Abstract
Background. To improve acute myocardial infarction (AMI) care in the region ‘Hollands-Midden’ (the Netherlands), a standardised guideline-based care program was developed (MISSION!). This study aimed to evaluate the outcome of the pre-hospital part of the MISSION! program and to study potential differences in pre-hospital care between four areas of residency.
Methods. Time-to-treatment delays, AMI risk profile, cardiac enzymes, hospital stay, in-hospital mortality, and pre-AMI medication was evaluated in consecutive AMI patients (n=863, 61±13years, 75% male) transferred to the Leiden University Medical Center for primary percutaneous coronary intervention (PCI).
Results. Median time interval between onset of symptoms and arrival at the catheterisation laboratory was 150 (interquartile range [IQR] 101-280) minutes. The alert of emergency services to arrival at the hospital time was 48 (IQR 40-60) minutes and the door-to-catheterisation laboratory time was 23 (IQR 13-42) minutes. Despite significant regional differences in ambulance transportation times no difference in total time from onset of symptoms to arrival at the catheterisation room was found. Peak troponin T was 3.33 (IQR 1.23-7.04) μg/l, hospital stay was 2 (IQR 2-3) days and in-hospital mortality was 2.3%. Twelve percent had 0 known risk factors, 30% had one risk factor, 45% two to three risk factors and 13% had four or more risk factors. No significant differences were observed for AMI risk profiles and medication pre-AMI.
Conclusions. This study shows that a standardised regional AMI treatment protocol achieved optimal and uniformly distributed pre-hospital performance in the region ‘Hollands-Midden’, resulting in minimal time delays regardless of area of residence. Hospital stay was short and in-hospital mortality low. Of the patients, 88% had ≥1 modifiable risk factor. (Neth Heart J 2010;18:408–15.)
Keywords: Myocardial Infarction/therapy; Angioplasty, Transluminal, Percutaneous Coronary; Prevention & Control; Time Factors
Coronary heart disease (CHD) is the leading cause of death in the Western world. Current guidelines are therefore aimed at optimising care and outcome of patients with acute myocardial infarction (AMI).1,2 In the past 20 years the risk of dying from CHD in the Netherlands was successfully reduced by almost 33%.3 This was in part the result of increased efforts to improve acute treatment and secondary prevention strategies.3-5
In the acute phase AMI patients require rapid diagnosis and early reperfusion to minimise infarct size and to prevent complications. Several factors determine treatment delay with its major contributors being patient delay, physician delay and in-hospital delay. In order to minimise treatment delay an intensive collaboration is therefore needed between primary care physicians, regional ambulance services, community hospitals (without percutaneous coronary intervention (PCI) facilities), and PCI centers.
A regional AMI guideline implementation program (MISSION!) was developed to optimise the use of evidence-based medicine in practice.6 MISSION! contains a pre-hospital, in-hospital and outpatient clinical framework for decision-making and treatment of AMI patients. The main goal of this study was to investigate the outcome of the pre-hospital part of MISSION! and to evaluate and identify potential regional differences in multidisciplinary performance and related patient factors in the region ‘Hollands-Midden’.
