Abstract
Background
Evidence-based interventions have been found effective in increasing colorectal cancer (CRC) screening. Translating these successful interventions into real world settings, such as health plans, can be challenging.
Methods
CHOICE (Communicating Health Options through Information and Cancer Education) is a controlled trial to test the effectiveness of a patient and practice-level intervention to increase use of recommended CRC screening tests. The patient-level intervention was a patient decision aid and stage-targeted brochures, mailed to eligible health plan members, to provide information about CRC,available screening tests, and how to obtain CRC screening at their doctors’ practices. The practice-level intervention was academic detailing to prepare practices to facilitate CRC testing once the patient was activated by the decision aid. Surveys and claims data will be used to assess CRC screening test completion.
Results
Thirty-two primary care practices in Florida and Georgia participated. We recruited 443 participating health plan members for the trial; 211 were patients in intervention practices; 232 were in usual care practices. Study participants reflected an insured population; the majority were white,and less than age 60. We also mailed the intervention to 343 people from intervention practices who did not respond to the eligibility baseline survey. Receipt of screening in that group will be compared to screening among 319 people from usual care practices who did not respond to these surveys using claims data.
Conclusions
The CHOICE study will demonstrate the effect of two combined evidence-based interventions on CRC screening test completion among health plan members.
Keywords: primary prevention, cancer screening, colonic neoplasms, intervention studies, prepaid health plans
INTRODUCTION
Colorectal cancer (CRC) is the third most common cancer diagnosis and the third leading cause of cancer death among men and women living in the United States.1 In 2008, an estimated 148,810 people in the U.S. were diagnosed with CRC, and 49,960 died from the disease.2
Although use of CRC screening has increased since 2002, current screening rates remain modest, with only 60% of age-eligible U.S. adults up-to-date with screening in 2006.2, 3 Another analysis using NHIS survey data indicated that, on average, about 50% of U.S. adults obtained CRC screening within recommended time frames.4 Despite strong evidence and recommendations supporting its use, CRC screening is significantly underutilized.2, 3
Effective and efficient methods to promote colon cancer screening are needed to increase screening utilization in clinical practice and to decrease morbidity and mortality from colon cancer. Further, it is important to test whether interventions that are found efficacious in controlled trials can be translated to less controlled settings, such as health insurance plans.5-9 The CHOICE (Communicating Health Options through Information and Cancer Education) trial tests the effect of a combination of two evidence-based interventions, a decision aid for health plan members and academic detailing for physician practices, on CRC screening test completion by health plan members. This article describes the study design, interventions, and baseline findings.
METHODS
CHOICE is a collaboration between two university research groups (at Emory University and the University of North Carolina) and Aetna's Southeast Region Quality Management Department.
Identification of Potential Participants
This study received IRB approval from Emory University and the University of North Carolina. A partial HIPAA waiver was granted to allow access to information in Aetna's claims data repository for the purposes of identifying eligible health plan members. In addition, a full HIPAA waiver was obtained to send the decision aid intervention to non-responders who were potentially eligible in the intervention group and to permit access to follow-up claims data for non-responders in both the usual care and intervention groups.
Practice Recruitment and Randomization
To identify potential physician practices for participation, the study team obtained from Aetna a list of primary care physicians (family practice, general practice, and internal medicine) in the Atlanta, Tampa, and Orlando areas who participated in the Aetna HMO product. Medical practices recruited to the study had a minimum of 50 Aetna members between 52 and 75 years. Practices were recruited with a mailed introductory packet and telephone follow-up, supplemented with in-person visits, if requested by the practice.
As practices were enrolled into the study, they were grouped into three waves of 10 practices each. The first two waves were randomized into intervention and usual care groups. Randomization was done using matched pairs and a blocking procedure. Practices were matched on the number of study-eligible members per practice and rural vs. urban practices. These variables were chosen, because they may influence the effect of the intervention. When the third wave was recruited, intervention practice groups were unbalanced in practice size. Thus, purposive assignment to treatment group was used, resulting in a hybrid randomization procedure. Two additional practices were not randomized but included. These two practices initially were used as pilot practices (one intervention and one usual care). Because the intervention was not modified, and there were no differences in member characteristics for these two practices, the two practices also were included in the main trial.
Study Population and Recruitment
Potentially eligible participants were identified using claims data from Aetna for members between the ages of 52 and 80 whose primary care physicians had agreed to participate in CHOICE. Members who were not current with CRC screening were eligible for the study. Potentially eligible members were identified by claims data in three waves across 2005 and 2006 as practices were recruited into the study. A final claims extract was obtained in March 2007 to identify newly-eligible members in participating practices and to determine whether any of the eligibility survey non-respondents were no longer eligible for the study due to new medical exclusions. Each extract included data for the current year and the three previous years, which is the time frame contained in the member claims database.
