Abstract
Background
Most internal medicine residency programs use a night float system to comply with resident duty hour limits. Night float assignments often comprise 7 to 10 weeks of scheduled clinical time during training. Despite this substantial allotment of time to night float, few studies have assessed the adequacy of learning opportunities during these rotations. We designed an exploratory study to assess resident and faculty views about the educational aspects of a typical internal medicine night float system.
Methods
Wright State University Boonshoft School of Medicine internal medicine residents and attending faculty were asked to complete a 25-item voluntary, anonymous survey. A 5-point Likert scale was used to assess perceptions of education during day and night rotations.
Results
The response rate was 52% (85 of 164). Residents rated teaching and learning on day rotations more positively than on night rotations for 17 of 25 (68%) items. Regarding night float, residents rated 14 of 25 items below 3.00; only one item was rated below 3.00 (“…H & P skills observed by attending”) for day rotations. Attending physicians rated day rotations more highly for all 25 survey items. Faculty rated 13 of 25 items below 3.00 for night float and they rated no items below 3.00 for day rotations. Resident and faculty ratings differed significantly for 10 items, with 5 items receiving higher ratings by residents and 5 being rated more positively by faculty.
Conclusion
Despite a substantial allotment of time to night rotations, there appear to be lost teaching and learning opportunities in the current night float system. Modification of the existing format may improve its educational value.
Background
Most internal medicine residency programs use night float systems to comply with resident duty hour limits.1 Night float assignments typically comprise 7 to 10 weeks of scheduled clinical time, but programs may assign as much as 4 months of night rotations over 3 years. Despite restricted duty hours, some critics argue that residents continue to suffer sleep deprivation, which consequently may threaten patient safety.2,3 The sleep community and some safety groups advocate restrictions on continuous duty. If adopted, changes could result in more time spent in night float rotations.4
Much has been learned about night float since duty hour limits were established by the Accreditation Council for Graduate Medical Education in 2003. Reported advantages of night float include less resident stress and fatigue and enhanced alertness5,6 as well as perceptions of improved patient care and fewer errors.7 Other studies have focused on potential disadvantages such as service versus education,8,9 discontinuous patient care,10 nurse and patient satisfaction,11 and the nuances of patient sign-outs.12 The perceptions of night float are inconsistent in these reports; some aspects are viewed positively and others are viewed as neutral or negative.
Despite the substantial allotment of time given to night float, few studies have assessed the quality of educational activities or the adequacy of teaching opportunities during these rotations. Lefrak et al13 found that surgery residents on night float attended fewer conferences, had fewer teaching interactions, and performed fewer operative procedures than their colleagues on day rotations. To address those concerns and to improve faculty presence, additional nighttime conferences and tutorials, supervised by attending physicians, were initiated. Akl et al11 compared the perceptions of residents, attending physicians, and nurses for the domains of patient care, resident training, and resident performance for an internal medicine night float system. Although perceptions about the night float system were generally negative, residents had more positive perceptions than attending physicians and nurses, especially regarding patient care. Jasti et al7 found that internal medicine residents believed that night float improved the quality of patient care and resulted in fewer medical errors. Most residents favored night float compared with traditional call, but also thought that there was less emphasis on education and more emphasis on service during night float rotations.
We conducted an exploratory survey to better understand resident and faculty perceptions regarding specific learning opportunities and teaching effectiveness during night float hospital rotations in our internal medicine residency program. The end-of-rotation evaluations completed by residents have always assessed night float education and teaching positively (an average of 4.3 on a 5-point scale). Nevertheless, we hypothesized that direct comparison of night and day rotations would indicate opportunities for improvement on night float.
Methods
Night Rotations at Our Institution
The Wright State University Boonshoft School of Medicine uses 4 hospitals (2 community hospitals, 1 military institution, and 1 Veterans Affairs medical center) in the education of its 85 internal medicine residents. Each site has night float team coverage for 6 days each week. The system at each site is similar and has been in place for 6 years. The current night float routine has not been modified in any substantial way during the training of all residents responding to the questionnaire.
Residents spend approximately the same amount of clinical time at each site, and their night float assignments are also equally distributed among sites. Each night float team consists of a first-year resident and a senior resident or 2 senior residents. Residents admit patients between 7:30 pm and 7:30 am and cross-cover for other residents. Night float residents participate in morning and evening patient checkout conferences as well as weekday morning reports. Each year, a resident completes two 2-week night float rotations; a resident is never assigned to 2 consecutive night rotations. Thus, a resident's 12 weeks of night rotations over 3 years total 8% to 10% of his/her clinical time.
