Abstract
Context:
Although the number of US ice hockey participants doubled from 1990 to 2006, no nationally representative studies have examined US ice hockey injuries among participants of all ages during this period.
Objective:
To describe patients with ice hockey injuries presenting to a representative sample of US emergency departments (EDs) from 1990 through 2006.
Design:
Prospective injury surveillance study.
Setting:
The US Consumer Product Safety Commission collects data from 100 nationally representative EDs via the National Electronic Injury Surveillance System (NEISS).
Patients or Other Participants:
Individuals injured while playing ice hockey and presenting to a NEISS-affiliated ED from 1990 through 2006.
Main Outcome Measure(s):
Incidence and patterns of ice hockey–related injuries.
Results:
From 1990 through 2006, 8228 patients with ice hockey–related injuries presented to NEISS-affiliated EDs, representing an estimated 302 368 ice hockey–related injuries sustained nationally during this time. Injuries occurred predominantly among males (93.5%). More than half of the injured were aged 9 to 14 years (28.9%) or 15 to 18 years (30.1%), and injury incidence in these age groups increased over the study period (P = .009 and P < .001, respectively). The most commonly injured body sites were the face (19.1%), wrist/hand/finger (14.1%), shoulder/upper arm (13.8%), and lower leg/ankle/foot (11.1%). Lacerations (27.0%), contusions/abrasions (23.6%), fractures (17.3%), and sprains/strains (16.9%) were the most common injuries. Falls (16.5%), contact with boards (13.6%), and contact with stick (13.0%) were the most common injury mechanisms. Compared with those aged 9 to 18 years, those aged 2 to 8 years and those older than 18 years sustained larger proportions of face (injury proportion ratio [IPR] = 2.66; 95% confidence interval [CI] = 2.29, 3.08) and mouth (IPR = 4.34; 95% CI = 2.87, 6.56) injuries. Concussions were more common among those aged 2 to 18 years (9.0%) than in those who were older than 18 years (3.7%) (IPR = 2.47; 95% CI = 1.75, 3.49).
Conclusions:
Ice hockey injury patterns vary by age and sex. Our findings indicate that many trips to the ED might be prevented by using protective equipment appropriately.
Keywords: epidemiology, injury surveillance, face shields, mouth guards, body checking
Key Points.
Ice hockey injury patterns varied with age and sex.
Emergency department visits for ice hockey injuries might be reduced if players use appropriate protective equipment that is effective and relatively inexpensive and that does not hinder athletic performance.
Ice hockey is an exciting, fast-paced collision sport. Since 1990, the number of participants registered with USA Hockey has more than doubled in the United States, increasing to more than 457 000 in 2006.1 As is the case with other sports, ice hockey offers a number of positive benefits that include improved physical health and increased self-confidence.2 Ice hockey is a unique sport in which players can skate up to 30 mph (48 kph) and hit pucks at speeds up to 100 mph (161 kph),3 with the almost-constant possibility of colliding with another player, the puck, or a rigid wall. To help prevent injury, youth ice hockey participants in organized play are required to wear full-body protective gear (ie, helmet, face mask, mouth guard, shoulder pads, elbow pads, gloves, padded hockey pants, knee pads, and shin guards).4 However, adults and individuals playing recreationally may not wear all of the recommended protective gear.
Past ice hockey injury investigators have addressed age,5–11 sex,5,6,9–11 diagnosis,3,5–9,11–15 mechanism of injury,3,5,6,16,17 and location on the ice.5,6 Although research has been conducted on ice hockey injuries in the United States5,6,12,13,15,18 and globally,8,14,16,17,19 most prior studies were limited to a specific age group,5,6,10,11,18,20,21 to a relatively short (less than 5-year) time period,5,7,9,14,17,18,21,22 or to a relatively small geographic area.17,22 No authors have examined US ice hockey injuries among all ages over an extended period of time.
Our goal was to describe patients with ice hockey injuries presenting to a representative sample of US emergency departments (EDs) from 1990 through 2006. Our specific aims were to (1) calculate nationally estimated injury incidence; (2) describe body site, diagnosis, and mechanism of injury; and (3) compare body site, diagnosis, and mechanism of injury by age and sex. Such important information is needed by team physicians, certified athletic trainers, equipment managers, coaches, parents, and players to develop targeted preventive interventions.
METHODS
The US Consumer Product Safety Commission's (CPSC's) National Electronic Injury Surveillance System (NEISS) collects data from 100 US hospitals.23 At NEISS hospitals (a stratified probability sample of all US hospitals with at least 6 beds and a 24-hour ED), trained coders review all ED records daily and enter demographic, injury-related, and event-related information into the NEISS database. For individuals sustaining multiple injuries, only the most serious injury per event is recorded. Coders also assign 1 or 2 CPSC-specific product codes to each case. These codes designate the products being used or the activities engaged in at the time of injury or both.
