are shown.
HCV RNA cannot induce an antiviral state in IRF-3-deficient MEFs.
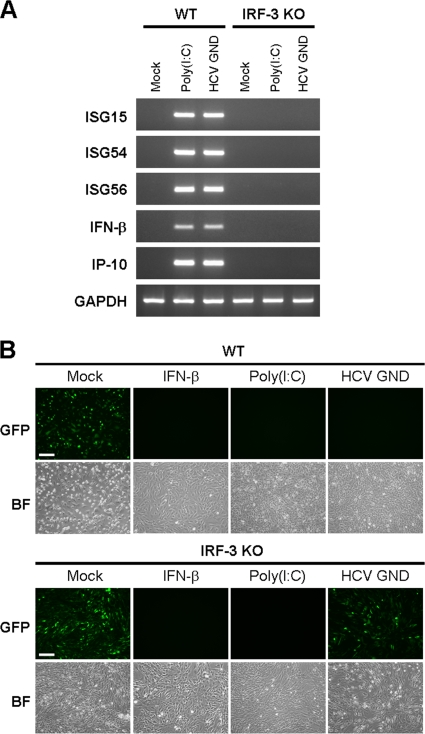
The induction of type I IFNs and the ISGs can dramatically inhibit the replication capacity of HCV RNA (34). We postulated that the enhanced ability of HCV RNA to replicate in IRF-3-deficient murine cells was due to a diminished antiviral response. To validate this hypothesis, we examined the expression of IFN-β and several IRF-3-associated ISGs, including ISG15, ISG54, ISG56, and IP-10 (5), in WT and IRF-3 null MEFs in the presence of HCV RNA. HCV RNA is recognized by RIG-I, through the single-stranded-RNA 3′-poly(U/UC) region (63), which subsequently triggers hepatic innate immunity through activation of IRF-3 (65). The nonreplicative, in vitro-transcribed, single-stranded HCV GND RNA was used in our experiment, and poly(I:C) was included as a control in experiments designed to trigger the antiviral response. HCV GND RNA or poly(I:C) was introduced into WT MEFs and IRF-3-deficient MEFs by electroporation, and the presence of ISG15, ISG54, ISG56, IFN-β, and IP-10 mRNAs was assessed 6 h later by RT-PCR. The induction of an ISG response was completely absent in IRF-3-deficient cells (Fig. 3 A). To determine whether the induction of IFN-β and ISGs reflected the establishment of a true antiviral state within the MEFs, we performed a VSV interferon bioassay by inoculating mouse cells with VSV-GFP after they had been induced for 24 h with either electroporated HCV GND RNA or poly(I:C). As expected, the antiviral response triggered by HCV GND RNA was sufficient to block VSV infection in WT MEFs but not in IRF-3 null cells (Fig. 3B). Interestingly, the presence of poly(I:C) established an antiviral state in both WT and IRF-3-deficient MEFs, which confirms recent reports in the literature that poly(I:C) can trigger an IRF-3-independent antiviral response (24). In summary, our results suggest that HCV RNA can trigger an antiviral state in WT MEFs and that IRF-3, type I IFN, and activation of downstream ISGs prevent the establishment of HCV replicons in these cells. Deletion of IRF-3 alleviates this situation and permits the synthesis of HCV RNA and expression of viral proteins.
FIG. 3.
HCV RNA does not induce an antiviral state against VSV in IRF-3-deficient (KO) MEFs. (A) RT-PCR analysis of IRF-3-associated ISGs in WT and IRF-3-deficient (KO) MEFs following mock electroporation with buffer or electroporation with 10 μg of nonreplicating subgenomic HCV GND RNA or poly(I:C). Total RNA was harvested at 6 h postelectroporation and subjected to RT-PCR for the indicated genes, using gene-specific oligonucleotide primers. Representative data from two independent experiments are shown. (B) VSV interferon bioassay on WT and IRF-3-deficient (KO) MEFs that were mock electroporated or electroporated with 10 μg of HCV GND RNA or poly(I:C). Twenty-four hours following electroporation, a VSV-GFP infectivity assay (MOI = 0.01) was carried out, and images were taken between 24 and 48 h postinfection, at a magnification of ×100. An IFN-β-positive control on mock-electroporated cells was also included. GFP, green fluorescent protein; BF, bright field. Bars, 200 μm. Representative images are from two independent experiments.
Liver-specific miR-122 promotes subgenomic HCV replication in WT and IRF-3−/− MEFs.
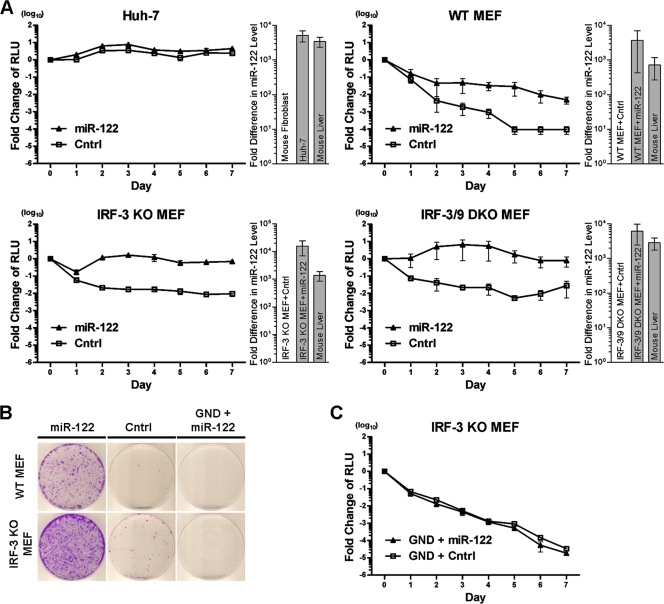
While we observed that deletion of a host innate immune factor such as IRF-3 contributed to permissive HCV RNA replication, we speculated that other human liver-specific host factors could affect HCV RNA production in mouse cells. We therefore examined the effects of miR-122, which is known to promote HCV propagation in nonhepatic human cells (19). The mature sequence of the liver-specific miR-122 is actually conserved between humans and mice (20). We used miR-122 in both transient luciferase and cell colony formation assays by coelectroporating cells with HCV replicon RNA and miRNA into the different mouse fibroblasts. The presence of exogenously introduced miR-122 in mouse fibroblasts was verified by TaqMan probe qPCR, and miR-122 levels in mouse liver cells were assayed and included as a positive control. miR-122 was detected only in the transfected MEFs or in the mouse liver cells, with levels in both cell types being comparable (Fig. 4 A, bar graphs on the right of each panel).
