Abstract
OBJECTIVES
To examine the relationship between anxiety and functional decline.
DESIGN
A 5-year longitudinal cohort study of well-functioning adults.
SETTING
The Health, Aging and Body Composition (Health ABC) Study.
PARTICIPANTS
Two thousand nine hundred forty adults aged 70 to 79 (48% male, 41% black), initially free of self-reported mobility difficulty.
MEASUREMENTS
In 1997/98, presence of three anxiety symptoms (feeling fearful, tense or keyed up, or shaky or nervous) from the Hopkins Symptom Checklist were ascertained. Physical function was examined over 5 years using the Health ABC performance battery (continuous range 0–4) consisting of chair stands, usual and narrow course gait speed, and difficulty with standing balance and self-reported mobility, defined as difficulty walking one-quarter of a mile or difficulty climbing 10 steps.
RESULTS
Participants with anxiety symptoms had similar baseline physical performance scores. After adjustment for potential confounders, subjects with anxiety symptoms had similar declines in physical performance over 5 years as participants without anxiety symptoms. Adults with anxiety symptoms were more likely to report incident mobility difficulty, with a hazard ratio of 1.4 (95% confidence interval =1.3–1.6), compared with adults without anxiety symptoms. These results persisted after adjustment for depressive symptoms, demographics, comorbidity, and use of antianxiety, depressant, and sedative hypnotic medications.
CONCLUSION
Anxiety symptoms are not associated with declines in objectively measured physical performance over 5 years but are associated with declines in self-reported functioning. Future studies are needed to determine why anxiety has a differential effect on performance-based and self-reported measures of functioning.
Keywords: aged, anxiety symptoms, depressive symptoms, functional decline
Anxiety symptoms are common, affecting from 8% to 18% of community-dwelling older adults and up to half of those with depression,1–3 and can be quite debilitating.4 Several studies link depressive symptoms to functional decline,5,6 but despite the strong interrelationship between anxiety and depression, few have examined anxiety symptoms’ unique contribution to functional decline.7,8
Functional decline is an important consequence of increasing frailty in older adults, characterized by decreasing physical performance and increased reliance on others for assistance in mobility and other basic activities of daily living. Such decline represents an important precursor of disability, loss of independence, and death.9,10 Performance-based and self-report measures have been used to measure functional status, and both are strongly associated with disability and mortality. These measures complement one another, and both can be used to describe decline.11
Prior longitudinal studies of anxiety symptoms and disability suggest high co-occurrence of depression and anxiety.7 These studies have used a variety of screening instruments to define anxiety symptoms, including the Hospital Anxiety and Depression Scale, the Speilberger State Trait Anxiety Inventory, and the Hopkins Symptom Checklist,8,12,13 but none have examined the effect of anxiety symptoms on incident disability independent of depressive symptoms. To better understand the relationship between anxiety symptoms and functional decline, longitudinal data from participants in the Health, Aging and Body Composition (Health ABC) Study were analyzed. It was hypothesized that older adults with anxiety symptoms would experience greater declines in self-reported mobility difficulty and performance-based functional decline over 5 years.
METHODS
Study Population
Potential participants in the Health ABC Study were identified using Medicare beneficiary lists in Pittsburgh, Pennsylvania, and Memphis, Tennessee.14 Recruitment from the entire black community was needed at both sites to meet recruitment goals. A total of 3,075 adults aged 70 to 79 participated. All participants signed informed consent, and the institutional review boards at the University of California at San Francisco, the University of Tennessee, Memphis, and the University of Pittsburgh approved this study. Participants were well functioning at baseline in 1997/98, because study exclusions were self-reported difficulty with walking one-quarter of a mile, climbing 10 steps without resting, performing basic activities of daily living, and requiring a walking aid. Respondents missing information on anxiety symptoms (n =34) or self-reported physical function (n =4) were excluded from the analysis. For respondents who died over the 5-year follow up (n =417), proxy informants were queried regarding their physical function before death, and of these, 97 reports were not given. Thus, the primary analytic cohort for this study contained 2,940 subjects.
