Abstract
Aim: Over the last years, health-related quality of life (HRQOL) has emerged as an important measure not only in somatic medicine but also in psychiatry. To date, there are only few reports on HRQOL in patients with autism-spectrum disorder (ASD). This study aimed at studying HRQOL in ASD patients with an IQ >70, using a self-report HRQOL questionnaire with cross-cultural validity.
Methods: In this cross-sectional study, twenty-six male adolescents and young adults with the diagnosis of Asperger Syndrome, high functioning autism and atypical autism were evaluated, using the German version of the WHOQOL-BREF HRQOL questionnaire.
Results: Mean WHOQOL-BREF global scores were 60.6 (SD ±26.1), mean WHOQOL-BREF subscale scores were 70.1 (SD ±19.1) for the domain “physical health”, 61.5 (SD ±21.9) for the domain “psychological health”, 53.8 (SD ±23.5) for the domain “social relationships” and 67.9 (SD ±17.4) for the domain “environment”. Compared to a reference population of healthy controls, our sample scored significantly lower in three of four WHOQOL-BREF domains. In comparison to a reference sample of individuals with schizophrenia spectrum disorder (SSD), HRQOL of our sample was significantly better in all domains except for the “social relations” domain. There was a significant association between HRQOL and the Vineland Adaptive Behavior Scales domain “daily living skills”, but not with age, IQ, or ADOS-G summary scores.
Conclusion: Overall self-reported HRQOL in patients with high functioning ASD seems to be lower than in healthy individuals, but better than in patients with SSD. Also, higher HRQOL was associated with better daily living skills. This interrelationship should especially be accounted for in the design and application of treatment programmes for individuals with ASD, as it is of importance for the level of self-perceived HRQOL.
Keywords: autism, autism-spectrum disorder, health-related quality of life, schizophrenia-spectrum disorder, WHOQOL-BREF
Abstract
Zielsetzung: In den vergangenen Jahren hat sich die gesundheitsbezogene Lebensqualität (gbLQ) als wichtige Zielgröße nicht nur in der somatischen Medizin, sondern auch in den psychiatrischen Fächern etabliert. Bisher liegen nur wenige Studien zur gbLQ von Patienten mit Autismus-Spektrum-Störung (ASS) vor. Ziel dieser Studie war die Erfassung der gbLQ von Patienten mit ASS mit IQ >70 aus Patientenperspektive unter Verwendung eines international eingesetzten und validierten gbLQ-Instruments.
Methodik: 26 männliche Jugendliche und junge Erwachsene mit den Diagnosen Asperger-Syndrom, High Functioning Autismus oder Atypischer Autismus wurden in einem querschnittlichen Design mithilfe der deutschen Version des WHOQOL-BREF, einem Fragebogenverfahren zur Erfassung der gbLQ, untersucht.
Ergebnisse: Der durchschnittliche Wert im WHOQOL-BREF betrug 60,6 (SD ±26,1). Die mittleren Werte in den WHOQOL-BREF-Subskalen waren 70,1 (SD ±19,1) für die Domaine „Körperliche Gesundheit“, 61,5 (SD ±21,9) für die Domaine „Psychische Gesundheit“, 53,8 (SD ±23,5) für die Domaine „Soziale Beziehungen“ und 67,9 (SD ±17,4) für die Domaine „Umwelt“. Verglichen mit Gesunden lagen die Ergebnisse der von uns untersuchten Population in drei von vier WHOQOL-BREF-Subskalen signifikant niedriger. Im Vergleich zu Patienten mit Schizophrenie-Spektrum-Störung (SSS) war die gbLQ der von uns untersuchten Population in fast allen Domänen (Ausnahme: Domäne „Soziale Beziehungen“) besser. Es zeigte sich eine signifikante Assoziation zwischen gbLQ und der Domäne „Lebenspraktische Fertigkeiten“, jedoch nicht mit Alter, IQ oder den Summenwerten im ADOS-G.
Fazit: Die gbLQ von Patienten mit hoch funktionalem ASS scheint niedriger als die gesunder Menschen, jedoch besser als die von an SSS Erkrankten zu sein. Vor dem Hintergrund der Assoziation von guten lebenspraktischen Fertigkeiten und besserer gbLQ sollten erstere bei der Entwicklung von Therapieprogrammen berücksichtigt werden, da sie anscheinend für das Mass an selbstbeurteilter gbLQ von Bedeutung sind.
Background
Autism spectrum disorders (ASD) are complex neurodevelopmental disorders characterized by qualitative impairments in three domains: Social interaction, communication and repetitive, stereotyped behaviour. ASD can have a detrimental impact on the well-being of affected individuals: Studies show an increased prevalence of psychiatric comorbidity such as social anxiety disorder, depression, attention-deficit/hyperactivity disorder (ADHD) and oppositional-defiant disorder (ODD) [1], [2], [3] and there is also data documenting an increased burden upon the families of individuals with ASD [4], [5], [6]. The psychosocial impairment of individuals with ASD is also well-known [7]: Affected persons regularly experience severe difficulties especially in interpersonal relationships and often appear as solitary “cranks”, who tend to choose non-mainstream vocations, combined with frequent change of jobs. Furthermore, recent studies confirm, that as well in people with ASD and good cognitive abilities, their adaptive skills significantly stay behind their cognitive level, thus leading to considerable impairment in everyday life [8].
