Abstract
Objective
To assess whether loss of consistency or systematic measurement error is introduced by allowing older individuals to use a cane during measurement of self-selected walking speed (SSWS).
Study Design and Setting
Observational study of women aged 65+ (Women’s Health and Aging Study I, n=1,002).
Results
Of individuals who use a cane in daily life, 201 (50.76%) did not use an aid during testing. The Coefficient of Variation was low in individuals who reported cane use in daily life but did not use one in testing (10.72%), and did not vary substantially if a cane was used (12.04%). The Intra-Class Correlation Coefficient was high: 0.958 for those who reported cane use in daily life but did not use one during testing and 0.962 for those who used a cane. In both groups, Bland-Altman plots revealed a small systematic difference between the first and second trials. There was no evidence of effect modification of the association between SSWS and mobility disability by cane use during testing.
Conclusion
This observational study found no evidence of poorer consistency nor increased measurement bias in SSWS recorded while using a cane compared to no assistive device.
Keywords: Assistive Devices, Walking Speed, Gait
1. Introduction
Self-selected walking speed (SSWS) provides valuable information on mobility and is easy to measure, leading to widespread use in studies of physical function in older adults and the suggestion that it be measured at clinical visits as a vital sign.[1] Sometimes referred to as usual or preferred walking speed or gait speed, SSWS is a potent prognostic indicator in older adults that has been shown to predict falls, institutionalization and death.[2, 3] It is commonly obtained by measuring the time it takes to complete a short course such as 4 meters and therefore does not require a special setting nor costly equipment.
In both research settings and clinical practice, SSWS is obtained by asking subjects to walk in a usual manner, allowing use of their customary assistive device, such as a cane. Such a protocol implicitly chooses between two limitations. On one hand, forbidding device use excludes individuals who are not willing or able to perform the test without their device and produces an observation that does not reflect real-world function for those who rely on devices for mobility. On the other hand, allowing use is analogous to a protocol that allows individuals to choose whether blood pressure is measured seated or supine. Since device use can change the energy demands of walking[4] it is possible that using a device modifies the relationship between recorded SSWS and mobility disability. Growth in the number of adults using assistive devices for walking[5] necessitates that we understand how to consistently gather and use the important information derived from the SSWS test.
It can reasonably be expected that the use of assistive devices for walking interferes with the rhythmic and balanced nature of gait in a manner equivalent to altering testing conditions; or, that device use is a potential marker for individuals with abnormal, irregular gait independent of a device effect per se. In either case, SSWS recorded while a subject uses a device would need to be measured or interpreted differently. Our paper examines the hypothesis that loss of consistency or systematic measurement error is introduced by allowing older individuals to use an assistive device during measurement of SSWS. We use data from an observational study of older women to compare individuals who chose to use a device during measurement of SSWS with those who did not. To ascertain the presence of measurement differences in SSWS according to device use, we examine the relationships between reported device use in daily life, use during testing, and SSWS. Then we estimate the consistency (or, test-retest reliability) of repeated trials in the two groups and compare plots of systematic variation in SSWS recorded with and without a device. Finally, we examine whether there is evidence that using a device while recording SSWS modifies the association between SSWS and mobility disability.
2. Methods
2.1. Data
Data are from the Women’s Health and Aging Study I, a population-based, prospective, observational study of moderately to severely disabled community-dwelling older women designed to study the course of physical disability.[6] The cohort was derived from an age-stratified random sample using Medicare data of 32,538 women aged ≥65 years living in eastern Baltimore city and county. Of 5,316 randomly selected women, 4,137 agreed to an in-home screening interview. Inclusion criteria were both of the following: self-report of difficulty or dependence with tasks in two or more of the following four functional domains: mobility, upper extremity function, higher functioning tasks, and self-care tasks; and Mini-Mental State Exam[7] score ≥18. A total of 1,002 women (78% of those eligible) enrolled. The Johns Hopkins Medicine Institutional Review Board approved the study.
2.2. Collection of SSWS, observed device use, and reported device use
Walking speed was obtained as the time (to 0.1 second) needed to cover a 4-meter course. A straight 4-meter course was not available in 85 participant homes, so a 3-meter course was used. Participants were told “Now we are going to observe how you normally walk. If you use a cane or a walking aid and would feel more comfortable with it, you may use it.” Time began with a verbal command to start walking (“Ready, Begin”) from a standing start with both feet touching a starting line, and ended when a foot broke the plane of the finishing line. Instructions and a demonstration were given to keep walking past the finish line without stopping. Human assistance was not allowed. Two trials were performed with no structured delay. A separate part of the exam encompassed an interview that asked about daily life, and all participants were asked “When you walk, do you use a cane? –walker? –wheelchair?” Responses to these questions were not mutually exclusive.
