ABSTRACT
INTRODUCTION
While the Chronic Care Model (CCM) has been shown to improve the care of patients with chronic illnesses, primary care physicians have been unprepared in its use, and residencies have encountered challenges in introducing it into the academic environment.
AIM
Our residency program has implemented a diabetes management program modeled on the CCM to evaluate its impact on health outcomes of diabetic patients and educational outcomes of residents.
SETTING
University-affiliated, community-based family medicine residency program.
PROGRAM DESCRIPTION
Six residents, two faculty clinicians, and clinic staff formed a diabetes management team. We redesigned the outpatient experience for diabetic patients by incorporating elements of the CCM: multidisciplinary team care through planned and group visits; creation of a diabetes registry; use of guidelines-based flow sheets; and incorporation of self-management goal-setting. Residents received extensive instruction in diabetes management, quality improvement, and patient self-management.
PROGRAM EVALUATION
We achieved overall improvement in all metabolic and process measures for patients, with the percentage achieving HbA1c, LDL, and BP goals simultaneously increasing from 5.7% to 17.1%. Educational outcomes for residents, as measured by compliance with review of provider performance reports and self-management goal-setting with patients, also significantly improved.
DISCUSSION
Through a learning collaborative experience, residency programs can successfully incorporate chronic care training for residents while addressing gaps in care for patients with diabetes.
KEY WORDS: chronic care model, learning collaborative, diabetes, residency education
INTRODUCTION
Today’s medical system is optimized for the delivery of acute, episodic care by individual physicians, yet the primary burden on the system is from chronic illnesses that are not effectively managed under the current healthcare system. The principal cause of disability and use of health services, with almost half of all Americans afflicted with at least one chronic condition, chronic illness consumes over 70% of healthcare expenditures in the U.S1–4.
The Chronic Care Model (CCM) is a framework for restructuring chronic illness management in six domains with interventions that change the culture and structure of medical practice5–9.
Differing from the traditional 1 room/1 provider/1 patient model, the CCM aims to facilitate productive interactions between “informed and activated patients” and “prepared, proactive practice teams” by focusing on improvement in six key areas: 1) integration of community resources, 2) healthcare organization redesign, 3) patient self-management support, 4) decision support (evidence-based guidelines for providers), 5) delivery system design (multidisciplinary team care through planned visits), and 6) clinical information systems (patient registries, reminder systems, and provider performance feedback).
Despite the CCM’s success for several chronic illnesses, implementation in primary care practices has been minimal10–12. The lack of physician training in chronic illness management is an obstacle13.
Residency programs can address this problem by teaching the skills needed to effectively manage patients with complex chronic illnesses. We describe the development and implementation of our diabetes management program, present clinical and educational outcomes, and provide a qualitative assessment of our learning process.
PROGRAM DESCRIPTION
Program Objective
From 2007-2008 the San Jose-O’Connor Family Medicine Residency Program (SJOFMRP) participated in the California Academic Chronic Care Collaborative (CA-ACCC). Our goal was to redesign our delivery of chronic illness care for diabetic patients by training residents to incorporate specific elements of the CCM into their practice. We used clinical and educational measures to monitor our progress toward achieving meaningful residency redesign. Our clinical objective was to achieve >25% overall improvement for our population of patients with diabetes in HbA1c, LDL, and blood pressure control and to demonstrate a >25% improvement in process measures for these patients. Our educational objective was to teach chronic illness management skills to residents with a focus on self-management support and population management. The project was exempted by the IRB at Stanford University and O’Connor Hospital.
Description of Residency Setting
The SJOFMRP is a 24-resident (then 18-resident) community-based training program at O’Connor Hospital affiliated with Stanford University. The project was implemented in the residency’s outpatient continuity clinic serving a multicultural population of primarily Medicaid patients. Prior to the collaborative, our program had no experience with the CCM or structured quality improvement efforts and did not have a chronic illness curriculum for residents.