Over recent years, Health-related quality of life (HRQOL) has increasingly been considered as a relevant endpoint and outcome criterion in evaluating the effects of medical intervention and prevention measures. It resembles a multidimensional construct which includes emotional well-being, interpersonal relations, material well-being (such as financial status, employment and housing), personal development (i.e. education, personal competence and performance), physical well-being (health, activities of daily living and leisure), self-determination, social inclusion and human and legal rights [9]. Beside the individual’s perception (self-reported HRQOL), HRQOL studies also include external (e.g. parents’ or teachers’) perspectives (proxy-reported HRQOL) as well as objective indicators. While some studies on HRQOL in adults with ASD have been published in recent years [10], [11], [12], [13], [14], [15], many of the participants of these studies had severe intellectual disabilities. Only few studies used standardized, cross-culturally evaluated psychometric instruments with self-report versions and there is no study yet concerning a German population.
The psychosocial impairment in individuals with ASD is well established [16], [17], even in persons with good intellectual abilities [18], [19]. Studies in this population which focused on the social outcome (mostly defined by objective factors like educational attainment, independence or employment [20], [21], [22]) have demonstrated heterogenous findings, ranging from good to very poor outcomes [23]. Beyond studies that focus on objective outcomes, studies on the subjective contentment of patients are equally important. In current clinical psychiatric research, the subjective perspective on outcomes is of high relevance in the measurement of quality of life [24], [25]. Also, until now, only little is known about the relationship between potential influencing factors and outcome [26].
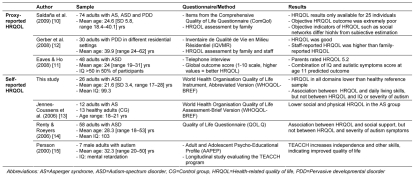
For these reasons, the aim of the present study was to evaluate HRQOL in young German adults with high functioning ASD, using the German version of a well-validated generic self-report HRQOL questionnaire: the World Health Organisation Quality of Life Instrument, Abbreviated Version (WHOQOL-BREF) [27]. Additionally, a possible association between self-reported HRQOL and potential influencing factors like IQ, results in ASD-specific diagnostic tests and adaptive behaviour was analysed. The rationale for this was the hypothesis that e.g. a higher IQ and better adaptive behaviour might lead to better social relationships and better coping with ASD-caused limitations, thus positively influencing HRQOL. In respect to the results of previous studies (see Table 1 (Tab. 1)), we hypothesized that – in comparison to healthy controls – self-reported HRQOL in individuals with high-functioning ASD is lower, especially in the domain of “social relationships”. Furthermore, it was hypothesized that HRQOL in individuals with ASD was impaired comparable to individuals with severe psychiatric disorders like schizophrenia.
Table 1. Review of HRQOL studies in individuals with ASD.
In respect to the relatively small sample size we examined the relationship between HRQOL and influencing factors in an exploratory data analysis.
Methods
Participants
For this cross-sectional study, we contacted 46 adolescents and young adults with the diagnosis of either Asperger Syndrome (AS), high functioning autism (HFA) or atypical autism (AA) (all male, mean age: 21.2 years) by mail during June 2008. Twenty-six individuals participated in the study (mean age 21.6, range 17–28 years). All patients had been extensively diagnosed at the outpatient clinic of our institution (department of child and adolescent psychiatry, tertiary referral centre for ASD) in the previous seven years.
The diagnostic classification was made according to the standardized criteria of the International Classification of Diseases, 10th revision (ICD-10) and comprised diagnostic categories F84.0, F84.1 and F84.5. The expression of autistic symptoms was assessed by the German version of the Autism Diagnostic Observation Scale-Generic (ADOS-G) [28] and a semi-structured ASD-specific parent interview (German version of the Autism Diagnostic Interview-Revised (ADI-R) [29]. The ADOS-G is a semi-structured, standardized assessment of communication, social interaction, play, and imagination designed for use in diagnostic evaluation of individuals with a suspected diagnosis of ASD. The ADOS-G encompasses four modules with different activities to observe behaviour in participants of particular developmental and language levels: ranging from those without expressive language to verbally fluent, from profound mental retardation to cognitively high-functioning children and adults. Activities are designed to provide planned opportunities to elicit autistic behaviors. The ADOS-G has shown an inter-rater reliability of 0.84 and both a sensitivity and specifity of 0.95. In this study, only modules 3 and 4 were used. The ADOS-G was administered by an examined clinician (IKB) who had completed research training and met standard requirements for research reliability [30]. Comorbidity was diagnosed by the attending psychologist/physician according to the ICD-10 criteria using the German version of the diagnostic interview of psychiatric disorders for children (Kinder-DIPS) [31]. The Kinder-DIPS is a structured interview that enables both lifetime and current diagnoses of externalizing behavior disorders, elimination disorders, depressive disorders, anxiety disorders, phobias, OCD, eating disorders, specific learning disabilities according to DSM-III-R/ICD-10. The interview is available both as a parent/proxy version and as a self-report version. Kappa coefficients are between 0.60 and 0.82 and Y-coefficients range from 0.74 and 0.94, while re-test reliability (Cohen’s Kappa) lies between 0.50 and 0.89. Until now, the Kinder-DIPS has not been employed in studies in children with ASD. In this study, the Kinder-DIPS was used to make lifetime diagnoses. Additionally, in one patient the clinical diagnosis of Tourette’s syndrome was made according to ICD-10 diagnostic criteria.
