Abstract
The Nouna Health and Demographic Surveillance System (HDSS) is located in rural Burkina Faso and has existed since 1992. Currently, it has about 78,000 inhabitants. It is a member of the International Network for the Demographic Evaluation of Populations and Their Health in Developing Countries (INDEPTH), a global network of members who conducts longitudinal health and demographic evaluation of populations in low- and middle-income countries. The health facilities consist of one hospital and 13 basic health centres (locally known as CSPS). The Nouna HDSS has been used as a sampling frame for numerous studies in the fields of clinical research, epidemiology, health economics, and health systems research. In this paper we review some of the main findings, and we describe the effects that almost 20 years of health research activities have shown in the population in general and in terms of the perception, economic implications, and other indicators. Longitudinal data analyses show that childhood, as well as overall mortality, has significantly decreased over the observation period 1993–2007. The under-five mortality rate dropped from about 40 per 1,000 person-years in the mid-1990s to below 30 per 1,000 in 2007. Further efforts are needed to meet goal four of the Millennium Development Goals, which is to reduce the under-five mortality rate by two-thirds between 1990 and 2015.
Keywords: epidemiology, Burkina Faso, Africa, INDEPTH network, public health, under-five mortality, malaria, malnutrition, health seeking behavior
The absence of reliable demographic and health data is a common problem in many developing countries especially in rural sub-Saharan Africa (SSA). Burkina Faso, a land-locked country of West Africa ranking as one of the poorest countries in the world, is no exception. Regular registration of births and deaths do not exist in large parts of SSA, in particular, not in the rural areas and population registers are also uncommon. Therefore, reliable basic demographic and epidemiologic indicators such as birth and death rates are largely estimated based on census analysis. Furthermore, the cause-of-death data are notoriously biased in low-income countries as they are based on facility reporting. Only a small proportion of deaths, however, occur within health services and those which do are not representative of the total population. Therefore, any cause of death statistic based on facility reports must be taken with great caution.
The lack of relevant health information is a hindrance to the assessment of the population health as well as to the development of health care interventions and their evaluation. Different methods have been tried to obtain such data. One of these methods are the ‘demographic health surveys’ (DHS), which are being performed in most African countries (http://www.measuredhs.com) as cross-sectional surveys from a representative sample of the population. Another method is the ‘demographic surveillance systems’ (DSS), which have been put in place in an increasing number of rural and urban areas and are designed to follow-up a population in a longitudinal way. The term DSS has recently been changed to HDSS with ‘H’ standing for ‘health’.
The HDSS is a dynamic cohort that is defined as the total population in a specified geographic area. Newborns and immigrants are included in the cohort and the birth or in-migration date is recorded. Similarly, deaths and out-migrations are recorded. Usually no effort is made to trace out-migrated cohort members. It begins with an initial census of the population and proceeds with monitoring – in a regular manner – vital events (births, deaths), migration, selected health outcomes, and other demographic and lifestyle variables. Control censuses are done to check the completeness of the follow-up procedures. As of today, 38 HDSS in 19 different countries exist that are organised in an international network named the International Network of Field Sites with Continuous Demographic Evaluation of Populations and Their Health in Developing Countries or INDEPTH (http://www.indepth-network.org). This network was established in Dar es Salaam, Tanzania, in 1998 to foster the established HDSS, promote the creation of new sites, coordinate activities, support uniform field procedures, allow comparative analyses, share know-how, and stimulate collaboration with international research institutions. INDEPTH also aims to promote South-South multi-site research and contribute to the global policy agenda.
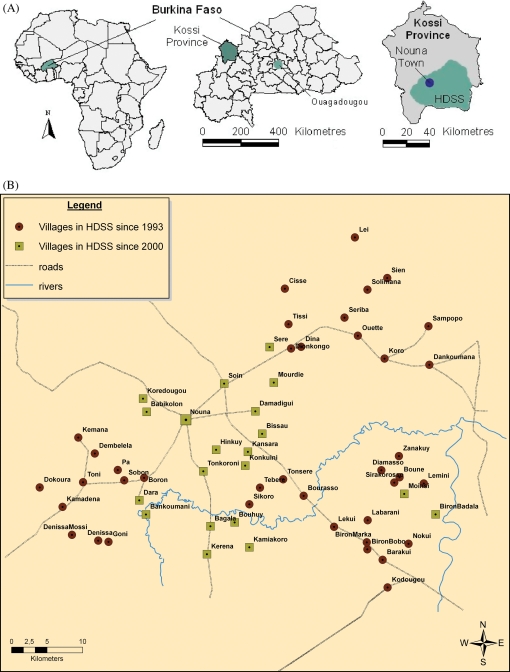
The HDSS presented in this paper is located in the town of Nouna and surrounding villages (Fig. 1). Nouna is a semi-urban town in the northwest of Burkina Faso and functions as the administrative centre of the Kossi province, which geographically corresponds to the Nouna Health District. It has a surface area of 7,464 km2 with a population estimated at 320,232 in 2009 after an adjustment from the national general census of 2006. It is distributed in 228 localities, served by 29 basic health facilities locally known as Centre de Santé et de Promotion Sociale (CSPS), and one district hospital with surgery capability known as the Centre Médical avec Antenne chirurgicale (CMA). The main aims of the HDSS was to provide reliable demographic and health indicators for a rural population in Burkina Faso, and to generate an infrastructure and a sampling frame for epidemiological and clinical studies nested into this dynamic cohort.
