Rates of sexually transmitted diseases (STDs) in China have soared over the past decade.1,2 Effective management of STDs is one of the cornerstones of HIV control and provides a unique opportunity for targeted education about HIV prevention.3,4
A recent study in Thailand revealed that 60% of patients suffering from an STD did not seek treatment from an STD clinic.5 To reach STD patients, it is important to determine the venues where people seek services and to evaluate the quality of treatment and prevention services in those facilities. The objectives of this study were to identify the facilities in Beijing where most people seek STD treatment and evaluate their prevention services.
The study was conducted in Chao Yang District, Beijing, where only large and moderate-sized hospitals are authorized to provide STD treatment.
Chao Yang District is 30% urban and 70% suburban/rural. There are 1.49 million residents, of whom 12.6% are farmers and 874,000 are migrants. The majority of the population and the large hospitals and other resources are concentrated in the smaller central and northwestern parts of Chao Yang.
A cross-sectional study was conducted from November to December 2002 among a sample of each type of STD treating facility. A stratified random sampling method was used to select the sample from the total of 48 comprehensive hospitals. Random samples of 2 of the 3 large hospitals, 5 of the 9 moderate-sized hospitals, and 10 of the 36 small hospitals were selected. In the large and moderate-sized hospitals, the departments providing STD services included dermatovenereology, gynecology, and urology; in the small hospitals, the departments included surgery and gynecology. Information was reviewed and records abstracted from logbooks. The numbers of people diagnosed with urethritis, epididymitis, cervicitis, or pelvic inflammatory disease were recorded. All patients from the STD Center were included.
Seven pharmacies were randomly selected. Pharmacy clerks asked all people purchasing antibiotics, podophyllotoxin tincture, or acyclovir whether it was for treating a STD. Attendees admitting genital symptoms or refusing to answer the questions were referred to the research team. After consenting, they completed a self-administered questionnaire.
In each study department of the sampled hospitals, the proportion of the diagnosed STD patients was calculated by dividing the number of diagnosed STD patients by the total number of patients seen in that department. The number of STD patients in the study department in all hospitals in that category was estimated by multiplying the proportion of diagnosed STD patients in the sampled hospitals by the total number of patients seen in the corresponding departments in all hospitals in that category in Chao Yang, assuming the proportion of the diagnosed STD patients in the study hospitals was representative for all the hospitals. The sum of the estimated diagnosed STD cases in all the study departments was considered to be the total number of diagnosed STD patients in all the large hospitals in Chao Yang. The total number of people seeking STD treatment in moderate-sized and small hospitals was estimated using the same method.
In the sampled pharmacies, the average number of people seeking treatment was estimated by dividing the total number of people seeking STD treatment in the sampled pharmacies by the number of days pharmacies were operating during the study period. The number of people seeking STD-related treatment in all pharmacies for the study month was extrapolated by multiplying the average number of people self-treating each pharmacy day multiplied by 195 (number of pharmacies) multiplied by 30 (number of study days), assuming that the average number was similar at all pharmacies during the study month. The sum of the estimated numbers of people seeking STD treatment in the 3 types of facilities was considered to be the total number of people seeking STD treatment in the study month. The distribution per type of facility was the estimated number of people seeking STD treatment in that type of facility over the estimated total number of STD patients in the study period. The reporting fraction was estimated by dividing the number of STD cases reported to the health department by the estimated total number of STD patients from various types of clinical settings. The proportion providing STD education was calculated by dividing the number of sampled facilities providing STD education by the total sample of facilities of its type. All statistical analyses were performed with STATA (version 7; Stata-Corp LP, College Station, TX), using a survey data analysis procedure.
The study was approved by the institutional review boards of the University of California, Los Angeles, and the China Center for Disease Control and Prevention.
“Diagnosed STD cases” was defined as first-time patients diagnosed with syphilis, gonorrhea, nongonococcal urethritis (NGU), genital warts, genital herpes, chancroid, or lymphogranuloma venereum.
