Abstract
Background
Research training is essential in a modern undergraduate medical curriculum. Our evaluation aimed to (a) gauge students' awareness of research activities, (b) compare students' perceptions of their transferable and research-specific skills competencies, (c) determine students' motivation for research and (d) obtain students' personal views on doing research.
Methods
Undergraduate medical students (N=317) completed a research skills questionnaire developed by the Centre for Excellence in Teaching and Learning in Applied Undergraduate Research Skills (CETL-AURS) at Reading University. The questionnaire assessed students' transferable skills, research-specific skills (e.g., study design, data collection and data analysis), research experience and attitude and motivation towards doing research.
Results
The majority of students are motivated to pursue research. Graduate entrants and male students appear to be the most confident regarding their research skills competencies. Although all students recognise the role of research in medical practice, many are unaware of the medical research activities or successes within their university. Of those who report no interest in a career incorporating research, a common perception was that researchers are isolated from patients and clinical practice.
Discussion
Students have a narrow definition of research and what it entails. An explanation for why research competence does not align more closely with research motivation is derived from students' lack of understanding of the concept of translational research, as well as a lack of awareness of the research activity being undertaken by their teachers and mentors. We plan to address this with specific research awareness initiatives.
Keywords: undergraduate, research skills, translational research, training, scholarly activity programmes
Scholarly activity programmes are essential components of the modern undergraduate medical curriculum (1–4). Such programmes can be elective options or required as part of the syllabus and typically entail mentored study in a specific topic area (5). Many programmes have a research focus ranging from thesis-level projects conducted over a year or more to programmes that can occur during a ‘research’ month (6). Contemporary medical school entrants come from diverse cultural and educational backgrounds and have varying levels of research knowledge and experience. Future medical research, specifically translational medical research, is dependent on the interaction between physician scientists, basic scientists and other health care providers undertaking innovative patient and disease-focused research (7, 8).
There has been much discussion over the past 25 years regarding the serious decline in medical graduates choosing clinician scientist careers (9–13). Until recently, public and private initiatives to revitalise this pathway have prioritised MD/PhD programmes and other approaches later in clinician training (14, 15). During the last decade, there has been renewed emphasis on the medical student research experience. Two large US programmes that have sought to engage students during this critical period of training are the National Institutes of Health (NIH) sponsored Medical Student Research Fellowship Programmes (MSRFs) (14) and the Doris Duke Clinical Research Fellowship (CRF) Programme (16). Examples from Europe include the Norwegian Medical Student Research Programme, which facilitates students who want to do research in parallel with their other studies (17), and in the Netherlands, students are required to do full-time individual research projects between years 4 and 6 (18). US scholarly activity programmes, such as the Baylor COM and Cleveland Clinic Learner COM, promote clinician scientist training, whereas others like Alpert Medical School of Brown University focus on the preparation of clinicians able to contribute to advancements in health care systems (19). In the UK, exposure to research principles is provided for all students within the student selected components (SSC) programme (20). Encouraging research and fostering the development of analytical skills among medical students is now a high priority (21, 22). Together with the development of transferable skills, such as communication, teamwork, time management and critical thinking, fostering of research-specific skills among undergraduate medical students has been strongly recommended by Tomorrows Doctors, the Scottish Deans Curriculum group and by the guide to Good Medical Practice USA (1, 2, 23). A recent review of scholarly activity programmes has shown that completion of such programmes can influence students' choice of clinical speciality or interest in research (24). However, little is known about how students perceive research (25).
There are two medical programmes at University College Cork (UCC), a 5-year undergraduate programme with approximately 120 students per year, and a new 4-year Graduate Entry Medicine (GEM) Programme, which commenced in 2008 with an intake of 50 students per year. Prior to the introduction of this 4-year course, graduates were admitted to the 5-year programme. One of the objectives of our new integrated medical curriculum is to expand the research skills of our students and to identify a range of opportunities that will allow them to experience research. This is achieved through elective scholarly activity or SSCs in the early years, and core mandatory research modules in the final years, where every attempt is made to match students to research-active mentors in an area that interests them. Like many other medical schools in Ireland, the UK and the wider European Union, we have a diverse multinational student population who arrive to the programme with varying research skills; attitudes towards doing research.
Research has a high profile in our institution. Faculty are research active, and 25% of the total institutional income is derived from research. A senior lecturer appointee is charged with overseeing undergraduate research initiatives and research skills training. All students must complete a substantive research project, which contributes to 10% of their final year aggregate mark. Projects are normally conducted over the period of a year and a half, starting in the fourth year and finishing in the spring of final year. Students are required to present their research orally and to submit a written submission (5,000 words) of their work. Prizes are awarded for the highest achievers.
This paper reports the baseline findings of our undergraduate research programme evaluation. During this first phase, we aimed to (a) gauge students' awareness of research activities at UCC, (b) compare students' perceptions of their transferable and research-specific skills competencies, (c) determine students' motivation for research and (d) obtain students' personal views on doing research.
Methods
Study design
All students registered on the undergraduate medical programme in UCC from Year 1 to Year 4 were eligible to participate in this baseline study. Final year medical students were excluded as they had participated in an older curriculum. This study and its forthcoming follow-up have been exempted from full ethical review by the Clinical Research Ethics Committee of the Cork teaching hospitals on the basis of educational research carried out in an established educational setting.
