Abstract
OBJECTIVES
Although cognitive impairment and depressive symptoms are associated with functional decline, it is not understood how these risk factors act together to affect the risk of functional decline. The purpose of this study is to determine the relative contributions of cognitive impairment and depressive symptoms on decline in activity of daily living (ADL) function over 2 years in an older cohort.
DESIGN
Prospective cohort study.
SETTING
A U.S. national prospective cohort study of older people, Asset and Health Dynamics in the Oldest Old.
PARTICIPANTS
Five thousand six hundred ninety-seven participants (mean age 77, 64% women, 86% white) followed from 1993 to 1995
MEASUREMENTS
Cognitive impairment and depressive symptoms were defined as the poorest scores: 1.5 standard deviations below the mean on a cognitive scale or 1.5 standard deviations above the mean on validated depression scales. Risk of functional decline in participants with depressive symptoms, cognitive impairment, and both, compared with neither risk factor, were calculated and stratified by baseline dependence. Analyses were adjusted for demographics and comorbidity.
RESULTS
Eight percent (n = 450) of subjects declined in ADL function. In participants who were independent in all ADLs at baseline, the relative risk (RR) of 2-year functional decline was 2.3 (95% confidence interval (CI) = 1.7–3.1) for participants with cognitive impairment, 1.9 (95% CI = 1.3–2.6) for participants with depressive symptoms, and 2.4 (95% CI = 1.4–3.7) for participants with cognitive impairment and depressive symptoms. In participants who were dependent in one or more ADLs at baseline, RR of 2-year functional decline was 1.9 (95% CI = 1.2–2.8) for participants with cognitive impairment, 0.6 (95% CI = 0.3–1.3) for participants with depressive symptoms, and 1.5 (95% CI = 0.8–2.6) for participants with cognitive impairment and depressive symptoms.
CONCLUSIONS
In participants with no ADL dependence at baseline, cognitive impairment and depressive symptoms are risk factors for decline, but that, in participants with dependence in ADL at baseline, cognitive impairment, but not depressive symptoms, is a risk factor for additional decline.
Keywords: physical functioning, functional decline, activities of daily living, cognitive impairment, depressive symptoms
One of the most pressing problems for adults as they age is maintaining independence in functioning. U.S. national statistics indicate that 20% of noninstitutionalized people who are aged 70 and older need help in performing at least one activity of daily living (ADL), including bathing, dressing, eating, toileting, and transferring.1 Maintaining functional independence is also important because of increasing caregiver burden and healthcare costs.
The relationship between cognitive status and depressive symptoms and their effect on functional decline is of significant clinical and public health importance because they are common, frequently coexist, and may be treatable. For example, depressive symptoms are thought to exacerbate cognitive problems in older people and may be an independent risk factor for cognitive impairment; conversely, cognitive impairment may lead to depression.2–4
Prior studies on the effect of cognitive impairment or depressive symptoms on functional decline have suggested that depressive symptoms and cognitive impairment are independently associated with functional decline,4–13 but prior studies are limited because they have not taken into consideration that cognitive impairment and depressive symptoms are interrelated, have not studied ethnically diverse populations, or have not evaluated these risk factors by degree of baseline functional dependence.
We designed this study to test three hypotheses underlying the triad of cognitive impairment, depressive symptoms, and functional decline; first, that cognitive impairment and depressive symptoms are independent predictors of functional decline; second, that cognitive impairment and depressive symptoms act synergistically to potentiate the risk of functional decline, such that the risk of functional decline associated with having both risk factors is greater than that predicted by either alone; and third, we tested whether baseline ADL dependence affects the relationship between cognitive impairment, depressive symptoms, and functional decline.
This study tests these hypotheses by analyzing data from a longitudinal cohort study of older Americans. Advantages of our study include use of a large nationally representative, ethnically diverse cohort; adjustment for a large number of potential confounders; and an analytic strategy that accounted for the combined effects of depressive symptoms and cognition in predicting functional decline.
