Abstract
Anorexia Nervosa (AN) is a serious mental illness characterized by reduced caloric intake that often persists after acute weight restoration. This preliminary study assesses the relationship between pre-meal anxiety and food intake in recently weight-restored individuals with AN. We hypothesized that pre-meal anxiety is inversely related to caloric intake in AN. Caloric intake and pre-meal anxiety were measured in 3 laboratory- based assessments (yogurt snack, multi-item lunch, macaroni and cheese lunch). Anxiety was measured by Spielberger State-Trait Anxiety Inventory (STAI-S) administered prior to the meal. Acutely weight-restored patients with AN were compared with healthy controls (HC). Associations between anxiety and intake were analyzed first within each meal type separately and then using a model to combine the sample. In the multi-item lunch and the macaroni & cheese lunch, AN ate significantly less than HC (p = 0.01, p<0.001). Pre-meal anxiety was significantly correlated with intake among AN, but not HC. In the yogurt snack, there was no significant association between anxiety and intake among patients or controls, and the groups did not differ in caloric intake. The association between pre-meal anxiety and intake among weight restored individuals with AN suggests a potential target for relapse prevention treatment.
Keywords: anorexia nervosa, anxiety, eating behavior
INTRODUCTION
Anorexia nervosa (AN) is a serious psychiatric illness with a mortality rate among the highest of any psychiatric illness (Papadopoulos, Ekbom, Brandt, & Ekselius, 2009). Mortality increases over time, and is estimated to be 5% per decade of illness (Sullivan, 1995). The disorder is characterized by severe weight loss, body image distortions/overemphasis on shape and weight, and fear of “fat” or weight gain. Initial treatment focuses on restoring normal weight and structured behavioral treatment programs are generally successful in achieving this goal. However, the relapse rate after acute weight restoration is substantial, with as many as 50% of patients requiring re-hospitalization with the year after discharge (Pike, 1998). Although many psychological symptoms improve with weight gain, often to within normal limits (Attia, Haiman, Walsh, & Flater, 1998), significant problems with food choice and caloric intake persist (Sysko, Walsh, Schebendach, & Wilson, 2005). Specifically, dietary choices made by weight restored patients on an inpatient unit have been shown to be associated with outcome such that those who made food choices lower in energy density and diet variety, even with similar caloric intakes, were more likely to have a poor outcome in the year following discharge (Schebendach, et al., 2008). Understanding the factors associated with the persistence of dysfunctional eating behavior after acute weight restoration may suggest novel targets for treatment.
The persistence of dysfunctional eating behaviors in individuals with AN may be related to anxiety (Steinglass, et al., 2010) . We recently proposed a model of AN linking eating behavior with anxiety. Baseline anxiety and obessionality lead to fear of food, avoidance of food, and rigid dieting behavior. These factors interact and lead to weight loss. Weight loss in turn increases baseline anxiety and obsessionality and serves to perpetuate the cycle of dysfunctional eating behavior. In support of this model, a previous study by our group found that patients, even after weight restoration and improvement in many psychological symptoms, continued to significantly restrict their eating during a laboratory test meal (Sysko, et al., 2005). A subsequent study demonstrated that repeated presentation of the same laboratory meal, with a therapist present for encouragement, led to increases in total intake (Steinglass, et al., 2007). To begin to address the question of the relationship between pre-meal anxiety and food intake in weight restored individuals with AN, we combined data from three ongoing studies that each include a laboratory-based eating assessment. We hypothesized that pre-meal anxiety would be inversely related to caloric intake among individuals with AN. As a preliminary test of this hypothesis, we examined each meal study separately and then pooled these data to create one model and thereby increase power to detect an effect.
METHODS
Subjects
Participants were recently weight-restored women with AN (n=27), inpatients and outpatients, and healthy controls (HC, n=23) enrolled in one of three ongoing eating behavior studies at the Columbia Center for Eating Disorders at the New York State Psychiatric Institute (NYSPI). Some individuals participated in more than one study (as described in more detail below). HC were healthy women with no current or prior eating disorder or any other psychiatric illness, as assessed by Structured Clinical Interview for DSM-IV(First, Spitzer, Gibbon, & Williams, 1995) and Eating Disorder Examination (Cooper & Fairburn, 1987) and no significant medical illness, as assessed by a clinical interview with an M.D. HC were recruited from the Columbia University and Medical Center campuses.
