Summary
Over 73,700 adults age 40–79, nearly 70% African American, were recruited at community health centers across 12 southeastern states; individual characteristics were recorded and biologic specimens collected at baseline for later follow-up. The Southern Community Cohort Study is a unique national resource for assessing determinants of racial/ethnic differentials in diseases.
Keywords: Cancer, cohort study, African Americans, health disparities, community health studies
The incidence of and mortality from several cancers, cardiovascular disease, stroke, diabetes, and many other chronic illnesses tend to be greater among African Americans than among other population groups in the United States.1,2 The Meharry-Vanderbilt Alliance, described in this issue of the Journal, has stimulated research addressing this national problem. One such major initiative launched by investigators at Vanderbilt, Meharry, the International Epidemiology Institute, and Community Health Centers throughout the Southeast is the Southern Community Cohort Study (SCCS).3 The goal of the SCCS is to elucidate and discover the sources of higher rates of cancer and other diseases among African Americans in comparison with Whites in this region. The SCCS protocols are reviewed and approved by Institutional Review Boards at Vanderbilt University and Meharry Medical College.
Here, we describe the partnership between scientific investigators and local health centers that has enabled the recruitment of large numbers of adults into the SCCS. The study methods are outlined, characteristics of the cohort are presented, and unique opportunities for research in the coming years are outlined.
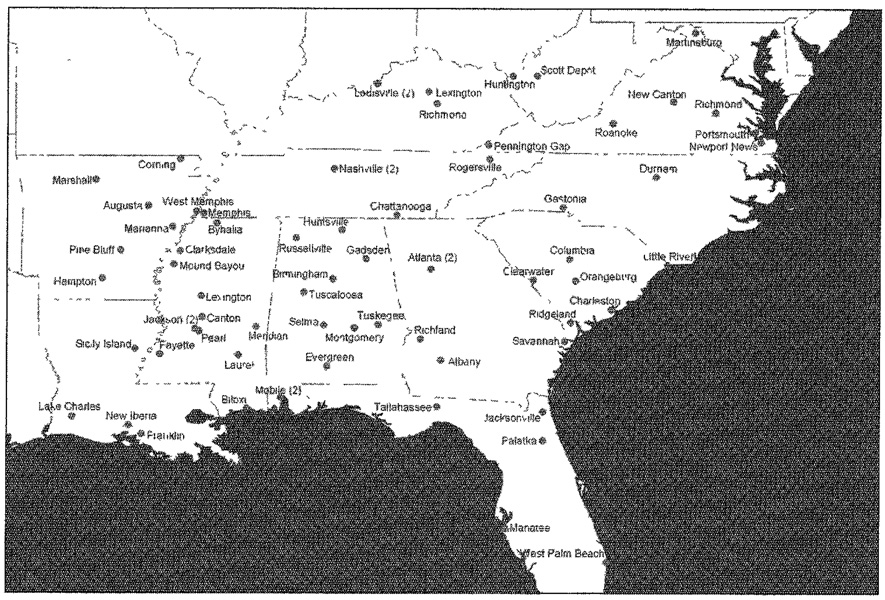
Recruitment of study subjects. Recruitment of participants into the SCCS across a 12-state area of the Southeast (Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, and West Virginia) (Figure 1) began in March 2002 and was completed in September 2009. Some participants entered the study by completing questionnaires mailed to random samples of adults, but most (approximately 85%) of the participants were enrolled at community health centers (CHCs), institutions offering basic health and preventative services mainly to the medically uninsured.4 We focus on the CHC component of the SCCS in this paper. The 71 CHCs working together with the SCCS, which are listed in Box 1, have provided a venue through which some of the barriers to recruitment of minorities and the poor into health research could be overcome. Paramount was the established relationship between the centers and the local community. The CHCs were a welcoming and familiar place where essential health and community services were routinely obtained by community residents; thus, when CHC interviewers approached people coming to the centers* and asked if they might be willing to join in a health study to assess the causes of cancer, many agreed and took the time to provide informed consent and complete the study interview. Prior to the SCCS, few CHCs had participated in large-scale epidemiologic studies and few existing cohorts had sizeable percentages of minority, poor, rural, or medically underserved participants. Thus the SCCS fills a gap in population coverage and provides a unique assembly of adults, nearly two-thirds African American, at elevated risk of cancer and several other chronic diseases.
