Abstract
Suicidal behavior (SB) represents a major public health issue. Clinical and basic research suggests that SB is a specific entity in psychiatric nosology involving a combination of personality traits, genetic factors, childhood abuse and neuroanatomical abnormalities. The principal risk factor for suicide is depression. More than 60% of patients who complete suicide are depressed at the time of suicide, most of them untreated. There has been a controversy concerning a possible increased risk of SB in some depressed patients treated with antidepressants. Most recent evidence suggests, however, that treatment of depressed patients is associated with a favorable benefit-risk ratio. A recent study has determined the effects of 6 weeks of antidepressant treatment with the serotonin and norepinephrine reuptake inhibitor, milnacipran, on suicidality in a cohort of 30 patients with mild to moderate depression. At baseline, mild suicidal thoughts were present in 46.7% of patients. Suicidal thoughts decreased progressively throughout the study in parallel with other depressive symptoms and were essentially absent at the end of the study. At no time during treatment was there any indication of an increased suicidal risk. Retardation and psychic anxiety decreased in parallel possibly explaining the lack of any “activation syndrome” in this study.
Keywords: suicide, milnacipran, SNRI, activation syndrome
Introduction
Suicidal behavior represents a major public health issue. Suicide is among the 10 leading causes of death for all ages.1 Every year more than 100,000 men and women commit suicide in Europe2 and the World Health Organization estimates that there will be about 1.5 million deaths by suicide per year worldwide by 2020.3
Suicide and depression
Mental disorders, especially depression, are present in more than 90% of suicides, and over 80% are untreated at the time of death.4,5 An often-quoted figure is that about 15% of patients with major depression will eventually die by suicide.6 This estimation was, however, derived largely from studies of severely depressed inpatients. A lifetime suicide risk of about 6% has been calculated for all depressed patients.7 The discrepancy between these figures may be erroneously interpreted as evidence that overt suicidal behavior occurs almost exclusively in severe depression, a notion which can lead to inappropriate management of less severely depressed patients. There is, however, clear evidence that suicidality (thoughts and behavior) is associated with any type of depressive disorder and any degree of severity.8,9
The increased use of pharmacological treatments in psychiatric diseases has had only a small effect at decreasing the rates of attempted and completed suicides over recent years.10 There is therefore a pressing need to revisit suicide prevention strategies in order to promote action specifically directed towards potential suicide victims. To achieve this goal, suicide prevention strategies require the identification of specific therapeutic targets. Using this approach, patients at risk of suicide could benefit from specific treatments, the prerequisite being to consider suicidal behaviour (SB) as a specific disorder.11
Suicidal behavior as a specific disorder
Epidemiological and clinical data led to the proposition of a stress vulnerability model for suicidal behavior.12 Indeed, from psychological autopsy studies, we know that virtually all subjects who completed suicide were suffering from a psychiatric disorder at the time of their suicide. We also know from the notes left by these subjects before their death, that environmental stresses are common triggers of suicidal behavior. However, only a minority of individuals who are faced with such adversities, resort to suicidal behavior. In this model, it is postulated that among people suffering from a psychiatric disorder and submitted to stressful life events, those who attempt suicidal acts have a specific vulnerability. One indicator of such vulnerability is the fact that the main risk factor of a suicidal behavior is the existence of a history of suicide attempts.
To summarize findings from both cross sectional and longitudinal studies, the vulnerability to suicidal behavior is associated with a personal and a family history of suicidal behavior, the existence of childhood maltreatment, and personality traits related to both impulsive aggression and hopelessness.13
Very strong support of the vulnerability stress model has come from the widely replicated findings showing that a serotonergic dysfunction is a trait marker of suicidal behavior.14 Recently, by using the neuroscientific toolbox, it has been possible to add evidence of a specific neurobiological vulnerability to suicidal behavior. Over the last 15 years, molecular genetic studies have identified a number of genetic polymorphisms associated with suicidal behavior, mainly modulating the effect of life stresses or childhood abuse.15,16
Neuropsychology and brain imaging are valuables tools to investigate in vivo brain functioning. Understanding cognitive dysfunctions and their underlying neural basis can shed light on the pathophysiology of vulnerability to SB. In a series of studies, we found that decision-making impairment was a cognitive vulnerability trait of SB, independently from any psychiatric disorders.17 Moreover, decision-making is modulated by serotonergic genotypes associated with the vulnerability to SB, and related to a dysfunction of the orbitofrontal cortex.18 According to the somatic marker hypothesis,19 an electrodermal response, reflecting the emotional arousal, is necessary to guide decision-making in healthy subjects.20
In the first fMRI study in SB, we found that in comparison to male patients with no history of suicide attempts, male suicide attempters had higher activation of the right orbito-frontal cortex in response to viewing angry vs neutral faces.21 These data, together with those from other brain imaging studies, suggest that the orbitofrontal region may play a key role in the vulnerability to SB, mediating the involvement of emotional dysregulation.