Patients with AN were included if they were between the ages of 16 and 45 years (for the multi-item lunch, the minimum age was 18 years) and met criteria for AN with or without amenorrhea (Attia & Roberto, 2009) at the time of hospital admission. Patients with AN participating in the yogurt snack and the mult-item lunch were receiving inpatient treatment on the inpatient Eating Disorders Unit at NYSPI and had achieved normal weight. Patients with AN participated in the macaroni & cheese lunch within 1 week of completing the inpatient treatment program, after hospital discharge, and were enrolled in outpatient relapse prevention treatment at the Eating Disorders Clinic. Inpatient treatment consisted of a structured, behavioral program (Attia, et al., 1998) and patients were weight restored to at least 90% of ideal body weight (BMI ≈19.5 kg/m2) as defined by the Metropolitan Life actuarial tables (Metropolitan Life Insurance, 1959). Height and weight were measured by calibrated beam balance scale (Detecto, Webb City, MO). All test meals occurred in the eating behavior laboratory at the Biological Studies Unit of NYSPI. All studies were approved by the Institutional Review Board of NYSPI, and written informed consent was obtained prior to participation.
Procedures
The three studies of eating behavior in AN are described below.
(1) Study utilizing a Yogurt Snack
Inpatients with AN participated in the test snack within one week after weight restoration. A standardized breakfast (300 kcal) was provided to patients (n=10) and HC (n=10) at 8 am and participants were asked to consume nothing else until the test snack at 10 am. Three patients with AN and 2 HC participated in a test snack at 3 pm, and received a standardized lunch at noon consisting of 580 kcal (instead of the standardized breakfast). Participants were administered the Spielberger State-Trait Anxiety Inventory, State version (STAI-S) (Spielberger, Gorsuch, & Lushene, 1970) immediately prior to entering the testing room. After a 3 minute acclimation period, a tray with a large bowl of vanilla yogurt, a large spoon and a napkin were provided to participants, who were instructed to eat a sufficient snack. This particular instruction was intended to focus the assessment on the individual’s eating-related anxiety and to mitigate anxiety around choosing whether to eat during this meal, and was developed from previous experience with laboratory meals. However, the impact of this instruction on the individual’s behavior was not evaluated. The bowl contained approximately 700 g of yogurt (550 kcal, 12.9% fat, 62.8% CHO, 24.8% protein).
(2) Study utilizing a Multi Item Lunch
Inpatients with AN participated 1-2 weeks after achieving weight restoration. Patients (n=23) and HC (n=20) received a standardized breakfast (300 kcal) at 8 am and did not eat or drink until the test lunch was served at 1 pm. Participants entered the testing room, where a multi-item buffet was arranged on the table and completed the STAI-S upon viewing the food in the buffet. Participants were instructed to eat as much as they liked. The multi-item buffet consisted of Stouffers macaroni & cheese, french fries, white and wheat bread, tuna, pickles, tossed salad, condiments, fruit salad, grilled chicken, fried chicken, popcorn, candy, cookies, doughnuts, ice cream, water, soda, and juice (a total of 15,000 kcal were available; details provided upon request).
(3) Study utilizing a Macaroni & Cheese Lunch
Patients with AN were acutely weight restored as inpatients and participated in testing within one week of hospital discharge. Test lunch occurred at noon. Patients (n=11) and HC (n=10) were instructed to eat a standardized breakfast (300 kcal) at 8 am and not to eat or drink between breakfast and the lunch test meal at 12 pm. Compliance with the standardized breakfast procedure was ascertained verbally prior to the test meal. Participants were administered the STAI-S immediately prior to entering the testing room. The participant was served a tray with a large bowl of macaroni and cheese (Stouffer’s, heated according to package instructions), an 8 oz bottle of water, a fork, a large spoon, and a napkin. The participant was instructed to eat a sufficient lunch. The bowl contained 1,000 g of macaroni and cheese (1557 kcal, 42.2% fat, 40.2% CHO, 17.5% protein).
For all test meals, patients were not informed of the caloric content of the meal. Intake was calculated by measuring the weight of the food (Acculab 7200 balance, readability 0.1g) before and after the meal and calculating calories consumed based on kcal/gram weight of the foods.
Individuals completed additional self-report psychological assessments of anxiety and depression, including the Spielberger State-Trait Anxiety Inventory, Trait version (STAI-T) (Spielberger, et al., 1970), the Beck Anxiety Inventory (BAI) (Beck, Epstein, Brown, & Steer, 1988), and the Beck Depression Inventory (BDI) (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961).
