Abstract
The goal of this study was to develop a willingness to pay (WTP) question for mammography that is appropriate for low income, ethnically-diverse women. Through qualitative research with 50 low income women of five ethnic groups we developed both a WTP question and a willingness to travel question (WTT). After being refined through interviews with 41 women, these questions were pilot tested on a random sample of 52 low income, ethnically-diverse women in the San Francisco area. Results show that the concepts underlying WTP and WTT were culturally appropriate to the five ethnicities in this study. Analyses generally confirm the validity of the WTP and WTT questions. As expected, WTP was associated with household income, perceived risk of cancer, and knowledge that one needs a mammogram even after a clinical breast examination. Despite the small samples, WTP varied among the ethnic groups. Additionally, WTT was moderately correlated with the natural log of WTP (r = 0.58, P < 0.001). These questions are now in use in a larger clinical trial and future analyses will explore willingness to pay and willingness to travel within and across the ethnic groups.
Keywords: Willingness to pay, Contingent valuation, Patient preferences, Cancer screening, Mammography
1. Introduction
Economists have a tradition of analyzing consumer behavior to determine what individuals would be willing to pay (WTP) for a commodity. Gaining wider acceptance is an alternative methodology that directly asks consumers what they would be willing to pay. Obtaining WTP amounts by analyzing behavior is referred to as revealed preferences (WTPRP), while the survey counterpart is called contingent valuation (WTPCV). As it implies, contingent valuation requires the respondent to place a monetary value on a specific good without having to actually make the purchase.
Contingent valuation is often used by health services researchers to get patients to value non-market goods or hypothetical treatments. Researchers can, for example, ask patients to value a hypothetical preventive asthma treatment that reduces the frequency of symptoms. The expectation is that people would be willing to spend some of their money to obtain the good — the more they value the good, the more they are willing to pay. In theory, one’s maximal willingness to pay represents the point where the marginal utility from having the money is equal to the marginal utility of the good being valued.
The use of WTPCV (hereafter referred to as WTP) is not without controversy. Advocates usually note that the metric underlying WTP is money, something with which everyone is familiar. Economists also often tout that willingness to pay adheres to welfare economics, enabling decisions based on production efficiency (Ref. [1], p. 208). Interpersonal comparisons of utility are possible by treating money as a ratio scale. Yet, critics say that comparing different individuals’ responses can be dangerous because people with more money are often willing and able to spend more. This issue, perhaps more than any other, makes many researchers uncomfortable with willingness to pay as a measure of benefit.
Although the WTP literature continues to expand, four salient points are apparent from reviewing the literature. First, as WTP has been developing as a methodology, most studies have relied on convenience samples. Consequently, samples usually draw on middle/upper class whites who speak English. Few studies even report race or ethnicity when describing the sample. Exceptions include Ramsey et al. [2] and O’Conor and Blomquist [3]. However, both of these samples were more than 85% white.
Second, most studies that used postal surveys had a significant percentage of incomplete data. Reported response rates have been as low as 45% [4]. Higher response rates were more typical among interviewer-administered surveys, which, for practical reasons, tend to be less common than postal surveys. Some believe that the incomplete data reflects distrust or discomfort when asked these questions. Such non-response is common when asking about household income. Yet the wide range of incomplete data suggests that these questions are not only objectionable to some patients, but that some WTP questions are probably confusing as well. Interestingly, few studies reported undertaking formative research to ensure the WTP question was clear and understandable to the target audience.
Third, in most WTP studies in medicine, respondents are asked to value a hypothetical medicine or medical procedure that will improve the individual’s health status by alleviating symptoms. Examples include paying for reductions in urinary incontinence symptoms [5] or reductions in angina symptoms [6]. Researchers are starting to branch out and ask WTP about other issues. One study, for example, asked people what they would be willing to pay for autologous blood donations to reduce the risk of contracting blood-borne illnesses [4].
Fourth, as mentioned above, there is a consistent positive relationship between WTP and ability to pay, as measured by household income. This is a predicted relationship according to economic theory. In fact, this association is often used as an internal validation check of the underlying economic model [7]. Yet many health practitioners are uncomfortable using a measure of benefit that varies so dramatically by household income. Some of these concerns can be handled statistically by adjusting for household income. However, concerns persist about the validity of WTP with very low income persons. Is WTP meaningful when the respondents have no ability to pay? People with very low incomes might perceive money very differently than those with more economic resources, making it difficult to compare these groups. Understanding WTP among persons with very low income is just starting to be addressed [8].
This study relates to all four issues by reporting on the development and pilot testing of a willingness to pay question for mammography. Developing the WTP item arose as preliminary work for a much larger randomized clinical study, now underway, to increase mammography and pap smear screening. The development process started with focus groups and individual interviews with low income women representing five race/ethnic groups (African American, Chinese, Filipino, Latino, and white) and four languages (English, Chinese, Spanish and Tagalog). The validity of willingness to pay question was then tested with a random sample of low income, ethnically diverse women.
