Abstract
Venezuelan equine encephalitis virus (VEEV) is a significant human and animal pathogen. The highlight of VEEV replication in vitro, in cells of vertebrate origin, is the rapid development of cytopathic effect (CPE), which is strongly dependent upon the expression of viral capsid protein. Besides being an integral part of virions, the latter protein is capable of (i) binding both the nuclear import and nuclear export receptors, (ii) accumulating in the nuclear pore complexes, (iii) inhibiting nucleocytoplasmic trafficking, and (iv) inhibiting transcription of cellular ribosomal and messenger RNAs. Using our knowledge of the mechanism of VEEV capsid protein function in these processes, we designed VEEV variants containing combinations of mutations in the capsid-coding sequences. These mutations made VEEV dramatically less cytopathic but had no effect on infectious virus production. In cell lines that have defects in type I interferon (IFN) signaling, the capsid mutants demonstrated very efficient persistent replication. In other cells, which have no defects in IFN production or signaling, the same mutants were capable of inducing a long-term antiviral state, downregulating virus replication to an almost undetectable level. However, ultimately, these cells also developed a persistent infection, characterized by continuous virus replication and beta IFN (IFN-β) release. The results of this study demonstrate that the long-term cellular antiviral state is determined by the synergistic effects of type I IFN signaling and the antiviral reaction induced by replicating viral RNA and/or the expression of VEEV-specific proteins. The designed mutants represent an important model for studying the mechanisms of cell interference with VEEV replication and development of persistent infection.
Venezuelan equine encephalitis virus (VEEV) is a significant human and animal pathogen (42). In natural conditions, viruses of the VEEV serocomplex are transmitted by mosquito vectors between vertebrate hosts and cause outbreaks of severe febrile illness and encephalitis in humans and horses in South and Central America (40). Some of the epidemics have extended to Texas and have had a strong economic impact on the United States (41). Moreover, VEEV is a very “user-friendly” virus, which can replicate to extremely high titers in most of the commonly used cell lines, is stable in lyophilized form, and can potentially be applied as a biological weapon.
In vertebrates, this virus causes severe, highly debilitating disease characterized by high-titer viremia and efficient virus replication in the lymphoid tissues and the brain (20). In mosquitoes, it develops persistent infection, which does not significantly affect the biology of these vectors. Infection in cultured cells mirrors the infection in vivo. VEEV persistently replicates in the cells of mosquito origin and is highly cytopathic in commonly used cell lines of vertebrate origin, in which its replication causes a cytopathic effect (CPE) within 24 to 48 h postinfection (16). CPE development is a multicomponent phenomenon caused by numerous, virus-induced changes in cellular biology. They not only result in modification of the intracellular environment to meet the needs of efficient virus replication but also are aimed at downregulation of cell signaling and, thus, inhibition of antiviral state development in both infected and yet-uninfected cells.
In cells infected with the Old World alphaviruses, such as Sindbis virus (SINV) and Semliki Forest virus (SFV), activation of cell signaling appears to be strongly affected by inhibition of both cellular translation and transcription (6, 10, 12, 15, 18). It was also demonstrated that nsP2 plays a key role in both of these phenomena. In the case of VEEV infection, viral structural protein, the capsid protein, but not nsP2, was shown to be a key player in the induction of transcriptional shutoff and CPE development (14, 16). Activity of capsid protein in these processes is mediated by binding of both nuclear import (importin-α/β) and export (CRM1) receptors to the amino-terminal, 39-amino-acid-long capsid peptide (termed H68). The tetrameric complex interacts with the nuclear pore complex (NPC) proteins, blocks NPC function, and inhibits nucleocytoplasmic protein transport (3). This ultimately leads to inhibition of transcription mediated by cellular DNA-dependent RNA polymerases I, II and, most likely, III, which appears to be a strong contributor to cell death (4). The difference in transcription inhibition between the New and the Old World alphaviruses is particularly evident in the cells infected with the alphavirus genome-derived replicons, which express no structural proteins. VEEV and eastern equine encephalitis virus (EEEV), but not SINV and SFV, replicons readily establish persistent replication in some of the commonly used cell lines of vertebrate origin (30, 38), and this is a strong indication that in the absence of capsid protein expression, inhibition of transcription in the cells infected with the New World alphavirus replicons does not reach the level that can cause cell death.
Capsid protein-mediated downregulation of cellular transcription appears to be a major phenomenon in VEEV-infected cells. However, capsid protein functions in NPC blocking in a stoichiometric, rather than catalytic, fashion. Therefore, its lower concentration in the cells that show to be less permissive for VEEV replication might be insufficient for complete inhibition of nucleocytoplasmic transport and transcription (3, 4). The same concern appears to be applicable to the Old World alphavirus nsP2. In this scenario, alphavirus-infected cells of vertebrate origin likely remain capable of mounting the antiviral response, characterized first of all by the induction of type I interferon (IFN) expression. Such a response is readily detectable in vivo (13, 32) after infection with the wild-type (wt) viruses, and this is an additional demonstration that inhibition of the antiviral response by replicating alphaviruses is incomplete.
Study of VEEV-host interaction in vitro is an important direction of research, but it is usually complicated by efficient CPE rapidly developing in the commonly used, permissive cell lines of vertebrate origin. Thus, the experiments aimed at studying the mechanisms of the cellular response are limited to a very short time postinfection. Application of the VEEV replicons allows for the performance of long-term experiments, but lack of expression of half of the viral genes (structural genes) in the replicon-containing cells raises a concern about the biological significance of the data.
In this study, we took advantage of the accumulated knowledge of the mechanism of VEEV capsid function in cellular transcription inhibition and designed VEEV TC-83 mutants whose capsid proteins were incapable of interfering with the transcription of cellular genes. The encoded capsid proteins contained point mutations in the nuclear localization/import signal (NLS) and/or in the peptide between the nuclear export signal (NES) and the NLS. These mutations had no noticeable effects on packaging of viral genomes into infectious particles and infectious virus production, but they made VEEV dramatically less cytopathic. The mutants represented an excellent model of virus replication under the conditions in which capsid expression was insufficient for inhibiting nuclear functions. In spite of infectious virus release to the titers of 1010 infectious units (inf. u)/ml, cells remained capable of growth. In the cell lines having defects in type I IFN signaling, capsid mutants continued replicating very efficiently, but cells having no defects in IFN production and signaling were capable of establishing a long-term antiviral state and downregulating virus replication to an almost undetectable level, but then ultimately developed a persistent infection characterized by continuous virus replication and release of alpha/beta IFN (IFN-α/β). The results strongly correlate with the previously published data about persistent alphavirus replication in vivo (2, 8, 21).
MATERIALS AND METHODS
Cell cultures.
The BHK-21 cells were kindly provided by Paul Olivo (Washington University, St. Louis, MO). The NIH 3T3 cells were obtained from the American Type Culture Collection (Manassas, VA). These cell lines were maintained at 37°C in alpha minimum essential medium (αMEM) supplemented with 10% fetal bovine serum (FBS) and vitamins. Mosquito C710 cells were kindly provided by Henry Huang (Washington University, St. Louis, MO). They were maintained in Dulbecco's MEM supplemented with 10% heat inactivated FBS and 10% tryptose phosphate broth. The IFN-α/βR−/− and wt mouse embryonic fibroblasts (MEFs) were kindly provided by Michael Diamond (Washington University, St. Louis, MO). STAT1−/− MEFs were kindly provided by Peter Mason (University of Texas Medical Branch, Galveston, TX). All of the MEFs were propagated in Dulbecco's MEM supplemented with 10% FBS and nonessential amino acids. L929 cells used for biological assay of IFN-α/β were provided by Samuel Baron (University of Texas Medical Branch, Galveston, TX). These cells were propagated in Dulbecco's MEM supplemented with 10% FBS.
Plasmid constructs.