Data Analysis
Continuous demographic and clinical measures in AN and HC groups were compared by two-sample t-test. Pearson correlation coefficients were calculated between anxiety measures (STAI-S) and intake for AN and HC and were compared by applying Fisher’s Z transformation (Kleinbaum, Kupper, Nizam, & Muller, 2007). Anxiety measures in AN were compared across three meal types by ANOVA.
To increase power, these data were combined to create a statistical model in which the relationship between pre-meal anxiety and caloric intake could be tested. Generalized estimating equation (GEE) (Liang & Zeger, 1986) was used to model the relationship between mean anxiety measures and intake, adjusting for age, BMI and meal type. Correlation between repeated measures of anxiety scores on the same subject (some subjects participated in more than one meal type) was accounted for by computing robust variance estimator in the GEE (Liang & Zeger, 1986). The model fitted a separate average intake and a separate relationship between anxiety and intake for AN subjects in each meal type. The association between pre-meal anxiety and caloric intake did not differ significantly across meal type in HC subjects (i.e. the relationship was sufficiently similar in each meal); therefore, one association was used as the comparison, with a different average intake for each meal type.
RESULTS
Clinical Characteristics & Demographics
In total, 27 women with AN participated in at least one laboratory-based test meal. One patient participated in all 3 meals; 7 participated in the macaroni & cheese and the multi-item lunch meals; 6 participated in the multi-item lunch and the yogurt snack; and the remainder participated in only 1 meal. Of the 23 healthy controls, 7 participated in all 3 meals; 1 participated in the multi-item meal and the macaroni & cheese meal; 2 participated in the macaroni & cheese meal and the yogurt meal; the remainder participated in only 1 meal. Analyses were based on data from 40 meals with HC and 44 meals with patients with AN.
In the total sample, there was no difference between HC and AN in mean age or BMI (see Table 1). As expected, the groups differed significantly (p<0.01) in mean STAI-S, STAI-T, BAI, and BDI (see Table 1). Among the patients, 32.1% were restricting subtype and 67.9% were binge-purge subtype. Nine patients had a current Axis I diagnosis in addition to AN (3 with major depressive disorder, 2 with obsessive-compulsive disorder, 3 with social phobia, and 1 with major depressive disorder and generalized anxiety disorder). Eleven patients had a lifetime diagnosis of a mood, anxiety or substance abuse disorder. Of the patients, 25 (89.3%) were Caucasian, 2 (7.1%) were Hispanic, and 1 was Asian (3.6%). Of the healthy controls, 17 (73.9%) were Caucasian, 3 (13.0%) were Hispanic, 2 (8.6%) were Asian, and 1 (4.3%) was African American.
Table 1.
Demographics and Clinical Characteristics
| HC (Mean ± SD) |
AN (Mean ± SD) |
|
|---|---|---|
| Age (yrs) | 24.6 ± 4.0 | 25.9 ± 7.0 |
| BMI (kg/m2) | 20.5 ± 0.9 | 20.2 ± 0.8 |
| STAI-Sa | 25.0 ± 4.6 | 52.9 ± 12.0* |
| STAI-Tb | 27.0 ± 4.1 | 54.4 ± 13.5* |
| BAIc | 1.8 ± 2.3 | 11.5 ± 8.6* |
| BDId | 0.13 ± 0.4 | 15.2 ± 10.8* |
Spielberger State-Trait Anxiety Inventory, State version
Spielberger State-Trait Anxiety Inventory, Trait version
Beck Anxiety Inventory
Beck Depression Inventory
p<0.01 between groups
Average caloric intake and anxiety
In the yogurt snack, mean caloric intake did not differ significantly between patients with AN and HC (116.9 ± 80.2 kcal vs. 151.3 ± 69.8 kcal). In the multi-item lunch, patients with AN ate significantly less than HC (492.1 ± 304.2 kcal vs. 750.7 ± 318.3 kcal, p = 0.01). The difference between patients and HC was the largest in the macaroni & cheese lunch, where patients ate 181.3 ± 235.9 kcal compared to 530.9 ± 178.3 kcal for HC (p<0.001).
