Abstract
Rhinocladiella mackenziei is a recognized cause of endemic cerebral phaeohyphomycosis in the Middle East area. Surgical resection of the abscesses and posaconazole treatment have improved the ominous prognosis of this disease. We describe the case of a native Afghan woman living in France who presented with brain abscesses due to R. mackenziei.
CASE REPORT
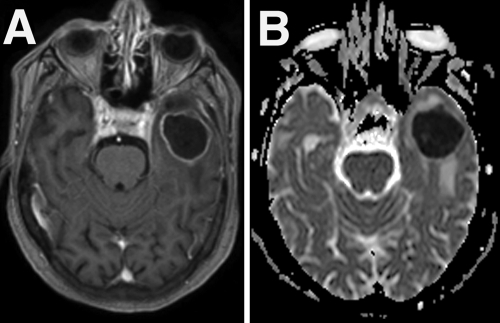
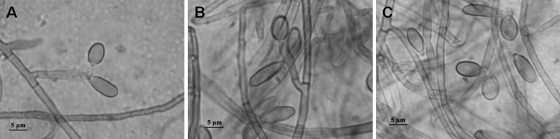
An 80-year-old Afghan woman, native of Kabul, with a history of ischemic heart disease and colon cancer, living in France for 20 years, with no travel to Middle Eastern countries and no return to her native country, was admitted to Antoine Charial Geriatric Hospital (Lyon, France) for a transient episode of aphasia. She was afebrile, alert, and experiencing residual expressive aphasia and had an unremarkable general evaluation. The leukocyte count was 11,400 cells/mm3, 50% of which were lymphocytes. C-reactive protein was at 19.1 mg/dl, and urinary and blood cultures were negative. Noncontrast cerebral computed tomography showed left frontal and temporal cystic lesions associated with a vasogenic edema. The total body scan was normal. Magnetic resonance (MR) imaging disclosed one frontal and one left temporal ring-enhancing lesion, with the largest in the temporal region, measuring 33 by 13 mm (Fig. 1 A). The axial diffusion-weighted MR images show increased signal intensity with a low apparent diffusion coefficient (ADC), indicating abscesses as opposed to solid tumors (Fig. 1B). A keyhole aspiration of the left temporal lesion was carried out, with the evacuation of 12 ml of creamy yellow pus. Direct microscopic examination of the aspiration fluid stained with Gram stain and hematoxylin-eosin stains revealed many leukocytes and several moniliform hyphal structures. Intravenous voriconazole, 200 mg twice daily (BID), was started. The seeding was done in blood agar, chocolate agar PolyViteX, Schaedler agar, and Schaedler broth with 0.02% of vitamin K. Detection of Aspergillus galactomannan and anti-Aspergillus antibodies in serum was negative. After 4 days of incubation at 37°C, black fungi appeared on all seeded cultures that were sent to the National Reference Center for Mycoses and Antifungals (Institut Pasteur, Paris, France). Colonies on 2% malt agar were olive green to brown, with a lanose texture. Microscopic examination revealed short conidiophores arising in right angles from dark-pigmented septate hyphae. At the apex of these conidiophores, unpigmented conidiogenous cells with short, cylindrical denticles produced conidia in sympodial succession (Fig. 2). Conidia were pale brown and ellipsoidal (8 to 10 by 4 to 5 μm), with a prominent basal scar. On the basis of the morphological features described above, the fungus was identified as Rhinocladiella mackenziei (formerly Ramichloridium mackenziei). Genomic DNA was extracted as described previously (18). The universal fungal primer pairs V9D/LS266 (10) and NL1/NL4 (15) were used to amplify the whole ITS1-5.8S-ITS2 region of the ribosomal DNA (rDNA) and the D1/D2 region of the large-subunit rDNA, respectively (9, 14, 18). PCR products were then sequenced at the sequencing facility of the Institut Pasteur. The nucleotide sequence analysis of the internal transcribed spacer (ITS) and the 28S region showed 96% and 99.2% identity, respectively, with the R. mackenziei type strain isolate CBS 650.93 (GenBank accession number AF050288). Unfortunately, at the time of writing, the culture stored at −80°C was no longer viable and prevented antifungal susceptibility testing. Two weeks after surgery, voriconazole treatment was stopped and oral posaconazole (400 mg BID) was initiated, based on a previous case report (3). Four months after surgery, the patient was conscious, with a stable neurological status. Brain computed tomography disclosed the disappearance of the right temporal lesion, seen in the previous brain computed tomography control, and a decrease of the size of the left frontal and temporal lesions. She was discharged, and treatment by posaconazole (400 mg BID) was maintained. The patient died 7 months postoperatively due to intercurrent inhalation pneumonia while still receiving posaconazole.
FIG. 1.