Methods
Patients
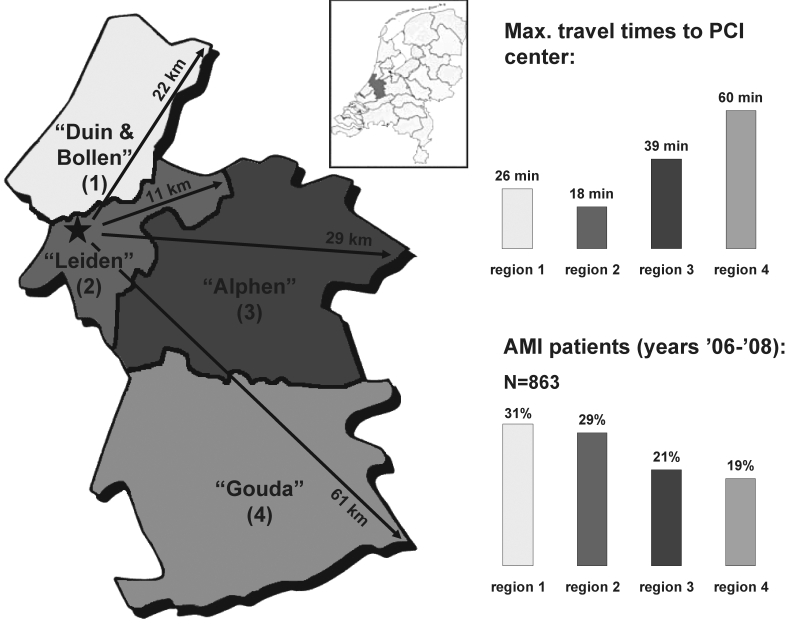
The geographical region studied (Hollands-Midden, meaning the centre of Holland) spans an area of 875 km2 with a population of approximately 750,000 inhabitants. Patients included in this study were all living in the region and were admitted with the diagnosis of AMI to the Leiden University Medical Center for primary PCI in the years 2006 to 2008. The study population was partitioned into four areas of residency within Hollands-Midden, classified as ‘Duin & Bollen’ (region 1), ‘Leiden’ (region 2), ‘Alphen’ (region 3) and ‘Gouda’ (region 4) (figure 1). AMI patients admitted for primary PCI living outside of the region Hollands-Midden were excluded.
Clinical protocol
To align AMI care, an intensive collaboration was established among primary care physicians, the regional ambulance services, three community hospitals without PCI facilities, three cardiac rehabilitation centres and the Leiden University Medical Center, serving as primary PCI facility. The MISSION! protocol was developed based on the American College of Cardiology/American Heart Association and European Society of Cardiology guidelines for AMI.2,7 The pre-hospital emergency care required trained ambulance personnel to obtain a 12-lead ECG at the patient’s home. In the case of suspect characteristics, the ECG was electronically transmitted to the PCI centre. Trained coronary care unit (CCU) nurses determined patient’s eligibility for primary PCI. Patients not eligible for PCI were transferred to a community hospital for further assessment. Patients eligible for primary PCI were transferred directly to the PCI centre’s Cardiac Care Unit. In the ambulance aspirin, abciximab and clopidogrel were administered to the patient. The catheterisation room was operational within 20 minutes, 24 hours a day, 7 days a week. After discharge, patients were offered a cardiac rehabilitation program and benefited from intensive outpatient follow-up for the period of one year. The current study focused on the pre-PCI phase of the MISSION! protocol.
Data collection
Data were recorded by ambulance personnel and medical staff at the hospital. All the data were registered in a departmental electronic patient system (EPD-Vision, LUMC, Leiden, the Netherlands).
Endpoints
Pre-clinical performance in the four residence areas was measured by the following time intervals (minutes): onset of symptoms to alert of emergency services (patient delay), onset of symptoms to arrival at catheterisation room (cath lab), door-to-cath lab (hospital delay) and interval between the alert of emergency services and arrival at the hospital. Additional endpoints of interest were peak troponin T and peak creatine phosphokinase (CPK) levels.
Furthermore, risk profile for CHD was compared between the four areas of residency within Hollands-Midden, including risk factors such as smoking, hypertension, hyperlipidaemia, positive family history, diabetes mellitus and prior myocardial infarction. Lastly, drug treatment before occurrence of AMI was studied. Pre-admission medication use of interest was β-blockers, statins, aspirin, ACE inhibitors, angiotensin II (AT2) antagonists, diuretics and calcium antagonists.
Statistical analysis
Sample comparisons were made with a Pearson Χ2 test for categorical variables using Yate’s correction where appropriate. A Kruskal-Wallis one-way analysis of variance was employed for the comparison of not normally distributed continuous variables such as time intervals. All tests were two-sided, a p-value of <0.05 was considered significant (using Bonferroni correction where appropriate). All data were analysed with SPSS 16.0.02.
