Abstract
Individual change and variation in emotional and behavioral disturbance in children and adolescents with intellectual disability has received little empirical investigation. Based on the Australian Child to Adult Development study, we report associations among individual differences in level, rate of change, and occasion-specific variation across subscales of the Developmental Behavior Checklist in a sample (n=506) aged 5–19 years. Correlations among the five DBC subscales ranged from .43 to .66 for level, .43 to .88 for rate of change, and .31 to .61 for occasion-specific variation, with the highest correlations observed consistently between Disruptive, Self-Absorbed, and Communication Disturbance behaviors. These interdependencies among dimensions of emotional and behavioral disturbance provide insight into the developmental dynamics of psychopathology from childhood through young adulthood.
Keywords: Intellectual Disability, Longitudinal, Change, Emotional Disturbance, Behavioral Disturbance
Introduction
Using checklists of behavior and emotional problems, substantially elevated levels of psychopathology have been reported in studies of children and adolescents with ID (for example, Dekker, Koot, van der Ende, & Verhulst, 2002; Einfeld et al., 2006; Linna et al., 1999; Richardson & Koller, 1996; Wallander, Dekker, & Koot, 2003). Studies of psychiatric diagnoses in children and adolescents with ID have also reported elevated rates of DSM and ICD diagnoses, and significant comorbidity (Dekker & Koot, 2003; Emerson, 2003). Whilst little research has addressed the issue of comorbidity, still less has considered associations among longitudinal change in psychopathology symptoms in children and adolescents with ID.
A British population study of 264 5–15 year olds with ID found that 16% had two or more ICD-10 (World Health Organization, 1992) diagnoses, and 3% had three or more diagnoses (Emerson, 2003). The children with an ID were 14 times more likely than their typically developing peers to have two diagnoses and 9.4 times more likely to have three diagnoses. n a sample of 474 individuals with ID (7–20 years of age), multiple DSM-IV (American Psychiatric Association, 1994) disorders were reported in 14.2% of the sample (Dekker & Koot, 2003). Of those who had a diagnosis, 36.8% met diagnostic criteria for more than one disorder. Seven percent of the total sample had coexisting anxiety and disruptive diagnoses, 0.4% had comorbid anxiety and mood disorders, 0.8% had a comorbid mood and disruptive disorder, and 2.3% met criteria for a diagnosis in each of these groupings. Almost four percent of the total sample had a comorbid diagnosis within the same major diagnostic grouping. Of the children with Attention Deficit Hyperactivity Disorder (ADHD), 44% also met criteria for Oppositional Defiant Disorder (ODD), whilst 79.5% of the sample with a mood disorder also met criteria for another DSM-IV disorder, most commonly a disruptive disorder.
More information is available on community populations of typically developing children and adolescents. In non-intellectually disabled children and adolescents who have one psychiatric diagnosis, rates of comorbidity (two or more psychiatric diagnoses) of around 30–40% have been reported (Costello et al., 1996; Fergusson, Horwood, & Lynskey, 1993; Newman et al., 1996). Significant relationships have been reported between conduct / oppositional disorders and ADHD, anxiety / mood disorders, and substance use disorders (Costello et al., 1996; Fergusson et al., 1993). Other associations include anxiety and mood disorders, anxiety / mood disorders and substance use, and mood disorders and ADHD (Costello et al., 1996; Fergusson et al., 1993). In terms of gender differences, results have been mixed, with reports of either higher rates of comorbidity in boys (Costello et al., 1996; Fergusson et al., 1993) or no gender differences (Newman et al., 1996). Sex differences in patterns of comorbidity have been observed, with depression and conduct disorder co-occurring in girls but not boys, and comorbid depression and substance use disorder in boys but not girls (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003).
Very little research has been undertaken on longitudinal change in patterns of symptomatology. One study examined psychopathology as described by the Child Behavior Checklist (Achenbach, 1991) for a population of typically developing Dutch children aged 4–11 years. Patterns and relationships between types of psychopathology were examined over a 6 year period. Cross-sectionally, results indicated positive associations between all of the subscales of the CBCL, with the strongest correlations between those subscales that describe related behaviors (e.g. Aggressive and Delinquent Behavior). There were also significant associations between the Anxious/Depressed subscale and the Aggressive Behavior scale, Aggressive Behavior and Attention Problems, Aggressive Behavior and Anxious/Depressed, and between both Attention Problems and Aggressive Behavior and Social Problems.
In terms of change over time, Aggressive Behavior at the initiation of a study was significantly associated with Anxious/Depressed, Social Problems, Attention Problems, and Delinquent Behavior at follow-up six years later (Verhulst & Vanderende, 1993). Significant correlations of scores across time (.27 and above) were also found between Withdrawn and Anxious/Depressed scales, Anxious/Depressed and Somatic Complaints, Anxious/Depressed and Aggressive Behavior, Social Problems and Anxious/Depressed, Social Problems and Aggressive Behavior, Social Problems and Attention Problems, Attention Problems and Aggressive Behavior/Delinquent Behavior, and Delinquent Behavior and Aggressive Behavior. Prinzie, Onghena, and Hellinckx (2006) report positive associations between individual trajectories of CBCL aggressive and delinquent problem behavior over a three-year period in boys and girls four to seven years of age, with a stronger association found for boys.
In previous work we found that four of the five Developmental Behavior Checklist (DBC) subscales show slight improvement, on average, through childhood and adolescence in a population of intellectually disabled children and adolescents whereas Social Relating problems were found to increase, on average (Einfeld et al., 2006). However, this work did not examine the extent to which these reductions in psychopathology tend to occur in the same individuals, or whether different individuals are improving in different areas. Knowledge of the relationships between individual trajectories on the five subscales would provide further insight into the developmental dynamics of psychopathology from childhood through young adulthood. For example, are individual differences in the rate of change of Social Relating behaviors correlated positively with change in Self-Absorbed behaviors? That is, do children who tend to worsen more than average in social-relating also tend to improve less than average in self-absorbed behaviors? Comparing mean trajectories is uninformative and potentially misleading with respect to inference about individual change, as means can go up (or down) together over time without this same pattern applying to particular individuals. The resolution of this issue has important theoretical and practical ramifications, as it would clarify the nature of psychopathology in this population – whether improvements in individual children typically involve isolated or general behavioral issues.