METHODS
Study Population
The Asset and Health Dynamics Among the Oldest Old (AHEAD) study is a biennial national prospective study, formulated as a supplement to the community-based Health and Retirement Study.14 In 1993, the U.S. birth cohorts of 1923 and earlier formed the sample frame for AHEAD. For the current study, we included primary respondents, who did not respond through a proxy (n = 6,656). Because we were interested in 2-year functional decline, our analytic cohort consisted of the 5,697 persons who completed both study waves, in 1993 and 1995 (607 participants had died, 341 were lost to follow-up, and 11 were missing functional status information).
A full description of the weighting procedures used in the AHEAD study was outlined previously.15 Blacks, Hispanics, and Florida state residents were oversampled. The AHEAD study employed telephone and in-person interviews at baseline and follow-up.
Cognitive Impairment and Depressive Symptoms Measurement
Several tests of cognitive function were measured in AHEAD at both waves. Memory was tested using an immediate and delayed free-recall test, in which 10 high-frequency nouns were given. The participant was asked to recall as many of the nouns as possible immediately and after a 5-minute delay and given a score of 0 to 10, one point for each correct noun. Calculation was assessed using the serial 7s test, in which participants start with 100 and consecutively subtract 7 five times, and were given one point for each correct subtraction, for a total of five points. In addition, the participant was asked to count backwards from 20 to 10 and 86 to 76; and name the month, day, year, day of the week, the object used to cut paper (scissors), the plant that lives in the desert (cactus), and the President and Vice President of the United States, for a total of 10 points, one point for each correct answer. An overall cognitive score was calculated as the sum of all cognitive tests, for a total of 35 points.16 We defined cognitive impairment to be present in subjects with scores lower than 1.5 standard deviations below the mean baseline overall cognitive score, or 11 points. Herzog et al. have reported on the cognitive scale used in AHEAD, including information on its validity.16
Depressive symptoms were assessed using eight items from the Center for Epidemiologic Study Depression (CES-D) scale.17 Specifically, participants were asked whether the following feelings had occurred during the prior week: depression, lack of happiness, loneliness, sadness, that everything was an effort, sleep was restless, inability to “get going,” and lack of energy. Each question was assigned one point, for a total of eight. We identified participants with a score 1.5 standard deviations above the mean baseline CES-D score (>4 points) as having depressive symptoms.18
Functional Decline Definition
Our primary measure of functional status at baseline was dependence in each of the six ADLs, defined as needing the help of another person with bathing, toileting, transferring, walking, dressing, and eating.19 An ADL dependence score was calculated, assigning one point for each of the activities in which a subject was dependent, at baseline and follow-up. We defined functional decline to be present if a subject had a greater number of ADL dependencies at follow-up than at baseline.
Other Measurements
Other measurements included sociodemographic characteristics (age, years of education, gender, race, and marital status), self-reported history of comorbid and medical conditions (vision problems, hearing problems, stroke, heart disease, hypertension, psychiatric illness other than depressive symptoms, lung disease, arthritis, cancer and diabetes mellitus), lifestyle characteristics (self-reported smoking and alcohol consumption), and total household income.
Statistical Analyses
All statistical analyses applied sampling weights to AHEAD data to account for oversampling in this study’s design. Chi-square and t test statistics were performed to assess the unadjusted association between potential confounders (sociodemographic characteristics, medical comorbidities, lifestyle characteristics) and the two main predictors (cognitive impairment and depressive symptoms) and between the confounders and the primary outcome (functional decline). Bivariate analyses were then conducted to assess the unadjusted association between cognitive impairment or depressive symptoms and functional decline. Bivariate analyses of cognitive impairment, depressive symptoms, and individual ADL dependence were also assessed. Using linear regression, we examined the relationship between cognitive impairment and depressive symptoms at baseline and number of ADL dependencies at follow-up. To examine the independent relationship between depressive symptoms and functional decline and between cognitive impairment and functional decline, we constructed a series of generalized linear and logistic regression models. In the first model, we simultaneously controlled for depressive symptoms and cognitive impairment (Model 1). In the second model, we created a series of multiple dichotomous indicator variables for baseline cognitive impairment alone, depressive symptoms alone, depressive symptoms and cognitive impairment together, and neither depressive symptoms nor cognitive impairment, to better understand the combined effects of cognitive impairment and depressive symptoms (Model 2). These models were then adjusted for sociodemographic characteristics, comorbid conditions, and economic factors that were predictors (P < .05) of functional decline in bivariate analyses (Models 3 and 4). Each of these models was stratified by whether the participant was dependent in one or more ADLs at baseline. Lastly, we constructed generalized linear models with a dependent variable of ADL score at Wave 2, stratified by ADL dependence at Wave 1. From the model, we estimated the marginal mean ADL score at 1993 and 1995 for the following groups: cognitive impairment alone, depressive symptoms alone, depressive symptoms and cognitive impairment, and neither depressive symptoms nor cognitive impairment (see Figures 1 and 2). These models included a depressive symptom by cognitive impairment interaction term.