Plasmids encoding VEEV genomes, pVEEV/GFP, pVEEV/C1/GFP, pVEEV/C2/GFP, and pVEEV/C3/GFP (see Fig. 1 for details) encoded an additional subgenomic promoter driving the expression of green fluorescent protein (GFP). Mutations in the capsid-coding sequence (Fig. 1) were introduced by PCR-mediated mutagenesis using appropriate primers and then sequenced and further cloned using standard protocols. pVEEV/C1/Neo had essentially the same design as pVEEV/C1/GFP, but the GFP sequence was replaced by the selectable marker neomycin phosphotransferase (Neo). pVEErep/GFP/Neo contained two subgenomic promoters, which controlled the expression of GFP and Neo. In all of the plasmids, viral genome- or replicon-coding cDNAs were cloned under the control of the SP6 promoter. All of the sequences and details of the cloning procedures can be provided upon request.
FIG. 1.
Schematic representation of recombinant VEEV TC-83 genomes having mutations in the H68 peptide of capsid protein, the infectivity of in vitro-synthesized viral RNAs, and virus titers at 24 after transfection of BHK-21 cells. SG indicates positions of the subgenomic promoters. Point mutations introduced into capsid protein are indicated by lowercase red letters. Boxes indicate nuclear export (NES) and nuclear import (NLS) signals. The connective peptide sequence is underlined.
RNA transcriptions.
Plasmids were purified by centrifugation in CsCl gradients. Before being subjected to a transcription reaction, plasmids were linearized using the MluI restriction site located downstream of the poly(A) sequence of the viral genomes and replicons. RNAs were synthesized by SP6 RNA polymerase in the presence of a cap analog under previously described conditions (31). The yield and integrity of transcripts were analyzed by gel electrophoresis under nondenaturing conditions. RNA concentration was measured with a FluorChem imager (Alpha Innotech), and transcription reactions were used for electroporation without additional purification.
Infectious center assay.
One μg of in vitro-synthesized, full-length RNA transcripts of viral genomes was used per electroporation. Ten-fold dilutions of electroporated BHK-21 cells were seeded in six-well Costar plates containing subconfluent naïve cells. After 1 h of incubation at 37°C in a 5% CO2 incubator, cells were overlaid with 2 ml of MEM-containing 0.5% Ultra-Pure agarose (Invitrogen) supplemented with 3% FBS. VEEV capsid mutants are capable of forming plaques under agarose cover in the presence of 3% FBS. Plaques were stained with crystal violet after 2 days of incubation at 37°C.
Viral replication analysis.
Cells were seeded at a concentration of 5 × 105 cells/35-mm dish. After 4 h of incubation at 37°C, monolayers were infected at a multiplicity of infection (MOI) of 20 PFU/cell for 1 h, washed with PBS, and overlaid with 1 ml of complete medium. At the times indicated in the figures, media were replaced by fresh media, and virus titers were determined by a plaque assay of BHK-21 cells as previously described (24). In some of the experiments, the same media were used for measuring the concentration of IFN-β.
Analysis of protein synthesis.
NIH 3T3 cells were seeded into 6-well Costar plates at a concentration of 5 × 105 cells/well and infected at an MOI of 20 PFU/cell. At the times indicated in the figure legends, the cells were incubated for 30 min in 0.8 ml of DMEM medium lacking methionine, supplemented with 0.1% FBS and 20 μCi/ml of [35S]methionine. After this incubation, they were scraped into the medium, pelleted at 1,500 rpm, and dissolved in 100 μl of standard protein loading buffer. Equal amounts of protein were loaded onto each lane of the sodium dodecyl sulfate-10% polyacrylamide gels (SDS-PAGE). After electrophoresis, the gels were dried, autoradiographed, and analyzed with a Storm 860 PhosphorImager (Molecular Dynamics). The amount of radioactivity detected in the protein band corresponding to actin was used to determine the level of residual host cell protein synthesis. The results were normalized to the amount of radioactivity detected in the same region of the lane that contained the lysate of the uninfected cells. Radioactivity in the capsid protein-specific band was used to evaluate the synthesis of viral structural proteins.
Analysis of RNA synthesis.
To analyze the synthesis of the virus-specific RNAs, the infected cells were metabolically labeled with [3H]uridine (20 μCi/ml) in the presence of actinomycin D (ActD) (1 μg/ml) for 4 h, beginning at 3 h posttransfection. Total cellular RNA was isolated by Trizol, according to the protocol recommended by the manufacturer (Invitrogen), and then denatured with glyoxal in dimethyl sulfoxide and analyzed by agarose gel electrophoresis, using previously described conditions (7). For assessment of cellular RNA synthesis, radiolabeling was performed in the absence of ActD, and the RNA analysis was executed as described elsewhere (17).
Reverse transcription-quantitative PCR (RT-qPCR).
Total RNA was isolated from NIH 3T3 cells infected with VEEV/C1/GFP or mock infected using Trizol (Invitrogen) and additionally purified with an RNeasy mini kit (Qiagen). RNA quality was analyzed by agarose gel electrophoresis. cDNA was synthesized by using 1 μg of total isolated RNA with a QuantiTect reverse transcription kit (Qiagen). Aliquots of the same cDNA solution were used for qPCR with different sets of primers. nsP2-specific primers (5′-CAGGACGATCTCATTCTCAC-3′ and 5′-TCATTCACCTTGTACCGAACG-3′) were used to evaluate the concentration of viral genomic RNA. Primers for the structural region (5′-CCACATATCTAATCACCCGCC-3′ and 5′-TTTCCCCATACAAACTCCCAC-3′) were used to quantify total viral RNA. qPCR was performed using SsoFast EvaGreen Supermix (Bio-Rad) in a CFX96 real-time PCR detection system (Bio-Rad) for 40 cycles with two steps per cycle, each step for 5 s (a denaturing step at 98°C, an annealing/extension step at 60°C). Data were analyzed with CFX Manager software. Specificity of the qPCR was confirmed by the melting curves of amplified products. Standard curves for total and genomic viral RNA were built using cDNA of a mixture of 0.9 μg total RNA from the mock-infected NIH 3T3 cells and 0.1 μg of the purified viral RNA, which was in vitro synthesized on the plasmid encoding the VEEV/C1/GFP genome. Results of the quantification were normalized to the amount of β-actin mRNA present in the same RNA samples. Each qPCR was performed in triplicate, and means and standard deviation (SD) were calculated.
IFN-α/β assay.
Concentrations of murine IFN-β in the media were determined by using a VeriKine mouse IFN-β enzyme-linked immunosorbent assay (ELISA) kit (PBL Interferon Source). In some experiments, concentrations of IFN-α/β in the media were additionally measured by a previously described biological assay (12).
RESULTS
VEEV variants with mutated H68 capsid-specific peptide.
In a previous study, we defined in the amino terminus of VEEV capsid protein a 39-aa-long active peptide (termed H68), which contained both a supraphysiological nuclear export signal (NES) and a nuclear localization/import signal (NLS) and efficiently interacted with the nuclear export and nuclear import receptors in cells of vertebrate origin (3, 4, 14). These data provided a unique opportunity to modify H68 and alter these critical interactions without affecting other capsid-specific functions in virus replication. To achieve this, we introduced combinations of point mutations into the capsid-specific NLS and into the short peptide located between the NES and NLS of the VEEV TC-83 genome. Based on our predictions, the mutations were supposed to have deleterious effects on the VEEV capsid protein functions in the inhibition of nucleocytoplasmic trafficking, transcription inhibition, and CPE development, without affecting capsid activities in the packaging of the viral genome and infectious virus production. VEEV/C1/GFP and VEEV/C2/GFP mutants contained previously identified attenuating mutations in both the connecting peptide and the NLS (3, 14), while VEEV/C3/GFP had mutations in the NLS only (Fig. 1). In all of the variants, the NES was left unchanged, because previous studies demonstrated an additional essential role of this alpha-helical peptide in capsid dimerization, which is required for the nucleocapsid formation (28, 29). All of the recombinant viral genomes also encoded GFP protein under the control of the second subgenomic promoter (Fig. 1). Expression of this protein was necessary for monitoring virus replication and spread in cultured cells in the absence of VEEV-specific CPE development. The genome of control variant VEEV/GFP had exactly the same design but encoded a wild-type VEEV capsid (Fig. 1).