Members were considered up-to-date with screening, and therefore ineligible, if claims data indicated that they had received fecal occult blood testing (FOBT) within the last year or a sigmoidoscopy, colonoscopy or barium enema during the period covered by the claims data. Other exclusions included individuals at increased risk for CRC (because the intervention was designed for average-risk patients) or with medical conditions that would limit their ability to participate in the study or might cause them tobe considered inappropriate candidates for screening and those unable to communicate effectively in English. Above average-risk persons were defined as adults with a personal history of CRC or polyps, a known history of CRC or polyps in a first-degree relative, or a known history of inflammatory bowel disease.
Potentially eligible members identified by claims data were sent a letter and a brief eligibility survey. The eligibility survey was used to obtain information about receipt of CRC screening that might not be in the claims data and to identify people at increased risk for CRC for whom the decision aid would not be appropriate (e.g. persons with a first degree relative with a history of CRC). Members who responded to the eligibility survey and who were eligible were sent a baseline survey . Those who responded to the baseline survey were enrolled.
The primary method of survey administration for health plan members was by mail. However, after two mailings (approximately one month apart), survey non-responders were given the opportunity to complete the surveys by telephone with trained research staff. An internet survey was available for those who preferred to respond online.
Theoretical Foundations of the Interventions
The intervention consisted of a combination of two evidence-based interventions, one targeted at the practice level (academic detailing) and the other at the patient level (decision aid). These two components of the intervention draw upon constructs from Social Cognitive Theory and The Transtheoretical Model or Stages of Change Model.10-12 Academic detailing sessions targeted constructs of collective self-efficacy and strategies of goal-setting and behavioral monitoring.10, 11 The decision aid intervention was based on constructs from the Transtheoretical Model (TTM)12 focusing on the pre-contemplation (not considering being screened), contemplation (considering being screened), and preparation (getting ready to be screened) stages.
Practice-Level Intervention: Academic Detailing
The academic detailing intervention was modeled after previously successful detailing interventions to improve cancer screening in primary care practices.6-9 The goal of detailing was to prepare practices to facilitate CRC testing once patients were activated by the decision aid. Our previous work suggests that practice-level barriers are important barriers to test completion.13
Detailing sessions were led by two of the investigators from UNC (MP, CL) and two general internists at Emory. Academic detailers participated in a three-hour training session where materials and processes for the detailing were reviewed.
Physician academic detailers visited each intervention practice twice during the study, once soon after randomization and again after most patients from the practice had received their decision aids. At the first meeting, the two physician detailers and a research assistant met with participating physicians and support staff. The lead detailing physician gave a fifteen minute presentation to review the burden of colon cancer, current recommendations and screening tests, barriers to colon cancer screening, and previous interventions shown to increase screening test completion in primary care practices. Practice-specific claims-based screening rates were presented to the groups to provide a baseline measure of screening completion. The detailing physicians showed clips from the decision aid.
Detailing physicians then led a discussion about the practice's colon screening strategies, including preferred and available testing options, current office systems to facilitate screening such as reminders, electronic medical records, and whether the office performs in-office flex-sig or FOBT. Referral practices for colonoscopy procedures also were reviewed. Practices were asked to explicitly map current processes for colon cancer screening, including procedures for receiving patient phone calls and scheduling referrals.
During these meetings, detailers led discussions about plans to modify office practices to better accommodate patient requests for specific tests. Physicians and staff from the practice helped to develop a plan in consultation with the physician detailers. Detailers recorded information from the discussion and helped clarify the plan. These written plans were sent to the practices after the meeting for confirmation.
The second session was held after most patient interventions were mailed. The same detailing team returned to practices whenever possible. Detailers reviewed plans with the practices and addressed questions or concerns including any procedural barriers the practices had faced. For two practices, these sessions were conducted over the phone.
To standardize the academic detailing process and assure quality control, standardized notes were taken during detailing sessions, and detailers held a debriefing after each session.
Member-Level Intervention: Decision Aid
The decision aid used in the CHOICE trial is a modified version of a previously tested decision aid, which had been found to be effective at increasing CRC screening rates (Pignone 2000). We refined the content and layout of the decision aid to include web-based interactive delivery. Following these changes, usability testing was performed using cognitive interviewing techniques. The decision aid was produced in DVD and VHS videotape formats to maximize usability by participants.
The duration of the decision aid was about 22 minutes. It included: 1) information on colorectal cancer and screening and 2) information about the specific screening tests and comparative information between tests (e.g efficacy) In the final section of the decision aid, the patient is asked to choose stage-targeted information in the form of a color-coded brochure corresponding to their readiness to be screened.
Decision Aid Mailings and Follow-Up
Decision aids were sent to intervention group members in a package that contained a tailored letter; decision aid with instructions for viewing; stage-targeted brochures; a co-payment and referral information sheet specific to Aetna members; CRC screening options chart; and a decision aid survey. The survey assessed the use of and reactions to the materials, and evaluated perceived changes in knowledge as a result of viewing the decision aid.