2. Methods
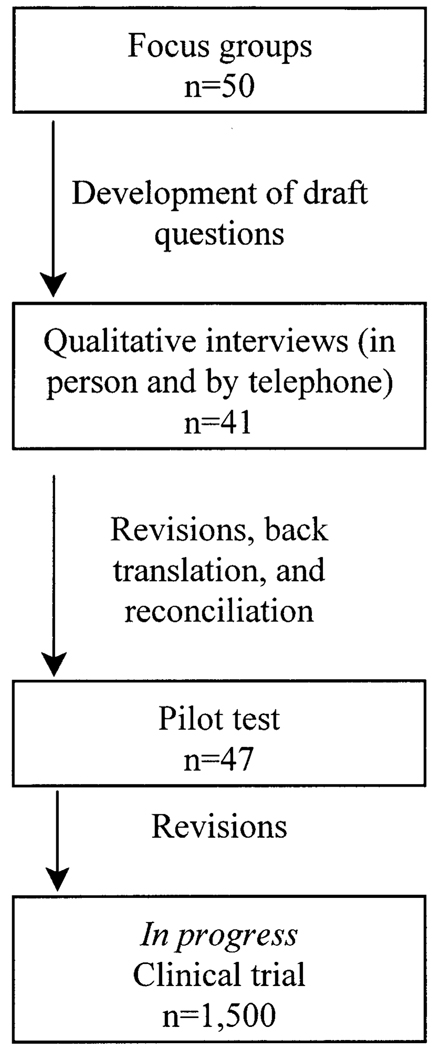
We followed three consecutive steps in developing the WTP questions for mammography screening. First, focus groups were conducted to discuss cost issues related to mammography screening and how the price affected willingness to obtain annual mammograms. Second, draft questions and response categories were developed and refined using qualitative interviews. Lastly, the WTP question was pilot tested with a sample of mostly low income women of diverse ethnicity and language. These steps are discussed in more detail below.
At the outset of the study, it was decided to develop two questions that would be potential alternatives to willingness to pay. This was due to concerns expressed by members of the research team that the respondents would find the WTP questions threatening, implying that they may be asked to pay for services that they currently receive for free. The two additional items were willingness to wait (WTW) and willingness to travel (WTT) to get a free mammogram. Fundamental to these three questions (i.e. WTP, WTW, WTT) is that the respondent must make a trade-off. In the WTP scenario, the individual is trading money for a hypothetical health care service. In the other two questions, the person is trading his/her time for free services.
2.1. Step 1: focus groups
For the focus groups, women 40–74 years of age were recruited from health clinics, churches and community-based organizations in San Francisco and Richmond. Recruitment was stratified by race/ethnicity and primary spoken language. The five strata were English-speaking white women, English-speaking African American women, Spanish-speaking Latinas, Cantonese-speaking Chinese women, and Tagalog-speaking Filipinas. Recruitment focused on low income women. This was done to ensure that the research would represent the views of low income, less educated, minority women. Human subjects approval was obtained and participants signed an informed consent.
A total of five focus groups, each with ten women, were conducted in San Francisco and Richmond, CA. These lasted ~2 h each. All of the focus group facilitators were women whose race/ethnicity and language matched the focus group participants. The facilitators were instructed on the willingness to pay concept and they followed a focus group discussion guide that was standardized across the four languages.1 The goal of the focus groups was to both learn more about how these women thought about money and to develop the survey instrument [9]. After introductions, each focus group opened with a discussion about health insurance and whether or not the insurance paid for mammograms. The group then discussed willingness to wait and willingness to travel, after which the willingness to pay concept was introduced.
Eventually participants were shown a placard with a prototype WTP question. They were asked to discuss what this question meant to them. Lastly, the facilitators asked them if they would be willing to pay $10 for a mammogram. If they said no, the facilitators lowered the amount. The facilitators then started raising the amount by $25 increments until no one would be willing to pay that amount for a mammogram. The purpose of this exercise was to establish responses categories that would span the lowest to highest amounts.
The focus groups were tape recorded. The tapes were then transcribed and the non-English sessions were translated into English. It was evident from the focus groups that the women had little trouble understanding the concept of willingness to pay and willingness to travel. However, some expressed discomfort with talking about willingness to pay. Many of the participants needed reassurance that their answers would not affect the services that they received and some said they might not answer such a question on a telephone interview.
Two other findings from the focus groups merit discussion. First, some women found it difficult to imagine that they would have to spend their money to get a mammogram. These women typically pay only small copayments for health care and most prior mammograms were provided free of charge. It was difficult for them to consider paying more than they usually do. They would often say that they would not pay $75 because they knew they could get one free. Throughout the focus groups, we often had to remind the participants that in the hypothetical scenario getting a free mammogram was not possible. Second, although not a common issue, some women thought that we were asking what they would be willing to pay for a mammogram if they were ill or if a breast lump had been found. Reassurance was given that the test was only a preventive measure. Subsequently, the interviewers for the pilot test were instructed to provide this context should the women question the reason for obtaining the mammogram.