The in vitro-synthesized RNAs were electroporated into BHK-21 cells, and those encoding the mutated form of capsid demonstrated the same infectivity in the infectious center assay as did the wt capsid-encoding VEEV/GFP (Fig. 1), indicating that no adaptive mutations were required for virus replication and spread. Cells electroporated with the mutant RNAs did not develop CPE and continued to grow, in spite of efficient GFP expression, which was indicative of virus replication. No profound morphological changes in the infected cells were detected either. Nevertheless, the mutants were still capable of forming plaques in BHK-21 cells under the agarose cover in low serum concentrations (serum depravation), as did previously described VEE/SINV chimeras (16). Therefore, all of the titers in Fig. 1 and the figures that follow are presented in PFU/ml. Infectious titers in the stocks of VEEV/GFP and the designed mutants were nearly identical and approached 1010 PFU/ml. Taken together, the data suggested that the H68-specific mutations in the capsid protein had no effect on virus replication but strongly affected the ability of the virus to induce CPE, at least in BHK-21 cells.
Replication of the VEEV capsid mutants in vitro is dependent on type I IFN signaling.
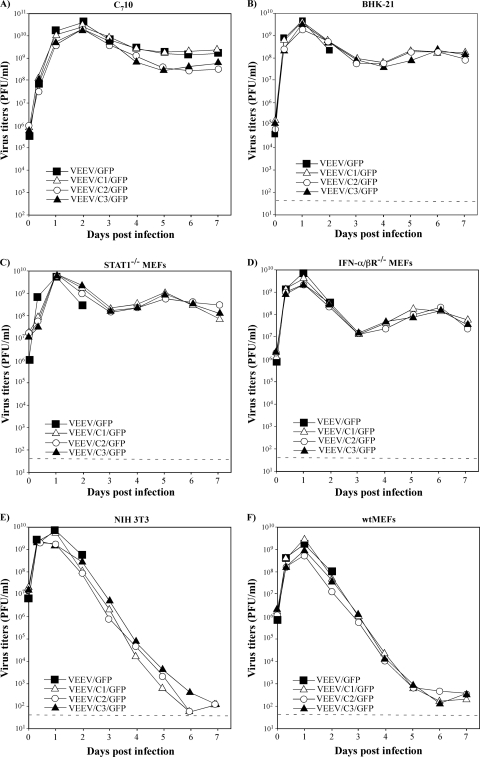
In the following experiments, we characterized replication of the designed mutants in cells of vertebrate and mosquito origin. Vertebrate cell lines were either defective in different steps of type I IFN signaling (BHK-21 cells, STAT1−/− MEFs, and IFN-α/βR−/− MEFs) or had no defects in IFN production and signaling (wt MEFs and NIH 3T3 cells). Within 24 to 48 h postinfection, VEEV/GFP caused complete CPE in all of the vertebrate cell lines used, but not in the mosquito C710 cells. The three designed mutants replicated at the same rates as the VEEV/GFP control and to the same titers but did not cause profound CPE in any cell type used. Their persistent, noncytopathic replication in mosquito cells (Fig. 2A) was not surprising, because this is a characteristic feature of all of the alphaviruses. However, the designed mutants also continued to productively replicate and were released to high titers from BHK-21 cells and IFN-α/βR−/− and STAT1−/− MEFs (Fig. 2B to D) days after all of the VEEV/GFP-infected cells were already dead, and their replication did not stop cell growth. wt MEFs and NIH 3T3 cells developed infection in a manner very different from that in the IFN-deficient cell lines (Fig. 2E and F). At the applied MOI, within 16 h postinfection, all of the cells were GFP positive, indicating virus replication in the entire monolayer. Within the first 24 h, variants with the mutated capsid replicated as efficiently as did VEEV/GFP, but after 2 to 3 days postinfection, cells stopped the production of virus. Subsequent experiments (see Fig. 5) demonstrated that the low titers detected at late times postinfection represented infectious virions still remaining in the media, but not those newly produced by cells in the monolayers. Figure 3 (see also Fig. 5C) presents different cell lines infected by VEEV/C1/GFP at day 6 postinfection. IFN-α/βR−/− and STAT1−/− MEFs continued to express GFP, indicating virus replication. NIH 3T3 and wt MEFs demonstrated a barely detectable level of GFP, suggesting that virus replication was almost over (see the following sections).
FIG. 2.
Replication of capsid mutant in the indicated cell lines. Cells were infected at an MOI of 20 PFU/cell, media were replaced at the indicated times, and virus titers were determined by a plaque assay using BHK-21 cells. Dashed lines indicate the limits of detection.
FIG. 3.
VEEV/C1/GFP develops persistent replication in STAT1−/− and IFN-α/βR−/− MEFs, but its replication is strongly inhibited in wt MEFs and NIH 3T3 cells. Cells (5 × 105) were infected with the VEEV/C1/GFP variant at an MOI of 20 PFU/cell. Images of the cells were acquired at day 6 postinfection with an inverted Nikon fluorescence microscope. The same exposure times were used for detection of GFP-positive cells.
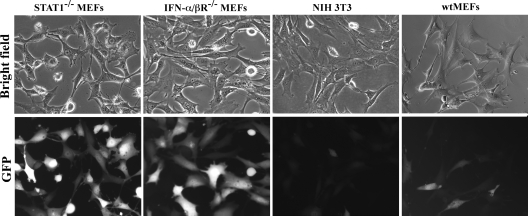
In the NIH 3T3 cells, all of the virus variants and VEEV/GFP demonstrated equal rates of viral RNA replication (Fig. 4 A). However, the distinguishing features of all of the designed mutants were (i) the inefficient inhibition of cellular ribosomal and mRNA transcription (Fig. 4B), (ii) early, high levels of IFN-β release (Fig. 4C), and (iii) the inability to induce profound translational shutoff (Fig. 4D and E). During the first 8 h postinfection, replication of capsid mutants had a negative effect on translation of cellular proteins, but translation of cellular templates did not decrease to the level detected with VEEV/GFP-infected cells (Fig. 4D and E). By 24 h, translation of mutated capsid and other viral structural proteins was barely detectable (Fig. 4D and F). Other experiments demonstrated that after 48 h postinfection, either synthesis of VEEV/C1/GFP-specific structural proteins or downregulation of translation of cellular templates is no longer detectable (Fig. 4G). Thus, the recovery of cellular translation correlated with the decrease in viral replication and translation of viral structural proteins.
FIG. 4.
Analysis of VEEV capsid mutants replication in the NIH 3T3 cells. (A) NIH 3T3 cells were infected with the indicated viruses at an MOI of 20 PFU/cell. Between 3 and 8 h postinfection, virus-specific RNAs were metabolically labeled with [3H]uridine in the presence of ActD as described in Materials and Methods and analyzed by agarose gel electrophoresis followed by autoradiography. (B) NIH 3T3 cells were infected as described above, and between 21 and 24 h postinfection, RNAs were metabolically labeled with [3H]uridine in the absence of ActD. Isolated RNAs were analyzed by gel electrophoresis followed by autoradiography. (C) NIH 3T3 cells were infected as described above. At the indicated time points, media were replaced and concentrations of released IFN-β were determined by ELISA. (D) NIH 3T3 cells were infected at an MOI of 20 PFU/cell. At the indicated time points, they were metabolically labeled with [35S]methionine for 30 min at 37°C, and equal amounts of cell lysates were analyzed by SDS-PAGE followed by autoradiography. The same gel was also analyzed with a phosphorimager to assess synthesis of cellular (E) and viral structural (F) proteins. (G) NIH 3T3 cells were infected with VEEV/C1/GFP at an MOI of 20 PFU/cell. At the indicated time points, they were metabolically labeled with [35S]methionine for 30 min at 37°C, and equal amounts of cell lysates were analyzed by SDS-PAGE followed by autoradiography. All of the presented experiments have been repeated at least twice, and one of the highly reproducible results is presented. Mock, mock-infected cells.