Participants in the intervention group who had not been screened as determined by self-report on the one year survey were sent a “booster” intervention. The booster consisted of a letter encouraging screening, information on how to learn more about CRC and CRC screening tests, and an action plan with steps to complete recommended screening tests.
Usual Care Condition
Usual care practices received no academic detailing. All members affiliated with practices in both the intervention and usual care groups received Aetna annual reminders to obtain CRC screening.
Mailings to Non-Responders
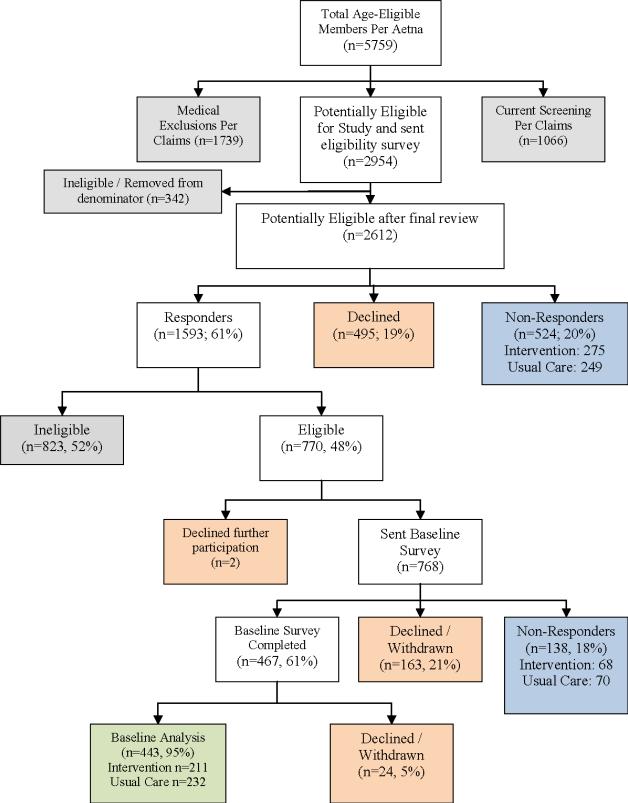
To assess the effect of the intervention in a broader context, decision aid packages were sent to non-responding members in intervention practices. These were health plan members in participating practices who did not respond to either the eligibility survey or the baseline survey but had not refused participation in the study (Figure 1). These members will be included in the intention to treat analyses for CRC screening test completion based on analysis of claims data.
Figure 1.
Consort Diagram of Member Eligibility, Participation and Group Assignment
Data Collection and Measures
Practice level measures
Intervention and usual care practices completed brief surveys to assess their CRC screening practices, referrals, and quality improvement initiatives prior to the intervention and again at the end of the study.
CRC Outcome Measures
We measured completion of CRC screening for health plan members through Aetna claims data and participants self-report. Claims data were assessed for CRC screening test completion for members in both the intervention and usual care groups who had completed the eligibility and baseline surveys, as well as those who did not complete the eligibility and/or baseline surveys but did not refuse participation (Figure 1). We measured CRC screening test completion by participant self-report through the baseline survey and follow-up surveys. Follow-up surveys were sent at 12 months, and at 18 months for those who were unscreened at one year. Interest in CRC screening, intent to ask providers about screening, and readiness to be screened also were assessed on the baseline and follow-up surveys.
Social Cognitive Construct Measures
We measured social cognitive constructs in baseline and follow-up surveys as potential mediating variables. We performed factor analyses on survey items measuring attitudes, beliefs14, and perceptions about colorectal cancer and cancer risk15 in order to group the individual items into discrete dimensions. Factor analyses revealed four clearly delineated composite variables: 1) Perceived Risk of colon cancer (4 items: e.g., what is your chance of getting colon cancer in your lifetime; response was 5 point scale from very low to very high); 2) General Beliefs about colon cancer (4 items: e.g., a person with colon cancer would always have symptoms; response options were 5 point Likert scale from strongly agree to strongly disagree); 3) Fears about colorectal cancer screening (4 items: e.g., I am afraid of having an abnormal screening test result for colon cancer; response options were 5 point Likert scale from strongly agree to strongly disagree); and 4) Intrusive Thoughts about colon cancer (3 items: e.g., during the past month, how often have you thought about your chances of getting colon cancer; response options on 4 point scale of not at all to almost all of the time).
Other social cognitive items measured participants’ knowledge of the age at which CRC screening should begin; perceptions about whether participants had enough information on CRC screening in general, as well as whether they had enough information about specific screening tests, intentions to talk to their doctor about CRC screening (two items), willingness to pay for screening tests16, and desire to participate in medical decisions.17
12 and 18 Month Follow up Surveys
Approximately one year from receipt of baseline surveys, we mailed participants 12-month surveys. Participants who reported that they were not screened at 12 months were sent the 18-Month Survey. Outcome measures and social cognitive construct measures were identical to the baseline survey.