Anxiety Symptom Measurement
During the baseline visit, a standardized questionnaire was administered to collect information on several health conditions and symptoms. Anxiety symptoms were ascertained using three items from the anxiety subscale of the Hopkins Symptom Checklist, a reliable and valid instrument15 that performs similarly to a physician interview for anxiety.16 The three items concerned feeling fearful, nervous or shaky inside, and tense or keyed up. Participants were first asked whether they had experienced the symptom at all in the previous week; those responding, “yes” were asked how frequently the symptom was experienced: a little, quite a bit, or a lot. Anxiety symptoms were considered present when any two symptoms occurred at least a little of the time or any one symptom occurred at least quite a bit. This definition is similar to that used in other population-based studies of older adults.17,18 In addition, two alternate, more-stringent definitions of anxiety symptoms were used. The first, severe symptoms, was defined as having all three symptoms at least a little of the time.8 The second required persistent symptoms, that is, having anxiety symptoms at baseline and at follow-up 5 years later.
Functional Decline
Functional decline was determined using performance-based measures and self-reported difficulty over the 5 years of follow up. Details of the Health ABC performance battery and scoring have been described previously.19 In brief, this battery includes five repeated chair stands, progressively more-challenging tests of standing balance (semitandem, full-tandem, and single leg stands) each held for 30 seconds, a 6-m walk to determine usual gait speed, and a narrow walk in which participants were instructed to walk between lines of colored tape 20 cm apart at their usual pace. Performance on chair stands was evaluated using a rate of chair stands per second. For the standing balance test, the time of each stand was held was summed for a maximum of 90 seconds. Gait speed was noted for both walks. Failure on the narrow walk yielded a score of 0 and consisted of stepping on or outside the tape two or more times over 6 m. Up to three trials were permitted. Performance was divided by the maximum possible performance for older adults on each test to create ratio scores that were summed for the four tests to obtain a continuous scale ranging from 0 to 4, with a lower score indicating poorer function.18
The self-report measures consisted of presence and level of difficulty walking one-quarter of a mile and climbing 10 steps without resting. Incident walking and stair-climbing limitation were defined as report of any difficulty or inability to walk one-quarter of a mile or climbing 10 steps, respectively. Self-reported lower extremity limitation was defined as the first new report of walking or stair climbing difficulty. For participants who died, proxy informants were asked whether the participant had difficulty with either function before death. If the proxy reported difficulty, limitation was considered present.
Covariates
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale,20 which has sensitivity of 97%, specificity of 84%, and positive predictive value of 85%, making it a good screening instrument for depression,21 and were considered present if the participant had a score of 16 or greater.
Other covariates examined were grouped in categories. Sociodemographic variables were age (continuous), race (black or white), sex, study site (Pittsburgh or Memphis), years of education (continuous), family income less than $10,000, and marital status (married or not). Comorbidities were positive history of myocardial infarction, stroke, hypertension, diabetes mellitus, visual impairment, hearing impairment, and poor sleep, defined as frequently not getting enough sleep or feeling sleepy during the day. Lifestyle factors encompassed current smoking, drinking three or more alcoholic drinks per week, and physical activity (continuous), measured as total kcal expended per week for recreational and daily activities.
From a medication inventory of prescription and over-the-counter medications, separate indicator variables were created for use of antianxiety medications such as benzodiazepines and barbiturates; antidepressants such as selective serotonin reuptake inhibitors, tricyclics, and monoamine oxidase inhibitors (yes/no); or any sedative hypnotics, including antihistamines, hypotensive agents, opioids, anticonvulsants, trazodone, benzodiazepines, barbiturates, other anxiolytics, codeine, and melatonin.