We evaluated all cases presenting to NEISS EDs between January 1, 1990, and December 31, 2006, that included an ice hockey product code (code 1279).24 Per NEISS protocol, any ED visit resulting from playing ice hockey or from an ice hockey skate, stick, or puck should receive the 1279 product code. We reviewed each injury's narrative to decide whether the injury occurred during active ice hockey participation. Injuries sustained while not playing ice hockey were excluded (eg, a hockey spectator hit by the puck, an individual who cut his hand while sharpening a skate). No distinction was made between structured (eg, school-sanctioned, travel-team) and unstructured (eg, pond, open-rink) activity. We analyzed age, sex, injured body site, diagnosis, mechanism of injury, and disposition. In order to align with USA Hockey divisions, age was categorized into the following 5 groups: 2 to 8 years, 9 to 14 years, 15 to 18 years, 19 to 29 years, and 30 years or older. The 26 injured body regions recorded by NEISS were grouped into the following categories: head, neck, face, mouth, shoulder/upper arm, elbow/lower arm, wrist/hand/finger, hip/trunk, upper leg/knee, lower leg/ankle/foot, and other/unknown. Injury diagnoses were categorized into laceration, contusion/abrasion, fracture, sprain/strain, concussion, dislocation, dental injury, and other/unknown categories. The concussion category included both injuries that were diagnosed as concussions as well as those that were diagnosed as internal organ injuries with a body site of head. The mechanism that initiated the injury event, ascertained by reading NEISS narratives, was categorized as follows: fall, contact with boards, contact with stick, player-to-player contact, contact with puck, contact with skate, and other/unknown. Disposition was categorized as treated and released or other.
We analyzed data using SPSS (version 15.0; SPSS Inc, Chicago, IL). Unless otherwise stated, incidence and analyses present national estimates calculated by applying CPSC statistical weights that account for the NEISS complex sample design. Linear regression was used to determine statistical significance for injury incidence trends over time. Categorical variables were analyzed via χ2 injury proportion ratios (IPRs) and 95% confidence intervals (CIs), with Pearson χ2 P values of less than .05 considered statistically significant. For example, the following IPR calculation compares the proportion of male and female injuries that were concussions:
The university's Institutional Review Board at The Research Institute at Nationwide Children's Hospital approved this study.
RESULTS
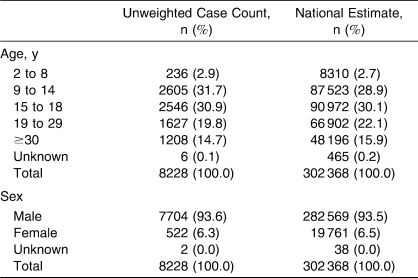
Incidence
From 1990 through 2006, 8228 patients with ice hockey–related injuries presented to NEISS EDs. These 8228 injuries represent an estimated 302 368 (95% CI = 201 239, 403 497) ice hockey–related injuries presenting to EDs nationally during this time period (Table 1). Ice hockey injuries occurred predominantly among males (n = 282 569, 93.5%). The most commonly injured age groups were the 15- to 18-year (n = 90 972, 30.1%), 9- to 14-year (n = 87 523, 28.9%), and 19- to 29-year (n = 66 902, 22.1%) groups.
Table 1.