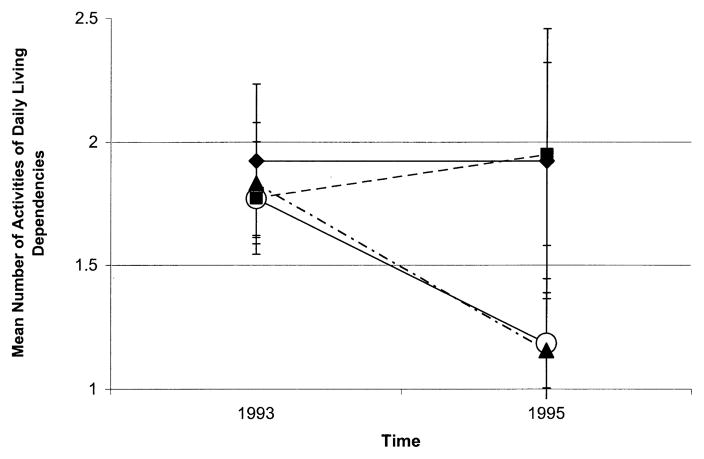
Figure 1.
Functional dependence according to cognitive impairment and depressive symptoms in participants who were dependent in activities of daily living at baseline (n = 525).
○ = Neither cognitive impairment nor depressive symptoms
□ = Cognitive impairment only
▲ = Depressive symptoms only
◆ = Cognitive impairment and depressive symptoms
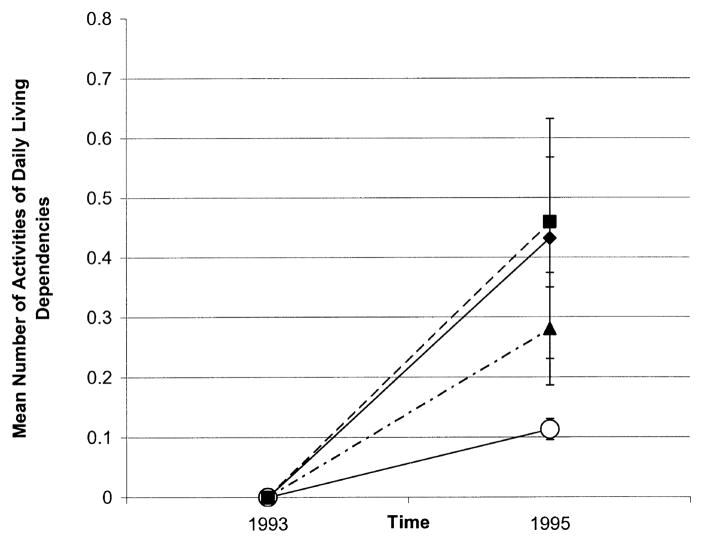
Figure 2.
Functional dependence according to cognitive impairment and depressive symptoms in participants who were independent in activities of daily living at baseline (incident dependence) (n = 5,172).
○ = Neither cognitive impairment nor depressive symptoms
□ = Cognitive impairment only
▲ = Depressive symptoms only
◆ = Cognitive impairment and depressive symptoms
Because odds ratios can sometimes overestimate the degree of association between predictor and outcome variables, we used the method of Zhang et al.20 to convert the odds ratios calculated in logistic regression analyses to approximate relative risks.
RESULTS
The mean age of the study population was 77; 64% were women and 86% were white (Table 1). Participants had an average of three comorbid conditions.
Table 1.