Pre-meal anxiety measured on the STAI-S was significantly higher for patients as compared to HC in each meal type (50.7 ± 11.8 vs. 23.3 ± 3.5, yogurt snack; 52.5 ± 12.9 vs. 25.5 ± 4.5, multi-item lunch; and 55.8 ± 10.9 vs. 25.6 ± 5.7; macaroni and cheese, p<0.001). STAI-S score increased slightly across meal types for patients, but this was not statistically significant.
Associations between anxiety and intake
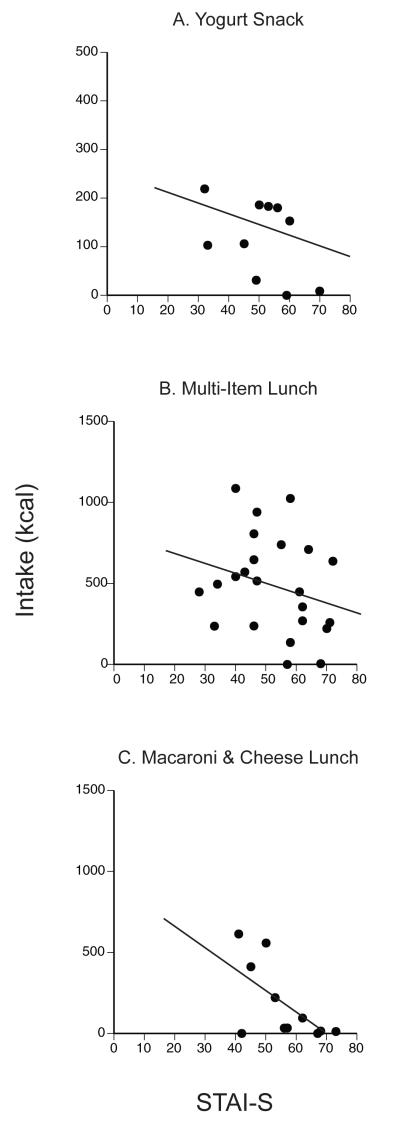
Pearson correlations between STAI-S and caloric intake were not significant for HC in any meal type. For patients, Pearson correlations in the yogurt snack (r=−0.44, p=0.21) and in the multi-item meal (r=−.26, p=0.23) were not significant. In the macaroni & cheese meal, the correlation was statistically significant (r = −.64, p=0.03, 95% CI: [−0.90, −0.07]). These data are presented in Figure 1.
Figure 1.
Pre-meal anxiety and caloric intake in patients with AN across 3 laboratory test meals. Pre-meal anxiety was measured by Spielberger State-Trait Inventory, State version (STAI-S). Pearson correlations: (A) Yogurt Snack (r=−0.44, p=0.21), Multi-item Lunch (r=−.26, p=0.23), Macaroni & Cheese Lunch (r = −.64, p=0.03). Using statistical modeling procedures (GEE analysis) to pool data and increase power, STAI-S was significantly associated with caloric intake in the Macaroni & Cheese Lunch (C) and the Multi-Item Lunch (B), but not in the Yogurt Snack (A).
Using the statistical model described above, which increased power to detect an association, the association between anxiety and intake within the AN group was tested and compared with the HC group. Among patients with AN, pre-meal anxiety was negatively associated with intake in the multi-item lunch (beta=−6.64, p=0.018, 95% CI: [−12.14, −1.14]) and macaroni & cheese lunch (beta=−8.84, p=0.001, 95% CI: [−14.01, −3.67]), but not in the yogurt snack (beta=−2.32, p=0.38, 95% CI:[−7.52, 2.88]). These relationships were compared with associations in the HC subjects. The relationship between anxiety and intake in the yogurt snack did not differ for patients with AN compared with HC. However, the associations did differ significantly between groups (patients compared with HC) in both the multi-item lunch (difference=−4.33, p=0.007, 95% CI: [−1.18, −2.69]) and the macaroni & cheese lunch (difference=−6.52, p<0.001, 95% CI: [−8.57, −4.48]). Furthermore, the association differences were significantly different by meal type (p<.001) (i.e. significant intake by diagnosis by meal type three way interaction: the difference in the association between anxiety and intake among individuals in AN versus HC subjects differed between each of the three meal types).