Figure 1.
Locations of community health center enrollment sites.
Box 1.
COMMUNITY HEALTH CENTERS PARTICIPATING IN THE SCCS (SOUTHERN COMMUNITY COHORT STUDY)
| Clinic Name | Main City | State |
|---|---|---|
| Birmingham Health Care, Inc. | Birmingham | AL |
| Central Alabama Comprehensive Health, Inc. | Tuskegee | AL |
| Central North Alabama Health Services, Inc. | Huntsville | AL |
| Family-Oriented Primary Health Care Clinic, Inc. | Mobile | AL |
| Franklin Primary Health Center, Inc. | Mobile | AL |
| Health Services, Inc. | Montgomery | AL |
| Mostellar Medical Center | Bayou La Batre | AL |
| Quality of Life Health Services, Inc. | Gadsden | AL |
| Rural Health Medical Program, Inc. | Selma | AL |
| Southern Rural Health Care Consortium | Russellville | AL |
| Tri-County Medical Center, Inc. | Evergreen | AL |
| Whatley Health Services, Inc. | Tuscaloosa | AL |
| Boston Mountain Rural Health Center | Marshall | AR |
| CABUN Rural Health Services, Inc. | Hampton | AR |
| Corning Area Healthcare, Inc. | Corning | AR |
| East Arkansas Family Health Center, Inc. | West Memphis | AR |
| Jefferson Comprehensive Care System, Inc. | Pine Bluff | AR |
| Lee County Cooperative Clinic, Inc. | Marianna | AR |
| White River Rural Health Center, Inc. | Augusta | AR |
| Bond Community Health Center | Tallahassee | FL |
| Family Medical and Dental Centers | Palatka | FL |
| Florida Community Health Centers, Inc. | W Palm Beach | FL |
| Jacksonville Community Health Center, Inc. | Jacksonville | FL |
| Manatee County Rural Health Services, Inc. | Parrish | FL |
| Albany Area Primary Health Care, Inc. | Albany | GA |
| Southside Medical Center, Inc. | Atlanta | GA |
| Stewart Webster Rural Health, Inc. | Richland | GA |
| West End Medical Centers, Inc. | Atlanta | GA |
| Westside-Urban Health Center | Savannah | GA |
| Family Health Centers, Inc. | Louisville | KY |
| Lexington-Fayette County Health Department | Lexington | KY |
| Park DuValle Community Health Center | Louisville | KY |
| White House Clinics | Richmond | KY |
| Catahoula Parish Hospital Service District No. 2 | Sicily Island | LA |
| Iberia Comprehensive Community Health Center | New Iberia | LA |
| Southwest Louisiana Center for Health Services | Lake Charles | LA |
| Teche Action Clinic | Franklin | LA |
| Aaron E. Henry Community Health Services Center, Inc. | Clarksdale | MS |
| Central Mississippi Health Services, Inc. | Jackson | MS |
| Coastal Family Health Center, Inc. | Biloxi | MS |
| Delta Health Center, Inc. | Mound Bayou | MS |
| Dr. Arenia C. Mallory Community Health Center, Inc. | Lexington | MS |
| Family Health Care Clinic, Inc. | Pearl | MS |
| Family Health Center, Inc. | Laurel | MS |
| G.A. Carmichael Family Health Center | Canton | MS |
| Greater Meridian Health Clinic, Inc. | Meridian | MS |
| Jackson-Hinds Comprehensive Health Center | Jackson | MS |
| Jefferson Comprehensive Health Center, Inc. | Fayette | MS |
| Northeast Mississippi Health Care, Inc. | Byhalia | MS |
| Gaston Family Health Services, Inc. | Gastonia | NC |
| Lincoln Community Health Center, Inc. | Durham | NC |
| Beaufort-Jasper-Hampton Comprehensive Health Services, Inc |
Ridgeland | SC |
| Eau Claire Cooperative Health Centers | Columbia | SC |
| Family Health Centers, Inc. | Orangeburg | SC |
| Franklin C. Fetter Family Health Center | Charleston | SC |
| Little River Medical Center, Inc. | Little River | SC |
| Margaret J. Weston Medical Center | Clearwater | SC |
| Matthew Walker Comprehensive Health Center, Inc. | Nashville | TN |
| Memphis Health Center, Inc. | Memphis | TN |
| Rural Health Services Consortium, Inc. | Rogersville | TN |
| Southside & Dodson Avenue Community Health Centers | Chattanooga | TN |
| United Neighborhood Health Services, Inc. | Nashville | TN |
| Central Virginia Community Health Center | New Canton | VA |
| New Horizons Healthcare | Roanoke | VA |
| Peninsula Institute for Community Health | Newport News | VA |
| Portsmouth Community Health Center | Portsmouth | VA |
| St. Charles Health Council, Inc. | Pennington Gap | VA |
| Vernon J. Harris Medical Center | Richmond | VA |
| Shenandoah Valley Medical System | Martinsburg | WV |
| Valley Health Systems, Inc. | Huntington | WV |
| WomenCare, Inc. | Scott Depot | WV |
