Abstract
Objective:
To investigate the possible association between untreated Attention Deficit Hyperactivity Disorder (ADHD) symptoms, as measured the Adult ADHD Self-Report Scale, and persistent nonmedical use of prescription stimulants.
Method:
Multinomial regression modeling was used to compare ADHD symptoms among three groups of college students enrolled in a longitudinal study over four years: 1) persistent nonmedical users of prescription stimulants; 2) persistent users of marijuana who did not use prescription stimulants nonmedically; and, 3) consistent non-users of drugs.
Results:
ADHD symptoms were associated with being a persistent nonmedical user of prescription stimulants, after adjustment for race/ethnicity, sex, SES, and other illicit drug use. No associations were observed between ADHD symptoms and being a persistent marijuana user or non-user.
Conclusions:
ADHD symptoms, and in particular inattention symptoms, appear to be associated with nonmedical use of prescription stimulants. Future studies are needed to clinically validate these observations.
Introduction
Nonmedical use of prescription stimulants (NPS), meaning use without a legitimate prescription, appears to be increasing among college students, with lifetime prevalence estimates ranging from 6.9% to 18.6% (Arria et al., 2008b; Carroll, McLaughlin, & Blake, 2006; Hall, Irwin, Bowman, Frankenberger, & Jewett, 2005; McCabe, Knight, Teter, & Wechsler, 2005; McCabe, Teter, & Boyd, 2006; Prudhomme-White, Becker-Blease, & Grace-Bishop, 2006; Teter, McCabe, LaGrange, Cranford, & Boyd, 2006). Athletes and fraternity members appear to be at particularly high risk for use (Bents & Marsh, 2006; DeSantis, Noar, & Webb, 2009). NPS has also been associated with being male (McCabe et al., 2005; McCabe et al., 2006), being White (McCabe et al., 2005; McCabe et al., 2006; Teter et al., 2006), having a lower GPA (McCabe et al., 2005) and having a history of illicit drug involvement (Arria et al., 2008b; McCabe et al., 2005; McCabe et al., 2006; Rabiner et al., 2009b; Teter, McCabe, Boyd, & Guthrie, 2003). Past-year prevalence estimates of NPS among college students range from 4.1% to 5.9% (McCabe et al., 2005; McCabe et al., 2006; Teter et al., 2006), with one study reporting that approximately one-third used a prescription stimulant nonmedically in the past year (Low & Gendaszek, 2002).
Many studies attempting to explain NPS focus on major motives of use, the most prevalent being to increase concentration when studying (Carroll et al., 2006; DeSantis et al., 2009; DuPont, Coleman, Bucher, & Wilford, 2008; Prudhomme-White et al., 2006; Rabiner et al., 2009b). Compared to non-users, students who use prescription stimulants in this way are more likely to have a history of other drug involvement and are more likely to skip class (Arria, O'Grady, Caldeira, Vincent, & Wish, 2008c; Arria et al., 2009). Consequently, for some students, NPS might be a compensatory behavior for those who are struggling academically because of chronic drug use or missed classes. Another possible scenario (not mutually exclusive from the first) may be that students with untreated Attention Deficit Hyperactivity Disorder (ADHD) symptoms are using stimulants nonmedically (Wilens et al., 2008) to “self-treat” their symptoms. Recent evidence supports that a modest proportion of college students (10.3%) who have never been treated for ADHD report levels of ADHD symptoms that might prompt a clinical assessment (Garnier-Dykstra et al., in press). When Rabiner et al. (2009b) compared nonmedical users of prescription stimulants to non-users on ADHD symptoms of inattention and hyperactivity, they found that users reported higher levels of inattention and hyperactivity-impulsivity symptoms than non-users; however, the study did not control for other substance use and mental health problems, and did not measure ADHD symptoms with a standardized instrument. A different study by this same group observed that attention difficulties predicted the initiation of NPS, but not the initiation of nonmedical use of other prescription drugs (Rabiner et al., 2009a).
The present study was designed to extend our current understanding of the extent to which untreated ADHD symptoms might play a role in NPS. We were able to examine this question by using data from a large longitudinal study of college students. Given prior evidence of an association between ADHD symptoms and incident NPS, we hypothesized that higher levels of ADHD symptoms would be associated with persistent NPS. We surmised that inattention problems (compared to hyperactivity-impulsivity symptoms) might be more likely to be associated with NPS because of the relationship between inattention and academic performance difficulties. We tested this hypothesis by using three different operational definitions of ADHD (the total Adult ADHD Self-Report Scale (ASRS) score, inattention and hyperactivity-impulsivity subscale scores, and meeting the “Clinical” threshold on the ASRS) and comparing these measures among three groups of young adults: 1) persistent nonmedical users of prescription stimulants; 2) persistent marijuana users who did not use prescription stimulants nonmedically; and 3) non-users of both illicit and prescription drugs (used nonmedically). Because almost all nonmedical users of prescription stimulants used marijuana (99.1% of our sample had tried marijuana at least once), we thought it was important to include persistent marijuana users as a comparison group. Such a strategy would help us to understand the degree to which elevated ADHD symptoms were specifically related to NPS, and not simply related to having a general propensity for drug involvement.
