Abstract
BACKGROUND
Unhealthy lifestyle choices frequently cause or worsen chronic diseases. Many internal medicine residents are inadequately trained to provide effective health behavior counseling, in part, due to prioritization of acute care in the traditional model of medical education and to other systemic barriers to teaching psychosocial aspects of patient care.
AIM
To address this gap in training, we developed and piloted a curriculum for a Primary Care Internal Medicine residency program that links a practical form of motivational interviewing (MI) training to the self-management support (SMS) component of the chronic care model.
PARTICIPANTS AND SETTING
All 30 primary care residents at Alameda County Medical Center were trained in the curriculum since it was initiated in 2007 during the California Academic Chronic Care Collaborative.
PROGRAM DESCRIPTION
Residents participated in three modules during which the chronic care model was introduced and motivational interviewing skills were linked to the model’s self-management support component. This training was then reinforced in the clinical setting. Case-based interactive instruction, teaching videotapes, group role-plays, faculty demonstration, and observation of resident-patient interactions in the clinical setting were used to teach the curriculum.
PROGRAM ASSESSMENT
A preliminary, qualitative assessment of this curriculum was done from a program standpoint and from the perspective of the learners. Residents reported increased sense of confidence when approaching patients about health behavior change. Faculty directly observed residents during clinical encounters using MI and SMS skills to work more collaboratively with patients and to improve patient readiness for self-management goal setting.
CONCLUSION
A curriculum that links motivational interviewing skills to the chronic care model’s self-management support component and is reinforced in the clinical setting is feasible to develop and implement. This curriculum may improve residents’ confidence with health behavior counseling and with preparing patients to become active participants in management of their chronic conditions.
KEY WORDS: chronic care model, self-management support, motivational interviewing, residency training, primary care
INTRODUCTION
Modifiable health behaviors contribute to chronic disease1. While many patients lack motivation and skills to maintain healthy behaviors2,3, academic training prioritizes acute care and reinforces overly directive interview styles, leaving residents ill prepared to provide health behavior counseling4-7. Residents frequently feel more comfortable intensifying medical management than they do collaborating with patients to promote healthy behavior.
A chronic care model (CCM)8,9 curriculum may address these training deficiencies by providing training in self-management support (SMS). SMS training prepares residents for the reality that patients, not physicians, manage chronic conditions through day-to-day decisions. This valuable CCM component assists patients in becoming good health self-managers and informed, active participants in their care10-13. SMS encourages healthy behaviors, provides information, teaches problem solving and disease management skills, assists with emotional support, and provides regular follow-up.
Our primary care medicine residency team participated in the California Academic Chronic Care Collaborative (CACCC) (2007–2008), whose goal was to improve chronic care education in academic settings. The CACCC emphasized training in collaborative action planning. This core SMS strategy assists patients in choosing behavior specific achievable self-management goals (e.g. walking 1/2 hour every other day) to build skills in health behavior change11. CACCC teams regularly reported on self-management goal setting, but with little discussion about preparing patients to be ready to support self-management when action plans failed. In our own setting, we observed residents having difficulty responding in a collaborative manner to patients who resisted setting personal action plans or supporting patients who had failed to complete their action plans. We felt that we could improve our residents’ experiences with SMS training by linking it with motivational interviewing (MI).
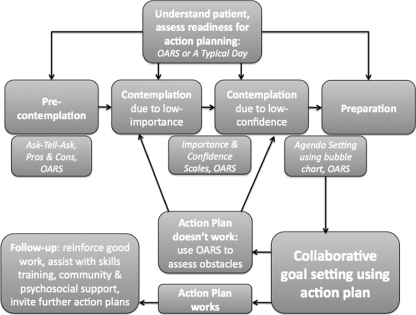
MI is an evidence-based counseling approach that SMS providers may use to help patients resolve ambivalence about health behavior change by developing discrepancy between actual and ideal behaviors14-19. Both SMS and MI philosophies emphasize internal over external motivation, collaboration, respect for the patient’s perspective, and support for patient self-efficacy (Fig. 1)10,15. A brief version of MI can be taught to residents20-27.