Patients With Ice Hockey Injuries Presenting to US Emergency Departments by Age and Sex, 1990–2006
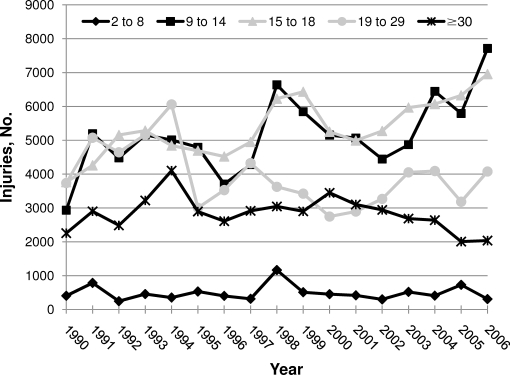
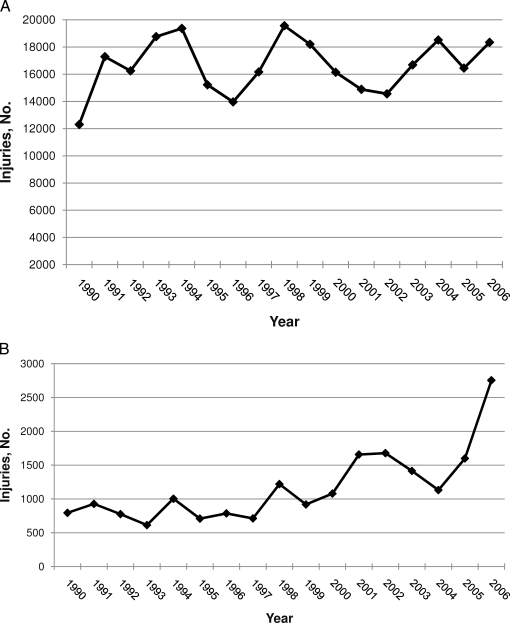
The nationally estimated incidence of ice hockey–related injuries increased from 13 097 in 1990 to 21 092 in 2006, although this change was not statistically significant (P = .147). However, the nationally estimated incidence of ice hockey–related injuries among those aged 9 to 14 years increased 163%, from 2935 (in 1990) to 7713 (in 2006) (P = .009), and the incidence among those aged 15 to 18 years increased 85%, from 3763 (in 1990) to 6957 (in 2006) (P < .001) (Figure 1). Among males, the nationally estimated incidence of ice hockey injuries remained steady at 12 303 (in 1990) and 18 338 (in 2006) (P = .454) (Figure 2A). Among females, the nationally estimated incidence of ice hockey injuries increased 347%, from 794 (in 1990) to 2754 (in 2006) (P < .001) (Figure 2B). Females also made up an increasingly larger proportion of ice hockey–related injuries over time, accounting for 4.8% (n = 8452) of all injuries from 1990 to 1999 and 8.9% (n = 11 308) of all injuries from 2000 to 2006 (P < .001).
Figure 1.
Nationally estimated incidence of patients with ice hockey injuries presenting to US emergency departments by age (y), 1990–2006.
Figure 2.
Nationally estimated incidence of patients with ice hockey injuries presenting to US emergency departments, 1990–2006. A, Males. B, Females. Because of the relatively small number of female cases (n = 522), yearly national estimates should be interpreted with caution.
Overall Injury Characteristics
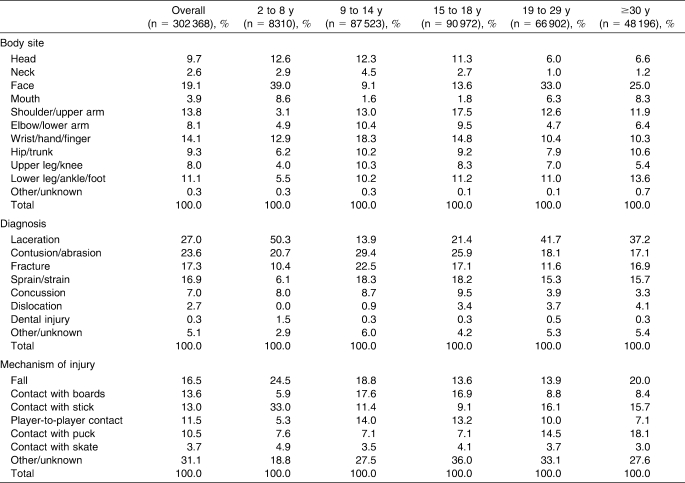
The majority of injuries resulted in the patient being treated and released (n = 296 272, 98.0%). The most commonly injured body sites were the face (n = 57 690, 19.1%), wrist/hand/finger (n = 42 599, 14.1%), shoulder/upper arm (n = 41 713, 13.8%), and lower leg/ankle/foot (n = 33 555, 11.1%) (Table 2). The mouth accounted for 3.9% (n = 11 934) of all injuries. Lacerations (n = 81 548, 27.0%), contusions/abrasions (n = 71 463, 23.6%), fractures (n = 52 219, 17.3%), and sprains/strains (n = 51 031, 16.9%) were the most common injury diagnoses. The most common body site–diagnosis combinations were facial lacerations (n = 49 670, 16.4%), head concussions (n = 21 202, 7.0%), and wrist/hand/finger fractures (n = 17 328, 5.7%). Falls (n = 49 857, 16.5%), contact with boards (n = 41 162, 13.6%), contact with stick (n = 39 358, 13.0%), player-to-player contact (n = 34 939, 11.5%), and contact with puck (n = 31 854, 10.5%) were the most common injury mechanisms. However, 31.1% (n = 94 075) of case narratives did not contain enough information to discern the mechanism of injury.