In this paper, we extend the univariate and group average findings of the Einfeld et al. (2006) paper to a multivariate individual differences emphasis to address the question of whether individual-level changes across dimensions of psychopathology are correlated. The Australian Child to Adult Development (ACAD) study, a 14-year (four occasions) Australian epidemiological longitudinal study in young people with ID, permits rigorous evaluation of the course and pattern of emotional and behavioral problems. The central outcomes include subscales of the Developmental Behavior Checklist (Einfeld & Tonge, 1992, 1995, 2002) indicating Disruptive/Antisocial, Self-Absorbed, Communication Disturbance, Anxiety, and Social Relating behaviors, shown with example items in Table 1.
Table 1.
Developmental Behavior Checklist (DBC) Subscales and Sample Items
| Subscale | Sample items |
|---|---|
| Anxiety (A) |
|
| Communication Disturbance (CD) |
|
| Disruptive (D) |
|
| Self-Absorbed (SA) |
|
| Social Relating (SR) |
|
Multivariate growth curve models provide estimates of covariation among individual differences in initial status (i.e., level), rates of linear change, and systematic occasion-specific deviations (i.e., within-person correlation). The growth curve model essentially summarizes each person’s data in terms of a regression line, with estimates of each individual’s intercept, slope, and occasion-specific residual used as the outcomes in simultaneous analyses. In this case, we have an intercept, slope and residual for each person on each of the DBC subscales, and have evaluated the degree to which these “characteristics” are related. Correlations among the initial levels (i.e., intercepts) indicate similarity in the relative ordering of individuals at their initial time point across outcomes (i.e., relations among individual differences in initial status). Correlations among the slopes indicate the extent to which individual differences in linear change in one outcome are related to individual differences in linear change in another (i.e., correlated change). These correlations are in the time frame of the span of 4 waves, and thus are analogous to slow change in individual traits. Within-person correlations among occasion-specific residuals, often neglected in the modeling of associations between trajectories, provide information regarding state-like, occasion-specific fluctuation in emotional and behavior disturbance after controlling for an individual’s trait-like growth trajectories. Whereas the correlation between slopes taps the association of long term trends, the correlation of residuals captures the extent to which short term departures from the trend occur together. Within-person variation could result from factors such as transient changes in the child (e.g., illness) or exogenous causes such as life events or external stressers (e.g., Sliwinski, Smyth, Hofer, & Stawski, 2006).
We also evaluate whether a common factor model provides a sufficiently good fit to the structure of covariation among levels, slopes, and residuals. This evaluation goes further than evaluating the degree of interdependence of the five subscales of the DBC in providing a formal test of whether these patterns of covariation are consistent with common factor models of psychopathology.
Method
Sample
The ACAD study epidemiological cohort (n=578) was recruited in 1991 from every health, education, and family agency that provided services to children with ID of all levels, aged 4–19 years at the first wave, whose families lived in 6 census districts of the states of New South Wales and Victoria, Australia. These areas were selected as representative of the Australian population in terms of social class, ethnicity, and urban/rural distribution (Einfeld & Tonge, 1996a). Of those invited to participate in the study, 80.2% of those with an IQ less than 50 agreed to participate, and 78.5% of those with an IQ above 50. For those with moderate, severe, and profound ID, the ascertainment process is likely to be virtually complete. The population of 4–18 year olds in the census area was 172,000 which equates to a prevalence rate in this cohort of 3.04 per 1000 comparable to a prevalence of 2.94 per 1000 in 5 to 9 year olds suggested by Quinn (1986). The recruitment procedure was likely to locate almost all children with moderate and more severe ID but only captures those with mild ID who receive services. As in other studies, some young people with the mildest forms of ID blend in to the normal population and were not identified because they may not have impairments in adaptive behavior that require services. Individuals in the cohort with mild ID may therefore be biased towards higher levels of disturbance. A selection of non- participants were contacted by telephone and asked the last question in the DBC regarding if their child had any major or minor problems with their emotions or behavior (Einfeld & Tonge, 1996b). There was no difference between the participants and non-participants on this question. The major reason for non-participation was an inability to contact or locate the carers presumably because they had moved. Full detail about recruitment and participant demographics are provided in Tonge & Einfeld (2003).
The mean age of the entire epidemiological cohort at Wave 1 was 12.1 years (SD = 4.4), at Wave 2 was 16.5 (SD = 4.5), at Wave 3 was 19.5 (SD = 4.5) and at Wave 4 was 23.5 (SD = 4.5). Participation has been consistently high throughout the study. The response rate (excluding the 31 participants who have died since Wave 1) was 82.5% at Wave 2 (n = 477), 78.5% (n = 448) at Wave 3 and 84% (n = 438) at Wave 4. Analyses were limited to individuals aged 5–19.5 years at the first wave (n = 506) because of the few individuals in the extreme range of sample ages. This analysis sample was comprised of 288 males and 218 females. In terms of intellectual disability, 165 were classified with mild ID (95 males, 70 females), 206 with moderate ID (112 males, 94 females), and 135 with severe/profound ID (81 males, 54 females).
Measures
Developmental Behavior Checklist (DBC)
The DBC-P (Einfeld & Tonge, 1992, 1995, 2002) is the primary measure of psychopathology for young people with ID aged 4–18 years. It is a 96-item instrument completed by parents or other primary caregivers (Primary Care Version: DBC-P) reporting problems with emotions or behavior over the previous six month period. For the purposes of this longitudinal analysis, the DBC was scored according to the factor-analytically derived subscales allowing for a description of 5 dimensions of disturbance (see Table 1): Disruptive/Antisocial (D; e.g., manipulates, abusive, tantrums, hits), Self-Absorbed (SA; e.g., eats non-food, preoccupied with trivial items, hums, grunts), Communication Disturbance (CD; e.g., echolalia, perseveration, talks to self), Anxiety (A; e.g., separation anxiety, distressed if alone, phobias, cries easily), and Social Relating (SR; e.g., doesn’t show affection, resists cuddling, aloof, doesn’t respond to other’s feelings). Evidence for content, criterion, construct, and concurrent validity has been demonstrated for the sub-scales (Einfeld & Tonge, 1992, 1995). The original psychometric validation of the DBC-P was established using the wave 1 cohort (Einfeld & Tonge, 1995). Subsequent studies and reviews have confirmed sound psychometric properties (Dekker, Nunn & Koot, 2002; Hastings et al., 2001, Lecavalier & Aman, 2005). All analyses were based on raw total scores for each DBC subscale.