Power Calculations and Statistical Analyses
Our power calculations were based on our expectation that the proportion screened in the intervention group would be 15 percentage points higher than the proportion screened in the usual care group (.40 Intervention Group and .25 Usual Care). This estimate was based on the efficacy trial of the CRC decision aid5 and related research on academic detailing.7, 9 To account for the design, a cluster randomized trial, we assumed a conservative estimate of the intraclass correlation, 0.0225 or less. Based on alpha=.05, a two-tailed test, and power set at 0.80, 10 practices in each arm would have sufficient power to detect a 15 percentage point difference in the proportion screened if at least 25 participants from each practice, or 500 total participants, were enrolled. To ensure a sample of this size, allowing for some practice drop-out and member non-participation, we aimed to recruit at least 30 practices (15 in each group), with each practice having a minimum of 50 Aetna members between the ages of 52 and 75 years.
We will employ an intent-to-treat approach for analyses, using outcome data on recent CRC screening. We will perform two separate analyses. First, we will analyze claims data for all health plan members who were determined to be eligible at the start of the study, and who did not opt-out (and thus received the intervention if their practice was randomized to that treatment group), even if they did not complete survey questionnaires. These analyses will include both active participants and non-respondents in practices participating in the CHOICE trial. Second, we will analyze CRC screening test completion for those who actively enrolled in the trial and completed surveys.
For baseline results in this paper, we report practice and member participation rates. We also report descriptive statistics from members’ eligibility and baseline surveys and the participating practice surveys. We compared demographic characteristics of those who responded to the eligibility survey to those who did not respond or refused, using chi-square tests. We also compared demographic and social cognitive characteristics for intervention and usual care groups using chi-square tests.
RESULTS
Medical Practices
Two hundred forty-two practices in two states (170 in Florida, 72 in Georgia) were approached to participate to obtain our target of 32 practices (15% participation rate). The main reasons given for non-participation in the trial were that the practices were too busy and that they did not want more paperwork. Comparing characteristics of the practices in the intervention and usual care groups revealed equal numbers of practices with electronic medical records (n=6). More practices in the usual care group reported having a CRC reminder system in place than in the intervention group (7 vs. 4) (Table 1).
Table 1.
Comparison of Intervention and Usual Care Practices (n=32)
| Intervention n=16 | Usual Care n=16 | |
|---|---|---|
| State | ||
| Florida | 8 | 9 |
| Georgia | 8 | 7 |
| Total Age-Eligible Aetna Patients | ||
| Mean | 144 | 205 |
| Median | 131 | 74 |
| Number of Primary Care Physicians Per Practice | ||
| 1 | 4 | 6 |
| 2-5 | 9 | 7 |
| > 5 | 3 | 3 |
| Has Electronic Medical Record | 6 | 6 |
| Has CRC Reminder System | 4 | 7 |
During the academic detailing sessions at intervention practices, a variety of office staff attended the sessions, including physicians, nurses, referral coordinators, and schedulers. For physicians, 33 of the 53 (62%) physicians in the intervention group attended the first academic detailing session. For the first sessions, an average of four other staff members attended. For the second detailing sessions, 20 physicians attended and, on average, one other staff member participated. Two of the sessions were conducted by phone because of scheduling difficulties.
Eligible Members by Claims Data
From claims data, we obtained information for 5759 Aetna HMO members (Figure 1). We excluded 1739 people due to high risk factors for CRC or other ineligibility criteria. The most common exclusions, based on claims data, included 1119 people who had previously been treated for cancer, and 495 who had a history of coronary artery disease. Of the remaining 4020 members, 27% (n=1066) were found to be up-to-date with CRC screening.
Eligible Members and Participants
We sent eligibility surveys to the remaining 2954 potentially eligible members to identify those who were ineligible for reasons not captured by the claims data. Among these, 1593 members (61%) returned eligibility surveys, 467 (61%) completed baseline surveys, and, 443 (211 in the intervention group and 232 in the control group) were included in analyses of baseline data.
A total of 662 members did not respond to eligibility surveys (n=524) or baseline surveys (n=138). Among these non-respondents, 343 were patients of intervention practices, of whom 297 were sent intervention materials; 319 were patients in usual care practices.
Group Comparisons
Using information from eligibility surveys, we compared characteristics of those who completed baseline surveys with those who did not respond to baseline surveys or withdrew from further participation (Table 2). The major difference between those who responded and those who did not or refused was race; whites were more likely to participate than Blacks and those of other races (p<0.0001).
Table 2.