(A) Postcontrast axial T1-weighted MR image showing the rim-enhancing left temporal lesion with a central hypointensity. (B) The low ADC suggests the diagnosis of abscesses.
FIG. 2.
(A and B) Conidial apparatus of R. mackenziei. (C) Sympodially proliferating conidiogenous cells and conidia.
Dematiaceous fungi represent a large and heterogeneous group of filamentous molds containing melanin in their cell walls. The term phaeohyphomycosis was proposed by Ajello and Georg in 1974 as “a collective name for a group of mycosis caused by diverse genera and species of dematiaceous fungi” (1). In 2007, Arzanlou et al. integrated DNA sequence data into morphological and cultural features to resolve the species concepts and generic limits of the taxa currently placed in Periconiella, Ramichloridium, Rhinocladiella, and Veronaea and found that Rhinocladiella mackenziei was the synonym of Ramichloridium mackenziei and proposed the former name (5). R. mackenziei is a neurotropic fungus limited to patients living or coming from Middle Eastern countries, mostly from Saudi Arabia and Kuwait (Table 1). This fungus has not yet been isolated from nature, and its predilection for people living in the Middle East suggests a preference for the saprophytic phase, if existent, within arid climates (11). Of note, Ur-Rahman et al. suggested the inhalation of the fungus as a presumable portal of entry after a report of a patient with small miliary lesions in the lungs (21). Hematogenous dissemination could explain the brain infection. Based on the present description, it may be hypothesized that the latency may persist for years, as our patient had not returned to Afghanistan for 20 years. To the best of our knowledge, 21 other cases have been reported between 1983 and 2010 (3, 4, 5, 8, 9, 13, 14, 17, 19, 21). The fungus affects adults with a median age of 62 years (range, 32 to 80 years), without male predominance. An underlying disease or immunosuppression has been noticed in 14 of the previously reported cases, while 5 did not present any particular underlying disease (8, 21). Information is lacking for the 2 remaining cases (Table 1). Brain abscess is the classic pathological form at clinical presentation. Single lesions were present in 70% of cases (3, 5, 6, 8, 12, 13, 14, 19, 21). Similar to pyogenic abscess, fungal abscesses, including those caused by R. mackenziei, show a hyperintensity in diffusion-weighted imaging sequences and hypointensity in ADC maps (9). The majority of patients were treated with a combination of medical and surgical treatments. Most commonly used antifungals were amphotericin B, flucytosine, usually associated with amphotericin B, and itraconazole. This classically medical treatment was associated with a mortality of 100% (4, 6, 8, 12, 13, 14, 17, 19, 20, 21). Al-Abdely et al. compared in vitro activities and experimental efficacies of posaconazole, amphotericin B, and itraconazole against R. mackenziei and found posaconazole to be superior in reducing the brain fungal burden (2). Posaconazole (16) was previously given in two cases, and Al-Abdely et al. reported the only case of prolonged survival (4 years) in combination with surgery (3). Badali et al. showed that posaconazole has the best in vitro activity; however, because no in vitro formula is available, isavuconazole might be second best (7). Surgical resection of the abscess was used in 33% of the cases, while 67% were treated by aspiration. Ur-Rahman et al. reported the presence of branching fungal hyphae in the peripheral zone of gliosis surrounding the abscess after histological evaluation of one operative case (21). Surgical aspiration provides a transient relief of the mass effect, but surgical resection seems to be a suitable treatment for eradicating the fungus. Although rarely described, cerebral phaeohyphomycosis by R. mackenziei should be suspected in people with an isolated cystic brain lesion living in or coming from the Middle East, even multiple years after having left the area where cerebral phaeohyphomycosis is endemic. In 2010, Badali et al. reported the first case of cerebral abscess by Rhinocladiella mackenziei in India, which should now be added to the list of areas where cerebral phaeohyphomycosis is endemic, like Afghanistan, based on the present observation (6). Knowing that United States and European troops are still based in Afghanistan, one should be aware of more imported cases in returning soldiers. Surgical resection of the abscesses when they are solitary, superficial, not in motor cerebral areas, and not beside the ventricle system seems to be the more suitable surgical option. Posaconazole therapy should be promptly initiated and maintained for months.
TABLE 1.
