Abstract
Background
Childhood mortality in Ghana has generally declined in the last four decades. However, estimates tend to conceal substantial variability among regions and districts. The lack of population-based data in Ghana, as in other less developed countries, has hindered the development of effective programmes targeted specifically at clusters where mortality levels are significantly higher.
Objective
This paper seeks to test for the existence of statistically significant clusters of childhood mortality within the Kintampo Health and Demographic Surveillance System (KHDSS) between 2005 and 2007.
Design
In this study, mortality rates were generated using mortality data extracted from the health and demographic surveillance database of the KHDSS and exported into STATA. The spatial and spatio-temporal scan statistic by Kulldorff was used to identify significant clusters of childhood mortality within the KHDSS.
Results
A significant cluster of villages with high under-five mortality in the south-eastern part of the KHDSS in 2006 was identified. This is a remote location where poverty levels are relatively higher, health facilities are more sparse and these are compounded by poor transport services in case of emergencies.
Conclusion
This study highlights the potential of the surveillance platform to demonstrate the spatial dimensions of childhood mortality clustering. It is apparent, though, that further studies need to be carried out in order to explore the underlying risk factors for potential mortality clusters that could emerge later.
Keywords: childhood mortality, clustering, surveillance, Kintampo, spatial analysis, spatio-temporal analysis
In less developed countries (LDCs), especially sub-Sahara Africa (SSA), infant and childhood mortality remains high (1). About 10.6 million children under the age of five years are dying each year, with the vast majority of deaths preventable by low-cost public health interventions (2). One estimate suggests that ‘roughly 40% of childhood deaths occur in the neonatal period (the first 4 weeks of life), with this proportion being considerably lower for regions with high absolute rates such as sub-Saharan Africa (SSA)’ (1). Furthermore, only six causes account for three-quarters of childhood deaths globally: pneumonia (19%), diarrhoea (18%), malaria (8%), neonatal pneumonia or sepsis (10%), preterm delivery (10%) and asphyxia at birth (8%). Malnutrition is a risk factor suspected to be an additional underlying cause in about half of all cases of childhood deaths (3).
Ghana, like other LDCs, is working towards reducing under-five mortality by two-thirds between 1990 and 2015, which is a key Millennium Development Goal. Over the last four decades, the level of child mortality in Ghana has declined substantially, from about 200 deaths per 1,000 live births in the early 1970s, to under 120 deaths per 1,000 live births in 2003. These summary figures tend to conceal a great degree of variability among the districts of the region and the various regions. For instance, the 2003 Ghana Demographic and Health Survey (GDHS) estimated the level of childhood mortality for the Greater Accra Region at around 75 deaths per 1,000 live births while that for the Upper-West Region is close to three times this figure (208 deaths per 1,000 live births). These differentials are even wider among districts within the same region. While ideally direct estimates are more reliable than indirect estimates, the available data do not allow the use of direct estimation. In general, the level of mortality is relatively high throughout the Northern Region and Upper-West Regions, compared with the national estimate.
The lack of population-based data in many LDCs hinders the development of effective programmes. Unfortunately, many countries in the SSA have an inadequate or no system for registering vital information. For example, of the 57 countries that make up the World Health Organisation's African and Southeast Asian Regions, only eight have usable vital events data, and only one has complete coverage of death. It is believed that, within the poor countries of the globe, there are one billion people whose births and deaths are never registered – no official or government agency ever acknowledges that these people exist. Administratively, the KHDSS is located in the Brong Ahafo Region (BAR), one of 10 regions in Ghana. Childhood mortality for the BAR for the 10-year period preceding 2003 was estimated at 91 deaths per 1,000 live births (4).
In Ghana, three research centres were set up in the major ecological zones (coastal, forest, savannah-sahelian) of the country in the early 1990s as part of the Ghana Health Service Research and Development division in the Ministry of Health. These centres provide a basis for field epidemiological and other health research interventions and also provide reliable health measurements to inform policy and programme direction. The Kintampo Health Research Centre (KHRC), which runs the Kintampo Health and Demographic Surveillance System (KHDSS), is situated in the forest-savannah transitional ecological zone (Central Ghana). KHRC has developed a Health and Demographic Surveillance System (HDSS) that provide core updates on on pregnancies, births, deaths and migrations (in and out) every 6 months.