From the qualitative work, we had trouble identifying the maximum amount of time that the women would be willing to wait. Many of these women already go to crowded public clinics where they typically wait 2 h to see the doctor. At the same time, many of the women who immigrated from China, Latin America or the Philippines expect to wait long times. Additionally, it was evident that the willingness to wait question consistently confused participants. Some women thought they were being asked to wait longer because the doctor was incompetent or because a serious problem was found. Alternative formulations were tried, but eventually we decided to drop the willingness to wait question.
2.2. Step 2: development and refinement of the draft questions
The focus groups sessions were tape recorded, transcribed, and the non-English sessions were translated into English. From the focus group transcripts, the willingness to pay and willingness to travel questions were drafted, along with response categories for both (Fig. 1). Cognitive debriefing interviews, in which the women were asked about their perceptions of the items, were then conducted over the phone with five English-speaking women (two African American women, two Latinas, one white woman). The questions and response categories were revised. Then a second round of five cognitive debriefing interviews (three African American women, two Latinas) were conducted over the phone; the WTP item did not go through the second cognitive debriefing as it was not needed. The WTP and WTT items were subsequently translated into Spanish, Cantonese, and Tagalog. A third round of cognitive debriefing interviews was done with 26 women, including seven Cantonese, six Tagalog, seven Spanish, and six English-speaking participants. After slight revisions, another set of cognitive debriefing interviews was done with four Chinese-speaking women, three Tagalog-speaking women, four Spanish-speaking women, and four English-speaking women. The questions were then revised in all languages, after which they were back translated into English. The forward and back translations were reconciled with the help of the focus group facilitators. The English versions of the willingness to pay and willingness to travel questions are listed in Appendix A.2 It should be noted that great effort was taken to make the introduction to the WTP easy for low income, low literate, ethnically-diverse women to understand.
Fig. 1.
Methods for questionnaire development.
2.3. Step 3: cross-cultural pilot testing of the draft questions
The final stage in questionnaire development involved a cross-cultural pilot test. This was part of a larger pilot test for a clinical trial. The questionnaire was administered using a computer-assisted telephone interview (CATI) system. Random digit dialing was done in selected zip codes known to have more low income households and higher rates of non-white residents. Ethnic surnames were also used to improve sampling among Filipinos, Hispanics, and Chinese. Included were women between 40 and 74 years of age, and women 50 and over were oversampled. If more than one eligible woman lived in the home, the interviews were instructed to first ask for women over age 50 and then sort by the most recent birthday. Excluded were women who did not self-identify as either Chinese/Chinese American, Filipina/Filipina American, Hispanic/Spanish, Black/African American/African, or white.
For the WTP and WTT questions, the starting ‘bids’ were $75 and 2 h each way, respectively. The second bid went up or down in amount, depending on the answer to the first one. Although there were seven response categories for each question, at most each woman was asked four follow-up bids. If the woman was willing to pay more than $200 or willing to travel more than 3.5 h each way, then an open-ended question was asked “What is the most money that you would be willing to pay to get a mammogram?” or “What is the most amount of time you would be willing to travel — each way — to get a free mammogram?”. Similarly, if the respondent said they would not pay $10 or would not travel 30 min each way, then the same open-ended question was asked. From the respondent’s answers to the bids, a total WTP and WTT amount was calculated.
2.4. Internal validity
To test internal validity, the WTP and WTT questions were correlated with annual household income, which was collected as a categorical variable. Due to the sample size, a single dummy variable was included that identified whether the participant was above or below the sample’s median income. It was expected that WTP would be positively associated with household income. Conversely, it was expected that WTT would be negatively associated with income because as income goes up, so does one’s opportunity cost (i.e. time becomes more valuable as wages increase). This hypothesis rests on the assumption that people seek to minimize travel time to the physician. This is consistent with past studies that have shown that travel time is an important cost in the demand for medical care [10–13].
2.5. Construct validity
WTP should vary by the scope of the benefits [14]. Such a test is difficult with mammograms because either the woman gets the mammogram or she does not. Thus, construct validity was tested by comparing both WTP and WTT with past screening behaviors, with perceived risk for breast cancer, and with attitudes toward mammography screening. Past screening behaviors included having ever had a mammogram and the number of mammograms in the past 5 years. It was expected that a prior history of getting a mammogram and a higher number of mammograms in the past 5 years would be positively associated with WTP and WTT. Perceived risk of cancer was based on whether the woman had a mother, sister or daughter (related by blood) with breast cancer. We expected that women with a family history of breast cancer would be willing to pay more for a mammogram. Lastly, attitudes toward mammography screening included what a woman perceived as her chances of surviving breast cancer, whether she felt that she needed a mammogram in addition to a clinical breast examination, and whether she felt that mammograms were the best way to detect cancer. It was expected that people who placed more importance on mammograms would be willing to pay more for one and travel a further distance to get one free of charge. These associations were estimated using chi-square statistics.