Fig. 1.
Geographical location of the Nouna Health and Demographic Surveillance System (HDSS) in Burkina Faso (A); with details of participating localities (B).
There has been an intense scientific contact between the University of Heidelberg in Germany and the Ministry of Health in Burkina Faso since the 1970s (1). This contributed to the implementation of a number of health system research projects in the Nouna Health District in collaboration with German developmental organisations. These developments led to the establishment of a DSS (now called HDSS) based in Nouna in 1992 and subsequently to the founding of a national health research centre in 1999, the Centre de Recherche en Santé de Nouna (CRSN). The Nouna HDSS is now administered by the CRSN.
In terms of capacity building, intensive efforts have been put on both infrastructure and human capacity since 1999. A major contribution to the research training of the scientists of Burkina Faso, including Nouna HDSS staff, was done in postgraduate training programs (MSc or PhD) at the University of Heidelberg/Germany, University of Montreal, University of Wits/South Africa, INED/Université de Paris XII/France and University of Ouagadougou. The setting was also upgraded in terms of infrastructure and equipment to fulfil the requirement of a high-quality research centre over the years.
During the last decade, over a hundred peer-reviewed manuscripts were published that either used the full Nouna HDSS database for descriptive epidemiological studies or that used the HDSS population as a sampling frame for studies on various research topics as further described below. In this paper we present relevant epidemiological measures, such as mortality and birth rates and provide time trend analyses. Furthermore, the main past findings from the HDSS are reviewed.
Study population and methods
The Nouna HDSS covers a subset of the Nouna Health Districts with about 78,000 inhabitants in 2007, distributed over 1,756 km2 (Fig. 1). Full population censuses were conducted for the HDSS in 1992, 2000, and 2009. With about 23,500 inhabitants, the town of Nouna represented 30% of the HDSS population in 2007. Starting in 1992, the HDSS covered three CSPS within 39 villages for a population of 26,626. Additions to the HDSS include the town of Nouna and two villages in the year 2000 and 17 villages in the year 2004 for a current total of 58 villages (Table S1 in the supplementary data). In 2009, the health facilities consist of one hospital and 13 CSPS out of the 29 for the whole district. The HDSS represents roughly one-quarter of the Nouna Health District both in terms of surface and population. Although the Nouna HDSS population is not selected randomly from the population in Burkina Faso, key variables are comparable to those observed at the national level (Table 1), such that it is appropriate to generalise results from the Nouna area with appropriate caution.
Table 1.
Basic demographic statistics of Nouna HDSS compared to the results of the general census of the population of 2006
| Variables | Nouna | National |
|---|---|---|
| Women | 49.97% | 51.72% |
| Men | 50.03% | 48.28% |
| Crude birth rate | 40.29 per 1,000 | 46 per 1,000 |
| Mean number of children per women | 6.1 | 6.2 |
| Crude death rate | 10.7 per 1,000 | 11.8 per 1,000 |
| Infant mortality rate | 75.94 per 1,000 | 91.7 per 1,000 |
| Life expectancy | 57 years | 56.7 years |
The household is the basic survey unit and is defined as an independent socio-economic unit. Household members usually live in the same house or compound, pulling resources together to meet basic dietary and other vital needs under the authority of one person recognised as the head of the household. Individual members within the household can usually be related and identify themselves as belonging to the household.
The mostly rural population of the multi-ethnic Kossi province consists predominantly of subsistence farmers and cattle keepers. The region is a dry orchard savannah and has a sub-Sahelian climate with a mean annual rainfall of 796 mm (range 483–1,083 mm) over the past five decades. The main ethnic groups in the Nouna Health District are the Dafing, Bwaba, Mossi, Peulh, and Samo. The Dioula language serves as a lingua franca, permitting communication between the different ethnic groups (1).
There are clear urban–rural differences between Nouna town and the surrounding villages, although Nouna town is often described as semi-rural. The town of Nouna has a better infrastructure as well as easier and better access to the education and health system. It has developed rapidly over the last decade and has seen a major improvement in the access to transport, drinking water, electricity, and more recently mobile phones and the Internet.
Village population in 2007 ranged from 78 to 3,199 persons (mean: 944 persons; median: 735 persons). The distances from villages to health centres ranged from 0 to 34 km (average: 8.5 km; median: 8.0 km) with a median time needed to reach the nearest health facility on foot estimated at 75 minutes in the dry season and 90 minutes in the rainy season.
Frequency of follow-up
Trained field staff visit households in the HDSS area systematically to record births and deaths – the base of the vital events registration (VER) system – as well as in- and out-migration. Regular household visits were performed every 3 months until 2006 and every 4 months since then. Field workers are supported by one key informant per village collecting vital events on a daily basis to ensure data accuracy locally.
Active vital events registration (VER)
Each individual is assigned a unique identification number, which is maintained regardless of household rearrangement (e.g. marriage). In accordance to general HDSS procedures, basic demographic parameters (date of birth, date of in- or out-migration, and date of death) are collected regularly. In addition, a questionnaire is administered that includes variables about religion, ethnic group, household characteristics, and individual members of the household, such as ID numbers of the parents (if a member of the HDSS). The parental ID allows identifying lineage and constructing relevant variables, such as age of parents at birth, birth order, or intervals between births.