Results
Study population
A total of 1002 consecutive AMI patients were admitted at the PCI centre between 2006 and 2008. Of these patients, 863 (86%) were Hollands-Midden residents and included in the final study population. Baseline characteristics are shown in table 1. The majority of patients was male (75%) and the mean age was 61±13 years. The distribution of patients from the areas of residence 1, 2, 3 and 4 was 31, 29, 21 and 19%, respectively (figure 1). The four most common risk factors were smoking (54%), a family history of coronary artery disease (CAD) which was present in 42% of patients, a body mass index (BMI) ≥30 kg/m2 (43%) and hypertension in 36% of patients. Median duration from onset of symptoms to arrival at the cath lab was 150 minutes (IQR 101-280 min). Median patient delay, measured as time between the onset of symptoms and the moment of alerting the emergency service, was 61 minutes (IQR 25-158 min), whereas the median time between the alert of emergency services and the arrival at the hospital was 48 minutes (IQR 40-60 min). Median door-to-cath lab time was 23 minutes (IQR 13-42 min). Hospital stay was only 2 (IQR 2-3) days and in-hospital mortality was 2.3% (20/863). Total 30-day mortality was 3.5% (30/863, including in-hospital mortality).
Table 1.
Patient characteristics (n=863).
| Male (%) | 646 (74.9) |
| Age (years) | 61±13 |
| BMI (kg/m2) | 28.4 (24.9-41.1) |
| - BMI ≥30 kg/m2 (%) | 374 (43.3) |
| Region of residency (%) | |
| - 1 | 265 (30.7) |
| - 2 | 253 (29.3) |
| - 3 | 185 (21.4) |
| - 4 | 160 (18.5) |
| Risk factors for coronary diseases (%) | |
| - Smoking | 462 (53.5) |
| - Hypertension | 307 (35.6) |
| - Hyperlipidaemia | 167 (19.4) |
| - Family history | 358 (41.5) |
| - Diabetes mellitus | 108 (12.5) |
| - Prior myocardial infarction | 90 (10.4) |
| Median time intervals in minutes (IQR) | |
| - Onset symptoms - arrival at cath lab | 150 (101-280) |
| - Door - arrival at cath lab | 23 (13-42) |
| - Onset symptoms - alert of emergency services | 61 (25-158) |
| - Alert of emergency services - arrival at hospital | 48 (40-60) |
| Hospitalisation | |
| - Days hospitalised (median [IQR]) | 2 (2-3) |
| - In-hospital mortality (%) | 20 (2.3) |
Values expressed as n (%), normally distributed data as mean ± standard deviation, otherwise as median (interquartile range [IQR]: 25th-75th percentile). BMI=body mass index, cath lab=catheterisation room.
Figure 1.
Schematic map of the region ‘Hollands-Midden’ (the Netherlands) further subdivided into the four areas of residency: ‘Duin & Bollen’ (region 1), ‘Leiden’ (region 2), ‘Alphen’ (region 3), ‘Gouda’ (region 4). The star within ‘Leiden’ (region 2) represents the location of the PCI centre. Maximal travel time to each area of residency (minutes) and percentage of patients per area are shown in the bar graphs on the right. AMI=acute myocardial infarction, km=kilometers, Max.=maximal, PCI=percutaneous coronary intervention.
Clinical characteristics per area of residency
Clinical characteristics according to the area of residency are shown in table 2. In summary, comparisons revealed a similar age and gender distribution between the four areas and similar risk profiles for CHD.
Table 2.
Patients’ medical history per region of residency.