Methods
Study Design
Data were derived from the College Life Study, a large ongoing longitudinal prospective study of college student health behaviors. The sample was ascertained in two stages. First, a screening survey was administered to 3,401 first-time first-year students at a large, public, mid-Atlantic university during Summer Orientation in 2004 (response rate=88.7%). Second, a longitudinal cohort sample, with purposive oversampling of students who had used an illicit drug or nonmedically used a prescription drug at least once prior to college entry, was recruited for follow-up. Sampling weights were computed to adjust for oversampling, and prevalence estimates presented in this paper are statistically weighted to reflect the general population of first-year students at the university where our sample was recruited. The response rate was 86.5% at baseline, yielding a sample of 1,253 students who were administered a face-to-face interview and completed self-administered questionnaires during their first year of college. Interviewers were mainly graduate and advanced undergraduate students who were extensively trained. All interviews were reviewed for quality and missing data by a senior staff member and both scheduled and random interview observations occurred. Instruments used in the interview and self-administered questionnaires were standardized whenever possible. More information about the interview and interviewer training is available elsewhere (Arria et al., 2008a). Participants completed similar assessments annually thereafter, regardless of continued college attendance, and were given $50 for each annual assessment, with a $20 bonus for timely response (within four weeks of the anniversary of their baseline interview). Data for the present study was taken from the fourth annual interview (follow-up rate 87.6%; n=1,097). Of those participants, 91.2% were still enrolled in college at Year 4 (n=1,000). This study was approved by the university's Institutional Review Board, and informed consent and a federal Certificate of Confidentiality were obtained. Additional information about sampling and data collection are available elsewhere (Arria et al., 2008a).
Sample
From the Year 4 participants, we excluded 108 individuals who had been previously diagnosed with ADHD by a medical professional (because we wished to focus our study on untreated ADHD symptoms), 17 individuals who were missing data on the ADHD measure (administered in Year 4), and 57 individuals who were missing data on NPS from one or more annual assessments. From the remaining 915 participants, 470 individuals were finally selected for analyses because they met criteria for inclusion in one of the following three comparison groups:
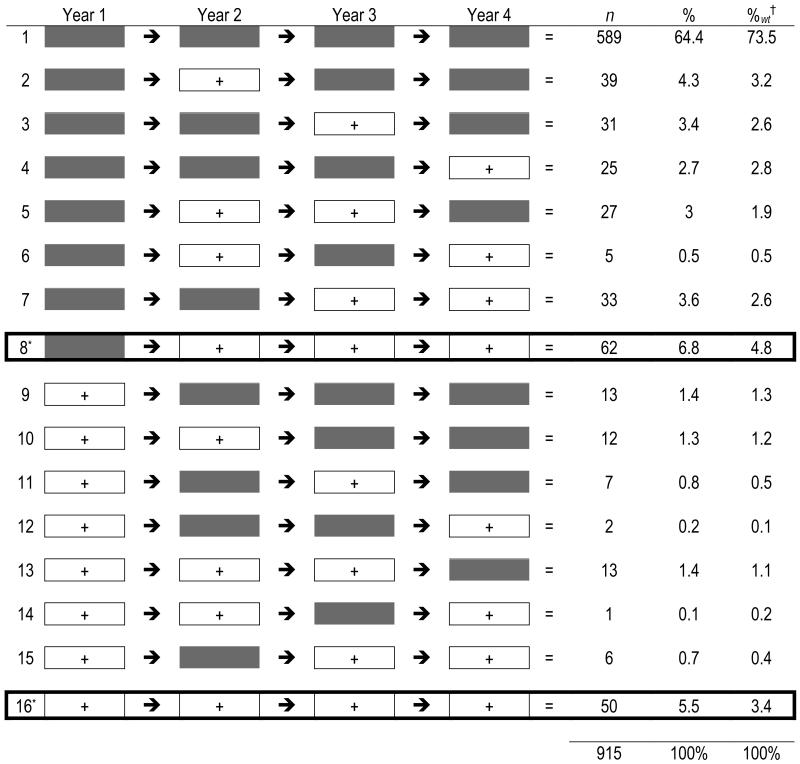
1) Persistent nonmedical users of prescription stimulants (n=112).1 Annually, participants were asked on how many days in the past 12 months they had nonmedically used Adderall,® Ritalin,® Concerta,® or any other prescription stimulant. Persistent NPS was defined as nonmedical use of a prescription stimulant at least once in the past year during all three consecutive follow-up years of the study (i.e., Years 2, 3, and 4), regardless of their use at baseline. Figure 1 displays the sample composition (n=915) with respect to longitudinal patterns of NPS. The two boxed rows represent the individuals we defined as persistent users. Among persistent users, the average number of times a prescription stimulant was used nonmedically in the past year was 14.03 times in Year 2 (range: 1 to 83); 16.45 times in Year 3 (range: 1 to 150) and 14.86 times in Year 4 (range: 1 to 180). For ease of presentation, this group is hereinafter referred to as the “Stimulant Group”. Participants who used a prescription stimulant nonmedically at some point in their life prior to entry into college and never used during the four years of study (n=49), were considered to be non-users (included in Line 1 of Figure 1).