2.3 Mobility Disability Measures
Two measures of mobility were used as outcomes to ensure convergence and avoid single-item variability. One was assessed by asking participants if they experienced difficulty walking across a small room (yes or no). The second was defined using a validated lower extremity functional limitation scale (scored 0–9) [8] drawn from additional questions regarding difficulty walking different distances and stooping.
2.4 Analytic Methods
We first compare SSWS across groups defined according to aid use during the test using summary statistics and box plots. By far the most used frequently used mobility aid was a cane and few women used other aids (e.g., walkers) during testing. Thus we perform statistical comparisons between individuals who used a cane or no aid during testing. We estimated intra-individual reliability for the two trials of SSWS using two indices of consistency. The within-subject Coefficient of Variation (CV) represents the standard deviation as a percentage of mean of the two paired trials and was calculated using root mean squared approach.[10, 11]. The Intra-Class Correlation Coefficient (ICC) represents the proportion of variability attributable to differences between individuals and was calculated using repeated measures analysis of variance to produce a measure of absolute agreement (type ICC2(A,k)).[9]
We assessed systematic variation in measurement between the repeated tests using Bland-Altman plots[12] and associated regression models. These plots show how the difference between the paired SSWS trials (on the y-axis) is associated with the mean of the two trials (on the x-axis). To test statistically whether the variability shown in the plots significantly increased or decreased with observed walking speed, we estimated linear regression models separately for non-aid and cane users, with the difference between SSWS trials as the dependent variable and the mean of trials as the predictor. We also estimated a linear regression model on the entire sample to test for a difference in slopes, by using difference in SSWS between trials as the dependent variable and mean of trials, observed cane use and an interaction term as predictors. Finally, we use logistic and linear regression to examine the association between SSWS and mobility disability by device use, using an interaction term for cane use * SSWS to test for a modification effect. Stata Special Edition version 9.2[13] was used for all analyses.
3. Results
3.1 Association of self-reported and observed device use and SSWS
Of the 1,002 participants in the study, 31 were missing data on self-reported use of a walking aid. An additional 17 participants had missing data on SSWS and 7 chose to use an “other aid” (such as pushing a wheelchair) rather than use a cane or walker during the test. The mean age of the women was 78.4 years and 28.0% were black. Participants’ average years of education was 9.7, average Mini-Mental State Exam score was 26.4 and average number of chronic diseases was 2.0.
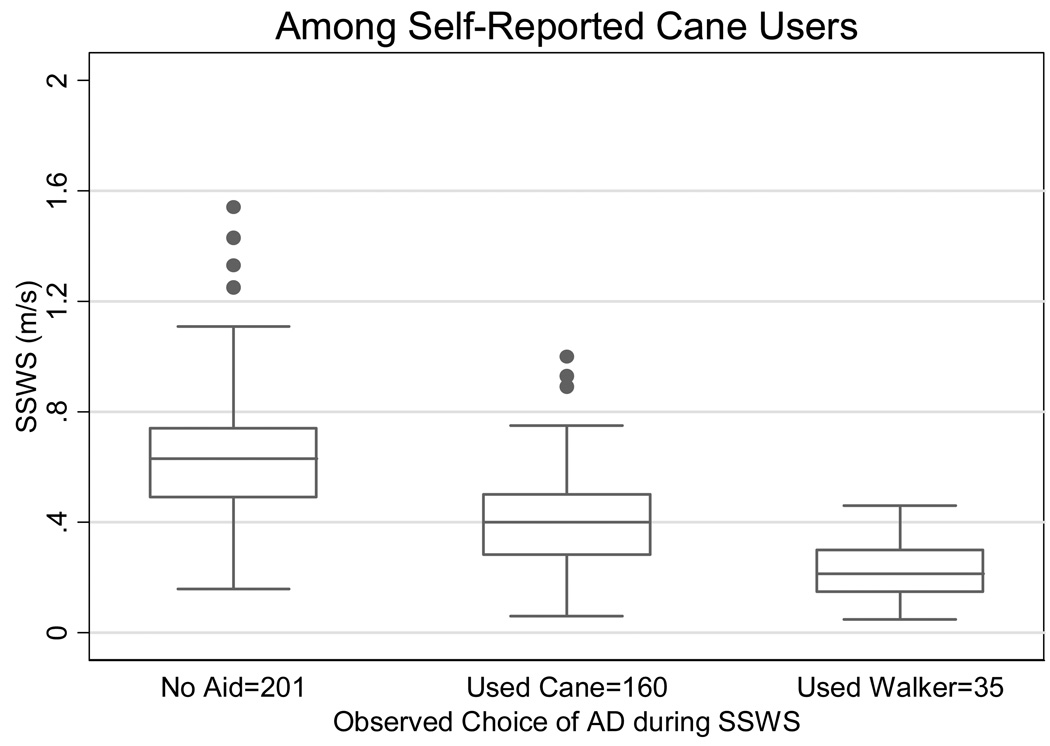