The development and evaluation of effective programmes to reduce the burden of disease requires a detailed knowledge of disease or mortality distribution and causal pathway. This knowledge could be derived from analytical epidemiological studies that use as a platform, large-scale health surveys and the above-described demographic surveillance systems (DSS) in which causal relationships between risk factors and diseases or mortality are investigated. It has been recommended that where general population-wide intervention programmes are too expensive to implement, it is necessary to focus these programmes on ‘high-risk units where certain adverse health effects are more likely to occur’ (5).
Consequently, this paper, seeks to investigate whether there are clusters where under-five mortality seem to converge. As mentioned earlier, the availability of routine surveillance data makes this a worthwhile exercise. In such a case, there is need to identify the determinants of such clustering, to enable local health personnel to identify them and to develop specific strategies targeted at these clusters, of which this paper is an important first step.
Population and methods
Study population
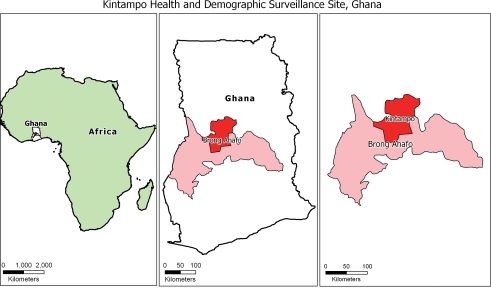
The KHDSS area covers the whole of Kintampo North Municipality and Kintampo South district in the BAR of Ghana. The BAR is one of the 10 regions of Ghana. Kintampo North Municipality and Kintampo South district lie in the forest-savannah transitional zones between the wet semi-equatorial and tropical continental climates. The KHDSS area is further divided into 12 sub-districts consisting of Busuama, Dawadawa, Gulumpe, Kadelso, Kintampo, Kunsu and New Longoro in the Kintampo North Municipality, while Kintampo South district is made up of Amoma, Anyima, Apesika, Jema and Mansie sub-districts. Fig. 1 shows the geographical location of the KHDSS in the BAR of Ghana.
Fig. 1.
Location of Kintampo Health and Demographic Surveillance site, Ghana.
In 2007, the KHDSS recorded a mid-year resident population of 126,315 people living in 129 villages. An additional 27 villages, which were previously not covered by the KHDSS because of their inaccessibility, were included in 2008 when the road network was improved and became motorable throughout the year. The major indigenous ethnic groups are the Bonos and the Mos. There is, however, a large immigrant population from the three Northern Regions (Dagarba, Dagomba and Konkomba), who are generally farmers. In 2007, there was a young population structure with 42.8% below 15 years of age and only 4% over 59 years of age. The dependency ratio in the KHDSS as at the end of 2007 was 88.2 dependents to every 100 persons aged 15–59.
The main economic activities within the districts are agriculture and small-scale merchandising. The average household size in 2007 was 5.3, with rural and urban villages having a household size of 5.6 and 4.7, respectively. Only 25.8% of the total population have access to electricity. Provision of potable water is about 58.7%; however, 76.8% of the urban population and only 48.4% of the rural population have access to potable water. This is significantly lower compared to the national average of 71%. The educational attainment of household heads by 2006 showed that 54.7% had no formal education, 30.4% had primary or middle/junior secondary school and 5.1% had secondary education with just 1% completing university.
Data
Deaths of all registered and eligible individuals are recorded, regardless of whether the individual died at home or at a health facility. Under-reporting of deaths is typically less of a problem than that of births, because a death is widely known and remembered. Exceptions are the deaths of very young (and yet unregistered) infants, particularly perinatal and neonatal deaths. The KHDSS collects more detailed information about deaths to establish the cause of death through verbal autopsies. The data is updated twice a year for each household as well as new households that have emerged since the last visit; the first update starts from January to June and the second update from July to December each year. A 3- or 4-month cycle is widely considered an appropriate interval to ensure comprehensive recording of births, deaths and migrations, which is the minimum requirement for maintaining the coherence of any DSS (6). The six-monthly update cycle of the KHDSS could, to some extent, result in under-enumeration of neonatal deaths, as has been reported in the DSS of two sites in Kenya with two update rounds in a year, similar to the KHDSS in Kintampo, which could not identify neonatal deaths, thereby resulting in sensitivities of 62 and 49% (7).