The adaptive behaviour was assessed by the Vineland Adaptive Behavior Scales (VABS) [32]. This is a 297-item interview-based tool assessing adaptive behaviour in three domains: communication (receptive, expressive and written), daily living skills (personal, domestic and community), and socialisation (interpersonal relations, play and leisure time and coping skills). The VABS is sensitive to the severity of impairment in ASD [7], [8], [33]. For intellectual testing, the respective age-appropriate German version of the Wechsler Intelligence Scales was applied [34], [35].
Materials
The World Health Organisation Quality of Life Instrument, Abbreviated Version (WHOQOL-BREF) has been designed for the assessment of subjectively perceived HRQOL in adults with physical or mental disorders and in healthy adults. The instrument can be used for research or for quality assurance in outpatient, day-care or inpatient care settings. The WHOQOL-BREF is only available as a self-report version. HRQOL is evaluated in the following domains: “Physical health” (e.g. physical pain, medical treatment), “psychological health” (e.g. negative feelings, ability to concentrate), “social relationships” (e.g. social support, personal relationships) and “environment” (e.g. access to health services, transport). WHOQOL-BREF results are expressed on the following scores: an overall score (range 0–100, with higher numbers indicating better HRQOL) and domain scores (range 0–100; with higher numbers indicating better HRQOL). For the German version of the WHOQOL-BREF, age-specific values from a reference sample (n=2055) are available for an age range from 18 to 85 years. Worldwide field studies and clinical studies have shown that the questionnaire differentiates very well between individuals with and without impaired health and between individuals with physical and mental health problems (e.g. schizophrenia, depression). The internal consistency (Cronbach‘s Alpha) for the WHOQOL-BREF subscales ranges from α=0.57 to α=0.88 [27].
For the exploratory analysis of the influencing factor “severity of autistic symptoms”, the ADOS data from modules 3 and 4 were taken together (“emphatic or emotional gestures”, “communication of own affect” and “responsibility” were omitted, because they are included in module 4 only). A sum score of all ADOS-items (not only algorithm items) was then calculated.
Procedure
A copy of the German version of the WHOQOL-BREF questionnaire, a sociodemographic data form and an informed consent form were sent to the patients by mail, accompanied by a letter explaining the purpose of the study.
Individuals willing to participate in the study sent back the completed questionnaires and forms to our clinic. The study was approved by the Institutional Review Board. Patients gave written informed consent for study participation.
Statistics
For statistical calculation, the Statistical Package for Social Sciences Version 17.0 (SPSS Inc., Chicago, IL, USA) was used. The tests were carried out using a significance level of 0.05 and two-tailed tests. Overall scores and domain scores for the WHOQOL-BREF were calculated according to the WHOQOL-BREF manual [27]. Differences between the means of the ASD sample and the healthy individuals/SSD reference sample were calculated using t-tests for independent samples. To estimate which variables predict HRQOL best, Pearson’s correlation coefficient and a linear regression analysis with backward selection were calculated, complemented by Durbin-Watson testing. The WHOQOL-BREF summary score and the domain scores were used as dependent variable, while the full scale IQ, severity of autistic symptoms (ADOS-G summary score) and the adaptive behaviour (VBAS) were used as predictor variables.
Results
Study sample
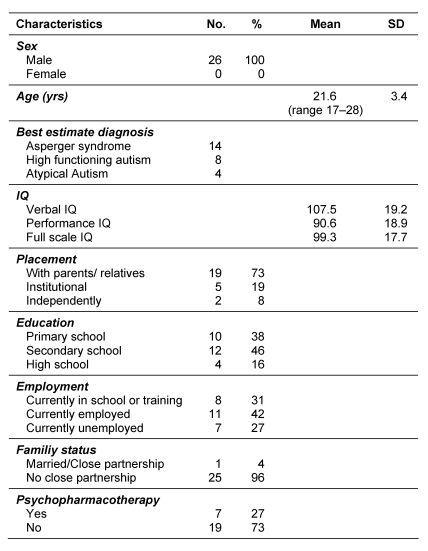
Of 46 individuals contacted by mail, 26 individuals participated in our study and sent back the WHOQOL-BREF questionnaires and the socio-demographic data form (e.g. placement, education, family status). The response rate was 57% (26/46). The group of non-participants had the following diagnoses: AS (n=10), HFA (n=8) and AA (n=2). There were no statistically significant differences between the participating and non-participating groups concerning age (p=0.759), IQ (p=0.310) or severity of autistic symptoms (p=0.770). Table 2 (Tab. 2) displays the sample characteristics.
Table 2. Sample characteristics.