Identification of Diabetes Management Team and Patient Population
Spearheading our clinic’s quality improvement efforts was the diabetes management team, consisting of one faculty physician, one behavioral science faculty member/physician assistant, clinic staff, and all six PGY-II residents who also constituted our resident learner population. These team members were all active participants in the learning collaborative. The patients consisted of 105 adult patients with type II diabetes mellitus, who fulfilled the following criteria: ICD-9 code of 250.xx or abnormal HbA1c, and seen by the six resident and two faculty providers within the past year.
Program Activities
Our diabetes management program developed as a result of our involvement in the CA-ACCC and consisted of resident educational activities and quality improvement activities, the culmination of which was the development of a diabetes teaching clinic.
Resident educational activities consisted of two half-day workshops on motivational interviewing and self-management goal-setting, as well as a series of didactic sessions on the CCM, diabetes management, glucometer use, and insulin initiation. A critical component was the monthly individual diabetes performance reports, in which the following thirteen metabolic and process measures were reported for each provider: % of patients with HbA1c < 7%, LDL < 100 mg/dL, & BP < 130/80 mmHg simultaneously; with HbA1c < 7%; with HbA1c > 9%; with LDL<100 mg/dL; with BP < 130/80 mmHg; with urine alb/Cr < 30 mg/g; with documented self-management goal-setting; with documented dilated eye exam within the last year; with documented foot exam within the last year; on ACE/ARB medication; 40 years and older and on statin medication; 30 years and older and on aspirin; and smokers with cessation discussion within the last year. These reports included not only information on individual performance but also a comparison to the previous month’s performance and the overall group’s performance. Discussion of these reports generated ideas for future QI activities and the sharing of best practices. In addition, we evaluated resident performance through direct observation of residents undertaking goal-setting with patients at least twice during the collaborative period.
Quality improvement activities consisted of team attendance at three collaborative-wide learning sessions; monthly team meetings; team participation in QI activities following the plan-do-study-act (PDSA) cycle format; creation and maintenance of an Excel-based diabetes patient registry; development of diabetes flow sheets with embedded evidence-based guidelines; and participation of a community ophthalmologist (Table 1)14–16.
Table 1.
Chronic Care Interventions by Educational and Quality Improvement Emphasis
| Intervention emphasis | ||
|---|---|---|
| CCM component | Educational activities | Quality improvement activities |
| Community linkages | ● Identification of one ophthalmologist to join team | |
| Self-management support | ● Resident workshops for self-management goal (SMG) training and motivational interviewing | ● Use of EMR messaging for SMG follow-up |
| ● Use of SMG form | ||
| Delivery system design | ● Staff involvement in patient outreach | |
| ● Monofilament testing protocol | ||
| ● Monthly team meetings | ||
| ● Expedited rescheduling of patients with missed appointments | ||
| ● Redesign of scheduling system to allow appointments three months into the future | ||
| ● System of identifying collaborative patients and interventions that are due | ||
| Decision support | ● Didactics on diabetes management | ● Creation of resident teaching protocol for insulin and glucometer use |
| ● Creation of patient teaching protocol for insulin and glucometer use | ||
| Clinical information systems | ● Monthly review of provider performance reports | ● Diabetes patient registry |
| ● Diabetes flow sheet with embedded guidelines | ||
| Integration of CCM components | ● Creation of multi-disciplinary diabetes teaching clinic | |
Over the course of the collaborative period, we recognized that creating a more structured format for integrating the CCM could improve not only patient care but also resident teaching. The rationale behind creating a separate teaching clinic was to design a more concentrated learning experience for residents while allowing the piloting of more complex system changes. In addition to residents’ care of diabetic patients in their regular continuity clinic, a twice monthly diabetes teaching clinic was integrated into the clinic in February 2008, incorporating multiple CCM elements such as involvement of a multidisciplinary team; point-of-care use of the diabetes registry and guidelines-based flow sheets; comprehensive care delivered during 30-minute planned visits; group care; and a focus on increasing patient self-management through goal-setting.
