Abstract
Background
The performance of a fiber-coupled fluorescence affinity sensor (FAS) was studied in vivo in small and large animal models, in order to assess its feasibility and safety for short-term glucose monitoring in humans.
Methods
Determination of interstitial glucose concentrations in skin tissue of hairless rats and small pigs was facilitated by measuring the fluorescence response of the implanted FAS over several hours and multiple days. Blood sugar changes in animals were induced by injections of insulin and dextrose. The Medtronic Minimed CGMS® (Medtronic Diabetes, Northridge, CA) was used for comparison.
Results
The acute in vivo performance study of the fiber-coupled FAS showed that more than 96% of the paired FAS/venous blood glucose readings were in the clinically acceptable A and B regions of the Clarke Error Grid. Mean absolute relative difference (MARD) and root mean squared error (RMSE) values for small and large animal models were 18.5% and 19.8 mg/dL and 15.9% and 16.3 mg/dL, respectively. In comparison, MARD and RMSE for the Medtronic Minimed CGMS in small and large animal models were similar (in rats, 25.4% and 19.8 mg/dL, respectively; in pigs, 18.4% and 16.2 mg/dL, respectively). No instance of irritation or infection was observed at any implantation site. The in vivo performance of FAS over a 3-day period was successfully demonstrated in both animal models.
Conclusions
Overall, the fiber-coupled FAS was safe, and its performance during 4-h and 3-day testing compared favorably to the commercially available Medtronic Minimed CGMS, indicating its potential value for diabetes management.
Introduction
To ensure a truly continuous sensor readout for the successful development of a complication-free artificial pancreas, improvements in operational functionalities of the current commercially implantable sensors for short-term glucose monitoring in individuals with type 1 diabetes are desirable.1 For example, the Medtronic Minimed CGMS® Gold System™ from Medtronic Diabetes (Northridge, CA) and the STS® sensor from DexCom (San Diego, CA), along with the FreeStyle Navigator® Continuous Glucose Monitor by Therasense/Abbott Diabetes Care (Alameda, CA) are the most advanced sensor systems to date.2–6 All three systems are based on a disposable electroenzymatic sensing platform, relying on the amperometric detection of glucose by glucose oxidase immobilized to an electrode. Both the Medtronic Minimed CGMS and DexCom STS sensors require several calibrations per day for reliable blood glucose detection over a period of 3–7 days. More importantly, both sensors require up to a 2-h warm-up period immediately after implantation or, in the case of the Medtronic Minimed CGMS sensor, whenever the sensor is reconnected to the readout unit (e.g., after bathing). Despite their promising value for diabetes management, it remains to be seen how these electroenzymatic-based devices can be successfully integrated into an artificial pancreas if they require extended warm-up periods and frequent “finger stick” calibrations and/or if their performance is unreliable because of shifts in the sensor sensitivity.
Over the last several years, research into fluorescence affinity sensors (FASs) for glucose detection has steadily gained acceptance among scientists and clinicians through the introduction of a number of improved glucose-sensitive assays based on either the glucose-specific protein concanavalin A (ConA),7–22 artificial glucose-specific receptors based on boronate derivatives,23,24 or an inactive form of the enzyme glucose oxidase.25 There are several intrinsic advantages of an FAS over electrode-enzymatic sensors in terms of practicality for in vivo sensing. For one, the light-based signal detection system does not suffer from the need for warm-up time when the sensor is disconnected from the readout unit, since the light-based signal is immediately available for glucose determination. Second, the absence of an electrode-based system eliminates potential interferences of electrode-active components that may enter interstitial fluid, such as ascorbate, urate, or acetaminophen.26,27 Third, the nature of ligand-binding interactions in receptor-based sensors eliminates the occurrence of “autodestructive” side products, e.g., hydrogen peroxide, as produced by electrode-enzymatic sensors. And, last but not least, the binding reaction in affinity-based sensors is equilibrium-driven, resulting in a signal sensitivity that is independent of the rate of glucose diffusion into the sensor. This is an advantage when compared to glucose-consumptive electroenzymatic sensors, whose signal is rate dependent.