In this study, mortality rates were generated using mortality data extracted from the health and demographic surveillance database of the KHDSS and exported into STATA. Although the KHDSS started its operations in 2003, data from 2005 to 2007 are used in this study because the updates cycle began in 2005. Table 1 shows the recorded deaths and the population of children aged less than 5 years in the KHDSS from 2005 to 2007.
Table 1.
Total deaths, population and mortality rates among KHDSS residents under five years, 2005–2007
| Year | Deaths | Population | Childhood mortality rate (per 1,000 person-years, 95% CI) |
|---|---|---|---|
| 2005 | 208 | 14,936 | 13.93 (12.07, 16.01) |
| 2006 | 218 | 16,078 | 13.56 (11.76, 15.35) |
| 2007 | 240 | 16,774 | 14.31 (12.50, 16.12) |
| Total (2005–2007) | 666 | 47,788 | 13.93 (12.87, 14.99) |
Methods of analysis
This study defines a cluster as a geographical area with a greater than expected number of child deaths within a period of time. A spatial scan statistic (8) is used to isolate any significant clusters of childhood mortality within the KHDSS area. This statistic checks if the observed excess is significant by year. SaTScan™ locates a cluster at any geographic position, up to a maximum size, and minimises the problem of multiple statistical tests. Since the study replicates a previous one in rural Burkina Faso, the settings for SaTScan™ were the same, searching only for villages with high childhood mortality rates (9). In spatial and spatio-temporal analyses, SaTScan™ identifies secondary clusters that are identical to the most likely cluster with almost as high likelihood value. There was no geographic overlap, so secondary clusters would not overlap the most likely cluster. The maximum cluster size was set to 50% of the total population at risk, to scan for small to large clusters. Again, the number of Monte Carlo replications was set to 999 for sufficient statistical power, and clusters with a statistical significance of p<0.05 were reported. Finally, a spatio-temporal scan was done to check deaths in the cluster areas to see if the excess persisted through time or not.
Results
Table 2 shows the population for 2007 and mortality rates (per 1,000 person-years) for the 129 villages in 12 sub-districts from 2005 to 2007.
Table 2.
Under-five population and childhood mortality rates by KHDSS sub-districts and year, 2005–2007
| Sub-district | Population (2007) | Mortality ratesa | ||
|---|---|---|---|---|
| 2005 | 2006 | 2007 | ||
| Busuama | 608.5 | 11.9 | 1.6 | 6.6 |
| Dawadawa | 854.8 | 20.2 | 10.2 | 5.8 |
| Gulumpe | 1432.5 | 17.7 | 14.9 | 23.0 |
| Kadelso | 662.6 | 16.9 | 21.6 | 21.1 |
| Kunsu | 487.7 | 14.3 | 10.4 | 4.1 |
| New Longoro | 389.0 | 5.8 | 8.2 | 10.3 |
| Kintampo | 4,679.3 | 12.9 | 12.4 | 10.9 |
| Amoma | 1,754.4 | 18.0 | 15.9 | 17.7 |
| Apesika | 1,190.6 | 5.1 | 17.0 | 23.5 |
| Jema | 2,854.9 | 12.1 | 15.5 | 15.4 |
| Mansie | 769.4 | 12.6 | 11.5 | 13.0 |
| Anyima | 1,090.0 | 18.6 | 14.8 | 12.8 |
| Total | 1,6773.7 | 13.9 | 13.7 | 14.3 |
aMortality rates are computed based on the populations for the respective years (2005–2007).
Space and spatio-temporal scan statistic results of under-five mortality
The results of the purely spatial analysis scanning for high rates using the Poisson model for 2005 to 2007 are shown in Table 3.
Table 3.