Verbal autopsies (VA)
While total mortality within the HDSS can be estimated with relatively high precision, more difficulties occur with cause-specific mortality. Verbal autopsies (VA) are interviews conducted by trained personnel in houses after a death has occurred (2, 3). They are useful to analyse mortality data by cause-of-death and help formulate more specific health interventions.
In Nouna HDSS, the trained field staff (without a medical background and not specifically trained in health care) visit houses where a death has been registered and ask pre-established questions relating to the signs and symptoms experienced by the deceased before death. The interview usually takes place about 6 months after the event with the person who assisted the deceased before his death. The standardised questionnaire developed at the CRSN includes demographic data and the clinical history before death (accident, symptoms, treatment, etc.). Two experienced local physicians later interpret the answers to the questionnaire and independently determine the most probable cause of death. In the case of disagreement, a third physician is consulted. Cause of death is attributed only if supported by at least two physicians using ICD-10. VA have been recorded since 1993 in the HDSS area, but data is considered complete only since 1999 when the active VER was implemented (4, 5). Despite their acknowledged limitations (6), VA are still considered the best possible method to get cause-of-death estimates in areas where VER systems are not available. Currently, the use of automated Bayesian models to assign the most likely causes of death (7) are under investigation in the Nouna HDSS.
Quality control
Quality control is ensured by several check mechanisms put in place at different stages of the survey. In the field, 5 to 10% of households are interviewed a second time by a supervisor. At the data entry level, a set of logical and consistency checks of the basic variables (e.g. sex, age, and the period of residence in the study area) ensure internal coherence of the data. In addition, a systematic mutual control is implemented among entry clerks. Multiple entries into the study area and individuals with missing values in the key variables are deleted from the database, or replaced by plausible values if possible.
Statistical methods
Mortality and birth rates were calculated as number of deaths/births per 1,000 person-years. Temporal trends were assessed with Poisson regression by modelling log (rates) as a linear function of the year. The attrition rate was computed for a given year as the number of individuals lost from the sample due to out-migration or loss to follow-up – but not death – over the total number of individuals registered in the HDSS that year.
Results
Population characteristics
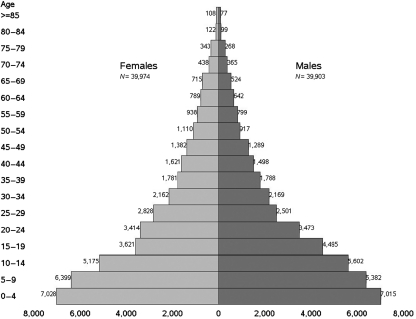
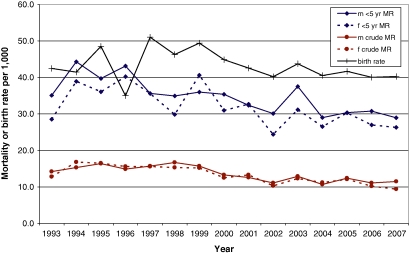
The age distribution as of 31 December 2007 showed the typical pattern of a developing country (Fig. 2). Fig. 3 shows birth rates and mortality rates from 1993 until 2007. The birth rates averaged 42.7 lived births per 1,000 over the period. Mortality rates for under five-year-olds averaged 32.1 per 1,000 and were slightly higher in males than in females (33.6 vs 30.6 per 1,000). Under 1-year-old mortality rates averaged 57.2 per 1,000 (58.5 in males; 55.8 in females). The total crude mortality rate was 12.7 per 1,000. Both the population distribution by age and the mortality rates reflect a typical pattern of population structures and total mortality in rural Africa as a whole (8). This corresponds to high childhood mortality and a young population with about 60% below age 25 and only about 10% above age 64.
Fig. 2.
Population pyramid on 31 December 2007, Nouna HDSS, Burkina Faso.
Fig. 3.
Mortality rates (MR; under 5 years and overall crude rate) by sex (m = male, f = female) and birth rate, 1993–2007, Nouna HDSS, Burkina Faso.
In the trend analysis, a decline was found for all mortality rates that is highly significant (p < 0.001). For childhood mortality the yearly decline is 2.4%, resulting in a 24% decrease per decade.
The birth rate appears to increase at the beginning of the HDSS and decrease after 1997. Overall, a significant decline is observed (p < 0.001). Assuming a linear trend after 1997, we observe a yearly decrease of 2.3% of the birth rate.
In the period from 1993 to 2007, the attrition rate ranged between 3.6 and 9.1% per year with an average of 6.5% (Table 2). It averaged at 5.4% (range 2.7%–8.0%) in males and at 7.6% (range 4.4%–10.4%) in females. Attrition was higher in females with an important contributing factor being young women marrying out of the HDSS area. The increase in the attrition rate over the years indicates an increased mobility of the population.
Table 2.