Figure 1.
Self-management support linked to brief motivational interviewing tools and stages of change11,14,15,21,30. Abbreviations: OARS, open-ended question, affirmation, reflection, summarizing. Motivational interviewing tools are italicized.
We describe a residency curriculum linking Brief MI to the CCM and its SMS component whose goal is to train residents to partner with patients in the care of their chronic conditions. It teaches a collaborative patient-care approach incorporating MI tools to help residents assist patients with chronic illness self-management by improving patient readiness for action planning. We piloted it during the CACCC and subsequently expanded it into a 3-year curriculum. We present the curriculum’s three modules, with its set of philosophies and multi-layered teaching strategies, and a preliminary curricular assessment. To our knowledge, we are the first to report a primary care residency curriculum linking MI to the CCM.
AIM
The Alameda County Medical Center (ACMC) primary care program developed a curriculum linking MI to SMS and the CCM. It aims to address residency training deficits in health behavior counseling by improving residents’ skills to activate low-motivated patients to better engage with self-management of their chronic conditions.
SETTING
Eighteen primary care internal medicine residents per year receive this curriculum at ACMC, an Oakland, California public hospital serving predominantly minority Medicaid and uninsured patients. On average, 55% of the trainees are underrepresented minorities, 70% are female, and their average age is 32. The authors, and other ACMC primary care faculty who participated in the CACCC, teach the curriculum. One author (S.A.), a behavioral medicine psychiatrist and an MI trainer, designed this curriculum. Two of the authors (L.B. and D.F.), who are internists and chronic disease specialists, developed Module 1.
PROGRAM DESCRIPTION
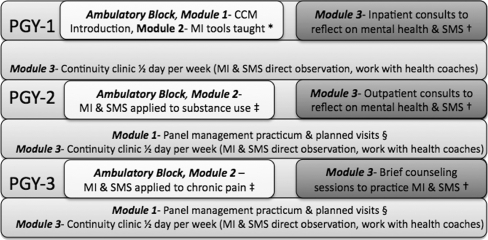
This curriculum includes three modules: 1) Introducing the CCM, 2) Teaching SMS Using Brief MI, and 3) Reinforcing in the Clinical Setting. We use case-based instruction, training videotapes, role-plays, experiential learning, direct observation with feedback, and modeling in clinical settings. The curriculum’s didactics occur during a four-week block rotation in each residency year. The remainder of the training occurs during the residents’ continuity clinics (one half-day per week during 46 weeks per year, on average), and during other rotations (Fig. 2). Embracing the continuous improvement approach, our curriculum is continually evolving. Some of the elements described are more fully implemented (e.g. MI didactic sessions) while others are in earlier stages of development (e.g. team care with premed health coaches).
Figure 2.
Curriculum linking motivational interviewing to self-management support and the chronic care model10,11,14,15,21,30. Each training year includes block activities (first row) and continuity clinic activities (second row). Abbreviations: CCM, chronic care model; SMS, self-management support; MI, motivational interviewing. • Module 1, ‘introducing the CCM,’ is 11 hours and includes local chronic care improvement projects presentation, observing health education classes, training in electronic population management system and panel registry reports. Module 2, ‘teaching SMS using Brief MI,’ includes 6 hours of training in the use of MI tools and action planning. † Module 3, ‘reinforcing in the clinical setting,’ includes using MI and SMS during an inpatient consultation rotation, an outpatient consultation rotation, and a brief counseling rotation. Each rotation is 3 hours per week during 4 weeks per year. ‡ MI & SMS training (Module 2) applied to substance use and chronic pain are each 3 hour didactics. § Panel management & planned visit training (Module 1) is 8 hours per week during 12 weeks per year.
Module 1: Introducing the Chronic Care Model
In Module 1, first year residents learn about the CCM as a six-component health systems improvement model with clinical applications8,9. This complements Module 2’s MI and SMS counseling training, where chronic care is taught at the doctor-patient interaction level.
