Abstract
Physical training is beneficial and should be included in the comprehensive management of all patients with COPD independently of disease severity. Different rehabilitative strategies and training modalities have been proposed to optimize exercise tolerance. Interval exercise training has been used as an effective alternative modality to continuous exercise in patients with moderate and severe COPD.
Although in healthy elderly individuals and patients with chronic heart failure there is evidence that this training modality is superior to continuous exercise in terms of physiological training effects, in patients with COPD, there is not such evidence. Nevertheless, in patients with COPD application of interval training has been shown to be equally effective to continuous exercise as it induces equivalent physiological training effects but with less symptoms of dyspnea and leg discomfort during training.
The main purpose of this review is to summarize previous studies of the effectiveness of interval training in COPD and also to provide arguments in support of the application of interval training to overcome the respiratory and peripheral muscle limiting factors of exercise capacity. To this end we make recommendations on how best to implement interval training in the COPD population in the rehabilitation setting so as to maximize training effects.
Key Words: interval exercise training, chronic obstructive pulmonary disease, exercise tolerance, pulmonary rehabilitation
INTRODUCTION
There is a considerable body of evidence that exercise training strategies in patients with chronic obstructive pulmonary disease (COPD) induce significant improvement in exercise tolerance and quality of life.1–4 Indeed a recent meta-analysis5 demonstrated that stable patients with COPD gain considerable benefits from comprehensive rehabilitation programs when exercise training is included (Evidence A).6
Intensity and duration of exercise are important determinants of the physiologic adaptations that occur in response to training.7 In COPD patients there are indications that greater physiological benefits can be obtained through high-intensity compared to moderate-intensity training.8,9 However, high-intensity exercise training may not be applicable to those COPD patients who are unable to sustain such intensities for long periods of time due to symptom limitation.10 In fact patients with severe COPD are so limited by dyspnea and/or locomotor muscle weakness that their ability to exercise is restricted to very low-intensity levels.10
In this context there have been different strategies employed to improve exercise capacity in patients with severe COPD, ie, heliox and oxygen supplementation,11–16 bronchodilator therapy,17,18 one-legged training,19 noninvasive mechanical ventilation (NIMV)12,20,21 as well as different training modalities of dis-continuous nature inducing lower ventilatory demands such as interval or intermittent exercise.22–25 Furthermore, in the rehabilitation setting strategies such heliox supplementation or NIMV would be expensive to implement in large cohort of patients whereas interval training could be cost effective and easily applicable.
Implementation of interval training has shown to allow lower limb exercise to be sustained at a high intensity which otherwise would not be tolerable. Interval training can be applied especially to those patients with advanced COPD, who are unable to sustain exercise intensities sufficiently long enough to obtain a physiological training effect because of ventilatory limitation.23,26 Importantly these patients can endure high-intensity interval training in a rehabilitation setting for long periods of time with lower symptoms of dyspnea and leg discomfort compared to the conventionally implemented continuous training.22,27,28
Although a recent systematic review of 8 randomized control trials (388 patients)4 failed to reveal the efficacy of interval training over that of continuous in terms of enhancing exercise tolerance and quality of life in patients with severe COPD, the authors presented some limitations (training protocols heterogeneity, small sample sizes), suggesting that further research is needed in order to reveal the superiority of interval training in severe COPD. Issues that were not fully addressed in previous studies (such as performing comparisons among training groups exercising at different total work-loads during the course of rehabilitation) need to be clarified by future research.
In support of the above argument there are studies in patients with chronic heart failure (CHF)29,30 and healthy elderly age-matched individuals31,32 advocating the superiority of high-intensity interval training in terms of improvement in aerobic capacity, cardiac hypertrophy, left ventricular systolic performance, and antioxidative status.32 Whether such disparity in the findings between different patient populations or healthy elderly individuals is due to the different factors (respiratory, cardiovascular, and or peripheral muscular) potentially limiting exercise tolerance remains to be investigated.
Accordingly, the primary purpose of this review is to explore the factors that limit exercise tolerance in patients with COPD, and also to make recommendations on how best to implement interval training so as to maximize training effects in patients with advanced COPD.
PHYSIOLOGICAL BASIS OF INTERVAL EXERCISE
Historically, the rationale for interval exercise training has been the ability to impose very high power outputs from peripheral muscles without overloading the cardiorespiratory capacity.33 Classical studies33 have shown that the metabolic response during interval exercise is very similar to continuous moderate exercise and, thus, is associated with a stable pattern of cardiorespiratory responses and low lactate concentration in the muscle throughout the relatively long exercise and recovery periods.
In healthy young people, high-intensity interval training induces greater improvement in oxygen consumption,34,35 work rate,35 ventilatory and lactate thresholds36 compared to continuous training.37 Studies on muscle fiber metabolism during interval exercise in healthy subjects have shown that glycogen depletion is similar between type I and II fibers, suggesting that both fiber types are recruited to a similar degree.33 Although, heavy intensity continuous exercise induces high blood lactate levels (due to the depletion of phosphocreatine and the use of myoglobin-bound oxygen reserves), interspersed periods of sub-lactate threshold work rates may facilitate lactate removal38 and partially restore the phosphocreatine levels.39 In addition, the capacity to reload myoglobin stores during the recovery phases, allowing a more oxidative degradation of glycogen and, hence, a partially reduced demand, has been proposed as the principal mechanism for the slowed glycolysis observed during interval training.33
Compared with the same total amount of work performed continuously, interval exercise imposes maximal loads on both peripheral muscles and oxygen-transporting organs without significant engagement of anaerobic processes and accumulation of lactic acid (less glycogen is used and the lactate concentration in the muscle is much lower).33 Apparently, in intermittent exercise with short exercise periods (< 30 sec) healthy young subjects can endure very high rates of exercise aerobically thereby yielding very little lactate production.33 This type of high-intensity periodic activity is shown to be effective not only in athletic training but also in COPD,22,24 CHF,29,30,40,41 and other chronic disease entities characterized by peripheral muscle wasting.42,43
A study by Ahmaidi et al31 investigating the effects of interval training on ventilatory threshold and cardiorespiratory responses in elderly healthy individuals showed significant improvement of both maximal aerobic capacity and submaximal exercise tolerance, with a significant decrease in heart rate after a 3-month program. Moreover, training was easily accepted and tolerated by the elderly with high levels of adherence and attendance. A latter study32 comparing continuous with intermittent exercise training in healthy elderly men, showed significantly lower cardiorespiratory and metabolic responses in the intermittent compared to continuous group when exercising at the same work-loads.