Survey
The authors and the internal medicine residency program director developed the 25-item questionnaire through an iterative process in which potential items were vetted, improved for clarity, and discarded if judged to be redundant. The questionnaire items (see tables 1–3) asked about both day and night rotations. Participants were not given guidance on how to interpret survey questions. A 5-point Likert scale was employed (1 = strongly disagree, 5 = strongly agree). The survey also requested open-ended comments.
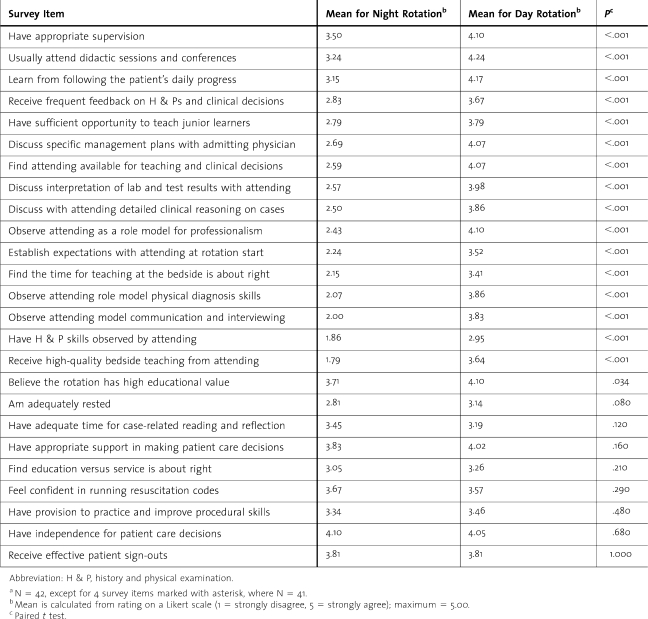
Table 1.
Night Rotation Versus Day Rotation: Internal Medicine Residentsa
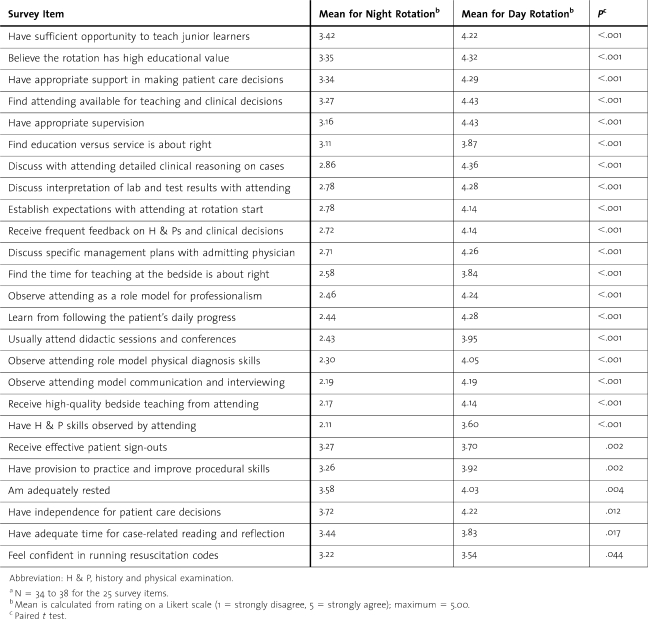
Table 2.
Night Rotation Versus Day Rotation: Internal Medicine Facultya
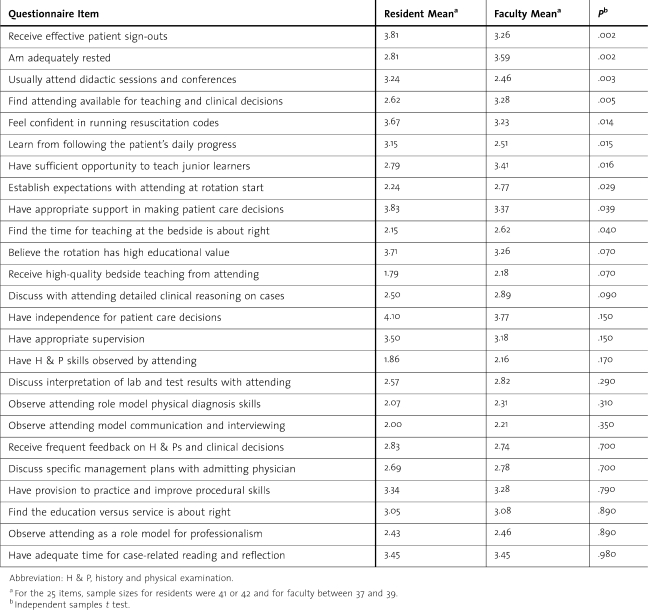
Table 3.