During the last 5 years, our group has made steady progress toward improvements and optimization of a ConA-based FAS for in vivo glucose monitoring.28,29 We have previously reported significant improvements in the chemical stability of the FAS over earlier ConA-based sensors by immobilizing ConA to a macroporous hydrogel, such as Sepharose, which eliminates precipitation of ConA and increases in vitro functionality of the FAS over a time period of up to 6 months at 37°C.28 ConA-Sepharose at 37°C has been maintained over 450 days with only 20% loss of activity.29 Besides our research on studying a transdermal FAS for long-term glucose monitoring in patients with type 1 and 2 diabetes,29 we have been concentrating our interest on developing a fiber-coupled FAS for short-term (3–5-day) interstitial glucose monitoring. The basic design of this prototype sensor is facilitated by interrogating a hollow dialysis fiber containing the fluorescent ConA-based assay with an optical fiber.30 This concept was first described by Schultz and co-workers, who demonstrated measurement of blood sugar in the jugular vein of a dog, as noted in the dissertation thesis of Mansouri.31 However, their sensor chemistry was ill-suited for longer in vivo interrogation because of strong photobleaching of short-wavelength fluorescent dyes (fluorescein) and elaborate and inferior assay chemistry. In contrast, we have employed much brighter and more photo-stable dyes (Alexa 647 and Alexa 750 [Invitrogen, Eugene, OR]) at longer wavelength, enabling us to detect fluorescence with off-the-shelf photodetectors instead of cumbersome and power-consuming photomultipliers.
In this paper we have summarized results of acute and chronic in vivo studies performed on a small and large animal model to evaluate efficacy and safety for potential preliminary human trials over several days.
Materials and Methods
FAS description
The fiber-coupled FAS is a needle-type, fiber optic-based glucose sensor whose detection principle is based on fluorescence resonance energy transfer of the glucose-specific chemistry—housed in a hollow fiber—in response to glucose level changes. The detailed description of design, manufacture, mechanism, and in vitro and in vivo performance of the BioTex (Houston, TX) FAS was reported in two earlier papers.28,30 In brief, one end of a 175-μm-diameter multi-mode polymer optical fiber was mechanically spliced to two 105-μm-diameter silica optical fibers. The proximal ends of the two smaller fibers were terminated with SMA-905 connectors. One of the fibers was attached to a collimated laser diode at 650 nm (Thorlabs, Newton, NJ), and the other was attached to a miniature spectrometer (USB-2000, Ocean Optics, Dunedin, FL). An individual hollow dialysis fiber (diameter 210 μm, length 5 mm) was carefully pushed onto the end of the 175-μm-diameter polymer optical fiber. The hollow fiber was then filled with sensing suspension by aspiration and sealed with cyanoacrylate (Loctite®, Henkel Corp., Düsseldorf, Germany) at both ends. An additional bonding sleeve made of thin-walled polyimide tubing was then attached over the junction between the optical fiber and sensor fiber. The entire fiber sensor assembly fit inside of a 20-gauge hypodermic needle for insertion into skin tissue.
FAS implantation and testing in hairless rats
Male hairless rats without diabetes weighing approximately 300 g were anesthetized and maintained with isoflurane by inhalation. The preclinical animal study included 25 hairless rats. Before implantation the sensors were bathed for 10 min in sterile saline. A 20-gauge hypodermic needle containing the fiber-coupled FAS was inserted intradermally at a shallow angle on the dorsum of the animal 1–4 cm from the midline. After the sensor and needle were pushed approximately 2 cm into the skin, the hypodermic needle was entirely withdrawn, leaving the sensor exposed to skin tissue. A fresh Medtronic Minimed CGMS SOF-Sensor™ (Medtronic Diabetes) was co-implanted in each rat in the subcutaneous tissue of the dorsal thoracic region for comparison purposes according to the manufacturer's instructions. After 1 h of baseline acquisition by the implanted FAS, “regular” fast-acting insulin (0.5 unit/kg) was administered subcutaneously. After another hour, a bolus glucose injection (50% dextrose, 3 mL/kg) was given intraperitoneally. Serial blood samples from the tail vein were taken approximately every 15–20 min over the 2–3-h period and measured using a FreeStyle glucometer (Abbott Diabetes Care). At the end of the experiment, blood glucose was normalized by intraperitoneal bolus injection of 50% dextrose, and the animal was returned to its cage. In a total of 25 animals, the protocol was repeated 2 days later. When a 3-day experiment was performed, the sensor sites were protected with bandages and tape to prevent sensor rupture or removal by the animal. On day 3, an identical glucose manipulation was performed. At the end of the experiment, the FASs were carefully removed from the sites, and the animal was returned to its cage. Overall, chronic experiments over more than 2 days were difficult to perform because of excessive movement of the rats while awake, even when the sensors were protected by bandages and tape around the animal's body.