These experiments demonstrated the following. (i) Mutations either in the NLS alone or the NES/NLS-connecting peptide of capsid make viruses noncytopathic in a variety of cell lines. To exclude any possibility of virus reversion to the wt phenotype, in the following experiments, we used the mutant VEEV/C1/GFP, which has the most extensive modifications (six mutations) in the H68 peptide. (ii) VEEV variants with mutated capsid are capable of developing persistent, highly productive infection in the cell lines having defects in IFN signaling. They cause no profound CPE, and the cells remain capable of growth in spite of the continuous release of infectious viruses. (iii) Mouse fibroblasts having no defects in type I IFN signaling efficiently inhibit replication of the VEEV capsid mutants. This was a strong indication that, in the absence of capsid-specific nucleocytoplasmic transport and transcription inhibition (3, 4), the autocrine and paracrine effects of the released IFN-α/β play critical roles in downregulation of VEEV replication.
VEEV encoding mutated capsid protein causes persistent infection in the cells having no defects in type I IFN synthesis and signaling.
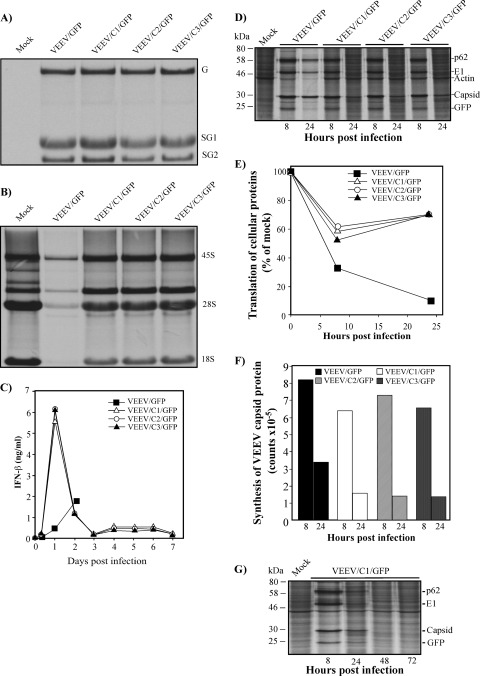
The above-described data suggested that cells competent in IFN-α/β production and signaling are capable of clearing efficiently replicating VEEV capsid mutants without CPE development. However, interactions of such virus mutants with host cells were found to be more sophisticated. In the next round of the experiments, we performed a study of the long-term VEEV/C1/GFP replication in the NIH 3T3 cells and a preliminary analysis of the antiviral state at different times postinfection. The experiments were performed in triplicate, and the results of one of these highly reproducible experiments are shown in Fig. 5. Within 24 h postinfection, all of the cells demonstrated a high level of GFP expression, and titers of the released virus were above 109 PFU/ml (Fig. 5A). At this time, IFN-β (Fig. 5B) was present in the media at concentrations approaching 9 ng/ml (which is equivalent to ∼900 to 1,000 IU/ml), and importantly, no cell death was detected. By day 5 to 6 postinfection, the concentration of IFN-β and titers of the newly released virus fell below the detection level (20 pg/ml [or ∼2 IU/ml] and 50 PFU/ml, respectively) (Fig. 5A and B). GFP fluorescence decreased below a detectable level as well (Fig. 5C), and VEEV nsP2 and capsid were also undetectable by Western blotting (Fig. 5D). Thus, the data suggested that NIH 3T3 cells could clear the infection after 5 days. However, this was not the case, because after day 10 postinfection, we reproducibly detected the second peak of VEEV/C1/GFP replication (Fig. 5A) and release of IFN-β (Fig. 5B), albeit at lower levels. Ultimately, VEEV/C1/GFP and NIH 3T3 cells developed a balanced replication system characterized by (i) the continuous presence of the virus in the media at a concentration of ∼106 PFU/ml (Fig. 5A), (ii) the presence of GFP-positive cells (Fig. 5C), and (iii) the secretion of low levels of IFN-β (Fig. 5B). The persistent replication continued at least until day 30 postinfection, when all of the experiments were finally terminated (data not shown).
FIG. 5.
Analysis of VEEV/C1/GFP replication and IFN-β induction in NIH 3T3 cells. NIH 3T3 cells (2.5 × 106) were infected with the VEEV/C1/GFP variant at an MOI of 20 PFU/cell. At the indicated time points, media were harvested, and virus titers (A) and the concentrations of IFN-β (B) were determined by plaque assay and ELISA, respectively (see Materials and Methods for details). At the same time points, cells were split at a 1:2 ratio. (C) Images of the cells were acquired before cell splitting at different times postinfection (PI) with an inverted Nikon fluorescence microscope. (D) During splitting, one-tenth of cells was harvested, and cell lysates were analyzed by Western blotting using VEEV nsP2 and VEEV capsid-specific antibodies, followed by quantitative analysis using a LICOR imager. (E) At the indicated time points, concentrations of viral genomic and subgenomic RNAs were measured by RT-qPCR as described in Materials and Methods.
These data were confirmed by qPCR using primers specific to the nsP2- and E1-coding sequences (Fig. 5E). At the time, when virus was no longer released at detectable levels, viral genomic RNA was readily detected in the cells at concentrations of 10 to 100 copies per ng of total cellular RNA (which is below 1 copy per cell). At 24 h postinfection, the subgenomic RNA was found at a concentration 3.5-fold higher than that of the genomic RNA, which was in agreement with results of previous studies (23). However, at days 6 to 8 postinfection, it was no longer detectable by the applied qPCR method. At the later times, after VEEV/C1/GFP reactivation, it was once again synthesized (Fig. 5E).
Thus, the NIH 3T3 cells infected with the VEEV capsid mutant were capable of developing a long-term antiviral state and decreasing virus replication to undetectable levels. However, this virus clearance was incomplete, viral genomes were present in the cells, albeit at low concentrations, and RNA replication was ultimately restored to a level sufficient for development of either a persistent and/or chronic infection.
VEEV capsid mutants induce a long-term antiviral state in the infected cells.
The above-presented data suggested that VEEV/C1/GFP-infected NIH 3T3 cells develop an antiviral state, and its establishment correlates with efficient type I IFN release within the first 24 h postinfection. To further understand whether the antiviral state was specific to VEEV, we performed a set of superinfection-based experiments.