Staffed by two faculty and 1-2 residents, the diabetes teaching clinic was initially directed toward higher risk patients, those identified through the registry as having HbA1c > 9% or not having a follow-up appointment in >6 months. After several months, it evolved to include all diabetic patients enrolled in the collaborative and all diabetes management team members. The structure also changed from planned visits only, to a combined format, consisting of a one-hour walk (an outdoor provider-facilitated walk of up to 2 miles during which patients set self-management goals), individual planned visits with a provider, and a drop-in group visit facilitated by 1-2 providers and focusing on diabetes education and patient support in a group setting. Each session was preceded by a pre-clinic huddle during which team members met to plan for each patient and to review any missing parameters. A post-clinic huddle to review patient evaluations, discuss how the session went, and make recommendations for the next session, concluded the morning.
PROGRAM EVALUATION
We conducted pre- and post-collaborative intervention assessments of our diabetes management program, examining outcomes for both residents and patients. Baseline practice data collection occurred in April 2007, implementation of the interventions began in May 2007, and follow-up data on the specified diabetes care indicators were collected on a monthly basis starting in May 2007 and continuing throughout the duration of the collaborative.
We used the Assessing Chronic Illness Care (ACIC) survey to measure the level of CCM implementation17–19. Three team members completed the survey instrument at the beginning of the collaborative and again at its completion. Baseline and follow-up results of the ACIC survey demonstrated that our practice began in the range of what is considered to be basic support for diabetes care and improved to the next level of good support (Table 2).
Table 2.
ACIC Results*
| Baseline (April 2007) | Final (May 2008) | |
|---|---|---|
| Organization of the healthcare delivery system | 3.0 | 7.7 |
| Community linkages | 4.6 | 5.2 |
| Self-management support | 4.5 | 7.3 |
| Decision support | 4.7 | 7.9 |
| Delivery system design | 3.0 | 7.0 |
| Clinical information systems | 2.4 | 8.7 |
| Integration of CCM components | 2.0 | 6.2 |
| Total average | 3.5 | 7.14 |
*Scores fall within four descriptive levels of CCM implementation ranging from “little or none” to a “fully-implemented intervention.” Responses are scaled from 0 to 11, with categories within this defined as follows: 0–2 (little or no support for chronic illness care); 3–5 (basic or intermediate support); 6–8 (good support); and 9–11 (optimal, or full-developed, support)
Educational Outcomes
Educational outcomes and qualitative responses were assessed for five of the original six participating residents, as one resident’s outcomes were not measured due to an extended leave of absence. Our two educational measures were the percentage of residents reviewing provider performance reports and percentage demonstrating self-management support strategies. These increased from 0% to 100% for both measures by the end of the collaborative. Qualitative evaluation of the residents through a focus group and a one-time anonymous survey administered at the end of the collaborative revealed that residents found the use of the registry and team approach to care as the two biggest factors representing a positive change for them (Table 3).
Table 3.
Resident Qualitative Feedback: What has Changed for Residents?
| Quotes from our residents | |
|---|---|
| Clinical tools | |
| ● Registry use for population management | ● “The biggest take-home point for me with this experience is the chronic disease registry which really helps me to manage chronic diseases” |
| ● Planned visit model | ● “Definitely will use a registry, unless an EMR prompts me automatically” |
| ● Ability to track one’s own progress (via diabetes performance reports) | ● “I plan to implement a registry for as many chronic diseases as possible as well as share this at the next residency program I attend” |
| Knowledge acquisition | |
| ● Greater knowledge of current guidelines | ● “More algorithmic approach. It (the approach) is all generally clearer in my head now” |
| Cultural change | |
| ● Combating clinical inertia (more aggressive and goal-directed treatment plans) | ● “PDSA model of change mechanism: No problem is too big to break down into smaller pieces” |
| ● More of a team approach in treating diabetes (all on the same page) | ● “I’ve also enjoyed the patient-centered and team approach way of caring” |
| ● Resident leadership team as physician champions |
Patient Outcomes
At baseline, our patient population was comparable to previously published national averages from the 2002 National Health and Nutrition Examination Survey (NHANES) in terms of HbA1c, LDL, and BP control20.