Population characteristics per year, Nouna HDSS, Burkina Faso
| Year | Population (1 January) | Households | Births | Deaths | In-migration | Out-migration | Attrition ratea (%) |
|---|---|---|---|---|---|---|---|
| 1993 | 27,896 | 3,600 | 1,208 | 390 | 1,688 | 1,072 | 3.84 |
| 1994 | 29,330 | 3,664 | 1,220 | 478 | 1,339 | 1,062 | 3.62 |
| 1995 | 30,349 | 3,789 | 1,476 | 501 | 1,463 | 1,286 | 4.24 |
| 1996 | 31,501 | 3,903 | 1,072 | 476 | 1,137 | 1,142 | 3.63 |
| 1997 | 32,092 | 3,994 | 1,605 | 495 | 1,379 | 1,513 | 4.71 |
| 1998 | 33,068 | 4,042 | 1,489 | 521 | 2,054 | 1,771 | 5.36 |
| 1999 | 34,319 | 4,027 | 1,644 | 518 | 2,182 | 1,858 | 5.41 |
| 2000b | 35,769 | 4,070 | 2,664 | 773 | 2,504 | 2,566 | 7.17 |
| 2001 | 63,047 | 7,499 | 2,571 | 784 | 4,658 | 5,641 | 8.95 |
| 2002 | 63,851 | 7,488 | 2,434 | 654 | 4,643 | 5,842 | 9.15 |
| 2003 | 64,432 | 7,488 | 2,688 | 784 | 4,332 | 5,133 | 7.97 |
| 2004b | 65,535 | 7,535 | 2,988 | 814 | 4,682 | 5,360 | 8.18 |
| 2005 | 77,439 | 9,049 | 3,119 | 923 | 5,507 | 7,047 | 9.10 |
| 2006 | 78,095 | 9,195 | 3,019 | 811 | 4,688 | 6,914 | 8.85 |
| 2007 | 78,072 | 9,260 | 2,984 | 805 | 3,905 | 5,341 | 6.84 |
aAttrition rate = out-migration/population×100.
bNouna town and two villages added in 2000 (28,489 individuals) and 17 villages added in 2004 (10,804 individuals); out-migration from these included in the following year.
Previous main findings
Mortality and morbidity
The full HDSS was primarily used to analyse mortality and morbidity patterns by year, area, and season, or to identify and quantify risk factors (9, 10). It thus contributed to the still imperfect knowledge of mortality and morbidity patterns along with their economic impact (11–13) in Burkina Faso in particular and in SSA in general. For example, Sankoh et al. (14) were able to identify villages with higher childhood mortality rates. This finding was the starting point to search for the underlying causes for disparities within an area with generally high childhood mortality. A strong seasonal pattern was observed with higher mortality within and shortly after the rainy season, which could be explained with higher malaria transmission during that time (15, 16). In the study of Ndugwa et al. (17), the childhood mortality trends were analysed and compared with those from a comparable HDSS in The Gambia. A decline was observed in both countries, which was more pronounced in The Gambia however. Also, the relative importance of malaria as the major cause of death was found to increase over time. Würthwein et al. (5) established the local burden of disease using years of life lost (YLL) analysis and compared it to the Global Burden of Disease Study (GBDS). As in the GBDS malaria, diarrhoeal diseases and lower respiratory infections ranked among the top three diseases although in different order and proportion. However, the pattern of the burden of disease also showed crucial differences, with protein–energy malnutrition, bacterial meningitis, and intestinal nematode infections being much more prominent in the HDSS than at the GDBS level. Further studies explored local disability weights and perception of the burden of disease (18, 19).
The HDSS has also been the sampling frame for several randomised clinical studies (20, 21), and has provided the base for a large number of cross-sectional and case-control studies. Topics studied are as varied as the effect of cooking with biomass on malaria (22) or the micro-epidemiology of malaria with respect to locally measured meteorological data and land cover such as bare soil, vegetation, crops, housing, or water bodies (23–26).
Malnutrition and malaria
Malnutrition and malaria are both very common in young children in the area. The prevalence, determinants, and interactions between malaria and malnutrition have been studied in much detail in the Nouna area (27–31). Moreover, malaria control strategies through bed netting use, medicine effectiveness, and access to quality treatment have been investigated (21, 32–38).
Health-seeking behaviour
Another series of studies used data from a household sample that was randomly selected from all households within the HDSS. A representative sample of 800 households of the HDSS population was drawn in 2000 (39) and updated in 2003 to 990 households (40), which has been followed-up as a panel survey ever since (for a description of the survey design and questionnaires, see Würthwein 39, 41). The survey added in-depth information regarding perceived morbidity (acute and chronic illnesses), health-seeking behaviour, household expenditures, revenues and assets, and other socio-economic variables. In particular, the economic aspect of the local burden of disease and household response and attitude have been studied (42–44).
Evaluation of health care interventions
Another major goal of the HDSS has been to support the design and scientific evaluation of population- and service-based health care interventions such as the improvement of the quality of care provided (45), the establishment of home care for malaria (46), the implementation of community-based health insurance (42, 47–51), or the improvement of maternal and child care in the study area. Innovative designs, such as the step wedge cluster randomised sampling for the insurance intervention trial were implemented to capture intervention effects (40).
Discussion
It is no easy task to maintain a HDSS in developing countries. Financial constraints and, in many places, unstable conditions are among the major obstacles. Because there are few longitudinal studies in SSA achieving this long-term, ongoing project is therefore a major strength of the Nouna HDSS. As a continuous source of data for over 15 years, it provides a good basis for studies in all areas of health research. It provided a denominator for epidemiological studies by giving a precise estimate of the population by age and sex in the study area. Continuous basic demographic information with a trend towards key variables could be related to the already ongoing health intervention and to feedback for the local policy makers. It could also lead to new interventions for health or general development and the analysis could be extrapolated to the national level. Furthermore the introduction of VA has refined considerably the epidemiological toolkit regarding mortality data. The verbal autopsy method, however, is still a method with limited sensitivity and specificity. Automated systems like the INTERVA model (7) are currently in the test phase in the Nouna HDSS and may improve the comparability between different HDSS sites.