FIG. 4.
Liver-specific miR-122 promotes HCV replication in mouse fibroblasts. (A) Transient replication assay using the HCV SGR-Luc-JFH1 Pol+ RNA with miR-122 or negative-control miRNA (Cntrl) in Huh-7 cells and WT, IRF-3-deficient (KO), and IRF-3/9-deficient (DKO) MEFs. Cells were coelectroporated with the HCV RNA in combination with miR-122 or negative-control miRNA, harvested at the indicated time points, and then assayed for luciferase activity. Data are plotted as in Fig. 1B, where each point represents the mean value for three independent experiments, with error bars showing the SEM. Shown on the right of each panel is the TaqMan probe qPCR detection of the exogenously introduced mature miR-122 sequence in comparison to control miRNA and mouse liver. Data from three independent experiments were plotted on a log scale, with error bars showing SEM. (B) Colony formation assay using HCV SGR-Bsd-JFH1 Pol+ RNA with miR-122 or control miRNA (Cntrl) and Pol− RNA (GND) with miR-122 in WT and IRF-3-deficient (KO) MEFs. Cells were coelectroporated with the HCV RNA in combination with miR-122 or control miRNA, seeded at a 1:10 dilution, and then selected with blasticidin for 2 to 3 weeks before being stained with crystal violet. Representative images are from three independent experiments. (C) Transient replication assays using the nonreplicating HCV SGR-Luc-JFH1 Pol− RNA (GND) with miR-122 or control miRNA (Cntrl) in IRF-3-deficient (KO) MEFs. Data are expressed as in panel A, with each point representing the mean value for three independent experiments, with error bars showing the SEM.
In transient assays, input of miR-122 into Huh-7 cells, which normally express high levels of endogenous miR-122, did not further enhance HCV replication, suggesting that the stimulatory effect of miR-122 was saturated (Fig. 4A). However, our data demonstrated that introduction of miR-122 into mouse fibroblasts could promote HCV RNA synthesis even when IRF-3 was present in the cell (Fig. 4A). This enhancement of HCV replication by miR-122 appeared stronger than the stimulation elicited by IRF-3 deletion (Fig. 4A versus Fig. 1B). The same results were evident when HCV replicon activity was measured in MEF colony formation assays performed in the presence or absence of exogenously introduced miR-122 (Fig. 4B and Table 1). Furthermore, the combination of the presence of miR-122 and the deficiency of IRF-3 was cooperative in MEFs and produced even higher HCV replication levels in luciferase reporter and colony formation assays. Again, deletion of IRF-9 did not enhance HCV replication due to IRF-3 deficiency, even in the presence of miR-122 (Fig. 4A). The levels of HCV replication obtained in the IRF-3-deficient MEFs containing miR-122 approached those obtained in Huh-7 cells, which seems to confirm that miR-122 expression and defects in innate immunity likely account for the robust replication of HCV in Huh-7 cells.
We also sought to clarify whether the enhancement of HCV replicon activity resulting from the presence of miR-122 was due to its effects on replication or the translation of the viral RNA. When we compared replicon luciferase activities from nonreplicating HCV GND subgenomic RNA in IRF-3-deficient MEFs either containing or not containing miR-122, we observed no difference (Fig. 4C). Similarly, IRF-3-deficient MEFs containing nonreplicating HCV GND subgenomic RNA did not form any replicon colonies in the presence or absence of miR-122 (Fig. 4B). These results seemed to indicate that miR-122 impacted viral RNA replication in order to increase replicon luciferase activity and colony formation. However, a role for miR-122 in translation and HCV protein synthesis cannot be ruled out completely.
Overall, our results suggest that the liver-specific miR-122 constitutes an important host factor for HCV replication in mouse fibroblasts, which also implies that the effect of miR-122 on HCV propagation in the liver is conserved in both humans and mice. Furthermore, while miR-122 can independently promote HCV RNA production, its effects are even more pronounced in the absence of the innate immune factor IRF-3.
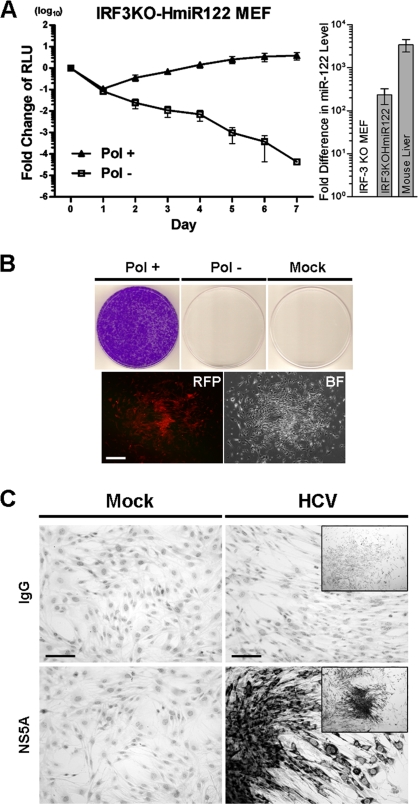
Efficient replication of HCV replicon RNA in IRF-3-deficient fibroblasts that stably express miR-122.