FAS implantation and glucose testing in pigs
A total of four juvenile farm pigs (weighing 25–30 kg) without diabetes were included in this study. Pigs were pre-anesthetized with ketamine (1 mL/50 kg), scrubbed thoroughly on the dorsal site with povidone and warm water, and then maintained with 1–4% isoflurane by mask. After saline rinse for 10 min, up to three fiber-coupled FASs were inserted in the upper back using a hypodermic needle as described in experiments with the small animal model (see above). We implanted several sensors for redundancy and to maximize our chances that sensors would remain in the animals. Sensors were secured with tape and covered with sterile Tegaderm™ (3M, St. Paul, MN) bandages and masking tape when not in use. At the time of the experiment, a Medtronic Minimed sensor was co-implanted in a similar area in each pig for comparison purposes. To modulate blood glucose, 25 mL of 50% dextrose was infused intravenously through an ear vein. Blood samples were collected from a vein in the contralateral ear. On day 3, all sensors remained implanted, and one was chosen for monitoring. A new CGMS sensor was implanted, and the glucose challenge test was repeated. After the experiments on day 3, sensors were carefully removed, and the pig was returned to its cage.
All animal studies were carried out at an Association for the Assessment and Accreditation of Laboratory Animal Care-accredited facility and in accordance with an Institutional Animal Care and Use Committee-approved protocol.
Signal analysis
Determination of glucose concentrations with FAS was performed retrospectively after simultaneously measuring both the glucose-sensitive emission at 675 nm and the reference dye emission at 780 nm at rate of five to 10 measurements per hour, which were then stored on a notebook computer. After each experiment, the 675 nm and 780 nm signals were analyzed for drift, most likely due to photobleaching, and normalized accordingly. Normalization was performed by determining the slope of the change in emission at 675 nm and 780 nm, respectively, before and after the experiment (usually 2–3 h) at the same glucose concentration. Then the corrected ratio signal was calculated. For calibration purposes, the initial baseline period during which no changes in blood glucose were measured (usually 50–60 min) was used for one-point blood glucose calibration based on paired readings of FAS and venous blood glucose levels. If the one-point glucose calibration reading was not in agreement with the in vitro calibration curve for FAS obtained 12–24 h before the in vivo experiment, the calibration curve was shifted along the y-axis accordingly with the slope remaining constant.
Calibration of the Medtronic Minimed CGMS was internally performed by the CGMS monitor unit (model MMT-7310, version 3.0B). These data were extracted from the unit using Minimed Solutions software and fed into Windows XP Excel™ (Microsoft, Redmond, WA) by a Matlab® application (version 4.2c.1, The Mathworks, Inc., Natick, MA). No further calibration adjustments were performed.
Data and safety analysis
Retrospectively analyzed and corrected data from the Biotex FAS and the Medtronic Minimed CGMS were pooled for each animal model and analyzed. For each animal model, a correlation coefficient (R), a mean absolute relative difference (MARD), and a root mean standard error (RMSE) was calculated by pooling all sensor data. A one-sided Student's t test was performed to test for differences in MARD between the BioTex FAS and Medtronic Minimed CGMS. In addition, for the BioTex FAS a Clarke Error Grid was constructed, and the percentage of points falling into the A, B, C, D, and E regions of the Clarke Error Grid were then calculated. For sensor evaluation, we chose the “classical” error grid analysis in combination with MARD rather than the continuous glucose error grid analysis both developed by Clarke et al.,32,33 because it was less labor intensive and time-consuming and the results were easier to interpret, as was also discussed and recommended in detail by Wentholt et al.34 To evaluate the agreement between glucose concentrations of the FAS sensor reading and venous blood glucose measurement obtained by fingerprick, the differences between the individual data pairs were plotted against their means as described by Bland and Altman.35 The mean difference between both types of glucose measurements and the limits of agreement (including 95% of the differences) were calculated.
We assessed safety in two ways by (1) error grid analysis and (2) visual examination of the skin site during sensor operation and after sensor removal.
