Abstract
Total scalp avulsion is a rare but potentially devastating injury that when treated (following a few basic principles) can have very good reconstructive results. The present article reviews the current literature and describes the steps involved in the successful replantation of a complete avulsed scalp of a 33-year-old woman. To the authors’ knowledge, the present case regarding replantation of a complete avulsed scalp using only a single artery is the first to be described in the Canadian literature.
Keywords: Scalp avulsion, Scalp replantation
Abstract
L’avulsion totale du cuir chevelu est un traumatisme rare au potentiel dévastateur qui, lorsqu’elle est traitée conformément à quelques principes fondamentaux, peut donner de très bons résultats en chirurgie de reconstruction. Le présent article contient une analyse des publications à jour et décrit les étapes utilisées pour réimplanter avec succès une avulsion complète du cuir chevelu chez une femme de 33 ans. À la connaissance des auteurs, le présent cas portant sur la réimplantation d’une avulsion complète du cuir chevelu au moyen d’une seule artère est le premier à être décrit dans les publications canadiennes.
Avulsion of the scalp most commonly results from the entrapment of long hair in high-speed rotary parts of industrial machinery, although it has also occurred as a result of dogbites and assaults (1,2). Although there is tremendous variability seen in the patterns of avulsion for sharp force and animal attack scalpings, there is very little variability seen in the patterns of industrial scalpings, which tend to follow similar lines of least resistance along the insertions of the frontalis and temporalis muscles anteriorly, and the occipitalis muscle posteriorly (3–5). When tearing through the skin above these insertions, the avulsed portion may include the eyebrows as well as all or part of the ears. The deep plane of cleavage is generally through the loose connective tissue between the galea aponeurotica and the periosteum, although it does occasionally include part or all of the periosteum. Because it is a rare and disfiguring occurrence, numerous methods have been described over the years with respect to the acute management of this injury as well as secondary reconstruction of the defects. Before the advent of microsurgical techniques, acute management of an avulsed scalp typically involved simply replacing the avulsed portion as a free graft and suturing it back in place (6,7). This technique generally had poor results with the exception of one case involving a partially avulsed scalp of a child as described by Lu (7) in 1969.
Microvascular replantation of an avulsed scalp was first described by Miller et al (8) in 1976, when both superficial temporal arteries along with five veins were reanastomosed successfully. Since this procedure, many avulsed scalps, both partial and complete, have been replanted successfully using a widely variable number of arteries and veins – the vast majority using two or more arteries and as many veins as possible (8–10). One consistent finding in these replanted scalps has been postoperative congestion in the occipital region (3,8,9,11–14); various methods have been attempted to control this including decreasing the number of arteries reanastomosed to increase the vein-to-artery ratio (11) as well as the use of leeches postoperatively (15). Although most articles still seem to highlight their authors’ attempts at reanastomosing as many vessels as possible, many articles have demonstrated that a scalp (even including up to two-thirds of the face [16]) can be successfully replanted using as few as one artery and one vein (11,16). A consistent point that most authors seem to agree on, however, is that if more veins are viable, then at least two veins should be used to decrease the incidence of venous congestion that results from the excellent arterial reperfusion. We present a case of total scalp avulsion to highlight some of the aforementioned treatment and outcome issues. Despite the increasing number of publications describing scalp replantation after traumatic avulsion, there has not yet been a case reported in Canada in which a scalp has been replanted using vascular repair. To the authors’ knowledge, the present case regarding replantation of a complete avulsed scalp using only a single artery is the first to be described in the Canadian literature.
CASE PRESENTATION
A 33-year-old woman presented to the hospital with a complete avulsed scalp after catching her hair in the rollers of a paper manufacturing machine. The laceration extended across both supratarsal folds into the temporal region bilaterally, including the eyebrows. The frontalis muscle had been torn as had the right temporal branch of the facial nerve. The laceration extended bilaterally across the helical roots, including the post-auricular skin in the flap, then continued behind the mastoids onto the neck and completed the avulsion at the level of C6 – a total laceration length of approximately 35 cm (Figures 1 and 2). The laceration in the occipital portion extended obliquely through the subcutaneous and dermal layers, leaving a very thin area of the flap that had also been crushed in the rolling machine.
Figure 1).
Avulsed scalp flap on side table before preparation for replantation
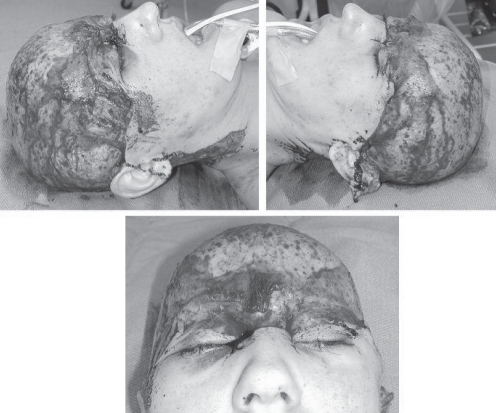
Figure 2).