In the second and third years of training, residents participate in a panel management practicum that reinforces their understanding of CCM components. Activities include using a registry to identify patients who do not meet clinical guidelines, protected time for telephone follow-ups, study of evidence-based guidelines for targeted chronic diseases, and work with panel managers to broaden team care experiences. During patient follow-up, residents use MI to assess patients and prepare them for SMS. To further this type of experiential learning, we have begun integrating planned visits. All residents are expected to design a quality improvement project using plan-do-Study-Act cycles to test small changes before broader implementation (Model for Improvement)28,29.
Module 2: Teaching Self-Management Support Using Brief Motivational Interviewing
Introduction to Clinical Empathy
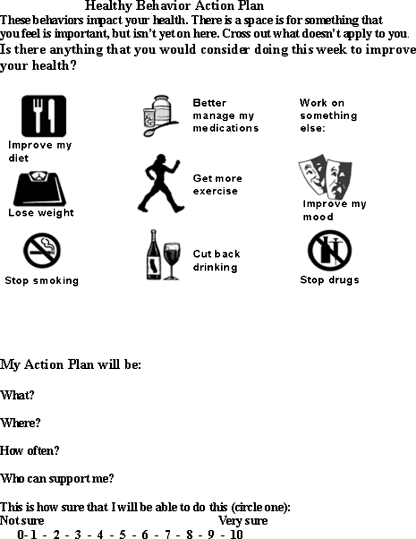
SMS and MI promote provider-patient collaboration based on understanding patients’ viewpoints. Our curriculum incorporates empathy-building exercises learned from other CACCC teams to improve residents’ understanding of patients living with chronic conditions: 1) Residents discuss medical, social and emotional self-management needs of diabetics, and 2) They use an agenda setting chart (Fig. 3) to devise 2-week stress-reduction action plans for themselves, to experience challenges with self-management goal setting.
Figure 3.
Agenda setting and health behavior action planning tool11,21.
Despite these exercises, when residents try to elicit patients’ perspectives, many struggle with how to express empathy. To teach this, our curriculum uses training videos and role-plays demonstrating the MI strategies of open-ended questions, affirmations, reflective listening and summarizing (OARS)15. To demonstrate how OARS is a first step before action planning, residents participate in a role-play with a standardized patient. The group learns that even after a cardiologist added another medication, this immigrant woman had persistent hypertension. A resident investigates:
• Resident: “How’s it going with your medicines?” (Open-ended question)
• Patient: “I’m always tired and need to urinate. But I still swim!”
• Resident: “Great, you’re swimming! But you’re concerned that your medicines make you feel bad.” (Affirmation and reflection)
• Patient: “Right, sometimes I don’t take those water pills. To not offend him, I didn't tell the heart doctor.”
• Resident: “So the heart doctor thought you needed more medicine, and really you weren’t comfortable taking the water pills?” (Summarizing)
This role-play illustrates the value of understanding ‘where a patient is’ before jumping to action planning. Someone from a culture deferential to authority might ‘comply’ with action planning, yet her hypertension does not improve. OARS is designed to help residents address patient–physician relationship barriers that may be overlooked if the resident is overly focused on action planning.
Brief MI and SMS Six-Pack of Tools
The CACCC encouraged residents to do collaborative action planning with most patients. We observed residents becoming frustrated when low-motivated patients did not follow through. Reworking action plans led to further frustration. Residents required other tools to activate these patients. During the CACCC, we addressed this problem with action planning by expanding our existing MI curriculum (a set of brief MI strategies applied to the stages of change (SOC)) into an MI-based SMS curriculum20,30,31. First, we trained residents to identify patients’ stages on a change continuum from denial (pre-contemplation), to ambivalence (contemplation), to preparation, to taking action (Fig. 1). The goal was to use MI tools to help low-motivated patients move along this change continuum until they reached a readiness stage to be ‘informed and activated’ in the care of their chronic conditions. Residents became less frustrated when they understood that their task was not to change patients, but to help them move to the next SOC. Testing (using a plan-do-study-act cycle28,29) during the CACCC showed this approach made sense to residents.