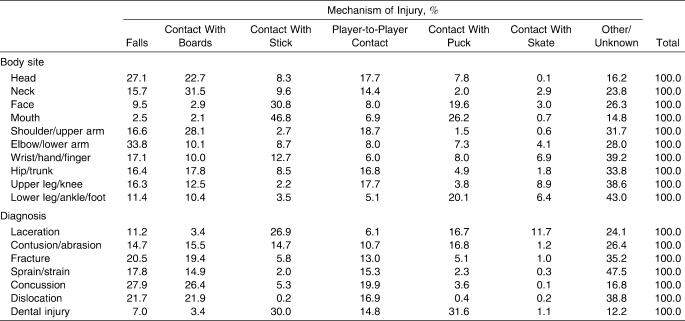
Table 2.
Patients With Ice Hockey Injuries Presenting to US Emergency Departments by Age, 1990–2006: Body Site, Diagnosis, and Mechanism of Injury (n = 302 368)
Falls were the most common mechanism of injury leading to elbow/lower arm (n = 8240, 33.8%), head (n = 7963, 27.1%), and wrist/hand/finger (n = 7286, 17.1%) injuries (Table 3). Neck (n = 2504, 31.5%), shoulder/upper arm (n = 11 703, 28.1%), and hip/trunk injuries (n = 5017, 17.8%) were most often caused by contact with boards. Contact with sticks caused large proportions of mouth (n = 5585, 46.8%) and facial (n = 17 755, 30.8%) injuries. Player-to-player contact was the most common mechanism of upper leg/knee injury (n = 4298, 17.7%), and contact with puck was the most common mechanism of lower leg/ankle/foot injury (n = 6747, 20.1%).
Table 3.
Patients With Ice Hockey Injuries Presenting to US Emergency Departments, 1990–2006: Mechanism of Injury by Body Site and Diagnosis (n = 302 368)
Falls were a common mechanism of concussions (n = 5918, 27.9%), dislocations (n = 1798, 21.7%), fractures (n = 10 696, 20.5%), and sprains/strains (n = 9093, 17.8%). Dental injuries (n = 313, 30.0%) and lacerations (n = 21 954, 26.9%) commonly resulted from contact with the stick, while contusions/abrasions commonly resulted from contact with the puck (n = 12 022, 16.8%).
Age-Specific Injury Characteristics
Body site, diagnosis, and mechanism of injury differed by age. Facial injuries were common among those aged 2 to 8 years (n = 3241, 39.0%), 19 to 29 years (n = 22 080, 33.0%), and 30 years or older (n = 12 034, 25.0%) (Table 2). Those aged 9 to 14 years most commonly injured the wrist/hand/finger (n = 16 005, 18.3%), and those aged 15 to 18 years most commonly injured the shoulder/upper arm (n = 15 934, 17.5%). Compared with those aged 9 to 18 years, those aged 2 to 8 years and older than 18 years sustained larger proportions of face (n = 20 335 [11.4%] and n = 37 355 [30.3%], respectively; IPR = 2.66; 95% CI = 2.29, 3.08; P < .001) and mouth (n = 2982 [1.7%] and n = 8952 [7.3%], respectively; IPR = 4.34; 95% CI = 2.87, 6.56; P < .001) injuries. Neck injuries were more common among those aged 9 to 14 years (n = 3931, 4.5%) compared with all other age groups (n = 3935, 1.8%; IPR = 2.45; 95% CI = 1.87, 3.20; P < .001).
Laceration was the most common injury among those aged 2 to 8 years (n = 4180, 50.3%), 19 to 29 years (n = 27 871, 41.7%), and 30 years or older (n = 17 929, 37.2%). Contusion/abrasion was the most common diagnosis for those aged 9 to 14 years (n = 25 749, 29.4%) and 15 to 18 years (n = 23 586, 25.9%). Lacerations were more common among those aged 2 to 8 years and older than 18 years (n = 49 979, 40.5%) compared with those aged 9 to 18 years (n = 31 570, 17.7%; IPR = 2.29; 95% CI = 2.04, 2.57; P < .001). Concussions were more common among those aged 2 to 18 years (n = 16 905, 9.0%) compared with those who were older than 18 years (n = 4215, 3.7%; IPR = 2.47; 95% CI = 1.75, 3.49; P < .001).
Facial laceration was the most common body site–diagnosis combination among those aged 2 to 8 years (n = 2780, 33.4%), 15 to 18 years (n = 10 915, 12.0%), 19 to 29 years (n = 19 610, 29.3%), and 30 years or older (n = 10 401, 21.6%). Persons aged 9 to 14 years sustained concussions most frequently (n = 7605, 8.7%), followed by wrist/hand/finger fractures (n = 6764, 7.7%).