Patients had been diagnosed with the following lifetime psychiatric comorbidities: Obsessive-compulsive disorder (n=7; 26.9%), depression (n=2; 7.7%), dysthymia (n=1; 3.8%), enuresis (n=2; 7.7%), attention-deficit/hyperactivity disorder (n=2; 7.7%), specific phobia (n=2; 7.7%), oppositional-defiant disorder (n=1; 3.8%) and Tourette’s syndrome (n=1; 3.8%). Seven patients (26.9%) received psychopharmacotherapy (substances: risperidone, olanzapine, methylphenidate, duloxetine).
WHOQOL-BREF
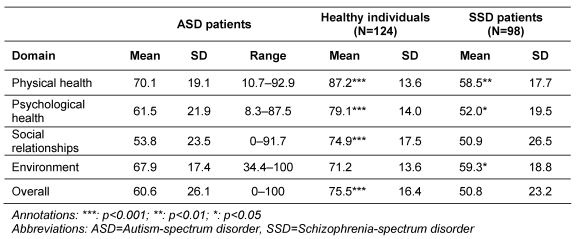
The WHOQOL-BREF results for our sample are displayed in Table 3 (Tab. 3).
Table 3. WHOQOL-BREF results (overall score and domain scores) of our sample in comparison with reference samples of healthy individuals and SSD patients.
The highest HRQOL score was reached in the domain “physical health”, followed by the domains “environment” and “psychologial health”. The lowest HRQOL score was found in the “social relationships” domain. When comparing the WHOQOL-BREF scores of our sample to a reference population of healthy individuals (male, age: 18–25 years) [27], the scores of the ASD patients were significantly (all p<0.001) lower in the domains “physical health”, “psychological health”, “social relationships” and in the overall score (Table 3 (Tab. 3)).
In comparison with a WHOQOL-BREF reference population with schizophrenia-spectrum disorders (SSD) [27], ASD patients rated their HRQOL significantly better in the “physical health”, “psychological health” and “environment” domain. In the “social relationships” domain, there was no significant difference in WHOQOL-BREF scores between both groups. As demonstrated in Table 3 (Tab. 3), the domain “social relationships” is the most impaired WHOQOL-BREF domain in our sample.
Concerning potential influencing factors, there was no significant association between WHOQOL-BREF overall scores and full scale IQ (r=0.087, p=0.680), ADOS-G summary score (r=0.175, p=0.403), and VABS total score (r=0.372, p=0.080). A significant association was found between the VABS domain “daily living skills” and the WHOQOL-BREF scales “physical health” (r=0.434, p=0.039), “psychological health” (r=0.452, p=0.030) and WHQQOL-BREF sum score (r=0.515, p=0.012).
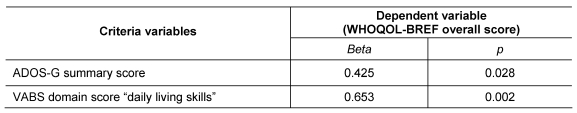
A linear regression analysis with stepwise backward selection, including ADOS-G summary score, VABS domains and full scale IQ, attained significant explanation (F=7.444, p=0.004) and accounted for a sufficient amount of explained variance (R²=0.427, adjusted R²=0.369). Table 4 (Tab. 4) presents the final model, in which only two of the five influence factors are included. The overall HRQOL score was best predicted by the VABS domain “daily living skills” (p=0.002) in combination with the amount of autistic symptoms (ADOS-G sum-score) (p=0.028).
Table 4. Results of the linear regression analysis.
In the final model with these two independent variables (VABS domain “daily living skills”, ADOS-G sum-score), we found tolerances of 0.89 for both variables, thus excluding colinearity. Durbin-Watson testing was used to rule out autocorrelation (d=1.8).
No significant difference in overall HRQOL was found between participants which received psychopharmacotherapy (n=7) and those who did not (n=19) (p=0.900).
Discussion
The main finding of our study can be summarized as follows: Compared with young healthy adults, the HRQOL of adolescents and young adults with ASD appears to be lower. This result is in line with one of the few studies that include individuals with high-functioning autism [13]. In contrast, another comparable study found satisfying levels of HRQOL in a sample of 58 adults with high-functioning autism [14]. Albeit, they detected an association between HRQOL and social support that could not be replicated in our study.
Generally, the comparison of our results with other studies (Table 1 (Tab. 1)) is hampered by the small number of studies on HRQOL in young adults with ASD. Moreover, there are considerable differences in patient population (e.g. diagnoses, mean age, age range, IQ, setting), design, treatment, HRQOL assessment (proxy vs. self-report) and outcome measures, which make a comparison difficult.