Based on these findings, a general model has been proposed postulating that interactions between genes and childhood abuse alter the functioning of the serotonergic system and HPA axis. These biochemical impairments translate into personality traits related to impulsive aggression, neuroticism or hopelessness, which confer vulnerability to SB that is expressed in the context of aversive events.
The demonstration of the existence of psychobiological abnormalities involved in vulnerability to SB, independent of related psychiatric disorders, led to a historic turning point in suicidology. Indeed, foremost researchers in the field have advocated considering SB as an entity per se in the psychiatric nosology. Indeed, there is now robust evidence that SB conforms well to the criteria proposed by Robins and Guze22 for establishing the validity of clinical syndromes.11 In a further step, Oquendo et al23 recently recommended “that suicidal behavior be considered a separate diagnostic category” in the future version of the Diagnostic and Statistical Manual of Mental Disorders. Their proposal would be advantageous to patients, since “practically, an axis for suicidal acts would compel clinical and administrative structures to determine the suicide risk status of individuals assessed in psychiatric settings”.
Do antidepressants increase the risk of suicide?
Antidepressant therapy, which is effective in managing the symptoms of major depressive disorder, is expected to reduce or prevent suicidal behavior associated with depression.24 Recent randomized controlled trials have, however, raised some doubt as to whether antidepressants do, in fact, reduce suicidal thoughts and behaviors.25,26 Reports of higher rates of suicide-related adverse events during treatment with selective serotonin reuptake inhibitors (SSRIs) and other antidepressants compared to placebo have prompted regulatory bodies in the US and Europe to issue warnings alerting clinicians to the risk of suicide during the first weeks of antidepressant treatment.27,28 These warnings have had an impact on antidepressant prescribing and may have paradoxically increased the risk of suicide in the depressed population.29
A recent meta-analysis30 of 372 double-blind, randomized, placebo-controlled trials involving a total of 99,231 adults revealed a favorable benefit-risk ratio for treating depressed patients with antidepressants with the possible exception of those under 25 years of age. The study found that the odds ratio for suicidality (ideation or worse) was significantly less with antidepressants than with placebo. When the data were analyzed by age, all age groups had a reduced risk with antidepressants with the single exception of patients under 25 years in whom there was a tendency for an increased risk of suicidality compared to placebo.
Thus the most recent evidence suggests a favorable benefit-risk ratio for treating depressed patients with antide-pressants with the possible exception of those under 25 years of age. Nevertheless patients should be carefully assessed during treatment, especially during the first weeks of treatment when an activation syndrome may increase suicidal risk in some patients with certain antidepressants.
A study investigating the effect of milnacipran on suicidality
In the light of this controversy, the effect of an antidepressant on suicidal ideation clearly remains an important question. Thus, a recent Russian study,31 in addition to assessing the general efficacy and tolerability of milnacipran (Ixel®), a serotonin and norepinephrine reuptake inhibitor (SNRI)32 recently introduced into Russia, investigated the effects of the drug on the occurrence and intensity of suicidal thoughts and behavior in patients with mild to moderate depressive disorders.
Of the 30 patients enrolled in the study, 60% had a diagnosis of a single depressive episode and the majority (86.6%) were moderately depressed with baseline Hamilton depression rating score (HDRS17) of 23.9 ± 1.8 and Beck depression inventory score (BDI) of 37.7 ± 3.9.