Falls were the most common injury mechanism for those aged 9 to 14 years (n = 16 448, 18.8%) and 30 years or older (n = 9647, 20.0%). Contact with the boards was the most common injury mechanism for those aged 15 to 18 years (n = 15 341, 16.9%). Contact with sticks was the most common injury mechanism for those aged 2 to 8 years (n = 2740, 33.0%) and 19 to 29 years (n = 10 752, 16.1%). Those aged 2 to 8 years were more likely than participants older than 8 years of age to be injured after contact with the stick (n = 2740 [33.0%] and n = 36 618 [12.5%], respectively; IPR = 2.64; 95% CI = 2.12, 3.29; P < .001) and during falls (n = 2036 [24.5%] and n = 47 736 [16.3%], respectively; IPR = 1.51; 95% CI = 1.16, 1.96; P = .004). Those aged 9 to 18 years were more likely than participants aged 2 to 8 years and participants older than 18 years to be injured by contact with boards (n = 30 784 [17.2%] and n = 10 378 [8.4%], respectively; IPR = 2.05; 95% CI = 1.69, 2.49; P < .001) and player-to-player contact (n = 24 305 [13.6%] and n = 10 552 [8.6%], respectively; IPR = 1.59; 95% CI = 1.26, 2.02; P < .001). Those aged 19 years and older were more likely than younger participants to be injured by contact with a puck (n = 18 846 [16.0%] and n = 13 330 [7.1%], respectively; IPR = 2.25; 95% CI = 1.86, 2.71; P < .001).
Sex-Specific Injury Characteristics
Injury patterns differed by sex. The most commonly injured body sites among males were the face (n = 55 010, 19.5%), shoulder/upper arm (n = 39 922, 14.1%), and wrist/hand/finger (n = 39 301, 13.9%). Females most often sustained head (n = 3942, 19.9%), wrist/hand/finger (n = 3298, 16.7%), and face (n = 2665, 13.5%) injuries. Compared with males, females sustained larger proportions of head injuries (IPR = 2.22; 95% CI = 1.78, 2.77; P < .001), whereas males sustained larger proportions of facial injuries (IPR = 1.44; 95% CI = 1.02, 2.04; P = .031). Males most commonly sustained lacerations (n = 77 740, 27.5%), contusions/abrasions (n = 66 076, 23.4%), and fractures (n = 49 727, 17.6%), whereas females most commonly sustained contusions/abrasions (n = 5387, 27.3%), sprains/strains (n = 3969, 20.1%), and lacerations (n = 3808, 19.3%). Compared with males, females sustained larger proportions of concussions (n = 2775 [14.0%] and n = 18 427 [6.5%], respectively; IPR = 2.15; 95% CI = 1.61, 2.89; P < .001), whereas males sustained larger proportions of fractures (n = 49 727 [17.6%] and n = 2454 [12.4%], respectively; IPR = 1.42; 95% CI = 1.02, 1.97; P = .030). Males most frequently sustained injuries after falls (n = 45 235, 16.0%), contact with boards (n = 38 964, 13.8%), and contact with sticks (n = 37 023, 13.1%). Females most often sustained injuries after falls (n = 4621, 23.4%), contact with puck (n = 2922, 14.8%), and contact with stick (n = 2335, 11.8%). Females sustained a higher proportion of injuries from falls (IPR = 1.46; 95% CI = 1.17, 1.82; P = .001) or from contact with the puck (IPR = 1.44; 95% CI = 1.07, 1.96; P = .021) than did males. Concussions among females most frequently resulted from falls (n = 988, 35.6%), contact with the boards (n = 567, 20.4%), or player-to-player contact (n = 500, 18.0%).
DISCUSSION
In this study, the first long-term assessment of US ice hockey injuries in a broad national sample, we found that more than 20 000 patients with ice hockey injuries presented to US EDs annually. Furthermore, important age-specific and sex-specific differences were evident. The incidence of ice hockey injuries will likely continue to increase, reflecting the sport's growing popularity, unless a concerted effort is made to implement effective, evidence-based preventive interventions. By describing age-specific and sex-specific injury patterns, we highlight areas where targeted interventions are needed.
From 1990 through 2006, the nationally estimated incidence of ice hockey injuries increased 163% among youths aged 9 to 14 years and 85% among youths aged 15 to 18 years. Part of this increase was undoubtedly due to expanding participation. For example, the number of high school students playing ice hockey in school-sanctioned leagues increased 88% from 1990 to 2006,25 with much of this increased participation occurring during the 1990s. High school participation increased only 12% from 2000 to 2006.25 However, we found that injury incidence among 9- to 18-year-olds continued to increase through 2006, seemingly outpacing this modest participation growth. Therefore, other factors must also be contributing to the growing injury incidence. One possibility is that participants are devoting more time to their sport. As ice hockey has grown into a popular US sport, more opportunities may have arisen for aspiring young hockey stars to compete year-round in multiple venues, including school teams, traveling leagues, and pick-up games. Adolescent teams may practice longer and harder or participate in more tournaments. As players develop more quickly, coaches may teach their players advanced skills, such as body checking, at a younger age. Future research is needed to determine whether these possible trends are occurring.