Comparison Between Residents And Faculty: Night Rotation
All 85 internal medicine residents were asked to complete the questionnaire between May 2009 and June 2009 (ie, shortly before the end of the 2008–2009 academic year). Consequently, most first-year residents had experienced 2 to 4 weeks of night float, most second-year residents had experienced between 6 and 8 weeks, and most third-year residents had experienced between 10 and 12 weeks at the time of survey.
During May to June 2009, the survey was also administered to 79 teaching faculty who regularly attend on the inpatient general medicine service, typically from 1 to 3 months each year. Faculty respondents were Veterans Affairs physicians, Air Force physicians, and paid Wright State University Boonshoft School of Medicine physicians. Night float education and service activities and faculty expectations are similar for each site. The attending physician has responsibility for all patient care on the service and supervises residents, although the attending physician does not need to be physically present during each patient encounter. Attending physicians take calls from home, averaging 2 phone calls per night; they do not often come to the hospital at night, but are expected to participate in the resident checkout conference.
Statistical Analysis
All 25 items on the survey were phrased so that an agree rating was positive. Consequently, a participant's response was coded as follows: strongly disagree = 1, disagree = 2, neutral = 3, agree = 4, and strongly agree = 5. The paired t test was used to compare responses about night float versus day rotations for residents and faculty. Additionally, resident perceptions about night float rotations were compared with faculty perceptions about night float using the independent samples t test. Inferences were made at the .05 level of significance with no correction for multiple comparisons.
The survey was approved by the Wright State University Institutional Review Board (SC No. 3923) and completed anonymously and voluntarily.
Results
The overall response rate was 52% (85 of 164); 46 of 85 (54%) residents and 39 of 79 (49%) faculty responded. Residents rated day rotations higher than night rotations for 17 of the 25 items (table 1). The 8 items on which day and night did not differ for residents were independence for patient care decisions, appropriate support for clinical decisions, receiving effective patient sign-outs, adequate time for case-related reading and reflection, confidence in running resuscitation codes, adequate rest, balance between service and education, and provision for practicing and improving procedural skills. On the key item of adequate rest, both day (3.14) and night (2.81) scores were close to a mean rating of neutral. Regarding night float, residents rated 14 of 25 items below 3.00; only 1 item was below 3.00 for day rotations, (“….H & P skills observed by attending”).
For all 25 items, faculty rated day rotations superior to night. Regarding night float, faculty rated 13 of 25 items below 3.00; no items were below 3.00 for day rotations (table 2).
table 3 shows the comparisons between residents and faculty on night rotations. Compared with faculty, residents gave higher ratings to 5 survey items. Residents were more positive regarding their attendance at didactic conferences during night float, having appropriate support for patient care decisions, learning from following the daily progress of patients, receiving effective patient sign-outs, and having confidence in running resuscitation codes. In contrast, faculty rated 5 items higher than residents: sufficient opportunity for residents to teach junior learners, availability of attending physicians for teaching and clinical decisions, establishing expectations at the start of a night rotation, residents being adequately rested, and having appropriate amount of time for bedside teaching.
Nearly one-fourth of residents who completed the survey (11 of 46) wrote open-ended comments. Almost all comments emphasized positive aspects of the night float rotation, often citing independent decision making and the honing of time-efficiency skills (eg, “night float serves as a crash course in time management”; “I learned the most because I covered a lot of patients with serious issues”). Although generally considered a valuable experience, 10% of responses invited greater involvement by attending physicians in night float rotations.
Discussion
Past studies have generally found reduction in resident fatigue, improvement in quality of life, and perceptions of better patient care when programs change from the traditional (overnight) call system to night float scheduling. Yet both residents and faculty view many aspects of night float less favorably than day rotations. Our study adds to the understanding of the educational value of night float rotations and what elements might be addressed to enhance the experience.
The list of potential educational activities we studied is not exhaustive. The items studied are among many key activities historically considered to be important clinical education components for inpatient rotations, but most have not been studied previously in regard to night float activities. In prior studies of night float, residents have reported that their training is potentially impaired by reduced continuity of care, less educational emphasis, and decreased availability of attending physicians.7,11 In our study, residents rated day rotations more favorably than night rotations for most educational opportunities and faculty rated day rotations superior in all educational aspects. In sum, both residents and faculty perceive night float to be potentially inadequate in the broader domains of attending physician role-modeling, trainee observation, feedback, bedside teaching, and clinical reasoning.