2.6. Predictors of WTP and WTT
We then used multivariate regression analysis to determine which factors predicted WTP and WTT. For this analysis, WTP and WTT were treated as continuous variables. In addition to the variables discussed above, age and education were included in the model. The distributions for WTP and WTT were visually inspected using a kernel density diagram. A kernel density diagram is similar to a histogram, although it avoids problems associated with binning the data. Because WTP was right skewed, as is often the case with economic data, a log transformation was used; these results were compared to the non-transformed WTP model.
3. Results
3.1. Sample characteristics
A total of 52 women were interviewed on the phone. In the sample, there were 12 African Americans, ten Filipinas, ten Latinas, 12 white women and three Chinese women. The data from five other Chinese women were lost due to a technical problem. Table 1 shows that the age of the remaining 47 respondents ranged from 48 to 69, with a mean of 58 (S.D. = 5.7). The respondents had a wide range of annual household incomes; 30% had a household income of less than $10 000, and 55% had an income under $30 000. In comparison, the 1995 estimated median household income in San Francisco and Alameda County was $37 854 and $44 653, respectively (compared to $34 076 nationally).
Table 1.
Sample characteristics (n = 47)
| Frequency |
||
|---|---|---|
| n | % | |
| Women | 47 | 100.0 |
| Race/ethnicity | ||
| African American | 12 | 25.5 |
| Chinese | 3 | 6.4 |
| Filipina | 10 | 21.3 |
| Latina | 10 | 21.3 |
| White | 12 | 25.5 |
| Age: mean (S.D.) | 57.6 (5.7) | |
| Years of schooling completed: mean (S.D.) | 12.3 (4.0) | |
| Past screening behaviors | ||
| Ever had mammogram | 45 | 95.7 |
| Number of mammograms in last 5 years: mean (S.D.) | 3.8 (1.5) | |
| Perceived risk of breast cancer | ||
| Sister, mother or daughter (related by blood) had breast cancer | 8 | 17.0 |
| Attitudes to mammograms | ||
| Perceived chance of survival for early detection (% who said excellent) | 21 | 44.7 |
| Need mammogram after clinical breast examination (% who agreed) | 6 | 12.8 |
| Mammogram is best method for detecting breast cancer (% who agreed) | 35 | 74.5 |
All but two all of the respondents had had a mammogram in the past 5 years. In fact, 49% reported having had five mammograms in the past 5 years. When asked if they planned to get a mammogram in the next year, 83% of the women said yes. In addition, 17% of the women reported that their mother, sister or daughter (related by blood) had had breast cancer.
Generally, the women had positive attitudes toward mammography screening (Table 1). When asked if they thought a woman their age needed a mammogram, 87% said yes. A total of 45% (n = 21) said that the chances of surviving breast cancer were ‘excellent’ if it is detected early, whereas 47% said their chances were ‘good’; none said that their chance was ‘fair’ or ‘poor’. When asked if they could do without a mammogram after having a clinical breast examination, 87% disagreed, though 13% agreed. When asked whether mammograms were the best way to detect cancer, 70% ‘strongly’ agreed, while 21% disagreed ‘strongly’ or ‘somewhat’.
3.2. Internal validity
As expected, WTP was positively associated with income. Women with a household income of greater than $30 000 had a mean WTP of $176 (S.D. = $134), whereas women with less income were willing to pay approximately $59 (S.D. = $28) for a mammogram (χ2 = 44.2 (16); P < 0.001). Also, as predicted, WTT varied inversely by income. Women with a household income of less than $10 000 were willing to travel on average 20 min longer to get a free mammogram. However, this difference was not statistically significant (χ2 = 15.7 (12); P = 0.21).
3.3. Construct validity
Construct validity was tested by correlating both WTP and WTT with past screening behaviors, with perceived risk for breast cancer, and with attitudes toward mammography screening. Since almost every woman had had a prior mammogram, we were unable to correlate past screening behaviors with WTP or WTT. Number of mammograms in the past 5 years had more variation and was predicted to positively correlate with WTP and WTT. In both cases, we found the opposite to be true: people with more mammograms in the past 5 years were willing to pay less (P = 0.002) and willing to travel less (P = 0.063).
Family history of cancer, which affects the woman’s perceived risk, was strongly related to WTP and WTT, as was predicted. Women whose sister, mother, or daughter had had cancer were willing to pay significantly more (χ2 = 20.4 (8); P < 0.009) and were also willing to travel further to get a free mammogram (χ2 = 13.1 (8); P = 0.07).