Study measures
Students completed a questionnaire adapted from measures originally developed to assess research skills with Zoology and Ecology students by the Centre for Excellence in Teaching and Learning in Applied Undergraduate Research Skills (CETL-AURS) at Reading University (http://www.reading.ac.uk/cetl-aurs/). We chose this questionnaire because there are no standardised tools to assess medical student engagement in research and we found the CETL-AURS measures appropriate for our stated objectives. We modified the questionnaire so that it required approximately 15 min completion time. The adapted research skills questionnaire was divided into five short sections. Details of each section of the questionnaire are illustrated in Table 1.
Table 1.
Research skills questionnaire sections and items
| Section heading | Items | Measure |
|---|---|---|
| Your demographics | 1. Gender, age, nationality, previous degree | 1. Boxes and free text |
| 2. Elective scholarly activities taken | 2. Yes/no box and free text | |
| 3. Summer research placements taken | 3. Yes/no box and free text | |
| Your Understanding of Research | 1. Understanding of the term researcha | 1. Free text |
| 2. True and false statements about the research processa | 2. Nine items. True/false options | |
| Your Skills | 1. Perceived levels of competence in transferable skillsa | 1. 10 items. 10-point rating scales from low competence to high competence |
| 2. Perceived levels of competence in research-specific skillsa | 2. Six items. 10-point rating scales from low competence to high competence | |
| 3. Skills to improvea | 3. Free text | |
| Research at University College Cork and your interests | 1. Awareness of university research activitiesa | 1. 4-point Likert scale |
| 2. Areas of interest in medicine and researcha | 2. Yes/no option, free text | |
| 3. Motivation towards doing research | 3. 16 items. 7-point low to high motivation scale | |
| 4. How a researcher thinks | 4. Free text | |
| Your future career | 1. Type of medical career chosena | 1. Yes/no box and free text |
| 2. Appeal of a career in researcha | 2. Yes/no box and free text |
aModified from original CETL-AURS.
Minor modifications were made to the questionnaire after we piloted it with a small group of first, second and third year medical students undertaking a library-based SSC. In the current study, the Cronbach alpha coefficient for the scales on ‘general skills’ was 0.87 and for ‘research skills’ it was 0.88, indicating good internal consistency (see Table 1 ‘Your Skills’ No. 1 and 2). The Student Motivation scale has good reliability (r = 0.94) (26, 27) and a Cronbach alpha coefficient of 0.92 for the current study (see Table 1 ‘Research at University College Cork and Your Interests’ No. 3).
Procedures
The questionnaires were completed at the end of large group lectures between December 2008 and February 2009. Before the questionnaires were administered, we briefed the students on the purpose of the survey and informed them that their participation was voluntary. We explained that we would require student identification numbers and that responses would be kept confidential and used for medical educational research purposes only.
Data analysis
Descriptive statistics are reported through means, medians and bar charts. For descriptive purposes, the data on students' perceived levels of competency were grouped into lower and higher levels using two equal cut-off points. The data were visually checked for normal distribution using histograms and Q–Q plots and tested using the Kolmogorov–Smirnoff statistic. Mann–Whitney U and Kruskal–Wallis tests were used to examine the differences between perceived levels of competence with transferable and research-specific skills. T tests and ANOVA were used to examine the data on levels of motivation for research. Categorical data on students' awareness of research activities at UCC were tested using Pearson's Chi–Square test. Qualitative data on students' understanding of the term ‘research’ and the appeal of a medical research career were analysed using a thematic approach and constant comparison techniques by authors LB and SOF. The initial qualitative analysis was performed by LB, and these results were cross-checked and refined by SOF.
Results
Demographic characteristics
A total of 317 students participated in our survey. Response rates were 70% (N = 85) from first years, 64% (N = 125) from second years, 39% (N = 42) from third years, 60% (N = 78) from fourth years and 76% (N = 32) from the Year 1 GEM class. This gave an overall response rate of 60%. At the time of sampling, third year students were on community placements or regional rotations and attendance at large group lectures was lower, resulting in a lower response rate for this group. A demographic breakdown of participants is provided in Table 2. One hundred and eighty four (58%) students were female and over half (69%) of the total group were aged between 17 and 23. The majority of students were of Irish and European nationality (62%) followed by Asian (23%) and North American and Canadian (15%). The gender and age demographics are representative of our student body, however there was a higher non-respondent rate in our European students as these students comprised 70% of our entire cohort in the years sampled, while Asian and North American and Canadian comprised 19% and 11%, respectively. Combining the direct entry and GEM students, a total of 81 (25.6%) had completed a previous degree. Twenty-one percent of students were currently studying or had previously studied a research-focused SSC, or had undertaken a significant research programme in a previous degree.
Table 2.