Another important aspect is that a structure has been put in place and data quality has improved over the years. With over a decade of experience in the area, it has also contributed to local capacity building along with the building of the physical infrastructure and establishment of electronic databases. The HDSS staff have received formal training (Msc, PhD) in epidemiology, public health, demography, biochemistry, and microbiology (molecular parasitology, molecular virology). Training on the job and short courses are also offered to keep the staff updated in various domains. Currently, the HDSS is widely contributing to the research training of scientists together with the local and abroad universities by hosting master and PhD students for their field activities. The CRSN has undergone profound changes over the past decades with staff, infrastructure, and equipment capacity strengthening that allow moving from a local centre to a national centre attractive to international funders.
The local population has benefited to some extent in terms of health services and economic activity. The CRSN is now the largest employer in the Nouna Health District. Overall, there is a good relationship between the study population and the researchers from Nouna HDSS. This is particularly supported by the staff recruitment policy in place that gives to local people. Currently, almost all the support staff and some senior staff are from the Nouna area. Ethical issues, with regard to long-term research, concern themselves with benefits that the communities get in exchange for their time for repeated interviews. This is balanced by the existence of ever-increasing intervention projects such as free ITN distribution, malaria drug studies with free treatment for participants, health insurance project, and so on from which the communities benefit directly. Additionally the CRSN has put a lot of emphasis on the Nouna hospital to improve the quality of care by providing good diagnosis tools, additional physicians, and subsidising health care fees for the communities.
Regarding weaknesses, interview fatigue from within the households visited every 3 to 4 months represents a challenge to the sustainability of the HDSS and data accuracy. Therefore, there has been a qualitative research project to assess the perceptions of the community on the HDSS activities and the field procedures that have been adapted accordingly. Furthermore, some of the senior researchers originate from the area, which has enabled them to always engage in constructive discussions with the communities for problems that arise.
Another difficulty is to keep track of evolving households with time. First, as the population grows and migrates, households are subject to divide, merge, or physically move. Second, household members may move from one household to another (for example, as young women marry). Such changes can lead to confusion and inaccuracies in the database. To help resolve these problems, the latest census done in 2009 has re-emphasised that individuals keep their ID regardless of household affiliation, has remapped households, and re-established member affiliation to the household. Thus, the ID is given only once and not subject to any change despite the change of residence. Currently, only the CRSN staff know the individuals' IDs and introducing ID card provisions to HDSS members will facilitate the process.
However, retrospective affiliation of members to households may be neither feasible nor desirable. The introduction of small field computers or PDAs at some point in the future may help tackle some of the issues by making data collection less burdensome and more accurate.
In summary, the Nouna HDSS population has been the sampling frame for many studies in all areas of health science. High-quality studies have been performed and are acknowledged by the scientific community. Maintaining high data quality is challenging, however reliable descriptive results have been obtained. The observed declining trend in mortality over the last 15 years in this rural area of Burkina Faso is positive.
The CRSN is one of the three research institutions belonging to the Ministry of Health (MoH) and directly link to the General secretariat of the MoH. All research activities conducted in Nouna are related to the national research priorities and therefore involve the authorities of the ministry of health. Furthermore, because of the close relationship between the Nouna district health team and the CRSN, intervention projects are first jointly discussed and then jointly implemented. The results of the drug trial conducted in Nouna were instrumental in the change of malaria treatment policy, the bed nets policy, and its distribution strategy in the country.
Acknowledgements
The authors wish to thank the individuals of the Nouna HDSS for their cooperation in this long-term project. Their willingness to participate in the regular survey and numerous studies is duly acknowledged recognising that without it the level of success reached by this enterprise could not have been achieved. We thank Peter Dambach for providing a map of the Nouna HDSS and Séraphin Simboro for supplying Geographical Information System (GIS) working material. We also thank the staff of the CRSN and the teams of field interviewers who participated in the field work over the years. Their hard work and dedication was and is key to the high quality research being done at the Nouna HDSS.
Supplementary Material.
Table S1.
Localities in the Nouna HDSS. In bold localities with a health facility (in parenthesis opening date)
| Date in HDSS | Name of Locality (opening date of health centre) |
|---|---|
| 1992 (39 villages) | Barakui, Biron Bobo, Biron Marka, Boron, Bouné, Bourasso (1956), Cissé, Dankoumana, Dembéléla, Denissa, Denissa Mossi, Diamasso, Dina, Dionkongo, Dokoura, Goni (2006), Kamadena (2008), Kèmena, Kodougou, Koro (1964), Labarani (2006), Leï, Lékuy (2003), Lémini, Nokui, Ouetté, Pâ, Sampopo, Sériba, Sien, Sikoro (2008), Sirakorosso, Sobon, Solimana (2009), Tèbèrè, Tissi, Toni (1991), Tonséré, Zanakuy, |
| 2000 (+2 villages + Nouna Town) | Bankoumani, Dara (1995), Nouna (Nouna district hospital, CSPSa in 2005), |
| 2004 (+17 villages) | Babekolon, Bagala (1994), Biron Badala, Bissau, Bouhuy, Damandigui, Hinkuy, Kamiakoro, Kansara, Kéréna, Konkuini, Korédougou, Moinsi, Mourdié (2008), Sèrè, Soin, Tonkoroni. |
aCSPS = Centre de Santé et de Promotion Sociale = basic health facility.