Attitudes toward mammography screening generally varied with WTP and WTT in the predicted directions, however, the effects were not always statistically significant. Women who felt that they had an ‘excellent’ chance of surviving if the breast cancer was detected early were willing to pay more (χ2 = 19.2 (7); P = 0.008) and willing to travel further (χ2 = 15.7 (7); P = 0.03) than women who felt their chances of survival were ‘good’. Women who felt that they needed a mammogram in addition to a clinical breast examination were willing to pay more (χ2 = 23.3 (8); P = 0.03) and willing to travel further (χ2 = 9.9 (7); P = 0.20) than women who did not feel this way. Lastly, women who felt that mammograms were the best way to get screened for cancer were willing to pay more (χ2 = 14.6 (8); P = 0.07) and willing to travel further (χ2 = 18.8 (7); P = 0.009) than women who felt that there were better detection methods.
3.4. Determinants of WTP and WTT
Table 2 shows that the mean WTP was $112 (S.D. = $107). A total of seven women (15%) refused to answer the question and of those who did, willingness to pay varied from $5 to $500 (Table 2). On average, women were willing to travel 102 min (S.D. = 74) each way to get a free mammogram. Responses varied from 0 to 240 min. Of the 47 women, two refused to answer the question.
Table 2.
Variation in willingness to pay (WTP) and willingness to travel (WTT)a
| Total | African American | Chinese | Filipina | Latina | White | |
|---|---|---|---|---|---|---|
| Sample size | 47 | 12 | 3 | 10 | 10 | 12 |
| WTP in dollars | ||||||
| Mean | 112 | 96 | 88 | 63 | 100 | 172 |
| (S.D.) | (107) | (73) | (18) | (30) | (47) | (171) |
| WTT in minutes | ||||||
| Mean | 102 | 105 | 105 | 60 | 132 | 110 |
| (S.D.) | (74) | (94) | (21) | (66) | (81) | (43) |
Differences in WTP and WTT across the groups of women were statistically significant at P < 0.01.
Table 3 shows the determinants of log transformed WTP (logWTP) and WTT in the multivariate analysis. Significant factors that were associated with logWTP, were number of mammograms in the past 5 years, family history of breast cancer, perceived chance of survival if breast cancer is detected early and household income. Age was also positively associated with logWTP, but this effect was only marginally significant. The model had an R2 of 0.81, partly due to the limited degrees of freedom, and was highly significant (F11,24 = 9.52, P < 0.001). The factors that were associated with the logWTP remained important when regressed on WTP (data not shown). Interestingly, the only variable associated with WTT was family history of breast cancer and being Latina. For WTT, the model accounted for 53% of the variance (F11,28 = 2.91, P = 0.01).
Table 3.
Determinants of WTP and WTTa
| OLSb |
SURb |
|||
|---|---|---|---|---|
| LogWTP | WTT | LogWTP | WTT | |
| Number of mammograms in the last 5 years? (0–5) | −0.294** | −29.581* | −0.294** | −21.162** |
| (2.769) | (2.190) | (3.391) | (2.989) | |
| Sister, mother or daughter (related by blood) had breast cancer (1 = yes, 0 = no) | 0.988** | 101.420** | 0.988** | 86.643** |
| (3.932) | (3.060) | (4.815) | (5.173) | |
| Perceived chance of survival for early detection (excellent = 1; good = 0) | −0.323 | −16.866 | −0.323 | −106.644** |
| (1.078) | (0.499) | (1.320) | (5.347) | |
| Need mammogram after clinical breast examination (agree = 1; disagree = 0) | 1.246* | 9.166 | 1.246** | 0.865 |
| (2.351) | (0.131) | (2.879) | (0.025) | |
| Mammogram is best method for detecting breast cancer (agree = 1; disagree = 0) | −0.384 | −44.539 | −0.384 | −10.023 |
| (1.437) | (1.307) | (1.760) | (0.563) | |
| Income (1 = $30 000+, 0 = otherwise) | 1.502** | 14.490 | 1.502** | 14.188 |
| (6.096) | (0.444) | (7.466) | (0.864) | |
| Years of schooling (2–20) | 0.093 | 4.371 | 0.093* | 0.586 |
| (1.888) | (0.680) | (2.312) | (0.179) | |
| Age | 0.012 | −0.248 | 0.012 | −5.305** |
| (0.465) | (0.076) | (0.569) | (3.064) | |
| African American | 0.999* | 110.206 | 0.999** | 127.824** |
| (2.122) | (1.796) | (2.599) | (4.076) | |
| Filipina | 0.413 | 53.416 | 0.413 | −17.589 |
| (0.918) | (0.953) | (1.125) | (0.587) | |
| Latina | 1.186* | 142.011* | 1.186** | 119.272** |
| (2.576) | (2.373) | (3.155) | (3.888) | |
| Constant | 2.563 | 115.524 | 2.563 | 478.295** |
| (1.354) | (0.488) | (1.658) | (3.792) | |
| Observations | 36 | 40 | 36 | 36 |
| R-squared (pseudo R-squared for SUR) | 0.81 | 0.53 | 0.81 | 0.82 |
| Adjusted R-squared | 0.73 | 0.35 | – | – |
| Model statistics (F-statistic for OLS, χ2 for SUR)c | 9.52** | 2.87** | 157.1** | 161.1** |
Absolute value of t-statistics in parentheses.