The most likely clusters of childhood mortality in the KHDSS using purely spatial analysis scanning for high rates
| Year | Type | Cluster villages (n)a | Radius (km) | Cases | Expected | Relative risk | p-Value |
|---|---|---|---|---|---|---|---|
| 2005 | Most likely | 33 | 36.69 | 80 | 58.88 | 1.583 | 0.25 |
| 2006 | Most likely | 20 | 6.98 | 25 | 10.25 | 2.624 | 0.016 |
| 2007 | Most likely | 7 | 16.17 | 45 | 26.92 | 1.827 | 0.133 |
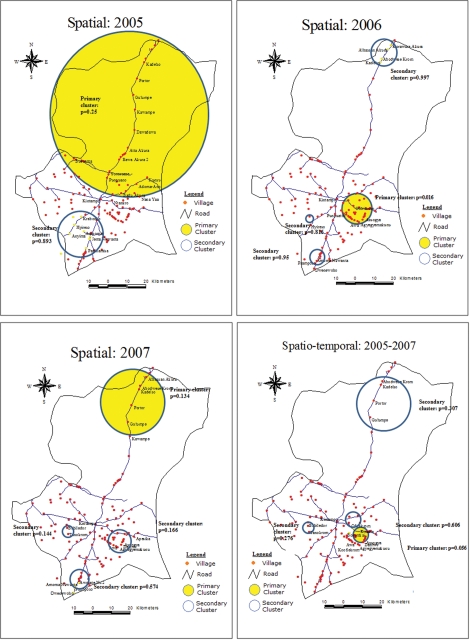
aSee Fig. 2 for the location of the clusters.
Fig. 2.
Map of Kintampo Health and Demographic Surveillance System showing spatial and spatio-temporal clusters of high childhood mortality, 2005–2007.
For 2005 and 2007, no statistically significant cluster was observed. In 2005, the most likely cluster of 33 villages was identified, covering much of the north of the KHDSS, and within a radius of close to 37 km. Villages such as Alhassan Akura, Abodwesekrom, Gulumpe, Kadelso and Portor, which were among the most likely cluster for 2005, were again found in the most likely cluster for 2007, and as both a secondary spatial and a secondary spatio-temporal cluster in 2006. Although these clusters were not statistically significant, they suggest an underlying potential for mortality clustering in the north. The villages in this part of the KHDSS are geographically scattered, on average about 6 km apart. Compared to the villages in the south of the KHDSS, there are fewer health facilities, more arid climatic conditions and, therefore, greater difficulty with water access.
The spatial scan for 2006 indicated a statistically significant cluster of 20 villages in the south-eastern part of the KHDSS, within a radius of about 7 km. Secondary clusters identified include the single village cluster of Hyireso, where six under-five deaths were observed, and another to the south, which has the villages of Amoma Nkwanta, Pramposo and Dwenewoho, within a radius of 6 km. This cluster in the south persisted in 2007 as a secondary cluster, though statistically insignificant. In 2007, there was another secondary cluster identified in the south-west, consisting of the villages of Tanokrom and Babiledor, which was also statistically insignificant. The scan results of the spatio-temporal analysis for the period 2005–2007 are shown in Table 4.
Table 4.
The most likely clusters of childhood mortality in the KHDSS using spatial-time analysis scanning for high rates
| Type | Cluster villages (n)a | Time frame | Radius (km) | Cases | Expected | Relative risk | Log likelihood ratio | p-value |
|---|---|---|---|---|---|---|---|---|
| Most likely | 5 | 2006 | 3.51 | 12 | 3.01 | 4.042 | 7.668 | 0.056 |
aSee Fig. 2 for the location of the cluster.
The most likely spatio-temporal cluster was identified within 2006, covering a radius of about 4 km. The cluster was marginally significant, with 12 cases observed as against 3.01 expected. Villages such as Agyegyemakunu, Koofiekrom, Dantwi, Awa and Asuogya, which were located within the cluster, were found to be significant in the purely spatial scan for 2006.
Discussion
On average, the under-five mortality rate for children for the period was 13.93 per 1,000 person-years. This estimate, when transformed to a 5-year cumulative rate by the formula: 1–exp(−0.01393*5), gives a rate of 67 per 1,000 person-years. Compared to the national average of 111 per 1,000 live births (as recorded on the GDHS and 142 per 1,000 live births for the BAR recorded in the Ghana Multiple Indicator Cluster Survey 2006 (10)), the rate within the KHDSS was lower. However, this may be due to some level of under-enumeration, which often arises as a difficulty in data collection in many parts of rural Africa.
Under-enumeration of neonatal deaths is not uncommon in demographic surveillance sites; this may be due to factors such as the periodicity of the update cycles and other constraints. For instance, there is evidence to support the assertion that it is not possible to achieve a record of all deaths because of conditions under which data are collected in rural areas, such as under-reporting of these deaths by respondents (7, 9). These conditions could apply to the KHDSS as well. This paper recognises the potential effects that the clinical and interventions studies that are ongoing in the KHDSS area could have on childhood mortality rates determined as compared to similar but non-HDSS districts in Ghana. With the KHRC's history of carrying out clinical trials, morbidity levels of trial recruits for any study are closely monitored and prompt/appropriate treatment given as a matter of policy. Hospital services are facilitated for the study population on a continuous basis, in collaboration with the government services. Malaria episodes are treated as recommended by the Ministry of Health of Ghana. Home visitations are frequent as children or other groups of interest are monitored (11–13). These activities could potentially avert childhood deaths in the KHDSS, which may have occurred elsewhere.
