Abstract
Background
The National Institute of Mental Health Collaborative HIV/Sexually Transmitted Disease Prevention Trial provided a unique opportunity to test whether, with the community-based diffusion of HIV/sexually transmitted disease prevention information and an elevated understanding of HIV, the level of stigmatizing attitudes toward people living with HIV/AIDS in the community would be reduced.
Method
A total of 4510 market workers in Fuzhou, China, participated in the study, and longitudinal analyses included study samples of 3785 participants in the 12-month follow-up and 3716 participants in the 24-month follow-up. We graphically examined the change in HIV-related stigma indicators over time between control and intervention groups using boxplot and kernel density estimation. A logistic regression analysis with proportional odds model was further used to examine the intervention effect on HIV-related stigmatizing attitudes.
Results
Compared with no change over time for the control group, the intervention successfully reduced the level of HIV-related stigmatizing attitudes among the target population at the 12-month follow-up, and the effect increased by two-fold (with respect to odds ratios) at the 24-month follow-up.
Discussion
The intervention demonstrated positive attitude changes associated with HIV-related stigma. Our results show the importance of social norms, rather than simply individual behaviors, in developing and implementing stigma reduction campaigns.
Keywords: China, HIV, stigma
Introduction
HIV-related stigma and discrimination have been identified internationally as major barriers to HIV control and prevention [1–5]. HIV-related stigma creates social distance that cuts off people living with HIV/AIDS (PLWHA) from social interaction and support and strengthens existing inequalities of class, race, and sexuality [6]. Dr Peter Piot [7], Executive Director of the Joint United Nations Programme on HIV/AIDS, described the challenge of stigma as ‘perhaps the greatest of all those facing the AIDS response’ ([7], p. 529).
Previous studies [1,8,9] have demonstrated that a lack of information about HIV/AIDS and misperceptions about HIV transmission routes are important factors contributing to stigma and discrimination. Although HIV knowledge may not be sufficient to reduce the fears and stigmatizing attitudes [10], it may be a necessary first step to reduce HIV-related stigma, as misconceptions about acquiring HIV infection through casual contact may lead to an avoidance of social situations [11,12]. Other studies [13–15] of HIV-related stigma suggested that stigma was associated with increased risk behavior. It could be beneficial to both HIV prevention and HIV stigma reduction programs to investigate their specific strategies and linkage.
It is estimated that there are about 700 000 PLWHA in China [16]. The HIV/AIDS epidemic has evoked widespread stigma and discrimination toward PLWHA in the country [13,17]. A study [18] of Chinese urban market workers found that the majority of the sample believed that PLWHA should be forbidden to take care of other people’s children and should be isolated and punished. Another study [19] revealed that service providers were reported being stigmatized by others because they took care of patients living with HIV/AIDS. In a study [20] in Anhui, China, PLWHA reported being charged more for services or not having access to services at all as a result of HIV status. Similar to other countries, China faces the challenges of both controlling the epidemic and overcoming stigma and discrimination [21–23].
The present study was part of the National Institute of Mental Health (NIMH) Collaborative HIV/Sexually Transmitted Disease (STD) Prevention Trial in international settings, including China, India, Peru, Russia, and Zimbabwe [24]. The trial was designed to identify, recruit, train, and engage community popular opinion leaders (C-POL) in a defined population to convey HIV risk-reduction messages. The primary objective was to reduce HIV/STD incidence and risky sexual behaviors [25]. The principles of the intervention were grounded in the ‘diffusion of innovation theory’ [26]. Although the intervention was designed to target risk behavior for HIV/STD prevention [27] rather than stigma reduction, we hypothesized that, with the community-based diffusion of information related to HIV/STD prevention and an elevated understanding of the epidemic, the level of stigmatizing attitudes toward PLWHA would be reduced.
Methods
Study background and sample
The study was conducted from 2005 to 2007 among food market vendors in Fuzhou, a large city in eastern China. The target population was selected because it had a sufficient base rate of STDs. In addition, the markets were geographically discrete communities in which vendors socialize extensively. The population was stable with the vendors knew one another and presented regularly in the market to be exposed to the ongoing intervention [28]. The market selection procedure was based on the size and geographic location of the markets. Participants were recruited from 40 out of approximately 150 food markets throughout the city. The selected markets were randomized to an intervention arm and a control arm after completing the baseline assessment.