Conflict of interest and funding
This work was supported by the German Research Foundation (DFG) under research grant SFB 544.
References
- 1.Becher H, Kouyaté B. Berlin: Springer; 2005. Health research in developing countries a collaboration between Burkina Faso and Germany. [Google Scholar]
- 2.Anker M. The effect of misclassification error on reported cause-specific mortality fractions from verbal autopsy. Int J Epidemiol. 1997;26:1090–6. doi: 10.1093/ije/26.5.1090. [DOI] [PubMed] [Google Scholar]
- 3.Chandramohan D, Maude GH, Rodrigues LC, Hayes RJ. Verbal autopsies for adult deaths: their development and validation in a multicentre study. Trop Med Int Health. 1998;3:436–46. doi: 10.1046/j.1365-3156.1998.00255.x. [DOI] [PubMed] [Google Scholar]
- 4.Hammer GP, Kouyaté B, Ramroth H, Becher H. Risk factors for childhood mortality in sub-Saharan Africa. A comparison of data from a Demographic and Health Survey and from a Demographic Surveillance System. Acta Trop. 2006;98:212–8. doi: 10.1016/j.actatropica.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Würthwein R, Gbangou A, Sauerborn R, Schmidt CM. Measuring the local burden of disease. A study of years of life lost in sub-Saharan Africa. Int J Epidemiol. 2001;30:501–8. doi: 10.1093/ije/30.3.501. [DOI] [PubMed] [Google Scholar]
- 6.Chandramohan D, Setel P, Quigley M. Effect of misclassification of causes of death in verbal autopsy: can it be adjusted? Int J Epidemiol. 2001;30:509–14. doi: 10.1093/ije/30.3.509. [DOI] [PubMed] [Google Scholar]
- 7.Byass P, Huong DL, Minh HV. A probabilistic approach to interpreting verbal autopsies: methodology and preliminary validation in Vietnam. Scand J Public Health Suppl. 2003;62:32–7. doi: 10.1080/14034950310015086. [DOI] [PubMed] [Google Scholar]
- 8.INDEPTH-Network. Ottawa: International Development Research Centre; 2002. Population and health in developing countries – Population, Health, and Survival at INDEPTH sites. [Google Scholar]
- 9.Kynast-Wolf G, Sankoh OA, Gbangou A, Kouyaté B, Becher H. Mortality patterns, 1993–98, in a rural area of Burkina Faso, West Africa, based on the Nouna demographic surveillance system. Trop Med Int Health. 2002;7:349–56. doi: 10.1046/j.1365-3156.2002.00863.x. [DOI] [PubMed] [Google Scholar]
- 10.Becher H, Mueller O, Jahn A, Gbangou A, Kynast-Wolf G, Kouyaté B. Risk factors of infant and child mortality in rural Burkina Faso. Bull World Health Organ. 2004;82:265–73. [PMC free article] [PubMed] [Google Scholar]
- 11.Sauerborn R, Ibrango I, Nougtara A, Borchert M, Hien M, Benzler J, et al. The economic costs of illness for rural households in Burkina Faso. Trop Med Parasitol. 1995;46:54–60. [PubMed] [Google Scholar]
- 12.Sauerborn R, Adams A, Hien M. Household strategies to cope with the economic costs of illness. Soc Sci Med. 1996;43:291–301. doi: 10.1016/0277-9536(95)00375-4. [DOI] [PubMed] [Google Scholar]
- 13.Sauerborn R, Nougtara A, Hien M, Diesfeld HJ. Seasonal variations of household costs of illness in Burkina Faso. Soc Sci Med. 1996;43:281–90. doi: 10.1016/0277-9536(95)00374-6. [DOI] [PubMed] [Google Scholar]
- 14.Sankoh OA, Yé Y, Sauerborn R, Mueller O, Becher H. Clustering of childhood mortality in rural Burkina Faso. Int J Epidemiol. 2001;30:485–92. doi: 10.1093/ije/30.3.485. [DOI] [PubMed] [Google Scholar]
- 15.Becher H, Kynast-Wolf G, Sié A, Ndugwa R, Ramroth H, Kouyaté B, et al. Patterns of malaria: cause-specific and all-cause mortality in a malaria-endemic area of west Africa. Am J Trop Med Hyg. 2008;78:106–13. [PubMed] [Google Scholar]
- 16.Kynast-Wolf G, Hammer GP, Mueller O, Kouyaté B, Becher H. Season of death and birth predict patterns of mortality in Burkina Faso. Int J Epidemiol. 2006;35:427–35. doi: 10.1093/ije/dyi150. [DOI] [PubMed] [Google Scholar]
- 17.Ndugwa RP, Ramroth H, Mueller O, Jasseh M, Sié A, Kouyaté B, et al. Comparison of all-cause and malaria-specific mortality from two West African countries with different malaria transmission patterns. Malar J. 2008;7:15. doi: 10.1186/1475-2875-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baltussen RM, Sanon M, Sommerfeld J, Würthwein R. Obtaining disability weights in rural Burkina Faso using a culturally adapted visual analogue scale. Health Econ. 2002;11:155–63. doi: 10.1002/hec.658. [DOI] [PubMed] [Google Scholar]
- 19.Akunne AF, Bridges JF, Sanon M, Sauerborn R. Comparison of individual and group valuation of health state scenarios across communities in West Africa. Appl Health Econ Health Policy. 2006;5:261–8. doi: 10.2165/00148365-200605040-00007. [DOI] [PubMed] [Google Scholar]