Student demographic characteristics
| Student characteristics | No. respondents | % |
|---|---|---|
| Gender | ||
| Female | 184 | 58.2 |
| Male | 133 | 41.8 |
| Age groups | ||
| 17–20 | 114 | 36.0 |
| 21–23 | 106 | 33.4 |
| 24–29 | 78 | 24.6 |
| 30–40 | 13 | 4.1 |
| Age not given | 6 | 1.9 |
| Student year | ||
| First year | 85 | 26.8 |
| Second year | 80 | 25.2 |
| Third year | 42 | 13.2 |
| Fourth year | 78 | 24.6 |
| Graduate entry (Year 1) | 32 | 10.2 |
| Nationality | ||
| Europe | 196 | 61.8 |
| USA/Canada | 48 | 15.1 |
| Asia and other | 73 | 23.1 |
| Previous degree | ||
| Yes | 81 | 25.6 |
| Summer research placement | ||
| Yes | 9 | 3.8 |
| Research module | ||
| Yes | 67 | 21.1 |
| Awareness of research at UCC | ||
| Totally unaware | 96 | 30.6 |
| Mostly unaware | 158 | 50.3 |
| Somewhat aware | 49 | 15.6 |
| Very aware | 11 | 3.5 |
| Understanding of the term ‘research’ | ||
| Discovering new things | 51 | 16.1 |
| Advancing knowledge | 92 | 29.2 |
| Experimenting/testing hypotheses | 109 | 34.6 |
| Gathering information | 55 | 17.4 |
| Appraising information | 8 | 0.02 |
| Medical research career appeal | ||
| Yes | 155 | 51.5 |
Eighty-one percent of students reported that they were either ‘unaware’ or ‘totally unaware’ of any research activities in their own university. On categorisation of qualitative student statements, the largest proportion understood the term ‘research’ to indicate ‘experimenting and/or testing hypotheses’ with a minority of just eight students who felt that research involves appraising information. Of the total number of students surveyed, over half (51.5%) answered ‘yes’ when asked if a career incorporating medical research appealed.
Perceived competence in transferable and research skills
students' perceived competencies in transferable skills such as communication skills and time management and in research skills such as biological statistics and paper preparation are summarised in Table 3. The majority of students reported higher scores in transferable skills such as teamwork (median score 8/10: percentage in higher competency group = 91.8%) and the ability to work independently (median score 8/10: percentage in higher competency group = 94.6%). A lower proportion reported higher scores in research-specific skills such as designing a study (median score 5/10: percentage in higher competency group = 38.9%) and study sampling (median score 5/10: percentage in higher competency group = 37.7%).
Table 3.
Median and mean scores and percentage competency in transferable and research skills by total students surveyed
| Total surveyed | Total % competency | Gender | Nationality | |||||
|---|---|---|---|---|---|---|---|---|
| Total (N = 317) Med () | Lower competence (%) | Higher competence (%) | Males (N = 133) Med () | Females (N = 184) Med () | US/Canada (N = 48) Med () | Europe (N = 196) Med () | Asian and other (N = 73) Med () | |
| Transferable skill | ||||||||
| 1. Communication–writing | 8.0 (7.3) | 14.8 | 85.2 | 8.0 (7.4) | 7.0 (7.1) | 8.0 (7.8) | 8.0 (7.4) | 6.0 (6.3) |
| 2. Communication–oral | 7.0 (7.3) | 12.9 | 87.1 | 8.0 (7.4) | 7.0 (7.1) | 8.0 (7.5) | 8.0 (7.6) | 6.0 (6.2) |
| 3. Information gathering | 7.0 (6.6) | 24.7 | 75.3 | 7.0 (6.6) | 7.0 (6.5) | 8.0 (7.3) | 7.0 (6.4) | 7.0 (6.6) |
| 4. Information evaluation | 7.0 (6.6) | 23.1 | 76.9 | 7.0 (7.0) | 7.0 (6.4) | 7.0 (7.1) | 7.0 (6.7) | 6.0 (6.4) |
| 5. Numeracy | 8.0 (7.3) | 17.4 | 82.6 | 8.0 (7.6) | 7.0 (7.0) | 7.0 (7.4) | 8.0 (7.4) | 7.0 (6.8) |
| 6. Teamwork | 8.0 (7.8) | 8.2 | 91.8 | 8.0 (7.8) | 8.0 (7.8) | 8.0 (8.0) | 8.0 (8.0) | 7.0 (7.1) |
| 7. Work independently | 8.0 (8.0) | 5.4 | 94.6 | 8.0 (8.1) | 8.0 (7.9) | 9.0 (8.4) | 8.0 (8.1) | 7.0 (7.3) |
| 8. Project management | 7.0 (6.8) | 23.3 | 76.7 | 7.0 (7.0) | 7.0 (6.5) | 8.0 (7.4) | 7.0 (6.7) | 6.0 (6.3) |
| 9. Time management | 7.0 (6.6) | 25.6 | 74.4 | 7.0 (6.6) | 7.0 (6.7) | 7.5 (8.1) | 7.0 (6.6) | 7.0 (6.5) |
| 10. Problem solving | 8.0 (7.4) | 8.2 | 91.8 | 8.0 (7.8) | 7.0 (7.2) | 8.0 (8.0) | 8.0 (7.6) | 7.0 (6.6) |
| Research skill | ||||||||
| 1. Designing a study | 5.0 (4.8) | 61.1 | 38.9 | 5.0 (5.1) | 5.0 (4.6) | 6.0 (5.5) | 5.0 (4.7) | 5.0 (4.8) |
| 2. Study sampling | 5.0 (4.7) | 62.3 | 37.7 | 5.0 (4.9) | 5.0 (4.5) | 5.0 (4.9) | 5.0 (4.5) | 5.0 (4.9) |
| 3. Participant recruitment | 5.0 (5.2) | 54.6 | 45.4 | 5.0 (5.2) | 5.0 (5.2) | 5.0 (4.8) | 5.0 (5.4) | 5.0 (5.0) |
| 4. Biological statistics | 5.0 (4.9) | 58.2 | 41.85 | 5.0 (5.2) | 5.0 (4.7) | 6.0 (5.4) | 5.0 (4.7) | 5.0 (5.0) |
| 5. Paper preparation | 5.0 (5.3) | 52.2 | 47.8 | 6.0 (5.5) | 5.0 (5.1) | 7.0 (6.2) | 5.0 (5.2) | 5.0 (5.0) |
| 6. Paper presenting | 6.0 (5.8) | 38.9 | 61.1 | 6.0 (6.1) | 6.0 (5.5) | 7.0 (6.8) | 6.0 (5.7) | 6.0 (5.3) |
Note: Median (Med), mean () scores by student gender and nationality. All scores were rated on a 10-point scale from low competence to high competence.