Results
In vivo response of fiber-coupled FAS in small animal model
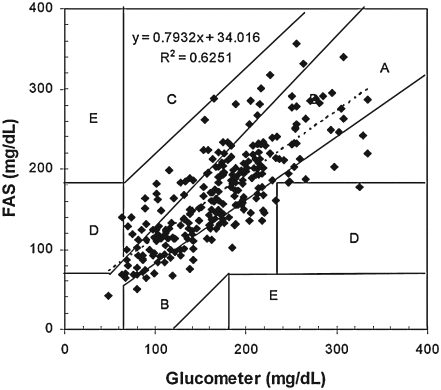
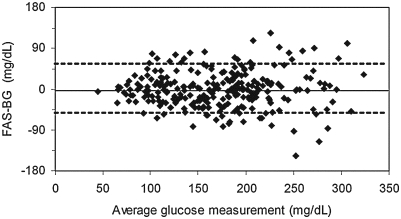
Acute in vivo performance studies with the fiber-coupled FAS were performed in rats. The MARD of the FAS compared to the Abbott FreeStyle glucometer was 18.5% (259 paired samples), and the average correlation coefficient (R) was 0.62. A RMSE of 19.8 mg/dL was calculated. The Clarke Error Grid indicated that of the total of 259 readings, 98.5% of the readings were in the clinically acceptable A and B regions, and 1.5% were in C and D regions, respectively (Fig. 1). Table 1 shows the percentage of points falling within each zone, stratified according to the range of glucose concentrations. Within the glucose range from 40 to 350 mg/dL, 55% of readings were within 20% and 71% within 30%. Table 2 shows that almost at least 50% of paired readings were within 20% of the glucometer readings. Figure 2 shows the differences between capillary blood glucose and FAS values plotted against their averages (Bland-Altman plot).35 The mean of the differences was −1.1 mg/dL, and their standard deviation was 25.8 mg/dL, which would indicate a 95% confidence interval for agreement of 51 mg/dL. The difference appears to be a function of concentration. The data in Figure 2 indicate a −1.1 mg/dL mean difference in FAS and blood glucose readings, giving us confidence that we are not introducing a bias into the FAS response.
FIG. 1.
Glucose values obtained from small animal model experiments in hairless rats plotted in the Clarke Error Grid.
Table 1.
Stratified Clarke Error Grid of FAS Readings in the Small Animal Model
| |
|
Clarke Error Grid zone (%) |
|||||
|---|---|---|---|---|---|---|---|
| Glucose range (mg/dL) | Number of paired readings | A + B | A | B | C | D | E |
| <80 | 10 | 70 | 70 | 0 | 0 | 30 | 0 |
| 81–120 | 50 | 100 | 50 | 50 | 0 | 0 | 0 |
| 121–240 | 166 | 98 | 62 | 36 | 2 | 1 | 0 |
| >241 | 33 | 91 | 58 | 33 | 6 | 3 | 0 |
| Total 40–400 | 259 | 96 | 59 | 37 | 2 | 2 | 0 |
Table 2.
Percentage of FAS Readings Within 20%, 30%, and 40% of Glucometer Readings by Range in the Small Animal Model
| Glucose range (mg/dL) | Number of paired readings | <20% | <30% | <40% |
|---|---|---|---|---|
| <80 | 21 | 48 | 61 | 71 |
| 81–120 | 45 | 58 | 71 | 82 |
| 121–240 | 162 | 61 | 82 | 90 |
| >241 | 31 | 52 | 71 | 87 |
FIG. 2.
Bland-Altman plots for FAS evaluated in the small animal model. The x-axis shows the average of blood and sensor glucose measurements, and the y-axis represents the difference between sensor and concomitant blood glucose (BG) measurements. The solid line is drawn at the mean difference (−1.1 mg/dL); dotted lines are drawn at the mean difference ±1.96 times the SD of the differences (±51 mg/dL).
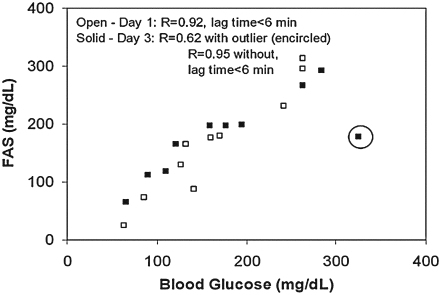
For an animal implanted with the FAS for 3 days, the response on day 1 was comparable to the response on day 3 (Fig. 3). The lower correlation coefficient (R) of 0.62 on day 3 versus 0.92 on day 1 was heavily influenced by the faster rate of change in blood glucose compared to the response by the sensor as illustrated by the data point (encircled) in Figure 3. The sensor was unable to track this artificially high rate of blood glucose change (18 mg/dL/min). However, several studies have shown that rates of blood glucose changes larger than 3 mg/dL/min occur with a probability of less than 1%.36 The corresponding correlation coefficient (R) calculated without the influence of this single point was 0.95 for day 3, indicating excellent stability of sensor response.
FIG. 3.
Comparison of stability of FAS response over a 3-day period in a hairless rat. The sensor was implanted on Day 1 in an anesthetized rat, and its acute response to variation in blood glucose due to injection of insulin and dextrose was measured (open squares). The animal was allowed to freely move around on Day 2. On Day 3, the sensor response was tested again (solid squares). R denotes correlation coefficient between blood glucose values and FAS signal. The encircled data point was the result of a much faster rise of glucose level (18 mg/dL) in blood than in interstitial fluid measured by sensor (see text for further details).
During the entire study, no major acute effects were found as the result of sensor implantation. Minor adverse effects that were observed included bleeding at the insertion site, edema (swelling), and erythema (redness). All were mild and required no treatment.