No patients had made any previous suicidal attempts and at baseline no plans or preparation for suicide were noted. Suicidal ideation was observed, however, in 14 patients (46.7%). The mean baseline level of suicidality, as indicated by Beck Scale for Suicidal ideation (BSS),33 was 4.9 ± 4.9, indicating a mild level of suicidality. A total of 57 suicidal manifestations were recorded throughout the study (Table 1). The most were thoughts of “inanity of existence (life has no meaning)”, thoughts that death could resolve existing sufferings, suicidal thoughts and unwillingness to live.
Table 1.
Suicidal manifestations (thoughts and behavior) reported during the study
| Number of patients reportinga | % Of all reported suicidal thoughts and behavior | |
|---|---|---|
| Thoughts of inanity of existence | 11 | 19.4 |
| Thoughts of death | 9 | 15.8 |
| Thoughts of suicide | 7 | 12.3 |
| Unwillingness to live | 6 | 10.5 |
| Visions of suicide | 5 | 8.8 |
| Visions of death | 4 | 7.0 |
| Visions of funerals | 4 | 7.0 |
| Death instinct | 4 | 7.0 |
| Suicidal fantasies | 2 | 3.5 |
| Compulsive thoughts of suicide | 2 | 3.5 |
| Compulsive thoughts of funerals | 2 | 3.5 |
| Compulsive thoughts death | 1 | 1.7 |
Some patients reported more than one suicidal manifestations.
More rarely, other signs of suicidality were reported such as visualization of one’s own suicide, death or funeral, as well as a supraliminal death instinct. Only in a few patients did these suicidal ideations develop into either compulsive thoughts of death and funerals or suicidal fantasies.
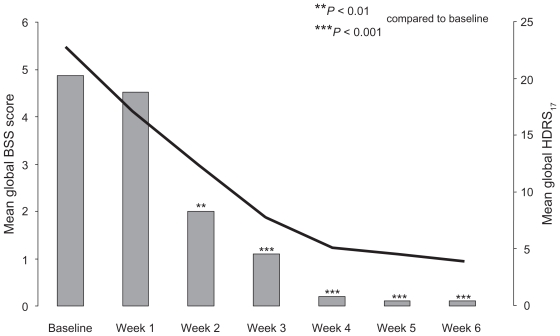
Milnacipran was administered for 2 to 3 days, at 25 to 50 mg/day depending on the severity of depressive symptoms and then increased to 100 mg/day (50 mg twice daily). The antidepressant efficacy of the milnacipran treatment was demonstrated by the steady reduction of the mean HDRS17 score throughout the study (Figure 1). Statistically significant differences compared to baseline occurred from the first week of therapy. At endpoint (after 6 weeks of treatment) mean HDRS17 was 9.5 ± 4.4 with 60% of patients classified as treatment responders (reduction of baseline HDRS17 of at least 50%).
Figure 1.
Parallel reduction of depressive symptoms and suicidality during the study.
**P< 0.01; ***P< 0.001 compared to baseline values.
Note: Solid black line, mean global HDRS17 scores; Gray column, mean global BSS scores.
Suicidality as measured by the BSS decreased rapidly with a significant reduction observed from the second week of treatment (Figure 1). After 4 weeks of treatment, mean BSS scores were close to zero indicating a virtual absence of suicidality in treated patients. None of the patients showed any increase, even transitory, in BSS score during milnacipran treatment indicating an absence of any “activation syndrome”, sometimes observed at the early stages of therapy with certain antidepressants.8 Even the occurrence in some patients of anxiety as an adverse event during milnacipran therapy did not negatively affect the general suicidality of these patients.
Analysis of the “suicidal thoughts/attempts” item of the HDRS17 (item 3) at baseline showed a score of 1 in 10 patients (33.3%) and of 2 in one patient. The number of patients with scores 1 or 2 decreased progressively throughout the study. At endpoint only 3 patients had a score of 1.