Demographic Comparisons of Those Who Responded to Baseline Surveys with Those Who Did Not Respond or Refused
| Responder | Non-Responder | Refuser | P-Value | ||||
|---|---|---|---|---|---|---|---|
| Description | n | Percent | n | Percent | n | Percent | |
| Overall | 443 | 57.5 | 138 | 17.9 | 189 | 24.5 | |
| Gender | |||||||
| Female | 275 | 62.1 | 79 | 57.2 | 122 | 64.6 | 0.40 |
| Male | 168 | 37.9 | 59 | 42.8 | 67 | 35.4 | |
| State | |||||||
| FL | 251 | 56.7 | 77 | 55.8 | 107 | 56.6 | 0.98 |
| GA | 192 | 43.3 | 61 | 44.2 | 82 | 43.4 | |
| Age | |||||||
| 52 to 59 | 336 | 75.8 | 111 | 80.4 | 129 | 68.3 | 0.08 |
| 60 to 64 | 87 | 19.6 | 22 | 15.9 | 42 | 22.2 | |
| 65 to 69 | 16 | 3.6 | 5 | 3.6 | 15 | 7.9 | |
| 70 to 82 | 4 | 0.9 | 0 | 0.0 | 3 | 1.6 | |
| Race | |||||||
| White/Caucasian | 356 | 80.9 | 84 | 60.9 | 140 | 74.5 | <.0001 |
| Black/African-American | 67 | 15.2 | 42 | 30.4 | 32 | 17.0 | |
| Other | 17 | 3.9 | 12 | 8.7 | 16 | 8.5 | |
| Education | |||||||
| High school, GED, or less | 87 | 19.7 | 40 | 29.0 | 48 | 25.5 | 0.23 |
| Some college or technical school | 150 | 33.9 | 49 | 35.5 | 62 | 33.0 | |
| College graduate | 115 | 26.0 | 28 | 20.3 | 42 | 22.3 | |
| Postgraduate or professional degree | 90 | 20.4 | 21 | 15.2 | 36 | 19.1 | |
| Health | |||||||
| Poor/Fair | 41 | 9.3 | 19 | 13.8 | 27 | 14.4 | 0.27 |
| Good | 210 | 47.6 | 56 | 40.6 | 76 | 40.6 | |
| Very good | 136 | 30.8 | 49 | 35.5 | 58 | 31.0 | |
| Excellent | 54 | 12.2 | 14 | 10.1 | 26 | 13.9 | |
| Smoking | |||||||
| No, I never smoked | 199 | 45.0 | 58 | 42.0 | 93 | 49.5 | 0.20 |
| No, but I am a former smoker | 180 | 40.7 | 51 | 37.0 | 63 | 33.5 | |
| Yes | 63 | 14.3 | 29 | 21.0 | 32 | 17.0 | |
Among 443 participants, most were women, white, and less than age 60 (Table 3). The majority had at least some college education, about a third had an income between $50,000 and $100,000. About half reported no chronic illnesses and about half visited the doctor 3 or more times over the last year.
Table 3.
Comparison of Member Characteristics for Intervention and Usual Care
| Overall | Intervention | Usual Care | |||||
|---|---|---|---|---|---|---|---|
| Description | n | % | n | % | n | % | p-value |
| Overall | 443 | 211 | 47.6 | 232 | 52.4 | ||
| Gender | |||||||
| Female | 275 | 62.1 | 128 | 60.7 | 147 | 63.4 | 0.56 |
| Male | 168 | 37.9 | 83 | 39.3 | 85 | 36.6 | |
| Age | |||||||
| 52 to 59 | 336 | 75.8 | 162 | 76.8 | 174 | 75.0 | 0.66 |
| 60 to 82 | 107 | 24.2 | 49 | 23.2 | 58 | 25.0 | |
| Race | |||||||
| White Non-Hispanic | 356 | 80.9 | 160 | 75.8 | 196 | 85.6 | 0.002 |
| Black/African-American | 67 | 15.2 | 45 | 21.3 | 22 | 9.6 | |
| Other | 17 | 3.9 | 6 | 2.8 | 11 | 4.8 | |
| Education | |||||||
| High school, GED, or less | 87 | 19.7 | 43 | 20.4 | 44 | 19.0 | 0.70 |
| Some college or technical school | 150 | 33.9 | 73 | 34.6 | 77 | 33.3 | |
| College graduate | 115 | 26.0 | 57 | 27.0 | 58 | 25.1 | |
| Postgraduate or professional degree | 90 | 20.4 | 38 | 18.0 | 52 | 22.5 | |
| Income | |||||||
| Up to $50,000 | 163 | 37.1 | 75 | 35.7 | 88 | 38.4 | 0.15 |
| Between $50,001 and $100,000 | 148 | 33.7 | 70 | 33.3 | 78 | 34.1 | |
| Over $100,000 | 59 | 13.4 | 36 | 17.1 | 23 | 10.0 | |
| Don't know / Prefer not to answer | 69 | 15.7 | 29 | 13.8 | 40 | 17.5 | |
| State | |||||||
| Florida | 251 | 56.7 | 92 | 43.6 | 159 | 68.5 | <0.001 |
| Georgia | 192 | 43.3 | 119 | 56.4 | 73 | 31.5 | |
| Chronic Illness | |||||||
| 0 | 224 | 50.6 | 102 | 48.3 | 122 | 52.6 | 0.37 |
| 1 or more | 219 | 49.4 | 109 | 51.7 | 110 | 47.4 | |
| Doctor Visits Past Year | |||||||
| 0 times | 45 | 10.6 | 21 | 10.4 | 24 | 10.7 | 0.33 |
| 1-2 times | 174 | 40.8 | 75 | 37.3 | 99 | 44.0 | |
| 3 or more times | 207 | 48.6 | 105 | 52.2 | 102 | 45.3 | |
| Colorectal Cancer Screening History | |||||||
| Yes | 208 | 47.0 | 101 | 47.9 | 107 | 46.1 | 0.71 |
| No | 235 | 53.0 | 110 | 52.1 | 125 | 53.9 | |
| Screened at baseline | |||||||
| Yes | 44 | 9.9 | 22 | 10.4 | 22 | 9.5 | 0.75 |
| No/Unknown | 399 | 90.1 | 189 | 89.6 | 210 | 90.5 | |