Statistical Analyses
Bivariate associations were examined between anxiety symptoms and Health ABC performance score using analysis of variance testing. To evaluate the overall association between anxiety symptoms and performance-based functional decline over 5 years, mixed-effects regression models were calculated, with change in Health ABC performance score as the outcome (range 0–4). This model contained indicator variables for anxiety symptoms. Three correlation structures used in mixed-effects regression models with repeated measures were assessed: unstructured, Huynh-Feldt and compound symmetry. The model with the smallest Akaike information criterion (best fit) was chosen.
To evaluate the association between anxiety symptoms and self-report of limitations (walking, stair climbing, and lower extremity), a series of Cox proportional hazards models were calculated, with the origin as the baseline visit and time calculated to the onset of a functional limitation or censoring at the 5-year study follow-up. Each model contained an indicator variable for anxiety symptoms.
To account for differences in baseline physical performance, the baseline physical performance score was added to all models of self-reported functional outcomes. To test whether depressive symptoms mediated the association between anxiety symptoms and functional decline, an indicator for depressive symptoms was added to the models described above. In addition, other potential covariates were tested if they were associated with anxiety symptoms at a level of 0.10. To assess whether the use of anxiety, depressive, or sedative hypnotic medication altered the association between anxiety symptoms and functional decline, indicators representing the use of these medications were added to the covariates model. Each model was tested for fit and accuracy. Lastly, two sensitivity analyses were conducted in which the more stringent definitions of anxiety symptoms (severe and persistent) were used. All analyses were repeated with the alternate definitions.
RESULTS
The mean age of study participants was 73.6 ± 3, 41% were black, 52% were female, 50% were from Pittsburgh, they averaged 13 years of education, 13% had a household income less than $10,000, and 45% were not married. Demographic characteristics were similar for participants with and without anxiety symptoms, except that those with anxiety symptoms were more likely to be female (P<.001) and unmarried (P =.003) (Table 1). Participants with anxiety symptoms were more likely to have hypertension, vision impairment, hearing impairment, poor sleep, and depressive symptoms and to take antianxiety or antidepressant medication than participants without anxiety symptoms (P<.05 for all).
Table 1.
Baseline Characteristics of the 2,940 Health, Aging and Body Composition Study Participants
| Characteristic | No Anxiety Symptoms (n =2,392, 81%) | Anxiety Symptoms* (n =548, 19%) | P-value† |
|---|---|---|---|
| Age, mean ± SD | 73.6 ± 3 | 73.6 ± 3 | .79 |
| Black, % | 42 | 40 | .44 |
| Female, % | 50 | 63 | <.001 |
| Pittsburgh study site, % | 50 | 49 | .61 |
| Education, years, mean ± SD | 13 ± 3 | 13 ± 3 | .67 |
| Family income <$10,000, % | 14 | 12 | .53 |
| Not married, % | 44 | 51 | .003 |
| Myocardial infarction, %†§ | 11 | 13 | .30 |
| Stroke, %‡ | 2 | 3 | .54 |
| Hypertension, %‡ | 49 | 57 | <.001 |
| Diabetes mellitus, %‡ | 15 | 14 | .34 |
| Vision impairment, %‡ | 3 | 4 | .05 |
| Hearing impairment, %‡ | 8 | 12 | .005 |
| Poor sleep, %‡ | 8 | 18 | <.001 |
| >3 alcoholic drinks/week, % | 18 | 15 | .06 |
| Current smoker, % | 12 | 12 | .71 |
| Depressive symptoms, %§ | 2 | 16 | <.001 |
| Antianxiety or antidepressant medication, % | 10 | 24 | <.001 |
Anxiety symptoms defined using the Hopkins Symptom Checklist (1 symptom quite a bit or 2 symptoms a little).
Calculated using t-tests and chi-squared statistics.
Self-reported medical history.
Center for Epidemiologic Study Depression Scale score ≥16.
SD =standard deviation.