Interval exercise training in CHF patients with a history of myocardial infarction30 has resulted in an increase in exercise capacity over that achieved with a continuous exercise training. Reports from studies in severe CHF patients have shown that short-term interval training (with a work-recovery ratio of 1:2, ie, 30 second work phases/60 second recovery phases) can improve exercise capacity, prevent high lactate accumulation, and allow more intense exercise stimuli to the peripheral muscles with minimal cardiac strain.40,44 This finding has been confirmed by latter studies showing that interval training induced a significant improvement in exercise capacity in patients with CHF with lower heart rate at peak exercise, compared to those trained with continuous exercise, thereby suggesting improved stroke volume.45,46 Lastly, a study on the oxygen uptake kinetic responses has shown improvement of the time constant in CHF patients, suggesting significant peripheral oxidative adaptations (enhanced mitochondrial enzyme activity and vasodilatory capacity of the skeletal muscle vasculature) following interval training.47
Improvement of myocardial contractile function after interval exercise training has also been reported in a study by Whislof30 in patients with left ventricular dysfunction (ejection fraction 29%). Twelve weeks of a supervised interval training (twice a week/38 minutes) at intensities of 90% to 95% of peak heart rate had superior effects in peak oxygen uptake, anaerobic threshold, left ventricular systolic function, skeletal muscles proteins, and muscle antioxidative status when compared to continuous exercise sustained at an intensity of 70% to 75% of peak heart rate.
Based on the above, one would expect that interval training would be superior to continuous training in COPD as well, as these patients demonstrate severely compromised exercise capacity and are limited by ventilatory constraints, which are particularly apparent during high-intensity prolonged exercise. Brief bouts of high-intensity interval exercise in COPD do not exacerbate the ventilatory requirement as lactic acid concentration and its effect on arterial blood pH are significantly lower compared to moderate intensity constant-load exercise.23,26 However, most studies in COPD patients have failed to show the superiority of interval training in exercise capacity compared to the conventionally implemented continuous training in the rehabilitation setting.22,24,27,28,48–50
PHYSIOLOGICAL RATIONALE FOR INTERVAL EXERCISE INPLEMENTATION IN COPD
People with COPD may respond to training in a different way than healthy subjects, or their age-matched counterparts, as the determinants of exercise limitation appear to be multifactorial. Such factors refer to expiratory flow limitation, dynamic lung hyperinflation, gas exchange abnormalities, insufficient energy supply to the peripheral and the respiratory muscles, morphological alterations in lower leg muscle fibers, and functional metabolic capacity.51–53
Dealing with ventilatory limitations
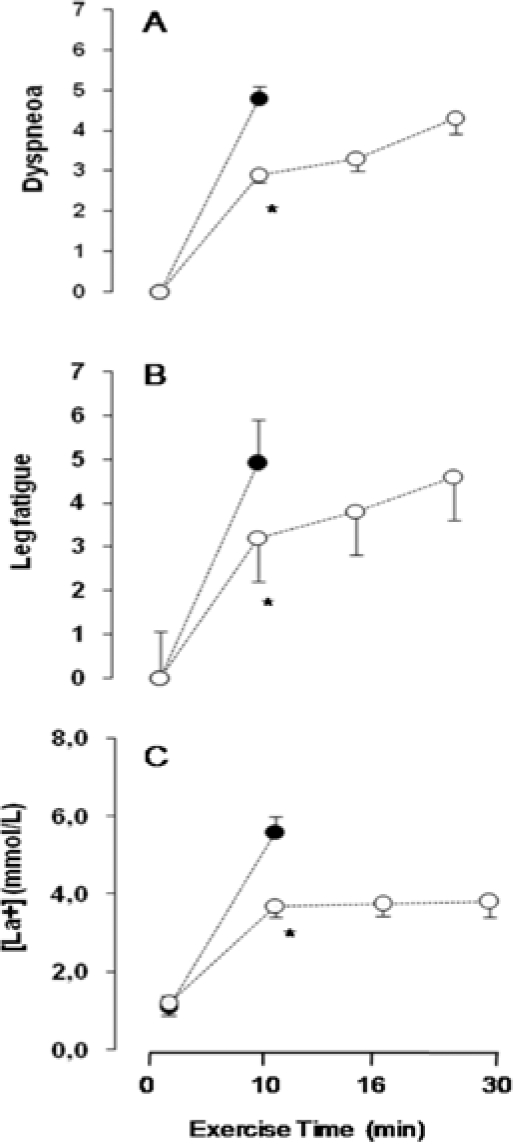
Patients with severe COPD may demonstrate flow limitation even at rest or experience expiratory flow limitations during low and moderate exercise54 limiting their capacity to exercise continuously at high work rates due to intense dyspnea sensations.26,51 As lactic acidosis puts particular stress on the ventilatory system, the small increase in arterial lactate concentration observed during interval exercise as compared to continuous exercise,23,26 appears to be beneficial for COPD patients by reducing some of the acid stimulus to breathe,8 thereby allowing ventilation and dyspnea sensations to be tolerated for a prolonged period of time (Figure 1).