Using the same statistical model, we examined the associations between BAI, BDI, STAI-T and intake as well, and found similar relationships for BDI and STAI-T. For HC, the associations between BAI, BDI, STAI-T and caloric intake were not significant. For patients, there were no significant associations in yogurt snack (BAI: beta=−1.14, p= 0.62, 95% CI [−5.56, 3.29]; BDI: beta=−0.65, p=0.65, 95% CI [−3.44, 2.15]; STAI-T: beta=−3.87, p=0.21, 95% CI [−9.87, 2.13]); but there were significant associations for each of the measures with intake in the multi-item meal (BAI: beta= −15.61, p=0.004, 95% CI [−26.19, −5.02]; BDI: beta=−17.41, p<.001, 95% CI [−24.28, −10.55]; STAI-T: beta=−9.47, p=0.004, 95% CI [−15.97, −2.98]) and in the macaroni & cheese meal (BAI: beta=−17.48, p<.001, 95% CI [−24.53, −10.43]; BDI: beta=−19.38, p<.001, 95% CI [−24.78, −13.98]; STAI-T: beta=− 10.98, p<.001, 95% CI [−16.79, −5.18]). The measures BAI, BDI, STAI-T and STAI-S themselves are highly correlated in the data: among patients, the correlations between STAI-S and BAI, BDI, and STAI-T were, respectively, r=0.61 (p<0.001), r=0.75 (p<0.001), and r=0.75 (p<0.001).
To further test whether there was a relationship between anxiety and intake for HC, we examined the association estimated from the model. The association for HC was beta=−4.5 (p=0.47, 95% CI: [−16.8, 7.8]), i.e. the slope for the controls is not significantly different from zero, suggesting that there was no association between anxiety and intake among HC.
The reliability of the findings was evaluated through the estimation of several models, where the assumptions about the expected relationships for repeated measures were varied. To execute these sensitivity analyses, the GEE model was fitted with exchangeable, AR-1, unstructured and working independence correlations. Each model makes different assumptions about the between-subject and within-subject correlations for the outcome variable. The results of these model indicated that parameters were stable, i.e., the estimated coefficients and corresponding p-values are similar for all models with different correlation structures.
DISCUSSION
For patients with AN, greater pre-meal anxiety was associated with lower caloric intake in 2 types of laboratory meals. This relationship was not present among healthy controls. The strength of the association between anxiety and intake for individuals with AN differed by meal type. The significant association between anxiety and intake suggests that pre-meal anxiety is a potential therapeutic target. Anxiety has long been noted to be an important feature of AN. Substantial comorbidity between AN and anxiety disorders is well established (Kaye, Bulik, Thornton, Barbarich, & Masters, 2004) and the available data indicate that anxiety disorders often precede the development of AN (Bulik, Sullivan, Fear, & Joyce, 1997; Raney, et al., 2008), suggesting anxiety may be a predisposing factor. The current study adds to this literature by suggesting a direct association between anxiety and the restrictive eating behavior that is the core behavioral disturbance of AN.
Treatment studies for AN, to date, have been disappointing (Steinhausen, 2002). Few approaches have emphasized the importance of focusing directly on eating behavior. Previous treatments that have emphasized normalizing eating behavior have focused on training patients on rate of eating (Bergh, Brodin, Lindberg, & Sodersten, 2002), without dramatic effect. Medication trials have emphasized the role of depressive symptoms and therefore pursued antidepressant treatments; yet, these treatments have been similarly disappointing (Attia, et al., 1998; Walsh, et al., 2006). No treatment to date has specifically targeted anxiety as a method of improving healthy eating. The present findings lend support to the therapeutic idea that decreasing pre-meal anxiety could improve dietary intake among individuals with AN.
In the patient group, the association between anxiety and intake differed by meal type, and was not significant in the yogurt snack. This difference was present despite fairly similar levels of pre-meal anxiety. One possible interpretation is that the small differences in STAI-S, though not statistically significant, do matter clinically. Alternatively, there may be another meal-related factor, not measured by STAI-S, that interacts with anxiety. One possible interpretation of this is that the multi-item meal and macaroni & cheese were more “threatening” meals than yogurt, and that macaroni & cheese presented greater “threat” than a multi-item meal in which a range of options were available. Both subjective anxiety and meal type may affect eating behavior and caloric intake among individuals with AN, even after acute weight restoration.