Market workers, 18–49 years old, who worked in a selected market were eligible for the assessment. Study participation was completely voluntary, with a less than 8% refusal rate. After the administration of informed consent, participants completed three surveys using a computer-assisted personal interview (CAPI) at baseline, 12-month, and 24-month follow-ups. All participants were compensated 20 Yuan ($3) for each assessment. The study was approved by the Institutional Review Boards at the University of California, Los Angeles, and the Chinese Center for Disease Control and Prevention.
We conducted the baseline survey among 4510 participants. Three thousand, seven hundred and eighty-five and 3716 of them participated in the survey at the 12-month and 24-month follow-up, respectively (with retention rates of 83.9 and 82.4%, respectively). The retention rate was high because market vendors were a relatively stable population.
Intervention
For markets in the intervention arm, three approaches were systematically used to identify the C-POLs. First, project staff observed individuals who most often and most positively interacted with others in the market. Second, gatekeepers of the markets identified individuals known to be influential to others. Finally, 30 people were randomly selected at each market to nominate C-POLs who were considered to be popular and influential.
Once identified, the C-POLs attended four weekly group training sessions and 10–12 reunion sessions over a 2-year period. In the sessions, participants were first inspired to take on roles as AIDS prevention advocates in the market and then learn skills about how to disseminate HIV risk-reduction messages during everyday conversations. Well trained intervention facilitators came from various backgrounds, including local government health educators, intervention specialists, and project staff. The intervention incorporated interaction, discussion, modeling, role-play, and other interactive techniques to help C-POLs practice and refine their skills to comfortably deliver HIV prevention messages to people in the markets. At the end of each session, C-POLs set goals to engage in HIV education conversations with others in the market. The conversational outcomes of the C-POL were reviewed, discussed, and reinforced during the next training session.
The control markets had no C-POLs identified or trained. However, market vendors in the control arm completed the same study assessments at the same time as the intervention participants.
Measures
Four HIV-related stigma questions were used to measure the participants’ attitudes toward PLWHA: first, ‘A person with HIV must have done something wrong and deserves to be punished;’ second, ‘I think people with HIV should be isolated;’ third, ‘It is safe for someone with HIV to take care of other people’s children;’ and fourth, ‘I do not want to be a friend with someone with AIDS.’ Responses were coded on a 1 (strongly agree) to 5 (strongly disagree) scale. The HIV-related stigma score was constructed by taking sum of all four items (α = 0.7). After the direction for the first, second, and fourth questions being reversed, a higher score indicated a higher level of HIV-related stigma (range of score: 4–20). The stigma score was analyzed as an ordinal response with three levels: low (≤9), median (>9 to ≤15), and high (>15). Our main interest was to estimate the change in the odds of a higher level of HIV-related stigma (two types of odds: high vs. medium or low levels of stigma, high or medium vs. low levels of stigma). Four demographic variables were employed in the study: sex, age, education, and monthly discretionary income.
Data analysis
Differences for demographic and baseline variables were tested using chi-squared (χ2) and t-tests for categorical and continuous variables, respectively. To describe the response pattern of each individual HIV-related stigma question, we presented the frequencies of each question per visit by group.
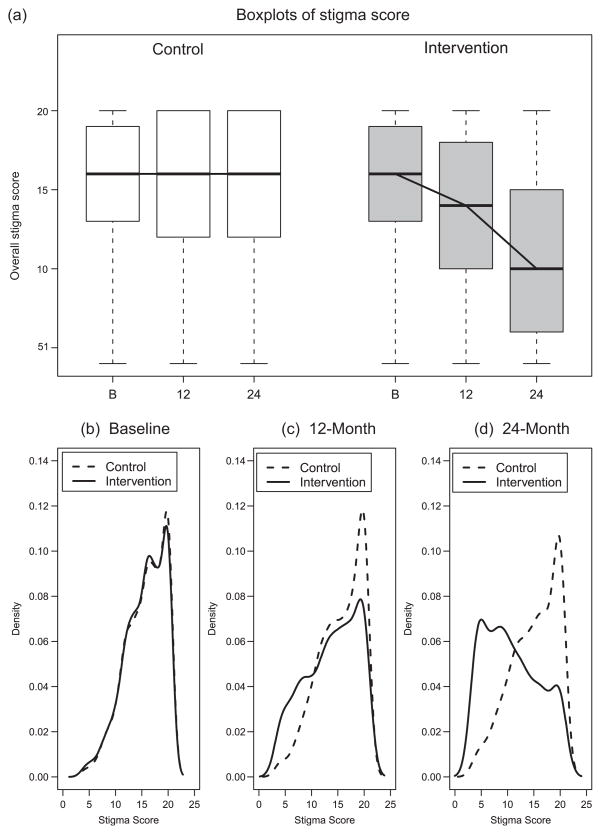
We graphically examined the change in HIV-related stigma score over time between control and intervention groups using two methods: boxplot and kernel density estimation (KDE). A boxplot is a convenient way of graphically depicting groups of numerical data through their five-number summaries (minimum, lower quartile, median, upper quartile, and maximum). KDE is a nonparametric way of estimating the probability density function of a random variable. The purpose of using the KDE method is to show the change in the distributions of the HIV-related stigma score between groups at each follow-up. We calculated KDE curves of the stigma score and plotted them over time by group.