Anterior, left and right lateral views of the zone of injury
The patient was brought to the operating room with the scalp wrapped in saline-soaked gauze and placed on ice, and the hair was then cut on the back table. Under loop magnification, the superficial temporal arteries and veins were identified on the scalp first and then on the patient. It was believed that the anterior branch of the right superficial temporal artery was the least damaged; consequently, it was dissected proximally in the patient and distally in the flap to mobilize as much length as possible for the reanastomosis. The temporal veins were mobilized bilaterally. The vessels were then cut back beyond the zones of injury, cleaned of any loose adventitia and placed in the microclamp. Under microscopic magnification, the right superficial temporal artery was reanastomosed in a back-to-front fashion using 10-0 nylon microsutures. Once the clamp was removed, there was good flow across the anastomosis; however, this revealed a tear in the intima distally that was not previously visible and the vessel was reclamped. The distal portion was trimmed beyond the intimal tear, a second anastomosis was performed and good flow was achieved (Figure 3). The scalp was then tacked into place and the right, then left, temporal veins were anastomosed in a similar manner to the artery. Good flow was noted throughout the scalp; however, venous congestion was noted in the occipital area that had been more severely traumatized and, due to the crush, had no veins available for reanastomosis. Because there was good flow to the area, it was decided not to debride any tissue at this time.
Figure 3).
Microvascular reanastomoses of the right superficial temporal artery and vein
The flap was then aligned into its anatomical position and the frontalis muscle, which had been torn, was then sutured using 4-0 polysorb sutures. Because of the local edema and trauma, it was impossible to adequately identify the avulsed temporal branch of the facial nerve for repair. The skin closure was then completed circumferentially and the perfusion reassessed and found to be adequate throughout the scalp, with the exception of the slightly sluggish and congested area at the occiput. The total ischemic time was 9 h.
The scalp remained well perfused through the patient’s six-day hospital stay and, despite the congestion in the occipital area, the tissue appeared to be viable. At three-week follow-up, however, the occipital tissue had become nonviable and required a debridement and split-thickness skin graft for coverage. Nine months postoperatively, there was some residual scarring at the nape of the neck and in the right upper eyelid that required simple excision, as well as some scar webbing in the lateral nasal region bilaterally that required z-plasty lengthening. At nine months, the patient had progressed to a full recovery of her frontalis function (Figure 4).
Figure 4).
Nine-month postoperative results showing area of alopecia on occiput, and eyebrow elevation demonstrating frontalis function
At two years postinjury, the patient requested a secondary reconstruction for the alopecia in the occipital area that had been skin grafted. This was corrected using a 500 mL skin expander, with later excision of the affected tissue and closure with a rotation advancement flap.
DISCUSSION
Scalp replantation is a relatively rare occurrence and, therefore, many trainees may not have the opportunity to encounter such a case during residency. Although there is no consensus on the number of vessels to anastomose to ensure viability, the present case highlights the principles of scalp replantation for these challenging cases. The first step in replanting an avulsed scalp is its preparation for microsurgery by either cutting or shaving the hair. One problem described frequently in the literature is the presence of hair on the underside of the scalp, requiring extensive and tedious cleaning and irrigation – this was certainly an issue with our case. One recommendation made by Sabapathy et al (17) was the use of a sterile bucket on which to place the scalp while shaving it to recreate its natural convex shape, allowing the hair to rinse off the scalp without becoming attached to the underside of the galea.
Once the scalp has been cleaned of hair, the next step is the preparation of the vessels for reanastomosis. Because there is often severe trauma to the vessels within the zone of injury (requiring a significant amount of length to be cut back), many authors have recommended the use of interposed vein grafts when replanting the scalp to provide adequate length for a tension-free anastomosis (9,10,18,19). While this certainly increases the length of the vessels, making for an easier anastomosis, it also has the drawbacks of doubling the number of anastomoses that can leak, clot or fail during the postoperative period; creating surgical complications in the area of harvest; and increasing ischemia time due to the time required for harvest, preparation and the extra anastomoses. While the first two issues can be mitigated by good surgical technique, to minimize operative time, Cheng et al (10) have even gone so far as to recommend having two surgical teams operating simultaneously, placing vein grafts on the arteries in the patient and onto the veins in the scalp. The fact that the right superficial temporal artery in the present case had to be cut back not only once, but twice, to remove the entire zone of injury, yet was still anastomosed without tension and without autologous vein graft, demonstrates that adequate mobilization of the vessels is certainly feasible and preferable to vein grafting. Furthermore, because we successfully replanted the scalp using only one artery and two veins, and other studies have used even fewer vessels (3,11,13,20), one need only find a single artery that can be mobilized sufficiently for a tension-free anastomosis to provide a viable replant. This too reduces the likelihood of needing a vein graft. Although single vein anastomoses have been described with excellent survival, because failure in these replants is overwhelmingly due to venous congestion, it is recommended to use a minimum of two veins. Finally, in cases in which the scalp seems so traumatized that no viable arteries are available, the use of an arterial-venous anastomosis has been described (21); thus giving the surgeon the leeway to choose the most easily mobilized vessels for the anastomoses.