Figure 1.
Time course of a) dyspnea, b) leg fatigue assessed with the 0-10 Borg Scale and c) blood lactate concentration during interval (open circles) and constant-load (closed circles) exercise. *asterisks denotes significant differences (p < .05) between exercise modes. Modified from the European Respiratory Society.26
Vogiatzis et al26 have shown that patients with severe COPD (FEV1: 40% predicted) can almost triple the total exercise duration with significantly lower and more stable metabolic and ventilatory responses compared to continuous exercise. Although patients exercised for longer times (32-35 vs 9-12 minutes) at a higher intensity (100% vs 80% WRmax) with the interval mode, they had lower metabolic demands and less ventilatory restrictions at the end of a symptom-limited exercise (Table 1).
Table 1.
Responses to Maximal Tolerable Interval Exercise (IE) and Constant-load Exercise (CLE) in Patients with Severe COPD
| End of IE | End of CLE | |
|---|---|---|
| Total Exercise time (min) | 32.7 ± 3.0 | 1 0.3 ± 1.6* |
| VO2 (L/min) | 0.81 ± 0.05 | 0.94 ± 0.07* |
| VCO2 (L/min) | 0.75 ± 0.04 | 0.95 ± 0.07* |
| VE (L/min) | 33.1 ± 1.5 | 38.4 ± 2.2* |
| VE/MVV % | 76 ± 4 | 85 ± 3* |
| VT(L) | 1.01 ± 0.05 | 1.14 ± 0.06* |
| VT/IC % | 66.4 ± 2.0 | 75.2 ± 1.7* |
| IRV(L) | 0.58 ± 0.06 | 0.38 ± 0.03* |
| IRV%pred. TLC | 8.9 ± 0.8 | 5.9 ± 0.5* |
| Paco2 (mmHg) | 44.0 ± 1.3 | 45.4 ± 1.2* |
| pH | 7.38 ± 0.06 | 7.34 ± 0.07* |
| VD(L) | 0.48 ± 0.02 | 0.53 ± 0.02* |
| Arterial Lactate cone. (mMol/L) | 3.89 ± 0.36 | 5.81 ± 0.41* |
Modified from the European Respiratory Society.26 Data are presented as mean ± SEM. VO2: oxygen uptake; VCO2: carbon dioxide output; VE: minute ventilation; MVV: maximum voluntary ventilation; VT: tidal volume; IC: inspiratory capacity; IRV: inspiratory reserve volume; PaCO2: arterial carbon dioxide tension; VD: physiological dead space; cone: concentration.
Significant differences (p<.05) between IE and CLE
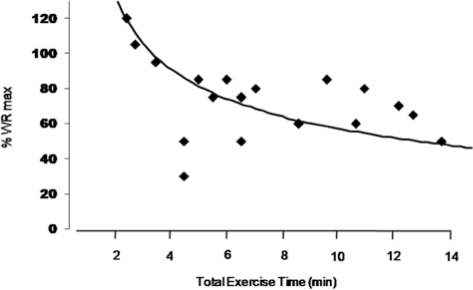
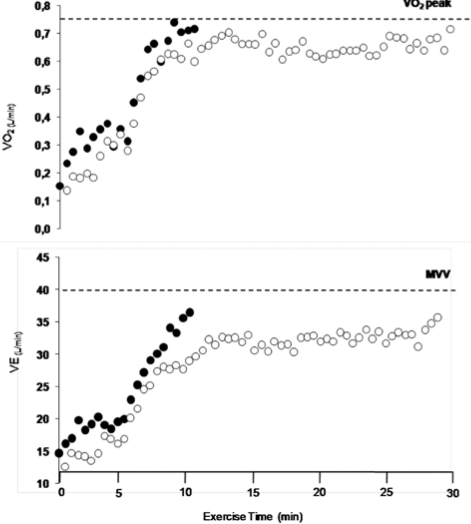
Conversely, exercising continuously without any rest periods, severe COPD patients can tolerate high work rates (50-80% of their maximum exercise capacity) for only 5 to 12 minutes, at the end of which they are completely exhausted (Figure 2).8,26,51,55–59 At intensities of 85% to 95% of WRpeak, severe COPD patients (FEV1< 50% predicted) can sustain only 4 to 5 minutes of work,8,51,55,59 and only up to 13 minutes for lower intensities (60-80% WRmax)8,26,51,59 (Figure 2). As such, implementing continuous exercise training for patients with advanced COPD will be ineffective as they will have to rest for several minutes before they start exercising again. In contrast, interval training can enable patients to complete short periods of high-intensity exercise that would not be possible with a continuous-exercise mode. When patients exercise for short periods (eg, 30 seconds), alternated with short rest intervals lasting for 30 seconds, they complete the total work with moderate exertion and relatively stable metabolic and ventilatory response23,26 (Table 2, Figure 3).
Figure 2.
Total exercise time (min) and total work rate (% WRmax) with continuous exercise training in studies with COPD patients of different disease severity. Each symbol represents a different exercise training intensity in patients with FEV1 > 40% predicted (refs:8,23,51,56,59) and FEV1 < 40% predicted (refs: 26,55,57,58).
Table 2.