Ordinary least squares regression (OLS); Zellner’s seemingly unrelated regression (SUR).
The models have 11 parameters; degrees of freedom = observations – parameters – 1.
Significant at 5% level (two-tailed test).
Significant at 1% level (two-tailed test).
The models for logWTP and WTT were also estimated simultaneously using Zellner’s seemingly unrelated regression. The results show that logWTP and WTT were highly correlated (r = 0.58, P < 0.001). Taking advantage of joint covariance allowed us to more efficiently estimate the models’ coefficient. Factors significantly associated with WTT included family history of breast cancer, need to have a mammogram in addition to a clinical breast examination, educational attainment, and age (Table 3). The standard errors for most of these coefficients was relatively large, which is related to the small sample sizes. Interestingly, further analyses indicated that WTP (untransformed) and WTT were not significantly correlated.
4. Discussion
In an era when patients and consumers are being increasingly asked willingness to pay questions in research studies, it is reassuring to note that the ethnically-diverse women in the focus groups understood the concept of willingness to pay. The qualitative testing provided further evidence that the concepts behind WTP and WTT were culturally appropriate to the five groups in this study.
Despite the extensive qualitative work, there were substantial missing data in the pilot test. This was not expected. A total of seven women (15%) did not answer the WTP question. Missing data was significantly less of a problem for the WTT and household income questions, for which only one woman (2%; P = 0.016) did not provide an answer for each. The respondent who did not answer the WTT also did not answer the WTP question, but she did answer the income question.
The concept of directly asking people how far they would travel to get a free health service is relatively novel. We are only aware of one similar study. Johannesson and colleagues [15,16] developed a question that asked if people would give up some leisure time to participate in a lipid lowering treatment program. However, the concept of leisure time differs from travel time to the physician in that people seek to maximize leisure time and to minimize travel time. Nonetheless, both can be used in cost-benefit analysis if opportunity costs and travel costs are estimated.
While directly asking people about travel time might be novel, using an individual’s actual travel time as a determinant of medical care utilization has a longer tradition [10–13,17]. Recently, Clarke, [18] used travel costs, which include time, as part of a cost-benefit model for mobile mammography screening units. He found that travel costs, standardized by income, varied substantially and that they were negatively associated with getting a mammogram. This provides some reassurance that women consider travel time when deciding whether to get a mammogram. Because actual travel time can easily be collected in survey, it would be worthwhile for future research to directly compare these alternative mesures of benefit.
The responses scales for the WTT and WTP questions were designed as iterative bids. While we could have used a single binary question where we varied the bid amounts, as is often done [7,19], we wanted more precise answers given that the study follows people over time. Consistent with past findings [20], a single binary response would have reduced our ability to detect small but meaningful within-person changes over time. Alternatively, we could have used an open-ended response, but this method is not recommended [14,21,22]. Although one study found that bid scales can lead to starting-point bias [23], another did not [24]. Whether this study was affected by starting-point bias could not be ascertained.
Results from the pilot data generally confirm the validity of the WTP and WTT questions. Most of the factors associated with WTP and WTT were in the predicted direction, although the standard errors were often relatively large. One unexpected finding was that number of mammograms in the last 5 years was inversely related to WTP and WTT, contrary to expectations. This may reflect that women who had more mammograms had more knowledge about free mammogram services available in the community and thus we not willing to pay as much money out of their pockets. If this is true, then this finding is disconcerting because it suggests that the respondents had a hard time envisioning the hypothetical scenario in which they could not receive a free mammogram. However, other factors might also be responsible for this effect and this issue will be reexamined with the data that we are currently collecting.
Despite the small sample, Table 3 shows that WTP and WTT varied by ethnic group. Although further subgroup analyses were precluded due to the sample size, these measures are currently in the field as part of baseline assessment in a larger clinical trial (n = 1500). These data will also allow us to more thoroughly explore the association between ethnicity and WTP and WTT. In addition, we expect to use this clinical trial data to learn more about changes in WTP and WTT over time. We will then compare the changes in these measures over time to the costs of the intervention; we hope this will provide useful information about whether the tailored educational intervention is cost-beneficial.
To our knowledge this is the first study to conduct qualitative research and then quantitatively measure WTP and WTT among low income, ethnically-diverse women with regard to preventive health care services. Although this article addresses some gaps in the literature, clearly additional multidisciplinary research is warranted. This study also supports the conclusion that proper formative work is necessary in order to develop items that are appropriate for the target audience. Although researchers can start by using already developed questions, studies that skip the cognitive debriefing and pilot testing altogether may end up using poorly worded or confusing questions, thereby jeopardizing data quality.