Tool #1: Assessing the Stage of Change
We train residents in two strategies, OARS and a typical day, to assess the SOC. Before initiating action planning, residents practice OARS to elicit verbal cues indicative of each SOC for typical chronic care patients. They then practice a typical day, which provides a relevant view of the personal context of a health behavior21. They ask a standardized patient, a diabetic who had failed diet action plans, to walk them through her typical day and food. They learn that she bakes pastries to share with neighbors, and remained in a contemplative SOC regarding weight loss, because dieting would have impeded her social routine. The residents help her create an action plan to find other ways to socialize.
Tools #2 and #3: Ask-Tell-Ask and Pros-and-Cons
Our curriculum includes two MI tools (‘ask-tell-ask’ and ‘pros-and-cons’) to help residents build motivation in pre-contemplative patients. We explain that these tools should be used with patients at this SOC instead of action planning.
‘Ask-tell-ask’ is popular among SMS providers, because it provides information by collaborating with patient self-expertise14,21. Residents ask and affirm what patients know; they ask permission to tell information; they ask for patient feedback. We find residents need reminding ‘to ask’ and ‘not tell’ whenever providing medical information. ‘ask-tell-ask’ can also develop discrepancy in low-motivated patients. Using a role-play, residents collaboratively engage a low motivated drinker in a discussion about alcoholic hepatitis. This leaves him room to discuss his fear of cirrhosis, thus disrupting his comfort with drinking.
‘Pros-and-cons’ asks a patient to consider both sides of behavior. To practice, residents list ‘pros-and-cons’ of drinking: “What are good things about drinking?” is followed by, “What are the less good things about drinking?” Describing cons after pros pushes a patient ‘in denial’ to argue for change, called ‘change talk’. Using this tool, and watching patients move from ‘denial’ to ambivalence, enhances resident self-efficacy. This newfound ambivalence moves the patient one step closer towards readiness to become informed and activated.
Residents practice tools one through three in paired role-plays involving a patient with chronic disease, who is ‘in denial’ about a behavior exacerbating his condition.
Tool #4: Importance and Confidence Scales
CACCC participants learned that SMS builds self-efficacy10,11. Despite this, we observed residents lecturing patients about the importance of changing behaviors—even when patients agreed and were, in fact, struggling with poor health self-management skills. Conversely, some residents persisted in reworking action plans—even when patients did not follow-up, usually because something more important prevented that action. We realized that our curriculum needed to maintain a focus not only on ‘self-efficacy,’ but also on ‘importance’ as motivation factors15.
In our curriculum, residents learn to assess patients for low self-efficacy and low importance, using ‘importance and confidence scales’. Practicing it with themselves, they rate from 0–10 how important it is for them to counsel smokers. By asking why most chose higher and not lower numbers, residents argue for the importance of counseling smokers. When repeated with a confidence scale, most chose lower numbers. By asking what would it take to choose a higher number, residents discuss ways to improve their counseling efficacy. We then discuss how an HIV patient was a ‘no-show’ until a clinic began offering grocery vouchers. Before vouchers raised the ‘importance’ of attending appointments, a patient generated action plan that worked out bus routes to the clinic had failed.
Using this tool helps residents figure out what is needed to activate patients. If low importance, ask patients what they need to raise the importance of a healthier choice; if low confidence, use action planning to improve self-efficacy.
Tools #5 and #6: Agenda Setting and Action Planning
The ‘agenda-setting tool’ (MI’s term) or ‘bubble chart’ (SMS’s term) helps patients pick behaviors they want to work on21,32. We designed our ‘bubble chart’ for our diverse, low literacy cardiovascular patients based on testing during the CACCC. Residents use it with a standardized patient, a poorly controlled diabetic. After being cued, she points to the mood image (Fig. 3). Grief from her sister’s death leaves her unable to monitor blood sugars. Residents learn an important SMS concept; emotional support can be a disease management strategy.