The Developmental Behavior Checklist for Adults (Mohr, 2003; Mohr, Tonge, & Einfeld, 2005) (DBC-A) is a 107-item caregiver-completed checklist adapted from the DBC-P that includes 12 new items added with a few other minor modifications. The DBC-A (adult version), designed for individuals over age 19, was developed after Wave 3 and implemented in Wave 4. Therefore, all individuals over 19 years of age were assessed with the DBC-P through Wave 3. Mohr, Tonge, & Einfeld (2005) report test -retest reliability of 0.75 and 0.85 for paid carers and family carers, respectively, and inter-rater reliability (family carers) of 0.72. Additionally, concurrent validity coefficients of the DBC-A with the Aberrant Behavior Checklist (Aman et al., 1985) and the PAS-ADD (Moss et al., 1998) are 0.63 and 0.61, respectively. For purposes of analysis across all four waves of assessment, the DBC-A was scored in the same manner and, for consistency, using the same items as the DBC-P.
Degree of Intellectual Disability
Children were categorized as having a mild, moderate, or severe/profound degree of ID. Categorization was based upon the results of IQ assessments (typically one of the Wechsler measures, as determined by the child’s chronological age, or the Stanford-Binet) according to the ranges of ID specified by the DSM-IV (American Psychiatric Association, 1994). Specifically, the IQ cutoffs used were 50–55 to 70 (mild ID), 35–40 to 50–55 (moderate ID), below 35 (severe to profound ID), dependent upon the standard deviation of the measure used. Assignment to categories was based upon the results of existing assessments as provided by parents/carers. In the absence of a current cognitive or developmental assessment, assessment was undertaken by one of the study psychologists.
Procedure
The ACAD study gathers data on a broad range of potential biopsychosocial risk and protective variables including the receipt of mental health services (Einfeld & Tonge, 1995). Data collection has taken place at four time points: Wave 1 (1991–1992), Wave 2 (1995–1996), Wave 3 (1999), and Wave 4 (2002–2003) through a mail survey of a questionnaire booklet to the parents and caregivers of the young people with ID. Of the 506 participants, 60% lived at home and were rated by their mothers (67% including any family respondent). Only 14% of children lived in care situations outside the home. Of these, 74% were rated by a professional carer. The remaining children were either rated by family while living at an unknown location (16%), rated by a professional carer while living at an unknown location (<2%) or had missing data on both rater and living arrangement variables. Few individuals who entered the study while living at home transitioned subsequently to a care (n=24) or independent (n=16) situations. In 71% of transitions to care, rating was subsequently done by a professional carer.
Statistical Analysis
Multivariate growth curve modeling was used to estimate the associations among individual differences in change in distinct features of psychopathology. In longitudinal designs, time is nested within person, and methods such as growth curve models (a specific case of mixed or random effects models) are a means of properly addressing the corresponding within-person correlations (see Willett, Singer, & Martin, 1998 for application in psychopathology research). Conceptually, these models involve estimating the regression of the outcome of interest (i.e., DBC subscales) on time for each individual (often labeled “Level 1”) and predicting the regression parameters of these within-person trajectories (i.e., each participant’s level and slope) with between-person covariates (“Level 2”). The model summarizes individual DBC values at each occasion of measurement in terms of “true” initial level of disturbance (intercept), slope (rate of change), and occasion-specific residual variance parameters. It is useful to think of this residual as a mix of random error and systematic state-like short-term fluctuation around the model-implied trajectory. Within each growth curve, residuals have an expectation of zero at any particular occasion. Correlations would be expected if individual differences in two or more psychopathology scales exhibited related systematic patterns of fluctuation at each occasion.
Models of correlated age-conditional slopes at the between-person level are typically based on smoothed (e.g., linear) individual model-implied trajectories over time, with the time-to-time dynamics usually considered unmodeled residual error components. The latent growth metric used here is time-in-study, with age at baseline used as a level-2 (between-person) predictor to account for the initial age heterogeneity in the sample. The analysis of coupled change is based on the recognition of the state-like component of these residuals, and attention to covariation among the state portions of two or more growth curves. This provides information regarding the systematic occasion-specific fluctuation across different types of psychopathology indicated by the DBC subscales. For parsimony, the state-residuals are assumed to have equal variance across occasions (i.e., they are estimated as a single model parameter) and to be uncorrelated over time within each outcome. However, the between outcome covariances of these occasion-specific residuals are estimated and interpreted as lower-bounds of the degree to which state fluctuations are “coupled” within individuals as these residuals are composed of both systematic and error variance.
The associations of level, slope, and occasion-specific residuals for each pair of growth curves form ordinary covariance matrices that may in turn yeild additional information about developmental processes. A matrix of level covariances can be formed, a matrix of slope covariances can be formed, and a matrix of occasion-specific residuals can be formed. Factor analysis of these covariance matrices can help reveal the extent to which common underlying causes may be responsible for the estimated correlations and couplings (e.g., does a common cause account for model estimated levels?, … for model estimates rates of change?, … for the state-like time specific fluctuations?)