We tested students' perceived skills competencies using summary and individual item scores. US/Canadian students rated significantly higher competencies in transferable skills (χ2 = 29.437, p < 0.001) than Asian and European students. US/Canadian students rated significantly higher scores in research-specific skills but only when we excluded the GEM students from the analysis (χ2 = 7.253, p = 0.027). Students with a previous degree had significantly higher competencies in both transferable (Z = –4.21, p < 0.001) and research-specific skills (Z = –2.22, p = 0.026). There were no significant differences in research-specific competencies between students who completed research-focused SSCs or previous research modules and those who had not.
Male students felt significantly more competent than female students with their transferable skills (Z = –2.37, p = 0.018) and with their research-specific skills, study design (Z = –2.03, p = 0.042), biological statistics (Z = –2.03, p = 0.042) and paper presenting (Z = –2.14, p = 0.032). There were significant differences in relation to gender and nationality with male US/Canadians perceiving the most competence in transferable skills (χ2 = 16.306, p < 0.000) but not research-specific skills. Female US/Canadian students felt significantly more competent in terms of transferable skills (χ2 = 13.590, p < 0.001) and research skills competencies (χ2 = 6.266, p = 0.044) than other female students.
When we examined our group of Asian and European students with no prior degree, we found that Asian students had significantly less perceived competence in transferable skills than European students (Z = –3.84, p < 0.000). Although there were no significant differences between male Europeans and male Asians in terms of research-specific skills, female Asian students had significantly greater competencies than female European students with respect to study sampling (Z = –2.33, p = 0.019) and biological statistics (Z = –2.68, p = 0.007).
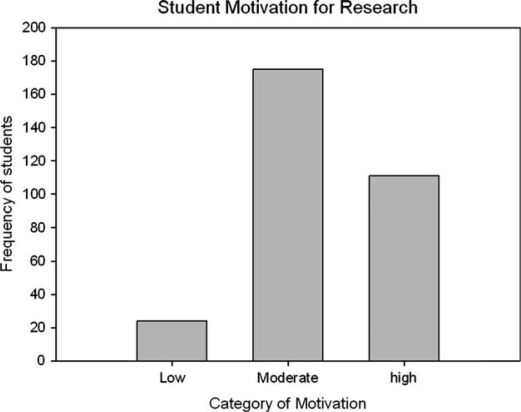
Research motivation
We categorised students' self-rated levels of motivation towards doing research into low, moderate and high, using equal cut-off points (See Fig. 1). Over half the students (56.5%) rated moderate motivation, over one third rated high motivation (35.8%) and just 24 (7.7%) rated low motivation. We found no significant differences between student groups with respect to gender, nationality, year of study, age group, previous degree, career intentions or the appeal of a career incorporating research. We found a statistically significant albeit low correlation between students' perceived competency with their research skills and their motivation towards doing research (Pearson's r = 0.324, p < 0.001).
Fig. 1.
Student Motivation for Research.
When we excluded the GEM (Year 1) students from the analysis, we found that students who had completed a previous degree (mean score = 77.93) were significantly more motivated than those who had not (mean score = 72.55; t = 2.036, p = 0.046). We also found that students who reported a career incorporating medical research as appealing (mean score = 80.20) were significantly more motivated than those who did not (mean score = 66.65; t = 7.114, p < 0.001).
Perceptions of research
Qualitative analysis of student responses (N = 235/317) as to whether a career incorporating medical research appealed elicited predominantly positive responses (Table 4). Five themes were identified: research is necessary to advance and improve (professionally) (N = 75, 32%), it is necessary for career progression (N = 23, 10%) and satisfaction (N = 12, 5%), it is integral to all aspects of medical practice (N = 28, 12%) and it is desirable as a part-time or occasional activity (N = 11, 5%).
Table 4.