In vivo performance of FAS in large animal model
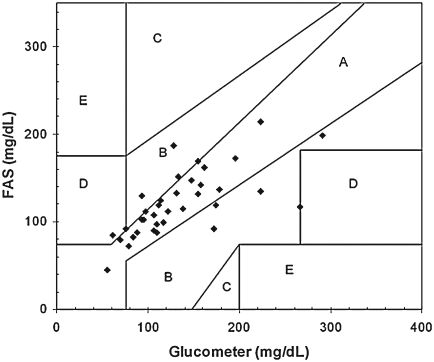
Acute in vivo performance studies with the fiber-coupled FAS were performed in pigs. The retrospective MARD of all sensor data including acute experiments over a 4-h period compared to the Abbott FreeStyle glucometer was 15% (37 paired readings), and the average R value was 0.61. The Clarke Error Grid indicated that from the total of 37 readings, 97% of the readings were in the clinically acceptable A and B regions, and 3% were in the D region (Fig. 4). Table 3 shows the percentage of points falling within each zone, stratified according to the range of glucose concentrations. Within the glucose range from 40 to 350 mg/dL, 56% of readings were within 20% and 83% within 30%.
FIG. 4.
Glucose values obtained from large animal model experiments in pigs plotted in the Clarke Error Grid.
Table 3.
Percentage of FAS Readings Within 20%, 30%, and 40% of Glucometer Readings by Range in the Large Animal Model
| Glucose range (mg/dL) | Number of paired readings | <20% | <30% | <40% |
|---|---|---|---|---|
| <80 | 6 | 67 | 83 | 100 |
| 81–120 | 13 | 92 | 92 | 100 |
| 121–240 | 16 | 68 | 75 | 87 |
| >241 | 1 | 0 | 0 | 100 |
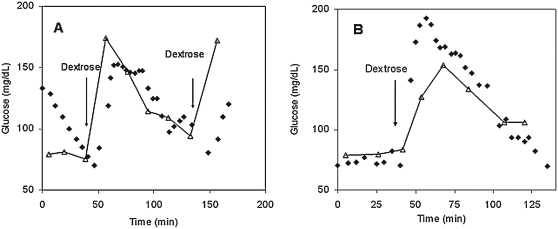
Figure 5 shows the results of one sensor during a 3-day implantation experiment. The correlation coefficient (R) values of 0.89 and 0.88 for Day 1 and Day 3, respectively, demonstrate good stability of the sensor response over a period of 3 days. Sensors were generally well tolerated by the animals. Visual assessment of one implantation site after ex-plantation on Day 3 showed only slight redness at the insertion site, possibly the result of minor bleeding after FAS insertion on day 1, which subsided after a few days. No gross evidence of inflammation, irritation, or infection was noticed based on visual observation at any of the implantation sites.
FIG. 5.
Comparison of stability of FAS response over a 3-day period in a small pig. The sensor was implanted on Day 1 in an anesthetized pig, and (A) its acute response to variation in blood glucose due to injection of insulin and dextrose was measured. The animal was allowed to freely move around on Day 2. (B) On Day 3, the sensor response was tested again. Solid diamonds, FAS response in interstitial fluid; open triangles, glucometer readings in blood.
In vivo performance comparison between FAS and CGMS
A summary of the performance of the BioTex FAS and the Medtronic Minimed CGMS is shown in Table 4. Overall, both sensors performed quite similar in both animal models. We note, however, that the BioTex FAS showed a slightly better performance in hairless rats compared to the CGMS, illustrated by a slightly higher correlation coefficient (0.62 vs. 0.55) and a lower MARD value (18.5% vs. 25.4%, P = 0.005).
Table 4.
Comparison of Acute In Vivo Performance of the BioTex FAS with the Medtronic Minimed CGMS
| Manufacturer and name of glucose sensor, animal model | Number of sensors | Number of paired readings | Correlation coefficient (R) | MARD (%) | RMSE (mg/dL) |
|---|---|---|---|---|---|
| BioTex FAS | |||||
| Hairless rat | 24 | 259 | 0.79 | 18.5 | 19.8 |
| Pig | 4 | 38 | 0.78 | 15.9 | 16.3 |
| Medtronic Minimed CGMS | |||||
| Hairless rat | 16 | 123 | 0.74 | 25.4 | 19.8 |
| Pig | 3 | 18 | 0.80 | 18.4 | 16.2 |
Conclusions
The purpose of this study was to assess feasibility and safety of the fiber-coupled FAS in small and large animal models. While the advantage of hairless rats rested in the ease of handling, the benefits of using pigs for sensor testing are similarities to skin anatomy and general physiology with humans. Although pigs also tended to engage in behaviors that could result in dislodging or damaging the sensors (e.g., rolling, scratching, rubbing), we experienced a reduced failure rate in the large animal model.