2) Persistent marijuana users who did not use prescription stimulants nonmedically (n=163). Annually, participants were asked on how many days in the past 12 months they had used marijuana. Persistent use of marijuana was defined as marijuana use at least once in the past year during all three consecutive follow-up years of the study (i.e., Years 2, 3, and 4) regardless of their use at baseline. Among persistent marijuana users, the average number of times marijuana was used in the past year in Years 2, 3, and 4 was 31.29, 41.29, and 44.06, respectively. This group is hereinafter referred to as the “Marijuana Group”.
3) Consistent non-users of other drugs (n=195). Annually, questions were asked about past-year use of eight illicit drugs (i.e., marijuana, inhalants, cocaine, hallucinogens, heroin, amphetamines, methamphetamine, and ecstasy) and nonmedical use of three classes of prescription drugs (i.e., stimulants, analgesics, and tranquilizers/benzodiazepines). Consistent non-use of drugs was defined as non-use of all eleven substances in all four assessments. Alcohol and tobacco use were not considered in this definition, and therefore did not disqualify participants from being included in this group, hereinafter referred to as the “Non-user Group”.
Figure 1. Patterns of nonmedical use of prescription stimulants across four years of study.
Note: Gray boxes = No use in the past 12 months; White boxes (+) = Used in the past 12 months
† Weighted Percent: Individuals who used drugs prior to college were purposively oversampled; however, we were able to statistically correct for our high-risk sampling design by computing sampling weights.
* Boxed rows represent individuals defined as “persistent nonmedical users of prescription stimulants.”
Measures
Adult ADHD symptoms
ADHD symptoms were measured in the Year 4 assessment using the Adult ADHD Self-Report Scale (ASRS; Kessler et al., 2005). The ASRS consists of 18 items that correspond to the DSM-IV criteria for ADHD (American Psychiatric Association, 1994). Nine questions comprised the inattention subscale, while the remaining nine comprised the hyperactivity-impulsivity subscale. This measure has demonstrated good internal consistency (Adler et al., 2006), sensitivity and specificity (Kessler et al., 2005), and excellent validity (Adler et al., 2006; Kessler et al., 2005; Reuter, Kirsch, & Hennig, 2006) in clinical and population samples.
For the present analyses, ADHD symptoms were operationalized in three ways. First, the total ASRS score was derived by summing the number of items endorsed at levels specified by Kessler et al. (2005; possible range 0-18). Second, subscale scores for inattention and hyperactivity-impulsivity were derived by summing the items pertaining to these two domains, respectively. Lastly, the “clinical threshold” for being at high-risk for ADHD (i.e., having an ASRS score of nine or higher) was used to dichotomize the sample into groups at high- and low-risk for ADHD (Kessler et al., 2005).
Other illicit and nonmedical drug use in the past year
As explained above, our analytic strategy included the Marijuana Group to understand the specificity of any observed associations between ADHD symptoms and NPS. To be conservative, we also included a variable that was a measure of general drug involvement. A summary measure was created based on the number of drugs used at least once in the past year at Year 4 (Caldeira, Arria, O'Grady, Vincent, & Wish, 2008). When computing this index, marijuana and NPS were excluded in the count, because their persistent use defined two of the groups. Consequently, the maximum total possible for the number of drugs used in the past year was nine.
Demographics
Data on sex and race were gathered in previous annual interviews. Sex was coded as observed by the interviewer at baseline, and race was obtained via self-report. A little less than half of the 470 participants were male (47%). Because over two-thirds of the sample were White (73.6%), race was dichotomized into White and non-White. Socioeconomic status (SES) was estimated from the average Adjusted Gross Income (AGI, reported in $10,000 increments) of the student's home zip code during 2003 (the participant's last year in high school).2 The study sample had a slightly higher representation of White students than the student population from which the sample was drawn, but no other demographic differences were observed.
Statistical Analyses
The analyses were conducted in two stages. First, simple descriptive comparisons of demographic characteristics and ADHD measures were made among the three groups. Chi-square tests were used to detect significant differences in categorical variables. One-way ANOVA was used to identify overall significant differences among the three groups. When a significant F-value was obtained from the overall ANOVA, we tested for particular subgroup differences using Tukey's Honestly Significant Difference (HSD) tests.
Second, a series of multinomial logistic regression analyses were conducted to examine the possible association of ADHD symptoms with the likelihood of membership in the three groups, and all possible comparisons between groups were evaluated. In these models, ADHD symptoms are the primary independent variables of interest, and group membership is the dependent variable. Separate models were developed based on the three different ways we operationalized ADHD symptoms, namely, the ASRS scale score, the two ASRS subscales separately, and the dichotomous variable representing “high risk” for ADHD (i.e., a score of nine or higher on the ASRS). Following the initial analysis, three additional models were developed to compare the stimulant group to the marijuana group on the basis of these three operational definitions of ADHD symptoms, controlling for past year drug use (data not shown in a table). All models controlled for sex, race, and SES. The threshold for significance was p≤.05.