Supporting verbatim examples from themes positively oriented towards doing research from ‘following your degree does a career incorporating medical research appeal to you?’
| Theme | Verbatim examples |
|---|---|
| Advance and improve (N = 75) | ‘I think new knowledge is uncovered everyday and I want to be a part of that’ (First year female, age 20) |
| ‘Would like to do some work in developing treatments/disease investigation as well as using said treatments’ (Second year male, age 20) | |
| Career satisfaction (N = 12) | ‘I think it is an important part of a well rounded, successful and enjoyable medical career’ (Third year female, age 20) |
| ‘It is interesting and rewarding, it spices up clinical, it gives true benefit to the profession’ (Fourth year male, age 22) | |
| Career progression (N = 23) | ‘To keep myself informed to produce quality work and further my career’ (Third year female, age 27) |
| ‘I know I will have to do some to achieve other goals in my career such as becoming consultant’ (Fourth year male, age 23) | |
| Integral to practice (N = 28) | ‘Research applies to all fields and I believe that it is imperative to continue it as it is the basis of current practice and will be the basis of future practice’ (Fourth year male, age 22) |
| ‘I believe that new research will help in the progression of the medical field as a whole and help to improve the standard of patient care’ (First year female, age 19) | |
| Part time (N = 11) | ‘I am interested in some research but do not want to focus 100% of my time on it” However I would consider lecturing as this has diversity of activity whilst incorporating research’ (GEM female, age 27) |
| ‘I some way I do want to get involved in new therapy research but not as my 100% job description, part time research does interest me’ (Fourth year male, age 30) |
Over one quarter (N = 60) of the qualitative comments were negative (Table 5). Thematic analysis of these responses suggested that students were reluctant to pursue research because they felt that doing so would isolate them from interaction with people and patients (N = 22, 9%). Another group (N = 31, 13%), themed ‘no appeal’, were strongly against doing research on the basis of its being overly challenging, unstimulating and generally uninteresting. A small cohort (N = 7, 3%) cited previous negative experiences with research. A final group of students (N = 26, 11%) reported that they had not decided if research would form part of their careers, principally because they were unsure about what research entailed.
Table 5.
Supporting verbatim examples from themes negatively oriented towards/unsure about doing research from ‘following your degree does a career incorporating medical research appeal to you?’
| Theme | Verbatim examples |
|---|---|
| People and patients (N = 22) | ‘Because I think I would prefer something more practical and hands on because I see research as being detached life from patients and boring’ (First year male, age 18) |
| ‘I want to practise medicine, deal with people; I don't want to write grants and papers’ (GEM female, age 22) | |
| Negative prior experience (N = 7) | ‘I have researched in the past, does not suit me’ (Third year male, age 28) |
| ‘Have done a bit of lab work and I do not enjoy it that's why I went to med school to get out of research’ (Second year female, age 29) | |
| No appeal (N = 31) | ‘Not at the moment because it seems to take years before you find anything significant’ (Second year female, age 20) |
| ‘I find it hard to motivate myself to do research, find it time consuming’ (Third year male, age 23) | |
| Wait and see (N = 26) | ‘I have not had much exposure yet … however I realise how important it is not only for society but for furthering ones career and this may change in the future following further exposure to research’ (Fourth year female, age 21) |
| ‘At the moment research seems very much beyond me because I am not very confident analysing and reviewing things on my own’ (Second year female, age 21) |
Discussion
Our study has shown that medical students are largely unaware of the research activities in their host institution. Nevertheless, over half reported that they are interested in a career incorporating medical research, and over one fifth have taken a research-based SSC. Students with higher perceived research skills competency are more motivated to pursue research. In their understanding of research, students appear focused on hypothesis testing, advancement of knowledge, data gathering and discovering new things.
There are several limitations to this study. Firstly, our findings are based on self-reports and ratings by medical students from a single medical school. Self-reported measures are commonly used in cross-sectional studies but are subject to participant overestimation and recall bias. Comparison with objective measures such as student research output (written submissions and oral presentation) would help to validate our findings. Secondly, the skills competency items in the CELT-AURS questionnaire, although based on appropriate scales, and modified and piloted for use with medical students, have not been formally standardised. Thirdly, although we attempted to obtain responses from all medical students from 1 to 4 years and the GEM group, we only managed a 60% response rate, and European students are underrepresented in the respondent profile. Finally, our questionnaire did not directly examine students' perceptions of basic versus clinical research, which would have enabled us to gauge the extent of the view that research is distanced from patients and practice.
With regard to research skills, US/Canadian students had significantly higher levels of perceived competency concerning transferable skills and for the individual research skills: study design, paper preparation and paper presentation. This becomes most evident when Year 1 GEM students are excluded from the analysis and raises interesting questions. Do US/Canadian students, all of whom are graduates, arrive to our programme better primed for research training than their European/Asian counterparts? Do they consequently benefit most from research skills training, which becomes evident as they progress through the course, but is not yet apparent in Year 1?
Those with a previous degree reported significantly higher perceived competencies in both transferable and research-specific skills than school-leaver entrants. That students with a previous degree have a better understanding of research methodology has already been reported (28). There were also significantly higher levels of motivation for research among experienced (graduate) students, but only when we excluded the GEM group from the analysis. Overall, a majority of students indicated moderate to high levels of motivation towards doing research. When we tested the full dataset, there were no significant differences between groups in terms of age, gender, nationality or whether a career incorporating research was appealing. However, when we excluded the Year 1 GEM students, we found that students were significantly more motivated if they had completed a previous degree or if they found a career incorporating medical research appealing. Perhaps a previous degree primes research motivation, which is only then expressed as students become more research enabled and can appreciate the relevance of research as they progress in the medical course. Certainly, completion of SSCs and dedicated undergraduate research programmes have been shown to foster interest in research (17, 24) and scientific output (18). Others have found little evidence to support the oft-held premise that graduate entrants tend to be more research active than school leavers (29), so it will be interesting to track our students prospectively.