| Region 1 | Region 2 | Region 3 | Region 4 | P value | |
|---|---|---|---|---|---|
| (n=265) | (n=253) | (n=185) | (n=160) | ||
| Patient characteristics | |||||
| - Male (%) | 203 (76.6) | 190 (75.1) | 130 (70.3) | 123 (76.9) | 0.415 |
| - Age (years) | 61±13 | 61±13 | 61±13 | 62±12 | 0.931 |
| - BMI (kg/m2) | 28.7 (25.5-42.6) | 28.4 (25.0-40.4) | 27.5 (24.5-39.6) | 27.8 (24.7-42.3) | 0.466 |
| Risk factors (%) | |||||
| - Smoking | 151 (57.0) | 128 (50.8) | 105 (57.1) | 78 (49.1) | 0.239 |
| - Hypertension | 102 (38.5) | 86 (34.3) | 68 (37.0) | 51 (32.1) | 0.540 |
| - Hyperlipidaemia | 50 (18.9) | 49 (19.4) | 35 (19.0) | 33 (20.8) | 0.969 |
| - Family history | 115 (43.4) | 99 (39.3) | 81 (44.0) | 63 (39.6) | 0.658 |
| - Diabetes mellitus | 29 (11.0) | 36 (14.3) | 26 (14.1) | 17 (10.7) | 0.533 |
| - Prior MI | 24 (9.1) | 34 (13.5) | 16 (8.7) | 16 (10.1) | 0.304 |
| - Prior PCI | 21 (8.0) | 22 (8.7) | 10 (5.4) | 9 (5.7) | 0.471 |
| - CABG in past | 6 (2.3) | 8 (3.2) | 3 (1.6) | 3 (1.9) | 0.724 |
| - History of AP | 33 (12.6) | 43 (17.5) | 28 (15.6) | 25 (15.8) | 0.498 |
| No. of risk factors | |||||
| - 0 | 39 (14.7) | 31 (12.3) | 12 (6.5) | 20 (12.5) | 0.063 |
| - 1-2 | 139 (52.5) | 145 (57.3) | 119 (64.3) | 97 (60.6) | 0.076 |
| - 3-4 | 73 (27.5) | 63 (24.9) | 45 (24.3) | 37 (23.1) | 0.747 |
| - ≥4 | 36 (13.6) | 39 (15.4) | 23 (12.4) | 15 (9.4) | 0.352 |
| Medication before MI (%) | |||||
| - β-blocker | 67 (25.4) | 45 (18.0) | 41 (22.4) | 27 (17.0) | 0.104 |
| - Aspirin | 51 (19.2) | 52 (20.8) | 33 (18.0) | 20 (12.6) | 0.195 |
| - Statin | 52 (19.7) | 48 (19.2) | 34 (18.6) | 21 (13.2) | 0.354 |
| - ACE inhibitor | 35 (13.2) | 33 (13.2) | 20 (10.9) | 17 (10.7) | 0.779 |
| - Ang II antagonist | 15 (5.7)* | 16 (6.4) | 25 (13.7)* | 10 (6.3) | 0.008* |
| - Diuretic | 31 (11.7) | 25 (10.0) | 22 (12.0) | 23 (14.5) | 0.598 |
| - Calcium antagonist | 30 (11.3) | 25 (10.0) | 21 (11.5) | 15 (9.4) | 0.893 |
| Peak troponin T (μg/l) | 3.45 (1.28-7.14) | 2.81 (0.92-6.39) | 3.34 (1.24-6.68) | 3.95 (1.98-7.87) | 0.083 |
| Peak CPK (U/l) | 1388 (587-2618) | 997 (448-2165) | 1323 (522-2727) | 1586 (755-3146) | 0.008* |
| LVEF 3 months post-MI (%) | 56 (47-64) | 56 (47-64) | 55 (49-63) | 55 (47-63) | 0.887 |
Values expressed as n (%), normally distributed data as mean ± standard deviation, otherwise as median (interquartile range [IQR]: 25th-75th percentile). * p<0.05. ACE=angiotensin-converting enzyme, ANG=angiotensin, AP=angina pectoris, BMI=body mass index, CABG=coronary artery bypass surgery, CPK=creatine phosphokinase, LVEF=left ventricular ejection fraction, MI=myocardial infarction, PCI=percutaneous coronary intervention.
Medication prior to AMI was similar between the four patient groups except for a significantly larger percentage of patients using AT2-antagonist living in region 3 when compared with patients living in the region 1 (13.7 vs. 5.7%, respectively).
