Abstract
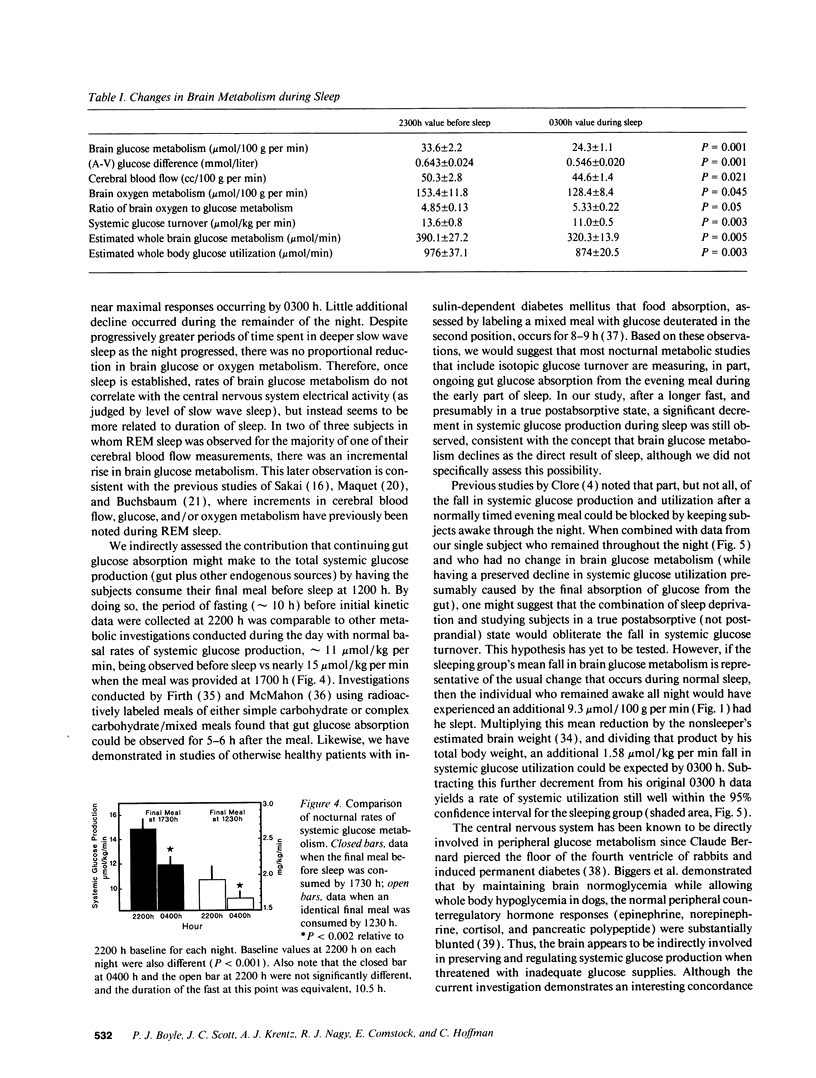
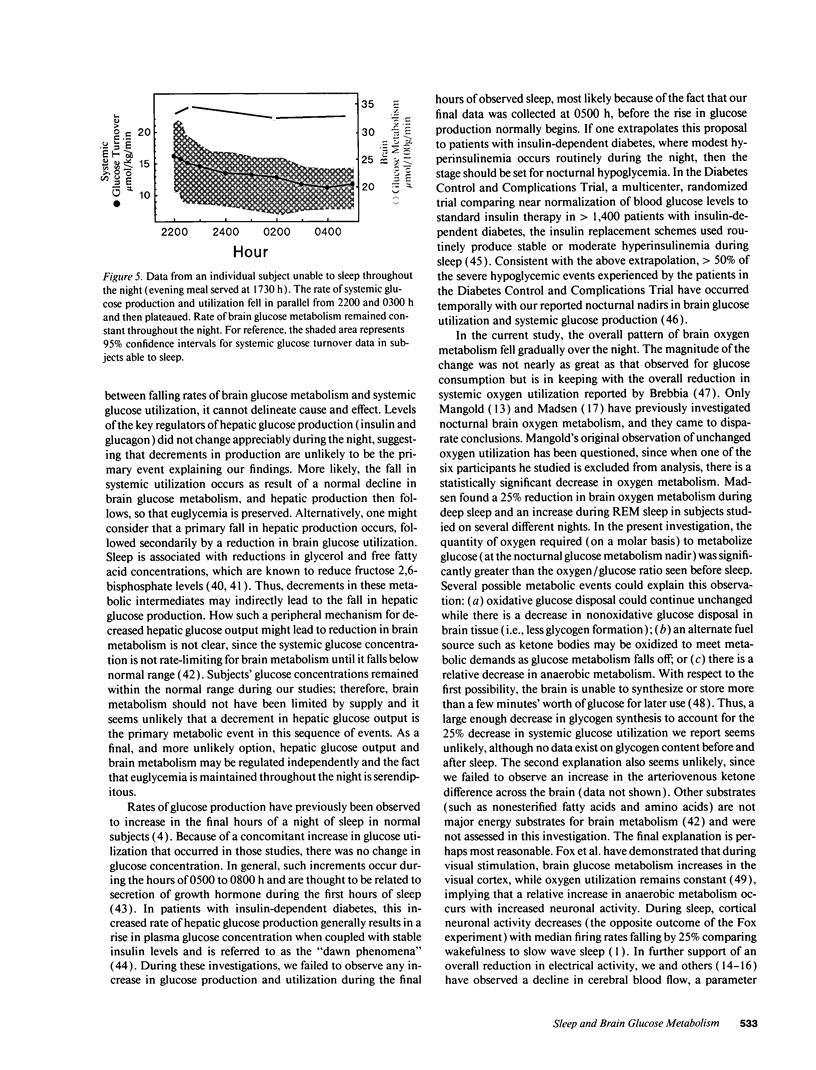
Systemic glucose utilization declines during sleep in man. We tested the hypothesis that this decline in utilization is largely accounted for by reduced brain glucose metabolism. 10 normal subjects underwent internal jugular and radial artery cannulation to determine cerebral blood flow by N2O equilibrium technique and to quantitate cross-brain glucose and oxygen differences before and every 3 h during sleep. Sleep stage was graded by continuous electroencephalogram, and systemic glucose turnover was estimated by isotope dilution. Brain glucose metabolism fell from 33.6 +/- 2.2 mumol/100 g per min (mean +/- SE) before sleep (2300 h) to a mean nadir of 24.3 +/- 1.1 mumol/100 g per min at 0300 h during sleep (P = 0.001). Corresponding rates of systemic glucose utilization fell from 13.2 +/- 0.8 to 11.0 +/- 0.5 mumol/kg per min (P = 0.003). Diminished brain glucose metabolism was the product of a reduced arteriovenous glucose difference, 0.643 +/- 0.024 to 0.546 +/- 0.020 mmol/liter (P = 0.002), and cerebral blood flow, 50.3 +/- 2.8 to 44.6 +/- 1.4 cc/100 g per min (P = 0.021). Brain oxygen metabolism fell commensurately from 153.4 +/- 11.8 to 128.0 +/- 8.4 mumol/100 g per min (P = 0.045). The observed reduction in brain metabolism occurred independent of stage of central nervous system electrical activity (electroencephalographic data), and was more closely linked to duration of sleep. We conclude that a decline in brain glucose metabolism is a significant determinant of falling rates of systemic glucose utilization during sleep.