To examine whether there was any association between the HIV-related stigma score and each of the four demographic variables, we performed a logistic regression analysis with the proportional odds model [29] on the categorized stigma score for each factor. Covariates in each model included these four factors: intervention status as a binary variable (0 for control and 1 for intervention), time (baseline, 12-month, and 24-month), two-way interactions (intervention-by-time, intervention-by-factor, factor-by-time), and three-way interactions (intervention-by-time-by-factor). None of the three-way interactions was significant.
Lastly, we used a logistic regression analysis with proportional odds model to examine the intervention effect on the HIV-related stigma score. Covariates included sex, age, education level, spare money, intervention status, time, and an intervention status-by-time interaction. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated.
Results
Demographic characteristics of the sample
Demographic and baseline characteristics are summarized in Table 1. The study sample consisted of 4510 participants, 2262 (50.2%) from the intervention group and 2248 (49.8%) from the control group. Among all participants, about 53% were women and about 39% were 30–40 years old. Approximately, 13% had a high school education or above, and 73.4% of the sample reported having discretionary money of 500 Yuan ($74) per month or less. The control participants were younger than the intervention participants. No significant differences between the two groups were observed in sex, the education level, or the amount of discretionary money per month.
Table 1.
Sample description.
| Demographic characteristics | Total (n = 4510) | Control (n = 2248) | Intervention (n = 2262) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Sex | |||
| Male | 2132 (47.3) | 1055 (46.9) | 1077 (47.6) |
| Female | 2378 (52.7) | 1193 (53.1) | 1185 (52.4) |
| Agea (years) | |||
| ≤30 | 1580 (35.0) | 814 (36.2) | 766 (33.9) |
| >30–40 | 1750 (38.8) | 890 (39.6) | 860 (38.0) |
| >40 | 1180 (26.2) | 544 (24.2) | 636 (28.1) |
| Meana (SD) | 34.1 (8.8) | 33.7 (8.6) | 34.4 (8.9) |
| Education | |||
| No schooling | 379 (8.4) | 194 (8.6) | 185 (8.2) |
| Primary school | 1667 (37.0) | 851 (37.9) | 816 (36.1) |
| Junior high school | 1882 (41.7) | 930 (41.4) | 952 (42.1) |
| High school | 557 (12.4) | 260 (11.6) | 297 (13.1) |
| College or higher | 25 (0.6) | 13 (0.6) | 12 (0.5) |
| Mean (SD) | 6.7 (3.4) | 6.6 (3.5) | 6.8 (3.4) |
| Discretionary money (Yuan)/month | |||
| ≤200 | 1597 (35.4) | 804 (35.8) | 793 (35.1) |
| >200–500 | 1714 (38.0) | 867 (38.6) | 847 (37.4) |
| >500–1000 | 907 (20.1) | 435 (19.4) | 472 (20.9) |
| >1000 | 292 (6.5) | 142 (6.3) | 150 (6.6) |
| Mean (SD) | 486.1 (562.4) | 483.6 (598.4) | 488.5 (524.3) |
Significant age difference was found between control and intervention (P < 0.05). No other significances were observed.
HIV-related stigma
Table 2 presents the frequency distribution of participants’ perceptions on punishment, isolation, childcare safety, and friendship for the control and intervention groups over time. At baseline, about 78% of the participants per group thought that it was not safe for PLWHA to take care of other people’s children. At the 12-month follow-up, 78.1% of the control participants vs. 68.9% of the intervention participants continued to believe so. A more substantial change was observed in the intervention group at the 24th month, in which less than half of the sample (48.9%) was concerned about the safety of PLWHA taking care of other people’s children. Almost no change was seen in the control group.