Stability of Metabolic and Ventilatory Responses to Interval Exercise at Temporally Matched Time Points in Severe COPD Patients
| 30% total time | 60% total time | 90% total time | |
|---|---|---|---|
| VO2 (L/min) | 0.74 ± 0.04 | 0.77 ± 0.05 | 0.78 ± 0.04* |
| VE (L/min) | 31.1 ± 1.6 | 32.0 ± 1.8 | 32.7 ± 2.2* |
| IC(L) | 1.55 ± 0.08 | 1.61 ± 0.08 | 1.59 ± 0.08* |
Data are presented as mean ± SEM. VO2: oxygen uptake; VE: minute ventilation; IC: inspiratory capacity.
No significant differences were found between the different time points during interval exercise. Modified from the European Respiratory Society.26
Figure 3.
Oxygen uptake (VO2) and minute ventilation (VE) in COPD patients during interval (open circles) and constant-load (closed circles) exercise protocol. Interval exercise was sustained for 30 sec at 100% of peak baseline capacity alternated by 30 sec rest, whereas continuous exercise was sustained at 75% of peak baseline capacity. Modified from the European Respiratory Society.26
Dealing with peripheral muscle dysfunction
Experimental evidence from peripheral skeletal muscle biopsies of patients with severe COPD indicate that the baseline energy status can be shifted towards an increased glycolytic capacity and a concomitant decrease in aerobic enzyme capacity.53,60 This is due to the decrease in the proportion of type I fibers (slow oxidative) and the increase in the proportion of type IIa (fast oxidative and glycolytic) and IIb (fast glycolytic) muscle fibres of peripheral musculature.53,61 Such alterations in structure and function of peripheral muscle fibers may affect aerobic exercise tolerance in patients with moderately severe and severe COPD.53 Since there is a fiber shift toward a more glycolytic profile, it is obvious that exercise training in COPD patients should be adapted at those morphologic alterations.
Implementation of interval exercise training in patients with advanced COPD has been shown to be effective in terms of improvements in vastus lateralis capillarization28 and muscle fiber oxidative capacity39 thus enhancing the utilization of oxygen by the exercising muscles. In a study by Vogiatzis et al,28 it was reported that interval training at an intensity of 100% to 140% of Wpeak for 10 weeks (30 sessions for 45 min each) increased muscle oxidative capacity, the cross sectional area (CSA) of both type I and IIa fibers and reduced the proportion of type IIb fibers. Furthermore, a latter study revealed that there were no differences between interval and continuous training in terms of increasing the expression of genes regulating muscle fiber hypertrophy (IGF-I, MGF) and regeneration (ie, MyoD).62 These findings demonstrate that it is possible to induce shifts in the distribution of the subgroups of the muscle fibers with interval training28 in a similar fashion to continuous training.63,64
As mentioned above, the rationale for the potential superiority of interval exercise is that it is associated with a small increase in arterial lactate concentration (less than 4 mmol/L), reduced ventilatory demand (lower ventilation and degrees of dynamic hyperinflation),23,25,26,27 and lower symptoms of dyspnea23,28 and leg discomfort22,27,28 during the training sessions compared to continuous training. Furthermore, comparing the metabolic and respiratory responses between the two training modalities at isotime, interval training seems superior to continuous, suggesting that it would be of benefit to COPD patients whose exercise tolerance is limited either by respiratory or peripheral muscle factors.23,25,26
Potential benefits of interval training
Based on the above physiological advantages, most randomized trials have shown that interval training in the rehabilitation setting is equally effective to continuous training in terms of improving exercise capacity and health-related quality of life in COPD patients with varying disease severity.22,24,25,27,48,49 Both training modes elicit similar training responses in the lower leg musculature,28,48 while interval training induced less symptoms of dyspnea and leg discomfort during exercise sessions.22,23,26–28 A few studies have shown contradictory results reporting no differences in symptoms between training modalities.48,49 Differences between studies might be attributed to the interval durations.
Given that the total training work load is an important determinant of the training response, it is important to highlight that in all previous studies the total amount of work sustained during exercise training was not significantly different between the two modalities (ie, continuous and interval) most likely precluding a significant difference in all primary outcomes22,24,25,27,28,48–50.
Accordingly, it is highly likely that in order to induce substantial improvements in exercise capacity and demonstrate the superiority of interval training over continuous conditioning, the total work-load should be much higher (up to the limit of patients' perception of leg discomfort) and the exercise duration must be longer. To the authors' knowledge, no studies in the literature have implemented interval exercise training based on the intensity of the leg discomfort (eg, using the Borg scale up to the limits of heavy perception or 5 on the scale of 10).
Hence, when: (1) the total amount of training work is targeted to be significantly greater than that of continuous exercise, (2) the duration of the exercise training bouts is as short as 30 seconds22,26,28 to 60 seconds23,24 and (3) the exercise intensity induces leg discomfort levels comparable to those reported during continuous exercise (between 4 to 5 on the 1-10 Borg scale), then interval training might be a more effective modality in patients with advanced and severe COPD. More specifically, if exercise duration is kept similar (eg, 30-40 minutes) and exercise intensity is increased to levels to induce comparable intensity of leg discomfort while maintaining lower dyspnea sensations (by alternating the exercise and the rest periods), then the magnitude of central and peripheral muscle adaptations to interval training might be superior to those achieved with continuous training.
Eventually, it is recommended to increase the training duration to more than an hour and to progress the training intensity to 150% of the baseline peak capacity so as to expose the body to a training overload that is appropriate to achieve even greater physiological responses than when exposed to continuous training.