Hunger and fullness rating were not measured in this study. It is possible that these factors contributed to our findings; however, studies examining intake in the laboratory in patients with AN have shown consistently low ratings of hunger and high ratings of fullness, despite highly variable amounts of intake (Halmi & Sunday, 1991) and Sysko and colleagues (Sysko, et al., 2005) did not find a correlation between hunger and satiety and intake. In the current study, time since last meal was shortest for the yogurt snack, thus one might expect hunger to be lowest in this meal. Yet, there was no difference between patients and HC in the snack meal. Taken together, these findings suggest that it is not likely that hunger or satiety significantly affected the results in these laboratory meals.
Among the study’s limitations is the fact that the data presented were obtained from separate studies and are not derived from a single study designed specifically to address the impact of anxiety on intake. The timing of the administration of the STAI-S was not identical between test meals, and the number of subjects in the yogurt meal may have been too small a sample size to detect a difference between patients and controls. Many individuals participated in more than one test meal, therefore the use of the statistical model to pool data is somewhat limited by repeated measures. Several individuals ate virtually nothing in the macaroni and cheese meal, and it is plausible to consider whether these few data points are driving the statistically significant finding. We controlled for repeated assessments in the statistical model, and have examined the finding using different methods; all approaches have yielded the same result, supporting the presence of an association. Nonetheless, further study of anxiety and intake would be helpful to corroborate this finding.
One major limitation of the current study is that, since the findings are of correlations between symptoms and behavior, causality cannot be assessed. Future studies to examine a mechanistic link between pre-meal anxiety and food intake might consider experimentally controlling the level of anxiety symptomatology and examining the resultant impact on eating (e.g., by pharmacologically controlling anxiety). In our study the range of pre-meal anxiety scores differed between the AN and HC groups. The STAI-S scores among participants with AN ranged from 28 to 73, whereas among HC participants the range was 20 to 36. The small amount of overlap in anxiety complicates the interpretation of the role of anxiety in intake among HC. That is, it may be that there is no relationship between anxiety and intake, as we found in this sample, or it may be that the relationship is non-linear, and high levels of anxiety may impact intake across all individuals, above an unknown threshold of STAI-S. Thus the findings among HC should be interpreted with caution. Regardless of whether an association is present for HC, the presence of an association among patients with AN is noteworthy. Patients with AN in this study were acutely weight restored; that is, had achieved a normal weight for 1-6 weeks, depending on the study. It may be that pre-meal anxiety would decrease with a longer maintenance of normal weight. However, relapse is known to occur very rapidly post discharge (Kaplan, et al., 2009), and therefore pre-meal anxiety in the acutely weight restored individual remains an important variable.
Despite the limitations, the results of this study are consistent with the hypothesis that pre-meal anxiety is associated with intake among patients with AN. Future studies are needed to determine whether this link is indeed causal. Other measures of anxiety and depression were also correlated with intake. High correlations between these measures have been widely reported in the literature (Beck, et al., 1988; Dobson, 1985; Tanaka-Matsumi & Kameoka, 1986). While mood and anxiety may be inextricably linked psychological phenomena, the direct association between anxiety and intake in this study suggests a new and promising avenue for treatment development.
Acknowledgements
The authors would like to acknowledge Michael J. Devlin, MD, the Eating Disorders Research Unit staff, and the participants for their contributions.
This project was supported by NIMH (K23MH076195-02, R01MH08273602), NIA (R03AG031113-01A2), Irving Institute for Clinical and Translational Research Clinical Trials Pilot Study Award, NARSAD Young Investigator Award, and the Davis Foundation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Literature Cited
- Attia E, Haiman C, Walsh BT, Flater SR. Does fluoxetine augment the inpatient treatment of anorexia nervosa? Am J Psychiatry. 1998;155(4):548–551. doi: 10.1176/ajp.155.4.548. [DOI] [PubMed] [Google Scholar]