Results
Table 1 presents descriptive comparisons of the three groups studied. The three groups were significantly different with respect to sex and Race/Ethnicity, with Whites and males being over-represented in the Stimulant Group and Marijuana Group compared to the Non-user Group. Moreover, the Stimulant Group used more drugs in the past year than the Marijuana Group (3.53 vs. 1.40), and scored higher on the total ASRS scale (m=4.96, SD=3.72) than the Marijuana Group (m=3.65, SD=3.24) and Non-user Group (m=3.64, SD=3.22). The Stimulant Group also scored higher on the Inattention Subscale of the ASRS (m=3.08, SD=2.26) than the other two groups (m=2.12, SD=2.03 and m=2.19, SD=2.26, respectively). By contrast, hyperactivity-impulsivity subscale scores were similar across all three groups. Finally, with respect to meeting the ASRS clinical cutoff score, sample prevalence was greatest in the Stimulant Group (17.0%) as compared to the Non-user Group (8.2%) and the Marijuana Group (9.2%).
Table 1.
Comparison of persistent nonmedical prescription stimulant users, persistent marijuana users, and consistent non-users of drugs with respect to demographics and Attention Deficit Hyperactivity Disorder (ADHD) symptoms measured by the Adult ADHD Self-Report Scale (ASRS).
| Stimulant Group n=112 |
Marijuana Group n=163 |
Non-User Group n=195 |
|
|---|---|---|---|
| Categorical Variablesa | n (%) | n (%) | n (%) |
|
| |||
| Sex (% male)* | 65 (58.0) | 84 (51.5) | 72 (36.9) |
| Race (% White)* | 95 (84.8) | 130 (79.8) | 121 (62.1) |
| High risk for ADHD (ASRS ≥ 9)*** | 19 (17.0) | 15 (9.2) | 16 (8.2) |
|
| |||
| Continuous Variablesb | m (SD) | m (SD) | m (SD) |
|
| |||
| Average AGI for parents zip codec | 7.62 (3.68) | 7.51 (3.58) | 7.12 (3.45) |
| Number drugs used in past year** | 3.53 (1.66) | 1.40 (0.72) | N/A |
| ASRS Inattention subscale score*** | 3.08 (2.26) | 2.12 (2.03) | 2.19 (2.26) |
| ASRS Hyperactivity-Impulsivity subscale score | 1.85 (1.97) | 1.53 (1.72) | 1.45 (1.49) |
| Total ASRS score*** | 4.96 (3.72) | 3.65 (3.24) | 3.64 (3.22) |
Chi square tests were used to detect statistically significant differences among groups.
One-way ANOVA was used to detect overall statistically significant differences among all groups; Tukey's HSD test was used to detect specific group differences.
The mean adjusted gross income (AGI) reported by the Internal Revenue Service for each participant's home ZIP code during their last year in high school, measured in ten thousands.
The Stimulant Group and the Marijuana Group are significantly different from the Non-User Group (p≤.05).
The Stimulant Group is significantly different from the Marijuana Group (p≤.05).
The Stimulant Group is significantly different from the Marijuana Group and the Non-User Group (p≤.05).
Table 2 displays results of the multinomial logistic regression analyses. In all three models, holding constant demographics, higher levels of ADHD symptoms were significantly related to being in the Stimulant Group (relative to either the Marijuana or the Non-user Group), but not with being in the Marijuana Group (relative to the Non-user Group). For example, looking at Model 1 in Table 2, the total ASRS score is associated with an increase in the likelihood of being in the Stimulant Group as compared to the Non-user Group (AOR=1.13, p<.01), and an increase in the likelihood of being in the Stimulant Group as compared to the Marijuana Group (AOR=1.12, p<.01). The association between the total ASRS score and the likelihood of being in the Stimulant Group as compared to the Marijuana Group remained significant when past-year drug use was controlled for in the model. There was no relationship between total ASRS score and the likelihood of being in the Marijuana Group as compared to the Non-user Group.
Table 2.