Acknowledgements
This work was supported by a grant from the National Cancer Institute (2PO1 CA 55112-05A1). The opinions expressed are those of the authors and do not reflect affiliated or sponsoring organizations. Thanks to Stephen McPhee and Kathryn Phillips for comments and suggestions.
Appendix A
English versions of the willingness to pay (WTP) and willingness to travel (WTT) questions
Willingness to pay
The following questions ask how important you think mammograms are. I am going to ask how much you would be willing to pay to get a mammogram. Please be assured that answering these questions will not increase the cost of any medical services. Your answer simply tells us what the mammogram is worth to you in dollars. Okay, here are the questions.
| 1. Many women get mammograms free of charge. But suppose that there was no way to get a free mammogram. Would you get a mommogram if it cost $75? | ||
| 1. | Yes | GO TO 2 |
| 2. | No | GO TO 5 |
| 3. | {DON’T READ} NO, WOULD NOT PAY ANYTHING | STOP, End Qx |
| 7. | {DON’T READ} NOT APPLICABLE | GO TO 8 |
| 8. | {DON’T READ} REFUSED | GO TO 8 |
| 2. Would you be willing to pay $100 for a mammogram? | ||
| 1. | Yes | GO TO 3 |
| 2. | No | STOP, End Qx |
| 3. Would you be willing to pay $125? | ||
| 1. | Yes | GO TO 4 |
| 2. | No | STOP, End Qx |
| 4. Would you be willing to pay $150? | ||
| 1. | Yes | GO TO 8 |
| 2. | No | STOP, End Qx |
| 5. Would you be willing to pay $50 for a mammogram? | ||
| 1. | Yes | STOP, End Qx |
| 2. | No | GO TO 6 |
| 6. Would you be willing to pay $25? | ||
| 1. | Yes | STOP, End Qx |
| 2. | No | GO TO 7 |
| 7. Would you be willing to pay $10? | ||
| 1. | Yes | STOP, End Qx |
| 2. | No | GO TO 8 |
| 8. What is the most money that you would be willing to pay to get a mammogram? (PROBE): Considering what you can afford right now, what is the most money that you would be willing to pay for a mammogram? | ||
| INTERVIEWER: Payment for routine mammograms only | ||
| AMOUNT (dollars) | (Logical range = 0–500) | |
| Willingness to travel | ||
| 1. Suppose that there was a clinic offering free mammograms. However, in order to get a mammogram, you would have to travel to the clinic. If you had to travel 2 h each way, would you make the trip for the free mammogram? | ||
| INTERVIEWER: Travel for routine mammograms only | ||
| 1. | Yes | GO TO 2 |
| 2. | No | GO TO 5 |
| 3. | {DON’T READ} NO, WOULD NOT TRAVEL | STOP, End,Qx |
| 7. | {DON’T READ} NOT APPLICABLE | GO TO 8 |
| 8. | {DON’T READ} DON’T KNOW:NOT SURE | GO TO 8 |
| 9. | {DON’T READ} REFUSED | GO TO 8 |
| 2. Would you travel 2.5 h each way for a free mammogram? | ||
| 1. | Yes | GO TO 3 |
| 2. | No | STOP, End Qx |
| 3. Would you travel 3 h each way? | ||
| 1. | Yes | GO TO 4 |
| 2. | No | STOP, End Qx |
| 4. Would you travel 3.5 h each way? | ||
| 1. | Yes | GO TO 8 |
| 2. | No | STOP, End Qx |
| 5. Would you travel 1.5 h each way for a free mammogram? | ||
| 1. | Yes | STOP, End Qx |
| 2. | No, GO TO 6 | |
| 6. Would you travel 1 h each way? | ||
| 1. | Yes | STOP, End Qx |
| 2. | No | GO TO 7 |
| 7. Would you travel 0.5 h each way? | ||
| 1. | Yes | STOP, End Qx |
| 2. | No | GO TO 7 |
| 8. What is the most amount of time you would be willing to travel — each way — to get a free mammogram? | ||
| HS (each way) | (Logical range = 0–10) | |
| MINS (each way) | (Logical range = 0–59) | |
| 9995. {DON’T READ} NO, WOULD NOT TRAVEL | ||
| 9996. {DON’T READ} NO LIMIT, WOULD TRAVEL HOWEVER LONG IT TAKES | ||
| 9997. {DON’T READ} NOT APPLICABLE | ||
| 9998. {DON’T READ} DON’T KNOW:NOT SURE | ||
| 9999. {DON’T READ} REFUSED | ||
Footnotes
The discussion guide can be obtained from the authors.
The various translations of these questions can be obtained from the authors.