Full text
PDF




Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Argoud G. M., Schade D. S., Eaton R. P. Underestimation of hepatic glucose production by radioactive and stable tracers. Am J Physiol. 1987 May;252(5 Pt 1):E606–E615. doi: 10.1152/ajpendo.1987.252.5.E606. [DOI] [PubMed] [Google Scholar]
- Biggers D. W., Myers S. R., Neal D., Stinson R., Cooper N. B., Jaspan J. B., Williams P. E., Cherrington A. D., Frizzell R. T. Role of brain in counterregulation of insulin-induced hypoglycemia in dogs. Diabetes. 1989 Jan;38(1):7–16. doi: 10.2337/diab.38.1.7. [DOI] [PubMed] [Google Scholar]
- Boyle P. J., Avogaro A., Smith L., Shah S. D., Cryer P. E., Santiago J. V. Absence of the dawn phenomenon and abnormal lipolysis in type 1 (insulin-dependent) diabetic patients with chronic growth hormone deficiency. Diabetologia. 1992 Apr;35(4):372–379. doi: 10.1007/BF00401205. [DOI] [PubMed] [Google Scholar]
- Boyle P. J., Avogaro A., Smith L., Shah S. D., Cryer P. E., Santiago J. V. Absence of the dawn phenomenon and abnormal lipolysis in type 1 (insulin-dependent) diabetic patients with chronic growth hormone deficiency. Diabetologia. 1992 Apr;35(4):372–379. doi: 10.1007/BF00401205. [DOI] [PubMed] [Google Scholar]
- Boyle P. J., Liggett S. B., Shah S. D., Cryer P. E. Direct muscarinic cholinergic inhibition of hepatic glucose production in humans. J Clin Invest. 1988 Aug;82(2):445–449. doi: 10.1172/JCI113617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle P. J., Shah S. D., Cryer P. E. Insulin, glucagon, and catecholamines in prevention of hypoglycemia during fasting. Am J Physiol. 1989 May;256(5 Pt 1):E651–E661. doi: 10.1152/ajpendo.1989.256.5.E651. [DOI] [PubMed] [Google Scholar]
- Brebbia D. R., Altshuler K. Z. Oxygen consumption rate and electroencephalographic stage of sleep. Science. 1965 Dec 17;150(3703):1621–1623. doi: 10.1126/science.150.3703.1621. [DOI] [PubMed] [Google Scholar]
- Buchsbaum M. S., Gillin J. C., Wu J., Hazlett E., Sicotte N., Dupont R. M., Bunney W. E., Jr Regional cerebral glucose metabolic rate in human sleep assessed by positron emission tomography. Life Sci. 1989;45(15):1349–1356. doi: 10.1016/0024-3205(89)90021-0. [DOI] [PubMed] [Google Scholar]
- Campbell P. J., Bolli G. B., Cryer P. E., Gerich J. E. Pathogenesis of the dawn phenomenon in patients with insulin-dependent diabetes mellitus. Accelerated glucose production and impaired glucose utilization due to nocturnal surges in growth hormone secretion. N Engl J Med. 1985 Jun 6;312(23):1473–1479. doi: 10.1056/NEJM198506063122302. [DOI] [PubMed] [Google Scholar]
- Campbell P. J., Bolli G. B., Cryer P. E., Gerich J. E. Pathogenesis of the dawn phenomenon in patients with insulin-dependent diabetes mellitus. Accelerated glucose production and impaired glucose utilization due to nocturnal surges in growth hormone secretion. N Engl J Med. 1985 Jun 6;312(23):1473–1479. doi: 10.1056/NEJM198506063122302. [DOI] [PubMed] [Google Scholar]
- Clore J. N., Nestler J. E., Blackard W. G. Sleep-associated fall in glucose disposal and hepatic glucose output in normal humans. Putative signaling mechanism linking peripheral and hepatic events. Diabetes. 1989 Mar;38(3):285–290. doi: 10.2337/diab.38.3.285. [DOI] [PubMed] [Google Scholar]