Table 2.
Frequency distribution of perceived stigma measures.
| Control |
Intervention |
|||||
|---|---|---|---|---|---|---|
| Baseline | 12-month | 24-month | Baseline | 12-month | 24-month | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Punishment | ||||||
| Strongly/somewhat agree | 1076 (48.0) | 800 (43.6) | 707 (38.8) | 1052 (46.5) | 662 (34.4) | 386 (20.5) |
| Not sure | 582 (26.0) | 490 (26.7) | 516 (28.3) | 606 (26.8) | 446 (23.2) | 382 (20.3) |
| Strongly/somewhat disagree | 583 (26.0) | 547 (29.8) | 601 (33.0) | 603 (26.7) | 818 (42.5) | 1116 (59.2) |
| Isolation | ||||||
| Strongly/somewhat agree | 1511 (67.5) | 1157 (62.8) | 1054 (57.7) | 1508 (66.7) | 991 (51.2) | 531 (28.2) |
| Not sure | 349 (15.6) | 274 (14.9) | 322 (17.6) | 350 (15.5) | 258 (13.3) | 206 (10.9) |
| Strongly/somewhat disagree | 379 (16.9) | 411 (22.3) | 450 (24.6) | 402 (17.8) | 685 (35.4) | 1147 (60.9) |
| Child care safety | ||||||
| Strongly/somewhat agree | 1764 (78.7) | 1441 (78.1) | 1400 (76.5) | 1756 (77.7) | 1334 (68.9) | 922 (48.9) |
| Not sure | 301 (13.4) | 234 (12.7) | 221 (12.1) | 314 (13.9) | 232 (12.0) | 183 (9.7) |
| Strongly/somewhat disagree | 177 (7.9) | 170 (9.2) | 210 (11.5) | 191 (8.5) | 370 (19.1) | 779 (41.4) |
| Friendship | ||||||
| Strongly/somewhat agree | 1468 (65.5) | 1232 (66.7) | 1199 (65.5) | 1479 (65.4) | 1079 (55.7) | 732 (38.9) |
| Not sure | 306 (13.7) | 227 (12.3) | 234 (12.8) | 310 (13.7) | 187 (9.6) | 186 (9.9) |
| Strongly/somewhat disagree | 468 (20.9) | 388 (21.0) | 398 (21.7) | 472 (20.9) | 670 (34.6) | 966 (51.3) |
Note: The results from the proportional odds models indicated that the reductions in the agreements of the individual stigma measures (punishment, isolation, child care safety, and friendship) from baseline to 12-month and 24-month follow-ups were significantly higher in the intervention than control (P < 0.0001).
Similar patterns were observed with the other three statements that measure the stigmatizing attitudes. For example, slightly less than half of the sample at baseline supported the idea that PLWHA deserve to be punished. The reduction in percentages was about 4.4% for control (48.0–43.6%) and 12% for intervention (46.5–34.4%) at the 12-month follow-up; a higher reduction in this agreement was reported in the intervention group (34.4–20.5%) than in the control group (43.6–38.8%) between the 12-month and 24-month follow-ups.
Boxplots and kernel density estimation curves of perceptions of stigma over time
At baseline, the means of HIV-related stigma score were 15.7 and 15.6 for the control and intervention groups, respectively. Figure 1(a) represents the boxplots of stigma score at baseline and the two follow-ups by group. Compared with no change over time for control, a clear decreasing trend for intervention was observed. Figure 1(b) shows the KDE curves of the stigma score at baseline, indicating that the control and intervention curves almost completelyoverlap. The intervention curve shifted towards the left in Fig. 1(c), implying that the level of HIV-related stigma decreased at the 12-month follow-up, whereas no change was observed for control. The separation of the intervention and control curves was further clearly observed in Fig. 1(d) at the 24-month follow-up.
Fig. 1. Boxplots and kernel density estimation of stigma scores at baseline and the two follow-ups by group.
Boxplots of stigma scores (a) and kernel density estimation curves of stigma scores for control and intervention groups at (b) baseline, (c) 12-month, and (d) 24-month follow-up visits. Here, clear box in (a) and dashed line in (b)–(d) represent control; shaded box in (a) and solid line in (b)–(d) represent intervention.