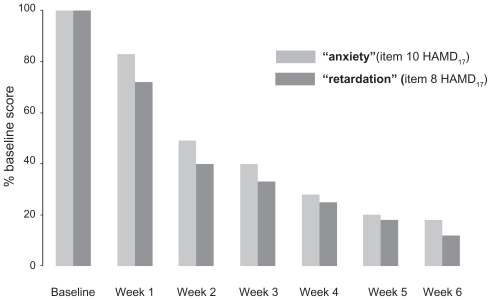
The HDRS17 items of “psychic anxiety” (item 10) and “retardation” (item 8) showed a similar and parallel progressive reduction throughout the study (Figure 2). At the end of the study anxiety was reduced by 82% and retardation by 88%. The fact that the anxiety/retardation ratio remained approximately constant during milnacipran therapy probably explains the absence of any “activation syndrome”.
Figure 2.
Reduction of mean “anxiety” and “retardation” scores during the study.
The wide prevalence of different suicidal manifestations in patients with mild to moderate depressive disorders shown in this study is important since, even in absence of a behavioral component, suicidal manifestations are a powerful predictor of future suicidal behavior.24,34
A meta-analysis of suicidal behaviors and ideation in clinical trials in depression with another SNRI, duloxetine, has also demonstrated the absence of any increased risk of suicidal behaviors or ideation during treatment with the SNRI compared with placebo.35
Discussion
Since major depression is present in at least 60% of patients who completed suicides, it seems reasonable to propose that a major objective in suicide prevention is related to the adequate treatment of depression.36 In a recent pharmaco-epidemiological study, the authors estimated that prescribing antidepressants to all patients diagnosed with depression would prevent more than one out of three suicide deaths compared to the no antidepressants strategy, irrespective of age, gender or parasuicide history.37 However, a controversial issue concerning the potential risk of suicide associated with antidepressants generated numerous papers in the media and in the scientific literature. The consensual position that has emerged considers that a very careful assessment of suicide risk has to be performed before and after the initiation of the antidepressant. This improvement in quality of care should help to detect patients at risk, and to detect a potential emergence of suicidal risk particularly within the first weeks after the initiation of the antidepressant drug. Even if specific profiles of antidepressant drugs have to be investigated regarding this specific risk, the emergence or aggravation of suicidal risk may be conceptualized as an interaction between a specific antidepressant and a specific patient. In recent studies from the STAR*D and the GENDEP cohorts, it has been reported that depressed patients presenting an emergence of suicidal ideation when treated with antidepressants carried specific genetic polymorphisms of CREB, glutamate related genes, BDNF, NTRK2.38–40 Moreover, in an imaging genetics study, Perlis et al41 found that in healthy volunteers, the polymorphism of CREB associated with this specific suicidal phenotype was modulating the insular activity in aversive conditions. These data are promising as they complete the identification of vulnerability markers of suicidality, in this case in specific condition of antidepressant treatments, and because they emphasize the role of the ventromedial prefrontal cortex-related regions in the neuroanatomy of SB.
Studies should be performed using these specific biomarkers in the development of new drugs, in order to investigate potential preventive effects on suicidal behavior, as well as potential deleterious effects.
Footnotes
Disclosure
The author declares no conflicts of interest.
References
- 1.World Health Organization. SDR, suicide and self inflicted injury all ages per 100000, last available (2001–2003) WHO, European health for all database (HFA-DB) 2004 [Google Scholar]
- 2.World Health Organization – Suicide prevention (SUPRE) http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/print.html.