Adjusted odds ratios (AOR) for the multinomial logistic regression predicting comparative likelihood of membership in three groups: persistent nonmedical users of prescription stimulants, persistent marijuana users, and consistent non-users of drugs on the basis of different operational definitions of ADHD.a
| Group Membership | Model 1: Total ASRS Score AOR (CI) |
Model 2: Subscale Scores AOR (CI) |
Model 3: Clinical Cutoff Score AOR (CI) |
|---|---|---|---|
| Stimulant Group vs. Non-user Group | |||
| Male | 2.38 (1.45-3.93)* | 2.33 (1.40-3.87)* | 2.48 (1.50-4.09)* |
| White | 3.61 (1.94-6.72)* | 3.93 (2.08-7.43)* | 3.63 (1.95-6.73)* |
| Average AGI for parents zip codeb | 1.04 (0.97-1.12) | 1.04 (0.97-1.12) | 1.04 (0.97-1.12) |
| Total ASRS Score | 1.13 (1.05-1.21)* | ||
| Inattention Subscale Score | 1.18 (1.04-1.34)* | ||
| Hyperactivity-Impulsivity Subscale Score | 1.05 (0.88-1.24) | ||
| ASRS score ≥ 9 | 2.80 (1.32-5.95)* | ||
| Marijuana Group vs. Non-user Group | |||
| Male | 1.76 (1.14-2.72)* | 1.82 (1.17-2.83)* | 1.78 (1.15-2.76)* |
| White | 2.30 (1.41-3.75)* | 2.28 (1.40-3.71)* | 2.31 (1.42-3.76)* |
| Average AGI for parents zip codeb | 1.04 (0.97-1.10) | 1.04 (0.97-1.10) | 1.04 (0.97-1.10) |
| Total ASRS score | 1.01 (0.94-1.08) | ||
| Inattention Subscale Score | 0.96 (0.85-1.08) | ||
| Hyperactivity-Impulsivity Subscale Score | 1.07 (0.92-1.25) | ||
| ASRS score ≥ 9 | 1.29 (0.60-2.75) | ||
| Stimulant Group vs. Marijuana Group | |||
| Male | 1.36 (0.83-2.23) | 1.28 (0.77-2.12) | 1.39 (0.84-2.29) |
| White | 1.57 (0.81-3.03) | 1.73 (0.89-3.40) | 1.57 (0.81-3.03) |
| Average AGI for parents zip codeb | 1.00 (0.94-1.07) | 1.01 (0.94-1.08) | 1.01 (0.94-1.07) |
| Total ASRS score | 1.12 (1.04-1.20)* | ||
| Inattention Subscale Score | 1.23 (1.08-1.40)* | ||
| Hyperactivity-Impulsivity Subscale Score | 0.97 (0.82-1.15) | ||
| ASRS score ≥ 9 | 2.18 (1.04-4.56)* |
Operational definitions of ADHD: the total Adult ADHD Self-Report Scale (ASRS) score, inattention and hyperactivity-impulsivity subscale scores, and meeting the “Clinical” threshold on the ASRS
The mean adjusted gross income (AGI) reported by the Internal Revenue Service for each participant's home ZIP code during their last year in high school, measured in ten thousands.
p≤.05
As shown in Model 2, when the two subscale scores for inattention and hyperactivityimpulsivity were entered independently into the models, results indicated a significant effect for the inattention subscale but not the hyperactivity-impulsivity subscale. For example, each additional symptom endorsed on the inattention subscale resulted in an 18% increase in the likelihood of being in the Stimulant Group as compared to the Non-user Group (AOR=1.18, p=.01) and a 23% increase in the likelihood of being in the Stimulant Group as compared to the Marijuana Group (AOR=1.23, p<.01). The relationship between inattention symptoms and the likelihood of being in the Stimulant Group as compared to the Marijuana Group remained significant even controlling for past-year drug use. Neither subscale score was related to the likelihood of being in the Marijuana Group as compared to the Non-user Group. The hyperactivity-impulsivity scale score had no significant effect in any of the models.
Finally, Model 3 examines the association between meeting the ASRS clinical cutoff score and the likelihood of group membership. Having an ASRS scale score of nine or higher more than doubled the likelihood of being in the Stimulant Group as compared to the Non-user Group (AOR=2.80, p<.01) and as compared to the Marijuana Group (AOR=2.18, p=.04). The association between having an ASRS scale score of nine or higher and being in the Stimulant Group as compared to the Marijuana Group remained significant when past-year drug use was introduced into the model. Similar to above, meeting the ASRS clinical cutoff was not related to the likelihood of being in the Marijuana Group as compared to the Non-user Group.
Post-Hoc Analysis
A shortened version of the ASRS, consisting of six of the original 18 items, has demonstrated good sensitivity and specificity with a clinical diagnosis of ADHD (Kessler et al., 2005). A post-hoc analysis was performed examining the utility of this shorter version of the ASRS scale as a score in the multinomial model described above because it might have utility in future research studies where time and resources might be constrained. Moreover, the short form might pose less respondent burden especially in cases where attention problems are a concern. Similar to the original model results, controlling for sex, race, and SES, higher scores on the six-item ASRS scale significantly increased the likelihood of being in the Stimulant Group as compared to the Non-user Group (AOR=1.26, p<.01) or the Marijuana Group (AOR=1.34, p<.01; data not shown in a table), but had no relationship with the likelihood of being in the Marijuana Group as compared to the Non-user Group.
Discussion
This study provides strong and consistent evidence of an association between untreated ADHD symptoms and NPS. Using three different operational measures of ADHD symptoms derived from the ASRS, we observed significantly higher levels of ADHD symptoms among individuals who had an ongoing pattern of persistent NPS throughout college, regardless of whether we compared them with consistent non-users of drugs or persistent marijuana users. Importantly, these differences remained even after statistical adjustment for group differences in sex, race, SES, and other illicit drug use. Contrary to findings by Rabiner et al. (2009b), we observed no association between persistent NPS and the hyperactivity-impulsivity subscale of the ASRS.
Finally, it is important to note that although some ADHD symptoms appear to be related to NPS, many other factors contribute to persistent NPS. In the present study, of the 112 cases of persistent NPS we identified (i.e., the Stimulant Group), only 17% scored in the range for meeting “clinical criteria” for ADHD according to the ASRS. This suggests that although ADHD symptoms might contribute to NPS, further study is warranted to understand the role of other possible contributing factors, such as underlying problems with drug use and untreated mental health symptoms other than ADHD.