We found that almost 1 in 4 ice hockey injuries were to the face or mouth. Protective equipment use is not currently collected systematically by NEISS. However, when worn appropriately, full face shields and mouth guards have proven16,26–28 effective in preventing the vast majority of face and mouth injuries in ice hockey. Thus, our findings indicate that either protective equipment is not always being worn or that it is being worn improperly. Previous authors29 studying protective equipment use reported that 20% of recreational hockey players used no facial protection at the time of a prior serious injury. Furthermore, reported20,30 mouth-guard use ranges from 13% to 67%. The hockey community must strengthen efforts to encourage the use of full face shields and mouth guards among all players and should consider making such protection required in all venues. Because previous research20 indicates that players are much less likely to wear full face shields and mouth guards during practice, targeted education efforts should focus on the importance of wearing protective equipment at all times. Additionally, targeted education should focus on players 19 years of age and older, in whom injuries were 3 times more likely to affect the face or mouth (compared with players aged 9 to 18 years).
Young children are not immune to face and mouth injuries. We found that such injuries accounted for almost half of all injuries sustained by children aged 2 to 8 years; the most common injury mechanisms were being hit by a stick and falling on the ice. This indicates that younger players may not be wearing appropriate protective gear or that they may be wearing it inappropriately. Parents must keep in mind that even though noncontact activities such as skating and puck handling may seem low risk, the potential for injury by falls or through incidental contact is always present. As indicated in previous research,31 children falling on ice are more likely to sustain a facial injury than are children falling on land, because their hands often slip when they are trying to break the fall. Thus, coaches and athletic trainers should stress to parents and guardians of young children that helmets with full face shields and mouth guards need to be worn every time the players are on the ice, whether during an organized competition or practice or during recreational play. Just as important is instructing players in the proper fit of such equipment.
We found little difference in injury patterns between players aged 9 to 14 years and players aged 15 to 18 years. Their injury profiles reflect previous findings6,7,18,21 in youth, high school, and collegiate ice hockey players, with a high proportion of injuries resulting from body-to-body contact and contact with the boards. The similarity between these age groups' injury profiles is likely due to similar styles of play, because male ice hockey players at the Pee Wee level (ages 11 to 12 years) and above are currently permitted to body check. However, the American Academy of Pediatrics32 recommends a minimum checking age of 15 years. As a result of the high risk of injury from body checking,8 such a change would likely greatly decrease injury incidence among 11- to 14-year-olds. Given that 9- to 14-year-olds accounted for more than one-quarter of all patients with ice hockey–related injuries presenting to EDs, this proposed rule change would likely prevent thousands of ED visits.
The increasing incidence of female ice hockey injuries from 1990 to 2006 reflects the participation growth among US females. Among high school students, female participation increased by a factor of 100 during the study period, from only 74 participants in 1990 to 7350 participants in 2006.25 Interestingly, we found that females sustained a larger proportion of concussions than males. Most concussions among females resulted from falls, person-to-person contact, or contact with the boards. Because women's ice hockey leagues do not allow body checking,33 much of this person-to-person contact was likely incidental.5,22 Ice hockey is still a relatively new sport for females, and many females may not begin playing until their teens or even during adulthood. Thus, teams are often composed of players with vastly different skill levels, skating abilities, and body compositions.5 Coaches previously accustomed to coaching male teams must be cognizant of these differences when coaching females and should focus on developing skating skills among beginning players. As with any player new to the sport, females should be capable of maintaining their balance during complex skating drills before being allowed to compete. As female ice hockey participation continues to grow, it should become easier for leagues to structure competitions between female teams of comparable skill levels.
Our study limitations correspond to the limitations of the NEISS data set. Athletes with ice hockey injuries presenting to EDs represent only the most severe ice hockey injuries, and factors such as age and insurance status may affect the generalizability of ED presentations to all injuries. However, patients with injuries presenting to the ED are an important subgroup. Because NEISS only records the most serious injury per injury event, the true injury incidence is likely higher than that reported here. Although we could not calculate age-specific and sex-specific injury rates because accurate, event-based exposure data do not exist, the incidence data presented here provide useful information. Finally, one-third of all cases had a nondiscernible mechanism of injury. Despite such limitations, these data are the only nationally representative sample of US ice hockey injuries among all players, and the data-set's stability allows changes over time to be monitored. The utility of these data, in the absence of ongoing community-level surveillance systems for ice hockey injuries, is their importance for monitoring injury patterns, identifying risk factors, and driving the development of evidence-based preventive interventions.