Logistic regression analyses with proportional odds models
Results of multivariate logistic regression analyses with the proportional odds model are presented in Table 3. The control participants at 12-month follow-up were more likely to have a higher level of HIV-related stigma than those in the intervention group for both men (OR 1.88; P < 0.0001) and women (OR 1.88; P < 0.0001). The estimated odds of a higher level of HIV-related stigma in the control group at the 24-month follow-up was about five times higher than in the intervention group (OR 5.11 for men and OR 4.76 for women; both P < 0.0001).
Table 3.
Estimated odds ratios (control vs. intervention) with 95% confidence intervals from proportional odds model.
| Parameter (reference = intervention) | Time |
||
|---|---|---|---|
| Baseline | 12-month | 24-month | |
| Sexa | |||
| Male | 1.02 (0.87, 1.19) | 1.88 (1.56, 2.27)* | 5.11 (4.19, 6.22)* |
| Female | 1.03 (0.88, 1.23) | 1.88 (1.58, 2.22)* | 4.76 (4.02, 5.64)* |
| Agea,b (years) | |||
| ≤30 | 1.00 (0.84, 1.19) | 1.90 (1.54, 2.37)* | 4.73 (3.78, 5.92)* |
| >30–40 | 1.10 (0.91, 1.32) | 2.06 (1.68, 2.51)* | 4.83 (3.94, 5.92)* |
| >40 | 1.14 (0.90, 1.46) | 1.90 (1.49, 2.42)* | 5.94 (4.64, 7.61)* |
| Educationa,b | |||
| Primary or lower | 0.98 (0.81, 1.18) | 1.99 (1.63, 2.43)* | 5.47 (4.49, 6.66)* |
| Junior high or above | 1.04 (0.90, 1.20) | 1.83 (1.56, 2.16)* | 4.66 (3.92, 5.54)* |
| Discretionary moneya (Yuan) | |||
| Low (≤500) | 1.00 (0.87, 1.14) | 1.91 (1.65, 2.22)* | 4.95 (4.25, 5.76)* |
| High (>500) | 1.11 (0.90, 1.37) | 1.67 (1.32, 2.11)* | 4.25 (3.35, 5.40)* |
| Final model | |||
| Intervention effectc | 1.02 (0.91, 1.15) | 1.95 (1.72, 2.22)* | 5.36 (4.69, 6.13)* |
Three-way interaction was not significant.
Significant time-by-age and time-by-education interactions (P = 0.0381 and P = 0.0003, respectively).
Controlling for sex, age, education, and spare money. A significant intervention status-by-time was found (P < 0.0001). All the covariates were significantly associated with the HIV-related stigma (P < 0.0001 for sex, age, and education; P = 0.0139 for discretionary money).
P < 0.0001.
Control participants in each of the three age categories (≤30, >30–40, and >40 years) were about two times more likely to report a higher level of HIV-related stigma than those in the intervention group at the 12-month follow-up (all P < 0.0001) (Table 3). The participants who were older than 40 years had the highest OR at the 24-month follow-up (OR 5.94; P < 0.0001) and were almost six times more likely to report a higher level of HIV-related stigma than those in the intervention group. At the 12-month follow-up, the control participants who were less educated (primary or lower) were two times more likely to be associated with a higher level of HIV-related stigma than those in the intervention group (OR 1.99; P < 0.0001); the estimated OR increased from 2 to 5.5 at the 24-month follow-up (OR 5.47; P < 0.0001). Similar results were observed for participants with higher education. A significant time-by-education interaction was found, meaning that the time trends were different between less and more educated groups (P = 0.0003). The participants who were less educated benefited more from the intervention than those who were more educated with respect to the reduction of HIV-related stigma.
Final model
After adjusting for age, sex, education level, and discretionary money, the results from multivariate logistic regression analysis with the proportional odds model showed that, at baseline, there was no statistically significant difference in participants’ perceptions of stigma between the two groups. The estimated odds of a higher level of HIV-related stigma was almost twice as much for control vs. intervention at the 12-month follow-up (OR 1.95; P < 0.0001) and more than five times at the 24-month follow-up (OR 5.36; P < 0.0001). An intervention-by-time interaction was found statistically significant, meaning that the time trends were significantly different between control and intervention (P < 0.0001).
Discussion
The Chinese government has put enormous effort into HIV prevention campaigns for the general population. Although numerous other factors, including national and local HIV awareness and prevention campaigns, may have affected the societal stigma towards PLWHA during the 2-year study period, our results still showed that, compared with no change over time for the control group, the intervention successfully reduced the level of HIV-related stigma among the intervention arm participants at the 12-month and 24-month follow-ups.