Further studies are required to investigate the appropriate time and/or interval training work load in COPD patients with different disease severity. Like in patients with CHF,29,40 or in elderly people,32 the shortest rest intervals (up to or less than 1 minute) used in some COPD studies22,23,24,26 may be better tolerated than longer rest intervals or low-intensity exercise intervals25,27,48,49 in patients with ventilatory limitations. Short rest intervals result in lower VO2 as well as VCO2, minute ventilation, and heart rate values.23 During the 30-second breaks, when patients focus on breathing techniques without being interfered by cycling exercise, physiotherapists can teach them to adopt pursed-lip breathing to promote improvements in tidal volume, arterial saturation,65 and decrease end-expiratory lung volume, thus reducing breathlessness during exercise.66
A final reason that makes interval training modality a promising approach in rehabilitation programs is that the most severely impaired patients with greater dyspnea sensations, dynamic hyperinflation, arterial hypoxemia, and lower baseline exercise capacity can better tolerate an interval exercise protocol than a continuous exercise one and they may demonstrate more adherence to the rehabilitation program.24,67
PRACTICAL ISSUES AND RECOMMENDATIONS
According to the above physiological concepts, training in COPD patients aims to increase aerobic capacity with a relatively low peak demand on the respiratory and the circulatory system. Improvement in aerobic exercise capacity following rehabilitation is dependent on the total exercise duration and the total work load applied. Hence, to enable COPD patients to tolerate high-intensity exercise for sufficiently long periods of time with less symptoms of dyspnea and leg discomfort, interval training may be superior to other training modalities.
Practically speaking, physiotherapists who develop an exercise plan should consider that the heavier the work rate, the shorter should be the exercise periods (∼30 seconds) and also, the longer the rest intervals (∼60 seconds) ought to be. Short intensity intervals may be better tolerated by people with severe COPD. Based on the above, exercise training on a cycle ergometer might be as follows: considering frequency, interval mode, intensity, and duration of exercise:
Frequency: 3-4 times weekly.
Interval mode: 30 seconds exercise period with 30 seconds rest or even 20 seconds exercise – 40 seconds rest.
Intensity and duration: initially familiarize the patients on the cycle ergometer at an intensity equivalent to 80% of the maximal work load for 15 to 20 minutes for the first 3 to 4 sessions. The Borg Scale of perceived exertion can be used to more easily monitor exercise intensity. Increase training work load by 5% to10% of peak capacity when patients rate their perceived dyspnea as moderate. If the 10-point Borg scale is used to describe exercise intensity, most exercise should be performed between 5 to 6 intensity for the legs and 3 to 4 for dyspnea.
Increase total exercise time from 30 to 90 minutes per session (including rest periods), at intensities that progressively reach 150% of the baseline maximum work load.
Suggest pursed-lip breathing during rest periods to increase tidal volume and reduce breathing frequency.
Teach patients to perform all daily activities (eg, stair climbing, uphill walking) at an interval mode consisting of short bouts of activity lasting 10 to 15 sec and rest periods of 15 sec.
Give written instructions to the patients for home practice.
Such a training program might last longer per session than one using continuous exercise and sometimes is not easily applicable in the clinical setting. However, interval training may be followed at home as it is easily tolerated by patients.
CONCLUSION
There is evidence that dyspnea and leg discomfort limit the ability of COPD patients to exercise, and as the patients' response to exercise is highly variable,67,68 it is challenging to follow training regimes that are effective, more tolerable (with fewer breaks in each training sessions and better adherence to exercise),24 less frustrating for the patients, and encouraging in terms of increasing the long-term adherence to pulmonary rehabilitation programs.
Interval training in severely disabled COPD patients is associated with stable metabolic demands,23 low minute ventilation and rates of dynamic hyperinflation, and increased total exercise duration than that of constant-load exercise.23,26 Hence, the application of this method in the rehabilitation setting has the potential to convey important clinical benefits, as it allows the application of intense loads on peripheral muscles for sufficiently long periods of time. Interval exercise may, therefore, provide a good alternative to constant-load exercise training in order to improve compliance with exercise and, thus, the effectiveness of this treatment. Studies are required to determine the efficacy of interval exercise training in long-term follow up and on adherence in pulmonary rehabilitation programs.