Surprisingly, there were no significant differences in perceived research competencies between students who had taken a research-focused SSC and those who had not. This initial evaluation would seem to suggest that research-focused SSCs did not significantly influence perceived competencies. However, we suspect that some students are accessing these SSCs in order to address their own perceived deficits, and it is only by analysing perceived competencies before and after such SSCs that a true determination of their impact can be made. This is part of our ongoing research programme in the Medical School. Clearly, the previous educational background of our students influences their research skills confidence and suggests a need for a tailored approach to research skills training in recognition of this.
With regard to gender, male students reported feeling significantly more competent in terms of transferable skills and the individual research-specific skills: study design, biological statistics and paper presenting. We are loath to over interpret these findings, but it merits further investigation as female attrition in MD/PhD schemes is a cause for concern (30–34). US/Canadian males had higher levels of perceived competency than the other two male groups in terms of transferable but not research-specific skills. US/Canadian females had greater perceived competencies in both skills sets than their European and Asian colleagues. European males felt significantly more competent than Asian males with transferable but not with research-specific skills. Female European students reported significantly higher competencies in transferable skills, and Asian females had significantly greater perceived competencies with respect to the research skills, study sampling and biological statistics. Gender and cultural issues, identified as influences in other areas of medical education, also extend to research skills training, and one wonders whether this persists or influences career choice.
Qualitative analysis revealed that a large proportion (N = 75, 32%) of the students who were positive about a career involving research felt that it would enable them to make advances and improvements in the medical field. Other groups of students felt that research is necessary for career progression and satisfaction and is an integral part of being a medical practitioner. There were less students (N = 60, 26%) who were negative about a career incorporating research, reporting that they felt it would be isolating and uninteresting or that they had previous negative experiences. A third group of students indicated that they were still unsure about the appeal of a career in research. That engagement in undergraduate medical research motivates students to pursue further research has been reported (24, 35).
The majority of students appear to be positively motivated towards engaging in research and, if one accepts that the intention to engage in research is highly predictive of doing so, this is reassuring (36). Interestingly, a number of students intend to engage in research activities for purely strategic reasons in order to support their career progression. Their responses do not espouse any true commitment to research activity. This corresponds to findings elsewhere, which indicate that those who have acquired MD PhDs are not necessarily research active (30).
There was a low, albeit significant, correlation between students' perceived competency with research skills and their levels of research motivation. We wonder if the reasons for this could be inferred from the comments of students who were negatively oriented towards research (Table 5). It is interesting that a proportion of our students retain a very traditional impression of research as being distanced from the patient population and from people. It is of concern that students do not fully understand the concepts or processes involved in medical translational research. Ironically, many of their mentors and educators are engaged in active research programmes, but arguably have not been given an opportunity to convey this to the students.
Furthermore, the majority of students are unaware of the research activities at UCC. Their attitudes towards pursuing a career in research mirrors other findings (37), but their lack of awareness of the research activity in their home institution is somewhat surprising given that we have initiatives in place that have addressed this and successfully encouraged student research elsewhere (38). These initiatives include informing students about research opportunities, advertising research events, funding and acknowledgement of student research success, and organising lunch time meetings where staff brief students about their research and invite participation. Two new initiatives are also in development for roll out by the end of the year. The first is an interactive research website for medical students, which will highlight ongoing medical research in the university and provide research skills training resources. The second is a monthly email research newsletter tailored specifically for medical students at UCC. Furthermore, GB and SOF recently received funding from the National Academy for Integration of Research Teaching and Learning (NAIRTL) and the College of Medicine & Health, at UCC, to support medical students' summer research bursaries (6-week project grant) and research travel grants (to present research findings at conferences).
Highly motivated and research-enabled students must be mentored by highly motivated staff. There are obvious incentives for researchers to recruit students to pursue postgraduate qualifications but perhaps less tangible benefits for principal investigators to include students in a research group for shorter periods of time. Funding to support undergraduate medical student research is less available than that for MD, PhD and clinician scientist programmes. Perhaps future programmes should incentivise and mandate the inclusion of undergraduate medical researchers where appropriate. Fostering a supportive undergraduate research environment is recommended (15, 39). It is also essential to examine ways to increase staff engagement in student research. This can be done through formal training in student supervision and protection of staff time for student project work, since gaining access to research supervision has been shown to be challenging for students (28).
Conclusions
There is a need for medical educators to focus on the integration of specific research skills training within all aspects of the undergraduate medical curriculum so that these skills are perceived by undergraduates to be relevant to the routine practice of all doctors and not just those engaged in full-time research. The core curriculum must ensure that relevant and appropriate research expertise is attained by all graduates who are then provided with a suitable foundation from which they can develop such specialised research skills as may be required in their careers. Educators also need to recognise that research skills training needs and research motivation are influenced by previous educational background, research experience and also possibly culture and gender.