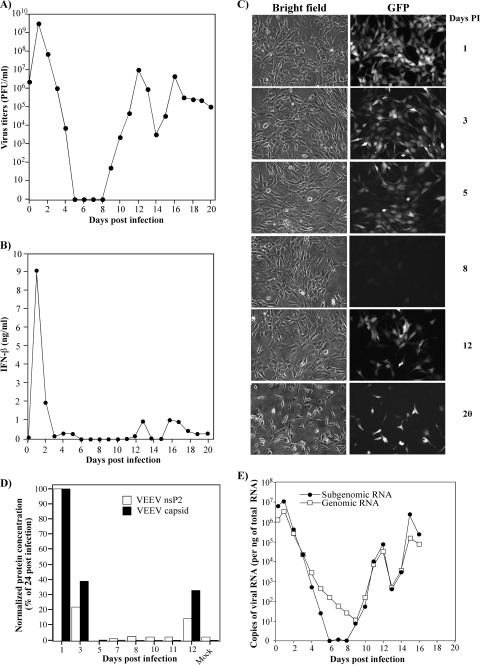
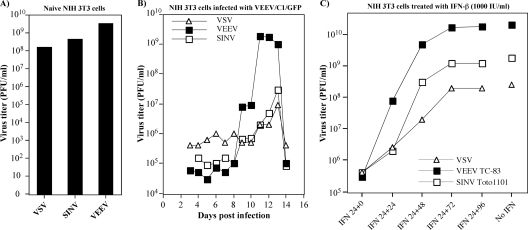
First, we analyzed the ability of the VEEV/C1/GFP-infected NIH 3T3 cells to support replication of other viruses at different times postinfection. The superinfecting viruses included vesicular stomatitis virus (VSV; a nonrelated virus), VEEV TC-83 (a homologous virus) and SINV Toto1101 (a heterologous alphavirus). Naïve NIH 3T3 cells supported a very efficient replication of the indicated viruses alone (Fig. 6A). However, after infection with VEEV/C1/GFP, they developed resistance and were no longer susceptible to VSV, SINV, and VEEV infection for 9 to 10 days (Fig. 6B). These cells became capable of supporting superinfection with the indicated viruses only within a small window of time, between days 10 and 14 postinfection, which correlated with the cells' ability to reinitiate VEEV/C1/GFP replication and release (Fig. 5A).
FIG. 6.
Analysis of replication of superinfecting viruses VEEV TC-83, SINV Toto1101, and VSV in NIH 3T3 cells persistently infected with VEEV/C1/GFP. (A) Titers of the indicated viruses at 48 h postinfection of the naïve NIH 3T3 cells at an MOI of 20 PFU/cell. (B) NIH 3T3 cells were infected with VEEV/C1/GFP in the experiment presented in Fig. 4 and superinfected with the indicated viruses at an MOI of 20 PFU/cell. Medium was added to the cells without removing the inoculum. Titers were measured following a 48-h incubation at 37°C. (C) NIH 3T3 cells were treated with IFN-β at a concentration of 1,000 IU/ml, corresponding to IFN-β concentrations detected in the medium of the NIH 3T3 cells at 24 h postinfection with VEEV/C1/GFP (see Fig. 2 and 4 for details). After 24 h of treatment, media were replaced by those containing no IFN, and at the indicated time points, cells were infected with the viruses at an MOI of 20 PFU/ml. Titers of the released viruses were determined at 24 h postinfection by using a plaque assay on BHK-21 cells.
The simplest explanation for the superinfection exclusion could be the induction of the antiviral state by type I IFN released from the NIH 3T3 cells in response to VEEV/C1/GFP replication. To test this possibility, the NIH 3T3 cells were treated for 24 h with IFN-β at a concentration of 1,000 IU/ml (corresponding to its concentration found in the media at 24 h postinfection with VEEV/C1/GFP) and infected with VEEV TC-83, SINV, and VSV at different times after the treatment was stopped. IFN-β induced only a short-term resistance to infection, and cells became capable of supporting VEEV, VSV, and SINV replication within 48 to 72 h after the media were replaced (Fig. 6C). Thus, the antiviral state that developed in the NIH 3T3 cells as a response to VEEV/C1/GFP replication certainly had an IFN-dependent component, but at the same time, this resistance to infection could not be explained merely by IFN autocrine signaling. The detected long-term interference with the superinfecting viruses suggests that the noncytopathic VEEV/C1/GFP induced an additional antiviral response which prevented their productive replication.
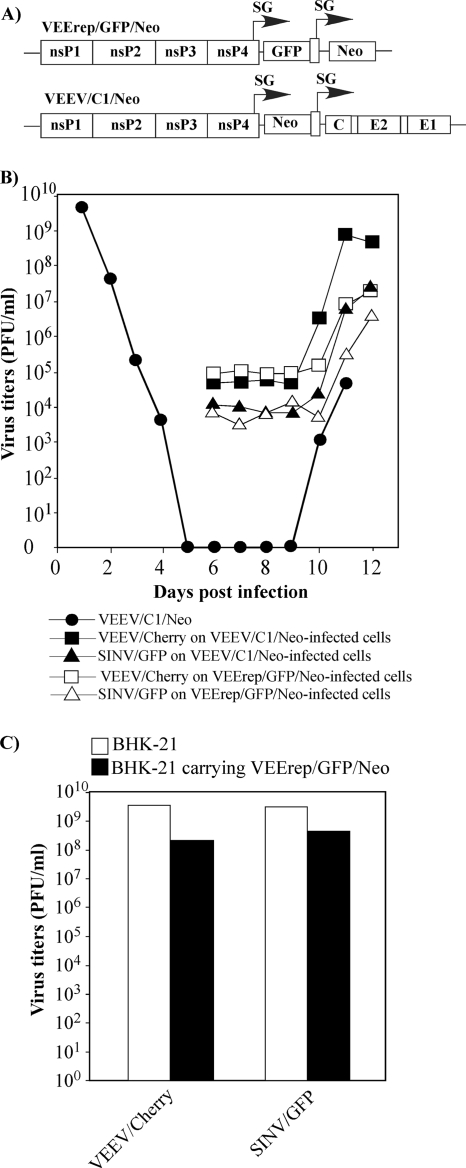
Another possible explanation for the antiviral state could be in the intracellular accumulation of fully processed viral nonstructural proteins, such as nsP2, and/or structural proteins and their subsequent interference with the replication of the superinfecting viruses. However, neither nsP2 nor structural viral proteins were detected in the NIH 3T3 cells by Western blotting using specific antibodies after day 4 postinfection (Fig. 5D). Considering the low protein detection efficiency of Western blotting, the role of structural proteins in the exclusion of superinfection was additionally assessed by infecting NIH 3T3 cells with VEEV/C1/Neo (a double subgenomic virus expressing Neo as a selectable marker) or packaged VEErep/GFP/Neo replicons encoding both GFP and Neo genes under different subgenomic promoters (Fig. 7A). In both cases, the G418 selection was applied at 6 h postinfection to eliminate possible uninfected cells. As shown in Fig. 7B, both cell types were resistant to superinfection with VEEV TC-83 expressing Cherry fluorescent protein from the second subgenomic promoter (VEEV/Cherry) and SINV/GFP (12). This was a strong indication that VEEV structural proteins are not essential for the establishment of superinfection exclusion.
FIG. 7.
Analysis of VEEV, SINV, and VSV replication in the cells carrying VEEV replicons or infected with VEEV capsid mutant. (A) The schematic representation of VEErep/GFP/Neo replicon and VEEV/C1/Neo viral genomes. (B) NIH 3T3 cells were infected with packaged replicons and virus at MOIs of 20 inf.u/cell and 20 PFU/cell, respectively. G418 selection was started at 6 h postinfection, and cells were superinfected with VEEV/Cherry or SINV/GFP at an MOI of 20 PFU/cell. Viruses were harvested after a 48-h incubation at 37°C. Titers were determined by a plaque assay on BHK-21 cells. VEEV/Cherry and SINV/GFP titers corresponding to 105 and 104 PFU/ml, respectively, represent the residual viruses used for infection, as tested in additional experiments (data not shown). (C) BHK-21 cells were infected with the packaged VEErep/Neo/GFP replicon at an MOI of 20 inf.u/cell and, at 48 h after primary infection, superinfected with VEEV/Cherry or SINV/GFP at an MOI of 20 PFU/cell. The same numbers of naïve BHK-21 cells were infected as controls. Viruses were harvested at 48 h postinfection, and titers were determined by plaque assay on BHK-21 cells. The experiments were repeated with the indicated constructs and other viruses four times and produced very similar, reproducible results.