Simultaneous multivariate models of all five DBC subscales were fitted using Mplus v5.0 (Muthén & Muthén, 1998–2008) based on a time-in-study data structure with individually-varying intervals between occasions of measurement. Maximum likelihood estimation was used to accommodate incomplete data (missing values; attrition) and provide unbiased population estimates under the assumption that the data are “missing at random” (i.e., missingness is accounted for by covariates and prior values in a longitudinal study; see Little & Rubin 1987). The intercept (i.e., level) was specified to be at the first occasion of measurement for each individual, with both the level and linear slope conditional on age at the Wave 1 baseline. The participant’s age was centered relative to the mean Wave 1 age (M = 12.0, SD = 3.9), permitting interpretation of this between person effect to reflect the average age of the sample. Follow up occurred an average of 4.5, 7.5, and 11.5 years later for Waves 2, 3, and 4, respectively. Time-in-study was used as the metric of change in order to obtain separate estimates of the between-person (cross-sectional) and within-person (longitudinal) effects of age, respectively represented on level-2 by centered age at Wave 1 and on level-1 by time since Wave 1. Other level-2 predictors included sex (with boys as the reference) and ID (mild, moderate, or severe, with mild ID as the reference). For each bivariate growth curve model, the occasion-specific residual variances and covariances were constrained to equality, with one estimate for the residual parameter of each outcome and a single covariance parameter between occasion-specific residual variances. As standardized estimates (i.e, correlations) are not provided by the Mplus software when individually-varying time intervals are modeled, these correlations were computed based on the estimated variances and covariances for each of the parameters of interest.
We report results from a reduced (minimally conditioned) model that conditions time-in-study change only on age at baseline and contrast these results to those from a fully conditoned model that included on age, sex, ID status and all two-way interactions as predictors of the growth parameters. The degree to which the associations among rates of change are accounted for by these additional level-2 predictors, provides a basis for understanding the influence of gender and intellectual deficit characteristics on correlated and coupled change processes. Subsequently, secondary analyses of the estimated variances and covariances were undertaken to evaluate whether the covariation among initial status, linear rates of change, and occasion-specific residuals could be accounted for by common factor models.
Results
We first examined the shape of the subscale trajectories and the extent to which trajectory parameters varied between individuals. A model including only fixed effects for linear and quadratic components of time was compared to a mixed model with the same fixed effects of time but in which an additional random-effect allowed the linear fixed-effect of time to vary over individuals. The difference in the deviance statistics (−2 log likelihood) between these two models was significant for each outcome, indicating that individual differences in the rate of change (in addition to the level) was significant for all of the outcomes. The quadratic fixed-effect of time was not significant, so it was not retained; change was therefore modeled as a straight line with a fixed (group averaged) and random (individual) component. The linear model provided a good fit to each DBC subscale and polynomial models did not improve model fit.
Table 2 provides the coefficients and standard errors for each DBC subscale based on the multivariate model with level and slope conditional on baseline age. Between-person differences in age predicted behavior problem level for Anxiety, Self-Absorbed and Social Relating, with older individuals showing worse problems on Social Relating, but fewer problems on Anxiety or Self-Absorbed. A statistically significant change over time (linear slope growth factor) was observed for all subscales. All scales except Social Relating indicated decreasing problem behaviors over time. Age also predicted rate of change for all subscales except Disruptive, with older individuals showing more rapid decline in Communication Disturbance, slower decline in Anxiety and Self-Absorbed behaviors, and slower increases in Social Relating problems.
Table 2.
Fixed and Random Effects Estimates and Standard Errors for Developmental Behavior Checklist (DBC) Subscales for the Time-Based Model Conditional on Age
|
DBC Subscales |
|||||
|---|---|---|---|---|---|
| A | CD | D | SA | SR | |
| Fixed Effects | |||||
| Level | |||||
| Estimate | 4.090* (0.136) | 5.774* (0.191) | 13.485* (0.426) | 14.201* (0.452) | 4.494* (0.148) |
| Age (12) | −0.078* (0.036) | 0.003 (0.047) | −0.023 (0.107) | −0.396* (0.111) | 0.116* (0.037) |
| Rate of Change | |||||
| Estimate | −0.062* (0.015) | −0.054* (0.020) | −0.270* (0.038) | −0.315* (0.036) | 0.057* (0.016) |
| Age (12) | 0.008* (0.004) | −0.013* (0.005) | 0.005 (0.010) | 0.023* (0.009) | −0.009* (0.004) |
| Variance Components | |||||
| Level Variance | 6.270* (.685) | 13.487* (1.254) | 74.427* (6.153) | 86.609* (7.112) | 7.276* (0.804) |
| Slope Variance | 0.039* (0.009) | 0.071* (0.016) | 0.309* (0.054) | 0.268* (0.052) | 0.033* (0.009) |
| Residual Variance | 3.799* (0.280) | 6.220* (0.439) | 21.524* (1.669) | 20.730* (1.667) | 4.655* (0.344) |
Note. Standard errors are shown in parentheses.
p < 0.01. A: anxiety, CD: communication disturbance, D: disruptive/antisocial, SA: self absorbed, and SR: social relating. For details of full model in univariate analysis, see Einfeld et al. (2006).
Correlations between subscale levels, slopes and residuals derived from the models including the predictors age, sex, and ID status were very similar to those from the age-conditional model (correlations differed by < .02). Accordingly, results for the age-only models are presented. Table 3 shows the correlations among levels, slopes, and occasion-specific residuals for the age conditional growth model estimates. Correlations ranged from .43 to .66 for initial levels, from .43 to .88 for slopes, and .31 to .61 for within-person residuals. The highest correlations were consistently between Disruptive, Self-Absorbed, and Communication Disturbance behaviours. All covariance estimates from which the correlations were derived were significant at the p < .05 level.
Table 3.
Random Effects Correlation Estimates for Developmental Behavior (DBC) Checklist Subscales
| DBC Subscales | Subscale Correlations: Conditional on Age and Age/Sex/IQ | |||||
|---|---|---|---|---|---|---|
| Level | Slope | Occasion-Specific Residual | ||||
| Age Only | Age/Sex/IQ | Age Only | Age/Sex/IQ | Age Only | Age/Sex/IQ | |
| A with… | ||||||
| CD | 0.50 | 0.49 | 0.53 | 0.52 | 0.39 | 0.39 |
| D | 0.50 | 0.48 | 0.47 | 0.44 | 0.42 | 0.42 |
| SA | 0.37 | 0.47 | 0.46 | 0.43 | 0.38 | 0.38 |
| SR | 0.46 | 0.50 | 0.39 | 0.44 | 0.31 | 0.31 |
| CD with… | ||||||
| D | 0.60 | 0.57 | 0.80 | 0.81 | 0.50 | 0.50 |
| SA | 0.46 | 0.64 | 0.85 | 0.83 | 0.52 | 0.52 |
| SR | 0.42 | 0.52 | 0.56 | 0.57 | 0.40 | 0.40 |
| D with… | ||||||
| SA | 0.42 | 0.62 | 0.87 | 0.88 | 0.61 | 0.61 |
| SR | 0.34 | 0.43 | 0.57 | 0.62 | 0.39 | 0.39 |
| SA with… | ||||||
| SR | 0.67 | 0.66 | 0.56 | 0.57 | 0.45 | 0.46 |
Note. All associations are statistically significant at the p < .01 level. D: disruptive/antisocial (e.g., manipulates, abusive, tantrums, hits), SA: self absorbed (e.g., eats non-food, preoccupied with trivial items, hums, grunts), CD: communication disturbance (e.g., echolalia, perseveration, talks to self), A: anxiety (e.g., separation anxiety, distressed if alone, phobias, cries easily), and SR: social relating (e.g., doesn’t show affection, resists cuddling, aloof, doesn’t respond to other’s feelings).