Baseline Characteristics of the 5,697 Participants in the Asset and Health Dynamics in the Oldest Old Study
| Baseline Characteristic | Value |
|---|---|
| Age, mean years ± SD | 77 ± 5.5 |
| Female, % | 64 |
| Education <high school, % | 39 |
| White, % | 86 |
| Black, % | 10 |
| Hispanic/other, % | 4 |
| Married, % | 50 |
| Current smoker, % | 9 |
| ≥1 Alcoholic drink/day, % | 12 |
| Number of comorbid conditions, mean ± SD | 3 ± 1.7 |
| High blood pressure, % | 50 |
| Diabetes mellitus, % | 12 |
| Cancer, % | 13 |
| Heart disease, % | 30 |
| Lung disease, % | 10 |
| Arthritis, % | 25 |
| Psychiatric disease, not depression, % | 11 |
| Vision problems, % | 23 |
| Hearing problems, % | 23 |
Note: Missing data: current smoker, 0.01%; ≥1 alcoholic drink/day, 0.05%; hearing problems, 0.02%; cancer, 0.04%; high blood pressure and diabetes mellitus, 0.09%; heart disease, 0.06%; vision problems, 0.11%; and hearing problems, 0.02%. SD = standard deviation.
At baseline, 547 participants had depressive symptoms (9.6%) and 610 had cognitive impairment (10.7%). Participants with cognitive impairment or depressive symptoms were older than participants with neither condition, (78 vs. 77 years, P < .0001, and 80 vs. 77 years, P < .0001, respectively). Depressive symptoms and cognitive impairment were modestly associated with each other (r = .22, P < .001). Participants with cognitive impairment were more likely to have depressive symptoms than participants without cognitive impairment (23% vs. 8%, P < .001). Nine percent of participants (n = 525) had ADL dependence at baseline, and almost 8% (n = 451) experienced functional decline over the 2-year follow-up period. Age, education, race, gender, marital status, medical comorbidities, smoking, alcohol use, Medicare insurance use, and income were associated with functional decline (P < .05 for all). Cognitive impairment and depressive symptoms were most strongly associated with dependence in bathing, followed by dressing, walking, and transferring.
Cognitively impaired individuals were more than three times as likely to have subsequent functional decline than nonimpaired individuals (Table 2, Model 1), with a relative risk (RR) of 3.3 (95% confidence interval (CI) = 2.8– 4.0). Depressed individuals were twice as likely to have subsequent decline as nondepressed individuals (RR = 2.1, 95% CI = 1.7–2.6). Simultaneous assessment of cognitive impairment, depressive symptoms, and both (Table 2, Model 2) result in effect sizes similar to those in Model 1, with only a slightly higher effect size for depressive symptoms and cognitive impairment together (RR = 3.8, 95% CI = 2.8–5.2) than for cognitive impairment alone (RR = 3.5, 95% CI = 2.8–4.3).
Table 2.
Cognitive Impairment, Depressive Symptoms, and Relative Risk of 2-Year Functional Decline, Bivariate Results
| Model | Participant Group | Functional Decline* % | Relative Risk (95% Confidence Interval) |
|---|---|---|---|
| 1 | All participants (n = 5,697)† | 8 | |
| Cognitive impairment (n = 610)‡ | 21 | 3.3 (2.8–4.0) | |
| No impairment (n = 5,104) | 6 | 1.0 | |
| Depressive symptoms (n = 547)§ | 15 | 2.1 (1.7–2.6) | |
| No depressive symptoms (n = 5,167) | 7 | 1.0 | |
| 2 | Cognitive impairment and depressive symptoms (n = 139) | 22 | 3.8 (2.8–5.2) |
| Cognitive impairment alone (n = 471) | 20 | 3.5 (2.8–4.3) | |
| Depressive symptoms alone (n = 408) | 13 | 2.1 (1.6–2.8) | |
| Neither depressive symptoms nor cognitive impairment (n = 4,696) | 6 | 1.0 |
An increased dependence in an activity of daily living from 1993–1995.
Applying study weights to 5,697 Asset and Health Dynamics in the Oldest Old (AHEAD) participants yielded an analytic sample of 5,714.
Participants whose scores on the multi-domain AHEAD cognition scale were ≤ 1.5 standard deviations below the mean.