In both animal models more than 97% of the paired readings were within the clinically relevant zone A and B regions. Sensor accuracies expressed as RMSE and MARD in both animal models were comparable (16.3 and 19.8 mg/dL and 18.5% and 15.9%, respectively). Moreover, one of the most significant results of the acute in vivo study is the excellent performance of our prototype FAS in comparison to the clinically applied CGMS from Medtronic Minimed. In terms of accuracy with regard to blood glucose level, no major differences were found. Values for the correlation coefficient and MARD were slightly better for the BioTex FAS than for the CGMS. For the Guardian RT system studied in humans over a 72-h period followed by retrospective data analysis, Medtronic Minimed reported a MARD of 17.32%.37 DexCom's STS sensor performed similarly in humans over a 72-h period with a reported MARD of 20.3% based on retrospective analysis.38 Although these MARD values, which are very similar to the BioTex FAS, may not be directly comparable because of differing experimental protocols, the BioTex FAS performance appears very promising and suggests that consideration of initial human trials is appropriate.
During 3-day sensor testing in both animal models, the FAS sensor response was quite acceptable and only hampered by the challenge of keeping the sensor tightly fastened when the highly agile rats were awake. In both cases, the sensor response after 3 days was still measurable. The decrease in response was probably caused by mechanically based fatigue of sensor integrity. We are currently in the process of significantly improving the mechanical robustness of the FAS, which would be imperative when employed in human trials.
Time delay of the FAS in response to blood glucose modulators was modest and did not exceed more than 10 min, even in pigs. We observed very short time lags in rats. We noticed quite often in pigs longer lag times immediately after implantation, which might be due to subacute insertion trauma or other reasons that are still under investigation. Different degrees of vascularization and fat content at the implantation site in the pig might have had an impact on the time response of FAS. These preliminary results confirm that initial trauma due to FAS implantation was minimal and that the short-term biocompatibility of the sensor materials was more than adequate. In two earlier publications, we also addressed safety concerns regarding the use of ConA. We demonstrated supportive experimental and empirical evidence for the absence of systemic toxicity at low ConA doses injected subcutaneously.29,39 Despite the encouraging preclinical safety data obtained from a preliminary host response toxicity study and the sensor performance study reported here, biosafety of the FAS device will continue to be an important concern, and study protocols should be designed to minimize or mitigate potential risks (for example, hyper-sensitization, irritation, anaphylaxis) that may be associated with exposure to sensor materials including ConA.
To provide a superior glucose monitoring tool for patients with diabetes, real-time glucose monitoring of the FAS will be essential. We are optimistic that further improvements of the FAS in terms of its mechanical integrity—which will help to minimize drift—will simultaneously decrease the number of recalibrations (approximately once per day) during sensor operation over several days. If successful, the FAS might become a feasible candidate for potential integration in an artificial pancreas.
In summary, the fiber-coupled FAS was safe, and its performance during 4-h and 3-day testing compared favorably to other continuous glucose monitoring platforms and indicates its potential value for diabetes therapy. The major benefit of the FAS would be the absence of “autode-structive” side products and any device-related warm-up time after sensor reconnection, which would be expected to improve its integration into an “artificial pancreas” system. Overall, these results suggest the suitability of the fiber-coupled FAS for preliminary acute human trials over several hours.
Acknowledgments
This research was supported by grant R43DK067754A from the National Institutes of Health.
Author Disclosure Statement
All authors are employees of BioTex, Inc.