Based upon the previous observations, we attempted to establish HCV replication in IRF-3-deficient MEFs that stably expressed the human primary transcript for miR-122 (pri-miR-122). The pri-miR-122 transcript was introduced into these cells with a VSV-G-pseudotyped pLemiR lentivirus expression vector from Open Biosystems. Expression of the processed mature miR-122 was validated by TaqMan probe real-time qPCR specific only for the mature sequence of miR-122. In addition, expression of TurboRFP, which is also encoded in the lentivirus expression vector, and of puromycin resistance indicated successful transduction into the target cells. We could detect the mature miR-122 sequence in the transduced cells, demonstrating that the human precursor (pre-miR-122) was cleaved in the mouse system. Although the levels of lentivirus-expressed miR-122 levels were lower than those detected in transfected cells (Fig. 4A versus Fig. 5 A, bar graphs), the transduced miR-122 effectively stimulated transient HCV RNA replication and replicon colony formation in these cells (IRF3KO-HmiR122 MEFs). Specifically, the IRF3KO-HmiR122 MEFs produced a firefly luciferase activity profile with a magnitude that more closely resembled that observed in Huh-7 cells than that in the parental miR-122-negative IRF-3-deficient fibroblasts (Fig. 5A versus Fig. 1B). Similarly, the number of cell colonies obtained with the IRF3KO-HmiR122 MEFs was 10-fold higher than that obtained with IRF-3-deficient fibroblasts alone and, again, approached the levels seen in Huh-7 cells. The result obtained was also comparable to that observed previously during the transient introduction of exogenous miR-122 (Fig. 5B and Table 1). Authentic HCV replication and NS5A protein production were also verified in these miR-122-expressing fibroblast colonies (Fig. 5C), and genomic integration of the Bsd gene or HCV cDNA was not detected (data not shown). This cell model validates our observations that the deficiency of IRF-3 and the presence of liver-specific miR-122 provide a favorable environment for replication of HCV subgenomic replicon RNA in mouse fibroblasts.
FIG. 5.
HCV replicon RNA replicates efficiently in IRF-3-deficient MEFs stably expressing miR-122, introduced into cells by lentivirus transduction. (A) Transient replication assay using the HCV SGR-Luc-JFH1 RNA in IRF-3-deficient (KO) cells stably expressing human liver-specific miR-122 (IRF3KO-HmiR122 MEFs). The assay was performed as described in the legend to Fig. 1B. Each point represents the mean value for three independent experiments, with error bars showing the SEM. Pol + (solid triangles), polymerase-active HCV RNA; Pol − (open squares), polymerase-defective (nonreplicating; GND) control. The bar graph on the right is the TaqMan probe qPCR detection of the mature miR-122 sequence in the IRF3KO-HmiR122 MEFs in comparison to parental IRF-3-deficient (KO) MEFs and mouse liver for three independent experiments, with the data plotted on a log scale and error bars showing SEM. (B) Colony formation assay using HCV SGR-Bsd-JFH1 RNA in IRF3KO-HmiR122 MEFs. The assay was performed as described in the legend to Fig. 1C, with electroporated cells seeded at a 1:2 ratio. The images shown are representative images from three independent experiments. The established colonies express TurboRFP (bottom panels) due to miR-122 expression. The photomicrographs were taken at a magnification of ×50. Bar, 200 μm. Pol +, polymerase-active HCV replicon RNA; Pol −, polymerase-defective (nonreplicating; GND) replicon control; mock, mock electroporation with buffer; RFP, red fluorescent protein; BF, bright field. (C) Detection of HCV NS5A protein in IRFKO-HmiR122 MEF colonies established with HCV SGR-Bsd-JFH1 RNA. The assay was performed as described in the legend to Fig. 2, using primary mouse anti-NS5A antibodies, alkaline phosphatase goat anti-mouse secondary antibodies, and NBT/BCIP detection. Photomicrographs were taken at a magnification of ×200, and the insets showing colonies were photographed at a magnification of ×50. Bars, 100 μm. Representative images are from two independent experiments.
DISCUSSION
Restriction of HCV replication in mouse cells can be attributed to the presence or absence of primate- or organ-specific factors that affect virus attachment, entry, replication, packaging, and assembly. Determinants for HCV entry into rodent cells have been investigated previously (31, 50, 51, 59, 60, 76, 80), and many of the limiting entry factors necessary for the uptake of the virus have been identified. Specifically, expression of the tetraspanin human cluster of differentiation 81 (CD81) and the tight-junction protein occludin (OCLN) can overcome the receptor entry block of HCV particles into mouse cells. Other entry factors, such as claudin 1 (CLDN1), glycosaminoglycans (GAG), low-density lipoprotein receptor (LDLR), and scavenger receptor class B member 1 (SR-BI), are highly homologous to their mouse counterparts and still function in the rodent host (60). However, no infectious particles are released from rodent cell lines expressing human CD81 and OCLN, indicating that other host and tissue restriction factors prevail to inhibit virus replication and virion assembly (52, 73).
Host innate immunity is a determining factor for permissive infections and tropism in many viral systems (30, 53). Myxoma virus infections are specific for rabbits, and this tropism is mediated by interferon STAT-1-mediated type I IFN responses. Wild-type mice are normally resistant to myxoma virus but succumb to infection if the STAT-1 gene is deleted (74). Vaccinia virus virulence genes that target the antiviral protein PKR, including E3L and K3L, can allow the virus to replicate in HeLa and BHK21 cells, but these cells are nonpermissive to viruses in which these genes have been deleted (11, 12). Another example of the importance of host innate immunity in determining host resistance is the mouse model for measles virus. Rodents are normally resistant to measles virus, but transient infections can be achieved in mice expressing primate-specific receptors (CD46 and CD150) for the virus, although these infections are limited due to the presence of an intact innate immune system (17). However, greatly improved replication of measles virus can be observed if the CD46/CD150 mouse is bred into a STAT-1-deficient or interferon receptor-deficient background (27, 77). The preceding examples provide a precedent for the importance of both receptors and innate immunity in determining whether a particular host is susceptible to virus infections.