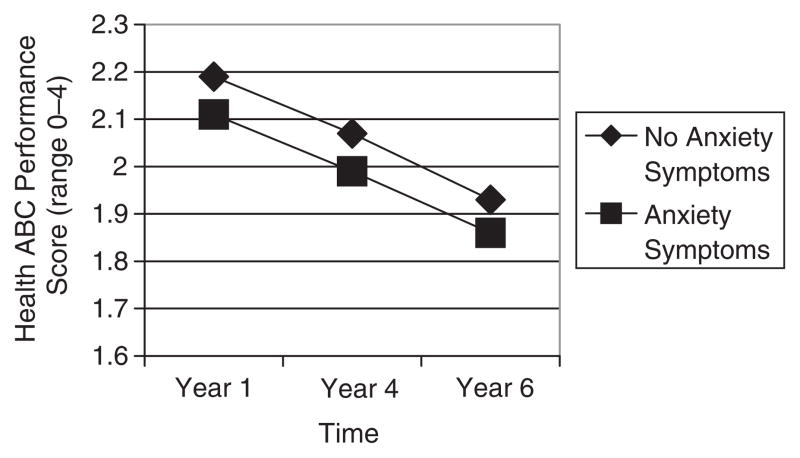
Participants with anxiety symptoms had lower (worse) unadjusted baseline physical performance scores (2.11) than participants without anxiety symptoms (2.19) (P =.002). These participants declined at a similar rate (− 0.32 points over the 5-year study period) as participants without anxiety symptoms (−0.35 points over 5 years), P =.25) (Figure 1). After applying mixed-effects regression modeling, adults with anxiety symptoms had similar baseline physical performance scores (− 0.06, P =.25) and similar least squared mean change in performance over 5 years as those without anxiety symptoms (− 0.02, P =.26). After adjustment for depressive symptoms, neither anxiety nor depressive symptoms were associated with baseline physical performance (anxiety symptoms, P =.55; depressive symptoms, P =.06) or physical performance change over 5 years (anxiety symptoms, P =.42; depressive symptoms, P =.40)
Figure 1.
5-year change in the Health, Aging and Body Composition (Health ABC) Study physical performance score by presence of anxiety symptoms. y-axis: Health ABC performance score (range 0–4).
In contrast, adults with anxiety symptoms alone had a 40% greater hazard of developing self-reported mobility limitations (hazard ratio (HR) =1.4, 95% confidence interval (CI) =1.2–1.6) than those without symptoms, independent of baseline physical performance. Similar relationships were found for self-reported walking and stair climbing limitations (Table 2). Additional adjustment for depressive symptoms and sociodemographics, comorbidities, and lifestyle factors attenuated but did not eliminate the associations. Several covariates slightly reduced the relationship between anxiety symptoms and self-report of mobility difficulty: depressive symptoms (HR =1.5, 95% CI =1.2–1.8), history of hypertension (HR =1.4, 95% CI =1.3–1.5), hearing impairment (HR =1.2, 95% CI =1.0–1.4), poor sleep (HR =1.3, 95% CI =1.2–1.6), and more than three alcoholic drinks per week (HR =0.8, 95% CI =0.7–0.9). Further adjustment for antianxiety, antidepressant, and sedative-hypnotic medication did not alter the results appreciably. There was no statistically significant interaction between anxiety and depressive symptoms for self-reported mobility difficulty, walking, or stair climbing limitation (P =.49 to .70).
Table 2.
Anxiety Symptoms and Time to Self-Report of Walking, Stair Climbing, and Lower Extremity Limitations in Health, Aging and Body Composition Study Participants over 5 Years (N =2,940)
| Incident Limitation % | Base Model† | + Depressive. Symptoms‡ | + Covariates§ | ||
|---|---|---|---|---|---|
| Self-Reported Mobility Limitation* | Anxiety Symptoms | Hazard Ratio (95% Confidence Interval) | |||
| Lower extremity | Yes | 76 | 1.4 (1.2–1.6) | 1.3 (1.2–1.5) | 1.2 (1.1–1.4) |
| No | 62 | 1.0 | |||
| Walking | Yes | 70 | 1.4 (1.3–1.6) | 1.3 (1.2–1.5) | 1.3 (1.1–1.5) |
| No | 56 | 1.0 | |||
| Stair climbing | Yes | 62 | 1.3 (1.2–1.5) | 1.2 (1.1–1.4) | 1.2 (1.0–1.4) |
| No | 48 | 1.0 | |||
Incident limitation defined as the first report of having any difficulty walking one-quarter of a mile (walking), climbing 10 steps (stair climbing), or both (lower extremity limitation).