Participants whose scores on the Center for Epidemiologic Study Depression Scale were ≥ 1.5 standard deviations above the mean.
In a linear regression model, in which our outcome was number of dependent ADLs at follow-up, cognitive impairment at baseline was associated with 0.31 (95% CI = 0.24–0.37) more ADL dependencies at follow-up, whereas depressive symptoms at baseline were associated with 0.04 (95% CI = −0.03–0.10) more dependencies at follow-up.
Table 3 reports the likelihood of experiencing functional decline according to cognitive impairment and depressive symptoms after multivariate adjustment and stratification by baseline dependence. For participants who were dependent in ADLs at baseline, cognitive impairment increased the risk of further decline (RR = 1.9, 95% CI = 1.2–2.8), but depressive symptoms did not (RR = 0.6, 95% CI = 0.3–1.3). In addition, there was no evidence of additive effects for participants who had both risk factors (RR = 1.5, 95% CI = 0.8–2.6).
Table 3.
Cognitive Impairment, Depressive Symptoms, and Relative Risk of 2-Year Functional Decline, Multivariate Results, by Baseline Activities of Daily Living Status (N = 5,697)
| Relative Risk (95% Confidence Interval)* |
|||
|---|---|---|---|
| Model | Participant Group | Dependent at Baseline (n = 525) | Independent at Baseline (n = 5,172) |
| 3 | Cognitive impairment | 1.9 (1.3–2.7) | 2.2 (1.6–2.8) |
| No impairment | 1 | 1 | |
| Depressive symptoms | 0.8 (0.5–1.2) | 1.7 (1.3–2.2) | |
| No depressive symptoms | 1 | 1 | |
| 4 | Cognitive impairment alone | 1.9 (1.2–2.8) | 2.3 (1.7–3.1) |
| Depressive symptoms alone | 0.6 (0.3–1.3) | 1.9 (1.3–2.6) | |
| Cognitive impairment and depressive symptoms | 1.5 (0.8–2.6) | 2.4 (1.4–3.7) | |
| Neither depressive symptoms nor cognitive impairment | 1 | 1 | |
Full adjustment for age, education, race, gender, marital status, medical comorbidities, smoking and alcohol use, Medicare insurance, and income.
For participants who were independent at baseline, cognitive impairment (RR = 2.3, 95% CI = 1.7–3.1) and depressive symptoms (RR = 1.9, 95% CI = 1.3–2.6) together predicted the risk of incident functional decline. In addition, participants with cognitive impairment and epressive symptoms had slightly higher risk than either alone (RR = 2.4, 95% CI = 1.4–3.7).
Figure 1 illustrates the relationship between cognitive impairment, depressive symptoms, and ADL score in participants with baseline ADL dependence. On average, participants with neither risk factor tended to have less functional dependence over the 2-year interval (by 0.56 ADLs, 95% CI = 0.40–0.72), similar to participants with depressive symptoms alone (by 0.69 ADLs, 95% CI = 0.30–0.88). Participants with cognitive impairment alone had more dependence (by 0.01 ADLs, 95% CI = −0.27–0.29). Participants with cognitive impairment and depressive symptoms at baseline had the highest number of baseline dependencies (1.9) and changed little over the 2-year follow-up interval. The model term for depressive symptoms by cognitive impairment was not statistically significant (P = .75) when the analysis was restricted to participants with ADL dependence at baseline. Thus, in participants with baseline ADL dependence, there was no evidence for interaction of depressive symptoms and cognitive impairment for further functional dependence over 2 years.
Figure 2 illustrates the relationship between cognitive impairment and depressive symptoms in all participants who were independent at baseline (incident ADL dependence). Participants with neither cognitive impairment nor depressive symptoms changed little over the follow-up period (0.11 ADLs, 95% CI = 0.10–0.13 dependencies). Those with cognitive impairment at baseline become more dependent, (decline = 0.39 points, 95% CI = 0.32–0.46 ADLs) similar to participants with depressive symptoms (decline = 0.28, 95% CI = 0.20–0.34 ADLs) and a similar mean to participants with cognitive impairment and depressive symptoms (0.39, 95% CI = 0.26–0.52 ADLs). The model term for depressive symptoms by cognitive impairment was borderline statistically significant (P = .05) when the analysis was restricted to participants with no baseline ADL dependencies.