- Firth R. G., Bell P. M., Marsh H. M., Hansen I., Rizza R. A. Postprandial hyperglycemia in patients with noninsulin-dependent diabetes mellitus. Role of hepatic and extrahepatic tissues. J Clin Invest. 1986 May;77(5):1525–1532. doi: 10.1172/JCI112467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox P. T., Raichle M. E., Mintun M. A., Dence C. Nonoxidative glucose consumption during focal physiologic neural activity. Science. 1988 Jul 22;241(4864):462–464. doi: 10.1126/science.3260686. [DOI] [PubMed] [Google Scholar]
- Heiss W. D., Pawlik G., Herholz K., Wagner R., Wienhard K. Regional cerebral glucose metabolism in man during wakefulness, sleep, and dreaming. Brain Res. 1985 Feb 18;327(1-2):362–366. doi: 10.1016/0006-8993(85)91537-9. [DOI] [PubMed] [Google Scholar]
- Hobson J. A., McCarley R. W. Cortical unit activity in sleep and waking. Electroencephalogr Clin Neurophysiol. 1971 Feb;30(2):97–112. doi: 10.1016/0013-4694(71)90271-9. [DOI] [PubMed] [Google Scholar]
- Hue L., Rider M. H. Role of fructose 2,6-bisphosphate in the control of glycolysis in mammalian tissues. Biochem J. 1987 Jul 15;245(2):313–324. doi: 10.1042/bj2450313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy C., Gillin J. C., Mendelson W., Suda S., Miyaoka M., Ito M., Nakamura R. K., Storch F. I., Pettigrew K., Mishkin M. Local cerebral glucose utilization in non-rapid eye movement sleep. Nature. 1982 May 27;297(5864):325–327. doi: 10.1038/297325a0. [DOI] [PubMed] [Google Scholar]
- Kety S. S., Schmidt C. F. THE NITROUS OXIDE METHOD FOR THE QUANTITATIVE DETERMINATION OF CEREBRAL BLOOD FLOW IN MAN: THEORY, PROCEDURE AND NORMAL VALUES. J Clin Invest. 1948 Jul;27(4):476–483. doi: 10.1172/JCI101994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuzuya H., Blix P. M., Horwitz D. L., Steiner D. F., Rubenstein A. H. Determination of free and total insulin and C-peptide in insulin-treated diabetics. Diabetes. 1977 Jan;26(1):22–29. doi: 10.2337/diab.26.1.22. [DOI] [PubMed] [Google Scholar]
- LASSEN N. A., LANE M. H. Validity of internal jugular blood for study of cerebral blood flow and metabolism. J Appl Physiol. 1961 Mar;16:313–320. doi: 10.1152/jappl.1961.16.2.313. [DOI] [PubMed] [Google Scholar]
- Lou H. C., Edvinsson L., MacKenzie E. T. The concept of coupling blood flow to brain function: revision required? Ann Neurol. 1987 Sep;22(3):289–297. doi: 10.1002/ana.410220302. [DOI] [PubMed] [Google Scholar]
- MANGOLD R., SOKOLOFF L., CONNER E., KLEINERMAN J., THERMAN P. O., KETY S. S. The effects of sleep and lack of sleep on the cerebral circulation and metabolism of normal young men. J Clin Invest. 1955 Jul;34(7 Pt 1):1092–1100. doi: 10.1172/JCI103158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madsen P. L., Holm S., Vorstrup S., Friberg L., Lassen N. A., Wildschiødtz G. Human regional cerebral blood flow during rapid-eye-movement sleep. J Cereb Blood Flow Metab. 1991 May;11(3):502–507. doi: 10.1038/jcbfm.1991.94. [DOI] [PubMed] [Google Scholar]
- Madsen P. L., Schmidt J. F., Wildschiødtz G., Friberg L., Holm S., Vorstrup S., Lassen N. A. Cerebral O2 metabolism and cerebral blood flow in humans during deep and rapid-eye-movement sleep. J Appl Physiol (1985) 1991 Jun;70(6):2597–2601. doi: 10.1152/jappl.1991.70.6.2597. [DOI] [PubMed] [Google Scholar]