Base model includes indicator term for presence of anxiety symptoms and baseline performance score.
Base model with additional adjustment for Center for Epidemiologic Study Depression Scale score ≥16 and baseline performance score.
Additional adjustment for sociodemographics (age, sex, race, study site, marital status) and all significant (P<.10) covariates, including comorbidities (hypertension, vision impairment, hearing impairment), management/lifestyle (drinking alcohol ≥3 times per week and feeling sleepy during the day), and baseline performance score.
Two sensitivity analyses were conducted using stricter definitions of anxiety symptoms. There was no association between severe anxiety symptoms, that is, experiencing at least a little of the three anxiety symptoms, and baseline physical performance (P =.41) or change in physical performance over 5 years (P =.32). Severe anxiety symptoms were associated with a 70% greater hazard of self-reported mobility limitation (HR =1.7, 95% CI =1.3–2.1) than for adults without these limitations. Similar associations were observed for incident self-report of walking limitation (HR =1.5, 95% CI =1.2–1.9) and self-report of stair climbing limitation (HR =1.6, 95% CI =1.2–2.0). Persistent anxiety symptoms were associated with a 40% greater hazard of self-reported mobility limitation (HR =1.4, 95% CI =1.2–1.8) than for adults without persistent anxiety. Similar relationships were found for self-reports of incident walking limitation (HR =1.5, 95% CI =1.2–1.9) and self-reports of stair climbing limitation (HR =1.5, 95% CI =1.2–1.9).
DISCUSSION
In this population-based cohort of 2,900 well-functioning older people, anxiety symptoms were not associated with declines in objectively assessed measures of physical performance over 5 years of follow-up. In contrast, anxiety symptoms were associated with greater hazard of self-reported mobility limitation, including difficulty walking and stair climbing. This finding was stronger for persistent and severe anxiety and was independent of depressive symptoms and other potential confounders. It is not clear why the association between anxiety and performance-based functional decline and self-reported mobility limitation differed. One possibility is that there is a mismatch between the limited, isolated tasks measured as part of the performance testing and the complex tasks performed by individuals in nonstructured environments such as their homes. Another possibility is that anxiety biases reports of mobility difficulty, causing subjects to report mobility difficulty out of proportion to their actual functional deficits.
Prior epidemiological studies have suggested that physical performance declines are sensitive measures for early functional decline. In these studies, physical performance served as a more-sensitive marker for change in function than self-reported decline. Thus, there has been a recent trend toward using physical performance as a criterion standard over self-reported measures of function in epidemiological studies. The current study suggests that anxiety symptoms are associated with self-reported measures of function and not performance-based measures. This is counterintuitive, because according to prior literature, decline is generally realized in performance first and self-reported outcomes later.
Self-reported mobility limitation and physical performance decline are important outcomes in older adults. There is a substantial literature on the association between self-reported limitations as a predictor of mortality. For example, a recent predictive index suggested that mobility limitation is associated with twice the hazard of mortality (HR =2.1, 95% CI =1.8–2.4).22 Other studies have suggested that physical performance markers are strong independent predictors of mortality,23 which are considered better than clinical history.24 Because self-reported measures of mobility and objective physical performance are predictors of mortality, it is important to understand each in the context of anxiety symptoms.
Studies of the relationship between anxiety symptoms and functional decline in older adults are limited; only a few have been longitudinal,8,12,13 and only one prior study assessed whether the effect of anxiety was independent of depressive symptoms and simultaneously considered self-reported and performance-based measures of function. Similar to the current study, this study found that anxiety symptoms were associated with self-reported disability after controlling for physical performance,8 although the findings of this prior study are only applicable to older women with existing limitations. The current work provides the most-comprehensive analysis of the effect of anxiety symptoms on functional decline because of the extended follow-up, use of self-reported and performance based measures of function, and adjustment for depressive symptoms.