| Screening Intentions (among those not screened at baseline, n=399) | |||||||
| Yes | 231 | 57.9 | 114 | 60.3 | 117 | 55.7 | 0.35 |
| No | 168 | 42.1 | 75 | 39.7 | 93 | 44.3 | |
There were some differences at baseline between the intervention and usual care groups, which we expected because we did not allocate at the patient level. Specifically, there were more white patients in the usual care group and more patients in Florida participating in the usual care group. A little less than half in both groups reported ever having received CRC screening on the eligibility survey. When asked again on the baseline survey, 10% in both groups reported screening within the past 3 months since the completing the baseline survey. Among those who did not report recent screening, 60% in the intervention and 56% in the usual care group (P=0.35) reported an intention to undergo screening in the next 6 months
Social Cognitive Factors at Baseline
At baseline, about 75% of participants perceived their CRC risk to be medium to high; most did not report having intrusive thoughts about getting colon cancer (Table 4). Less than half of patients expressed agreement with statements about colon cancer and CRC screening that would denote lower belief in the benefits of CRC screening. Less than half answered the knowledge question correctly. Most reported that they had already talked to their doctors about CRC screening. About 30% reported not having enough information about getting CRC screening and over 40% reported that they did not have enough information on types of screening tests. Approximately 40% expressed concerns about receiving CRC screening. Nearly 40% were willing to pay $200 or more out of their pocket to obtain CRC screening. Comparing the two groups in regard to social cognitive characteristics reveals some differences in general beliefs about colon cancer screening. Patients in the usual care group had a higher level of agreement with statements that indicate lower belief in the benefits of CRC screening, Other characteristics were similar.
Table 4.
Comparison of Social Cognitive Characteristics for Intervention and Usual Care
| Overall | Intervention | Usual Care | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-value | |
| Perceived Risk | |||||||
| Low | 100 | 22.7 | 48 | 23.1 | 52 | 22.4 | 0.79 |
| Medium | 246 | 55.9 | 113 | 54.3 | 133 | 57.3 | |
| High | 94 | 21.4 | 47 | 22.6 | 47 | 20.3 | |
| General Beliefs about CRC screening* | |||||||
| Disagree | 123 | 27.8 | 73 | 34.6 | 50 | 21.6 | 0.01 |
| Neutral | 121 | 27.3 | 51 | 24.2 | 70 | 30.2 | |
| Agree | 199 | 44.9 | 87 | 41.2 | 112 | 48.3 | |
| Fears about screening | |||||||
| Unconcerned | 186 | 42.1 | 93 | 44.3 | 93 | 40.1 | 0.37 |
| Neutral | 83 | 18.8 | 42 | 20.0 | 41 | 17.7 | |
| Concerned | 173 | 39.1 | 75 | 35.7 | 98 | 42.2 | |
| Intrusive Thoughts | |||||||
| Not at all | 296 | 67.1 | 139 | 66.2 | 157 | 68.0 | 0.92 |
| Sometimes | 135 | 30.6 | 66 | 31.4 | 69 | 29.9 | |
| Often | 10 | 2.3 | 5 | 2.4 | 5 | 2.2 | |
| Knowledge of age at which screening is recommended | |||||||
| Correct | 200 | 46.0 | 93 | 45.1 | 107 | 46.7 | 0.74 |
| Incorrect/Don't Know | 235 | 54.0 | 113 | 54.9 | 122 | 53.3 | |
| Medical Decision Preference | |||||||
| Make decision myself | 31 | 7.0 | 17 | 8.1 | 14 | 6.0 | 0.09 |
| Make decision with doctors opinion | 186 | 42.2 | 93 | 44.5 | 93 | 40.1 | |
| Make decision together with doctor | 196 | 44.4 | 82 | 39.2 | 114 | 49.1 | |
| Let doctor decide with my opinion | 18 | 4.1 | 9 | 4.3 | 9 | 3.9 | |
| Let doctor decide | 10 | 2.3 | 8 | 3.8 | 2 | 0.9 | |
| Talk To Doctor | |||||||
| Already talked to Doctor | 245 | 55.3 | 123 | 58.3 | 122 | 52.6 | 0.46 |
| Likely to talk to MD in next 6 months | 79 | 17.8 | 34 | 16.1 | 45 | 19.4 | |
| Unlikely to talk to MD in next 6 months | 119 | 26.9 | 54 | 25.6 | 65 | 28.0 | |
| Enough Information - About getting screening | |||||||
| Yes, definitely | 131 | 29.8 | 64 | 30.8 | 67 | 28.9 | 0.70 |
| Yes, probably | 180 | 40.9 | 87 | 41.8 | 93 | 40.1 | |
| No | 129 | 29.3 | 57 | 27.4 | 72 | 31.0 | |