Since the beginning of the HIV/AIDS epidemic over 25 years ago, stigma has been a barrier to HIV testing, diagnosis, treatment, and care. As policy makers, advocates, and researchers search for and scale up intervention programs to reduce and eliminate HIV-related stigma and discrimination, the findings of this study have some interesting implications.
The C-POL intervention trial was designed with the primary goal of reducing HIV/STD incidence and risky sexual behavior. On the basis of the preliminary report, no statistically significant differences in either behavioral or biological outcomes were found between the intervention and control venues [30]. The ‘unintended’ outcomes of stigma reduction in China – reported in this study – are both encouraging and puzzling. Unlike natural science, in which some of the most important discoveries are made unexpectedly, behavioral research tends to focus on expected outcomes as articulated in program or intervention design [31]. The findings of this study provide an opportunity to look beyond findings specified by the design and learn lessons from the variance between expected and unexpected outcomes.
First, the C-POL intervention was a community-based intervention delivered through identified social networks within the target population. The intervention was implemented by fully engaging the community and social network, which is imperative for any stigma reduction interventions. In China, as in many other countries, the strong bonds between family and community demand that stigma and discrimination should be viewed as social and cultural phenomena that require the actions of groups of people, not simply individuals. The outcome of stigma alleviation observed in this study implies that interventions that mobilize the whole community and penetrate its social network could be used as strategies for a resource for tackling HIV-related stigma and discrimination.
Second, the significant outcomes on stigma could also be associated with the simple fact that, with the implementation of the C-POL intervention, HIV knowledge has been diffused in a nonstigmatized fashion in the community. As the knowledge–attitude–behavior (KAB) continuum in other areas of health and behavior, the change of knowledge is often present before changes in attitude or behavior. In this trial, intervention facilitators not only delivered HIV transmission knowledge but also provided skill training for C-POLs to communicate with others in the community about HIV prevention and safer behaviors. As part of the intervention, trained C-POLs were encouraged to talk to their coworkers about these topics during day-to-day, casual conversations. These communications of behavior change were based on the assumption that HIV can be discussed in a nonstigmatized setting as a part of everyday life. These activities could provide the opportunity to talk about basic factors of the disease that were relatively new to the population. It is possible that the increased familiarity with HIV and comfort level of talking about the disease lead to a climate, in which acceptance attitudes also increase and are shared among community members.
Third, it would seem worthwhile to note the implications relevant to the POL intervention model in particular. Bertrand [32] described observability – how visible the intervention results are to others in the community – as one of the attributes that can affect the intervention outcomes. This certainly challenges HIV-preventive interventions in which the main intervention outcome, the safer sexual behavior, is not readily observable. It is true that communications related to stigmatizing perceptions do not necessarily result in an observable improvement in behaviors. However, the conversations and expressions could be highly desired in the community, given the overall social climate in China. In the past decade, the Chinese government has increasingly employed mass media for HIV prevention campaigns, as exemplified by Premier Wen Jiabao comforting PLHWA patients at a hospital [33] and by Yao Ming and Magic Johnson appearing as AIDS spokesman on television to fight for HIV discrimination [34,35]. Under these circumstances, to communicate or express a nonstigmatizing view about HIV could bring C-POLs immediate rewards (e.g., to be seen as educated, empathetic, and modern). It is reasonable to speculate that rewarding experiences could further encourage C-POLs’ diffusion of intervention messages. This once again reminds us of the importance of social norms rather than merely individual behaviors in the C-POL intervention and the interpretations of its results.
Finally, the findings of this study have implications for reexamining the connection between HIV prevention and stigma reduction programs. HIV prevention and stigma reduction programs often take place in a parallel fashion because of funding mechanisms, issues addressed, or investigators’ expertise. Although HIV prevention interventions have been conducted around the world, stigma associated with HIV, homosexuality, commercial sex, and drug use makes it difficult for HIV prevention programs to be implemented effectively in a variety of settings. Thus, HIV-related stigma and discrimination not only lead to stress for PLHWA but also add to the challenges for HIV prevention.
HIV prevention and stigma reduction interventions, although built upon different conceptual frameworks, can be integrated. Program developers, policy makers, and researchers must incorporate effective strategies from both frameworks into their programs and learn from predictable changes as well as unintended consequences. This study has limitations, as the perceived societal stigma and discrimination of PLWHA were not measured. Reports on changes in stigma and discrimination from their point of view would be a good supplement to this study.