This study provides evidence that the relationship between anxiety and function differs for subjective (self-report) and objective (physical performance) measures, but the data do not indicate why these relationships differ. The first possible reason is a fundamental difference between the limited, isolated tasks performed in a structured environment compared with the complex tasks performed in a nonstructured environment, which in this study, were assessed using objective performance-based measures and self-reported measures, respectively.
A second potential explanation for the mismatch is that anxiety biases self-reported measures of functioning. This might occur, because anxiety affects confidence and self-efficacy without resulting in any meaningful decrement in ability to perform functional tasks. For example, it is possible that, during performance testing in a standardized, supportive, and safe environment, participants can perform at or near their peak capacity,25 whereas outside this environment, anxious individuals may not be able to perform at their peak capacity and may have more functional difficulties. Future studies of the relationship between anxiety and functional decline will need to include performance measures that closely mimic measures of day-to-day functioning such as a real-world stair climbing task to determine whether anxiety-associated decline is related to differential task performance or reporting bias.
Older adults with anxiety symptoms may report increased mobility limitation, because, in their usual environment, they feel less confident in their mobility. This may be due to a variety of reasons, such as poor lighting, uneven walkways, lack of a companion, and fear of falling. A substantial literature indicates that older adults who are afraid of falling may avoid mobility activities, even if they are able to perform them.26–28 Related to this point is that activity restriction might represent a type of phobic behavior in older adults. Potential correlates could include lack of confidence, fear of falling, and a manifestation of the phobic behavior.
The findings did not show a lower hazard for functional decline for participants taking antianxiety, antidepressant, or sedative-hypnotic medication. This could be due to limited power or confounding by indication, because presumably only participants who had severe anxiety or depression were given these medications. Randomized, placebo-controlled trials of the effects of anxiety and depression treatment on self-report of mobility difficulty are necessary to determine whether treating these symptoms has the effect of increasing functional performance and decreasing reports of limitation. Because older adults taking antidepressants and sedative hypnotics are more likely to fall,29 sedative-hypnotic use in older adults with anxiety symptoms should be further evaluated.
Some potential limitations of this study warrant comment. Depressive and anxiety symptoms were assessed using standardized instruments commonly used in epidemiological studies, but these evaluations did not include detailed clinical history of lifetime anxiety or depressive symptoms, so it was not possible to address whether a clinical diagnosis or cumulative burden of these symptoms over the life-course influenced decline. A definition of severe anxiety symptoms was used that has not been assessed in a clinical setting; therefore, the analyses using the severe definition should be interpreted with caution. In addition, this study used a medical chest inventory to indicate anxiety, depression, and sedative-hypnotic medication use that did not account for when the medication was taken or the indication.
The outcome measures also have some limitations. For example, the self-reported functional decline measures used in this study have not been validated for older adults with anxiety. In addition, it is possible that having the same informant report on anxiety symptoms and incident functional limitations introduces an informant bias, particularly if an anxious subject is more likely to report functional limitation because of another mechanism such as fear of falling. Future studies of anxiety symptoms and functional limitations could address this issue by comparing the self-reports of limitation to reports from a proxy informant and by comparing self-reports of limitation to objective measures that closely model day-to-day activities, such as stair climbing.
In summary, in older adults, anxiety symptoms predict functional decline as assessed using self-reported but not objective performance-based measures. Future studies are needed to examine the reasons underlying anxiety’s differential effect on performance-based and self-reported measures of functioning.