- Maquet P., Dive D., Salmon E., Sadzot B., Franco G., Poirrier R., von Frenckell R., Franck G. Cerebral glucose utilization during sleep-wake cycle in man determined by positron emission tomography and [18F]2-fluoro-2-deoxy-D-glucose method. Brain Res. 1990 Apr 9;513(1):136–143. doi: 10.1016/0006-8993(90)91099-3. [DOI] [PubMed] [Google Scholar]
- McMahon M., Marsh H., Rizza R. Comparison of the pattern of postprandial carbohydrate metabolism after ingestion of a glucose drink or a mixed meal. J Clin Endocrinol Metab. 1989 Mar;68(3):647–653. doi: 10.1210/jcem-68-3-647. [DOI] [PubMed] [Google Scholar]
- Miller J. C., Horvath S. M. Cardiac output during human sleep. Aviat Space Environ Med. 1976 Oct;47(10):1046–1051. [PubMed] [Google Scholar]
- Pardridge W. M. Brain metabolism: a perspective from the blood-brain barrier. Physiol Rev. 1983 Oct;63(4):1481–1535. doi: 10.1152/physrev.1983.63.4.1481. [DOI] [PubMed] [Google Scholar]
- Ravussin E., Lillioja S., Anderson T. E., Christin L., Bogardus C. Determinants of 24-hour energy expenditure in man. Methods and results using a respiratory chamber. J Clin Invest. 1986 Dec;78(6):1568–1578. doi: 10.1172/JCI112749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson C. S., Narayan R. K., Gokaslan Z. L., Pahwa R., Grossman R. G., Caram P., Jr, Allen E. Cerebral arteriovenous oxygen difference as an estimate of cerebral blood flow in comatose patients. J Neurosurg. 1989 Feb;70(2):222–230. doi: 10.3171/jns.1989.70.2.0222. [DOI] [PubMed] [Google Scholar]
- SCHALCH D. S., PARKER M. L. A SENSITIVE DOUBLE ANTIBODY IMMUNOASSAY FOR HUMAN GROWTH HORMONE IN PLASMA. Nature. 1964 Sep 12;203:1141–1142. doi: 10.1038/2031141a0. [DOI] [PubMed] [Google Scholar]
- Sakai F., Meyer J. S., Karacan I., Derman S., Yamamoto M. Normal human sleep: regional cerebral hemodynamics. Ann Neurol. 1980 May;7(5):471–478. doi: 10.1002/ana.410070514. [DOI] [PubMed] [Google Scholar]
- Sawaya R., Ingvar D. H. Cerebral blood flow and metabolism in sleep. Acta Neurol Scand. 1989 Dec;80(6):481–491. doi: 10.1111/j.1600-0404.1989.tb03915.x. [DOI] [PubMed] [Google Scholar]
- Sherwin R. S. Role of the liver in glucose homeostasis. Diabetes Care. 1980 Mar-Apr;3(2):261–265. doi: 10.2337/diacare.3.2.261. [DOI] [PubMed] [Google Scholar]
- Takahashi Y., Kipnis D. M., Daughaday W. H. Growth hormone secretion during sleep. J Clin Invest. 1968 Sep;47(9):2079–2090. doi: 10.1172/JCI105893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka K., Nicholson W. E., Orth D. N. Diurnal rhythm and disappearance half-time of endogenous plasma immunoreactive beta-MSH (LPH) and ACTH in man. J Clin Endocrinol Metab. 1978 Jun;46(6):883–890. doi: 10.1210/jcem-46-6-883. [DOI] [PubMed] [Google Scholar]
- Townsend R. E., Prinz P. N., Obrist W. D. Human cerebral blood flow during sleep and waking. J Appl Physiol. 1973 Nov;35(5):620–625. doi: 10.1152/jappl.1973.35.5.620. [DOI] [PubMed] [Google Scholar]
- Uyeda K., Furuya E., Richards C. S., Yokoyama M. Fructose-2,6-P2, chemistry and biological function. Mol Cell Biochem. 1982 Oct 18;48(2):97–120. doi: 10.1007/BF00227610. [DOI] [PubMed] [Google Scholar]