DISCUSSION
Our results from a population-based longitudinal study of 5,697 older people followed for 2 years provide data that clarify the relationship between cognitive impairment, depressive symptoms, and functional decline. First, cognitive impairment and depressive symptoms are independent predictors of ADL dependence in participants who are independent in all ADLs at baseline. In addition, in these participants, cognitive impairment and depressive symptoms were robust risk factors; those with both risk factors had a slightly greater risk of decline than those with either risk factor alone. Second, in participants who already had ADL dependence at baseline, cognitive impairment was associated with further decline, whereas depressive symptoms were not.
In participants who are independent in ADLs at baseline, cognitive impairment and depressive symptoms are independent predictors of functional decline, even after adjusting for each other. This suggests that both risk factors contribute to incident ADL dependence and do not simply act via each other. This is consistent with prior work by Gill et al. that demonstrates that the risk of functional dependence steadily increases as the degree of baseline vulnerability increases.11 Cognitive impairment and depressive symptoms may lead to an erosion of the physical skills needed to maintain functional independence and may leave a person less resistant to acute stressors, such as hospitalization, that often accelerate functional dependence in older people.21–23
In participants with baseline ADL dependence, cognitive impairment predicted further loss of ADL function, but depressive symptoms did not predict further functional decline, and, in fact, subjects with depressive symptoms, on average, demonstrated a slight improvement in ADL function, similar to subjects with neither condition. This may reflect fundamental differences in the natural history of cognitive impairment and depressive symptoms. In general, cognitively impaired participants deteriorate progressively over time. As a result, participants who have experienced functional decline secondary to cognitive impairment are likely to experience further functional decline as the cognitive impairment worsens. In contrast, depressive symptoms often improve, especially if effective treatment is administered. As a result, in participants with functional decline, the presence of depressive symptoms may be a marker for potential reversibility.
Prior studies that have evaluated depressive symptoms and cognitive function have suggested that depressive symptoms or cognitive impairment may predict functional decline, with varied effect sizes.4–13 The variance in prior reports may be due to lack of stratification by baseline ADL function, incomplete adjustment of confounders, or use of nonvalidated assessment of cognitive function or depressive symptoms. Our results describing incident ADL dependence are in accord with the few studies that have discussed the two risk factors together and have found cognitive impairment and depressive symptoms to be significant predictors in multivariate models.12,13 Because the current study undertook to stratify by ADL at baseline, adjusted for a large number of covariates, and used validated instruments for evaluation of cognitive impairment and depression, it was able to better clarify the independent and combined effects of cognitive impairment and depressive symptoms on functional decline.
Several limitations deserve comment. First, there is a potential attrition bias because of differential mortality, a factor common to studies of older people. For this cohort, participants who died had greater ADL dependence and more cognitive impairment and depressive symptoms at baseline. Second, the cognitive scale developed for AHEAD is unfamiliar, and thus the results may not be widely generalizable, but the AHEAD cognitive scale contains similar questions to the Mini-Mental State Examination, (MMSE)24 and has some evidence of construct validity.16 Alternatively, the MMSE itself has limitations, and the AHEAD cognitive scale may share these limitations. For example, the MMSE is insensitive to the cognitive effects of frontal system lesions. In particular, frontal system lesions may affect executive control functions, and executive control is not well measured by the MMSE.25 Because frontal system lesions are associated with disability26 and depression,27 there is a danger that cognitive deficits not detected by the AHEAD instrument may be mediating the apparent association between ADL function and depressive symptoms. Finally, there are potential limitations in the measurement of our primary outcome, change in ADL function, based on self-reports, but we do not believe that these limitations lessen the generalizability of these findings, because there is some evidence that the assessment of ADL is reliable in older populations, even those with cognitive problems.28,29
We also did not have information on the severity of ADL dependence, because dependence was assessed as a dichotomous yes/no response. Future studies could develop a gradient of dependence including questions about the nature of the help received, how often it was received, and how much activity could be performed if alone.