It is known that HCV translation and genome replication can be influenced by host-specific factors that have been elucidated from experiments with nonliver and nonprimate cells (2, 21, 52, 59, 73, 79, 80, 82). Although the growth and establishment of HCV replicons can be optimized for RNA synthesis through adaptive mutations within the viral genome in the host cell (15, 41, 47, 48), the presence or absence of these host-specific factors significantly influences HCV replication in a particular cell type (8, 9, 47). An appreciation for the impact of the host cell environment on HCV replication is gained by emphasizing the narrow range of cell lines that are susceptible to viral replication. Through functional genetic and proteomic approaches, exhaustive lists of host factors influencing the HCV life cycle have been assembled (recently reviewed in references 18, 56, and 61). Components related to immunity (TRAF2, JAK1, cyclophilin A/B, and lymphotoxin β) and the miRNA processing and effector system (miR-122, miR-199a, DICER1, and RNA helicase) are some of the factors in these lists. Our findings that IRF-3 and miR-122 act as independent host factors influencing HCV RNA replication validate this approach and suggest that they may have roles in regulating HCV infections in a mouse genetic background.
The importance of host innate immunity in controlling HCV is underscored by the IFN-α-based therapies currently used for treatment of hepatitis C. It is also believed that the innate immune response helps to determine the quality and strength of adaptive immunity and its effect on the outcome of an infection, i.e., resolution or establishment of a chronic persistent infection (26, 30, 71). HCV is very adept at crippling the host's innate immune system. For instance, the HCV NS3/4A protease cleaves the IFN-β promoter stimulator 1 (IPS-1) (49) and Toll-interleukin-1 receptor-domain-containing adapter-inducing IFN-β (TRIF) (45) adaptor proteins, thereby blocking and attenuating the RIG-I- and TLR3-mediated activation of the IRF-3/type I IFN pathway (28, 29). Although HCV possesses these immune evasion strategies, they may not be efficient enough to escape innate immune surveillance in vitro. We postulated that the relative potency of the host cell innate immune system could determine the efficiency of HCV replication in vitro. The immune characteristics of Huh-7 (TLR3 deficient) (44) and Huh-7.5 (TLR3 and RIG-I defective) (70) cells support this notion. Interestingly, defects in Huh-7 cell lines leading to enhanced HCV replication all revolve around inactivation of IRF-3, thus emphasizing IRF-3's critical role in controlling HCV (29, 64, 78). On the other hand, several studies indicated only limited participation of this transcription factor in inhibiting the virus (1, 4) and in permissiveness of Huh-7 cells to HCV replication (14). However, our results clearly demonstrate that the IRF-3 pathway and the subsequent activation of type I IFN and induction of ISGs play a principal role in controlling HCV in mouse cells. Deletion of IRF-3 seemed sufficient for these outcomes, since an additional deletion of IRF-9 leading to decreased production of IRF-7 in the IRF-3−/− IRF-9−/− MEFs did not further stimulate HCV replication. Previous questions about the importance of IRF-3 in controlling HCV replication could be due to host species-specific differences in the immune proteins and alternative IRF-3/IRF-7-independent pathways that are present in some cell types (22, 23, 44).
The positive effect mediated by miR-122 on the growth of HCV is now widely accepted and was recently shown to be a valuable therapeutic target for decreasing HCV loads in chimpanzees (42). Indeed, from our transient assays or colony formation studies, exogenous introduction of liver-specific miR-122 into mouse fibroblasts created a permissive environment for HCV replication, irrespective of whether IRF-3 was expressed or not. However, HCV replication was still enhanced significantly in IRF-3-deficient mouse fibroblasts compared to that of the same replicon in wild-type fibroblasts. The presence of miR-122 and a crippled innate immune system likely explain why Huh-7 cells and derivative cell lines (Huh-7.5 and Huh-7.5.1) are the cell lines of choice for in vitro studies with HCV (16, 47, 81). More specifically, we observed an effect of miR-122 on HCV RNA replication only and found that it did not appear to enhance translation and protein synthesis from a nonreplicating subgenomic replicon. In this regard, the precise mechanism by which miR-122 enhances HCV production is still hotly debated. Both the regulation of viral RNA abundance/amplification (19, 36, 37, 68) and the stimulation of viral RNA translation (25, 32) have been proposed as possible targets of action for miR-122. However, the use of a bicistronic replicon system could complicate the debate due to the presence of the picornavirus (encephalomyocarditis virus [EMCV]) IRES that is used to control translation of the HCV nonstructural proteins. The EMCV IRES is not recognized by miR-122, and although the reporter gene or drug selection marker is under the control of the HCV IRES, the foreign IRES could prevent an enhancement of viral translation and production of HCV proteins (57). Nevertheless, we did observe that miR-122 facilitates the synthesis of HCV subgenomic replicons in mouse fibroblasts. Further investigation with a full-length HCV replicon solely under the control of the HCV 5′-UTR IRES may clarify the controversy about the enhancement of translation or replication. A recent report examined this issue by using such a full-length replicon reporter, demonstrating that miR-122 promoted viral translation to yield efficient virion production (35). However, the authors concluded that miR-122 is likely involved in other aspects of viral genome amplification.
Our study is an important step in overcoming the HCV replication barrier in mice by use of a minimal number of factors to drive HCV replication in rodent cells. The information provided here could be a prelude to exploring viral packaging steps in murine host cells. The next step would be to express human-specific receptors for the virus (CD81 and OCLN) in IRF-3-deficient MEFs expressing miR-122 or in IRF-3-deficient hepatocytes and to study virion packaging, assembly, and egress from the host cell. Additional host factors derived from the liver may have to be identified to facilitate understanding the complete life cycle of HCV in mouse cells. These studies will eventually translate to the generation of efficient small-animal models and will offer improvements over existing in vivo HCV systems. Knowledge related to these processes will also undoubtedly expose new targets for antiviral therapy.