Study questionnaire. After signing the informed consent document describing the study’s rationale, risks, and benefits, the participants completed the baseline 45–60 minute in-person interview. The interview was administered by CHC personnel specially trained in computer-assisted interviewing techniques. The laptop computers housed the structured study questionnaire, as well as prompts and skips induced by certain responses, which aided in the flow of the interview and the standardization of the information collected. The questionnaire delved into various aspects of the participant’s characteristics, behaviors, and health status. Sections included demographic characteristics (education, income, residence); tobacco use; medical history; family history of cancer, heart disease, and diabetes; medication use; physical activity; emotional well-being and spirituality; health services utilization; home environment; occupation; and (via a food frequency questionnaire [FFQ]) diet and nutrition.
Biologic specimens. The SCCS also sought and obtained biologic specimen donations from many of the participants. At the CHCs participants were asked to donate a 20-ml blood sample and, beginning in the third year of the study, a urine specimen, but a buccal cell or saliva specimen was accepted if the subject did not wish to donate blood.
Validation studies. Although many of the questions in the SCCS questionnaire were adapted from questionnaires used and validated in other settings, a series of validation studies were also carried out to assess the reliability of the questionnaires within the SCCS. Selecting samples of approximately 150 to 800 SCCS participants (size depending on the needs of the particular validation study), we sought to validate FFQ information via 24-hour dietary recalls and/or nutrient biomarkers, physical activity patterns via repeat interviews and use of accelerometers, tobacco use status via measurement of serum cotinine, and disease occurrence for self-reported diabetes via confirmation in medical records and by measurement of HbAlc. Self-reported height and weight were compared with contemporaneous clinic recorded measurements for over 20% of the participants. We also collected and banked repeat blood samples from over 650 participants and repeat urine samples from over 240 participants for future comparability assays to check for concordance of biomarker levels over time periods spanning one to three years.
Follow-up of participants. Active follow-up has begun for approximately 30,000 of the early (March 2002–August 2004) entrants into the SCCS. A four-page follow-up questionnaire (one for males, one for females) was mailed, with second and third mailings to non-responders succeeded by telephone calling. Subsequent mailings/telephone calls to the remainder of the cohort participants will be conducted in batches in an attempt to have the first follow-up questionnaire completed approximately five years after entry into the SCCS, and additional follow-up questionnaires completed every five years thereafter.
The roster of participants enrolled in the SCCS was recently submitted to the Social Security Administration (SSA) for determination of current vital status. Cohort member information for those known through SSA to have died (or whose current status is unknown to SSA) will be sent to the National Death Index (NDI) to ascertain cause (or fact and cause) of death. The SSA and NDI submissions will then be updated annually.
The process of linkage with cancer registries has also begun in the 12 states in which recruitment has taken place. These searches will be the primary means of identification of incident cancer diagnoses. Although reporting lags of one to two years are common, the registries provide nearly complete and unbiased ascertainment of cancers diagnosed among the participants after their entry into the SCCS. Once sufficient numbers of cancer cases have been identified, a series of case-control studies nested within the SCCS will be launched to test specific hypotheses about etiologic factors for specific cancers and other diseases and the sources of racial disparities. The major cancers (those occurring in the lung, breast, prostate and colon/rectum) will be evaluated in the next several years, followed by cancers with less frequent occurrence thereafter.