Summary of clinical data of cerebral case reports of Rhinocladiella mackenziei
| Case(s) described in indicated reference or source | Year of publication | Patient age/gender/country or nationality | Underlying condition(s) | Probable portal of entry | No. of abscesses | Surgical treatment | Antifungal therapya | Outcome |
|---|---|---|---|---|---|---|---|---|
| 21 | 1988 | 55/F/Saudi Arabia | None | Lung | 1 | Craniotomy | AMB, 5FC | Died after 6 months |
| 80/M/Saudi Arabia | None | 1 | Aspiration | AMB, 5FC, KTC | Died after 2 months | |||
| 60/M/Saudi Arabia | None | >1 | Aspiration | AMB, 5FC, KTC | Died after 8 weeks | |||
| 8 | 1993 | 70/M/Saudi Arabia | Unknown | 1 | Aspiration | AMB | Died | |
| 70/M/Saudi Arabia | Extensive bowel surgery | >1 | Aspiration | AMB, 5FC | Died | |||
| About 60/F/Israel | Surgery | 1 | Aspiration | Unknown | Unknown | |||
| 55/M/Qatar | Renal transplant, hepatic mass, fungal eye infection | 1 | Aspiration | AMB | Died | |||
| 32/F/Oman | Renal transplant | 1 | Aspiration | Unknown | Unknown | |||
| Unknown/unknown/United Arab Emirates | 1 | Died | ||||||
| 75/F/Saudi Arabia | None | >1 | Aspiration | Unknown | Unknown | |||
| 19 | 1998 | 36/M/Saudi living in United States | Hodgkin's disease, chronic hepatitis B | 1 | Craniotomy | ITC | Died after 8 months | |
| 17 | 1999 | 58/F/Kuwaiti living in United States | Hemodialysis, steroids | >1 | Aspiration | AMB, ITC | Died after 1 month | |
| 13 | 2000 | 67/F/Saudi Arabia | Diabetes mellitus | 1 | Aspiration | AMB | Died after 10 days | |
| 65/F/Saudi Arabia | Hodgkin's lymphoma | 1 | Aspiration | AMB | Died after 3 weeks | |||
| 12 | 2001 | 71/M/Saudi Arabia | Chronic leukemia | >1 | Craniotomy | AMB, ITC | Died after 10 days | |
| 42/M/Saudi Arabia | None | 1 | Craniotomy | AMB, FLC, ITC | Died after 2 weeks | |||
| 14 | 2002 | 56/M/Egyptian living in Kuwait | Chronic hepatitis B | 1 | Aspiration | AMB | Died after 18 days | |
| 3 | 2005 | 62/M/Saudi Arabia | Renal transplant | 1 | Aspiration, craniotomy | AMB, ITC, 5FC, POS | Cured | |
| 4 | 2007 | 66/F/Saudi Arabia | Diabetes mellitus, steroids, systemic lupus erythematosus | >1 | Aspiration | AMB, VRC | Died after 5 weeks | |
| 20 | 2010 | 59/F/Qatar | Breast cancer surgery, chemotherapy | 1 | Craniotomy | AMB, VRC, POS | Died after 58 days | |
| 6 | 2010 | 50/M/India | Diabetes mellitus | 1 | Craniotomy | AMB | Died after 2 weeks | |
| Present study | 2010 | 80/F/Afghan living in France | Colon cancer surgery | >1 | Aspiration | VRC, POS | Died after 7 months |
AMB, amphotericin B; 5FC, 5 flucytosine; KTC, ketoconazole; ITC, itraconazole; FLC, fluconazole; POS, posaconazole; VRC, voriconazole.
Nucleotide sequence accession numbers.
Nucleotide sequences were deposited in GenBank under accession numbers HM359013 (ITS) and HM359014 (D1/D2).
Acknowledgments
We gratefully acknowledge the technical help of Laure Diancourt and Coralie Tran at the sequencing facility (PF-8 Genotyping of Pathogens and Public Health, Institut Pasteur).
Footnotes
Published ahead of print on 30 June 2010.
REFERENCES
- 1.Ajello, L., and L. K. Georg. 1974. A case of phaeohyphomycosis caused by a new species of Phialophora. Mycologia 66:490-498. [PubMed] [Google Scholar]
- 2.Al-Abdely, H. M., L. Najvar, R. Bocanegra, A. Fothergill, D. Loebenberg, M. G. Rinaldi, and J. R. Graybill. 2000. SCH 56592, amphotericin B, or itraconazole therapy of experimental murine cerebral phaeohyphomycosis due to Ramichloridium obovoideum (“Ramichloridium mackenziei”). Antimicrob. Agents Chemother. 44:1159-1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Abdely, H. M., A. M. Alkhunaizi, J. A. Al-Tawfiq, M. Hassounah, M. G. Rinaldi, and D. A. Sutton. 2005. Successful therapy of cerebral phaeohyphomycosis due to Ramichloridium mackenziei with the new triazole posaconazole. Med. Mycol. 43:91-95. [DOI] [PubMed] [Google Scholar]
- 4.Amr, S. S., and J. A. Al-Tawfiq. 2007. Aspiration cytology of brain abscess from a fatal case of cerebral phaeohyphomycosis due to Ramichloridium mackenziei. Diagn. Cytopathol. 35:695-699. [DOI] [PubMed] [Google Scholar]