Acknowledgments
This study was funded by NIMH grant number U10MH61513, a five-country Cooperative Agreement being conducted in China, India, Peru, Russia, and Zimbabwe. Each site has selected a different venue and population with which to implement the prevention program entitled Community Public Opinion Leader (C-POL) Intervention.
L.L. conceptualized the analysis plan and wrote the article. L.-J.L. analyzed the data and drafted the results. C.L. assisted in writing the article. Z.W. and M.J.R.-B. originated the C-POL project – China site – and oversaw data collection. All authors contributed to the interpretation of results and revision of the article.
References
- 1.Herek GM, Capitanio JP. AIDS stigma and sexual prejudice. Am Behav Sci. 1999;42:1126–1143. [Google Scholar]
- 2.Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counseling and testing in a black township in Cape Town, South Africa. Sex Transm Infect. 2003;79:442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22 (Suppl 2):S67–S79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malcolm A, Aggleton P, Bronfman M, Galvao J, Mane P, Verrall J. HIV-related stigmatization and discrimination: its forms and contexts. Crit Public Health. 1998;8:347–370. [Google Scholar]
- 5.UNAIDS. [Accessed 2 February 2009];Fact sheet on stigma and discrimination. 2003 December; http://data.unaids.org/Publications/Fact-sheets03/fs_stigma_discrimination_en.pdf?preview_true.
- 6.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57:13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 7.Piot P. AIDS: from crisis management to sustained strategic response. Lancet. 2006;368:526–530. doi: 10.1016/S0140-6736(06)69161-7. [DOI] [PubMed] [Google Scholar]
- 8.Manijsin T, Sangyos D, Pirom P. Families and communities living with AIDS, Ban Haed District, Khon Kaen Province, Thailand. Khon Kaen: Sirinthorn Hospital; 2003. [Google Scholar]
- 9.Sweat MD, Levin M. HIV/AIDS knowledge among the U.S. population. AIDS Educ Prev. 1995;7:355–372. [PubMed] [Google Scholar]
- 10.Nyblade L, Pandey R, Mathur S, MacQuarrie K, Kidd R, Banteyerga H, et al. Disentangling HIV and AIDS stigma in Ethiopia, Tanzania, and Zambia. Washington, DC: International Center for Research on Women; 2003. [Google Scholar]
- 11.Apinundecha C, Laohasiriwong W, Cameron MP, Lim S. A community participation intervention to reduce HIV/AIDS stigma, Nakhon Ratchasima province, northeast Thailand. AIDS Care. 2007;19:1157–1165. doi: 10.1080/09540120701335204. [DOI] [PubMed] [Google Scholar]
- 12.Liu HJ, Hu Z, Li XM, Stanton B, Naar-king S, Yang HM. Understanding interrelationships among HIV-related stigma, concern about HIV infection, and intent to disclose HIV serostatus: a pretest–posttest study in a rural area of eastern China. AIDS Patient Care STDs. 2006;2:133–142. doi: 10.1089/apc.2006.20.133. [DOI] [PubMed] [Google Scholar]
- 13.Chen J, Choe MK, Chen S, Zhang S. Community environment and HIV/AIDS related stigma in China. AIDS Educ Prev. 2005;17:1–11. doi: 10.1521/aeap.17.1.1.58689. [DOI] [PubMed] [Google Scholar]
- 14.Peretti-Watel P, Spire B, Obadia Y, Moatti JP The VESPA Group. Discrimination against HIV-infected people and the spread of HIV: some evidence from France. PLoS One. 2007;2:e411. doi: 10.1371/journal.pone.0000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simbayi LC, Kalichman SC, Strebel A, Cloete A, Henda N, Mgeketo A. Disclosure of HIV status to sex partners and sexual risk behaviours among HIV-positive men and women, Cape Town, South Africa. Sex Transm Infect. 2007;83:29–34. doi: 10.1136/sti.2006.019893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.State Council AIDS Working Committee Office, UN Theme Group on AIDS in China. A joint assessment of HIV/AIDS prevention, treatment and care in China. Beijing: Ministry of Health; 2007. [Google Scholar]