Overview of initial findings. A total of approximately 73,700 men and women age 40–79 have been enrolled in the SCCS at the CHCs shown in Box 1. The composition of the cohort reflects the composition of persons in the study age range seen at the CHCs, with nearly 70% being African American and the remainder mainly non-Hispanic White, and 60% being female (Table 1). The median age at entry was approximately 51 years.
Table 1.
NUMBERS OF PARTICIPANTS ENROLLED IN THE SOUTHERN COMMUNITY COHORT STUDY AT COMMUNITY HEALTH CENTERS ACCORDING TO SEX, RACE, AND AGE
| Sex | Race | Age at Entry (years) | Na |
|---|---|---|---|
| Male | African American | 40–49 | 11,200 |
| 50–59 | 7,000 | ||
| 60–79 | 2,900 | ||
| Total | 21,100 | ||
| Otherb | 40–49 | 3,700 | |
| 50–59 | 2,600 | ||
| 60–79 | 1,700 | ||
| Total | 8,000 | ||
| Female | African American | 40–49 | 14,300 |
| 50–59 | 9,700 | ||
| 60–79 | 5,500 | ||
| Total | 29,500 | ||
| Otherb | 40–49 | 6,100 | |
| 50–59 | 5,100 | ||
| 60–79 | 3,800 | ||
| Total | 15,100 | ||
| Total | Total | Total | 73,700 |
Rounded to nearest 100.
Among males, “Other” race is comprised of Caucasians (83 7%), Hispanic (2.3%), Asian or Pacific Islander (0 3%), American Indian or Alaska Native (1.3%), Other racial group (1.6%), Mixed racial group (6.5%), or unknown/missing racial group (4.4%). Among females, “Other” race is comprised of Caucasians (83.0%), Hispanic (2.2%), Asian or Pacific Islander (0.4%), American Indian or Alaska Native (1.3%), Other racial group (1.4%), Mixed racial group (6.2%), or unknown/missing racial group (5.6%).
Table 2 shows that the majority of these SCCS participants reported low household incomes, and that nearly one-third had not completed high school. Table 2 also shows selected characteristics of the participants which place them at elevated risk for future adverse health outcomes. Notable are the high prevalences of (1) current cigarette smokers (reaching nearly 60% among Black men), (2) obesity (reaching 57% among Black women), and (3) diabetes (affecting nearly one-fifth of the cohort members).
Table 2.
SELECTED CHARACTERISTICS OF SOUTHERN COMMUNITY COHORT STUDY PARTICIPANTS ENROLLED AT COMMUNITY HEALTH CENTERSa
| Males |
Females |
||||
|---|---|---|---|---|---|
| African American |
Otherc | African American |
Otherc | ||
| Indicator | Level | (n=21,100)b | (n=8,000)b | (n=29,500)b | (n=15,100)b |
| Education (years) | <12 | 35 | 30 | 32 | 28 |
| 12 | 37 | 35 | 34 | 34 | |
| >12 | 27 | 35 | 34 | 38 | |
| Income ($ 1000s) | <15 | 64 | 58 | 62 | 56 |
| 15–25 | 22 | 21 | 23 | 20 | |
| >25 | 15 | 21 | 15 | 23 | |
| Body Mass | <25 | 38 | 30 | 17 | 25 |
| Index (kg/m2) | 25–29 | 35 | 35 | 25 | 26 |
| 30–34 | 17 | 20 | 25 | 22 | |
| 35–39 | 7 | 9 | 17 | 13 | |
| >40 | 4 | 6 | 16 | 14 | |
| Smoker | Never | 21 | 20 | 47 | 37 |
| Former | 19 | 27 | 19 | 24 | |
| Current | 60 | 53 | 34 | 39 | |
| Diabetes | Yes | 18 | 20 | 25 | 22 |
Numbers in the body of the table are percentages.