While agenda setting works best for patients prepared to change, it may also help patients in contemplation with low self-efficacy. The act of ‘considering’ multiple options for change may move patients ‘to decide’ to act.
When agenda setting leads to goal setting, residents collaboratively help patients to action plan. Our curriculum promotes action planning for: 1) the preparation SOC, or 2) for contemplation patients who feel change is important, but have low confidence that they can make changes. We teach agenda setting and action planning as connected, but separate strategies. Agenda setting requires patients ‘to consider’ change, action planning requires patients ‘to try’ change. This helps residents understand why patients create seemingly achievable action plans and, in the end, rate their motivation as low to carry it out. These patients were not yet ready to go from ‘considering’ to ‘trying’ change.
Residents learn action planning through training videos and group role-plays.
To integrate tools four through six, residents practice paired role-plays where they help a patient move from contemplation to action planning.
Brief MI and SMS Review
Using case-based discussions and group role-plays, our curriculum includes annual workshops where we review SMS and MI strategies and apply them to challenging clinical scenarios (Fig. 2).
Module 3: Reinforcement in the Clinical Setting
Reinforcement of our curriculum occurs in the continuity clinic and utilizes several teaching methodologies, including a behavioral medicine specialist joining residents in continuity clinics to observe their SMS and MI skills, and offer feedback and modeling (Fig. 2).
During the CACCC, another team developed a health coach model using salaried health workers. Health coaches are non-physician primary care team members who assist patients in achieving SMS goals. Building on others’ successes with using health coaches in clinical practices33,34, we recruited premedical volunteers and trained them in SMS and MI. After observing the resident-patient interview, while residents are discussing cases with faculty, these coaches provide patients with SMS. Our curriculum now includes training residents to partner with coaches, which they do enthusiastically. In turn, we have observed, that this team-care experience further activates residents to include SMS in patient care.
PROGRAM EVALUATION
During the CACCC, we began preliminary qualitative assessments of this curriculum from both a program standpoint and from the learner’s perspective with the goal of continuously improving the curriculum. Learners complete anonymous evaluations after didactics, practicum, and at the completion of residency. Additionally, residents discuss this curriculum during group feedback sessions with faculty. From a program perspective, our faculty discusses this curriculum quarterly, including obstacles to teaching it. Instructors also directly observe residents’ implementation of MI and SMS skills during patient encounters.
Residents’ preliminary feedback is encouraging. They report improved understanding of the CCM; increased confidence with assisting patients in health behavior change and more awareness of socioeconomic obstacles; increased SMS engagement when working with premed health coaches; and improved patient–physician collaboration. Faculty directly observed residents during clinical encounters using MI and SMS skills to work more collaboratively with patients and to improve patient readiness for self-management goal setting.
Residents and faculty report obstacles to integrating MI and SMS skills into daily practice, including the urgency of acute care, other time constraints, forgetting specifics of MI tools, and lack of reinforcement by faculty not trained in these skills. We have increased faculty development sessions devoted to teaching MI and SMS.
As our curriculum progresses, we plan a more systematic and robust evaluation of resident learning and practice behaviors. Knowledge assessment will include videotaped patient interviews whereby residents will identify the SOC and/or MI tool being demonstrated. We plan to use direct observation with standardized checklists for SMS and MI-based competencies during resident-patient encounters. To assess patients’ experience of the care provided by residents trained in this curriculum, we will use the Patient Assessment of Chronic Illness Care (PACIC) survey35.
CONCLUSION
During the California Academic Chronic Care Collaborative, we began developing and implementing a curriculum that teaches internal medicine residents to use chronic care model components to improve clinical care, and motivational interviewing (MI) skills to better prepare patients at different levels of motivation to become activated in the self-care of their chronic conditions.