The study best comparable to ours is the report of Jennes-Coussens et al. [13], who used the WHOQOL-BREF to evaluate young adults with Asperger syndrome and found lower HRQOL in the domains „social relationships“ and „physical health“, compared with healthy controls. Our findings are in line with theirs, but additionally show impairment for the domain „psychological health“ and the overall score. The detriment of the „social relationships“ domain reflects a core symptom of ASD, the qualitative impairment in social interaction. The impaired scores in the ”psychological health” domain, which encompasses items like negative emotions or the capacity to enjoy life, may reflect our sample’s comorbid psychiatric disorders (e.g. depression). Rather unexpected are the low scores on the „physical health“ domain, as physical impairment is no key component of ASD. Here, it can be hypothesized, that the item composition of this domain, including items like „How satisfied are you with your ability to perform your daily living activities?“ or „How satisfied are you with your capacity for work?“ reflects not only physical health, but also the ability to participate in everyday life – which is certainly reduced in ASD patients [8].
When comparing our results with those of HRQOL studies in children with ASD, there are some similarities: Individuals with ASD seem to have lower HRQOL than healthy controls [36], [37]. In comparison with other psychiatric disorders, results are inconsistent: While Lee et al. found HRQOL in children with ADHD to be better than in those with ASD [36], Kamp-Becker et al. [37] found better HRQOL in children with ASD when compared to a sample of inpatient and outpatient children with Axis-I-psychiatric disorders [38].
Unfortunately, a direct comparison of HRQOL in children with ASD with HRQOL in young adults with ASD is not feasible, as there are no questionnaires which span the age range from childhood to adulthood. Therefore, it can only be speculated upon the relationship between those age groups in terms of HRQOL. On the one hand, it can be hypothesized that HRQOL in adults with ASD is lower than in children with ASD, as parental support decreases and impaired social skills (in contrast to healthy peers) might be perceived more intensively than in childhood. On the other hand, it can be assumed that – especially in well-fostered children – the fruits of social skills and behaviour training programs may be harvested in adulthood and thus lead to better HRQOL.
In the context of self-reported HRQOL, it has to be discussed how precise ratings are, as there may be a potentially limited ability of individuals with ASD to rate their HRQOL adequately: Several studies indicate a profound deficit in self representation in children and adolescents with ASD [39], [40], [41]. These impairments affect the identification of emotional states in other people as well as self-referential cognition [40], [42]. This lack of theory of mind might be an explanation for the discrepant results of self-report and proxy versions, as demonstrated by Johnson et al., who found youths with ASD to report significantly fewer autistic traits and more empathic features than their parents attributed to them [43].
However, while literature on this topic is still scarce, there are some hints that ASD patients have sufficient ability to rate their emotions appropriately. Hobson et al. argue, that the disability of self-reflection only concerns certain domains, e.g. children were found to be impaired in recognition and expression of embarrassment or shame, but were able to describe their own experiences of pride and (more rarely) guilt [44].
Finally, we did not find a significant association between IQ or ADOS-G scores and patients’ HRQOL. The possible reasons for these findings – which are in line with those of Renty and Royers [14] – also point to some limitations of this report: The number of participants may have been too small for the detection of small and medium effects. Nevertheless, we found a significant correlation between HRQOL and the VABS domain “daily living skills”. This finding is of importance for therapeutic programmes and implies that – next to the autistic symptomatology – the daily living skills are of high relevance. The resulting autonomy in everyday life may be an important factor for adults with high functioning ASD in respect to physical and psychological well-being.
There was no significant difference in HRQOL between individuals with and without psychopharmacotherapy. It can be hypothesized that especially patients with distinct psychiatric symptoms (negatively influencing HRQOL) have been prescribed medication. Under successful psychopharmacotherapy, symptoms should have improved, thus raising their HRQOL to a level equally to those who are not in need of medication.
Concerning the sample composition, there might have been a higher proportion of individuals with positively estimated HRQOL in the response sample, despite sociodemographic equivalence in comparison to the baseline sample.
ADI-R, ADOS-G and IQ data had been collected previous to this HRQOL study. As reports on stability of those data in the course of time are heterogenous [23], [45], these data might not have reflected patients’ current condition with highest precision and therefore might have caused imprecision in the calculations. Nevertheless, good daily living skills (as measured in the VABS) showed a predictive value for superior HRQOL in ASD patients.
Another possible limitation of our study lies in the psychiatric comorbidities in our sample, which may have influenced patients’ HRQOL assessment. Then again, given the high rate of psychiatric comorbidity, our study population just represents the reality of psychopathology in ASD patients [1], [46].
Considering the clinical usefulness of HRQOL assessment in ASD patients, a main purpose could be longitudinal HRQOL measurement as a means to evaluate the effectiveness of therapeutic interventions. Additionally, high patient-reported HRQOL might help to explain lacking motivation for therapeutic interventions, as those patients do not feel the need to improve their (subjectively felt) satisfying condition [43].
Concerning future research directions in the field of HRQOL in patients with ASD, studies with larger samples, longitudinal design and more specifically designed psychometric instruments are required to evaluate HRQOL in this population comprehensively.
Conclusions
In our study, HRQOL in adolescents and young adults with ASD was lower than in healthy individuals and better than in patients with SSD. Also, higher HRQOL was associated with better daily living skills. This interrelationship should especially be accounted for in the design and application of treatment programmes for individuals with ASD, as it is of importance for the level of self-perceived HRQOL.
Notes
Conflicts of interest
None declared.