The mean proportion of diagnosed STD cases, total number of attendees, estimated numbers of diagnosed STD cases, and proportion seen in each type of facility are presented in Table 1. The highest proportion of STD cases seen at medical facilities was in the dermatology departments of moderate-sized hospitals. Small hospitals that are not authorized to treat STDS saw 22% of the total.
TABLE 1.
Distribution of Diagnosed STD Cases in the Various Departments in Hospitals
| Hospital Type and Study Departments |
Mean Proportion of Diagnosed STD Cases Among Department Attendees (1/1,000) |
No. Total Attendees in the Department |
Estimate of Diagnosed STD Cases in All Hospitals |
95% CI of the Estimates |
|---|---|---|---|---|
| STD center | — | 176 | 176 (14%)* | — |
| Large hospital | ||||
| Dermatology | 8.7 | 19,578 | 170 (14%) | 164–176 |
| Gynecology | 4.7 | 17,890 | 84 (7%) | 81–89 |
| Urology | 5.7 | 8,338 | 47 (4%) | 47–48 |
| Moderate-sized hospital | ||||
| Dermatology | 30.3 | 1,3,207 | 400 (33%) | 375–425 |
| Gynecology | 2.5 | 17,900 | 45 (4%) | 43–47 |
| Urology | 6.3 | 4,370 | 28 (2%) | 21–35 |
| Small hospital | ||||
| Surgery | 9.7 | 13,071 | 127 (10%) | 107–148 |
| Gynecology | 10.0 | 14,262 | 143 (12%) | 101–183 |
Percentage of total seen in medical facilities.
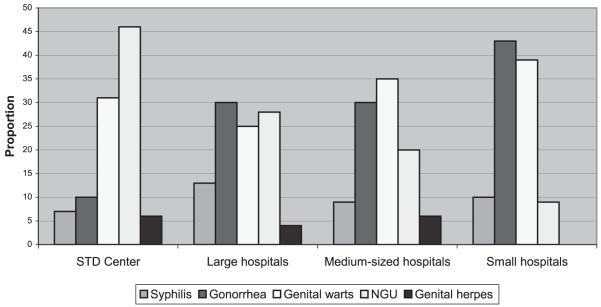
As shown in Figure 1, 10% and 46% of all diagnosed STDs cases were gonorrhea and NGU, respectively. In the hospitals, gonorrhea accounted for more than 30% and NGU for less than 30% of all diagnosed STD cases. In the small hospitals, no genital herpes was diagnosed, and gonorrhea and genital warts were the most frequently diagnosed STDs (Fig. 1). A higher proportion of NGUs was diagnosed in the STD Center and departments of dermatovenereology. A higher proportion of gonorrhea was diagnosed in the departments of urology in large and moderate-sized hospitals and in the departments of surgery in small hospitals. Fewer genital wart cases were diagnosed in the departments of urology (data not shown).
Fig. 1.
Proportion of different types of STDs diagnosed in the sampled clinical settings.
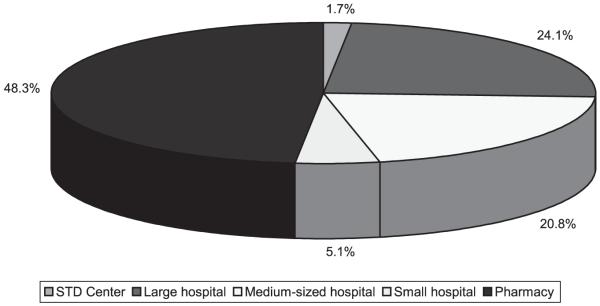
During the study month, the estimated total seeking treatment was 10,525. Just over 48% [95% confidence interval (CI), 35.5%–61.1%] sought treatment at pharmacies, 24.1% (95% CI 18.0%–30.2%) at large hospitals, 20.8% (95% CI 9.0%–32.6%) at moderate-sized hospitals, 5.1% (95% CI 3.8%–6.4%) at small hospitals, and 1.7% (95% CI 1.3%–2.1%) at the STD Center (Fig. 2). At hospitals, 18.7% of patients sought STD treatment in departments of dermatovenereology, 13.4% in departments of gynecology, and 15.3% in departments of urology. Only 39% of patients sought STD diagnosis and treatment in the authorized STD treatment facilities.