Through developing this curriculum, we have learned that teaching patient-centered health behavior counseling is a multi-layered process. Not only classroom teaching, also on-going experiential training is required at the point of care. In addition to counseling within 15-minute clinic visits, we added another layer of counseling experience by having residents provide four 45-minute MI-oriented sessions to select patients. We also reinforced this ambulatory-based curriculum with consultations on hospitalized patients to expand the residents’ context for applying concepts of self-management. Further, recognizing that our faculty needed support in learning these new concepts, we layered in a faculty development component. We have also learned that teaching a collaborative chronic care philosophy requires a collaborative teaching philosophy based on small encouraging steps of learning. While this curriculum competes with other training priorities within a residency, we are optimistic about its perceived value for resident education.
We intend to implement more robust evaluation methods. Further studies are also needed to link clinical outcomes with our approach to self-management. MI and SMS emphasize flexible strategies tailored to unique provider-patient dyads. However, research depends on standardized and replicable interventions, making objective study of this curriculum challenging36.
We successfully developed and implemented a curriculum designed to provide residents the knowledge and skills needed to integrate MI with SMS strategies when providing care to patients with chronic conditions. Although our assessment is preliminary, this curriculum may improve residents’ confidence in assisting patients with health behavior change. Our ultimate goal is to improve our residents’ abilities to activate patients at varying levels of motivation to better engage with self-management of their chronic conditions.
Acknowledgments
Funders This work was partially funded by a Health Resources and Services Administration Grant for Training in Primary Care Medicine and Dentistry.
Conflict of Interests None disclosed.
References
- 1.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–45. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Dalle Grave R, Melchionda N, Calugi S, et al. Continuous care in the treatment of obesity: an observational multicentre study. J Intern Med. 2005;258:265–73. doi: 10.1111/j.1365-2796.2005.01524.x. [DOI] [PubMed] [Google Scholar]
- 3.King DE, Mainous AG, 3rd, Carnemolla M, Everett CJ. Adherence to healthy lifestyle habits in US adults, 1988–2006. Am J Med. 2009;122:528–34. doi: 10.1016/j.amjmed.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Park ER, Wolfe TJ, Gokhale M, Winickoff JP, Rigotti NA. Perceived preparedness to provide preventive counseling: reports of graduating primary care residents at academic health centers. J Gen Intern Med. 2005;20:386–91. doi: 10.1111/j.1525-1497.2005.0024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Merkel WT, Margolis RB, Smith RC. Teaching humanistic and psychosocial aspects of care: current practices and attitudes. J Gen Intern Med. 1990;5:34–41. doi: 10.1007/BF02602307. [DOI] [PubMed] [Google Scholar]
- 6.Hoppe RB, Farquhar LJ, Henry R, Stoffelmayr B. Residents' attitudes towards and skills in counseling: using undetected standardized patients. J Gen Intern Med. 1990;5:415–20. doi: 10.1007/BF02599430. [DOI] [PubMed] [Google Scholar]
- 7.Moulmein JR, Caracas’s GJ. Evaluating the interview performance of internal medicine interns. Accad Med. 1989;64:277–9. doi: 10.1097/00001888-198905000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–9. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 9.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288:1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 10.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–75. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 11.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 12.Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. 2004;164:1641–9. doi: 10.1001/archinte.164.15.1641. [DOI] [PubMed] [Google Scholar]
- 13.Dennis SM, Zwar N, Griffiths R, et al. Chronic disease management in primary care: from evidence to policy. Med J Aust. 2008;188(8 Suppl):S53–6. doi: 10.5694/j.1326-5377.2008.tb01745.x. [DOI] [PubMed] [Google Scholar]
- 14.Bodenheimer T, MacGregor K, Shafiri C. Helping Patients Manage Their Chronic Conditions. California HealthCare Foundation; 2005.