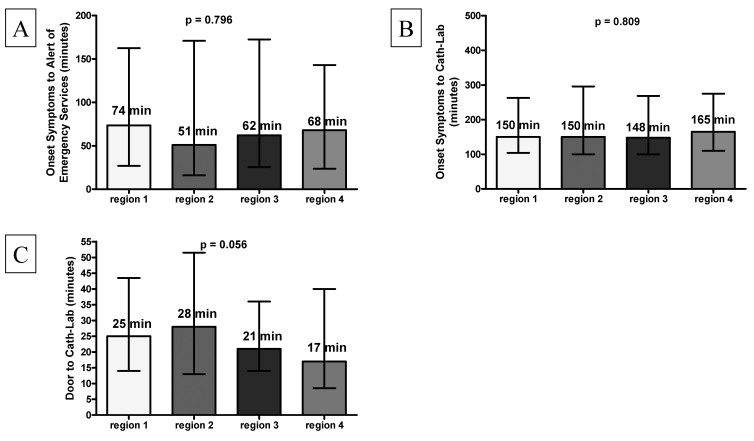
Pre-hospital care
Pre-hospital time delays per area of residency are illustrated in figure 2. Patient delays were similar between the four areas of residency as revealed by the median time between onset of symptoms to alert of emergency services (panel A: range of a median 51 min for region 2 to a median 74 min for region 1; p=0.796). In addition, total time elapsing between the onset of symptoms and the arrival at the catheterisation laboratory was also similar for patients from all four areas of residency (panel B: median 148 min for region 3 to median 165 min for region 4; p=0.809). Panel C furthermore shows that median in-hospital delay was relatively short (median 17 min for region 4 to median 28 min for region 2) and comparable between the patient groups (p=0.056).
Figure 2.
Time to treatment delay. Bar graphs showing patient delay defined as time from onset of symptoms to alert of emergency services (panel A); time interval from symptom onset to arrival at the catheterisation room (cath lab) (panel B) and hospital delay expressed as time from arrival at the hospital to arrival at the cath lab (panel C). Top of bar represents median time (minutes). Error bars indicate 25th and 75th percentile (minutes). Abbreviations as in figure 1.
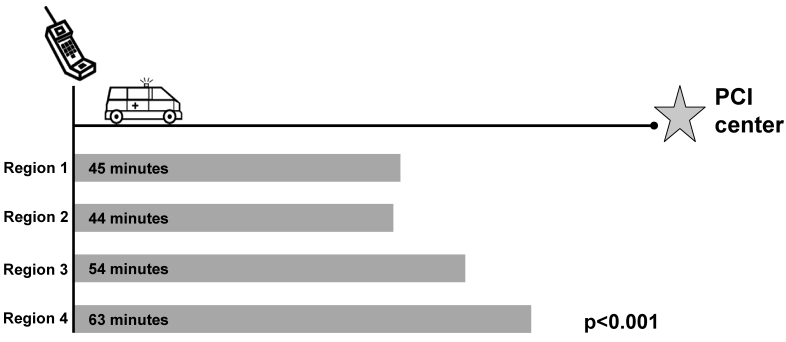
Figure 3 shows that significant differences were present between the four areas of residence in the total time needed for emergency services to arrive at the patient (from the moment of the 911 call) in addition to the amount of time needed to transport the patient to the PCI centre (p<0.001). Only two areas of residency did not differ significantly: region 1 and region 2 (median of 45 min and 44 min respectively). Patients living outside of this area all needed significantly more time to reach the PCI centre (≥50 min). Transportation time of patients from region 4 was the longest (median of 63 min). Of interest, these patients had the shortest door to cath lab time (17 min) when compared with patients from other areas.
Figure 3.
Time from alert of emergency services to arrival at PCI centre. Bars represent time interval (median minutes) from 911 call to the arrival at PCI centre (represented by star) per region of residency. Abbreviations as in figure 1.
Discussion
The main findings of this study were: (1) the pre-hospital MISSION! protocol succeeded in achieving equally high-quality pre-hospital performance in all areas of the region Hollands-Midden regardless of the distance from the PCI centre, (2) time delay due to geographical distance (‘Gouda’ [region 4] patients) was counterbalanced by a short in-hospital delay, and (3) there was no significant difference in pre-AMI medication use and risk profile of patients between the four areas of residency.
Structured care for AMI patients
Previous reports demonstrated that a standardised guideline-based treatment system can improve the quality of AMI care and can even result in a lower in-hospital and one-year mortality.8-11 Collaboration between general practitioner, ambulance services and hospital is essential in prevention, acute care and rehabilitation of (potential) AMI patients. Results of this study demonstrate the efficacy of the pre-hospital MISSION! protocol in achieving predefined targets.6 Furthermore, despite significant differences in transportation time (due to differences in distance from the PCI centre) similar time intervals between the onset of symptoms to arrival at the cath lab in all four areas of residence demonstrate that the multidisciplinary pre-hospital care is uniformly distributed and well organised in the region Hollands-Midden. Furthermore, even though physical distance was of influence on the time needed to get the patient to the hospital (from the start of symptoms), the short door-to-cath lab time (median 23 min) levelled out these differences.