Rounded to nearest 100
Among males, “Other” race is comprised of Caucasians (83.7%), Hispanic (2.3%), Asian or Pacific Islander (0 3%), American Indian or Alaska Native (1.3%), Other racial group (1.6%), Mixed racial group (6 5%), or unknown/missing racial group (4.4%) Among females, “Other” race is comprised of Caucasians (83.0%), Hispanic (2 2%), Asian or Pacific Islander (0.4%), American Indian or Alaska Native (1.3%), Other racial group (1.4%), Mixed racial group (6.2%), or unknown/missing racial group (5.6%).
As shown in Table 3, biologic specimens have been donated by 90% (54% blood, 39% buccal cell, with 2% donating both) and have been shipped and placed in long-term frozen storage in our facilities at Vanderbilt. Since we began to collect urine specimens, nearly 60% of the CHC participants have provided the supplemental urine specimen. With blood separated into 14 vials, buccal cells into one vial, and urine into eight vials, the SCCS biospecimen repository now contains over 750,000 aliquots.
Table 3.
SOUTHERN COMMUNITY COHORT STUDY BIOSPECIMEN DONATIONS AT COMMUNITY HEALTH CENTERS
| Blood | Buccal | Urine | ||
|---|---|---|---|---|
| Sex | Race | Na | Na | Na |
| Male | African American | 11,500 | 7,600 | 5,900 |
| Otherb | 4,600 | 2,400 | 3,100 | |
| Female | African American | 15,000 | 13,400 | 8,600 |
| Otherb | 8,600 | 5,300 | 6,100 | |
| Total | Total | 39,700 | 28,700 | 23,700 |
Rounded to nearest 100.
Among males, “Other” race is comprised of Caucasians (83.7%), Hispanic (2 3%), Asian or Pacific Islander (0.3%), American Indian or Alaska Native (1.3%), Other racial group (1 6%), Mixed racial group (6.5%), or unknown/missing racial group (4.4%). Among females, “Other” race is comprised of Caucasians (83 0%), Hispanic (2.2%), Asian or Pacific Islander (0 4%), American Indian or Alaska Native (1.3%), Other racial group (1.4%), Mixed racial group (6 2%), or unknown/missing racial group (5.6%).
Questionnaire validation efforts are nearing completion. Results to date show correlations between self-reported and clinic recorded height and weight exceeding 0.95, and we have validated 96% of self-reported diabetes diagnoses from confirmatory medical records or elevated HbAlc measurements. Ongoing analyses show much lower correlations between multiple nutrient and physical activity indices derived from the questionnaire responses vs. from the special validation surveys, but the associations were significant and generally in line with those reported in other cohorts.
With the establishment of the cohort completed and the systematic follow-up now identifying cases of death and illness among study participants, opportunities abound for the utilization of the SCCS resource to help identify the causes of cancer and other chronic diseases and contributors to the higher incidence and/or mortality rates among African Americans than among Whites. To date, most SCCS studies have been cross-sectional, using the baseline questionnaire data and stored biologic specimens, but incidence-based prospective analyses will be feasible in the coming years.
Highlights of some of the recent cross-sectional analyses include findings that: (1) While national studies show up to two-fold excesses of diabetes in Blacks compared with Whites, in the SCCS, where socioeconomic differences are minimal, the crude prevalence of diabetes was only 34% higher among African American than White women, with the excess cut in half when body mass index and other factors were adjusted for, and there was little racial differential among men;5 (2) African Americans in the South had markedly lower levels of serum vitamin D (25(OH)D) than Whites, with nearly half the SCCS Black population having levels below 15 ng/ml, and that even among those with supposed adequate dietary vitamin D intakes, nearly one-third had insufficient levels;6 (3) colonoscopy screening was only half as common among Black as among White participants, even among those with family histories of colorectal cancer;7,8 (4) high (>3 mg/1) C-reactive protein levels were four times more common among the obese than those with BMI <25 kg/m2, significantly increased by 60 to 80% among smokers and women, and after adjustment for these factors 40% more common among Blacks than Whites;9 (5) benign prostatic hyperplasia (BPH) was reported only half as often by Black (4.4%) than White (9.9%) male SCCS participants, although among those with BPH, Blacks more often than Whites underwent surgical intervention for treatment of the condition;10 and (6) development of a nutrient database taking gender, race and geographic region into account provided improvements, compared with using overall national food composition data, in food frequency questionnaire scoring for most micro- and macro-nutrients.11
Discussion
The SCCS is now established as a national resource for research into the causes of chronic diseases among African Americans and into differentials in risk factors and outcomes between Blacks and Whites. The data collected on each individual are extensive, and cover a wide range of behavioral, environmental, medical, and other attributes. All observational epidemiologic studies are subject to some misclassification of information, and pure gold standards to assess the true status of reported exposures or conditions are often not available. However, the validation efforts completed thus far indicate that the survey questionnaire used in the SCCS yields information that can be considered as generally reliable and repeatable, with concordances between study questionnaire data and that from the validation sub-studies typically similar to those reported in other cohorts. The biospecimen repository is a particular strength of the SCCS, with DNA available for 90% and stored blood and urine samples for large subsets of the cohort.