This study sought to analyse the spatial and spatio-temporal pattern of childhood mortality, using KHDSS data. The rates are reported at sub-district level because the number of deaths per village are small. Again, it is not possible to explore household factors related to the observed clustering (despite its obvious utility) because geographic information system data are only available for the centroids of the villages and at compound levels in the large villages, where a compound is made up on average of four households.
The results, however, showed that there was one significant cluster in 2006 consisting of 20 villages including Agyegyemakunu, Koofiekrom, Dantwi Awa and Asuogya, while none was found in 2005 and 2007. In the spatio-temporal analysis, the five villages listed above again formed a cluster, though marginally significant. It is not immediately clear why these villages within a radius of 6.98 km of each other and located in the south-eastern corridor of the KHDSS had a significantly higher level of mortality in 2006. What can be attributed to it is that these areas are relatively further away from the health facilities in the district.
Further analyses, however, show interesting differences between this cluster of villages and other rural villages lying outside the cluster. For instance, villages within the cluster were significantly more deprived, i.e. while half of the cluster households were classified as in the poorest wealth quintile, less than 30% of non-cluster villages fit this category. Again, though differences were less pronounced, 62% of women in reproductive age had no education within the cluster, compared to 58% of those outside the cluster. These differences were found to be significant. The linkages between household wealth and child mortality, and also female education and child mortality have been documented (14, 15).
It is also important to note that these villages are located in remote parts of the district, where physical access to health facilities in emergencies is difficult because of unavailable transportation and poor road network. There is neither a clinic nor other health facility within the cluster, covering a radius of close to 7 km. Kintampo town, which stands out as the largest urban community in the KHDSS and the main source of health care, is up to 10 km on average from the villages in the cluster. There are no vehicles permanently stationed in these communities, so they depend on vehicles that come in from Kintampo town and return. Again, these villages lack potable water and electricity supply.
The observed spatial and spatio-temporal cluster may also be hinting at the differential effects of structural problems and disparities in access to health care. For instance, while the significant spatial cluster was located in the Jema sub-district, the clustering involved 20 out of 35 villages (57.1%) and five communities of the 35 (14.3%) of the spatio-temporal cluster. The non-cluster villages also in the sub-district (without Jema town, the district capital) were significantly better off in terms of household wealth and access to transportation (and by implication, ability to get to a health centre). They were also physically closer to the health facility in Jema town.
Despite its utility, one problem of the Kulldorff method is that clusters are defined as circles, such that if a clustering of cases is along a line, a circle is not the appropriate form to detect it. Again, if a village with low mortality is surrounded by villages with high mortality, it is always included in the cluster, although some characteristics of this village may be different from the others. For instance, no childhood deaths were recorded in six villages, which were included in the significant cluster of 2006.
Conclusion
Despite significant gains made in reducing the incidence of childhood deaths in Ghana, a lot still needs to be done to meet set targets for the Millennium Development Goals. This study has shown the potential of the KHDSS to explore the spatial dimensions of childhood mortality clustering. The significant cluster identified in 2006 was in a remote area where access to education and health is very limited. While this study indicates a potential cluster that needs intervention, other studies may be required, perhaps using other methods, to further explain the patterns of childhood mortality observed in this study, to explore the underlying risk factors for potential mortality clusters that could emerge later.