This study contributes important new information about a possible risk factor for NPS, namely untreated ADHD symptoms, and, in particular, inattention difficulties. The finding that ADHD symptoms were associated with NPS is consistent with prior evidence showing that a primary motive for NPS is to enhance concentration or wakefulness while studying (Carroll et al., 2006; DeSantis et al., 2009; DuPont et al., 2008; Prudhomme-White et al., 2006; Rabiner et al., 2009b). The idea that students with untreated ADHD symptoms might experience this motive more intensely than other students is intuitively appealing. However, the possibility that the ADHD symptoms are a result of other illicit drug use cannot be ruled out. Only a clinical evaluation would be able to determine whether students experiencing attention difficulties met clinical criteria for ADHD or whether the attention problems were a result of heavy drinking and other illicit drug use commonly seen in students who engage in NPS (Arria et al., 2008c; Arria et al., 2009). NPS most likely results from a complex set of circumstances. Future studies are needed to disentangle the various risk factors that appear to underlie NPS so that appropriate and distinct prevention and intervention strategies can be implemented.
Limitations
Several limitations of this study must be noted. First, as mentioned earlier, the ASRS was administered only in Year 4, whereas NPS was assessed all four years. Thus, with no information about the timing of the onset of ADHD symptoms, we cannot sort out the temporality between ADHD symptoms and NPS. Future research should examine longitudinal associations between ASRS scores and NPS in order to rule out the possibility that persistent NPS or coexisting substance use contributes to inattention problems. Second, although our measure of ADHD symptoms (the ASRS scale) has good reliability and validity (Adler et al., 2006; Kessler et al., 2005; Reuter et al., 2006), it is not a substitute for a thorough clinical evaluation. The ASRS measured current symptom levels and did not gather information about lifetime history of ADHD symptoms. Only through a clinical assessment can these features of ADHD be well characterized and investigated for their possible relationship to the onset of NPS. Third, information on other mental health problems or learning disabilities were not analyzed as possible contributors to NPS. It is possible that other mental health disorders that might have overlapping symptoms with ADHD (such as some anxiety disorders) might be related to both reported ADHD symptoms and NPS. Fourth, data were derived from self-report measures and thus are subject to bias. Future studies should attempt to collect corroborating information from key informants such as roommates and perhaps teachers regarding the onset and severity of inattention symptoms. These findings are most generalizable to college students attending large public universities and should not be construed to be generalizable to other postsecondary institutional settings like small private colleges, or young adults not attending college. Lastly, because we restricted our subsets of drug users to individuals with a longstanding pattern of use over several years, we cannot say how the observed associations might have been affected by the exclusion of individuals who used drugs less often or only intermittently.
Notwithstanding these limitations, the study has several noteworthy strengths, including the large sample size, the longitudinal design, the use of a standardized screening instrument for ADHD, and the ability to exclude cases with a previous clinical diagnosis of ADHD. Future longitudinal studies should investigate changes in ADHD symptoms over time and look for possible reciprocal effects of NPS and ADHD symptoms in an effort to better understand temporal patterning and possible causal pathways. Although the central focus was to contrast persistent nonmedical prescription stimulant users with non-users, future research is warranted to investigate the interrelationships between frequency and subjective effects of NPS and ADHD symptom severity. For example, it is possible that individuals who engage in NPS in order to study because they believe it improves concentration may use stimulants less frequently and more sporadically (i.e., largely around midterms and finals, with little to no use when classes are not in session) as compared to individuals who frequently use a variety of other drugs and use stimulants to get high. Furthermore, it may be of interest to examine whether persistent use is associated with experiencing positive subjective effects and what factors persistent and intermittent users differ on. Individuals who perceive benefits or find this form of drug use reinforcing might be more likely to continue the behavior. In addition, other analytic strategies could be employed, such as using the number of years of NPS to predict ADHD symptoms, rather than dividing the sample into groups.
Implications
This study provides evidence that persistent NPS among college students may be related to higher levels of ADHD symptoms in a way that appears to be quite distinct from other forms of drug use. This finding has implications for both health care professionals and prevention specialists. Clinical evaluations might be warranted when NPS coexists with self-reported high levels of inattention. A clinical evaluation can assess the degree to which these individuals are experiencing problems completing their work at the college level, and are nonmedically using prescription stimulants to improve academic performance. Research has linked untreated ADHD with lowered academic performance (Biederman, Faraone, Spencer, & Wilens, 1993; de Graaf et al., 2008; Kessler, Lane, Stang, & Van Brunt, 2008; Mannuzza & Klein, 2000; Weyandt & DuPaul, 2006). Given the strong association between NPS and other forms of illicit drug use (Arria et al., 2008b; McCabe et al., 2005; McCabe et al., 2006; Rabiner et al., 2009b; Teter et al., 2003), clinicians should conduct urine drug screens to evaluate the possibility that other drug use might also be a contributing factor to ADHD symptoms in nonmedical prescription stimulant users.