The cohort was assembled through the cooperation of a network of community health centers throughout the South, enabling important access to a vulnerable segment of the American population often not included in health research. The characteristics of the enrollees, particularly the high rates of smoking and of obesity, are such that the cohort is likely to experience elevated incidences of cancer, cardiovascular disease, kidney disease, and other chronic illnesses in the years to come. We hope that the knowledge gained from the research enabled by the SCCS will provide needed information to develop effective strategies aimed at primary cancer and other disease prevention (identifying the determinants of an illness so that steps can be taken to avoid its occurrence), secondary prevention (identifying the process of disease development at a preclinical or an early enough stage when it is more amenable to treatment), and tertiary prevention or control (minimizing the adverse impacts of the disease once it occurs). Such strategies can then be tested for effectiveness within the SCCS population itself, or within the CHC patient population generally.
The SCCS has strong community ties and adheres to many of the principles of community-based participatory research (CBPR), although some elements of CBPR are not incorporated, primarily due to the extended geographical area and large size and scope of this project. The study investigators and CHC partners have clearly engaged underserved communities to specific action around health issues of concern to them. Although the entire community could not be part of the research design process, directors and staff of the CHCs had significant impact on early design choices, selection of recruitment methods and questionnaire design, and also allowed the piloting of design options to occur within the CHCs. The SCCS has also increased community capacity in carrying out research, as many CHCs now have the expertise necessary to take part in or oversee other research activities. De-identified data are also available to the CHCs. However, the community does not share full control in data analysis or interpretation and formal community advisory boards do not guide the direction of the research, although CHC leaders are consulted in a number of topic areas.
The SCCS resource is being utilized by faculty at Vanderbilt and Meharry, and the Meharry-Vanderbilt Alliance, but is available to scientific researchers globally. Plans are underway for the routine computation by the SCCS study team of rates among cohort members classified by race, gender, and various baseline characteristics of the following health outcomes: overall mortality; cause-specific mortality; cause-specific cancer incidence; and, pending governmental approvals, cause-specific rates of hospitalization for cardiovascular and cerebrovascular disease, diabetes, end-stage renal disease, and other conditions. We will also continue direct follow-up of the cohort via mail and telephone survey. As cancer cases accrue from the cohort follow up, nested case-control studies can begin, first testing hypotheses related to the determinants among African Americans of lung, breast, prostate, and colorectal cancer and of common non-malignant diseases, and assessing the underlying reasons for cancer and other health disparities.
Additional research opportunities utilizing the SCCS abound. The cohort provides a unique resource for new investigations studying determinants of the higher rates and poorer outcomes not just of cancer but also of various other chronic diseases among African Americans, and for determining contributors to health disparities.
In addition to cancer investigations, a few of the possibilities for additional research include studies involving: (1) linkage of the cohort with Medicare and Medicaid files maintained by the CMS to ascertain diagnoses and compute rates of cardiovascular, cerebrovascular, neurologic and other diseases, as well as data on physician encounters, medications, and costs associated with these illnesses; (2) assessment of the natural history of chronic renal disease, including characterizing serum creatinine levels and linkage of the cohort with the national end-stage renal disease registry; (3) prospective studies of the characteristics and outcomes among the over 15,000 diabetics in the SCCS and evaluations of HbAlc and other markers for characterization of the prevalence and determinants of undetected diabetes; (4) evaluations of the correlates and determinants of obesity and the interrelationships of obesity with other morbidities; (5) barriers to access and utilization of health services experienced by the medically uninsured or underinsured; (6) assessment of serum 25(OH)D and other measures of Vitamin D and their relations to cardiovascular and other diseases; (7) assessment of blood and/or urinary biomarkers and exposure to various environmental agents and how they are associated with chronic disease outcomes; (8) quality of life, function, and other attributes of survivors of chronic illnesses; (9) depression as a risk and prognostic factor for various disease outcomes; and (10) utilization of the SCCS DNA repository for genetic studies, including genome-wide association studies, for a large variety of diseases.