| Enough Information - Type of screening | |||||||
| Yes, definitely | 97 | 22.1 | 50 | 24.0 | 47 | 20.3 | 0.63 |
| Yes, probably | 160 | 36.4 | 75 | 36.1 | 85 | 36.8 | |
| No | 182 | 41.5 | 83 | 39.9 | 99 | 42.9 | |
| Willingness To Pay | |||||||
| Up to $20.00 | 71 | 16.7 | 39 | 19.4 | 32 | 14.3 | 0.29 |
| $20.01 to $60.00 | 195 | 46.0 | 84 | 41.8 | 111 | 49.8 | |
| $60.01 to $200.00 | 123 | 29.0 | 59 | 29.4 | 64 | 28.7 | |
| More than $200.00 | 35 | 8.3 | 19 | 9.5 | 16 | 7.2 | |
Higher agreement denotes less belief in the benefits of CRC screening.
DISCUSSION
In this paper, we present the methods and baseline findings from the CHOICE (Communicating Health Options through Information and Cancer Education) study. Some aspects of study design, recruitment process, and participants could affect results of the trial and warrant discussion.
First, for the practice intervention, we successfully recruited an adequate number of practices. However, recruitment was more difficult than anticipated. We approached 242 practices approached to enroll 32 practices. As a result, our participating practices may be a select group more interested in colorectal cancer screening than other primary care practices, and are willing to participate in a researh study. If our intervention proves to be successful, our results may not be generalizable to other less motivated practices.
Among practices participating in the study, the usual care and intervention practices appear similar for many of the characteristics we measured. An important difference, however, is that the usual care group has more practices with a CRC reminder system in place. If this difference has an effect, we expect it would bias the results toward the null, because usual care practices may have more effective CRC screening systems in place compared to intervention practices. Additionally, when considering the practice level intervention, not all physicians attended detailing sessions. This could potentially attenuate its effect.
For the member level intervention, our study design was to recruit from an insurance plan. Thus, our results may not be generalizable to the general U.S. population. Furthermore, those members who chose to participate may not reflect the population of insured patients in these two states, especially in regards to colorectal cancer screenings. Most participants believed that screening is beneficial, reported having talked to their doctor about screening and having enough information about the tests. Participants may be more responsive to the patient level intervention than those who did not participate.
We allocated practices based on practice size and surrounding population anticipating that these could have an effect on the intervention. As with any allocation method, there may be unmeasured differences between groups that could affect results. Because we allocated participating members at the practice level, we expected some baseline differences between participants in the intervention and usual care groups. We noted differences with regards to race and state. We will control for these baseline differences in outcomes analyses.
.Finally, our study design could activate both groups to have colon cancer screening. The participant recruitment and data collection process addressed colorectal cancer and could serve as a reminder. Then, it may be more difficult to demonstrate an effect of the intervention, because both groups are activated by the data collection process. To address this, we will compare results for participants in the trial to those who did not participate using claims data. Making this comparison will help us determine extent to which activation occurred
Despite these limitations, the CHOICE trial addresses an important issue, the under-utilization of colorectal cancer screening among a population with health insurance. CHOICE will determine whether two combined evidence-based interventions implemented in community settings increases colorectal cancer screening test completion among health plan members.