The relationship between self-reported aid use, observed aid use and mean SSWS is shown in Table 1. Among individuals with full data, 396 (41.51%) reported using a cane and 120 (12.58%) reported walker use. Of individuals who use a cane in daily life, 201 (50.76%) did not use any aid during testing, consistent with the notion that many individuals who use a cane in daily life may not always need it, especially at home. Individuals who used a cane during the test walked significantly slower, on average, than individuals who used no aid, and faster than those who used a walker (0.409, versus 0.636 and 0.229 m/s, respectively; pairwise P-values all <0.001). Figure 1 demonstrates that this result may be because few cane users walked faster than 1.0 m/s and few walker users walked faster than 0.4 m/s.
Table 1.
Self-selected walking speed according to patterns of self-reported use in daily life and observed device use during testing.
| n | (%) | Mean SSWS, m/s | (95% CI) | ||
|---|---|---|---|---|---|
| Report do not use assistive device: | |||||
| Observed use during testing: |
No Aid | 485 | (99.18) | 0.78 | (0.76–0.80) |
| Used Cane | 3 | ( 0.61) | 0.27 | - | |
| Used Walker | 1 | ( 0.20) | 0.20 | - | |
| Total | 489 | ||||
| Report use cane*: | |||||
| Observed use during testing: |
No Aid | 201 | (50.76) | 0.64 | (0.61–0.67) |
| Used Cane | 160 | (40.40) | 0.41 | (0.38–0.44) | |
| Used Walker | 35 | ( 8.84) | 0.22 | (0.19–0.26) | |
| Total | 396 | ||||
| Report use walker*: | |||||
| Observed use during testing: |
No Aid | 22 | (18.33) | 0.54 | (0.46–0.63) |
| Used Cane | 28 | (23.33) | 0.34 | (0.28–0.41) | |
| Used Walker | 69 | (57.50) | 0.21 | (0.19–0.23) | |
| Total | 120 | ||||
Categories not mutually exclusive.
Figure 1.
Distribution of self-selected walking speed among individuals who report using a cane in daily life, according to use during testing.
3.2 Consistency
There was very little switching of devices between the two SSWS trials: 5 individuals used no aid during the first trial then a cane in the second; 1 individual used a walker then no aid (κ for device agreement between trials = 99.37%). These 6 individuals who switched and the 69 who used a walker were not included in consistency estimates, leaving a sample of 866. Table 2 shows consistency estimates stratified by self-reported daily life cane use and cane use during testing. The CV estimate was slightly higher in individuals who reported cane use in daily life and used a cane during testing (12.04%), compared to those who did not use a cane, regardless of self-report (both groups 10.72%). The ICC was high across all strata: 0.967 for individuals who did not use a cane in daily life nor the test, 0.958 for those who did use a cane in daily life but not the test and 0.962 for those who reported daily life use and used a cane during testing. Results for individuals who performed the 3-meter short course were consistent with the main findings with the exception that the CV was slightly higher among those who did not use an aid during testing: 14.49 (95% confidence interval 11.14–17.20).
Table 2.
Within-subject walking speed consistency (trial 1 vs. trial 2) according to self-reported cane use in daily life and cane use during testing.
| Self-Reported Use in Daily Life |
Used during SSWS testing |
n | CV | (95% CI) | ICC | (95% CI) |
|---|---|---|---|---|---|---|
| No aid | No aid | 502 | 10.72 | (9.65–11.70) | 0.96 | (0.96–0.97) |
| No aid | Used cane | 3 | - | - | - | - |
| Use Cane | No aid | 201 | 10.72 | (9.65–11.70) | 0.95 | (0.94–0.96) |
| Use Cane | Used cane | 160 | 12.04 | (10.50–13.40) | 0.96 | (0.95–0.96) |
CV=Coefficient of Variation. ICC = Intra-class Correlation Coefficient. 95% CI = 95% Confidence Intervals.