Acknowledgments
We thank Stanley M. Lemon, Charles M. Rice, John McLaughlan, Brian D. Lichty, and Brent Johnston for reagents and Chueh-Yao Chung and Ting-Ying Chen for technical assistance.
L.-T.L. is a recipient of a National CIHR Research Training Program in Hepatitis C (NCRTP-HepC) fellowship. This study was supported by an operating grant from the Canadian Institutes of Health Research (CIHR-EOP-38155) and by a Canadian Institutes of Health Research team grant (CIHR-85517).
The authors declare that no competing interests exist.
Footnotes
Published ahead of print on 30 June 2010.
REFERENCES
- 1.Ali, S., and G. Kukolj. 2005. Interferon regulatory factor 3-independent double-stranded RNA-induced inhibition of hepatitis C virus replicons in human embryonic kidney 293 cells. J. Virol. 79:3174-3178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ali, S., C. Pellerin, D. Lamarre, and G. Kukolj. 2004. Hepatitis C virus subgenomic replicons in the human embryonic kidney 293 cell line. J. Virol. 78:491-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alvarez-Garcia, I., and E. A. Miska. 2005. MicroRNA functions in animal development and human disease. Development 132:4653-4662. [DOI] [PubMed] [Google Scholar]
- 4.Aly, H. H., K. Watashi, M. Hijikata, H. Kaneko, Y. Takada, H. Egawa, S. Uemoto, and K. Shimotohno. 2007. Serum-derived hepatitis C virus infectivity in interferon regulatory factor-7-suppressed human primary hepatocytes. J. Hepatol. 46:26-36. [DOI] [PubMed] [Google Scholar]
- 5.Andersen, J., S. VanScoy, T. F. Cheng, D. Gomez, and N. C. Reich. 2008. IRF-3-dependent and augmented target genes during viral infection. Genes Immun. 9:168-175. [DOI] [PubMed] [Google Scholar]
- 6.Bartel, D. P. 2004. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116:281-297. [DOI] [PubMed] [Google Scholar]
- 7.Bartenschlager, R. 2006. Hepatitis C virus molecular clones: from cDNA to infectious virus particles in cell culture. Curr. Opin. Microbiol. 9:416-422. [DOI] [PubMed] [Google Scholar]
- 8.Bartenschlager, R., A. Kaul, and S. Sparacio. 2003. Replication of the hepatitis C virus in cell culture. Antiviral Res. 60:91-102. [DOI] [PubMed] [Google Scholar]
- 9.Bartenschlager, R., and T. Pietschmann. 2005. Efficient hepatitis C virus cell culture system: what a difference the host cell makes. Proc. Natl. Acad. Sci. U. S. A. 102:9739-9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barth, H., E. Robinet, T. J. Liang, and T. F. Baumert. 2008. Mouse models for the study of HCV infection and virus-host interactions. J. Hepatol. 49:134-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beattie, E., E. B. Kauffman, H. Martinez, M. E. Perkus, B. L. Jacobs, E. Paoletti, and J. Tartaglia. 1996. Host-range restriction of vaccinia virus E3L-specific deletion mutants. Virus Genes 12:89-94. [DOI] [PubMed] [Google Scholar]
- 12.Beattie, E., E. Paoletti, and J. Tartaglia. 1995. Distinct patterns of IFN sensitivity observed in cells infected with vaccinia K3L- and E3L-mutant viruses. Virology 210:254-263. [DOI] [PubMed] [Google Scholar]
- 13.Bialek, S. R., and N. A. Terrault. 2006. The changing epidemiology and natural history of hepatitis C virus infection. Clin. Liver Dis. 10:697-715. [DOI] [PubMed] [Google Scholar]
- 14.Binder, M., G. Kochs, R. Bartenschlager, and V. Lohmann. 2007. Hepatitis C virus escape from the interferon regulatory factor 3 pathway by a passive and active evasion strategy. Hepatology 46:1365-1374. [DOI] [PubMed] [Google Scholar]
- 15.Blight, K. J., A. A. Kolykhalov, and C. M. Rice. 2000. Efficient initiation of HCV RNA replication in cell culture. Science 290:1972-1974. [DOI] [PubMed] [Google Scholar]
- 16.Blight, K. J., J. A. McKeating, and C. M. Rice. 2002. Highly permissive cell lines for subgenomic and genomic hepatitis C virus RNA replication. J. Virol. 76:13001-13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blixenkrone-Moller, M., A. Bernard, A. Bencsik, N. Sixt, L. E. Diamond, J. S. Logan, and T. F. Wild. 1998. Role of CD46 in measles virus infection in CD46 transgenic mice. Virology 249:238-248. [DOI] [PubMed] [Google Scholar]
- 18.Bode, J. G., E. D. Brenndorfer, J. Karthe, and D. Haussinger. 2009. Interplay between host cell and hepatitis C virus in regulating viral replication. Biol. Chem. 390:1013-1032. [DOI] [PubMed] [Google Scholar]
- 19.Chang, J., J. T. Guo, D. Jiang, H. Guo, J. M. Taylor, and T. M. Block. 2008. Liver-specific microRNA miR-122 enhances the replication of hepatitis C virus in nonhepatic cells. J. Virol. 82:8215-8223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang, J., E. Nicolas, D. Marks, C. Sander, A. Lerro, M. A. Buendia, C. Xu, W. S. Mason, T. Moloshok, R. Bort, K. S. Zaret, and J. M. Taylor. 2004. miR-122, a mammalian liver-specific microRNA, is processed from hcr mRNA and may downregulate the high affinity cationic amino acid transporter CAT-1. RNA Biol. 1:106-113. [DOI] [PubMed] [Google Scholar]