Benefits of the standardised pre-hospital care program are also reflected in short admission duration (median 2 days) and low in-hospital mortality (2.3%). Peak cardiac enzyme levels per area of residency, such as troponin T levels, demonstrated that the final infarct size was similar, regardless of the geographical distance. Moreover, it corresponded well with left ventricular ejection fraction of patients as measured three months post-myocardial infarction by stress/rest myocardial perfusion scanning (table 2).
Hardly any significant differences were observed in medications prescribed by general practitioners prior to AMI and in risk factors for CHD between the four areas of residence within Hollands-Midden. Investigators of the EUROASPIRE Study investigated risk factor control in several countries in Europe.12 Compared with their most recent data, risk factors for CHD were less prevalent in our study population, except for smoking (this study: 54.0% vs. EUROASPIRE 18.3%) and BMI ≥30 kg/m2 (43% vs. 38.0%).13 Lower prevalence of hypertension (35.6% vs. 60.9%), hyperlipidaemia (19.4% vs. 46.2%) and diabetes (12.5% vs. 28.0%) point to a relatively successful risk factor control in the region Hollands-Midden. Possibly, greater attention for modifiable lifestyle factors, particularly smoking and obesity, may facilitate in further improving prevention of AMI in the region Hollands-Midden in the future.
Inconsistency of guideline implementation
Many organisations have recommended early reperfusion strategies and use of evidence-based medicine, together with long-term support programmes to stimulate healthier lifestyle for the treatment of patients with AMI.1,2 Although benefit of these guidelines has already been established, their implementation in the treatment of AMI patients is still inconsistent. Broer et al. showed that there were regional differences in pre-hospital time delays for AMI patients in the Netherlands.14 The EURASPIRE survey showed that there were significant differences in risk factor control and cardioprotective drug prescription between European countries.13
While guidelines recommend having at least 75% of patients treated within 90 minutes of presentation at the hospital, a study using the United States National Registry of Myocardial Infarction led investigators to conclude that this benchmark is rarely achieved for patients undergoing primary PCI in the United States. Only 4.2% of 4278 patients transferred for primary PCI at 419 hospitals were treated within 90 minutes and median door-to-balloon time was 180 minutes.15 More recently, the reported percentage of patients with door-to-balloon times of <90 minutes in a community-wide surveillance study of patients hospitalised with AMI (in a large central New England community in the United States) was less than 10%.16 In another Dutch study conducted by Broer et al., investigators reported hospital delays of 60 to 72 minutes.14 In contrast, the present study achieved a median door-to-cath lab time of 23 minutes, with 90% of patients reaching the cath lab in <90 minutes.
Clinical implications
Standardised protocols such as MISSION! contribute to improved adherence to evidence-based medicine in routine clinical practice and to the uniform implementation of structured care for patients with AMI, stressing the importance of close collaboration with all partners.
Limitations
No comparisons could be made between the current study population and a population not treated according to the MISSION! protocol in the region Hollands-Midden. Nevertheless, compared with previous studies, the MISSION! protocol performed well in the care of AMI patients.14-16
As this was a single-centre, single-region study conclusions may not pertain to larger regions. Furthermore, as data on prevalence of risk factors and medication use were derived in part from patient self-report, it should be considered with the necessary caution.
Conclusion
This study shows that a standardised regional AMI treatment protocol achieved optimal and uniformly distributed pre-hospital performance in the region Hollands-Midden, resulting in minimal time delays to treatment regardless of the area of residence. Furthermore hospital stay was short and in-hospital mortality low. Eighty-eight percent of patients had one or more modifiable risk factors.