- 15.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. New York: Guilford Press; 2002. [Google Scholar]
- 16.Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71:843–61. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- 17.Martins RK, McNeil DW. Review of motivational interviewing in promoting health behaviors. Clin Psychol Rev. 2009;29:283–93. doi: 10.1016/j.cpr.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55:305–12. [PMC free article] [PubMed] [Google Scholar]
- 19.MI Bibliography 1983–2009. Available at: www.motivationalinterview.org/library/biblio.html. Accessed Sept 27, 2009.
- 20.Rollnick S, Miller WM, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York: Guilford Press; 2008. [Google Scholar]
- 21.Rollnick S, Mason P, Butler C. Health Behavior Change: A Guide for Practitioners. Edinburgh: Churchill Livingstone; 1999. [Google Scholar]
- 22.Bell K, Cole BA. Improving medical students' success in promoting health behavior change: a curriculum evaluation. J Gen Intern Med. 2008;23:1503–6. doi: 10.1007/s11606-008-0678-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poirier MK, Clark MM, Cerhan JH, Pruthi S, Geda YE, Dale LC. Teaching motivational interviewing to first-year medical students to improve counseling skills in health behavior change. Mayo Clin Proc. 2004;79:327–31. doi: 10.4065/79.3.327. [DOI] [PubMed] [Google Scholar]
- 24.Rubak S, Sandbaek A, Lauritzen T, Borch-Johnsen K, Christensen B. General practitioners trained in motivational interviewing can positively affect the attitude to behaviour change in people with type 2 diabetes. one year follow-up of an RCT, ADDITION Denmark. Scand J Prim Health Care. 2009;27(3):172–9. doi: 10.1080/02813430903072876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scal P, Hennrikus D, Ehrlich L, Ireland M, Borowsky I. Preparing residents to counsel about smoking. Clin Pediatr Phila. 2004;43:703–8. doi: 10.1177/000992280404300803. [DOI] [PubMed] [Google Scholar]
- 26.Thijs GA. GP's consult and health behaviour change project. Developing a programme to train GPs in communication skills to achieve lifestyle improvements. Patient Educ Couns. 2007;67:267–71. doi: 10.1016/j.pec.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 27.White LL, Gazewood JD, Mounsey AL. Teaching students behavior change skills: description and assessment of a new Motivational interviewing curriculum. Med Teach. 2007;29:67–71. doi: 10.1080/01421590601032443. [DOI] [PubMed] [Google Scholar]
- 28.Deming WE. The New Economics for Industry, Government and Education. 2. Cambridge, MA: MIT Press; 2000. [Google Scholar]
- 29.Institute for Healthcare Improvement. Testing Changes. http://www.ihi.org/IHI/Topics/Improvement/ImprovementMethods/HowToImprove/testingchanges.htm. Accessed May 26, 2010.
- 30.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol Sep. 1992;47(9):1102–14. doi: 10.1037/0003-066X.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 31.Verheijden MW, Bakx JC, Delemarre IC, et al. GPs' assessment of patients' readiness to change diet, activity and smoking. Br J Gen Pract. 2005;55:452–7. [PMC free article] [PubMed] [Google Scholar]
- 32.Stott NC, Rees M, Rollnick S, Pill RM, Hackett P. Professional responses to innovation in clinical method: diabetes care and negotiating skills. Patient Educ Couns. 1996;29:67–73. doi: 10.1016/0738-3991(96)00935-4. [DOI] [PubMed] [Google Scholar]
- 33.Laing B, Ward L, Yeh T, Chen E, Bodenheimer T. Introducing the “Teamlet”: initiating a Primary Care Innovation at San Francisco General Hospital. Perm J. 2008;12:4–9. doi: 10.7812/tpp/07-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bodenheimer T, Laing B. The teamlet model of primary care. Ann Fam Med. 2007;5:457–61. doi: 10.1370/afm.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC) Med Care. 2005;43:436–44. doi: 10.1097/01.mlr.0000160375.47920.8c. [DOI] [PubMed] [Google Scholar]
- 36.Emmons KM, Rollnick S. Interviewing in health care settings. Opportunities and limitations. Am J Prev Med. 2001;20:68–74. doi: 10.1016/S0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]