Acknowledgments
Financial Disclosure: Dr. Mehta is currently supported by a Research Career Scientist Award from the National Institute on Aging (NIA, K-01AG025444–01A1) and was supported by a research supplement to the Center for Aging in Diverse Communities at the University of California at San Francisco, a part of the P30 AG 15272 Resource Centers for Minority Aging Research Program (NIA, National Institute of Nursing Research, and the Office for Minority Health and Research. This research was supported (in part) by the Intramural Research program of the National Institutes of Health, NIA. The Health ABC Study is funded by NIA Contracts N01-AG62101, N01-AG62103, and N01-AG62106. The authors would like to thank all individuals who helped with data collection and coordination of the Health ABC Study.
Sponsor’s Role: No sponsor.
Footnotes
Presented at the Gerontological Society of America Meeting, November 21, 2005, Orlando, Florida, and the American Geriatrics Society Meeting, May 5, 2006, Chicago, Illinois.
Author Contributions: Kala M. Mehta conceptualized study and study design; performed analysis and interpretation of data; prepared manuscript. Kristine Yaffe sponsored project acquisition of data, gave critical feedback on study design and manuscript. Gretchen A. Brenes, Anne B. Newman, Ronald I. Shorr, and Eleanor M. Simonsick gave critical feedback on manuscript. Hilsa N. Ayonayon and Susan M. Rubin gave comments on the manuscript. Kenneth E. Covinsky gave overall direction to Dr. Mehta and gave critical feedback on the manuscript.
References
- 1.Beekman AT, de Beurs E, van Balkom AJ, et al. Anxiety and depression in later life: Co-occurrence and communality of risk factors. Am J Psychiatry. 2000;157:89–95. doi: 10.1176/ajp.157.1.89. [DOI] [PubMed] [Google Scholar]
- 2.Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol Med. 2000;30:11–22. doi: 10.1017/s0033291799001452. [DOI] [PubMed] [Google Scholar]
- 3.Mehta KM, Simonsick EM, Penninx BW, et al. Prevalence and correlates of anxiety symptoms in well-functioning older adults: Findings from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2003;51:499–504. doi: 10.1046/j.1532-5415.2003.51158.x. [DOI] [PubMed] [Google Scholar]
- 4.Wilson RS, Bienias JL, Mendes de Leon CF, et al. Negative affect and mortality in older persons. Am J Epidemiol. 2003;158:827–835. doi: 10.1093/aje/kwg224. [DOI] [PubMed] [Google Scholar]
- 5.Lenze EJ, Schulz R, Martire LM, et al. The course of functional decline in older people with persistently elevated depressive symptoms: Longitudinal findings from the cardiovascular health study. J Am Geriatr Soc. 2005;53:569–575. doi: 10.1111/j.1532-5415.2005.53202.x. [DOI] [PubMed] [Google Scholar]
- 6.Stuck AE, Walthert JM, Nikolaus T, et al. Risk factors for functional status decline in community-living elderly people: A systematic literature review. Soc Sci Med. 1999;48:445–469. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 7.Lenze EJ, Rogers JC, Martire LM, et al. The association of late-life depression and anxiety with physical disability: A review of the literature and prospectus for future research. Am J Geriatr Psychiatry. 2001;9:113–135. [PubMed] [Google Scholar]
- 8.Brenes GA, Guralnik JM, Williamson JD, et al. The influence of anxiety on the progression of disability. J Am Geriatr Soc. 2005;53:34–39. doi: 10.1111/j.1532-5415.2005.53007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fortinsky RH, Covinsky KE, Palmer RM, et al. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999;54A:M521–M526. doi: 10.1093/gerona/54.10.m521. [DOI] [PubMed] [Google Scholar]
- 10.Walter LC, Brand RJ, Counsell SR, et al. Development and validation of a prognostic index for 1-year mortality in older adults after hospitalization. JAMA. 2001;285:2987–2994. doi: 10.1001/jama.285.23.2987. [DOI] [PubMed] [Google Scholar]