References
- 1.Klonoff DC. Technological advances in the treatment of diabetes mellitus: better bioengineering begets benefits in glucose measurement, the artificial pancreas, and insulin delivery. Pediatr Endocrinol Rev. 2003;2:94–100. [PubMed] [Google Scholar]
- 2.Klonoff DC. A review of continuous glucose monitoring technologies. Diabetes Technol Ther. 2005;7:770–775. doi: 10.1089/dia.2005.7.770. [DOI] [PubMed] [Google Scholar]
- 3.Mastrototaro J. The MiniMed continuous monitoring system. Diabetes Technol Ther. 2000;2(Suppl 1):S13–S18. doi: 10.1089/15209150050214078. [DOI] [PubMed] [Google Scholar]
- 4.Gross TM. Mastrototaro J. Efficacy and reliability of the continuous glucose monitoring system. Diabetes Technol Ther. 2000;2(Suppl 1):S27–S34. doi: 10.1089/15209150050214087. [DOI] [PubMed] [Google Scholar]
- 5.Feldman B. Brazg R. Schwartz S. Weinstein R. A continuous glucose sensor based on wired enzyme technology-results from a 3-day trial in patients with type 1 diabetes. Diabetes Technol Ther. 2003;5:769–779. doi: 10.1089/152091503322526978. [DOI] [PubMed] [Google Scholar]
- 6.Garg S. Zisser H. Schwartz S. Bailey T. Kaplan R. Ellis S. Jovanovic L. Improvement in glycemic excursions with a transcutaneous real-time continuous glucose sensor. Diabetes Care. 2006;29:44–50. doi: 10.2337/diacare.29.01.06.dc05-1686. [DOI] [PubMed] [Google Scholar]
- 7.Schultz JS. Sims G. Affinity sensors for individual metabolites. Biotechnol Bioeng Symp. 1979;9:65–71. [PubMed] [Google Scholar]
- 8.Schultz JS. Mansouri S. Goldstein IJ. Affinity sensor: a new technique for developing implantable sensors for glucose and other metabolites. Diabetes Care. 1982;5:245–253. doi: 10.2337/diacare.5.3.245. [DOI] [PubMed] [Google Scholar]
- 9.Mansouri S. Schultz JS. A miniature glucose sensor based on affinity binding. Biotechnology. 1984;2:885–890. [Google Scholar]
- 10.Meadows DL. Schultz JS. Design, manufacture and characterization of an optical fiber glucose affinity sensor based on a homogenous fluorescence energy transfer assay system. Anal Chim Acta. 1993;280:21–30. [Google Scholar]
- 11.Ballerstadt R. Schultz JS. Competitive-binding assay method based on fluorescence quenching of ligands held in close proximity by a multivalent receptor. Anal Chim Acta. 1997;345:203–212. [Google Scholar]
- 12.Russell RJ. Gefrides CC. McShane MJ. Cote GL. Pishko MV. A fluorescence-based glucose biosensor using tetramethyl-rhodamine concanavalin A and fluorescein isothiocyanate dextran encapsulated in a poly(ethylene glycol) hydrogel. Anal Chem. 1999;71:3126–3132. doi: 10.1021/ac990060r. [DOI] [PubMed] [Google Scholar]
- 13.Tolosa L. Malak H. Gao R. Lakowicz JR. Optical assay for glucose based on luminescence decay time of the long wavelength dye Cy5™. Sensors Actuators B Chemicals. 1997;45:93–99. doi: 10.1016/S0925-4005(97)00275-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ballerstadt R. Schultz JS. A fluorescence affinity hollow fiber sensor for continuous transdermal glucose monitoring. Anal Chem. 2000;72:4185–4192. doi: 10.1021/ac000215r. [DOI] [PubMed] [Google Scholar]
- 15.Ballerstadt R. Ehwald R. Suitability of aqueous dispersions of dextran and concanavalin A for glucose sensing in different variants of the affinity sensor. Biosensors Bioelectronics. 1994;9:557–567. [Google Scholar]
- 16.Ballerstadt R. Polak A. Beuhler A. Frye J. In vitro long-term performance study of near-infrared fluorescence affinity sensor for glucose monitoring. Biosensors Bioelectronics. 2004;19:905–914. doi: 10.1016/j.bios.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 17.Barnes C. D'Silva C. Jones JP. Lewis TJ. A concanavalin A-coated piezoelectric crystal biosensor. Sensors Actuators B. 1991;3:295–304. [Google Scholar]
- 18.Ehwald R. Ballerstadt R. Dautzenberg H. Viscometric affinity assay. Anal Biochem. 1996;234:1–8. doi: 10.1006/abio.1996.0040. [DOI] [PubMed] [Google Scholar]
- 19.March WF. Ochsner K. Horna J. Intraocular lens glucose sensor. Diabetes Technol Ther. 2000;2:27–30. doi: 10.1089/152091500316700. [DOI] [PubMed] [Google Scholar]