Fig. 2.
Distribution of people seeking STD services in various types of facilities.
During the study month, the estimated number of diagnosed STD cases in the clinical settings was 1220. Of these, 421 were reported, which was 34.5% of reportable STDs estimated in our study. If probable STD cases were also counted, the total would have been 5084, and the proportion of STD cases officially reported would drop to 8.3%.
During the study period, we also investigated provision of STD prevention services. Only the STD Center and dermatovenerology departments within the hospitals provided prevention services, including posters, leaflets, and a counseling room in the STD Center. In dermatovenerology departments, only 75% had posters, 33% had leaflets, and there were no counseling rooms available in any of the hospitals. There were no prevention services in the other facilities.
The restriction policy authorizing only large and moderate-sized hospitals limits the accessibility for treatment of STDs. To control STDs in the AIDS era, high-quality STD services should be decentralized and made widely available, even in rural health facilities that do not have appropriate laboratory facilities.
Serious underreporting of STD cases will mislead the government and society as to the magnitude of the problem and hides the potential for an AIDS epidemic through sexual transmission. Thus, there is a need for China to reconsider its policy on providing treatment for STDs.
Those seeking STD treatment provide a “teachable opportunity” to prevent further spread of these diseases, but this study indicated that no counseling was provided in any of the facilities. Posters and pamphlets were the only simple methods of health education in the authorized STD treatment facilities. To control the spread of STDs and AIDS, the Chinese government should mandate counseling services to everyone seeking STD services.
There were several limitations to this study. The number of STD cases in the small hospitals might be underreported. The definition of patients seeking STD treatment in the clinical settings and pharmacies differed. The numbers of sampled small hospitals and pharmacies were relatively small. Three private clinics claiming to treat STDs in rural Chao Yang refused to participate in the research. Most of these limitations would lead to underreporting of STD patients in unauthorized facilities and pharmacies. Thus, our results probably overestimate the proportion of STD patients seen in the authorized STD facilities and underestimate the proportions who receive inadequate STD treatment in pharmacies and unauthorized clinical facilities in Beijing. Although neither our sample nor Chao Yang is typical of China, it is probable that many of the problems with STD care and treatment-seeking observed in Chao Yang are also occurring in other parts of China.
Acknowledgments
This study was supported by NIH Fogarty International Center grant D43 TW000013 (R.D.).
References
- 1.Report on STD epidemic from national STD surveillance system in 2000. Chin J Prevent Control STD AIDS. 2001;7(suppl):192–194. [Google Scholar]
- 2.Chen Z-Q, Zhang G-C, Gong X-D, et al. Syphilis in China: Results of a national survey. Lancet. 2007;369:132–138. doi: 10.1016/S0140-6736(07)60074-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garnett GP, Anderson RM. Strategies for limiting the spread of HIV in developing countries: Conclusions based on studies of the transmission dynamics of the virus. J AIDS. 1994;9:500–513. [PubMed] [Google Scholar]
- 4.Over M, Piot P. Human immunodeficiency virus infection and other sexually transmitted diseases in developing countries: Public health importance and priorities for resource allocation. J Infect Dis. 1996;174(suppl 2):S162–S175. doi: 10.1093/infdis/174.supplement_2.s162. [DOI] [PubMed] [Google Scholar]
- 5.Prempree P, Detels R, Ungkasrithongkul M, et al. The sources of treatment of sexually transmitted infections in a rural community in central Thailand. Sex Health. 2007;4:17–19. doi: 10.1071/sh06035. [DOI] [PubMed] [Google Scholar]