We must focus our efforts on introducing and illustrating the concepts of translational research to target the student population who see research as an activity that is totally divorced from patient contact or patient relevance. Promoting institutional research projects, explaining the scope of these to students and involving them is one mechanism for achieving this. We have much work to do to eliminate responses of the ilk, ‘I might like research but I much prefer working with people’. Research is a people-oriented activity, and its output must translate into a tangible change for people or patients. We are not the only school who may have much work to do to convey this message to our undergraduate students. All opportunities to bring research-active staff and research-enthusiastic undergraduates together must be explored and the value of undergraduate research must be recognised by funding authorities.
Acknowledgements
The authors would like to thank Dr Anne Crook and staff at the Centre for Excellence in Teaching and Learning in Applied Undergraduate Research Skills at the University of Reading, UK, for their permission to modify and use their Research Skills Questionnaire. We would especially like to thank our medical students at University College Cork for participating in this study.
LB, SOF and GB designed and implemented the study. LB was involved in the data gathering and analysis and helped to draft the manuscript. SOF and GB helped to analyse the data and to draft the manuscript. All authors read and approved the final manuscript. GB also provided staff funding for this study.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- 1.General Medical Council UK. Tomorrows Doctors, outcomes and standards for undergraduate medical education; 2009. Sep, [Google Scholar]
- 2.Scottish Deans Medical Education Group. 3. Edinburgh, UK: Scottish Deans Medical Education Group; 2009. The Scottish Doctor: learning outcomes for the medical undergraduate in Scotland: a foundation for competent and reflective practitioners. [DOI] [PubMed] [Google Scholar]
- 3.Illing J. Thinking about research: frameworks, ethics and scholarship. Edinburgh, UK: ASME; 2007. [Google Scholar]
- 4.World Federation for Medical Education. International standards in medical education: assessment and accreditation of medical schools educational programmes. A WFME position paper. Med Educ. 1998;32:549–58. doi: 10.1046/j.1365-2923.1998.00302.x. [DOI] [PubMed] [Google Scholar]
- 5.Boninger M, Troen P, Green E, Borkan J, Lance-Jones C, Humphrey A, et al. Implementation of a longitudinal mentored scholarly project: an approach at two medical schools. Acad Med. 2010;85:429–37. doi: 10.1097/ACM.0b013e3181ccc96f. [DOI] [PubMed] [Google Scholar]
- 6.Parsonnet J, Gruppuso PA, Kanter SL, Boninger M. Required vs. elective research and in-depth scholarship programs in the medical student curriculum. Acad Med. 2010;85:405–8. doi: 10.1097/ACM.0b013e3181cccdc4. [DOI] [PubMed] [Google Scholar]
- 7.Varki A, Rosenberg LE. Emerging opportunities and career paths for the young physician–scientist. Nat Med. 2002;8:437–9. doi: 10.1038/nm0502-437. [DOI] [PubMed] [Google Scholar]
- 8.Nathan A. Careers in translational clinical research – historical perspectives, future challenges. JAMA. 2002;18:2424–7. doi: 10.1001/jama.287.18.2424. [DOI] [PubMed] [Google Scholar]
- 9.Wyngaarden JB. The clinical investigator as an endangered species. N Engl J Med. 1979;301:1254–9. doi: 10.1056/NEJM197912063012303. [DOI] [PubMed] [Google Scholar]
- 10.Gill NG. The end of the physician scientist? Am Sch. 1984;53:353–68. [Google Scholar]
- 11.Rosenberg LE. The physician–scientist: an essential – and fragile – link in the medical research chain. J Clin Invest. 1999;103:1621–6. doi: 10.1172/JCI7304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldstein JL, Brown MS. The clinical investigator: bewitched, bothered, and bewildered – but still beloved. J Clin Invest. 1997;99:2803–12. doi: 10.1172/JCI119470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ley TJ, Rosenberg LE. The physician-scientist career pipeline in 2005: build it, and they will come. JAMA. 2005;294:1343–51. doi: 10.1001/jama.294.11.1343. [DOI] [PubMed] [Google Scholar]
- 14.Solomon SS, Tom SC, Pitchert J, Wasserman D, Powers AC. Impact of medical student research in the development of physician–scientists. J Invest Med. 2003;51:149–56. doi: 10.1136/jim-51-03-17. [DOI] [PubMed] [Google Scholar]
- 15.Vujaklija A, Hren D, Sambunjak D, Vodopivec I, Ivanis A, Marusić A, et al. Can teaching research methodology influence students attitude toward science? Cohort study and nonrandomised trial in a single medical school. J Invest Med. 2010;58:282–86. doi: 10.2310/JIM.0b013e3181cb42d9. [DOI] [PubMed] [Google Scholar]
- 16.Gallin EK, Le Blancq SM. Launching a new Fellowship for Medical Students: the first years of the Doris Duke Clinical Research Fellowship Program. J Invest Med. 2005;53:73–81. doi: 10.2310/6650.2005.00202. [DOI] [PubMed] [Google Scholar]
- 17.Steiner H, Breivik J, Siebke M, Tommeras K, Figenschau K, Hansen JB. Evaluation of the medical student research programme in Norwegian medical schools. A survey of students and supervisors. BMC Med Ed. 2009;9:43. doi: 10.1186/1472-6920-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Eyk HJ, Hooiveld HW, Van Leeuwen TN, Van der Wurff BL, De Craen JM, Dekker FW. Scientific output of Dutch medical students. Med Teach. 2010;32:231–5. doi: 10.3109/01421591003596592. [DOI] [PubMed] [Google Scholar]
- 19.Green EP, Borkan JM, Pross SH, Adler SR, Nothnagle M, Parsonnet J, et al. Encouraging scholarship: medical school programs to promote student inquiry beyond the traditional medical curriculum. Acad Med. 2010;85:409–18. doi: 10.1097/ACM.0b013e3181cd3e00. [DOI] [PubMed] [Google Scholar]
- 20.Robinson L, Drewery S, Ellershaw J, Smith J, Whittle S, Murdoch-Eaton D. Research governance: impeding both research and teaching? A survey of impact on undergraduate research opportunities. Med Ed. 2007;41:729–36. doi: 10.1111/j.1365-2923.2007.02776.x. [DOI] [PubMed] [Google Scholar]
- 21.Detsky MED, Detsky AS. Encouraging medical students to do research and write papers. CMAJ. 2007;176(12):1719–21. doi: 10.1503/cmaj.061628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rivera JA, Levine RB, Wright SM. Completing a scholarly project during residency training. Perspectives of residents who have been successful. J Gen Intern Med. 2005;20:366–9. doi: 10.1111/j.1525-1497.2005.04157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Alliance for Physician Competence. Good medical practice – USA: the National Alliance. Version 1.0. 2007. Available from: http://www.gmpusa.org.