References
- 1.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. Available from: http://dx.doi.org/10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 2.Kanne SM, Christ SE, Reiersen AM. Psychiatric symptoms and psychosocial difficulties in young adults with autistic traits. J Autism Dev Disord. 2009;39(6):827–833. doi: 10.1007/s10803-008-0688-x. Available from: http://dx.doi.org/10.1007/s10803-008-0688-x. [DOI] [PubMed] [Google Scholar]
- 3.Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, Tager-Flusberg H, Lainhart JE. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Dev Disord. 2006;36(7):849–861. doi: 10.1007/s10803-006-0123-0. Available from: http://dx.doi.org/10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- 4.Mugno D, Ruta L, D'Arrigo VG, Mazzone L. Impairment of quality of life in parents of children and adolescents with pervasive developmental disorder. Health Qual Life Outcomes. 2007;5:22. doi: 10.1186/1477-7525-5-22. Available from: http://dx.doi.org/10.1186/1477-7525-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magaña S, Smith MJ. Psychological distress and well-being of Latina and non-Latina White mothers of youth and adults with an autism spectrum disorder: cultural attitudes towards coresidence status. Am J Orthopsychiatry. 2006;76(3):346–357. doi: 10.1037/0002-9432.76.3.346. Available from: http://dx.doi.org/10.1037/0002-9432.76.3.346. [DOI] [PubMed] [Google Scholar]
- 6.Allik H, Larsson JO, Smedje H. Health-related quality of life in parents of school-age children with Asperger Syndrome or High-Functioning Autism. Health Qual Life Outcomes. 2006;4:1. doi: 10.1186/1477-7525-4-1. Available from: http://dx.doi.org/10.1186/1477-7525-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klin A, Saulnier CA, Sparrow SS, Cicchetti DV, Volkmar F, Lord C. Social and communication abilities and disabilities in higher functioning individuals with Autism Spectrum Disorders: The Vineland and the ADOS. J Autism Dev Disord. 2007;37(4):748–759. doi: 10.1007/s10803-006-0229-4. Available from: http://dx.doi.org/10.1007/s10803-006-0229-4. [DOI] [PubMed] [Google Scholar]
- 8.Saulnier CA, Klin A. Social and Communication Abilities and Disabilities in Higher Functioning Individuals with Autism and Asperger Syndrome. J Autism Dev Disord. 2007;37(4):788–793. doi: 10.1007/s10803-006-0288-6. Available from: http://dx.doi.org/10.1007/s10803-006-0288-6. [DOI] [PubMed] [Google Scholar]
- 9.Schalock RL. The Concept of Quality of Life: What We Know and Do Not Know. J Intellect Disabil Res. 2004;48(Pt3):203–216. doi: 10.1111/j.1365-2788.2003.00558.x. Available from: http://dx.doi.org/10.1111/j.1365-2788.2003.00558.x. [DOI] [PubMed] [Google Scholar]
- 10.Saldaña D, Álvarez RM, Lobatón S, Lopez AM, Moreno M, Rojano M. Objective and subjective quality of life in adults with autism spectrum disorders in southern Spain. Autism. 2009;13(3):303–316. doi: 10.1177/1362361309103792. Available from: http://dx.doi.org/10.1177/1362361309103792. [DOI] [PubMed] [Google Scholar]
- 11.Eaves LC, Ho HH. Young adult outcome of autism spectrum disorders. J Autism Dev Disord. 2008;38(4):739–747. doi: 10.1007/s10803-007-0441-x. Available from: http://dx.doi.org/10.1007/s10803-007-0441-x. [DOI] [PubMed] [Google Scholar]
- 12.Gerber F, Baud M, Giroud M, Galli Carminati G. Quality of life of adults with pervasive developmental disorders and intellectual disabilities. J Autism Dev Disord. 2008;38(9):1654–1665. doi: 10.1007/s10803-008-0547-9. Available from: http://dx.doi.org/10.1007/s10803-008-0547-9. [DOI] [PubMed] [Google Scholar]
- 13.Jennes-Coussens M, Magill-Evans J, Koning C. The quality of life of young men with Asperger syndrome: a brief report. Autism. 2006;10(4):403–414. doi: 10.1177/1362361306064432. Available from: http://dx.doi.org/10.1177/1362361306064432. [DOI] [PubMed] [Google Scholar]
- 14.Renty JO, Roeyers H. Quality of life in high-functioning adults with autism spectrum disorder: The predictive value of disability and support characteristics. Autism. 2006;10(5):511–524. doi: 10.1177/1362361306066604. Available from: http://dx.doi.org/10.1177/1362361306066604. [DOI] [PubMed] [Google Scholar]
- 15.Persson B. A longitudinal study of quality of life and independence among adult men with autism. J Autism Dev Disord. 2000;30(1):61–66. doi: 10.1023/A:1005464128544. Available from: http://dx.doi.org/10.1023/A:1005464128544. [DOI] [PubMed] [Google Scholar]