Next, BHK-21 cells, which are defective in type I IFN signaling, were infected with the packaged VEErep/Neo/GFP replicon and, at 48 h after primary infection and later, superinfected with either VEEV/Cherry or SINV/GFP. The results presented in Fig. 7C demonstrate that as early as 48 h postinfection and at later times (data not shown), VEErep/GFP/Neo-infected cells were not resistant to superinfection (although some level of interference was detectable), suggesting that, as we had previously detected in other experiments (30), VEEV nsP2 might block replication of superinfecting homologous and heterologous viruses only at very early times postinfection, if at all.
Thus, the above-described experiments demonstrated the following. (i) The long-term cellular resistance to infection with homologous and heterologous viruses (caused by VEEV capsid mutant replication) is determined by at least two components rather than by type I IFN signaling alone, which induces only a short-term protection. This resistance is a synergistic combination of the autocrine effect of type I IFN release and the intracellular virus replication. (ii) Resistance of the cells to superinfection is not determined by the presence of virus-specific structural (Fig. 7B) and nonstructural (Fig. 7C) proteins, which could interfere with replication of the superinfecting virus. (iii) In the IFN-competent NIH 3T3 cells, the antiviral state is induced by replicons and viruses with equal efficiency.
SINV nsP2 mutants develop persistent infection in NIH 3T3 cells.
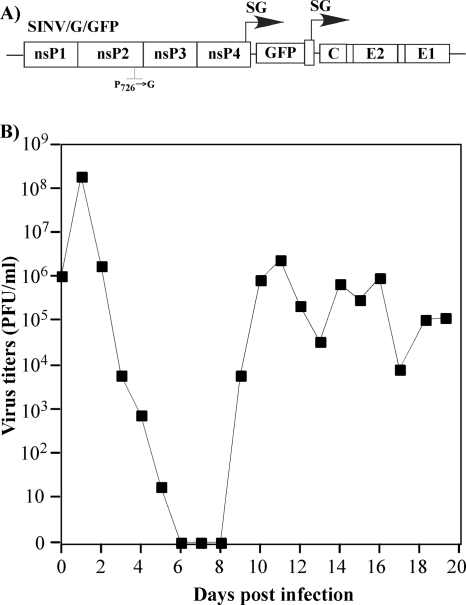
One of the critical questions in this study was whether the phenomenon of persistent/chronic virus replication in vitro is specific to VEEV capsid mutants or if other attenuated, noncytopathic alphaviruses are capable of developing a similar type of infection. To test this possibility, we applied another (Old World) alphavirus, Sindbis virus, encoding mutated nsP2 (12, 17). In the Old World alphaviruses, nsP2 exhibits nuclear functions similar to those of the VEEV capsid in terms of its ability to inhibit transcription of cellular ribosomal and messenger RNAs (15). The SINV/G/GFP variant (Fig. 8A) contains a point mutation in the nsP2 gene, P726→G, that makes this virus dramatically less cytopathic and incapable of downregulating cellular transcription and interfering with the type I IFN response (12). This SINV variant also encodes GFP under the control of the second subgenomic promoter.
FIG. 8.
Analysis of SINV/G/GFP replication in the NIH 3T3 cells. (A) The schematic representation of SINV/G/GFP genome having the previously described (11) P726→G mutation in nsP2. (B) NIH 3T3 cells (2.5 × 106) were infected with the SINV/G/GFP variant at an MOI of 20 PFU/cell. At the indicated time points, media were harvested, and virus titers were determined by plaque assay on BHK-21 cells. At the same time points, cells were trypsinized and split at a 1:2 ratio.
NIH 3T3 cells were infected at the same MOI as was used in the experiments with VEEV capsid mutants (20 inf.u/cell). Within 24 h postinfection, all of the cells became GFP positive, which was indicative of SINV replication, and released high levels of infectious virus (Fig. 8B). The infection then followed the exact same pattern as in the cells infected with VEEV/C1/GFP capsid mutants. We readily detected virus clearance, followed by its presence at an undetectable level and then development of a persistent infection. Thus, another distantly related Old World alphavirus incapable of transcription inhibition resulting from the mutation in nsP2 was almost completely cleared by the infected cells but then developed as a persistent infection.
DISCUSSION
In cells of vertebrate origin, replication of alphaviruses leads to the development of profound, characteristic CPE and complete destruction of the cell monolayer within 24 to 48 h postinfection (37). VEEV- and EEEV-specific capsid proteins play critical roles in CPE development, and point mutations in these proteins or replacement of the active H68 peptide by heterologous sequence make VEEV dramatically less cytopathic and incapable of inhibiting cellular transcription (1, 4, 14, 16). The transcription inhibitory functions strongly correlate with the ability of the capsid and H68 to inhibit nuclear transport (3, 4). To date, we cannot rule out the possibility that downregulation of transcription and nuclear transport are independent capsid functions determined by the same short H68 peptide, but it is more likely that they are connected to each other and that the mutations in H68 affect all of the above-described processes at the same time. To date, we have not identified any single mutant which was unable to interfere only with nuclear traffic or transcription. Importantly, downregulation of the nucleocytoplasmic trafficking by VEEV capsid is rather a result of its binding to the CRM1 and importin-α/β receptors in a stoichiometric mode (3). Therefore, capsid protein inhibitory activities and the function of the capsid in CPE induction appear to depend on the levels of virus replication, which in turn determine the concentration of this structural protein in the infected cells. In cells less permissive to virus replication, low concentrations of capsid (or the Old World alphavirus nsP2) would likely induce a less efficient CPE or no CPE at all (22, 33, 34). However, it is very difficult to study the effects of the less efficient VEEV capsid expression on virus-host interactions in vitro, because the cells used in common practice are highly permissive to VEEV replication and rapidly develop CPE. A theoretically plausible approach would be to develop and apply inefficiently replicating VEEV mutants having, for instance, modified RNA promoter elements. However, such modified viruses rapidly accumulate adaptive mutations in either promoter and/or ns polyproteins and readily evolve to the more efficiently replicating, cytopathic phenotype (23). In this study, we found a way around this problem by designing VEEV mutants having nuclear functions of capsid selectively inactivated by point mutations, without affecting the ability of the protein to package VEEV genomes and form infectious virions. Replication of such mutants in the commonly used cell lines mimics replication of VEEV in the context of low wt capsid protein production. Normally, the high replication efficiency, but not the ability to cause CPE, is a selective system for virus evolution in vitro. Supporting this evolutionary aspect, the capsid mutants demonstrating efficient replication remain noncytopathic during serial passaging. Thus, these new mutants represent an important new model for studying the numerous processes in virus-host cell interactions that are classically difficult to investigate during highly cytopathic replication of the wt VEEV.
In this study, we introduced combined point mutations into the previously identified VEEV capsid-specific NLS and the connecting peptide between NES and NLS. At early times postinfection, in different cells lines, all of these mutants demonstrated replication rates identical to those of VEEV encoding the wt capsid protein. However, in contrast to the latter virus, they did not induce CPE. In cells having defects in type I IFN signaling, such as BHK-21 cells, IFN-α/βR−/− MEFs, or STAT1−/− MEFs, they continued productive replication, characterized by efficient virus release. In NIH 3T3 cells and wt MEFs, which have no defects in type I IFN signaling, virus replication was strongly downregulated within a few days postinfection due to the inability of these viruses to inhibit cellular transcription and activation of IFN-β and IFN-inducible genes. It has been previously described that VEEV replicons can interfere with tyrosine phosphorylation and nuclear translocation of the transcription factor STAT1 (35); however, in our experiments, these effects were likely insufficient to block autocrine effects of the released IFN-β. This certainly does not exclude the possibility that these previously described effects play a role in the downregulation of type I IFN signaling, but they do not completely prevent activation of the antiviral state in cells with a replicating VEEV genome that encodes a mutated capsid protein. As a result, the infected cells (in our study, typically the NIH 3T3 cells) no longer support productive replication of the intracellular virus and cease being permissive to replication of superinfecting homologous and heterologous viruses for at least 10 days after primary infection. Importantly, this resistance cannot be explained merely by the autocrine effects of type I IFN. Treating naïve NIH 3T3 cells with a high concentration of IFN-β induces only a short-term resistance to viral infections, one that lasts 2 to 3 days. Thus, activation of pattern recognition receptors (PRRs), such as RIG-I, MDA5, protein kinase PKR, and possibly others, appears to have important synergistic effects. The molecular mechanisms underlying this resistance are currently under intensive investigation.