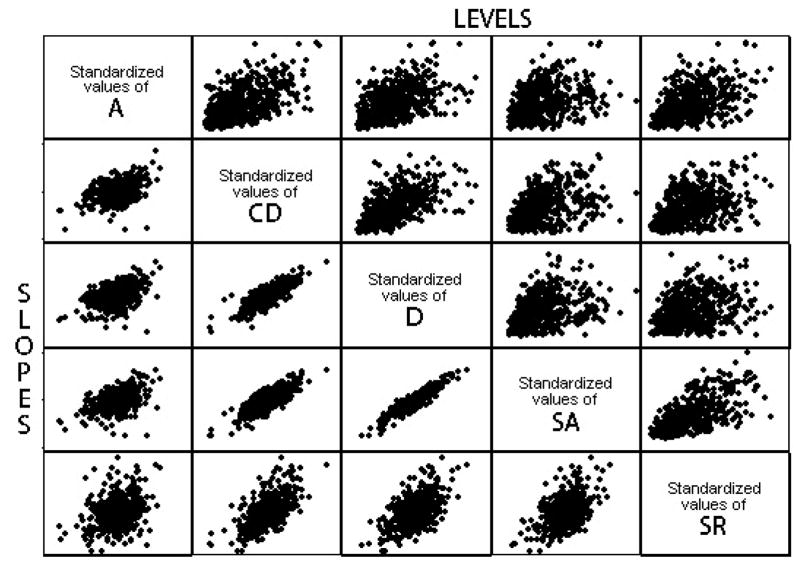
Correlations among the Levels (i.e., expected intercepts at age 12) are similar to what might be obtained by age-adjusted correlation between scales in a cross-sectional study. In a longitudinal model, however, these levels are based on the linear model for the individual repeated measures and provide more reliable estimates given the correction for occasion-specific variability. The strongest correlations were between Self-Absorbed and Social Relating, and between Communication Disorder and Disruptive, followed by Anxiety and Communication Disorder, Anxiety and Disruptive, and Anxiety and Social Relating. Scatterplots of the expected level-level associations (based on factor scores output from the longitudinal model) are shown in the upper triangle of Figure 1. Each scatterplot shown in the upper triangle graphically illustrates one of the correlations of levels reported in Table 3. For example the highest correlation, level of SA with level of SR (r=.67), show the tightest elongated scatter cloud. It can also be seen that the level-level scatterplots show a wider scatter at higher levels indicating that a substantial proportion of individuals can be high on one subscale, but not on the other. For example, it is not uncommon for a child to have very high levels of Disruptive behavior, but only moderate levels of Self-Absorbed behavior (cell 3, 4). In contrast, improvements in disruptive behavior over time are almost universally paired with improvements in Self-absorbed behavior (cell 4, 3).
Figure 1.
Scatterplots for level-level and slope-slope correlations across DBC subscales.
The slope-slope correlations represent the extent to which within-person trajectories of different types of problem behaviors are related between-persons. The strongest correlations were between Disruptive, Self-Absorbed, and Communication Disturbance. Figure 1 (lower triangle) is a graphical representation of these correlations, with most individuals who change substantially on one sub-scale also exhibiting change on the other. For example, the highest correlation, slope of D with slope of SA (r = .87), shows the tightest elongated scatter cloud, while the weakest slope correlation, A with SR (r = .39), shows the most diffuse scatter cloud.
The occasion-specific residual correlations represent the extent to which perturbations in an individual’s trajectory at particular occasions are related across outcomes after controlling for individual change. The estimates are moderate across most of the scales and provide evidence for systematic occasion-specific fluctuation in emotional and behavioral disturbance. In particular, occasion-specific variation in Disruptive, Communication Disturbance, and Self-Absorbed showed the strongest occasion-level correlations.
An evaluation of whether single common factor models could sufficiently account for the pattern of correlations among levels, slopes, and occasion-specific residuals was undertaken in a second stage analysis of the estimated correlations (reported in Table 3). Factor loadings, variance explained, and overall model fit statistics (CFI, TLI, and RMSEA) are provided in Table 4 for separate factor analyses of initial level, linear slope, and occasion-specific residuals. Conventional standards (Hu & Bentler, 1999) deem the Tucker-Lewis Index (TLI) >= 0.95 and the root mean squared error of approximation (RMSEA) <= .06 to be indicative of good model fit, although CFI and TLI >= 0.90 and RMSEA <= .10 are often considered adequate model fit.
Table 4.
Factor Loadings and Fit Statistics from Confirmatory Factor Analysis of the Covariance Structure of Intercepts, Slopes, and Occasion-Specific Residuals
| DBC Subscales | Level | Slope | Occasion-Specific Residual | |||
|---|---|---|---|---|---|---|
| Factor Loading | R2 | Factor Loading | R2 | Factor Loading | R2 | |
| A | .62 | .38 | .50 | .25 | .53 | .28 |
| CD | .76 | .57 | .88 | .78 | .67 | .46 |
| D | .71 | .51 | .93 | .87 | .76 | .57 |
| SA | .86 | .74 | .94 | .88 | .79 | .62 |
| SR | .73 | .53 | .64 | .41 | .56 | .32 |
| % variance | 55% | 64% | 45% | |||
| Goodness of Fit Indices | ||||||
| CFI | .96 | .97 | .99 | |||
| TLI | .91 | .94 | .99 | |||
| RMSEA (90% C.I.) | .13 (.10–.17) | .15 (.12–.18) | .04 (.00–.08) | |||
Note. R-square is the proportion of total variance explained in the indicator variable by the common factor. CFI: Comparative Fit Index; TLI: Tucker Lewis Index; RMSEA: Root Mean Square Error of Approximation.