REFERENCES
- 1.Lacasse Y, Guyatt GH, Goldstein RS. The components of a respiratory rehabilitation program: a systematic overview. Chest. 1997;111:1077–1088. doi: 10.1378/chest.111.4.1077. [DOI] [PubMed] [Google Scholar]
- 2.Lacasse Y, Brossea L, Milne S, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cohrane Database Syst Rev. 2002;3:3. doi: 10.1002/14651858.CD003793. CD003793. [DOI] [PubMed] [Google Scholar]
- 3.Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary rehabilitation: Joint ACCP/AACVPR Evidence-based Clinical Practice Guidelines. Chest. 2007;131:4S–42S. doi: 10.1378/chest.06-2418. [DOI] [PubMed] [Google Scholar]
- 4.Beauchamp MK, Nonoyama M, Goldstein R, et al. Interval versus continuous training in individuals with COPD – a systematic review. Thorax. 2010;65:157–164. doi: 10.1136/thx.2009.123000. [DOI] [PubMed] [Google Scholar]
- 5.Lacasse Y, Martin S, Lasserson TJ, et al. Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. A Cochrane systematic review. Eura Medicophys. 2007;43:475–485. [PubMed] [Google Scholar]
- 6.Global Initiative for Chronic Obstructive Lung Disease . Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. Updated 2009. www.goldcopd.org. [Google Scholar]
- 7.Rees K, Taylor R, Singh S, et al. Exercise based rehabilitation for heart failure. Cochrane Database Syst Rev. 2004 doi: 10.1002/14651858.CD003331.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casaburi R, Patessio A, Ioli F, et al. Reductions in exercise lactic acidosis and ventilation as a result of exercise training in patients with obstructive lung disease. Am Rev Respir Dis. 1991;143:9–18. doi: 10.1164/ajrccm/143.1.9. [DOI] [PubMed] [Google Scholar]
- 9.Casaburi R, Porszasz J, Burns MR, et al. Physiologic benefits of exercise training in rehabilitation of patients with severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1997;155:1541–1551. doi: 10.1164/ajrccm.155.5.9154855. [DOI] [PubMed] [Google Scholar]
- 10.Maltais F, LeBlanc P, Jobin J, et al. Intensity of training and physiologic adaptations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1997;155:555–561. doi: 10.1164/ajrccm.155.2.9032194. [DOI] [PubMed] [Google Scholar]
- 11.Garrod R, Paul EA, Wedzicha JA. Supplemental oxygen during pulmonary rehabilitation in patients with COPD with exercise hypoxaemia. Thorax. 2000;55:539–543. doi: 10.1136/thorax.55.7.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson JE, Gavin DJ, Adams-Dramiga S. Effects of training with heliox and noninvasive positive pressure ventilation on exercise ability in patients with severe COPD. Chest. 2002;122:464–472. doi: 10.1378/chest.122.2.464. [DOI] [PubMed] [Google Scholar]
- 13.Emtner M, Porszasz J, Bunrs M, et al. Benefits of supplemental oxygen in exercise training in non-hypoxemic COPD patients. Am J Respir Crit Care Med. 2003;68:1034–1042. doi: 10.1164/rccm.200212-1525OC. [DOI] [PubMed] [Google Scholar]
- 14.Laude EA, Duggy NC, Baveystock C, et al. The effect of helium and oxygen on exercise performance in chronic obstructive pulmonary disease: a randomized crossover trial. Am J Respir Crit Care Med. 2006;173:865–870. doi: 10.1164/rccm.200506-925OC. [DOI] [PubMed] [Google Scholar]
- 15.Eves ND, Petersen SR, Haykowsky MJ, et al. Helium-hyperoxia, exercise and respiratory mechanics in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;174:763–771. doi: 10.1164/rccm.200509-1533OC. [DOI] [PubMed] [Google Scholar]
- 16.Giappa GR, Queiroga F, Jr, Meda E, et al. Heliox improves oxygen delivery and utilization during dynamic exercise in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;179:1004–1010. doi: 10.1164/rccm.200811-1793OC. [DOI] [PubMed] [Google Scholar]
- 17.O'Donnell DE, Fluge T, Gerken F, et al. Effects of tiotropium on lung hyperinflation, dyspnea and exercise tolerance in COPD. Eur Respir J. 2004;23:832–840. doi: 10.1183/09031936.04.00116004. [DOI] [PubMed] [Google Scholar]
- 18.Casaburi R, Kukafka D, Cooper CB, et al. Improvement in exercise tolerance with the combination of tiotropium and pulmonary rehabilitation in patients with COPD. Chest. 2005;127:809–817. doi: 10.1378/chest.127.3.809. [DOI] [PubMed] [Google Scholar]
- 19.Dolmage TE, Goldstein RS. Effects of one-legged exercise training of patients with COPD. Chest. 2008;133:370–376. doi: 10.1378/chest.07-1423. [DOI] [PubMed] [Google Scholar]
- 20.Hawkins P, Johnson LC, Nikoletou D, et al. Proportional assist ventilation as an aid to exercise training in severe chronic obstructive pulmonary disease. Thorax. 2002;57:853–859. doi: 10.1136/thorax.57.10.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van't Hul Al, Gosselink R, Hollander P, et al. Training with inspiratory pressure support in patients with severe COPD. Eur Respir J. 2006;26:65–72. doi: 10.1183/09031936.06.00036505. [DOI] [PubMed] [Google Scholar]
- 22.Vogiatzis I, Nanas S, Roussos C. Interval training as an alternative modality to continuous exercise in patients with COPD. Eur Respir J. 2002;20:12–19. doi: 10.1183/09031936.02.01152001. [DOI] [PubMed] [Google Scholar]
- 23.Sabapathy S, Kingsley RA, Schneider DA, et al. Continuous and intermittent exercise responses in individuals with chronic obstructive pulmonary disease. Thorax. 2004;59:1026–1031. doi: 10.1136/thx.2004.026617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Puhan MA, Buschinh G, Schunemann HJ, et al. Interval versus continuous high-intensity exercise in chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2006;145:816–825. doi: 10.7326/0003-4819-145-11-200612050-00006. [DOI] [PubMed] [Google Scholar]