References
- 1.Drummond MF, O’Brien B, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 1997. [Google Scholar]
- 2.Ramsey SD, Sullivan SD, Psaty BM, Patrick DL. Willingness to pay for antihypertensive care: evidence from a staff-model HMO. Soc Sci Med. 1997;44:1911–1917. doi: 10.1016/s0277-9536(96)00300-0. [DOI] [PubMed] [Google Scholar]
- 3.O’Conor RM, Blomquist GC. Measurement of consumer-patient preferences using a hybrid contingent valuation method. J Health Econ. 1997;16:667–683. doi: 10.1016/s0167-6296(97)80198-1. [DOI] [PubMed] [Google Scholar]
- 4.Lee SJ, Neumann PJ, Churchill WH, Cannon ME, Weinstein MC, Johannesson M. Patients’ willingness to pay for autologous blood donation. Health Policy. 1997;40:1–12. doi: 10.1016/s0168-8510(96)00879-2. [DOI] [PubMed] [Google Scholar]
- 5.Johannesson M, O’Conor RM, Kobelt-Nguyen G, Mattiasson A. Willingness to pay for reduced incontinence symptoms. Br J Urol. 1997;80:557–562. doi: 10.1046/j.1464-410x.1997.00420.x. [DOI] [PubMed] [Google Scholar]
- 6.Chestnut LG, Keller LR, Lambert WE, Rowe RD. Measuring heart patients’ willingness to pay for changes in angina symptoms. Med Decis Mak. 1996;16:65–77. doi: 10.1177/0272989X9601600115. [DOI] [PubMed] [Google Scholar]
- 7.Ryan M. Should government fund assisted reproductive techniques? A study using willingness to pay. Appl Econ. 1997;29:841–849. [Google Scholar]
- 8.Donaldson C. Valuing the benefits of publicly-provided health care: does ‘ability to pay’ preclude the use of ‘willingness to pay’? Soc Sci Med. 1999;49:551–563. doi: 10.1016/s0277-9536(99)00173-2. [DOI] [PubMed] [Google Scholar]
- 9.O’Brien K. Using focus groups to develop health surveys: an example from research on social relationships and AIDS-preventive behavior. Health Educ Q. 1993;20:361–372. doi: 10.1177/109019819302000307. [DOI] [PubMed] [Google Scholar]
- 10.Cauley SD. The time price of medical care. Rev Econ Stat. 1987;69:59–66. [Google Scholar]
- 11.Coffey RM. The effect of time price on the demand for medical-care services. J Hum Res. 1983;18:407–424. [Google Scholar]
- 12.Gertler P, van der Gaag J. The willingness to pay for medical care: evidence from two developing countries. Baltimore, MD: Johns Hopkins University Press; 1990. [Google Scholar]
- 13.Torgerson DJ, Donaldson C, Reid DM. Private versus social opportunity cost of time: valuing time in the demand for health care. Health Econ. 1994;3:149–155. doi: 10.1002/hec.4730030304. [DOI] [PubMed] [Google Scholar]
- 14.NOAA. Report of the National Oceanic and Atmospheric Administration. Fed Reg. 1992;58:4601–4614.
- 15.Johannesson M. Economic evaluation of lipid lowering — a feasibility test of the contingent valuation approach. Health Policy. 1992;20:309–320. doi: 10.1016/0168-8510(92)90163-6. [DOI] [PubMed] [Google Scholar]
- 16.Johannesson M, Johansson P-O, Kristrom B, Borgquist L, Jonsson B. Willingness to pay for lipid lowering: a health production function approach. Appl Econ. 1993;25:1023–1031. [Google Scholar]
- 17.Acton JP. Non-monetary factors in the demand for medical services — some empirical evidence. J Political Econ. 1975;83:595–614. [Google Scholar]
- 18.Clarke PM. Cost-benefit analysis and mammographic screening: a travel cost approach. J Health Econ. 1998;17:767–787. doi: 10.1016/s0167-6296(98)00031-9. [DOI] [PubMed] [Google Scholar]
- 19.Hanemann WM. Valuing the environment through contingent valuation. J Econ Perspect. 1994;8:19–43. [Google Scholar]
- 20.Ready RC, Buzby JC, Hu D. Differences between continuous and discrete contingent value estimates. Land Econ. 1996;72:397–411. [Google Scholar]
- 21.Kartman B, Stalhammar NO, Johannesson M. Valuation of health changes with the contingent valuation method: a test of scope and question order effects. Health Econ. 1996;5:531–541. doi: 10.1002/(SICI)1099-1050(199611)5:6<531::AID-HEC235>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 22.Donaldson C, Thomas R, Torgerson DJ. Validity of open-ended and payment scale approaches to eliciting willingness to pay. Appl Econ. 1997;29:79–84. [Google Scholar]
- 23.Johannesson M, Jonsson B. Economic evaluation in health care: is there a role for cost-benefit analysis? Health Policy. 1991;17:1–23. doi: 10.1016/0168-8510(91)90114-d. [DOI] [PubMed] [Google Scholar]
- 24.O’Brien B, Viramontes JL. Willingness to pay: a valid and reliable measure of health state preference? Med Decis Mak. 1994;14:289–297. doi: 10.1177/0272989X9401400311. [DOI] [PubMed] [Google Scholar]