These are just a few of the many types of investigations that could be initiated within the SCCS at a fraction of the cost of de novo studies. The SCCS study team at Vanderbilt University, Meharry Medical College, and the International Epidemiology Institute welcomes inquiries and interests in collaborations to help fully make use of this national resource. Interested scientists can find instructions for gaining access to study materials by visiting the SCCS web site (www.southerncommunitystudy.org).
Footnotes
The large majority of participants were enrolled at the CHC facility itself, although some were recruited through outreach efforts in the surrounding community
Notes
- 1.National Center for Health Statistics. Health, United States, 2007, with chartbook on trends in the health of Americans. Hyattsville, MD: U.S. Department of Health and Human Services; 2007. [PubMed] [Google Scholar]
- 2.Horner MJ, Ries LAG, Krapcho M, et al., editors. Bethesda, MD: National Cancer Institute; SEER cancer statistics review, 1975–2006. 2009 Available at: http://seer.cancer.gov/csr/1975_2006/, based on November 2008 SEER data submission, posted to the SEER web site, 2009.
- 3.Signorello LB, Hargreaves MK, Steinwandel MD, et al. Southern Community Cohort Study: establishing a cohort to investigate health disparities. J Natl Med Assoc. 2005 Jul;97(7):972–979. [PMC free article] [PubMed] [Google Scholar]
- 4.Hargreaves MK, Arnold CW, Blot WJ. Community health centers: their role in the treatment of minorities and in health disparities research. In: Satcher D, Pamies R, editors. Multicultural medicine and health disparities. Columbus, OH: The McGraw-Hill Companies; 2006. [Google Scholar]
- 5.Signorello LB, Schlundt DG, Cohen SS, et al. Comparing diabetes prevalence between African Americans and Whites of similar socioeconomic status. Am J Public Health. 2007 Dec;97(12):2260–2267. doi: 10.2105/AJPH.2006.094482. Epub 2007 Oct 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Egan KM, Signorello LB, Munro HM, et al. Vitamin D insufficiency among African Americans in the southeastern United States: implications for cancer disparities (United States) Cancer Causes Control. 2008 Jun;19(5):527–535. doi: 10.1007/s10552-008-9115-z. Epub 2008 Jan 25. [DOI] [PubMed] [Google Scholar]
- 7.Murff HJ, Peterson NB, Fowke JH, et al. Colonoscopy screening in African-Americans and Whites with affected first-degree relatives. Arch Intern Med. 2008 Mar 24;168(6):625–631. doi: 10.1001/archinte.168.6.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peterson NB, Murff HJ, Fowke JH, et al. Use of colonoscopy and flexible sigmoidoscopy among African Americans and Whites in a low-income population. Prev Chronic Dis. 2008 Jan;5(1):A28. Epub 2007 Dec 15. [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang X, Shu XO, Signorello LB, et al. Correlates of high serum C-reactive protein levels in a socioeconomically disadvantaged population. Dis Markers. 2008;24(6):351–359. doi: 10.1155/2008/509138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fowke JH, Murff HJ, Signorello LB, et al. Race and socioeconomic status are independently associated with benign prostatic hyperplasia. J Urol. 2008 Nov;180(5):2091–2096. doi: 10.1016/j.juro.2008.07.059. Epub 2008 Sep 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Signorello LB, Munro HM, Buchowski MS, et al. Estimating nutrient intake from a food frequency questionnaire: incorporating the elements of race and geographic region. Am J Epidemiol. 2009 Jul 1;170(1):104–111. doi: 10.1093/aje/kwp098. Epub 2009 May 18. [DOI] [PMC free article] [PubMed] [Google Scholar]