- 11.Guralnik J, Simonsick E, Ferrucci L. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 12.de Beurs E, Beekman AT, van Balkom AJ, et al. Consequences of anxiety in older persons: Its effect on disability, well-being and use of health services. Psychol Med. 1999;29:583–593. doi: 10.1017/s0033291799008351. [DOI] [PubMed] [Google Scholar]
- 13.Tinetti ME, Inouye SK, Gill TM, et al. Shared risk factors for falls, incontinence, and functional dependence: Unifying the approach to geriatric syndromes. JAMA. 1995;273:1348–1353. [PubMed] [Google Scholar]
- 14.Harris TB, Visser M, Everhart J, et al. Waist circumference and sagittal diameter reflect total body fat better than visceral fat in older men and women. The Health, Aging and Body Composition Study. Ann N Y Acad Sci. 2000;904:462–473. doi: 10.1111/j.1749-6632.2000.tb06501.x. [DOI] [PubMed] [Google Scholar]
- 15.Derogatis LR, Lipman RS, Rickels K, et al. The Hopkins Symptom Checklist (HSCL). A measure of primary symptom dimensions. Mod Probl Pharmaco-psychiatry. 1974;7:79–110. doi: 10.1159/000395070. [DOI] [PubMed] [Google Scholar]
- 16.Glass RM, Allan AT, Uhlenhuth EH, et al. Psychiatric screening in a medical clinic. An evaluation of a self-report inventory. Arch Gen Psychiatry. 1978;35:1189–1195. doi: 10.1001/archpsyc.1978.01770340039003. [DOI] [PubMed] [Google Scholar]
- 17.Kasper JD, Simonsick EM. Mental health and general well-being. In: Guralnik JM, Fried LP, Simonsick EM, et al., editors. The Women’s Health and Aging Study: Health and Social Characteristics of Older Women with Disability [online] Bethesda, MD: National Institute on Aging; 1995. [Accessed October 24, 2006]. Available at www.grc.nia.nih.gov/branches/ledb/whasbook/tablcont.htm. [Google Scholar]
- 18.Simonsick EM, Guralnik JM, Fried LP. Who walks? Factors associated with walking behavior in disabled older women with and without self-reported walking difficulty. J Am Geriatr Soc. 1999;47:672–680. doi: 10.1111/j.1532-5415.1999.tb01588.x. [DOI] [PubMed] [Google Scholar]
- 19.Simonsick E, Newman A, Nevitt M, et al. Measuring higher level physical function in well functioning older adults: Expanding familiar approaches in the Health ABC Study. J Gerontol A Biol Sci Med Sci. 2001;56A:M644–M649. doi: 10.1093/gerona/56.10.m644. [DOI] [PubMed] [Google Scholar]
- 20.Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 21.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult. Criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Arch Intern Med. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- 22.Lee SJ, Lindquist K, Segal MR, et al. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295:801–808. doi: 10.1001/jama.295.7.801. [DOI] [PubMed] [Google Scholar]
- 23.Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295:2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 24.Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults. The Cardiovascular Health Study. JAMA. 1998;279:585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 25.Kivinen P, Sulkava R, Halonen P, et al. Self-reported and performance-based functional status and associated factors among elderly men: The Finnish cohorts of the Seven Countries Study. J Clin Epidemiol. 1998;51:1243–1252. doi: 10.1016/s0895-4356(98)00115-2. [DOI] [PubMed] [Google Scholar]
- 26.Hill KD, Stinson AT. A pilot study of falls, fear of falling, activity levels and fall prevention actions in older people with polio. Aging Clin Exp Res. 2004;16:126–131. doi: 10.1007/BF03324541. [DOI] [PubMed] [Google Scholar]
- 27.Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community-based seniors using home care services. Age Ageing. 2004;33:273–279. doi: 10.1093/ageing/afh077. [DOI] [PubMed] [Google Scholar]
- 28.Delbaere K, Crombez G, Vanderstraeten G, et al. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing. 2004;33:368–373. doi: 10.1093/ageing/afh106. [DOI] [PubMed] [Google Scholar]
- 29.Lawlor DA, Patel R, Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: Cross sectional study. BMJ. 2003;327:712–717. doi: 10.1136/bmj.327.7417.712. [DOI] [PMC free article] [PubMed] [Google Scholar]