- 20.Chinnayelka S. McShane M. Glucose-sensitive nanoassemblies comprising affinity-binding complexes trapped in fuzzy microshells. J Fluorescence. 2004;14:585–602. doi: 10.1023/b:jofl.0000039345.57924.f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pai CM. Bae YH. Mack EJ. Wilson DE. Kim SW. Concanavalin A microspheres for self-regulating insulin delivery system. J Pharm Sci. 1992;81:532–536. doi: 10.1002/jps.2600810612. [DOI] [PubMed] [Google Scholar]
- 22.Zhang J. Roll D. Geddes CD. Lakowicz JR. Aggregation of silver nanoparticle-dextran adducts with concanavalin A and competitive complexation with glucose. J Phys Chem. 2004;108:12210–12214. doi: 10.1021/jp037772c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ben-Moshe M. Alexeev VL. Asher S. A fast responsive crystalline colloidal array photonic crystal glucose sensors. Anal Chem. 2006;78:5149–5157. doi: 10.1021/ac060643i. [DOI] [PubMed] [Google Scholar]
- 24.Fang H. Kaur G. Wang B. Progress in boronic acid-based fluorescent glucose sensors. J Fluorescence. 2004;14:481–489. doi: 10.1023/b:jofl.0000039336.51399.3b. [DOI] [PubMed] [Google Scholar]
- 25.Chinnayelka S. McShane MJ. Microcapsule biosensors using competitive binding resonance energy transfer assays based on apoenzymes. Anal Chem. 2005;77:5501–5511. doi: 10.1021/ac050755u. [DOI] [PubMed] [Google Scholar]
- 26.Moatti-Sirat D. Capron F. Poitout V. Reach G. Bindra DS. Zhang Y. Wilson GS. Thevenot DR. Towards continuous glucose monitoring: in vivo evaluation of a miniaturized glucose sensor implanted for several days in rat subcutaneous tissue. Diabetologia. 1992;35:224–230. doi: 10.1007/BF00400921. [DOI] [PubMed] [Google Scholar]
- 27.Poitout V. Moatti D. Reach G. Bindra DS. Zhang Y. Wilson GS. Sternberg R. Thevenot DR. In vitro and in vivo evaluation in dogs of a miniaturized glucose sensor. J Trans Am Soc Artif Inter Organ. 1991;37:M298–M300. [PubMed] [Google Scholar]
- 28.Ballerstadt R. Gowda A. McNichols R. Fluorescence resonance energy transfer-based near-infrared fluorescence sensor for glucose monitoring. Diabetes Technol Ther. 2004;6:191–200. doi: 10.1089/152091504773731375. [DOI] [PubMed] [Google Scholar]
- 29.Ballerstadt R. Evans C. Gowda A. McNichols R. In vivo performance evaluation of a transdermal near-infrared fluorescence resonance energy transfer affinity sensor for continuous glucose monitoring. Diabetes Technol Ther. 2006;8:296–311. doi: 10.1089/dia.2006.8.296. [DOI] [PubMed] [Google Scholar]
- 30.Ballerstadt R. Evans C. Gowda A. McNichols R. Fiber-coupled fluorescence affinity sensor for 3-day in vivo glucose sensing. J Diabetes Sci Technol. 2007;1:384–393. doi: 10.1177/193229680700100311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mansouri S. Optical glucose sensor based on affinity binding [Ph.D. thesis] Ann Arbor: University of Michigan; 1983. [Google Scholar]
- 32.Clarke WL. Cox D. Gonder-Frederick LA. Carter W. Pohl SL. Evaluating clinical accuracy of systems for self-monitoring of blood glucose. Diabetes Care. 1987;10:622–628. doi: 10.2337/diacare.10.5.622. [DOI] [PubMed] [Google Scholar]
- 33.Clarke WL. Anderson S. Farthy L. Breton M. Gonder-Frederick L. Cox D. Kovatchev B. Evaluating the clinical accuracy of two continuous glucose sensors using continuous glucose sensor error grid analysis. Diabetes Care. 2005;28:2412–2417. doi: 10.2337/diacare.28.10.2412. [DOI] [PubMed] [Google Scholar]
- 34.Wentholt IM. Hoekstra JB. DeVries JH. A critical appraisal of the continuous glucose-error grid analysis. Diabetes Care. 2006;29:1805–1811. doi: 10.2337/dc06-0079. [DOI] [PubMed] [Google Scholar]
- 35.Bland JM. Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 36.Dunn TC. Eastman RC. Tamada JA. Rates of glucose change measured by blood glucose meter and the GlucoWatch Biographer during day, night, and around mealtimes. Diabetes Care. 2004;27:2161–2165. doi: 10.2337/diacare.27.9.2161. [DOI] [PubMed] [Google Scholar]
- 37.Guardian RT. Medtronic Minimed. Premarket Approval, PMA #980022, Supplement #S017. Northridge, CA: Medtronic Minimed; 2006. [Google Scholar]
- 38.DexCom. DexCom STS Continuous Glucose Monitoring System, Pre-Market Approval, PMA# 050012, Supplement #S005. San Diego, CA: DexCom; 2006. [Google Scholar]
- 39.Ballerstadt R. Evans C. Gowda A. McNichols R. Concanavalin A for in vivo glucose sensing: a biotoxicity review. Biosensors Bioelectronics. 2006;22:275–284. doi: 10.1016/j.bios.2006.01.008. [DOI] [PubMed] [Google Scholar]