- 17.Hesketh T, Duo L, Li H, Tomkins AM. Attitudes to HIV and HIV testing in high prevalence areas of China: informing the introduction of voluntary counseling and testing programmes. Sex Transm Infect. 2005;81:108–112. doi: 10.1136/sti.2004.009704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee M, Wu Z, Rotheram-Borus MJ, Detels R, Guan J, Li L. HIV-related stigma among market workers in China. Health Psychol. 2005;24:435–438. doi: 10.1037/0278-6133.24.4.435. [DOI] [PubMed] [Google Scholar]
- 19.Li L, Lin C, Wu Z, Wu S, Rotheram-Borus MJ, Detels R, et al. Stigmatization and shame: consequences of caring for HIV/AIDS patients in China. AIDS Care. 2007;19:258–263. doi: 10.1080/09540120600828473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cao X, Sullivan GS, Xu J, Wu Z the China CIPRA Project 2 Team. Understanding HIV-related stigma and discrimination in a ‘blameless’ population. AIDS Educ Prev. 2006;18:518–528. doi: 10.1521/aeap.2006.18.6.518. [DOI] [PubMed] [Google Scholar]
- 21.Gill B, Okie S. China and HIV: a window of opportunity. N Engl J Med. 2007;356:1801–1805. doi: 10.1056/NEJMp078010. [DOI] [PubMed] [Google Scholar]
- 22.Wu ZY, Sullivan SG, Yang Y, Rotheram MJ, Detels R. Evolution of China’s response to HIV/AIDS. Lancet. 2007;369:679–690. doi: 10.1016/S0140-6736(07)60315-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang H, Li X, Stanton B, Fang X, Lin D, Mao R, et al. Willingness to participate in HIV/STD prevention activities among Chinese rural-to-urban migrants. AIDS Educ Prev. 2004;16:557–570. doi: 10.1521/aeap.16.6.557.53792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Griensven F, Kalichman SC. Design and concept of the NIMH Collaborative HIV/STD Prevention Trial. AIDS. 2007;21 (Suppl 2):S1–S2. doi: 10.1097/01.aids.0000266452.36570.a3. [DOI] [PubMed] [Google Scholar]
- 25.NIMH Collaborative HIV/STD Prevention Trial Group. The community popular opinion leader HIV prevention programme: conceptual basis and intervention procedures. AIDS. 2007;21 (Suppl 2):S59–S68. doi: 10.1097/01.aids.0000266458.49138.fa. [DOI] [PubMed] [Google Scholar]
- 26.Rogers EM. Diffusion of innovations. New York, NY: Free Press; 1995. [Google Scholar]
- 27.Kelly JA, St Lawrence JS, Stevenson LY, Hauth AC, Kalichman SC, Diaz YE, et al. Randomized, controlled, community-level HIV prevention intervention for sexual risk behavior among homosexual men in U.S. cities. Lancet. 1997;350:1500–1505. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- 28.NIMH Collaborative HIV/STD Prevention Trial Group. Methodological overview of a five-country community-level HIV/Sexual transmitted disease prevention trial. AIDS. 2007;21 (Suppl 2):S3–S18. doi: 10.1097/01.aids.0000266453.18644.27. [DOI] [PubMed] [Google Scholar]
- 29.Hosmer DW, Lemeshow SL. Applied logistic regression. 2. New York: Wiley; 2000. [Google Scholar]
- 30.Pequengat W the NIMH Collaborative HIV/STD Prevention Trial Group. Results of the RTC to test the Community Popular Opinion Leader (C-POL) intervention in five countries [poster]. International AIDS Conference; 3–8 August 2008; Mexico City, Mexico. [Google Scholar]
- 31.Nitipaisalkul W. Valuing unexpected outcomes: a case study of an Indonesian training project. Canberra: Hassall & Associates International; 2007. [Google Scholar]
- 32.Bertrand JT. Diffusion of innovations and HIV/AIDS. J Health Commun. 2004;9:113–121. doi: 10.1080/10810730490271575. [DOI] [PubMed] [Google Scholar]
- 33.Washington Poster Foreign Service. Chinese leaders break AIDS taboo: premier’s appearance with patients signals end to silence about epidemic. [Accessed 10 November 2008];2003 December 2; http://www.media.tsinghua.edu.cn/data/2006/0225/article_44.html.
- 34.Wang LD. Fighting stigma and discrimination of HIV/AIDS in China: media art and social policy. [Accessed 10 November 2008];2005 http://www.asiasociety.org/speeches/longde.html.
- 35.Xinhua News Agency. Yao Ming, Magic Johnson TV ad launched to fight discrimination against HIV/AIDS patients. [Accessed 30 March 2008];2006 http://english.peopledaily.com.cn/200603/05/eng20060305_247944.html.