Conversely, clinicians who specialize in the management of ADHD, especially those who work in a college setting or who treat young adults in the community, should be cognizant of the prevalence of NPS and caution against diversion of these medications (Garnier et al., 2010). Moreover, they need to recognize the possible link between NPS and ADHD symptoms, and should inquire about NPS as a part of their clinical evaluation for ADHD. Given that 34.4% of the nonmedical users of prescription stimulants in this study were identified as persistent users, it is possible that more systematic attempts to evaluate and treat ADHD symptoms in these students may significantly decrease NPS.
From a prevention standpoint, it is important to target possible risk factors for NPS. While other studies have shown that heavy alcohol use, other illicit drug use, skipping class and lowered academic performance all are risk factors for NPS; this study highlights an additional risk factor to consider—namely, untreated ADHD symptoms. If the results of this study are replicated, prevention specialists should promote early identification and proper medical management of ADHD as one way of reducing NPS.
Despite the popular belief among students that NPS will increase their academic performance, there remains a lack of evidence supporting this claim. Rather, there is evidence suggesting an association between NPS and lower academic performance (Arria et al., 2008c; McCabe et al., 2005). There is a clear need for prevention messages that call into question the idea that NPS confers an advantage over traditional study habits. Furthermore, it is important to encourage college students to seek help for attention difficulties and untreated mental health symptoms. Most colleges employ personnel in counseling centers to help students who are experiencing academic difficulties. These campus-based offices typically offer classes on overcoming procrastination, test anxiety, and improving time management. In addition to these techniques, individuals who work in these offices could be trained to assess for untreated ADHD, NPS, mental health problems and substance use disorders that could be at the root of academic failure. Appropriate referrals for intervention and treatment could be given if warranted. This strategy might be a cost-effective way of targeting individuals who are most at risk for NPS and academic failure.
Footnotes
For the sake of brevity we are referring to all ADHD medications used nonmedically as prescription stimulants. However, two non-stimulant medications used to treat ADHD were used nonmedically by some participants in our sample (Provigil, n=1 and Strattera, n=5). However, all of these participants also nonmedically used stimulant-type ADHD medications.
Obtained from http://www.melissadata.com/lookups/taxzip.asp
References
- Adler LA, Spencer T, Faraone SV, Kessler RC, Howes MJ, Biederman J, Secnik K. Validity of pilot Adult ADHD Self- Report Scale (ASRS) to Rate Adult ADHD symptoms. Annals of Clinical Psychiatry. 2006;18(3):145–148. doi: 10.1080/10401230600801077. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. 4th ed. American Psychiatric Press; Washington, DC: 1994. [Google Scholar]
- Arria AM, Caldeira KM, O'Grady KE, Vincent KB, Fitzelle DB, Johnson EP, Wish ED. Drug exposure opportunities and use patterns among college students: Results of a longitudinal prospective cohort study. Substance Abuse. 2008a;29(4):19–38. doi: 10.1080/08897070802418451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Caldeira KM, O'Grady KE, Vincent KB, Johnson EP, Wish ED. Nonmedical use of prescription stimulants among college students: Associations with Attention-Deficit-Hyperactivity Disorder and polydrug use. Pharmacotherapy. 2008b;28(2):156–169. doi: 10.1592/phco.28.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, O'Grady KE, Caldeira KM, Vincent KB, Wish ED. Nonmedical use of prescription stimulants and analgesics: Associations with social and academic behaviors among college students. Journal of Drug Issues. 2008c;38(4):1045–1060. doi: 10.1177/002204260803800406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, Wilcox HC, Caldeira KM, Vincent KB, Wish ED, O'Grady KE. Dispelling the myth of smart drugs: Cannabis use problems and nonmedical use of prescription stimulants for studying; Paper presented at the College on Problems of Drug Dependence; 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bents RT, Marsh E. Patterns of Ephedra and other stimulant use in collegiate hockey athletes. International Journal of Sport Nutrition and Exercise Metabolism. 2006;16(6):636–643. doi: 10.1123/ijsnem.16.6.636. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Spencer T, Wilens T. Patterns of psychiatric comorbidity, cognition, and psychosocial functioning in adults with attention deficit hyperactivity disorder. American Journal of Psychiatry. 1993;150(12):1792–1798. doi: 10.1176/ajp.150.12.1792. [DOI] [PubMed] [Google Scholar]
- Caldeira KM, Arria AM, O'Grady KE, Vincent KB, Wish ED. The occurrence of cannabis use disorders and other cannabis-related problems among first-year college students. Addictive Behaviors. 2008;33(3):397–411. doi: 10.1016/j.addbeh.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll BC, McLaughlin TJ, Blake DR. Patterns and knowledge of nonmedical use of stimulants among college students. Archives of Pediatrics and Adolescent Medicine. 2006;160(5):481–485. doi: 10.1001/archpedi.160.5.481. [DOI] [PubMed] [Google Scholar]