Acknowledgements
The authors wish to thank the Municipal and District Assemblies, chiefs, elders, opinion leaders and community members in the Kintampo North Municipality and Kintampo South district for their goodwill and participation in the demographic surveillance system, staff of KHRC, especially the KHDSS staff in the field and computer centre, Drs Ayaga Bawah and Osman Sankoh of the INDEPTH Network headquarters and Professor Heiko Becher of the University of Heidelberg, Germany for their comments and support. Kintampo Health Research Centre is a member site of the INDEPTH Network. SaTScan™ is a trademark of Martin Kulldorff. The SaTScan™ software was developed under the joint auspices of (a) Martin Kulldorff, (b) the National Cancer Institute and (c) Farzad Mostashari of the New York City Department of Health and Mental Hygiene.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- 1.Hammer GP, Somé F, Müller O, Kynast-Wolf G, Kouyaté B, Becher H. Pattern of cause-specific childhood mortality in a malaria endemic area of Burkina Faso. Malaria J (online edition) 2006. Available from: http://www.malariajournal.com/content/5/1/47 [cited 21 August 2009] [DOI] [PMC free article] [PubMed]
- 2.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS the Bellagio Child Survival Study Group. How many child deaths can we prevent this year? Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 3.Muller O, Krawinkel M. Malnutrition and health in developing countries. Can Med Assoc J. 2005;173:279–86. doi: 10.1503/cmaj.050342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghana Statistical Service (GSS); Noguchi Memorial Institute for Medical Research (NMIMR); ORC Macro. Calverton, MD: GSS, NMIMR, and ORC Macro; 2004. Ghana demographic and health survey 2003; pp. 126–30. [Google Scholar]
- 5.Benzler J, Sauerborn R. Rapid risk household screening by neonatal arm circumference. Results from a cohort study in Burkina Faso. Trop Med Int Health. 1998;3:962–74. doi: 10.1046/j.1365-3156.1998.00340.x. [DOI] [PubMed] [Google Scholar]
- 6.INDEPTH Network. Volume 1: population, health and survival at INDEPTH sites [online edition] Ottawa, ON, Canada: International Development Research Centre; 2002. Population and health in developing countries. Available from: http://www.idrc.ca/en/ev-42993-201-1-DO_TOPIC.html [cited 13 June 2010] [Google Scholar]
- 7.Eisele TP, Lindblade KA, Rosen DH, Odhiambo F, Vulule JM, Slutsker L. Evaluating the completeness of demographic surveillance of children less than five years old in Western Kenya: a capture-recapture approach. Am J Trop Med Hyg. 2003;69:92–7. [PubMed] [Google Scholar]
- 8.Kulldorff M. A spatial scan statistic. Commun Stat Theory Methods. 1997;26:1481–96. [Google Scholar]
- 9.Sankoh OA, Ye Y, Sauerborn R, Muller O, Becher H. Clustering of childhood mortality in rural Burkina Faso. Int J Epidemiol. 2001;30:485–92. doi: 10.1093/ije/30.3.485. [DOI] [PubMed] [Google Scholar]
- 10.Ghana Statistical Service. Ministry of Health (Ghana), United States Agency for International Development. Ghana Multiple Indicator Cluster Survey. 2006. p. 16. Available from: http://www.measuredhs.com/pubs/pub_details.cfm?ID=872&srchTp=type [cited 29 January 2010]
- 11.Owusu-Agyei S, Asante KP, Owusu R, Adjuik M, Amenga-Etego S, Dosoo DK, et al. An open label, randomised trial of artesunate + amodiaquine, artesunate + chlorproguanil-dapsone and artemether-lumefantrine for the treatment of uncomplicated malaria. PLoS One. 2008;3:e2530. doi: 10.1371/journal.pone.0002530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Owusu-Agyei S, Asante KP, Adjuik M, Adjei G, Awini E, Adams M. Epidemiology of malaria in the forest-savanna transitional zone of Ghana. Malaria J (online edition) 2009. Available from: http://www.malariajournal.com/content/8/1/220 [cited 13 June 2010] [DOI] [PMC free article] [PubMed]
- 13.Owusu-Agyei S, Ansong D, Asante KP, Kwarteng Owusu S, Owusu R, Wireko Brobby NA, et al. Randomized controlled trial of RTS,S/AS02D and RTS,S/AS01E malaria candidate vaccines given according to different schedules in Ghanaian children. PLoS One. 2009;4:e7302. doi: 10.1371/journal.pone.0007302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bawah AA, Zuberu T. Socioeconomic status and child mortality: an illustration using housing and household characteristics from African census data. African Pop Stud (online edition) 2004;19 Available from: http://www.bioline.org.br/pdf?epo4033 [cited 19 May 2010] [Google Scholar]
- 15.Amouzou A, Hill K. Child mortality and socioeconomic status in sub-Saharan Africa. African Pop Stud (online edition) 2004. p. 19. Available from: http://tspace.library.utoronto.ca/bitstream/1807/3511/ep04001.pdf [cited 2 June 2010]