- 21.Chang, K. S., Z. Cai, C. Zhang, G. C. Sen, B. R. Williams, and G. Luo. 2006. Replication of hepatitis C virus (HCV) RNA in mouse embryonic fibroblasts: protein kinase R (PKR)-dependent and PKR-independent mechanisms for controlling HCV RNA replication and mediating interferon activities. J. Virol. 80:7364-7374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Daffis, S., M. A. Samuel, B. C. Keller, M. Gale, Jr., and M. S. Diamond. 2007. Cell-specific IRF-3 responses protect against West Nile virus infection by interferon-dependent and -independent mechanisms. PLoS Pathog. 3:e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daffis, S., M. S. Suthar, K. J. Szretter, M. Gale, Jr., and M. S. Diamond. 2009. Induction of IFN-beta and the innate antiviral response in myeloid cells occurs through an IPS-1-dependent signal that does not require IRF-3 and IRF-7. PLoS Pathog. 5:e1000607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DeWitte-Orr, S. J., D. R. Mehta, S. E. Collins, M. S. Suthar, M. Gale, Jr., and K. L. Mossman. 2009. Long double-stranded RNA induces an antiviral response independent of IFN regulatory factor 3, IFN-beta promoter stimulator 1, and IFN. J. Immunol. 183:6545-6553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diaz-Toledano, R., A. Ariza-Mateos, A. Birk, B. Martinez-Garcia, and J. Gomez. 2009. In vitro characterization of a miR-122-sensitive double-helical switch element in the 5′ region of hepatitis C virus RNA. Nucleic Acids Res. 37:5498-5510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dustin, L. B., and C. M. Rice. 2007. Flying under the radar: the immunobiology of hepatitis C. Annu. Rev. Immunol. 25:71-99. [DOI] [PubMed] [Google Scholar]
- 27.Ferreira, C. S., M. Frenzke, V. H. Leonard, G. G. Welstead, C. D. Richardson, and R. Cattaneo. 2010. Measles virus infection of alveolar macrophages and dendritic cells precedes spread to lymphatic organs in transgenic mice expressing human signaling lymphocytic activation molecule (SLAM, CD150). J. Virol. 84:3033-3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Foy, E., K. Li, R. Sumpter, Jr., Y. M. Loo, C. L. Johnson, C. Wang, P. M. Fish, M. Yoneyama, T. Fujita, S. M. Lemon, and M. Gale, Jr. 2005. Control of antiviral defenses through hepatitis C virus disruption of retinoic acid-inducible gene-I signaling. Proc. Natl. Acad. Sci. U. S. A. 102:2986-2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Foy, E., K. Li, C. Wang, R. Sumpter, Jr., M. Ikeda, S. M. Lemon, and M. Gale, Jr. 2003. Regulation of interferon regulatory factor-3 by the hepatitis C virus serine protease. Science 300:1145-1148. [DOI] [PubMed] [Google Scholar]
- 30.Gale, M., Jr., and E. M. Foy. 2005. Evasion of intracellular host defence by hepatitis C virus. Nature 436:939-945. [DOI] [PubMed] [Google Scholar]
- 31.Haid, S., M. P. Windisch, R. Bartenschlager, and T. Pietschmann. 2010. Mouse-specific residues of claudin-1 limit hepatitis C virus genotype 2a infection in a human hepatocyte cell line. J. Virol. 84:964-975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Henke, J. I., D. Goergen, J. Zheng, Y. Song, C. G. Schuttler, C. Fehr, C. Junemann, and M. Niepmann. 2008. microRNA-122 stimulates translation of hepatitis C virus RNA. EMBO J. 27:3300-3310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Honda, K., A. Takaoka, and T. Taniguchi. 2006. Type I interferon [corrected] gene induction by the interferon regulatory factor family of transcription factors. Immunity 25:349-360. [DOI] [PubMed] [Google Scholar]
- 34.Itsui, Y., N. Sakamoto, M. Kurosaki, N. Kanazawa, Y. Tanabe, T. Koyama, Y. Takeda, M. Nakagawa, S. Kakinuma, Y. Sekine, S. Maekawa, N. Enomoto, and M. Watanabe. 2006. Expressional screening of interferon-stimulated genes for antiviral activity against hepatitis C virus replication. J. Viral Hepat. 13:690-700. [DOI] [PubMed] [Google Scholar]
- 35.Jangra, R. K., M. Yi, and S. M. Lemon. 2010. Regulation of hepatitis C virus translation and infectious virus production by the microRNA miR-122. J. Virol. 84:6615-6625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jopling, C. L., S. Schutz, and P. Sarnow. 2008. Position-dependent function for a tandem microRNA miR-122-binding site located in the hepatitis C virus RNA genome. Cell Host Microbe 4:77-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jopling, C. L., M. Yi, A. M. Lancaster, S. M. Lemon, and P. Sarnow. 2005. Modulation of hepatitis C virus RNA abundance by a liver-specific microRNA. Science 309:1577-1581. [DOI] [PubMed] [Google Scholar]
- 38.Kato, T., T. Date, M. Miyamoto, A. Furusaka, K. Tokushige, M. Mizokami, and T. Wakita. 2003. Efficient replication of the genotype 2a hepatitis C virus subgenomic replicon. Gastroenterology 125:1808-1817. [DOI] [PubMed] [Google Scholar]
- 39.Kato, T., T. Date, M. Miyamoto, Z. Zhao, M. Mizokami, and T. Wakita. 2005. Nonhepatic cell lines HeLa and 293 support efficient replication of the hepatitis C virus genotype 2a subgenomic replicon. J. Virol. 79:592-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kawai, T., and S. Akira. 2006. Innate immune recognition of viral infection. Nat. Immunol. 7:131-137. [DOI] [PubMed] [Google Scholar]