Although loadings were high, and a single factor accounted for a substantial proportion of the variation of initial levels, fit indices lay outside ranges associated with acceptable overall model fit (TLI = .91, RMSEA = .13). This was also the case for the factor analysis of correlations of rates of change among the DBC subscales (TLI = .94; RMSEA = .15). A common factor model did, however, provide a very good fit for the occasion-specific residuals (TLI = .99, RMSEA = .04).
In the case of the occasion-specific residuals (i.e., within-person variation), there were no sources of significant misfit among the observed correlations. While there is certainly evidence for substantial shared covariation among levels and rates of change across the DBC subscales, the fit of these models would not generally be regarded as acceptable and indicates that pairs of subscales correlate more or less strongly than would be implied by a model positing a single latent variable ‘driving’ each of initial status, change and time specific responses. More specifically, the common factor model did not sufficiently account for the correlations among Self-Absorbed and Anxiety, Social Relating and Disruptive, and Social Relating and Self-Absorbed. The sources of model misfit for the common factor model of slopes were Communication Disturbance and Anxiety, Disruptive and Communication Disturbance, Self-Absorbed and Anxiety, Self-Absorbed and Disruptive, Social Relating and Anxiety, and Social Relating and Self-Absorbed. This is an indication of distinct individual differences in manifestations of psychopathology across individuals in both a cross-sectional and longitudinal change context. In summary, while there are significant associations among levels, slopes, and occasion-specific variation, a single underlying factor may not adequately account for the entire pattern of correlations among levels and slopes but does satisfactorily account for the pattern of within-person variation at each occasion.
Discussion
The present study modeled the interdependence of developmental change and variation in psychopathology as assessed by the Developmental Behavior Checklist (Einfeld & Tonge, 1995) within a population of individuals with ID. These multivariate analyses extend the univariate analysis of change reported by Einfeld et al. (2006) by considering the structure of change in psychopathology in terms of correlated levels and rates of change between persons and coupling of temporal dynamics within persons. The central finding of this study is evidence for moderate and systematic interdependencies across distinct aspects of emotional and behavioral disturbance. A better understanding of the dynamics (change and variation) in psychopathology from childhood to young adulthood is one of the major strengths of applying multivariate growth curve methodology to longitudinal data.
This study has adopted a dimensional approach to behavioral and emotional disturbance. An alternative would be a categorical one, either in respect of clinical “caseness” or “non-caseness”, or in respect of a categorical approach to specific psychiatric diagnoses. The disadvantage of the former would be that if many individuals start in the study close to the cutoff, one may see lots of apparent “change” that does not involve notable changes in behavior. In fact this is the case for the ACAD sample and the DBC. The modal DBC score was 42, close to the clinical cutoff of 46. However, if many individuals start far from the cut-off (much higher or lower) then larger real changes may not be noticed at all from the cut-off perspective. Stated another way, using cut-offs focuses the analysis on change in a very specific range of behavior rather than across the entire range. With respect to the measurement of specific diagnoses, this presumes that the reliability and validity of a broad range of potential diagnoses has been well-established in this population. With the possible exception of Autistic Disorder and Stereotypic Self-injury, this is still not the case (see Einfeld and Aman, 1995 for a discussion of this).
On average, the severity of psychopathology in four of the five DBC subscales declined over the course of the study, with the exception of the Social Relating scale. One possible explanation for the increase in Social Relating problems is that these children and youths appear more physically mature over time and are placed into more demanding social settings (e.g., school, day-care, occupational-settings) where the same level of behavioral disturbance may be rated more negatively. Alternatively, the behavior related to most of these items might be self-intensifying, and thus truly increase over time. The actual items and pattern of loadings for the Social Relating construct shows a broad/mixed item set ranging from non-social (e.g., Moves slowly, Underactive, Prefers to do things on his/her own) to behaviors that create social barriers (e.g., Avoids eye contact, Doesn’t respond to other’s feelings, Doesn’t show affection). It is important to consider the meaning of this construct in the developmental context when conceptualizing change in the Social Relating construct (Bontempo et al., 2008). Additionally, the increase in scores on the social relating subscale, when considering the population as a whole, may reflect the emergence of depression as the cohort reaches young adulthood, as a number of the items of this subscale suggest depressive symptoms, e.g., “Appears depressed, downcast or unhappy”. This possibility is the subject of ongoing investigation by us.
The current study found significant correlations between the levels of all of the subscales of the DBC, a finding comparable to earlier work. Correlations between the levels of the DBC subscales can be seen as the underlying dimensional foundation of previous research reporting higher rates of diagnostic comorbidity (Dekker & Koot, 2003; Emerson, 2003). The central focus of this report, however, is on the substantial heterogeneity in developmental change as well as in systematic occasion-specific variation. The multivariate analysis of the dimensions of emotional and behavioral disturbance tapped by the DBC subscales indicated moderate to substantial interdependence in long-term change patterns and moderate associations among occasion-specific fluctuations of psychopathology.
Beyond previous research, the multivariate growth model demonstrates that children who show increases or decreases over time on one subscale tend to exhibit similar changes (relative to other children) on another. Put simply, changes for an individual on one scale of the DBC tend to be mirrored by change in the other subscales. The strongest relationships were consistently between the Disruptive, Self-Absorbed, and Communication Disturbance subscales. The DBC Disruptive subscale is similar to the aggressive-delinquent subscale of the CBCL, being primarily concerned with externalizing behavior problems. The Self-Absorbed subscale describes withdrawn and non-social behaviors, whilst the Communication Disturbance subscale contains a mix of abnormal communication items and social difficulties. The Self-Absorbed and Communication Disturbance subscales both contain elements of non-social behaviors and social difficulties. The behaviors described by these three subscales ‘travel together’ in a substantial and statistically significant way. Changes in Anxiety were the least correlated with the other scales, although even changes on this scale were significantly correlated with the others.