Induction of the antiviral state was found to depend on the replication of VEEV-specific RNAs and/or synthesis of viral nonstructural proteins. Replicons, encoding no structural proteins, induce type I IFN and make cells resistant to superinfection with VEEV, SINV, and VSV. However, in the case of replicons, the magnitude of the type I IFN response is lower than that detected after infection of the cells by viral envelope glycoprotein-encoding constructs (data not shown). Most likely, in the case of VEEV infection, the endoplasmic reticulum (ER) stress (19) is a critical enhancer of IFN-α/β induction and plays a critical role in the development of a VEEV-specific antiviral reaction (data not shown).
One of the most important phenomena found in this study was the ability of VEEV capsid mutants to develop a persistent infection in cultured cells. The initial, efficient (acute) replication was followed by a decrease of virus production to almost undetectable levels. The following reactivation of its replication led to the development of a balanced virus-host cell replication system characterized by a low-level release of IFN-β in the media in the presence of the virus, albeit in titers lower than those detected during the initial infection. Thus, cells developed a moderate response, one sufficient to reduce virus replication to a low level but not to completely eliminate it.
These results are in agreement with those of previous studies of alphavirus replication in vivo. Ross River virus was found to persistently replicate in infected humans (36), murine macrophages (39), and chikungunya virus-specific IgM antibodies, which might be indicative of the ongoing virus replication, were detected in patients for as long as 1.5 years postinfection (5). Persistent replication of SINV has been detected using a murine model, where viral RNA was readily detected by PCR in brain tissues months after the virus was no longer detected by other, less sensitive methods (25, 26). Persistent SINV and SFV replication was even more evident in mice with severe deficiencies in the adaptive immune response, which demonstrated continuous viremia for weeks postinfection (2, 8, 21). VEEV is not an exception, and persistent replication of this virus was detected in the brains of T cell knockout mice up to 1 month postinfection without development of lethal disease (27).
Our in vitro model, VEEV viruses with mutations in the H68 capsid-specific peptide, was aimed at mimicking infection in cells producing low levels of VEEV capsid, which are insufficient to inhibit cellular transcription. The possibility of the existence of such cells and tissues, in which VEEV capsid incompletely inhibits cellular transcription, is strongly supported by the accumulated, above-described, in vivo experimental data. Numerous studies have demonstrated that in spite of the capsid's profound ability to cause transcriptional shutoff and type I IFN induction, animals do respond to VEEV replication (as well as to replication of other viruses) by the induction of a high level of IFN-α/β (9, 43). This is a strong indication that in many of the infected cells, inhibition of transcription is far from being complete, and cells do respond to virus replication by activating a virus-induced cell response.
Thus, the VEEV capsid mutants demonstrate an ability to persistently replicate not only in mosquito cells but also in cells of vertebrate origin. The mode of their replication suggests that persistent infection with wt alphaviruses is possible as long as it does not result in CPE development. Moreover, sequencing of the genomes of a few plaque-purified viruses isolated after only 1 week of persistent replication detected numerous mutations in the encoded proteins (data not shown), suggesting that such persistence might be an important system for viral evolution.
In summary, our study demonstrated that the previously identified amino-terminal H68 peptide in the VEEV capsid plays a critical role in virus-host cell interactions and determines the mode of virus replication. Point mutations in this peptide have deleterious effects on the ability of VEEV to interfere with cellular transcription, the development of virus-induced stress response, and the ability of VEEV to induce CPE without detectably affecting virus replication rates. Such viruses readily develop a persistent infection both in cells with defects in type I IFN signaling and those capable of type I IFN induction and signaling. These mutants represent an important model for studying virus-host interaction during VEEV replication.
Acknowledgments
This work was supported by Public Health Service grants AI070207 (I.F. and S.A.), R01AI050537 (A.L.), and R01AI073301 (E.F.).
Footnotes
Published ahead of print on 28 July 2010.
REFERENCES
- 1.Aguilar, P. V., S. C. Weaver, and C. F. Basler. 2007. Capsid protein of eastern equine encephalitis virus inhibits host cell gene expression. J. Virol. 81:3866-3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amor, S., M. F. Scallan, M. M. Morris, H. Dyson, and J. K. Fazakerley. 1996. Role of immune responses in protection and pathogenesis during Semliki Forest virus encephalitis. J. Gen. Virol. 77:281-291. [DOI] [PubMed] [Google Scholar]
- 3.Atasheva, S., A. Fish, M. Fornerod, and E. I. Frolova. 2010. Venezuelan equine encephalitis virus capsid protein forms a tetrameric complex with CRM1 and importin α/β that obstructs nuclear pore complex function. J. Virol. 84:4158-4171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atasheva, S., N. Garmashova, I. Frolov, and E. Frolova. 2008. Venezuelan equine encephalitis virus capsid protein inhibits nuclear import in mammalian but not in mosquito cells. J. Virol. 82:4028-4041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Borgherini, G., P. Poubeau, A. Jossaume, A. Gouix, L. Cotte, A. Michault, C. Arvin-Berod, and F. Paganin. 2008. Persistent arthralgia associated with chikungunya virus: a study of 88 adult patients on Reunion Island. Clin. Infect. Dis. 47:469-475. [DOI] [PubMed] [Google Scholar]
- 6.Breakwell, L., P. Dosenovic, G. B. Karlsson Hedestam, M. D'Amato, P. Liljestrom, J. Fazakerley, and G. M. McInerney. 2007. Semliki Forest virus nonstructural protein 2 is involved in suppression of the type I interferon response. J. Virol. 81:8677-8684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bredenbeek, P. J., I. Frolov, C. M. Rice, and S. Schlesinger. 1993. Sindbis virus expression vectors: packaging of RNA replicons by using defective helper RNAs. J. Virol. 67:6439-6446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burdeinick-Kerr, R., J. Wind, and D. E. Griffin. 2007. Synergistic roles of antibody and interferon in noncytolytic clearance of Sindbis virus from different regions of the central nervous system. J. Virol. 81:5628-5636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Charles, P. C., J. Trgovcich, N. L. Davis, and R. E. Johnston. 2001. Immunopathogenesis and immune modulation of Venezuelan equine encephalitis virus-induced disease in the mouse. Virology 284:190-202. [DOI] [PubMed] [Google Scholar]
- 10.Fazakerley, J. K., A. Boyd, M. L. Mikkola, and L. Kaariainen. 2002. A single amino acid change in the nuclear localization sequence of the nsP2 protein affects the neurovirulence of Semliki Forest virus. J. Virol. 76:392-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frolov, I., E. Agapov, T. A. Hoffman Jr., B. M. Prágai, M. Lippa, S. Schlesinger, and C. M. Rice. 1999. Selection of RNA replicons capable of persistent noncytopathic replication in mammalian cells. J. Virol. 73:3854-3865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frolova, E. I., R. Z. Fayzulin, S. H. Cook, D. E. Griffin, C. M. Rice, and I. Frolov. 2002. Roles of nonstructural protein nsP2 and alpha/beta interferons in determining the outcome of Sindbis virus infection. J. Virol. 76:11254-11264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gardner, C. L., C. W. Burke, M. Z. Tesfay, P. J. Glass, W. B. Klimstra, and K. D. Ryman. 2008. Eastern and Venezuelan equine encephalitis viruses differ in their ability to infect dendritic cells and macrophages: impact of altered cell tropism on pathogenesis. J. Virol. 82:10634-10646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garmashova, N., S. Atasheva, W. Kang, S. C. Weaver, E. Frolova, and I. Frolov. 2007. Analysis of Venezuelan equine encephalitis virus capsid protein function in the inhibition of cellular transcription. J. Virol. 81:13552-13565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garmashova, N., R. Gorchakov, E. Frolova, and I. Frolov. 2006. Sindbis virus nonstructural protein nsP2 is cytotoxic and inhibits cellular transcription. J. Virol. 80:5686-5696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garmashova, N., R. Gorchakov, E. Volkova, S. Paessler, E. Frolova, and I. Frolov. 2007. The Old World and New World alphaviruses use different virus-specific proteins for induction of transcriptional shutoff. J. Virol. 81:2472-2484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gorchakov, R., E. Frolova, and I. Frolov. 2005. Inhibition of transcription and translation in Sindbis virus-infected cells. J. Virol. 79:9397-9409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gorchakov, R., E. Frolova, S. Sawicki, S. Atasheva, D. Sawicki, and I. Frolov. 2008. A new role for ns polyprotein cleavage in Sindbis virus replication. J. Virol. 82:6218-6231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.He, B. 2006. Viruses, endoplasmic reticulum stress, and interferon responses. Cell Death Differ. 13:393-403. [DOI] [PubMed] [Google Scholar]
- 20.Johnston, R. E., and C. J. Peters. 1996. Alphaviruses, p. 843-898. In B. N. Fields, D. M. Knipe, and P. M. Howley (ed.), Fields virology, 3rd ed. Lippincott-Raven, New York, NY.