By describing the relationships between depressive symptoms, cognitive impairment, and functional decline, this study adds further insight into the factors responsible for functional decline. In addition, cognition and depressive symptoms may serve as targets for intervention, but this requires further study. Studies that address whether treatment of early depression by antidepressant medication, improving social networks, and addressing the potential effects of alcohol intake are warranted to determine whether these can prevent functional decline. Similarly, using current therapies and the development of new therapies for treating cognitive impairment may reduce concurrent ADL dependence and prevent increased decline.
This study suggests that depressive symptoms and cognitive impairment are independent predictors of incident ADL dependence. In addition, cognitive impairment is a more robust predictor of incident functional decline than are depressive symptoms because cognitive impairment predicts functional decline in subjects with and without baseline ADL dependence. Following from these results, early and adequate evaluation and treatment of cognitive problems and depressive symptoms are suggested. Future studies on the effect of treatment for depression and cognitive problems on functional decline outcome are warranted.
Acknowledgments
This project was supported by Grant R01AG19827-01 from the National Institute on Aging. Dr. Mehta was supported in part by a training grant from the National Institute on Aging (T32-AG00212–08), Dr. Yaffe by a patient-oriented research development award from the National Institute on Aging (K23-AG00888), and Dr. Covinsky by an independent scientist award from the Agency for Healthcare Research and Quality (K02 HS00006–01). Drs. Covinsky and Yaffe are Paul Beeson faculty scholars in aging research.
References
- 1.Kramarow E, Rooks R, Weeks J, et al. Health, United States, 1999. Hyattsville, MD: National Center for Health Statistics; 1999. Health and Aging Chartbook. [Google Scholar]
- 2.Yaffe K, Blackwell T, Gore R, et al. Depressive symptoms and cognitive decline in nondemented elderly women: A prospective study. Arch Gen Psychiatry. 1999;56:425–430. doi: 10.1001/archpsyc.56.5.425. [DOI] [PubMed] [Google Scholar]
- 3.Parmelee PA, Kleban MH, Lawton MP, et al. Depression and cognitive change among institutionalized aged. Psychol Aging. 1991;6:504–511. doi: 10.1037//0882-7974.6.4.504. [DOI] [PubMed] [Google Scholar]
- 4.Gallo JJ, Rabins PV. Depression without sadness: Alternative presentations of depression in late life. Am Fam Physician. 1999;60:820–826. [PubMed] [Google Scholar]
- 5.Cronin-Stubbs D, de Leon CF, Beckett LA, et al. Six-year effect of depressive symptoms on the course of physical disability in community-living older adults. Arch Intern Med. 2000;160:3074–3080. doi: 10.1001/archinte.160.20.3074. [DOI] [PubMed] [Google Scholar]
- 6.Penninx BW, Leveille S, Ferrucci L, et al. Exploring the effect of depression on physical disability: Longitudinal evidence from the Established Populations for Epidemiologic Studies of the Elderly. Am J Public Health. 1999;89:1346–1352. doi: 10.2105/ajph.89.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ormel J, Kempen GI, Deeg DJ, et al. Functioning, well-being, and health perception in late middle-aged and older people: Comparing the effects of depressive symptoms and chronic medical conditions. J Am Geriatr Soc. 1998;46:39–48. doi: 10.1111/j.1532-5415.1998.tb01011.x. [DOI] [PubMed] [Google Scholar]
- 8.Sarkisian CA, Liu H, Gutierrez PR, et al. Modifiable risk factors predict functional decline among older women: A prospectively validated clinical prediction tool. The Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 2000;48:170–178. doi: 10.1111/j.1532-5415.2000.tb03908.x. [DOI] [PubMed] [Google Scholar]
- 9.Seeman TE, Bruce ML, McAvay GJ. Social network characteristics and onset of ADL disability: MacArthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 1996;51:S191–S200. doi: 10.1093/geronb/51b.4.s191. [DOI] [PubMed] [Google Scholar]