- 25.Arnardottir RH, Boman G, Larsson K, et al. Interval training compared with continuous training in patients with COPD. Respir Med. 2007;101:1196–1204. doi: 10.1016/j.rmed.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 26.Vogiatzis I, Nanas S, Kastanakis E, et al. Dynamic hyper-inflation and tolerance to interval exercise in patients with advanced COPD. Eur Respir J. 2004;24:385–390. doi: 10.1183/09031936.04.00128903. [DOI] [PubMed] [Google Scholar]
- 27.Coppolse R, Schols AM, Baarends EM, et al. Interval versus continuous training in patients with severe COPD: a randomized clinical trial. Eur Respir J. 1999;14:258–263. doi: 10.1034/j.1399-3003.1999.14b04.x. [DOI] [PubMed] [Google Scholar]
- 28.Vogiatzis I, Terzis G, Nanas S, et al. Skeletal muscle adaptations to interval training in patients with advanced COPD. Chest. 2005;128:3838–3845. doi: 10.1378/chest.128.6.3838. [DOI] [PubMed] [Google Scholar]
- 29.Meyer K, Schwaibold M, Westbrook S, et al. Effects of short-term exercise training and activity restriction on functional capacity in patients with severe congestive heart failure. Am J Cardiol. 1996;78:1017–1022. doi: 10.1016/s0002-9149(96)00527-9. [DOI] [PubMed] [Google Scholar]
- 30.Whislof U, Stoylen A, Loennechen JP, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients. A randomized study. Circulation. 2007;115:3086–3094. doi: 10.1161/CIRCULATIONAHA.106.675041. [DOI] [PubMed] [Google Scholar]
- 31.Ahmaidi S, Masse-Biron J, Adam B, et al. Effects of interval training at the ventilatory threshold on clinical and cardiorespiratory responses in elderly humans. Eur J Appl Physiol Occup Physiol. 1998;78:170–176. doi: 10.1007/s004210050403. [DOI] [PubMed] [Google Scholar]
- 32.Morris N, Gass G, Thompson M, et al. Physiological responses to intermittent and continuous exercise at the same relative intensity in older men. Eur J Appl Physiol. 2003;90:620–625. doi: 10.1007/s00421-003-0918-z. [DOI] [PubMed] [Google Scholar]
- 33.Astrand PO, Rodahl K. Physical training. In: Astrand PO, Rodahl K, editors. Textbook of Work Physiology. New York, NY: McGraw-Hill; 1986. pp. 412–476. [Google Scholar]
- 34.Gaesser GA, Wilson LA. Effects of continuous and interval training on parameters of power-endurance time relationship for high-intensity exercise. Int J Sports Med. 1988;9:417–421. doi: 10.1055/s-2007-1025043. [DOI] [PubMed] [Google Scholar]
- 35.Gorostiaga EM, Walter CB, Foster C, et al. Uniqueness of interval and continuous training at the same maintained exercise intensity. Eur J Appl Physiol. 1991;63:101–107. doi: 10.1007/BF00235177. [DOI] [PubMed] [Google Scholar]
- 36.Poole DC, Gaesser GA. Response to ventilator and lactate thresholds to continuous and interval training. J Appl Physiol. 1985;58:1115–1121. doi: 10.1152/jappl.1985.58.4.1115. [DOI] [PubMed] [Google Scholar]
- 37.Slordahl SA, Madslien VO, Stoylen A, et al. Atrioventricular plane displacement in untrained and trained females. Med Sci Sports Exerc. 2004;36:1871–1875. doi: 10.1249/01.mss.0000145444.01292.3d. [DOI] [PubMed] [Google Scholar]
- 38.Billat VL. Interval training for performance: A scientific and empirical practice. Special recommendation for middle and long distance running. Part I: Aerobic interval training. Sports Med. 2001;31:13–31. doi: 10.2165/00007256-200131010-00002. [DOI] [PubMed] [Google Scholar]
- 39.Simoneau JA, Lortie G, Boulay MR, et al. Human skeletal muscle fiber type alteration with high intensity intermittent training. Eur J Appl Physiol. 1985;54:250–253. doi: 10.1007/BF00426141. [DOI] [PubMed] [Google Scholar]
- 40.Meyer K, Samek L, Schwaibold M, et al. Interval training in patients with severe chronic heart failure: analysis and recommendations for exercise procedures. Med Sci Sports Exerc. 1997;29:306–312. doi: 10.1097/00005768-199703000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Nilsson BB, Westhein A, Risberg MA. Effects of group high-intensity aerobic interval training in patients with chronic heart failure. Am J Cardiol. 2008;102:1361–1365. doi: 10.1016/j.amjcard.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 42.Tjonna AE, Lee AJ, Rognmo O, et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome. A pilot study. Circulation. 2008;118:346–354. doi: 10.1161/CIRCULATIONAHA.108.772822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Earnest C. The role of exercise interval training in treating cardiovascular disease risk factors. Curr Cardio Risk Rep. 2009;3:296–301. [Google Scholar]
- 44.Meyer K, Samek L, Schwaibold M, et al. Physical responses to different modes of interval exercise in patients with chronic heart failure-application to exercise training. Eur Heart J. 1996;17:1040–1047. doi: 10.1093/oxfordjournals.eurheartj.a015000. [DOI] [PubMed] [Google Scholar]
- 45.Dimopoulos S, Anastasiou-Nana M, Sakellariou D, et al. Effects of exercise rehabilitation program on heart rate recovery in patients with chronic heart failure. Eur J Cardiovasc Prev Rehabil. 2006;13:67–73. doi: 10.1097/01.hjr.0000198449.20775.7c. [DOI] [PubMed] [Google Scholar]
- 46.Roditis P, Dimopoulos S, Sakellariou D, et al. The effects of exercise training on the kinetics of oxygen up-take in patients with chronic heart failure. Eur J Cardiovasc Prev Rehabil. 2007;14:304–311. doi: 10.1097/hjr.0b013e32808621a3. [DOI] [PubMed] [Google Scholar]