- 20.Mueller O, Becher H, van Zweeden AB, Yé Y, Diallo DA, Konaté AT, et al. Effect of zinc supplementation on malaria and other causes of morbidity in west African children: randomised double blind placebo controlled trial. BMJ. 2001;322:1567. doi: 10.1136/bmj.322.7302.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mueller O, Traoré C, Kouyaté B, Yé Y, Frey C, Coulibaly B, et al. Effects of insecticide-treated bednets during early infancy in an African area of intense malaria transmission: a randomized controlled trial. Bull World Health Organ. 2006;84:120–6. doi: 10.2471/blt.05.023150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yamamoto S, Louis VR, Sié A, Sauerborn R. Household risk factors for clinical malaria in a semi-urban area of Burkina Faso: a case-control study. Trans R Soc Trop Med Hyg. 2009;104:61–5. doi: 10.1016/j.trstmh.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 23.Dambach P, Sié A, Lacaux JP, Vignolles C, Machault V, Sauerborn R. Using high spatial resolution remote sensing for risk mapping of malaria occurrence in the Nouna district, Burkina Faso. Glob Health Action. 2009:2. doi: 10.3402/gha.v2i0.2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yé Y, Hoshen M, Louis V, Séraphin S, Traoré I, Sauerborn R. Housing conditions and plasmodium falciparum infection: protective effect of iron-sheet roofed houses. Malar J. 2006;5:8. doi: 10.1186/1475-2875-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yé Y, Hoshen M, Kyobutungi C, Louis VR, Sauerborn R. Local scale prediction of Plasmodium falciparum malaria transmission in an endemic region using temperature and rainfall. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yé Y, Kyobutungi C, Louis VR, Sauerborn R. Micro-epidemiology of plasmodium falciparum malaria: is there any difference in transmission risk between neighbouring villages? Malar J. 2007;6:46. doi: 10.1186/1475-2875-6-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Benzler J, Sauerborn R. Rapid risk household screening by neonatal arm circumference: results from a cohort study in rural Burkina Faso. Trop Med Int Health. 1998;3:962–74. doi: 10.1046/j.1365-3156.1998.00340.x. [DOI] [PubMed] [Google Scholar]
- 28.Mueller O, Traoré C, Jahn A, Becher H. Severe anaemia in west African children: malaria or malnutrition? Lancet. 2003;361:86–7. doi: 10.1016/S0140-6736(03)12154-X. [DOI] [PubMed] [Google Scholar]
- 29.Mueller O, Garenne M, Reitmaier P, van Zweeden AB, Kouyaté B, Becher H. Effect of zinc supplementation on growth in West African children: a randomized double-blind placebo-controlled trial in rural Burkina Faso. Int J Epidemiol. 2003;32:1098–102. doi: 10.1093/ije/dyg190. [DOI] [PubMed] [Google Scholar]
- 30.Beiersmann C, Sanou A, Wladarsch E, De AM, Kouyaté B, Mueller O. Malaria in rural Burkina Faso: local illness concepts, patterns of traditional treatment and influence on health-seeking behaviour. Malar J. 2007;6:106. doi: 10.1186/1475-2875-6-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mueller O, Garenne M, Kouyaté B, Becher H. The association between protein-energy malnutrition, malaria morbidity and all-cause mortality in West African children. Trop Med Int Health. 2003;8:507–11. doi: 10.1046/j.1365-3156.2003.01043.x. [DOI] [PubMed] [Google Scholar]
- 32.Mandi G, Mockenhaupt FP, Coulibaly B, Meissner P, Mueller O. Efficacy of amodiaquine in the treatment of uncomplicated falciparum malaria in young children of rural north-western Burkina Faso. Malar J. 2008;7:58. doi: 10.1186/1475-2875-7-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meissner PE, Mandi G, Mockenhaupt FP, Witte S, Coulibaly B, Mansmann U, et al. Marked differences in the prevalence of chloroquine resistance between urban and rural communities in Burkina Faso. Acta Trop. 2008;105:81–6. doi: 10.1016/j.actatropica.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 34.Mueller O, Traoré C, Becher H, Kouyaté B. Malaria morbidity, treatment-seeking behaviour, and mortality in a cohort of young children in rural Burkina Faso. Trop Med Int Health. 2003;8:290–6. doi: 10.1046/j.1365-3156.2003.01030.x. [DOI] [PubMed] [Google Scholar]
- 35.Mueller O, Razum O, Traoré C, Kouyaté B. Community effectiveness of chloroquine and traditional remedies in the treatment of young children with falciparum malaria in rural Burkina Faso. Malar J. 2004;3:36. doi: 10.1186/1475-2875-3-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mueller O, De Allegri M, Becher H, Tiendrebéogo J, Beiersmann C, Yé M, et al. Distribution systems of insecticide-treated bed nets for malaria control in rural Burkina Faso: cluster-randomized controlled trial. PLoS ONE. 2008;3:e3182. doi: 10.1371/journal.pone.0003182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tipke M, Diallo S, Coulibaly B, Storzinger D, Hoppe-Tichy T, Sié A, et al. Substandard anti-malarial drugs in Burkina Faso. Malar J. 2008;7:95. doi: 10.1186/1475-2875-7-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tipke M, Louis VR, Yé M, De AM, Beiersmann C, Sié A, et al. Access to malaria treatment in young children of rural Burkina Faso. Malar J. 2009;8:266. doi: 10.1186/1475-2875-8-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Würthwein R. Measuring the burden of disease, the structure of income, and returns to education in rural West Africa. Heidelberg: Heidelberg University; 2002. [Google Scholar]