- 24.Bierer B, Chen HC. How to measure success: the impact of scholarly concentrations on students – a literature review. Acad Med. 2010;85:438–52. doi: 10.1097/ACM.0b013e3181cccbd4. [DOI] [PubMed] [Google Scholar]
- 25.Murdoch Eaton D, Drewery S, Elton S, Emmerson C, Marshall M, Smith JA, et al. What do medical students understand by research and research skills? Identifying research opportunities within undergraduate projects. Med Teach. 2010;32:e152–60. doi: 10.3109/01421591003657493. [DOI] [PubMed] [Google Scholar]
- 26.Christophel DM. The relationship among teacher immediacy behaviours, student motivation and learning. Commun Educ. 1990;39:323–40. [Google Scholar]
- 27.Beatty MJ. Student motivation scale. In: Rubin RB, Palmgreen P, Snyder HE, editors. Communication research measures: a sourcebook. New York: Guilford Press; 1994. pp. 343–6. [Google Scholar]
- 28.Siemens DR, Punnen S, Wong J, Kanji N. A survey on the attitudes towards research in medical school. BMC Med Ed. 2010;10:4. doi: 10.1186/1472-6920-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rolfe I, Ringland EC, Pearson S. Graduate entry to medical school? Testing some assumptions. Med Educ. 2004;38:778–86. doi: 10.1111/j.1365-2929.2004.01891.x. [DOI] [PubMed] [Google Scholar]
- 30.Andriole DA, Whelan AJ, Jeffe DB. Characteristics and career intentions of the emerging MD/PhD workforce. JAMA. 2008;300:1165–73. doi: 10.1001/jama.300.10.1165. [DOI] [PubMed] [Google Scholar]
- 31.Ghali WA, Saitz R, Eskew AH, Gupta M, Quan H, Hershman WY. Successful teaching in evidence-based medicine. Med Educ. 2000;34:18–22. doi: 10.1046/j.1365-2923.2000.00402.x. [DOI] [PubMed] [Google Scholar]
- 32.Parkes J, Hyde C, Deeks J, Milne R, Pujol-Ribera E, Foz G, et al. Teaching critical appraisal skills in health care settings. Cochrane Database Syst Rev. 2001;3:CD001270. doi: 10.1002/14651858.CD001270. [DOI] [PubMed] [Google Scholar]
- 33.Shaneyfelt T, Baum KD, Bell D, Feldstein D, Houston TK, Kaatz S, et al. Instruments for evaluating education in evidence-based practice: a systematic review. JAMA. 2006;296:1116–27. doi: 10.1001/jama.296.9.1116. [DOI] [PubMed] [Google Scholar]
- 34.Rosenberg LE. MD/PhD programs – a call for an accounting. JAMA. 2008;300:1208–9. doi: 10.1001/jama.300.10.1208. [DOI] [PubMed] [Google Scholar]
- 35.Jacobs CD, Cross PC. The value of medical student research: the experience at Standford University School of Medicine. Med Educ. 2005;29:342–6. doi: 10.1111/j.1365-2923.1995.tb00023.x. [DOI] [PubMed] [Google Scholar]
- 36.Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Soc Psychol. 2001;40:471–99. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 37.Hren D, Lukic IK, Marušić A, Vodopivec I, Vujaklija A, Hrabak M, et al. Teaching research methodology in medical schools: students' attitudes towards and knowledge about science. Med Educ. 2004;38:81–6. doi: 10.1111/j.1365-2923.2004.01735.x. [DOI] [PubMed] [Google Scholar]
- 38.Zier K, Stagnaro-Green A. A multifaceted program to encourage medical students' research. Acad Med. 2001;76:743–7. doi: 10.1097/00001888-200107000-00021. [DOI] [PubMed] [Google Scholar]
- 39.Mark AL, Kelch RP. Clinical scientist training programme: a proposal for training medical students in clinical research. J Invest Med. 2001;46:486–90. doi: 10.2310/6650.2001.33624. [DOI] [PubMed] [Google Scholar]