In conclusion, this study, an overdue presentation of trends and patterns among all US ice hockey players, found that injury patterns vary by age and sex. Importantly, these findings indicate that many trips to the ED might be prevented by appropriate use of protective equipment. In addition to required protective equipment, we recommend participants wear and appropriately use full face shields, mouth guards, and neck guards because of their minimal cost relative to the severity of injuries they prevent. Simply stated, these pieces of protective equipment are effective, relatively inexpensive, and do not inhibit athletic performance. Future researchers should focus on ways to increase the appropriate use of such equipment. Continued surveillance is warranted to evaluate ice hockey injury trends over time, and future researchers should consider expanding the collection of information related to protective equipment use.
Acknowledgments
We thank the US Consumer Product Safety Commission for providing us with National Electronic Injury Surveillance System data. This study was not supported by any funding agency.
REFERENCES
- 1.USA Hockey. Membership statistics. USA Hockey Web site. http://www.usahockey.com//Template_Usahockey.aspx?NAV=ME_03&ID=29074. Accessed January 20, 2009. [Google Scholar]
- 2.Le Menestrel S., Perkins D. F. An overview of how sports, out-of-school time, and youth well-being can and do intersect. New Dir Youth Dev. 2007;(115):13–25. doi: 10.1002/yd.220. [DOI] [PubMed] [Google Scholar]
- 3.Molsa J., Kujala U., Nasman O., Lehtipuu T. P., Airaksinen O. Injury profile in ice hockey from the 1970s through the 1990s in Finland. Am J Sports Med. 2000;28(3):322–327. doi: 10.1177/03635465000280030701. [DOI] [PubMed] [Google Scholar]
- 4.USA Hockey. 2007–2009 Official rules of ice hockey. USA Hockey Web site. http://www.usahockey.com/uploadedFiles/USAHockey/Menu_Officials/Menu_RulesEquipment/Rulebook%200709.pdf. Accessed April 10, 2008. [Google Scholar]
- 5.Agel J., Dick R., Nelson B., Marshall S. W., Dompier T. P. Descriptive epidemiology of collegiate women's ice hockey injuries: National Collegiate Athletic Association Injury Surveillance System, 2000–2001 through 2003–2004. J Athl Train. 2007;42(2):249–254. [PMC free article] [PubMed] [Google Scholar]
- 6.Agel J., Dompier T. P., Dick R., Marshall S. W. Descriptive epidemiology of collegiate men's ice hockey injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):241–248. [PMC free article] [PubMed] [Google Scholar]
- 7.Emery C. A., Meeuwisse W. H. Injury rates, risk factors, and mechanisms of injury in minor hockey. Am J Sports Med. 2006;34(12):1960–1969. doi: 10.1177/0363546506290061. [DOI] [PubMed] [Google Scholar]
- 8.Hagel B. E., Marko J., Dryden D., et al. Effect of bodychecking on injury rates among minor ice hockey players. CMAJ. 2006;175(2):155–160. doi: 10.1503/cmaj.051531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hostetler S. G., Xiang H., Smith G. A. Characteristics of ice hockey–related injuries treated in US emergency departments, 2001–2002. Pediatrics. 2004;114(6):e661–e666. doi: 10.1542/peds.2004-1565. [DOI] [PubMed] [Google Scholar]
- 10.Wattie N., Cobley S., MacPherson A., Howard A., Montelpare W. J., Baker J. Injuries in Canadian youth ice hockey: the influence of relative age. Pediatrics. 2007;120(1):142–148. doi: 10.1542/peds.2006-2672. [DOI] [PubMed] [Google Scholar]
- 11.Yard E. E., Comstock R. D. Injuries sustained by pediatric ice hockey, lacrosse, and field hockey athletes presenting to United States emergency departments, 1990–2003. J Athl Train. 2006;41(4):441–449. [PMC free article] [PubMed] [Google Scholar]
- 12.Delaney J. S. Head injuries presenting to emergency departments in the United States from 1990 to 1999 for ice hockey, soccer, and football. Clin J Sport Med. 2004;14(2):80–87. doi: 10.1097/00042752-200403000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Delaney J. S., Al-Kashmiri A. Neck injuries presenting to emergency departments in the United States from 1990 to 1999 for ice hockey, soccer, and American football. Br J Sports Med. 2005;39(4):e21. doi: 10.1136/bjsm.2004.015735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Molsa J., Kujala U., Myllynen P., Torstila I., Airaksinen O. Injuries to the upper extremity in ice hockey: analysis of a series of 760 injuries. Am J Sports Med. 2003;31(5):751–757. doi: 10.1177/03635465030310051901. [DOI] [PubMed] [Google Scholar]