- 3.World Health Organization. Suicide huge but preventable public health problem, says WHO. http://www.who.int/mediacentre/news/releases/2004/pr61/en/
- 4.Henriksson S, Boethius G, Isacsson G. Suicides are seldom prescribed antidepressants: findings from a prospective prescription database in Jamtland county, Sweden, 1985–1995. Acta Psychiatr Scand. 2001;103(4):301–306. doi: 10.1034/j.1600-0447.2001.00276.x. [DOI] [PubMed] [Google Scholar]
- 5.Lonnqvist JK, Henriksson MM, Isometsa ET, et al. Mental disorders and suicide prevention. Psychiatry Clin Neurosci. 1995;49(Suppl 1):S111–116. doi: 10.1111/j.1440-1819.1995.tb01912.x. [DOI] [PubMed] [Google Scholar]
- 6.Goodwin FK, Jamison KR. Manic-Depressive Illness. New York: Oxford University Press; 1990. [Google Scholar]
- 7.Inskip HM, Harris EC, Barraclough B. Lifetime risk of suicide for affective disorder, alcoholism and schizophrenia. Br J Psychiatry. 1998;172:35–37. doi: 10.1192/bjp.172.1.35. [DOI] [PubMed] [Google Scholar]
- 8.Culpepper L, Davidson JR, Dietrich AJ, et al. Suicidality as a possible side effect of antidepressant treatment. J Clin Psychiatry. 2004;65(6):742–749. doi: 10.4088/jcp.v65n0603. [DOI] [PubMed] [Google Scholar]
- 9.Savitz JB, Cupido CL, Ramesar RS. Trends in suicidology: personality as an endophenotype for molecular genetic investigations. PLoS Med. 2006;3(5):e107. doi: 10.1371/journal.pmed.0030107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kessler RC, Berglund P, Borges G, et al. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- 11.Leboyer M, Slama F, Siever L, Bellivier F. Suicidal disorders: a nosological entity per se? Am J Med Genet C Semin Med Genet. 2005;133C(1):3–7. doi: 10.1002/ajmg.c.30040. [DOI] [PubMed] [Google Scholar]
- 12.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156(2):181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 13.Oquendo MA, Galfalvy H, Russo S, et al. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry. 2004;161(8):1433–1441. doi: 10.1176/appi.ajp.161.8.1433. [DOI] [PubMed] [Google Scholar]
- 14.Asberg M, Thorén P, Träskman L, et al. “Serotonin depression” – a biochemical subgroup within the affective disorders? Science. 1976;191(4226):478–480. doi: 10.1126/science.1246632. [DOI] [PubMed] [Google Scholar]
- 15.Courtet P, Jollant F, Castelnau D, et al. Suicidal behavior: relationship between phenotype and serotonergic genotype. Am J Med Genet C Semin Med Genet. 2005;133C(1):25–33. doi: 10.1002/ajmg.c.30043. [DOI] [PubMed] [Google Scholar]
- 16.Perroud N, Courtet P, Vincze I, et al. Interaction between BDNF Val66Met and childhood trauma on adult’s violent suicide attempt. Genes Brain Behav. 2008;7(3):314–322. doi: 10.1111/j.1601-183X.2007.00354.x. [DOI] [PubMed] [Google Scholar]
- 17.Jollant F, Bellivier F, Leboyer M, et al. Impaired decision making in suicide attempters. Am J Psychiatry. 2005;162(2):304–310. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- 18.Jollant F, Buresi C, Guillaume S, et al. The influence of four serotonin-related genes on decision-making in suicide attempters. Am J Med Genet B Neuropsychiatr Genet. 2007;144B(5):615–624. doi: 10.1002/ajmg.b.30467. [DOI] [PubMed] [Google Scholar]
- 19.Damasio AR. Descartes’ error and the future of human life. Sci Am. 1994;271(4):144. doi: 10.1038/scientificamerican1094-144. [DOI] [PubMed] [Google Scholar]
- 20.Guillaume S, Jollant F, Jaussent I, et al. Somatic markers and explicit knowledge are both involved in decision-making. Neuropsychologia. 2009;47(10):2120–2124. doi: 10.1016/j.neuropsychologia.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 21.Jollant F, Lawrence NS, Giampietro V, et al. Orbitofrontal cortex response to angry faces in men with histories of suicide attempts. Am J Psychiatry. 2008;165(6):740–748. doi: 10.1176/appi.ajp.2008.07081239. [DOI] [PubMed] [Google Scholar]
- 22.Robins E, Guze SB. Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry. 1970;126(7):983–987. doi: 10.1176/ajp.126.7.983. [DOI] [PubMed] [Google Scholar]
- 23.Oquendo MA, Baca-García E, Mann JJ, Giner J. Issues for DSM-V: suicidal behavior as a separate diagnosis on a separate axis. Am J Psychiatry. 2008;165(11):1383–1384. doi: 10.1176/appi.ajp.2008.08020281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Isacsson G. Suicide prevention – a medical breakthrough? Acta Psychiatr Scand. 2000;102(2):113–117. doi: 10.1034/j.1600-0447.2000.102002113.x. [DOI] [PubMed] [Google Scholar]
- 25.Fergusson D, Doucette S, Glass KC, et al. Association between suicide attempts and selective serotonin reuptake inhibitors: systematic review of randomised controlled trials. BMJ. 2005;330(7488):396. doi: 10.1136/bmj.330.7488.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gunnell D, Saperia J, Ashby D. Selective serotonin reuptake inhibitors (SSRIs) and suicide in adults: meta-analysis of drug company data from placebo controlled, randomised controlled trials submitted to the MHRA’s safety review. BMJ. 2005;330(7488):385. doi: 10.1136/bmj.330.7488.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization – Suicide Prevention in Europe. The WHO European monitoring survey on national suicide prevention programmes and strategies. http://www.euro.who.int/document/E77922.pdf.