- 41.Krieger, N., V. Lohmann, and R. Bartenschlager. 2001. Enhancement of hepatitis C virus RNA replication by cell culture-adaptive mutations. J. Virol. 75:4614-4624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lanford, R. E., E. S. Hildebrandt-Eriksen, A. Petri, R. Persson, M. Lindow, M. E. Munk, S. Kauppinen, and H. Orum. 2010. Therapeutic silencing of microRNA-122 in primates with chronic hepatitis C virus infection. Science 327:198-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lavanchy, D. 2009. The global burden of hepatitis C. Liver Int. 29(Suppl. 1):74-81. [DOI] [PubMed] [Google Scholar]
- 44.Li, K., Z. Chen, N. Kato, M. Gale, Jr., and S. M. Lemon. 2005. Distinct poly(I-C) and virus-activated signaling pathways leading to interferon-beta production in hepatocytes. J. Biol. Chem. 280:16739-16747. [DOI] [PubMed] [Google Scholar]
- 45.Li, K., E. Foy, J. C. Ferreon, M. Nakamura, A. C. Ferreon, M. Ikeda, S. C. Ray, M. Gale, Jr., and S. M. Lemon. 2005. Immune evasion by hepatitis C virus NS3/4A protease-mediated cleavage of the Toll-like receptor 3 adaptor protein TRIF. Proc. Natl. Acad. Sci. U. S. A. 102:2992-2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lindenbach, B. D., M. J. Evans, A. J. Syder, B. Wolk, T. L. Tellinghuisen, C. C. Liu, T. Maruyama, R. O. Hynes, D. R. Burton, J. A. McKeating, and C. M. Rice. 2005. Complete replication of hepatitis C virus in cell culture. Science 309:623-626. [DOI] [PubMed] [Google Scholar]
- 47.Lohmann, V., S. Hoffmann, U. Herian, F. Penin, and R. Bartenschlager. 2003. Viral and cellular determinants of hepatitis C virus RNA replication in cell culture. J. Virol. 77:3007-3019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lohmann, V., F. Korner, A. Dobierzewska, and R. Bartenschlager. 2001. Mutations in hepatitis C virus RNAs conferring cell culture adaptation. J. Virol. 75:1437-1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Loo, Y. M., D. M. Owen, K. Li, A. K. Erickson, C. L. Johnson, P. M. Fish, D. S. Carney, T. Wang, H. Ishida, M. Yoneyama, T. Fujita, T. Saito, W. M. Lee, C. H. Hagedorn, D. T. Lau, S. A. Weinman, S. M. Lemon, and M. Gale, Jr. 2006. Viral and therapeutic control of IFN-beta promoter stimulator 1 during hepatitis C virus infection. Proc. Natl. Acad. Sci. U. S. A. 103:6001-6006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lv, L. P., S. Z. Jia, Q. L. Wang, Y. Y. Zhang, H. Zhou, and J. B. Xu. 2009. Hepatitis C virus infection of mouse hepatoma cell expressing human CD81 or LDLR. Acta Virol. 53:185-189. [DOI] [PubMed] [Google Scholar]
- 51.Masciopinto, F., G. Freer, V. L. Burgio, S. Levy, L. Galli-Stampino, M. Bendinelli, M. Houghton, S. Abrignani, and Y. Uematsu. 2002. Expression of human CD81 in transgenic mice does not confer susceptibility to hepatitis C virus infection. Virology 304:187-196. [DOI] [PubMed] [Google Scholar]
- 52.McCaffrey, A. P., K. Ohashi, L. Meuse, S. Shen, A. M. Lancaster, P. J. Lukavsky, P. Sarnow, and M. A. Kay. 2002. Determinants of hepatitis C translational initiation in vitro, in cultured cells and mice. Mol. Ther. 5:676-684. [DOI] [PubMed] [Google Scholar]
- 53.McFadden, G., M. R. Mohamed, M. M. Rahman, and E. Bartee. 2009. Cytokine determinants of viral tropism. Nat. Rev. Immunol. 9:645-655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mercer, D. F., D. E. Schiller, J. F. Elliott, D. N. Douglas, C. Hao, A. Rinfret, W. R. Addison, K. P. Fischer, T. A. Churchill, J. R. Lakey, D. L. Tyrrell, and N. M. Kneteman. 2001. Hepatitis C virus replication in mice with chimeric human livers. Nat. Med. 7:927-933. [DOI] [PubMed] [Google Scholar]
- 55.Moradpour, D., F. Penin, and C. M. Rice. 2007. Replication of hepatitis C virus. Nat. Rev. Microbiol. 5:453-463. [DOI] [PubMed] [Google Scholar]
- 56.Moriishi, K., and Y. Matsuura. 2007. Host factors involved in the replication of hepatitis C virus. Rev. Med. Virol. 17:343-354. [DOI] [PubMed] [Google Scholar]
- 57.Niepmann, M. 2009. Activation of hepatitis C virus translation by a liver-specific microRNA. Cell Cycle 8:1473-1477. [DOI] [PubMed] [Google Scholar]
- 58.Orinska, Z., E. Bulanova, V. Budagian, M. Metz, M. Maurer, and S. Bulfone-Paus. 2005. TLR3-induced activation of mast cells modulates CD8+ T-cell recruitment. Blood 106:978-987. [DOI] [PubMed] [Google Scholar]
- 59.Park, I. W., J. Ndjomou, Y. Fan, J. Henao-Mejia, and J. J. He. 2009. Hepatitis C virus is restricted at both entry and replication in mouse hepatocytes. Biochem. Biophys. Res. Commun. 387:489-493. [DOI] [PubMed] [Google Scholar]