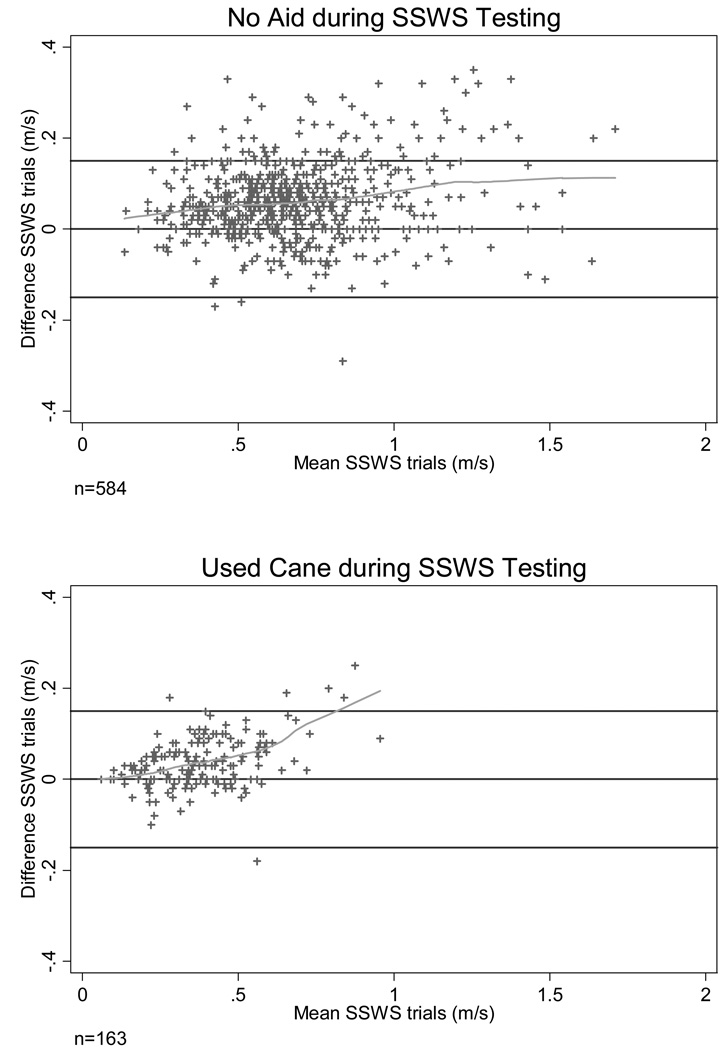
We explored the extent to which measurement error in SSWS may be systematic, and vary by cane use, through inspection of the Bland-Altman plots. Figure 2 shows that test-repeat variability varied across the range of observed values. There was a monotonic increase in the difference between SSWS trials across SSWS (top half of Figure 2) among individuals who used no aid. This suggests a systematic difference between the first and second trials of SSWS, namely that the second trial was more likely to be faster than the first (line above 0) and that the difference increased with increasing walking speeds (slope of line >0). Furthermore, this systematic variation appeared more pronounced among cane users than non-users (bottom half of Figure 2), though data are sparse between 0.4 and 1.0 m/s. These two findings were not accompanied by increased measurement error in either group, which would have been evident by a trumpet-shaped scatterplot. Both slopes significantly increased (coefficients from resistant linear regression models 0.047 and 0.158 respectively, both P-values <0.001). The two slopes were significantly different (P-value for cane use*mean SSWS interaction term = 0.005). Compared to those using no aid, the difference between SSWS from repeated trails was smaller among cane users (less vertical spread).
Figure 2.
Bland-Altman plots of SSWS: trial 1 vs. trial 2 at baseline, by cane use.
Dashed lines from locally-weighted scatterplot smoothers that allow non-linearity. Solid lines identify perfect agreement and +/− 1.96 standard deviations of difference. From linear regression, slope for no aid users = 0.047 (95%CI: 0.025–0.069) and for cane users 0.158 (0.11–0.21); Wald test for difference between slopes P-value = 0.005.
3.3 Effect modification of relationship between SSWS and mobility disability
Table 3 evaluates the hypothesis that using a device during walking modifies the relationship between measured walking speed and mobility disability. Results from the tests of effect modification using multivariable models are shown in Table 3. Six individuals were missing their initial SSWS measurement and 10 were missing the second measure, so analyses include 860 and 856 individuals, respectively. For both mobility disability measures, observed cane use was strongly associated with mobility after accounting for SSWS, however there was no evidence for effect modification of this relationship (interaction term P-values 0.880 for difficulty walking across room and 0.509 for lower extremity functional limitation scale). After adding self-reported cane use to the models, observed cane use remained associated with mobility disability and the interaction term remained insignificant.