- 15.Wennberg R. A., Tator C. H. National Hockey League reported concussions, 1986–87 to 2001–02. Can J Neurol Sci. 2003;30(3):206–209. doi: 10.1017/s0317167100002596. [DOI] [PubMed] [Google Scholar]
- 16.Benson B. W., Rose M. S., Meeuwisse W. H. The impact of face shield use on concussions in ice hockey: a multivariate analysis. Br J Sports Med. 2002;36(1):27–32. doi: 10.1136/bjsm.36.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dryden D. M., Francescutti L. H., Rowe B. H., Spence J. C., Voaklander D. L. Personal risk factors associated with injury among female recreational ice hockey players. J Sci Med Sport. 2000;3(2):140–149. doi: 10.1016/s1440-2440(00)80076-6. [DOI] [PubMed] [Google Scholar]
- 18.Flik K., Lyman S., Marx R. G. American collegiate men's ice hockey: an analysis of injuries. Am J Sports Med. 2005;33(2):183–187. doi: 10.1177/0363546504267349. [DOI] [PubMed] [Google Scholar]
- 19.Biasca N., Wirth S., Tegner Y. The avoidability of head and neck injuries in ice hockey: an historical review. Br J Sports Med. 2002;36(6):410–427. doi: 10.1136/bjsm.36.6.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berry D. C., Miller M. G., Leow W. Attitudes of Central Collegiate Hockey Association ice hockey players toward athletic mouthguard usage. J Public Health Dent. 2005;65(2):71–75. doi: 10.1111/j.1752-7325.2005.tb02789.x. [DOI] [PubMed] [Google Scholar]
- 21.McKnight C. M., Ferrara M. S., Czerwinska J. M. Intercollegiate ice hockey injuries: a three-year analysis. J Athl Train. 1992;27(4):338–343. [PMC free article] [PubMed] [Google Scholar]
- 22.Dryden D. M., Francescutti L. H., Rowe B. H., Spence J. C., Voaklander D. C. Epidemiology of women's recreational ice hockey injuries. Med Sci Sports Exerc. 2000;32(8):1378–1383. doi: 10.1097/00005768-200008000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Consumer Product Safety Commission. The NEISS sample (design and implementation): 1997 to present. http://www.cpsc.gov/neiss/2001d011-6b6.pdf. Accessed January 8, 2009. [Google Scholar]
- 24.Consumer Product Safety Commission. NEISS coding manual. http://www.cpsc.gov/neiss/completemanual.pdf. Accessed January 8, 2009. [Google Scholar]
- 25.National Federation of State High School Associations. NFHS participation figures search. http://www.nfhs.org/custom/participation_figures/default.aspx. Accessed January 14, 2009. [Google Scholar]
- 26.Benson B. W., Mohtadi N. G., Rose M. S., Meeuwisse W. H. Head and neck injuries among ice hockey players wearing full face shields vs half face shields. JAMA. 1999;282(24):2328–2332. doi: 10.1001/jama.282.24.2328. [DOI] [PubMed] [Google Scholar]
- 27.Stuart M. J., Smith A. M., Malo-Ortiguera S. A., Fischer T. L., Larson D. R. A comparison of facial protection and the incidence of head, neck, and facial injuries in Junior A hockey players: a function of individual playing time. Am J Sports Med. 2002;30(1):39–44. doi: 10.1177/03635465020300012001. [DOI] [PubMed] [Google Scholar]
- 28.Woods S. E., Diehl J., Zabat E., Daggy M., Engel A., Okragly R. Is it cost-effective to require recreational ice hockey players to wear face protection? South Med J. 2008;101(10):991–995. doi: 10.1097/SMJ.0b013e3181830d42. [DOI] [PubMed] [Google Scholar]
- 29.Woods S. E., Zabat E., Daggy M., Diehl J., Engel A., Okragly R. Face protection in recreational hockey players. Fam Med. 2007;39(7):473–476. [PubMed] [Google Scholar]
- 30.Neussl A. Mouthguards in the American Hockey League [AHL]. J Dent Hyg. 2008;82(5):44. [PubMed] [Google Scholar]
- 31.Knox C. L., Comstock R. D. Video analysis of falls experienced by paediatric iceskaters and roller/inline skaters. Br J Sports Med. 2006;40(3):268–271. doi: 10.1136/bjsm.2005.022855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Academy of Pediatrics. Committee on Sports Medicine and Fitness. Safety in youth ice hockey: the effects of body checking. Pediatrics. 2000;105(3, pt 1):657–658. doi: 10.1542/peds.105.3.657. [DOI] [PubMed] [Google Scholar]
- 33.USA Hockey. 2007–2009 Official rules of ice hockey. USA Hockey Web site. http://www.usahockey.com/uploadedFiles/USAHockey/Menu_Officials/Menu_RulesEquipment/Rulebook%200709.pdf. Accessed April 10, 2008. [Google Scholar]