Acknowledgements
The authors wish to thank the following for their assistance with the study: Raquel Vazquez, Lauren Taglialatela, Jonathan Hawley, Vicki Whitlatch, Jennifer Griffith, DrPH, Alison Brenner, Murtaza Cassoobhoy, MD, and Lisa Bernstein MD
Grant support: This research was supported by grant number PH000018 from the Centers for Disease Control and Prevention.
Footnotes
Financial disclosures: The authors have no financial disclosures to report
Statement of informed consent: The study received IRB approval to use a combination of a partial HIPAA Waiver for access to claims data, written consent for full participants, and a full HIPAA waiver to access data for non-responders. (See text for details)
REFERENCES
- 1.United States Cancer Statistics: 2004 Incidence and Mortality. US Department of Health and Human Services, CEDC, National Cancer Institute; Atlanta: 2007. [Google Scholar]
- 2.ACS [05/07/2007];How Many People Get Colorectal Cancer? Available from: http://www.cancer.org/docroot/CRI/content/CRI_2_2_1X_How_Many_People_Get_Colorectal_Cancer.asp?sitearea=.
- 3.MMWR Use of colorectal cancer tests--United States, 2002, 2004, and 2006. MMWR Morb Mortal Wkly Rep. 2008 Mar 14;57(10):253–258. [PubMed] [Google Scholar]
- 4.Shapiro JA, Seeff LC, Thompson TD, Nadel MR, Klabunde CN, Vernon SW. Colorectal cancer test use from the 2005 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2008 July;17(7):1623–1630. doi: 10.1158/1055-9965.EPI-07-2838. 2008. [DOI] [PubMed] [Google Scholar]
- 5.Pignone M, Harris R, Kinsinger L. Videotape-based decision aid for colon cancer screening. A randomized, controlled trial. Ann Intern Med. 2000 Nov 21;133(10):761–769. doi: 10.7326/0003-4819-133-10-200011210-00008. [DOI] [PubMed] [Google Scholar]
- 6.Dietrich AJ, Carney PA, Winchell CW, Sox CH, Reed SC. An office systems approach to cancer prevention in primary care. Cancer Pract. 1997 Nov-Dec;5(6):375–381. [PubMed] [Google Scholar]
- 7.Goldstein MG, Niaura R, Willey C, et al. An academic detailing intervention to disseminate physician-delivered smoking cessation counseling: smoking cessation outcomes of the Physicians Counseling Smokers Project. Preventive Medicine. 2003;26:185–196. doi: 10.1016/s0091-7435(02)00018-x. [DOI] [PubMed] [Google Scholar]
- 8.Siegal D, Lopez J, Meier J, et al. Academic detailing to improve antihypertensive prescribing patterns. American Journal of Hypertension. 2003;16:508–511. doi: 10.1016/s0895-7061(03)00060-8. [DOI] [PubMed] [Google Scholar]
- 9.Solomon DH, Van Houten L, Glynn RJ, et al. Academic detailing to improve use of broad-spectrum antibiotic at an academic medical center. Arch Intern Med. 2001;161:1897–1902. doi: 10.1001/archinte.161.15.1897. [DOI] [PubMed] [Google Scholar]
- 10.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 11.Bandura A. Self-Efficacy in Changing Societies. Cambridge University Press; New York: 1995. [Google Scholar]
- 12.Prochaska JO, Redding CA, Evers KE. The Transtheortical Model and Stages of Change. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research and Practice. 4th ed Jossey-Bass Inc.; San Francisco: pp. 97–121. [Google Scholar]
- 13.Kim J, Whitney A, Hayter S, et al. Development and initial testing of a computer-based patient decision aid to promote colorectal cancer screening for primary care practice. BMC Med Inform Decis Mak. 2005;5:36. doi: 10.1186/1472-6947-5-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glanz K, Steffen AD, Taglialatela LA. Effects of colon cancer risk counseling for first-degree relatives. Cancer Epidemiol Biomarkers Prev. 2007;16:1485–1491. doi: 10.1158/1055-9965.EPI-06-0914. [DOI] [PubMed] [Google Scholar]
- 15.Lipkus IM, Rimer BK, Lyna PR, Pradhan AA, Conaway M, Woods-Powell CT. Colorectal screening patterns and perceptions of risk among African-American users of a community health center. Journal of Community Health. 1996;21:409–427. doi: 10.1007/BF01702602. [DOI] [PubMed] [Google Scholar]
- 16.Jonas DE, Russell LB, Sandler RS, Chou J, Pignone M. Value of Patient Time Invested in the Colonoscopy Screening Process: Time Requirements for Colonoscopy Study. Med Decis Making. 2008 Jan-Feb;28(1):56–65. doi: 10.1177/0272989X07309643. 2008. [DOI] [PubMed] [Google Scholar]
- 17.Degner LF, Kristjanson LJ, Bowman D, et al. Information needs and decisional preferences in women with breast cancer. JAMA. 1997;277(18):1485–1492. [PubMed] [Google Scholar]