Finally, once the scalp has been successfully replanted, close monitoring is required because it is not uncommon for portions of the scalp to become congested and/or necrotic in the postoperative period. One very common location for postoperative necrosis to occur is in the area of the occiput, as in our case (3,9,11–14). Although we believe that our case was more likely related to the crush injury sustained by the flap in that specific area, the majority of reported cases of occipital failure seem to be due to postoperative venous congestion (11,13,14). This is likely a result of two factors: the small calibre of the occipital vessels and the difficulty in finding and using them in the anastomosis – particularly in this case due to the crush – and the gravitational dependence of the area. We believe this specific complication can be lessened by spending more effort to use at least one of the occipital veins to enable drainage. Unfortunately, due to the most common mechanism of injury – the occipital hair being caught in a rotary part of an industrial machine – the occipital scalp is often crushed and devoid of usable vessels, as was in the present case (11).
Finally, with regard to the length of ischemic time an avulsed flap can withstand and still remain viable, there is wide variation in the literature. Although there is no study that has described the precise length of time a scalp can survive, it has been demonstrated that a scalp can withstand up to 17 h of warm ischemia time (22) and up to 24 h of cold ischemia time (23) and still be successfully replanted. Of course, no one will disagree that the less time an avulsed flap spends unperfused, the better the chance of a positive outcome.
CONCLUSION
Avulsion of the scalp is a relatively uncommon occurrence; however, when it does occur, it is most frequently due to the entanglement of long hair in a high-speed rotary machine. Before the advent of microsurgery, the standard of care for these types of injuries was generally to treat the scalp as a free graft and simply replace it. Following Miller et al’s (8) successful microvascular replantation of an avulsed scalp in 1976, it has become the standard of care to do so whenever possible. Since that time, much debate has centred on how long a scalp can remain viable while ischemic, how many vessels should be reanastomosed and whether interpositional vein grafts should be used. A careful review of the literature reveals that although there is no consensus, several commonly accepted principles of treatment emerge:
Microvascular replantation should be attempted even in cases of prolonged ischemic time;
Careful cleaning and preparation of the scalp will help avoid the inclusion of hair and debris on the underside of the flap;
One artery is all that is necessary for successful reperfusion, and it should be maximally mobilized to avoid vein graft; and
One should attempt to reanastomose at least two veins, ideally one in the occiput, to avoid the common complication of venous congestion.
This type of injury is relatively rare and there is no consensus regarding its management. If one follows the simple principles we have outlined, then there is every reason to expect a successful outcome to this devastating injury.
Acknowledgments
All work originated from Sunnybrook Health Sciences Centre, Toronto, Ontario.