- 16.Billstedt E, Gillberg IC, Gillberg C. Autism in adults: symptom patterns and early childhood predictors. Use of the DISCO in a community sample followed from childhood. J Child Psychol Psychiatry. 2007;48(11):1102–1110. doi: 10.1111/j.1469-7610.2007.01774.x. Available from: http://dx.doi.org/10.1111/j.1469-7610.2007.01774.x. [DOI] [PubMed] [Google Scholar]
- 17.Howlin P. Outcome in high-functioning adults with autism with and without early language delays: Implication for the differentiation between autism and Asperger syndrome. J Autism Dev Disord. 2003;33(1):3–13. doi: 10.1023/A:1022270118899. Available from: http://dx.doi.org/10.1023/A:1022270118899. [DOI] [PubMed] [Google Scholar]
- 18.Sturm H, Fernell E, Gillberg C. Autism spectrum disorders in children with normal intellectual levels: associated impairments and subgroups. Dev Med Child Neurol. 2004;46(7):444–447. doi: 10.1111/j.1469-8749.2004.tb00503.x. Available from: http://dx.doi.org/10.1111/j.1469-8749.2004.tb00503.x. [DOI] [PubMed] [Google Scholar]
- 19.Tantam D, Girgis S. Recognition and treatment of Asperger syndrome in the community. Br Med Bull. 2009;89(1):41–62. doi: 10.1093/bmb/ldp006. Available from: http://dx.doi.org/10.1093/bmb/ldp006. [DOI] [PubMed] [Google Scholar]
- 20.Billstedt E, Gillberg IC, Gillberg C. Autism after adolescence: population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. J Autism Dev Disord. 2005;35(3):351–360. doi: 10.1007/s10803-005-3302-5. Available from: http://dx.doi.org/10.1007/s10803-005-3302-5. [DOI] [PubMed] [Google Scholar]
- 21.Howlin P, Alcock J, Burkin C. An 8 year follow-up of a specialist supported employment service for high-ability adults with autism or Asperger syndrome. Autism. 2005;9(5):533–549. doi: 10.1177/1362361305057871. Available from: http://dx.doi.org/10.1177/1362361305057871. [DOI] [PubMed] [Google Scholar]
- 22.Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. J Child Psychol Psychiatry. 2004;45(2):212–229. doi: 10.1111/j.1469-7610.2004.00215.x. Available from: http://dx.doi.org/10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- 23.Cederlund M, Hagberg B, Billstedt E, Gillberg IC, Gillberg C. Asperger syndrome and autism: a comparative longitudinal follow-up study more than 5 years after original diagnosis. J Autism Dev Disord. 2008;38(1):72–85. doi: 10.1007/s10803-007-0364-6. Available from: http://dx.doi.org/10.1007/s10803-007-0364-6. [DOI] [PubMed] [Google Scholar]
- 24.Haynes RB, Sackett DL, Guyatt GH, Tugwell P. Clinical Epidemiology. How to Do Clinical Practice Research. Philadelphia: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 25.Prince PN, Prince CR. Subjective quality of life in the evaluation of programs for people with serious and persistent mental illness. Clin Psychol Rev. 2001;21(7):1005–1036. doi: 10.1016/S0272-7358(00)00079-9. Available from: http://dx.doi.org/10.1016/S0272-7358(00)00079-9. [DOI] [PubMed] [Google Scholar]
- 26.Kamp-Becker I, Ghahreman M, Smidt J, Remschmidt H. Dimensional structure of the autism phenotype: relations between early development and current presentation. J Autism Dev Disord. 2009;39(4):557–571. doi: 10.1007/s10803-008-0656-5. Available from: http://dx.doi.org/10.1007/s10803-008-0656-5. [DOI] [PubMed] [Google Scholar]
- 27.Angermeyer MC, Kilian R, Matschinger H. WHOQOL-100 und WHOQOL-BREF. Handbuch für die deutschsprachigen Versionen der WHO-Instrumente zur internationalen Erfassung von Lebensqualität. Göttingen: Hogrefe; 2000. [Google Scholar]
- 28.Rühl D, Bölte S, Feineis-Matthews S, Poustka F. Diagnostische Beobachtungsskala für Autistische Störungen (ADOS) Bern: Huber; 2004. [DOI] [PubMed] [Google Scholar]
- 29.Rühl D, Schmötzer G, Thies G, Poustka F. Autismus Diagnostisches Interview - Revision (ADI-R) Frankfurt: J. W. Goethe-Universität, Klinik für Psychiatrie und Psychotherapie des Kindes- und Jugendalters; 1995. [Google Scholar]
- 30.Lord C, Rutter M, Goode S, Heemsbergen J, Jordan H, Mawhood L, Schopler E. Autism Diagnostic Observation Schedule: A standardized observation of communicative and social behavior. J Autism Dev Disord. 1989;19(2):185–212. doi: 10.1007/BF02211841. Available from: http://dx.doi.org/10.1007/BF02211841. [DOI] [PubMed] [Google Scholar]