- 10.Bruce ML, Seeman TE, Merrill SS, et al. The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. Am J Public Health. 1994;84:1796–1799. doi: 10.2105/ajph.84.11.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gill TM, Richardson ED, Tinetti ME. Evaluating the risk of dependence in activities of daily living among community-living older adults with mild to moderate cognitive impairment. J Gerontol A Biol Sci Med Sci. 1995;50:M235–M241. doi: 10.1093/gerona/50a.5.m235. [DOI] [PubMed] [Google Scholar]
- 12.Tinetti ME, Inouye SK, Gill TM, et al. Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA. 1995;273:1348–1353. [PubMed] [Google Scholar]
- 13.Ho SC, Woo J, Yuen YK, et al. Predictors of mobility decline: The Hong Kong old-old study. J Gerontol A Biol Sci Med Sci. 1997;52A:M356–M362. doi: 10.1093/gerona/52a.6.m356. [DOI] [PubMed] [Google Scholar]
- 14.Myers GC, Juster FT, Suzman RM. Asset and Health Dynamics Among the Oldest Old (AHEAD): Initial results from the longitudinal study. Introduction. J Gerontol B Psychol Sci Soc Sci. 1997;52B:v–viii. (Spec No) [PubMed] [Google Scholar]
- 15.Heeringa S. Technical Description of the Asset and Health Dynamics Survey Sample Design. Ann Arbor, MI: Institute for Social Research, University of Michigan; 1995. [Google Scholar]
- 16.Herzog AR, Wallace RB. Measures of cognitive functioning in the AHEAD Study. J Gerontol B Psychol Sci Soc Sci. 1997;52B(Spec):37–48. doi: 10.1093/geronb/52b.special_issue.37. [DOI] [PubMed] [Google Scholar]
- 17.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 18.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: Criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Arch Intern Med. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- 19.Rodgers W, Miller B. A comparative analysis of ADL questions in surveys of older people. J Gerontol B Psychol Sci Soc Sci. 1997;52B(Spec):21–36. doi: 10.1093/geronb/52b.special_issue.21. [DOI] [PubMed] [Google Scholar]
- 20.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 21.Covinsky KE, Kahana E, Chin MH, et al. Depressive symptoms and 3-year mortality in older hospitalized medical patients. Ann Intern Med. 1999;130:563–569. doi: 10.7326/0003-4819-130-7-199904060-00004. [DOI] [PubMed] [Google Scholar]
- 22.Roach MJ, Connors AF, Dawson NV, et al. Depressed mood and survival in seriously ill hospitalized adults. The SUPPORT Investigators. Arch Intern Med. 1998;158:397–404. doi: 10.1001/archinte.158.4.397. [DOI] [PubMed] [Google Scholar]
- 23.Covinsky KE, Fortinsky RH, Palmer RM, et al. Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons. Ann Intern Med. 1997;126:417–425. doi: 10.7326/0003-4819-126-6-199703150-00001. [DOI] [PubMed] [Google Scholar]
- 24.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 25.Royall DR. Executive cognitive impairment: A novel perspective on dementia. Neuroepidemiology. 2000;19:293–299. doi: 10.1159/000026268. [DOI] [PubMed] [Google Scholar]
- 26.Cahn-Weiner DA, Malloy PF, Boyle PA, et al. Prediction of functional status from neuropsychological tests in community-dwelling elderly individuals. Clin Neuropsychol. 2000;14:187–195. doi: 10.1076/1385-4046(200005)14:2;1-Z;FT187. [DOI] [PubMed] [Google Scholar]
- 27.Royall DR. Frontal systems impairment in major depression. Semin Clin Neuropsychiatry. 1999;4:13–23. doi: 10.1053/SCNP00400013. [DOI] [PubMed] [Google Scholar]
- 28.Magaziner J, Simonsick EM, Kashner TM, et al. Patient-proxy response comparability on measures of patient health and functional status. J Clin Epidemiol. 1988;41:1065–1074. doi: 10.1016/0895-4356(88)90076-5. [DOI] [PubMed] [Google Scholar]
- 29.Weinberger M, Samsa GP, Schmader K, et al. Comparing proxy and patients’ perceptions of patients’ functional status: Results from an outpatient geriatric clinic. J Am Geriatr Soc. 1992;40:585–588. doi: 10.1111/j.1532-5415.1992.tb02107.x. [DOI] [PubMed] [Google Scholar]