- 21.Kimura, T., and D. E. Griffin. 2003. Extensive immune-mediated hippocampal damage in mice surviving infection with neuroadapted Sindbis virus. Virology 311:28-39. [DOI] [PubMed] [Google Scholar]
- 22.Klimstra, W. B., and K. D. Ryman. 2009. Togaviruses, p. 353-372. In A. R. Brasier, A. García-Sastre, and S. M. Lemon (ed.). Cellular signaling and innate immune responses to RNA virus infections. ASM Press, Washington, DC.
- 23.Kulasegaran-Shylini, R., V. Thiviyanathan, D. G. Gorenstein, and I. Frolov. 2009. The 5′UTR-specific mutation in VEEV TC-83 genome has a strong effect on RNA replication and subgenomic RNA synthesis, but not on translation of the encoded proteins. Virology 387:211-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lemm, J. A., R. K. Durbin, V. Stollar, and C. M. Rice. 1990. Mutations which alter the level or structure of nsP4 can affect the efficiency of Sindbis virus replication in a host-dependent manner. J. Virol. 64:3001-3011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levine, B., and D. E. Griffin. 1992. Persistence of viral RNA in mouse brains after recovery from acute alphavirus encephalitis. J. Virol. 66:6429-6435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levine, B., J. M. Hardwick, and D. E. Griffin. 1994. Persistence of alphaviruses in vertebrate hosts. Trends Microbiol. 2:25-28. [DOI] [PubMed] [Google Scholar]
- 27.Paessler, S., N. E. Yun, B. M. Judy, N. Dziuba, M. A. Zacks, A. H. Grund, I. Frolov, G. A. Campbell, S. C. Weaver, and D. M. Estes. 2007. Alpha-beta T cells provide protection against lethal encephalitis in the murine model of VEEV infection. Virology 367:307-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perera, R., C. Navaratnarajah, and R. J. Kuhn. 2003. A heterologous coiled coil can substitute for helix I of the Sindbis virus capsid protein. J. Virol. 77:8345-8353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perera, R., K. E. Owen, T. L. Tellinghuisen, A. E. Gorbalenya, and R. J. Kuhn. 2001. Alphavirus nucleocapsid protein contains a putative coiled coil alpha-helix important for core assembly. J. Virol. 75:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Petrakova, O., E. Volkova, R. Gorchakov, S. Paessler, R. M. Kinney, and I. Frolov. 2005. Noncytopathic replication of Venezuelan equine encephalitis virus and eastern equine encephalitis virus replicons in Mammalian cells. J. Virol. 79:7597-7608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rice, C. M., R. Levis, J. H. Strauss, and H. V. Huang. 1987. Production of infectious RNA transcripts from Sindbis virus cDNA clones: mapping of lethal mutations, rescue of a temperature-sensitive marker, and in vitro mutagenesis to generate defined mutants. J. Virol. 61:3809-3819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ryman, K. D., and W. B. Klimstra. 2008. Host responses to alphavirus infection. Immunol. Rev. 225:27-45. [DOI] [PubMed] [Google Scholar]
- 33.Ryman, K. D., K. C. Meier, E. M. Nangle, S. L. Ragsdale, N. L. Korneeva, R. E. Rhoads, M. R. MacDonald, and W. B. Klimstra. 2005. Sindbis virus translation is inhibited by a PKR/RNase L-independent effector induced by alpha/beta interferon priming of dendritic cells. J. Virol. 79:1487-1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ryman, K. D., L. J. White, R. E. Johnston, and W. B. Klimstra. 2002. Effects of PKR/RNase L-dependent and alternative antiviral pathways on alphavirus replication and pathogenesis. Viral Immunol. 15:53-76. [DOI] [PubMed] [Google Scholar]
- 35.Simmons, J. D., L. J. White, T. E. Morrison, S. A. Montgomery, A. C. Whitmore, R. E. Johnston, and M. T. Heise. 2009. Venezuelan equine encephalitis virus disrupts STAT1 signaling by distinct mechanisms independent of host shutoff. J. Virol. 83:10571-10581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Soden, M., H. Vasudevan, B. Roberts, R. Coelen, G. Hamlin, S. Vasudevan, and J. La Brooy. 2000. Detection of viral ribonucleic acid and histologic analysis of inflamed synovium in Ross River virus infection. Arthritis Rheum. 43:365-369. [DOI] [PubMed] [Google Scholar]
- 37.Strauss, J. H., and E. G. Strauss. 1994. The alphaviruses: gene expression, replication, evolution. Microbiol. Rev. 58:491-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Volkova, E., R. Gorchakov, and I. Frolov. 2006. The efficient packaging of Venezuelan equine encephalitis virus-specific RNAs into viral particles is determined by nsP1-3 synthesis. Virology 344:315-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Way, S. J., B. A. Lidbury, and J. L. Banyer. 2002. Persistent Ross River virus infection of murine macrophages: an in vitro model for the study of viral relapse and immune modulation during long-term infection. Virology 301:281-292. [DOI] [PubMed] [Google Scholar]
- 40.Weaver, S. C., C. Ferro, R. Barrera, J. Boshell, and J. C. Navarro. 2004. Venezuelan equine encephalitis. Annu. Rev. Entomol. 49:141-174. [DOI] [PubMed] [Google Scholar]
- 41.Weaver, S. C., and I. Frolov. 2005. Togaviruses, p. 1010-1024. In B. W. J. Mahy and V. ter Meulen (ed.), Virology, vol. 2. IRL Press, Salisbury, United Kingdom. [Google Scholar]
- 42.Weaver, S. C., R. Salas, R. Rico-Hesse, G. V. Ludwig, M. S. Oberste, J. Boshell, and R. B. Tesh. 1996. Re-emergence of epidemic Venezuelan equine encephalomyelitis in South America. Lancet 348:436-440. [DOI] [PubMed] [Google Scholar]
- 43.White, L. J., J. G. Wang, N. L. Davis, and R. E. Johnston. 2001. Role of alpha/beta interferon in Venezuelan equine encephalitis virus pathogenesis: effect of an attenuating mutation in the 5′ untranslated region. J. Virol. 75:3706-3718. [DOI] [PMC free article] [PubMed] [Google Scholar]