REFERENCES
- 1.Yin JW, Matsuo JMS, Hsieh CH, et al. Replantation of total avulsed scalp with microsurgery: Experience of eight cases and literature review. J Trauma. 2008;64:796–802. doi: 10.1097/TA.0b013e3180341fdb. [DOI] [PubMed] [Google Scholar]
- 2.Ozek C, Guner U, Bilkay U, Alper M, Akin Y, Cagdas A. Superficial scalp necrosis after replantation. Ann Plast Surg. 2001;46:197–8. doi: 10.1097/00000637-200102000-00031. [DOI] [PubMed] [Google Scholar]
- 3.Borenstein A, Yaffe B, Seidman DS, Tsur H. Microsurgical replantation of two totally avulsed scalps. Isr J Med Sci. 1990;26:442–5. [PubMed] [Google Scholar]
- 4.Kaplan HY, Yaffe B, Borenstein A. Single artery replantation of totally avulsed scalp. Injury. 1993;24:488–90. doi: 10.1016/0020-1383(93)90157-2. [DOI] [PubMed] [Google Scholar]
- 5.Ohara-Speert M, Mullaly SG. Nursing Care of the patient with a complete scalp avulsion. J Emerg Nurs. 1996;22:552–9. doi: 10.1016/s0099-1767(96)80211-x. [DOI] [PubMed] [Google Scholar]
- 6.Horovitz IL. Scalp injury treated by free graft of avulsed scalp. Lancet. 1964;284:939. doi: 10.1016/s0140-6736(64)90866-9. [DOI] [PubMed] [Google Scholar]
- 7.Lu MM. Successful replacement of avulsed scalp – case report. Plast Reconstr Surg. 1969;43:231–4. doi: 10.1097/00006534-196903000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Miller GDH, Anstee EJ, Snell JA. Successful replantation of an avulsed scalp by microvascular anastomoses. Plast Reconstr Surg. 1976;58:133–6. doi: 10.1097/00006534-197608000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Mccann J, Odonoghue J, Ghazal SKA, Johnston S, Khan K. Microvascular replantation of a completely avulsed scalp. Microsurgery. 1994;15:639–42. doi: 10.1002/micr.1920150907. [DOI] [PubMed] [Google Scholar]
- 10.Cheng KX, Su Z, Jiang KC, et al. Microsurgical replantation of the avulsed scalp: Report of 20 cases. Plast Reconstr Surg. 1996;97:1099–106. doi: 10.1097/00006534-199605000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Nahai F, Hurteau J, Vasconez LO. Replantation of an entire scalp and ear by microvascular anastomoses of only 1 artery and 1 vein. Br J Plast Surg. 1978;31:339–42. doi: 10.1016/s0007-1226(78)90122-4. [DOI] [PubMed] [Google Scholar]
- 12.Arashiro K, Ohtsuka H, Ohtani K, et al. Entire scalp replantation: Case-report and review of the literature. J Reconstr Microsurg. 1995;11:245–50. doi: 10.1055/s-2007-1006539. [DOI] [PubMed] [Google Scholar]
- 13.Chou CK, Lin SD, Yang CC, Lai CS, Lin GT. Microsurgical replantation of avulsed scalp – two cases report. Gaoxiong Yi Xue Ke Xue Za Zhi. 1992;8:285–9. [PubMed] [Google Scholar]
- 14.Sadove AM, Moore TS, Eppley BL. Total scalp, ear, and eyebrow avulsion: Aesthetic adjustment of the replanted tissue. J Reconstr Microsurg. 1990;6:223–7. doi: 10.1055/s-2007-1006822. [DOI] [PubMed] [Google Scholar]
- 15.Henderson HP, Sully L. Problems encountered in replantation of an avulsed scalp – use of leeches in replantation surgery. Br J Plast Surg. 1983;36:235–9. doi: 10.1016/0007-1226(83)90099-1. [DOI] [PubMed] [Google Scholar]
- 16.Wilhelmi BJ, Kang RH, Movassaghi K, Ganchi PA, Lee WPA. First successful replantation of face and scalp with single-artery repair: Model for face and scalp transplantation. Ann Plast Surg. 2003;50:535–40. doi: 10.1097/01.SAP.0000037875.69379.56. [DOI] [PubMed] [Google Scholar]
- 17.Sabapathy SR, Venkatramani H, Bharathi RR, D’Silva J. Technical considerations in replantation of total scalp avulsions. J Plast Reconstr Aesth Surg. 2006;59:2–10. doi: 10.1016/j.bjps.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Barisoni D, Lorenzini M, Governa M. Two cases of scalp reimplantation based on one artery and one vein with interposed vein grafts. Eur J Plast Surg. 1997;20:51–3. [Google Scholar]
- 19.Maladry D, Berard V, Dupuis P, Mitz V, Lemerle JP. Scalp reconstruction after avulsion: Emergency microsurgery and secondary tissue expansion. Apropos of 3 cases caused by farming machines. Ann Chir Plast Esthet. 1994;39:169–75. [PubMed] [Google Scholar]
- 20.Zhou S, Chang TS, Guan WX, et al. Microsurgical replantation of the avulsed scalp – report of 6 cases. J Reconstr Microsurg. 1993;9:121–5. doi: 10.1055/s-2007-1006660. [DOI] [PubMed] [Google Scholar]
- 21.Morris SF, MacGill KA. Scalp replantation by arterialised venous network flow-through. Br J Plast Surg. 1992;45:187–92. doi: 10.1016/0007-1226(92)90074-8. [DOI] [PubMed] [Google Scholar]
- 22.Juri J, Irigaray A, Zeaiter C. Reimplantation of scalp. Ann Plast Surg. 1990;24:354–61. doi: 10.1097/00000637-199004000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Sirimaharaj W, Boonpadhanapong T. Scalp replantation: A case report of long ischemic time. J Med Assoc Thailand. 2001;84:1629–34. [PubMed] [Google Scholar]