- de Graaf R, Kessler RC, Fayyad J, ten Have M, Alonso J, Angermeyer M, Borges G, Demyttenaere K, Gasquet I, De Girolamo G, Haro JM, Jin R, Karam EG, Ormel J, Posada-Villa J. The prevalence and effects of adult attention-deficit/hyperactivitiy disorder (ADHD) on the performance of workers: Results from the WHO World Mental Health Survey Initiative. Occupational and Environmental Medicine. 2008;65:835–842. doi: 10.1136/oem.2007.038448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSantis A, Noar SM, Webb E. Non-medical ADHD stimulant use in fraternities. Journal of Studies on Alcohol and Drugs. 2009;70(6):952–954. doi: 10.15288/jsad.2009.70.952. [DOI] [PubMed] [Google Scholar]
- DuPont RL, Coleman JJ, Bucher RH, Wilford BB. Characteristics and motives of college students who engage in nonmedical use of methylphenidate. American Journal on Addictions. 2008;17(3):167–171. doi: 10.1080/10550490802019642. [DOI] [PubMed] [Google Scholar]
- Garnier-Dykstra LM, Pinchevsky GM, Caldeira KM, Vincent KB, Wish ED, Arria AM. Self-reported adult Attention Deficit Hyperactivity Disorder symptoms among college students. Journal of American College Health. doi: 10.1080/07448481.2010.483718. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnier LM, Arria AM, Caldeira KM, Vincent KB, O'Grady KE, Wish ED. Sharing and selling of prescription medications in a college student sample. Journal of Clinical Psychiatry. 2010;71(3):262–269. doi: 10.4088/JCP.09m05189ecr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall KM, Irwin MM, Bowman KA, Frankenberger W, Jewett DC. Illicit use of prescribed stimulant medication among college students. Journal of American College Health. 2005;53(4):167–174. doi: 10.3200/JACH.53.4.167-174. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, Ustun TB, Walters EE. The World Health Organization adult ADHD Self-Report Scale (ASRS): A short screening scale for use in the general population. Psychological Medicine. 2005;35:245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Lane M, Stang PE, Van Brunt DL. The prevalence and workplace costs of adult attention deficit hyperactivity disorder in a large manufacturing firm. Psychological Medicine. 2008;39:137–147. doi: 10.1017/S0033291708003309. [DOI] [PubMed] [Google Scholar]
- Low KG, Gendaszek AE. Illicit use of psychostimulants among college students: A preliminary study. Psychology, Health and Medicine. 2002;7(3):283–287. [Google Scholar]
- Mannuzza S, Klein RG. Long-term prognosis in attention-deficit/hyperactivity disorder. Child and Adolescent Psychiatric Clinics of North America. 2000;9(3):711–726. [PubMed] [Google Scholar]
- McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: Prevalence and correlates from a national survey. Addiction. 2005;99:96–106. doi: 10.1111/j.1360-0443.2005.00944.x. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. Journal of Psychoactive Drugs. 2006;38(1):43–56. doi: 10.1080/02791072.2006.10399827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prudhomme-White B, Becker-Blease KA, Grace-Bishop K. Stimulant medication use, misuse, and abuse in an undergraduate and graduate student sample. Journal of American College Health. 2006;54(5):261–268. doi: 10.3200/JACH.54.5.261-268. [DOI] [PubMed] [Google Scholar]
- Rabiner DL, Anastopoulos AD, Costello EJ, Hoyle RH, McCabe SE, Swartzwelder HS. The misuse and diversion of prescribed ADHD medications by college students. Journal of Attention Disorders. 2009a;13:144–153. doi: 10.1177/1087054708320414. [DOI] [PubMed] [Google Scholar]
- Rabiner DL, Anastopoulos AD, Costello EJ, Hoyle RH, McCabe SE, Swartzwelder HS. Motives and perceived consequences of nonmedical ADHD medication use by college students: Are students treating themselves for attention problems? Journal of Attention Disorders. 2009b;13(3):259–270. doi: 10.1177/1087054708320399. [DOI] [PubMed] [Google Scholar]
- Reuter M, Kirsch P, Hennig J. Inferring candidate genes for Attention Deficit Hyperactivity Disorder (ADHD) assessed by the World Health Organization Adult ADHD Self-Report Scale (ASRS) Journal of Neural Transmission. 2006;113:929–938. doi: 10.1007/s00702-005-0366-5. [DOI] [PubMed] [Google Scholar]
- Teter CJ, McCabe SE, Boyd CJ, Guthrie SK. Illicit methylphenidate use in an undergraduate student sample: Prevalence and risk factors. Pharmacotherapy. 2003;23(5):609–617. doi: 10.1592/phco.23.5.609.34187. [DOI] [PubMed] [Google Scholar]
- Teter CJ, McCabe SE, LaGrange K, Cranford JA, Boyd CJ. Illicit use of specific prescription stimulants among college students: prevalence, motives, and routes of administration. Pharmacotherapy. 2006;26(10):1501–1510. doi: 10.1592/phco.26.10.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weyandt LL, DuPaul G. ADHD in college students. Journal of Attention Disorders. 2006;10(1):9–19. doi: 10.1177/1087054705286061. [DOI] [PubMed] [Google Scholar]
- Wilens TE, Adler LA, Adams J, Sgambati S, Rotrosen J, Sawtelle R, Utzinger L, Fusillo S. Misuse and diversion of stimulants prescribed for ADHD: A systematic review of the literature. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(1):21–31. doi: 10.1097/chi.0b013e31815a56f1. [DOI] [PubMed] [Google Scholar]