- 28.Food and Drug Administration. Clinical review: relationship between antidepressant drugs and suicidality in adults. http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4272b1-01-FDA.pdf.
- 29.Valuck RJ, Libby AM, Orton HD, Morrato EH, Allen R, Baldessarini RJ. Spillover effects on treatment of adult depression in primary care after FDA advisory on risk of pediatric suicidality with SSRIs. Am J Psychiatry. 2007;164(8):1198–1205. doi: 10.1176/appi.ajp.2007.07010007. [DOI] [PubMed] [Google Scholar]
- 30.Stone M, Laughren T, Jones ML, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ. 2009;11(339):b2880. doi: 10.1136/bmj.b2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Avedisova A, Borodin V, Zakharova K, Aldushin A. Effect of milnacipran on suicidality in patients with mild to moderate depressive disorder. Neuropsychiatr Dis Treat. 2009;5:415–420. doi: 10.2147/ndt.s5467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stahl SM, Grady MM, Moret C, Briley M. SNRIs: their pharmacology, clinical efficacy, and tolerability in comparison with other classes of antidepressants. CNS Spectr. 2005;10(9):732–747. doi: 10.1017/s1092852900019726. [DOI] [PubMed] [Google Scholar]
- 33.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47(2):343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 34.Brådvik L, Berglund M. Suidical ideation in severe depression. Eur Arch Psychiatry Clin Neurosci. 2000;250(3):139–143. doi: 10.1007/s004060070030. [DOI] [PubMed] [Google Scholar]
- 35.Acharya N, Rosen AS, Polzer JP, et al. Duloxetine: meta-analyses of suicidal behaviors and ideation in clinical trials for major depressive disorder. J Clin Psychopharmacol. 2006;26(6):587–594. doi: 10.1097/01.jcp.0000246216.26400.db. [DOI] [PubMed] [Google Scholar]
- 36.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 37.Cougnard A, Verdoux H, Grolleau A, et al. Impact of antidepressants on the risk of suicide in patients with depression in real-life conditions: a decision analysis model. Psychol Med. 2009;39(8):1307–1315. doi: 10.1017/S003329170800473X. [DOI] [PubMed] [Google Scholar]
- 38.Perlis RH, Purcell S, Fava M, et al. Association between treatment-emergent suicidal ideation with citalopram and polymorphisms near cyclic adenosine monophosphate response element binding protein in the STAR*D study. Arch Gen Psychiatry. 2007;64(6):689–697. doi: 10.1001/archpsyc.64.6.689. [DOI] [PubMed] [Google Scholar]
- 39.Laje G, Paddock S, Manji H, et al. Genetic markers of suicidal ideation emerging during citalopram treatment of major depression. Am J Psychiatry. 2007;164(10):1530–1538. doi: 10.1176/appi.ajp.2007.06122018. [DOI] [PubMed] [Google Scholar]
- 40.Perroud N, Aitchison KJ, Uher R, et al. Genetic predictors of increase in suicidal ideation during antidepressant treatment in the GENDEP project. Neuropsychopharmacology. 2009;34(12):2517–2528. doi: 10.1038/npp.2009.81. [DOI] [PubMed] [Google Scholar]
- 41.Perlis RH, Holt DJ, Smoller JW, et al. Association of a polymorphism near CREB1 with differential aversion processing in the insula of healthy participants. Arch Gen Psychiatry. 2008;65(8):882–892. doi: 10.1001/archgenpsychiatry.2008.3. [DOI] [PMC free article] [PubMed] [Google Scholar]