- Attia E, Roberto CA. Should amenorrhea be a diagnostic criterion for anorexia nervosa? Int J Eat Disord. 2009;42(7):581–589. doi: 10.1002/eat.20720. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bergh C, Brodin U, Lindberg G, Sodersten P. Randomized controlled trial of a treatment for anorexia and bulimia nervosa. Proc Natl Acad Sci U S A. 2002;99(14):9486–9491. doi: 10.1073/pnas.142284799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Fear JL, Joyce PR. Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatr Scand. 1997;96(2):101–107. doi: 10.1111/j.1600-0447.1997.tb09913.x. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Fairburn CG. The Eating Disorder Examination: a semi-structured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders. 1987;6:1–8. [Google Scholar]
- Dobson KS. An analysis of anxiety and depression scales. J Pers Assess. 1985;49(5):522–527. doi: 10.1207/s15327752jpa4905_10. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P) version 2 New York State Psychiatric Institute, Biometrics Research; New York: 1995. [Google Scholar]
- Halmi KA, Sunday SR. Temporal patterns of hunger and fullness ratings and related cognitions in anorexia and bulimia. Appetite. 1991;16(3):219–237. doi: 10.1016/0195-6663(91)90060-6. [DOI] [PubMed] [Google Scholar]
- Kaplan AS, Walsh BT, Olmsted M, Attia E, Carter JC, Devlin MJ, et al. The slippery slope: prediction of successful weight maintenance in anorexia nervosa. Psychol Med. 2009;39(6):1037–1045. doi: 10.1017/S003329170800442X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am J Psychiatry. 2004;161(12):2215–2221. doi: 10.1176/appi.ajp.161.12.2215. [DOI] [PubMed] [Google Scholar]
- Kleinbaum D, Kupper L, Nizam A, Muller K. Applied Regression Analysis and other Multivariable Methods. 4 ed Duxbury Press; 2007. [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- MetropolitanLifeInsurance New weight standards for men and women. Statistical Bulletin. 1959;(40):1–4. [Google Scholar]
- Papadopoulos FC, Ekbom A, Brandt L, Ekselius L. Excess mortality, causes of death and prognostic factors in anorexia nervosa. Br J Psychiatry. 2009;194(1):10–17. doi: 10.1192/bjp.bp.108.054742. [DOI] [PubMed] [Google Scholar]
- Pike KM. Long-term course of anorexia nervosa: response, relapse, remission, and recovery. Clin Psychol Rev. 1998;18(4):447–475. doi: 10.1016/s0272-7358(98)00014-2. [DOI] [PubMed] [Google Scholar]
- Raney TJ, Thornton LM, Berrettini W, Brandt H, Crawford S, Fichter MM, et al. Influence of overanxious disorder of childhood on the expression of anorexia nervosa. Int J Eat Disord. 2008;41(4):326–332. doi: 10.1002/eat.20508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schebendach JE, Mayer LE, Devlin MJ, Attia E, Contento IR, Wolf RL, et al. Dietary energy density and diet variety as predictors of outcome in anorexia nervosa. Am J Clin Nutr. 2008;87(4):810–816. doi: 10.1093/ajcn/87.4.810. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the state-trait inventory. Consulting Psychologists Press; Palo Alto, CA: 1970. [Google Scholar]
- Steinglass J, Sysko R, Schebendach J, Broft A, Strober M, Walsh BT. The application of exposure therapy and D-cycloserine to the treatment of anorexia nervosa: a preliminary trial. J Psychiatr Pract. 2007;13(4):238–245. doi: 10.1097/01.pra.0000281484.89075.a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT. Rationale for the Application of Exposure Response Prevention to the Treatment of Anorexia Nervosa. Int J Eat Disord. 2010 doi: 10.1002/eat.20784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinhausen HC. The outcome of anorexia nervosa in the 20th century. American Journal of Psychiatry. 2002;159(8):1284–1293. doi: 10.1176/appi.ajp.159.8.1284. [DOI] [PubMed] [Google Scholar]
- Sullivan PF. Mortality in anorexia nervosa. American Journal of Psychiatry. 1995;152(7):1073–1075. doi: 10.1176/ajp.152.7.1073. [DOI] [PubMed] [Google Scholar]
- Sysko R, Walsh BT, Schebendach J, Wilson GT. Eating behavior among women with anorexia nervosa. Am J Clin Nutr. 2005;82(2):296–301. doi: 10.1093/ajcn.82.2.296. [DOI] [PubMed] [Google Scholar]
- Tanaka-Matsumi J, Kameoka VA. Reliabilities and concurrent validities of popular self-report measures of depression, anxiety, and social desirability. J Consult Clin Psychol. 1986;54(3):328–333. doi: 10.1037//0022-006x.54.3.328. [DOI] [PubMed] [Google Scholar]
- Walsh BT, Kaplan AS, Attia E, Olmsted M, Parides M, Carter JC, et al. Fluoxetine after weight restoration in anorexia nervosa: a randomized controlled trial. JAMA. 2006;295(22):2605–2612. doi: 10.1001/jama.295.22.2605. [DOI] [PubMed] [Google Scholar]