- 5.Arzanlou, M., J. Z. Groenewald, W. Gams, U. Braun, H.-D. Shin, and P. W. Crous. 2007. Phylogenetic and morphotaxonomic revision of Ramichloridium and allied genera. Stud. Mycol. 58:57-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Badali, H., J. Chander, S. Bansal, A. Aher, S. S. Borkar, J. F. Meis, and G. S. De Hoog. 2010. First autochthonous case of Rhinocladiella mackenziei cerebral abscess outside the Middle East. J. Clin. Microbiol. 48:646-649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Badali, H., G. S. de Hoog, I. Curfs-Breuker, and J. F. Meis. 2010. In vitro activities of antifungal drugs against Rhinocladiella mackenziei, an agent of fatal brain infection. J. Antimicrob. Chemother. 65:175-177. [DOI] [PubMed] [Google Scholar]
- 8.Campbell, C. K., and S. S. A. Al-Hedaithy. 1993. Phaeohyphomycosis of the brain caused by Ramichloridium mackenziei sp. nov. in Middle East countries. J. Med. Vet. Mycol. 31:325-332. [Google Scholar]
- 9.Gaviani, P., R. B. Schwartz, E. T. Hedley-Whyte, K. L. Ligon, A. Robicsek, P. Schaefer, and J. W. Henson. 2005. Diffusion-weighted imaging of fungal cerebral infection. Am. J. Neuroradiol. 26:1115-1121. [PMC free article] [PubMed] [Google Scholar]
- 10.Gerrits van den Ende, A. H. G., and G. S. de Hoog. 1999. Variability and molecular diagnostics of the neurotropic species Cladophialophora bantiana. Stud. Mycol. 43:151-162. [Google Scholar]
- 11.Horré, R., and G. S. de Hoog. 1999. Primary cerebral infections by melanized fungi: a review. Stud. Mycol. 43:176-193. [Google Scholar]
- 12.Kanj, S. S., S. S. Amr, and G. D. Roberts. 2001. Ramichloridium mackenziei brain abscess: report of two cases and review of the literature. Med. Mycol. 39:97-102. [DOI] [PubMed] [Google Scholar]
- 13.Kashgari, T. Q., H. Al-Miniawi, and M. K. Moawad Hanna. 2000. Cerebral phaeohyphomycosis caused by Ramichloridium mackenziei in the Eastern province of Saudi Arabia. Ann. Saudi Med. 20:457-460. [DOI] [PubMed] [Google Scholar]
- 14.Khan, Z. U., S. J. Lamdhade, M. Johny, J. Al-Khalidi, A. Thussu, H. N. Yossef, I. Al-Obaid, and A. A. Nasser. 2002. Additional case of Ramichloridium mackenziei cerebral phaeohyphomycosis from the Middle East. Med. Mycol. 40:429-433. [DOI] [PubMed] [Google Scholar]
- 15.Kurtzman, C. P., and C. J. Robnett. 1997. Identification of clinically important ascomycetous yeasts based on nucleotide divergence in the 5′ end of the large-subunit (26S) ribosomal DNA gene. J. Clin. Microbiol. 35:1216-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morris, I. M. 2009. Posaconazole: a new antifungal agent with an expanded spectrum of activity. Am. J. Health Syst. Pharm. 66:225-236. [DOI] [PubMed] [Google Scholar]
- 17.Podnos, Y. D., P. Anastasio, L. De La Maza, and R. Kim. 1999. Cerebral phaeohyphomycosis caused by Ramichloridium obovoideum (Ramichloridium mackenziei): case report. Neurosurgery 45:372-375. [DOI] [PubMed] [Google Scholar]
- 18.Schwarz, P., S. Bretagne, J. C. Gantier, D. Garcia-Hermoso, O. Lortholary, F. Dromer, and E. Dannaoui. 2006. Molecular identification of zygomycetes from culture and experimentally infected tissues. J. Clin. Microbiol. 44:340-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sutton, D. A., M. Slifkin, R. Yakulis, and M. G. Rinaldi. 1998. U.S. case report of cerebral phaeohyphomycosis caused by Ramichloridium obovoideum (R. mackenziei): criteria for identification, therapy, and review of other known dematiaceous neurotropic taxa. J. Clin. Microbiol. 36:97-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taj-Aldeen, S. J., M. Almaslamani, A. Alkhal, I. Al Bozom, A. M. Romanelli, B. L. Wickes, A. W. Fothergill, and D. Sutton. 2010. Cerebral phaeohyphomycosis due to Rhinocladiella mackenziei (formerly Ramichloridium mackenziei): a taxonomic update and review of the literature. Med. Mycol. 48:546-556. [DOI] [PubMed] [Google Scholar]
- 21.Ur-Rahman, N., E. S. Mahgoub, and A. H. Chagla. 1988. Fatal brain abscesses caused by Ramichloridium obovoideum: report of three cases. Acta Neurochir. (Wien) 93:92-95. [DOI] [PubMed] [Google Scholar]