- 47.Kemps HM, de Vries WR, Schmikli SL, et al. Assessment of the effects of physical training in patients with chronic heart failure: the utility of effort-independent exercise variables. Eur J Appl Physiol. 2010;108:469–476. doi: 10.1007/s00421-009-1230-3. [DOI] [PubMed] [Google Scholar]
- 48.Mador MJ, Krawza M, Alhajhusain A, et al. Interval training versus continuous training in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev. 2009;29:126–132. doi: 10.1097/HCR.0b013e31819a024f. [DOI] [PubMed] [Google Scholar]
- 49.Varga J, Porszasz J, Boda K, et al. Supervised high intensity continuous and interval training vs. self-paced training in COPD. Respir Med. 2007;101:2297–2304. doi: 10.1016/j.rmed.2007.06.017. [DOI] [PubMed] [Google Scholar]
- 50.Nasis I, Vogiatzis I, Stratakos G, et al. Effects of interval-load versus constant-load training on the BODE index in COPD patients. Respir Med. 2009;103:1392–1398. doi: 10.1016/j.rmed.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 51.Puente-Maestu L, Garcia G, Martinez-Abad Y, et al. Dyspnea, ventilatory system, and changes in dynamic hyperinflation related to the intensity of constant work rate exercise in COPD. Chest. 2005;128:651–656. doi: 10.1378/chest.128.2.651. [DOI] [PubMed] [Google Scholar]
- 52.Aliverti A, Quaranta M, Chakrabarti B, et al. Paradoxical movement of the lower ribcage at rest and during exercise in COPD patients. Eur Respir J. 2009;33:49–60. doi: 10.1183/09031936.00141607. [DOI] [PubMed] [Google Scholar]
- 53.Eliason G, Abdel-Halim S, Arvidsson B, et al. Physical performance and muscular characteristics in different stages of COPD. Scand J Med Sci Sports. 2008;19:865–870. doi: 10.1111/j.1600-0838.2008.00858.x. [DOI] [PubMed] [Google Scholar]
- 54.Koulouris NG, Dimopoulou I, Valta P, et al. Detection of expiratory flow limitation during exercise in COPD. J App Physiol. 1997;82:723–731. doi: 10.1152/jappl.1997.82.3.723. [DOI] [PubMed] [Google Scholar]
- 55.O'Donnell DE, McGuire M, Samis L, et al. General exercise training improves ventilator and peripheral muscle strength and endurance in chronic airflow limitation. Am J Respir Crit Care Med. 1998;157:1489–1497. doi: 10.1164/ajrccm.157.5.9708010. [DOI] [PubMed] [Google Scholar]
- 56.O'Donnell DE, Lam M, Webb K. Measurements of symptoms, lung hyperinflation and endurance during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;158:1557–1565. doi: 10.1164/ajrccm.158.5.9804004. [DOI] [PubMed] [Google Scholar]
- 57.O'Donnell DE, D'Arsigny C, Webb K. Effects of hyperoxia on ventilator limitation during exercise in advanced chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163:892–898. doi: 10.1164/ajrccm.163.4.2007026. [DOI] [PubMed] [Google Scholar]
- 58.Somfay A, Porszasz SM, Lee SM, et al. Dose-response effect of oxygen on hyperinflation and exercise endurance in nonhypoxaemic COPD patients. Eur Respir J. 2001;18:77–84. doi: 10.1183/09031936.01.00082201. [DOI] [PubMed] [Google Scholar]
- 59.Neder A, Jones PW, Nery LE, et al. Determinants of the exercise endurance capacity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;162:497–504. doi: 10.1164/ajrccm.162.2.9907122. [DOI] [PubMed] [Google Scholar]
- 60.Jakobsson P, Jorfeldt L, Henriksson J. Metabolic enzyme activity in the quadriceps femoris muscle in patients with severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1995;151:374–377. doi: 10.1164/ajrccm.151.2.7842194. [DOI] [PubMed] [Google Scholar]
- 61.Gosker HR, van Mameren H, van Dijk PJ, et al. Skeletal muscle fibre-type shifting and metabolic profile in patients eith chronic obstructive pulmonary disease. Eur Respir J. 2002;19:617–625. doi: 10.1183/09031936.02.00762001. [DOI] [PubMed] [Google Scholar]
- 62.Vogiatzis I, Stratakos G, Simoes D, et al. Effects of rehabilitative exercise on peripheral muscle TNFa, IL-6 and MyoD expression in patients with COPD. Thorax. 2007;62:950–956. doi: 10.1136/thx.2006.069310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Maltais F, LeBlanc P, Simard C, et al. Skeletal muscle adaptation to endurance training in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1995;154:442–447. doi: 10.1164/ajrccm.154.2.8756820. [DOI] [PubMed] [Google Scholar]
- 64.Whittom F, Jobin J, Simard PM, et al. Histochemical and morphological characteristics of the vastus lateralis muscle in patients with chronic obstructive pulmonary disease. Med Sci Sports Exerc. 1998;30:1467–1474. doi: 10.1097/00005768-199810000-00001. [DOI] [PubMed] [Google Scholar]
- 65.Breslin E. The pattern of respiratory muscle recruitment during pursed-lip breathing. Chest. 1992;101:75–78. doi: 10.1378/chest.101.1.75. [DOI] [PubMed] [Google Scholar]
- 66.Spahija J, de Marchie M, Grassino A. Effects of imposed pursed-lips breathing on respiratory mechanics and dyspnoea at rest and during exercise in COPD. Chest. 2005;128:640–650. doi: 10.1378/chest.128.2.640. [DOI] [PubMed] [Google Scholar]
- 67.Puhan MA, Schunemann HJ, Buesching G, et al. COPD patients' ability to follow exercise influences short-term outcomes of rehabilitation. Eur Respir J. 2008;31:304–310. doi: 10.1183/09031936.00078707. [DOI] [PubMed] [Google Scholar]
- 68.Troosters T, Gosselink R, Decramer M. Exericse training in COPD: how to distinguish responders from nonresponders. J Cardiopulm Rehabil. 2001;21:10–17. doi: 10.1097/00008483-200101000-00004. [DOI] [PubMed] [Google Scholar]