Common factor models were subsequently evaluated to provide evidence for common versus specific patterns of level, change, and occasion-specific residual variation in psychopathology. Whether or not a common factor model provides a fit to the data has more to do with the general pattern (i.e., consistency) of covariation than to the magnitude of correlation among DBC subscales and should not be taken as direct evidence for a common or unitary cause. It was only in the case of factor analysis of the occasion-specific residuals that the pattern of covariation was sufficiently consistent with a common factor model. The fit was marginal for level and rate of change in DBC subscales (i.e., some correlations among subscales that were not sufficiently accounted for by the factor model). The common factor model of residuals provides indirect evidence for consistent “state-like” transient behavioral and emotional disturbances across different features of psychopathology. This common covariation may be also be related to situational changes in a child’s circumstance, such as contextual stressors associated with changes in living conditions or life events, which are not cumulative. This finding is not an artifact of model misspecification as the linear model provided a satisfactory fit to each DBC subscale and polynomial models did not improve fit. Further examination of individual differences in within-person variation, in addition to systematic change over long periods of time, is certainly warranted and would benefit from short-term intensive measurement studies of within-person change and variation in psychopathology.
Our previous reports (Tonge and Einfeld, 2003; Einfeld et al, 2006) identified high levels of behavior disturbance even in the youngest members of the ACAD cohort. One model which may explain these findings is that the vulnerability to psychopathology is caused by the same process that causes developmental delay. We hypothesize that the process is brain impairment, sufficiently widespread to cause both intellectual impairment and wide-ranging behavioral and emotional disturbance. That brain impairment is caused by a multiplicity of factors, chiefly genetic, have been described previously for this cohort (Partington et al, 2000). The early high levels of emotional and behavioral problems, the persistence of these problems even given the relatively small steady decline in degree across all types of disturbance except for social relating behaviors, and the lack of influence of gender on the profile of disturbance, all point to the salience of the underlying organic deficits in brain functioning as the predominant cause of the broad range of types of disturbed behaviors and emotions. The progressive maturation of the brain, despite persistence of congenital or early-acquired impairment might account for an increase in resilience and a steady, though slow, decline in symptoms of anxiety, disruptive and self-absorbed behaviors and communication disturbance. Of course, the changes in psychopathology may reflect the benefits of education, family and community support, or acquisition of social and daily living skills. However, the study was not designed to test the contribution of these, so no comment can be offered in this regard.
The clinical implications of the continuing effects of impaired brain function on cognition, affect regulation, impulse control and social and adoptive behavior are that education, family support and general disability services are needed to address the burden of psychopathology in children with ID. Unless early intervention can be shown to be effective in altering the course of psychopathology as found in this study, then behavioral and mental health interventions will need to extend from early intervention through to young adulthood.
While this study examines changes in the severity of psychopathology over time, we are not currently able to evaluate whether the average decline or individual differences in change in psychopathology is related to particular individual interventions or treatments received. The sample was recruited from every health, education, and family agency that provided services to children with ID of all levels, though especially with respect to moderate, severe, and profound levels of intellectual deficit. While this study did not limit or encourage individual treatments such as use of psychotropic medications or behavioral interventions, less than 10% of the children in this study who had clinically significant levels of psychopathology received mental health services (Einfeld & Tonge, 1996a; 1996b). These findings of moderate interdependency of change in different aspects of behavioral and emotional disturbance are therefore likely to reflect the natural history of psychopathology that is relatively independent of any specific mental health intervention. The results of this paper highlight the links between disruptive behavior problems and withdrawn and non-social behaviors in children and adolescents with intellectual disability. Intervention planning should take this relationship into account, ensuring that treatment programs include elements aimed at assisting young people to develop their social interaction and communication skills and providing opportunities for supported social interaction. Research is needed to investigate this relationship further, with high priorities being examination of the broad impact of targeted treatments for disruptive behavior, and determination of whether subsequent improvements in social and communication behaviors are evident.
Acknowledgments
The Australian Child to Adult Development Study was supported by NHMRC (Australia) 113844 and NIH/NIMH grant MH61809.
References
- Achenbach TM. Manual for the child behavior checklist/4-18 and 1991 profile. Burlington, VT: Dept. of Psychiatry, University of Vermont; 1991. [Google Scholar]
- Aman MG, Singh NN, Stewart AW, Field CJ. The Aberrant Behavior Checklist: A behavior rating scale for the assessment of treatment effects. American Journal of Mental Deficiency. 1985;89:485–491. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Bontempo DE, Hofer SM, Mackinnon A, Piccinin AM, Gray K, Tonge B, et al. Factor structure of the developmental behavior checklist using confirmatory factor analysis of polytomous items. Journal of Applied Measurement. 2008;9(3):265–280. [PubMed] [Google Scholar]
- Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, et al. The Great Smoky Mountains Study of youth: Goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry. 1996;53(12):1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and Development of Psychiatric Disorders in Childhood and Adolescence. Archives of General Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Dekker MC, Nunn R, Koot HM. Psychometric properties of the revised Developmental Behaviour Checklist scales in Dutch children with intellectual disability. Journal of Intellectual Disability Research. 2002;46:61–75. doi: 10.1046/j.1365-2788.2002.00353.x. [DOI] [PubMed] [Google Scholar]