- 60.Ploss, A., M. J. Evans, V. A. Gaysinskaya, M. Panis, H. You, Y. P. de Jong, and C. M. Rice. 2009. Human occludin is a hepatitis C virus entry factor required for infection of mouse cells. Nature 457:882-886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ploss, A., and C. M. Rice. 2009. Towards a small animal model for hepatitis C. EMBO Rep. 10:1220-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sainz, B., Jr., N. Barretto, and S. L. Uprichard. 2009. Hepatitis C virus infection in phenotypically distinct Huh7 cell lines. PLoS One 4:e6561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Saito, T., and M. Gale, Jr. 2008. Differential recognition of double-stranded RNA by RIG-I-like receptors in antiviral immunity. J. Exp. Med. 205:1523-1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Saito, T., R. Hirai, Y. M. Loo, D. Owen, C. L. Johnson, S. C. Sinha, S. Akira, T. Fujita, and M. Gale, Jr. 2007. Regulation of innate antiviral defenses through a shared repressor domain in RIG-I and LGP2. Proc. Natl. Acad. Sci. U. S. A. 104:582-587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Saito, T., D. M. Owen, F. Jiang, J. Marcotrigiano, and M. Gale, Jr. 2008. Innate immunity induced by composition-dependent RIG-I recognition of hepatitis C virus RNA. Nature 454:523-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sato, M., H. Suemori, N. Hata, M. Asagiri, K. Ogasawara, K. Nakao, T. Nakaya, M. Katsuki, S. Noguchi, N. Tanaka, and T. Taniguchi. 2000. Distinct and essential roles of transcription factors IRF-3 and IRF-7 in response to viruses for IFN-alpha/beta gene induction. Immunity 13:539-548. [DOI] [PubMed] [Google Scholar]
- 67.Schickel, R., B. Boyerinas, S. M. Park, and M. E. Peter. 2008. MicroRNAs: key players in the immune system, differentiation, tumorigenesis and cell death. Oncogene 27:5959-5974. [DOI] [PubMed] [Google Scholar]
- 68.Shan, Y., J. Zheng, R. W. Lambrecht, and H. L. Bonkovsky. 2007. Reciprocal effects of micro-RNA-122 on expression of heme oxygenase-1 and hepatitis C virus genes in human hepatocytes. Gastroenterology 133:1166-1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stojdl, D. F., B. D. Lichty, B. R. tenOever, J. M. Paterson, A. T. Power, S. Knowles, R. Marius, J. Reynard, L. Poliquin, H. Atkins, E. G. Brown, R. K. Durbin, J. E. Durbin, J. Hiscott, and J. C. Bell. 2003. VSV strains with defects in their ability to shutdown innate immunity are potent systemic anti-cancer agents. Cancer Cell 4:263-275. [DOI] [PubMed] [Google Scholar]
- 70.Sumpter, R., Jr., Y. M. Loo, E. Foy, K. Li, M. Yoneyama, T. Fujita, S. M. Lemon, and M. Gale, Jr. 2005. Regulating intracellular antiviral defense and permissiveness to hepatitis C virus RNA replication through a cellular RNA helicase, RIG-I. J. Virol. 79:2689-2699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Szabo, G., and A. Dolganiuc. 2006. HCV immunopathogenesis: virus-induced strategies against host immunity. Clin. Liver Dis. 10:753-771. [DOI] [PubMed] [Google Scholar]
- 72.Targett-Adams, P., and J. McLauchlan. 2005. Development and characterization of a transient-replication assay for the genotype 2a hepatitis C virus subgenomic replicon. J. Gen. Virol. 86:3075-3080. [DOI] [PubMed] [Google Scholar]
- 73.Uprichard, S. L., J. Chung, F. V. Chisari, and T. Wakita. 2006. Replication of a hepatitis C virus replicon clone in mouse cells. Virol. J. 3:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang, F., Y. Ma, J. W. Barrett, X. Gao, J. Loh, E. Barton, H. W. Virgin, and G. McFadden. 2004. Disruption of Erk-dependent type I interferon induction breaks the myxoma virus species barrier. Nat. Immunol. 5:1266-1274. [DOI] [PubMed] [Google Scholar]
- 75.Wang, N., Y. Liang, S. Devaraj, J. Wang, S. M. Lemon, and K. Li. 2009. Toll-like receptor 3 mediates establishment of an antiviral state against hepatitis C virus in hepatoma cells. J. Virol. 83:9824-9834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wellnitz, S., B. Klumpp, H. Barth, S. Ito, E. Depla, J. Dubuisson, H. E. Blum, and T. F. Baumert. 2002. Binding of hepatitis C virus-like particles derived from infectious clone H77C to defined human cell lines. J. Virol. 76:1181-1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Welstead, G. G., C. Iorio, R. Draker, J. Bayani, J. Squire, S. Vongpunsawad, R. Cattaneo, and C. D. Richardson. 2005. Measles virus replication in lymphatic cells and organs of CD150 (SLAM) transgenic mice. Proc. Natl. Acad. Sci. U. S. A. 102:16415-16420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yamashiro, T., N. Sakamoto, M. Kurosaki, N. Kanazawa, Y. Tanabe, M. Nakagawa, C. H. Chen, Y. Itsui, T. Koyama, Y. Takeda, S. Maekawa, N. Enomoto, H. Sakugawa, and M. Watanabe. 2006. Negative regulation of intracellular hepatitis C virus replication by interferon regulatory factor 3. J. Gastroenterol. 41:750-757. [DOI] [PubMed] [Google Scholar]
- 79.Yeh, C. T., H. Y. Lai, T. C. Chen, C. M. Chu, and Y. F. Liaw. 2001. Identification of a hepatic factor capable of supporting hepatitis C virus replication in a nonpermissive cell line. J. Virol. 75:11017-11024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yeh, C. T., H. Y. Lai, Y. J. Yeh, and J. C. Cheng. 2008. Hepatitis C virus infection in mouse hepatoma cells co-expressing human CD81 and Sip-L. Biochem. Biophys. Res. Commun. 372:157-161. [DOI] [PubMed] [Google Scholar]
- 81.Zhong, J., P. Gastaminza, G. Cheng, S. Kapadia, T. Kato, D. R. Burton, S. F. Wieland, S. L. Uprichard, T. Wakita, and F. V. Chisari. 2005. Robust hepatitis C virus infection in vitro. Proc. Natl. Acad. Sci. U. S. A. 102:9294-9299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhu, Q., J. T. Guo, and C. Seeger. 2003. Replication of hepatitis C virus subgenomes in nonhepatic epithelial and mouse hepatoma cells. J. Virol. 77:9204-9210. [DOI] [PMC free article] [PubMed] [Google Scholar]