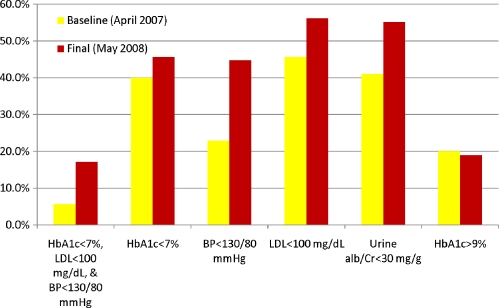
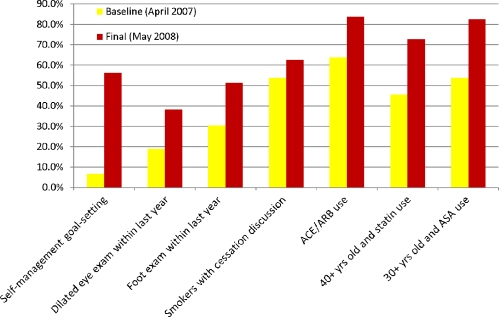
We used a “responder” rate as our primary metabolic outcome measure. Responders were defined as patients who met three parameters simultaneously (HbA1c < 7%, LDL <100, and BP < 130/80). Prior to the intervention, 5.7% of enrolled patients were responders, while post-intervention, 17.1% met the responder criteria. Consistent with this finding, follow-up data showed a trend for improvement in all metabolic measures (Fig. 1). Process measures showed even more improvement, with progress demonstrated for self-management goal-setting, dilated eye exams, foot exams, and medication use (Fig. 2).
Figure 1.
Patient Metabolic Measures: Improvement for all 6 metabolic measures was seen for the collaborative period from April 2007 to May 2008. Yellow bar: Baseline (April 2007). Red bar: Final (May 2008).
Figure 2.
Patient Process Measures: Improvement for all 7 process measures was seen for the collaborative period from April 2007 to May 2008. Yellow bar: Baseline (April 2007). Red bar: Final (May 2008).
DISCUSSION
Numerous barriers make transformation of care difficult in academic settings: clinicians with multiple competing priorities; resident turnover; few incentives to improve care; external regulatory requirements; and loosely organized and autonomous academic sites21,22. Previous studies have shown that physicians adhere to quality indicators for chronic illness care only 50% of the time, suggesting a large gap between optimal and actual physician practice23. Our baseline assessment of diabetes indicators supported this conclusion, as many of our pre-intervention process measures fell below the goals set by the Healthy People 2010 Objectives24.
Our setting had additional obstacles to overcome for full implementation of a CCM model. Continuity of care and timely follow-up were impeded by the economic status of our largely Medicaid-insured patients and our system of allowing them only one month advance appointment scheduling. A second barrier was the implementation of an electronic medical record in November 2007 that changed our workflow and necessitated a redesign of our flow sheet and system of documentation. Lastly, several unanticipated personnel changes disrupted the cohesion of our team, likely a typical issue in many programs.
Despite these barriers, our results confirmed our initial hypotheses that training sites can adapt to allow implementation of the CCM and that such a program for diabetic patients can begin to address gaps in care delivery. We found it considerably easier to improve process, rather than metabolic, measures. By creating a method which enabled providers to systematically perform, document, and track their patients’ ophthalmology referrals and foot exams, we significantly improved our practice’s outcomes for those parameters (19% to 38.1% for eye exams, 30.5% to 51.4% for foot exams, Fig. 2). By enforcing medication reconciliation through the use of point-of-care flow sheets, and subsequently, EMR and registry entry mechanisms, we were able to increase the percentage of our patients who were prescribed recommended medications (63.8% to 83.8% for ACE/ARB use, 45.7% to 72.6% for statin use, and 53.9% to 82.5% for ASA use, Fig. 2). By both integrating self-management goal-setting training into the residents’ educational curriculum and creating a formal structure for teaching and observing resident performance, we found that the percentages of residents and patients doing this activity increased from 0% to 100% and from 6.7% to 56.2%, respectively (Fig. 2). We would expect these process improvements to translate into superior metabolic outcomes with longer follow-up.