- Dekker MC, Koot HM. DSM-IV Disorders in Children With Borderline to Moderate Intellectual Disability. I: Prevalence and Impact. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(8):915–922. doi: 10.1097/01.CHI.0000046892.27264.1A. [DOI] [PubMed] [Google Scholar]
- Dekker MC, Koot HM, van der Ende J, Verhulst FC. Emotional and behavioral problems in children and adolescents with and without intellectual disability. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2002;43(8):1087–1098. doi: 10.1111/1469-7610.00235. [DOI] [PubMed] [Google Scholar]
- Einfeld SL, Aman M. Issues in the Taxonomy of Psychopathology in Mental Retardation. Journal of Autism & Developmental Disorders. 1995;25:143–167. doi: 10.1007/BF02178501. [DOI] [PubMed] [Google Scholar]
- Einfeld SL, Piccinin AM, Mackinnon A, Hofer SM, Taffe J, Gray KM, et al. Psychopathology in young people with intellectual disability. Journal of the American Medical Association. 2006;296(16):1981–1989. doi: 10.1001/jama.296.16.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Einfeld SL, Tonge BJ. Manual for the Developmental Behaviour Checklist Primary Carer Version (DBC-P) School of Psychiatry, University of NSW, and Center for Developmental Psychiatry, Monash University; 1992. [Google Scholar]
- Einfeld SL, Tonge BJ. The Developmental Behavior Checklist: The development and validation of an instrument to assess behavioral and emotional disturbance in children and adolescents with mental retardation. Journal of Autism and Developmental Disorders. 1995;25(2):81–104. doi: 10.1007/BF02178498. [DOI] [PubMed] [Google Scholar]
- Einfeld SL, Tonge BJ. Population prevalence of psychopathology in children and adolescents with intellectual disability: I. Rationale and methods. J Intellect Disabil Research. 1996a;40:91–98. doi: 10.1046/j.1365-2788.1996.767767.x. [DOI] [PubMed] [Google Scholar]
- Einfeld SL, Tonge BJ. Population prevalence of psychopathology in children and adolescents with intellectual disability: II. Epidemiological findings. J Intellect Disabil Research. 1996b;40:99–109. doi: 10.1046/j.1365-2788.1996.768768.x. [DOI] [PubMed] [Google Scholar]
- Einfeld SL, Tonge BJ. Manual for the Developmental Behaviour Checklist: Primary Carer Version and Teacher Version. 2. University of New South Wales and Monash University Centre for Developmental Psychiatry; 2002. [Google Scholar]
- Emerson E. Prevalence of psychiatric disorders in children and adolescents with and without intellectual disability. Journal of Intellectual Disability Research. 2003;47(1):51–58. doi: 10.1046/j.1365-2788.2003.00464.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Lynskey MT. Prevalence and comorbidity of DSM-III--R diagnoses in a birth cohort of 15 year olds. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(6):1127–1134. doi: 10.1097/00004583-199311000-00004. [DOI] [PubMed] [Google Scholar]
- Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Lecavalier L, Aman MG. Rating instruments. In: Matson JL, Matson ML, editors. Behavior modification for persons with developmental disabilities: Empirically supported treatments. Vol. 1. Kingston, NY: National Association for the Dually Diagnosed Press; 2005. pp. 160–189. [Google Scholar]
- Linna SL, Moilanen I, Ebeling H, Piha J, Kumpulainen K, Tamminen T, et al. Psychiatric symptoms in children with intellectual disability. European Child & Adolescent Psychiatry. 1999;8(4):77–82. doi: 10.1007/pl00010704. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- Mohr C. Unpublished Unpublished Doctoral thesis. Monash University; Victoria, Australia: 2003. Behavioural and emotional problems in adults with intellectual disability: The Developmental Behaviour Checklist for adults. [Google Scholar]
- Mohr C, Tonge BJ, Einfeld SL. The development of a new measure for the assessment of psychopathology in adults with intellectual disability. Journal of Intellectual Disability Research. 2005;49(7):469–480. doi: 10.1111/j.1365-2788.2005.00701.x. [DOI] [PubMed] [Google Scholar]
- Moss S, Prosser H, Costello H, Simpson N, Patel P, Rowe S, et al. Reliability and validity of the PAS-ADD Checklist for detecting psychiatric disorders in adults with intellectual disability. Journal of Intellectual Disability Research. 1998;42:173–183. doi: 10.1046/j.1365-2788.1998.00116.x. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK. MPlus User's Guide. 4. Los Angeles: Muthén & Muthén; 1998–2008. [Google Scholar]
- Muthén BO, Muthén LK. MPlus User's Guide. 4. Los Angeles: Muthén & Muthén; 1998–2008. [Google Scholar]
- Newman DL, Moffitt TE, Caspi A, Magdol L, Silva PA, Stanton WR. Psychiatric disorder in a birth cohort of young adults: Prevalence, comorbidity, clinical significance, and new case incidence from ages 11–21. Journal of Consulting and Clinical Psychology. 1996;64(3):552–562. [PubMed] [Google Scholar]
- Partington M, Turner G, Mowat D, Einfeld S, Tonge B. Genes on the X chromosome are important in the diagnosis of mental retardation. American Journal of Medical Genetics. 2000;92:57–61. doi: 10.1002/(sici)1096-8628(20000501)92:1<57::aid-ajmg10>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Richardson SA, Koller H. Twenty-two years: Causes and consequences of mental retardation. Cambridge, MA, US: Harvard University Press; 1996. [Google Scholar]
- Sliwinski MJ, Smyth JM, Hofer SM, Stawski RS. Intraindividual Coupling of Daily Stress and Cognition. Psychology and Aging. 2006;21(3):545–557. doi: 10.1037/0882-7974.21.3.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonge BJ, Einfeld SL. Psychopathology and Intellectual Disability. The Australian Child to Adult Longitudinal Study. In: Masters Glidden L, editor. International Review of Research in Mental Retardation. Vol. 26. Academic Press; California, USA: 2003. pp. 61–91. [Google Scholar]
- Verhulst FC, Vanderende J. “Comorbidity” in an epidemiological sample: A longitudinal perspective. Journal of Child Psychology and Psychiatry. 1993;34(5):767–783. doi: 10.1111/j.1469-7610.1993.tb01070.x. [DOI] [PubMed] [Google Scholar]
- Wallander JL, Dekker MC, Koot HM. Psychopathology in children and adolescents with intellectual disability: Measurement, prevalence, course, and risk. In: Glidden LM, editor. International review of research in mental retardation. Vol. 26. San Diego: Academic Press; 2003. pp. 93–134. [Google Scholar]
- Willett JB, Singer JD, Martin NC. The design and analysis of longitudinal studies of development and psychopathology in context: Statistical models and methodological recommendations. Development and Psychopathology. 1998;10:395–426. doi: 10.1017/s0954579498001667. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The ICD-10 classification of mental and behavioural disorders : clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. [Google Scholar]