- 40.De Allegri M, Pokhrel S, Becher H, Dong H, Mansmann U, Kouyate B, et al. Step-wedge cluster-randomised community-based trials: an application to the study of the impact of community health insurance. Health Res Policy Syst. 2008;6:10. doi: 10.1186/1478-4505-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Würthwein R, Gbangou A, Kouyaté B, Mugisha F, Yé Y, Becher H, et al. The Nouna health district household survey – design and implementation. SFB 544: control of tropical infectious diseases. Heidelberg. 2001. pp. 1–41. Available from: http://www.klinikum.uni-heidelberg.de/fileadmin/inst_hygiene/tropenhygiene/PDF/HealthSystems/Discussionpaper_3_2001_wuerthwein.pdf [cited 16 August 2010]
- 42.De Allegri M, Sanon M, Sauerborn R. “To enrol or not to enrol?”: a qualitative investigation of demand for health insurance in rural West Africa. Soc Sci Med. 2006;62:1520–7. doi: 10.1016/j.socscimed.2005.07.036. [DOI] [PubMed] [Google Scholar]
- 43.De Allegri M, Kouyate B, Becher H, Gbangou A, Pokhrel S, Sanon M, et al. Understanding enrolment in community health insurance in sub-Saharan Africa: a population-based case-control study in rural Burkina Faso. Bull World Health Organ. 2006;84:852–8. doi: 10.2471/blt.06.031336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sauerborn R, Gbangou A, Dong H, Przyborski JM, Lanzer M. Willingness to pay for hypothetical malaria vaccines in rural Burkina Faso. Scand J Public Health. 2005;33:146–50. doi: 10.1080/14034940510005743. [DOI] [PubMed] [Google Scholar]
- 45.Pfeiffer K, Somé F, Mueller O, Sié A, Kouyaté B, Haefeli WEO, et al. Clinical diagnosis of malaria and the risk of chloroquine self-medication in rural health centres in Burkina Faso. Trop Med Int Health. 2008;13:418–26. doi: 10.1111/j.1365-3156.2008.02017.x. [DOI] [PubMed] [Google Scholar]
- 46.Kouyaté B, Somé F, Jahn A, Coulibaly B, Eriksen J, Sauerborn R, et al. Process and effects of a community intervention on malaria in rural Burkina Faso: randomized controlled trial. Malar J. 2008;7:50. doi: 10.1186/1475-2875-7-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.De Allegri M, Pokhrel S, Sauerborn R. Health financing and access to services. Lancet. 2005;365:569–70. doi: 10.1016/S0140-6736(05)17898-2. [DOI] [PubMed] [Google Scholar]
- 48.Gnawali DP, Pokhrel S, Sié A, Sanon M, De Allegri M, Souares A, et al. The effect of community-based health insurance on the utilization of modern health care services: evidence from Burkina Faso. Health Policy. 2009;90:214–22. doi: 10.1016/j.healthpol.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 49.Dong H, Mugisha F, Gbangou A, Kouyaté B, Sauerborn R. The feasibility of community-based health insurance in Burkina Faso. Health Policy. 2004;69:45–53. doi: 10.1016/j.healthpol.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 50.Dong H, Kouyaté B, Cairns J, Sauerborn R. Differential willingness of household heads to pay community-based health insurance premia for themselves and other household members. Health Policy Plan. 2004;19:120–6. doi: 10.1093/heapol/czh014. [DOI] [PubMed] [Google Scholar]
- 51.Dong H, De Allegri M, Gnawali D, Souares A, Sauerborn R. Drop-out analysis of community-based health insurance membership at Nouna, Burkina Faso. Health Policy. 2009;92:174–9. doi: 10.1016/j.healthpol.2009.03.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Localities in the Nouna HDSS. In bold localities with a health facility (in parenthesis opening date)
| Date in HDSS | Name of Locality (opening date of health centre) |
|---|---|
| 1992 (39 villages) | Barakui, Biron Bobo, Biron Marka, Boron, Bouné, Bourasso (1956), Cissé, Dankoumana, Dembéléla, Denissa, Denissa Mossi, Diamasso, Dina, Dionkongo, Dokoura, Goni (2006), Kamadena (2008), Kèmena, Kodougou, Koro (1964), Labarani (2006), Leï, Lékuy (2003), Lémini, Nokui, Ouetté, Pâ, Sampopo, Sériba, Sien, Sikoro (2008), Sirakorosso, Sobon, Solimana (2009), Tèbèrè, Tissi, Toni (1991), Tonséré, Zanakuy, |
| 2000 (+2 villages + Nouna Town) | Bankoumani, Dara (1995), Nouna (Nouna district hospital, CSPSa in 2005), |
| 2004 (+17 villages) | Babekolon, Bagala (1994), Biron Badala, Bissau, Bouhuy, Damandigui, Hinkuy, Kamiakoro, Kansara, Kéréna, Konkuini, Korédougou, Moinsi, Mourdié (2008), Sèrè, Soin, Tonkoroni. |
aCSPS = Centre de Santé et de Promotion Sociale = basic health facility.