- 31.Unnewehr S, Schneider S, Margraf J, editors. Diagnostisches Interview bei psychischen Störungen im Kindes- und Jugendalter (Kinder-DIPS) Berlin: Springer; 1995. [DOI] [PubMed] [Google Scholar]
- 32.Sparrow SS, Balla DA, Cicchetti DV. Vineland Adaptive Behavior Scales. Circle Pines, MN: American Guidance Service; 1984. [Google Scholar]
- 33.Carter AS, Volkmar FR, Sparrow SS, Wang JJ, Lord C, Dawson G, Fombonne E, Loveland K, Mesibov G, Schopler E. The Vineland Adaptive Behavior Scales: supplementary norms for individuals with autism. J Autism Dev Disord. 1998;28(4):287–302. doi: 10.1023/A:1026056518470. Available from: http://dx.doi.org/10.1023/A:1026056518470. [DOI] [PubMed] [Google Scholar]
- 34.Tewes U, Rossmann P, Schallberger U, editors. Hamburg-Wechsler-Intelligenztest für Kinder - Dritte Version, HAWIK-III. Bern: Huber; 1999. [Google Scholar]
- 35.Tewes U. HAWIE-R. Hamburg-Wechsler Intelligenztest für Erwachsene. Revision 1991. Bern: Huber; 1994. [Google Scholar]
- 36.Lee LC, Harrington RA, Louie BB, Newschaffer CJ. Children with autism: quality of life and parental concerns. J Autism Dev Disord. 2008;38(6):1147–1160. doi: 10.1007/s10803-007-0491-0. Available from: http://dx.doi.org/10.1007/s10803-007-0491-0. [DOI] [PubMed] [Google Scholar]
- 37.Kamp-Becker I, Schröder J, Muehlan H, Remschmidt H, Bachmann C. Health-related quality of life in children with autism spectrum disorder. Z Kinder Jugendpsychiatr Psychother. doi: 10.1024/1422-4917/a000098. [DOI] [PubMed] [Google Scholar]
- 38.Mattejat F, König U, Barchewitz C, Felbel D, Herpertz-Dahlmann B, Höhne D, Janthur B, Jungmann J, Katzenski B, Kircher J, Naumann A, Nökel P, Schaff C, Schulz E, Warnke A, Wienand F, Remschmidt H. Zur Lebensqualität von psychisch kranken Kindern und ihren Eltern. Ergebnisse der ersten multizentrischen Studie mit der Elternversion des Inventares zur Erfassung der Lebensqualität bei Kindern und Jugendlichen (ILK) Kindh Entwickl. 2005;14(1):39–47. doi: 10.1026/0942-5403.14.1.39. Available from: http://dx.doi.org/10.1026/0942-5403.14.1.39. [DOI] [Google Scholar]
- 39.Baron-Cohen S. Theory of mind and autism: a fifteen year review. In: Baron-Cohen S, Tager-Flusberg H, Cohen DJ, editors. Understanding other minds. Oxford: Oxford University Press; 2000. [Google Scholar]
- 40.Lombardo MV, Barnes JL, Wheelwright SJ, Baron-Cohen S. Self-referential cognition and empathy in autism. PLoS ONE. 2007;2(9):e883. doi: 10.1371/journal.pone.0000883. Available from: http://dx.doi.org/10.1371/journal.pone.0000883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lombardo MV, Chakrabarti B, Bullmore ET, Sadek SA, Pasco G, Wheelwright SJ, Suckling J, Consortium MA, Baron-Cohen S. Atypical neural self-representation in autism. Brain. 2010;133(Pt 2):611–624. doi: 10.1093/brain/awp306. Available from: http://dx.doi.org/10.1093/brain/awp306. [DOI] [PubMed] [Google Scholar]
- 42.Decety J, Jackson PL. The functional architecture of human empathy. Behav Cogn Neurosci Rev. 2004;3(2):71–100. doi: 10.1177/1534582304267187. Available from: http://dx.doi.org/10.1177/1534582304267187. [DOI] [PubMed] [Google Scholar]
- 43.Johnson SA, Filliter JH, Murphy RR. Discrepancies Between Self- and Parent-Perceptions of Autistic Traits and Empathy in High Functioning Children and Adolescents on the Autism Spectrum. J Autism Dev Disord. 2009;39(12):1706–1714. doi: 10.1007/s10803-009-0809-1. Available from: http://dx.doi.org/10.1007/s10803-009-0809-1. [DOI] [PubMed] [Google Scholar]
- 44.Hobson PR, Chidambi G, Lee A, Meyer J. Foundations for self-awareness: An exploration through autism. Monogr Soc Res Child Dev. 2006;71(2):vii–166. doi: 10.1111/j.1540-5834.2006.00387.x. [DOI] [PubMed] [Google Scholar]
- 45.Moss J, Magiati I, Charman T, Howlin P. Stability of the autism diagnostic interview-revised from pre-school to elementary school age in children with autism spectrum disorders. J Autism Dev Disord. 2008;38(6):1081–1091. doi: 10.1007/s10803-007-0487-9. Available from: http://dx.doi.org/10.1007/s10803-007-0487-9. [DOI] [PubMed] [Google Scholar]
- 46.Gillberg C, Billstedt E. Autism and Asperger syndrome: coexistence with other clinical disorders. Acta Psychiatr Scand. 2000;102(5):321–330. doi: 10.1034/j.1600-0447.2000.102005321.x. Available from: http://dx.doi.org/10.1034/j.1600-0447.2000.102005321.x. [DOI] [PubMed] [Google Scholar]