Although night float scheduling may result in less resident fatigue than traditional call systems,6 studies suggest that the disturbances of sleep and mood that are common in night shift work are also present in night float rotations.5 We found similar results; that is, residents do not feel adequately rested during night rotations. The graduate medical education community continues to search for optimal solutions to the sleep deprivation problem. Sleep science studies support the need for faculty to recognize that increased fatigue results from night duty.14,15
Many medical educators advocate bedside teaching as the best vehicle to impart clinical skills (eg, history and examination skills, clinical ethics, humanism, and professionalism).16 Historically, residents spend only 16% of traditional call time directly involved in patient care and less than 3% of their time is directly supervised by attending physicians.17 Although the optimal amount of supervision may be debatable, increased faculty presence is associated with higher resident satisfaction and more favorable learning experiences.18 Perhaps modification of the current night float system to include an evening report with attending physicians or scheduled night shift rounding could address these issues and improve the quality of the resident learning experience.
Integrating hospitalist faculty into night rotations may address some of the educational inadequacies of night float, especially availability of attending physicians, role modeling, and discussions about clinical reasoning. It is unclear whether hospitalist educators substantially impact bedside teaching, but learners assess them positively for their teaching effectiveness and availability.19,20
Finally, although teaching methods such as evening report, night rounding, and real-time patient precepting at night are not well described in the literature, these instructional approaches hold promise and may be implemented at our institution. Regardless of the strategies used to promote greater nighttime presence of faculty, the approach should preserve appropriate resident independence, a perceived strength of the current system. Our residents do not believe their independence is limited during day rotations (mean = 4.05) when attending physicians are always present. Thus, increased faculty presence during night rotations does not need to reduce independence during this period. Lastly, the success of any new process rests heavily on the preparation and performance of faculty in creating an effective learning environment.
Our study has some limitations. First, the response rate (52%), while similar to that of other surveys of physicians,21 was not high. In addition, we surveyed a single residency program, which limits the generalizability of our results to other internal medicine residency programs and specialties. Future studies should include multiple residency programs and specialties. Also, our questionnaire had not been validated previously, but we chose questions designed to investigate typical teaching methods employed in our general medicine and subspecialty elective inpatient rotations.
Another limitation may be differences between residents and faculty in the interpretation of some survey items. Because formal didactic conferences are not scheduled during night float, it was surprising that residents gave this item a mean rating of 3.24 (vs 2.46 for faculty). Residents may have interpreted this item to include patient care conferences (morning report), while faculty did not categorize this session as a didactic conference. Further, faculty may have determined that the lack of noon lectures and journal clubs was reason to give a lower rating to this item. Similarly, residents rated learning from following the patient's daily progress during night float higher than faculty (3.15 vs 2.51). Perhaps this disparity was because residents were engaging in the follow-up care of patients either out of personal educational interest or through cross-cover. Finally, faculty rated the opportunity for trainees to teach junior learners during night float higher than residents (3.41 vs 2.79). Although our day rotation teams include medical students, they are not routinely part of night float teams. All residents are aware that students are not part of the night float team, but many faculty may not be aware of this scheduling decision.
Conclusion
Although differing in some perceptions about night float, residents and faculty generally found that trainees are less likely to experience many important elements of clinical education during night rotations compared with day rotations. Despite the substantial allotment of time to night rotations, there are many lost teaching and learning opportunities in the current night float system. Modification of the existing night float format may improve its overall educational value.
Footnotes
Both authors are at Boonshoft School of Medicine, Wright State University. Dean A. Bricker, MD, is Associate Program Director of the Internal Medicine Residency program; and Ronald J. Markert, PhD, is Professor of Medicine and Orthopedic Surgery and Vice Chair for Research, Department of Internal Medicine.