References
- 1.Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, et al. 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation. 2008;117:296-329. [DOI] [PubMed] [Google Scholar]
- 2.Van de Werf F, Ardissino D, Betriu A, Cokkinos DV, Falk E, Fox KA, et al. Management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2003;24:28-66. [DOI] [PubMed] [Google Scholar]
- 3.van der Meulen A. Sterfte aan hart- en vaatziekten sinds 1970 gehalveerd; bron: Statistics Netherlands. 2005. [Google Scholar]
- 4.Hunink MG, Goldman L, Tosteson AN, Mittleman MA, Goldman PA, Williams LW, et al. The recent decline in mortality from coronary heart disease, 1980-1990. The effect of secular trends in risk factors and treatment. JAMA. 1997;277:535-42. [PubMed] [Google Scholar]
- 5.McGovern PG, Pankow JS, Shahar E, Doliszny KM, Folsom AR, Blackburn H, et al. Recent trends in acute coronary heart disease--mortality, morbidity, medical care, and risk factors. The Minnesota Heart Survey Investigators. N Engl J Med. 1996;334:884-90. [DOI] [PubMed] [Google Scholar]
- 6.Liem SS, van der Hoeven BL, Oemrawsingh PV, Bax JJ, van der Bom JG, Bosch J, et al. MISSION!: optimization of acute and chronic care for patients with acute myocardial infarction. Am Heart J. 2007;153:14-11. [DOI] [PubMed] [Google Scholar]
- 7.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation. 2004;110:e82-292. [PubMed] [Google Scholar]
- 8.Eagle KA, Montoye CK, Riba AL, DeFranco AC, Parrish R, Skorcz S, et al. Guideline-based standardized care is associated with substantially lower mortality in medicare patients with acute myocardial infarction: the American College of Cardiology's Guidelines Applied in Practice (GAP) Projects in Michigan. J Am Coll Cardiol. 2005;46:1242-8. [DOI] [PubMed] [Google Scholar]
- 9.Fonarow GC, Gawlinski A, Moughrabi S, Tillisch JH. Improved treatment of coronary heart disease by implementation of a Cardiac Hospitalization Atherosclerosis Management Program (CHAMP). Am J Cardiol. 2001;87:819-22. [DOI] [PubMed] [Google Scholar]
- 10.Mehta RH, Montoye CK, Faul J, Nagle DJ, Kure J, Raj E, et al. Enhancing quality of care for acute myocardial infarction: shifting the focus of improvement from key indicators to process of care and tool use: the American College of Cardiology Acute Myocardial Infarction Guidelines Applied in Practice Project in Michigan: Flint and Saginaw Expansion. J Am Coll Cardiol. 2004;43:2166-73. [DOI] [PubMed] [Google Scholar]
- 11.Schiele F, Meneveau N, Seronde MF, Caulfield F, Fouche R, Lassabe G, et al. Compliance with guidelines and 1-year mortality in patients with acute myocardial infarction: a prospective study. Eur Heart J. 2005;26:873-80. [DOI] [PubMed] [Google Scholar]
- 12.Clinical reality of coronary prevention guidelines: a comparison of EUROASPIRE I and II in nine countries. EUROASPIRE I and II Group. European Action on Secondary Prevention by Intervention to Reduce Events. Lancet. 2001;357:995-1001. [DOI] [PubMed] [Google Scholar]
- 13.Kotseva K, Wood D, De BG, De Backer G, De Bacquer D, Pyorala K, Keil U. Cardiovascular prevention guidelines in daily practice: a comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet. 2009;373:929-40. [DOI] [PubMed] [Google Scholar]
- 14.Broer J, Bleeker JK, Bouma J, de Jongste MJ, Erdman RA, Meyboom-de JB. [Regional differences in prehospital time delay for patients with acute myocardial infarction; Rotterdam and Groningen, 1990-1995]. Ned Tijdschr Geneeskd. 2000;144:78-83. [PubMed] [Google Scholar]
- 15.Nallamothu BK, Bates ER, Herrin J, Wang Y, Bradley EH, Krumholz HM. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction (NRMI)-3/4 analysis. Circulation. 2005;15;111:761-7. [DOI] [PubMed] [Google Scholar]
- 16.Saczynski JS, Yarzebski J, Lessard D, Spencer FA, Gurwitz JH, Gore JM, et al. Trends in prehospital delay in patients with acute myocardial infarction (from the Worcester Heart Attack Study). Am J Cardiol. 2008;102:1589-94. [DOI] [PMC free article] [PubMed] [Google Scholar]