Metabolic measures also improved, most notably blood pressure control (22.9% to 44.8%, Fig. 1) and patients achieving HbA1c, LDL, and BP goals simultaneously (5.7% to 17.1%, Fig. 1). This is probably due to providers overcoming “clinical inertia” by taking an active and aggressive approach toward achieving metabolic targets25.
Overall, we identified two interventions that likely had the greatest influence on improving incorporation of the CCM. The first was the development of the diabetes registry, as it enabled patient outreach, guided the structure for the planned visits, aided us in tracking patient goals, and allowed us to create provider reports which formed the basis for many of the team’s PDSA cycles. The second intervention was the development of patient self-management support skills, which enabled both residents and patients to find a different orientation to shared responsibility for improvement.
In addition to these interventions, we found three factors to be critical to our success overall: leadership committed to change, increased involvement of clinic staff, and residents as change agents. Maintaining and implementing the CCM requires passionate ongoing internal advocacy. Secondly, staff involvement in the planning and execution of patient care services contributed to the program’s success. In addition to offering feedback at clinic meetings, staff were trained to deliver new patient education interventions and assist with outreach. Lastly, and most importantly, our residents took on a much larger role than passive recipients of the chronic illness training. Not only did they participate in all stages of planning and implementation of the diabetes clinic, but they also designed QI activities, performed population-based management, and became the physician champions for spreading change to other members of the residency program.
Our findings should be interpreted in light of several limitations. First, the financial and educational support provided through the collaborative enabled us to devote the resources needed to create systematic change in our clinic setting. In addition, our patient sample size was relatively small and we did not have a control group of patients receiving usual care; thus, we cannot be sure that the clinical changes we observed are a result of the redesigned practice.
In summary, the results of our diabetes management program demonstrate that a residency program through learning collaborative experience can successfully incorporate chronic care training for residents while addressing gaps in care for patients with diabetes. By transforming a healthcare delivery system within an academic setting, our model teaches primary care physicians to develop and promote chronic illness care in their future work sites. Given these promising results, a controlled study with a larger sample size and a more diverse patient population would be appropriate and desirable. For our residency program, we have expanded our diabetes teaching clinic to all family medicine residents and their diabetic patients and have added personnel to our diabetes management team. Moreover, the chronic illness curriculum created through our learning collaborative experience is now being taught to all of our residents.
Acknowledgements
This program was funded by Improving Chronic Illness Care and the California Health Care Foundation, in collaboration with the Association of American Medical Colleges. The authors would like to acknowledge the hard work of all of the participants of the OFHC Diabetes Management Team, with special thanks to the following individuals: David McKay, MD, MPH; Robert Norman, MD; Nancy Morioka-Douglas, MD, MPH; Leticia Martinez, RN; Jena Eidschun; David Hiroshima, MD; Tam Nguyen, MD; Rowan Paul, MD; Christie Shen, MD; and Katherine Vega, MD. The authors also thank the faculty of the CA-ACCC, Ed Wagner, MD, MPH; David Stevens, MD; Judith Bowen, MD; and Connie Sixta, RN, PhD, MBA, for their guidance and support, and the representatives of the other participating institutions for their sharing and dissemination of ideas and best practices.
Conflict of Interest None disclosed.
References
- 1.Improving Chronic Illness Care. The Chronic Care Model. Available at www.improvingchroniccare.org. Accessed October 4, 2009.
- 2.Holman H. Chronic disease – the need for a new clinical education. JAMA. 2004;292:1057–1059. doi: 10.1001/jama.292.9.1057. [DOI] [PubMed] [Google Scholar]
- 3.Hoffman C, Rice D, Sung HY. Persons with chronic conditions: their prevalence and costs. JAMA. 1996;276:1473–1479. doi: 10.1001/jama.276.18.1473. [DOI] [PubMed] [Google Scholar]
- 4.DeVol R, Bedroussian A. An unhealthy America: the economic burden of chronic disease – charting a new course to save lives and increase productivity and economic growth. Milken Institute. October 2007.