References
- 1.Wallach L. S., Alam K., Diaz N., Shine D. How do internal medicine residency programs evaluate their resident float experiences? South Med J. 2006;99(9):919–923. doi: 10.1097/01.smj.0000235501.62397.ef. [DOI] [PubMed] [Google Scholar]
- 2.Arora V. M., Georgitis E., Siddique J., et al. Association of workload of on-call medical interns with on-call sleep duration, shift duration, and participation in educational activities. JAMA. 2008;300(10):1146–1153. doi: 10.1001/jama.300.10.1146. [DOI] [PubMed] [Google Scholar]
- 3.Lockley S. W., Barger L. K., Ayas N. T., et al. Effects of health are provider work hours and sleep deprivation on safety and performance. Jt Comm J Qual Patient Saf. 2007;33(suppl 11):7–18. doi: 10.1016/s1553-7250(07)33109-7. [DOI] [PubMed] [Google Scholar]
- 4.Iglehart J. K. Revisiting duty-hour limits: IOM recommendations for patient safety and resident education. N Engl J Med. 2008;359(25):2633–2635. doi: 10.1056/NEJMp0808736. [DOI] [PubMed] [Google Scholar]
- 5.Cavallo A., Jaskiewicz J., Ris M. D. Impact of night-float rotation on sleep, mood, and alertness: the resident's perception. Chronobiol Int. 2002;19(5):893–902. doi: 10.1081/cbi-120014106. [DOI] [PubMed] [Google Scholar]
- 6.Goldstein M. J., Kim E., Widmann W. D., Hardy M. A. A 360 degrees evaluation of a night-float system for general surgery: a response to mandated work-hours reduction. Curr Surg. 2004;61(5):445–451. doi: 10.1016/j.cursur.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 7.Jasti H., Hanusa B. H., Switzer G. E., Granieri R., Elnicki M. Residents' perceptions of a night float system. BMC Med Educ. 2009;9:52. doi: 10.1186/1472-6920-9-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wood V. C., Markert R. J., McGlynn T. J. Internal medicine residents' perceptions of the balance between service and education in their night-call activities. Acad Med. 1993;68(8):640–642. doi: 10.1097/00001888-199308000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Hayward R. S., Rockwood K., Sheehan G. J., Bass E. B. A phenomenology of scut. Ann Intern Med. 1991;115(5):372–376. doi: 10.7326/0003-4819-115-5-372. [DOI] [PubMed] [Google Scholar]
- 10.Vaughn D. M., Stout C. L., McCampbell B. L., et al. Three-year results of mandated work hour restrictions: attending and resident perspectives and effects in a community hospital. Am Surg. 2008;74(6):542–546. [PubMed] [Google Scholar]
- 11.Akl E. A., Bais A., Rich E., Izzo J., Grant B. J., Schunemann H. J. Brief report: internal medicine residents', attendings', and nurses' perceptions of the night float system. J Gen Intern Med. 2006;21(5):494–497. doi: 10.1111/j.1525-1497.2006.00434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horwitz L. I., Moin T., Krumholz H. M., Wang L., Bradley E. H. Consequences of inadequate sign-out for patient care. Arch Intern Med. 2008;168(16):1755–1760. doi: 10.1001/archinte.168.16.1755. [DOI] [PubMed] [Google Scholar]
- 13.Lefrak S., Miller S., Schirmer B., Sanfey H. The night float system: ensuring educational benefit. Am J Surg. 2005;189(6):639–642. doi: 10.1016/j.amjsurg.2004.11.034. [DOI] [PubMed] [Google Scholar]
- 14.Gohar A., Adams A., Gertner E., et al. Working memory capacity is decreased in sleep-deprived internal medicine residents. J Clin Sleep Med. 2009;5(3):191–197. [PMC free article] [PubMed] [Google Scholar]
- 15.Rose M., Manser T., Ware J. C. Effects of call on sleep and mood in internal medicine residents. Behav Sleep Med. 2008;6(2):75–88. doi: 10.1080/15402000801952914. [DOI] [PubMed] [Google Scholar]
- 16.Janicik R. W., Fletcher K. E. Teaching at the bedside: a new model. Med Teach. 2003;25(2):127–130. doi: 10.1080/0142159031000092490. [DOI] [PubMed] [Google Scholar]
- 17.Nerenze D., Rosman H., Newcomb C., et al. The on-call experience of interns in internal medicine. Arch Intern Med. 1990;150(11):2294–2297. [PubMed] [Google Scholar]
- 18.Phy M. P., Offord K. P., Manning D. M., Bundrick J. B., Huddleston J. M. Increased faculty presence on inpatient teaching services. Mayo Clin Proc. 2004;79(3):332–336. doi: 10.4065/79.3.332. [DOI] [PubMed] [Google Scholar]
- 19.Crumlish C. M., Yialamas M. A., McMahon G. T. Quantification of bedside teaching by an academic hospitalist group. J Hosp Med. 2009;4(5):304–307. doi: 10.1002/jhm.540. [DOI] [PubMed] [Google Scholar]
- 20.Goldenberg J., Glasheen J. J. Hospitalist educators: future of inpatient internal medicine training. Mt Sinai J Med. 2008;75(5):430–435. doi: 10.1002/msj.20075. [DOI] [PubMed] [Google Scholar]
- 21.Kellerman S. E., Herold J. Physician response to surveys: a review of the literature. Am J Prev Med. 2001;20(1):61–67. doi: 10.1016/s0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]