- 5.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 6.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA. 2002;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 7.Wagner EH, Glasgow RE, Davis C, et al. Quality improvement in chronic illness care: a collaborative approach. Jt Comm J Qual Improv. 2001;27(2):63–80. doi: 10.1016/s1070-3241(01)27007-2. [DOI] [PubMed] [Google Scholar]
- 8.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff. 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 9.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff (Millwood) 2009;28(1):75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCulloch DK, Price MJ, Hindmarsh M, Wagner EH. A population-based approach to diabetes management in a primary care setting: early results and lessons learned. Eff Clin Pract. 1998;1(1):12–22. [PubMed] [Google Scholar]
- 11.Chin MH, Cook S, Drum ML, et al. Improving diabetes care in Midwest community health centers with the health disparities collaborative. Diab Care. 2004;27:2–8. doi: 10.2337/diacare.27.1.2. [DOI] [PubMed] [Google Scholar]
- 12.Wang A, Wolf M, Carlyle R, Wilkerson J, Porterfield D, Reaves J. The North Carolina experience with the diabetes health disparities collaboratives. Jt Comm J Qual Saf. 2004;30(7):396–404. doi: 10.1016/s1549-3741(04)30045-6. [DOI] [PubMed] [Google Scholar]
- 13.Darer JD, Hwang W, Pham HH, Bass EB, Anderson G. More training needed in chronic care: a survey of US physicians. Acad Med. 2004;79:541–548. doi: 10.1097/00001888-200406000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Langley GL, Nolan KM, Nolan TW, Norman CL, Provost LP. The improvement guide: a practical approach to enhancing organizational performance. 2. San Francisco: Jossey Bass; 2009. [Google Scholar]
- 15.Berwick DM. Developing and testing changes in delivery of care. Ann Int Med. 1998;128:651–656. doi: 10.7326/0003-4819-128-8-199804150-00009. [DOI] [PubMed] [Google Scholar]
- 16.Staker LV. Practice-based learning for improvement: the pursuit of clinical excellence. Tex Med. 2000;96:53–60. [PubMed] [Google Scholar]
- 17.Bonomi AE, Wagner EH, Glasgow RE, VonKorff M. Assessment of chronic illness care (ACIC): a practical tool to measure quality improvement. Health Serv Res. 2002;37(3):791–820. doi: 10.1111/1475-6773.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Solberg LI, Crain AL, Sperl-Hillen JM, Hroscikoski MC, Engebretson KI, O’Connor PJ. Care quality and implementation of the chronic care model: a quantitative study. Ann Fam Med. 2006;4(4):310–316. doi: 10.1370/afm.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Si D, Bailie R, Connors C, et al. Assessing health centre systems for guiding improvement in diabetes care. BMC Health Serv Res. 2005;5:56. doi: 10.1186/1472-6963-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Resnick HE, Foster GL, Bardsley J, Ratner RE. Achievement of American Diabetes Association clinical practice recommendations among U.S. adults with diabetes, 1999–2002: the national health and nutrition examination survey. Diab Care. 2006;29(3):531–537. doi: 10.2337/diacare.29.03.06.dc05-1254. [DOI] [PubMed] [Google Scholar]
- 21.Improving Chronic Illness Care. Practice change: working with academic medical centers. Available at www.improvingchroniccare.org. Accessed October 4, 2009.
- 22.Feifer C, Mora A, White B, Barnett BP. Challenges to improving chronic illness care and training in residencies. Acad Med. 2006;81(8):696–701. doi: 10.1097/00001888-200608000-00004. [DOI] [PubMed] [Google Scholar]
- 23.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Department of Health and Human Services. Healthy People 2010. 2nd ed. With understanding and improving health objectives for improving health. 2 vols. Washington, DC: U.S. Government Printing Office, November 2000.
- 25.O’Connor PJ. Commentary – improving diabetes care by combating clinical inertia. Health Serv Res. 2005;40(6):1854–1761. doi: 10.1111/j.1475-6773.2005.00437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]