Table 3.
Effect modification of relationship between SSWS and mobility disability measures by use of device during testing.
| Mobility Disability Measure |
Model 1 | Model 2 | ||
|---|---|---|---|---|
| OR | P-value | OR | P-value | |
| 1. Difficulty walking across room (yes/no): | ||||
| SSWS* | 0.69 | 0.000 | 0.71 | 0.000 |
| Used Cane during Testing |
3.54 | 0.036 | 3.00 | 0.072 |
| Interaction term | 1.20 | 0.880 | 0.77 | 0.835 |
| Self-Report Cane Use in Daily Life |
- | - | 2.10 | 0.003 |
| Model C-statistic | 0.82 | 0.83 | ||
| 2. Lower extremity functional limitation scale (0–9): | ||||
| Coefficient | P-value | Coefficient | P-value | |
| SSWS* | −0.34 | 0.000 | −0.30 | 0.000 |
| Used Cane during Testing |
2.42 | 0.000 | 2.02 | 0.000 |
| Interaction term | −0.72 | 0.509 | −1.28 | 0.228 |
| Self-Report Cane Use in Daily Life |
- | - | 1.17 | 0.000 |
| Model R2 | 0.32 | 0.34 | ||
For all models, observed cane and self-reported cane use variables maintain no aid use as reference. For mobility disability measure 1 models are logistic regression, for measure 2 linear regression.
SSWS scaled to 0.1 m/s to ease interpretability.
4. Discussion
This study rejects the hypothesis that allowing cane use while measuring self-selected walking speed introduces poor consistency and fails to find evidence that allowing a cane introduces a systematic measurement difference. We found that SSWS measured among individuals who used a cane was consistent, or reliable. The fact that cane use was seen only at slower walking speeds probably contributes to this consistency. The within-subject CVs suggest a reassuringly low level of test-repeat variability such that measured SSWS is a reasonable estimation of “true” SSWS. The ICCs reported here can be correctly interpreted as indicating that measured SSWS also meaningfully distinguishes between individuals. In other words most of the observed variation is due to differences between individuals, which is most often of clinical interest. In addition, SSWS measured with a cane has comparable systematic variability to SSWS recorded without an aid, such that a second trial tends to be faster.
Our findings support and extend prior work on the test-retest reliability of SSWS, which reports similar reliability in 230 healthy older individuals (ICC 0.903).[14] This finding held even among the slower individuals who use a cane during the test. In addition, this test has been found to be responsive[15] and to provide a reliable and objective measure of function over days or weeks.[16, 17]
Pending data from a definitive investigation of SSWS tested both with and without a device in individuals who report cane use during daily activities, our findings can reasonably lead to several recommendations for measurement of SSWS in older adults. First, we suggest that researchers and clinicians permit individuals to use their customary cane rather than exclude them from the test. Second, it is important that researchers and clinicians record whether a device was used during the SSWS test. It is noteworthy that our multivariate models of relationships to the mobility disability measures showed that observed device use remained significant in one case and borderline significant in the other, and had a larger coefficient than reported device use, suggesting that it is a marker of elevated likelihood of disability. Third, based on the small systematic tendency for the second trial to be faster than the first, and the amount of these differences (Figure 2), we recommend that protocols include two trials of walking speed. Finally, SSWS testing with and without a device in the same individual may be informative, as a significant proportion of individuals who use a cane do not use it all the time and it may be that device use alters the course of activity and disability in those individuals.
A limitation of this study is that it does not have the data that would most directly examine the potential effect of device use on measurement variability: SSWS with and without a device for the same individual. To our knowledge, such data have not been published. This is probably because there has been little to no research on individuals who use mobility devices intermittently and safety concerns may prohibit such examinations in a number of those subjects. We also note that the possibility of a type II error in interpreting the large P-value for the interaction term in our models of effect modification. Our analysis of over 850 older adults failed to find an effect, but this is not proof of an absence of effect. Another limitation of this study is that analysis is limited to cane use. The results may be different for other aids.
An important possibility not addressed in this paper is that individuals who chose to use their device during testing were more likely to have walking impairments than individuals who used no aid. Assistive devices for walking are not usually adopted by individuals with intact walking ability, probably because they do not add to their comfort or efficiency of walking under normal conditions. The findings here support other studies showing that device use is associated with poor performance, not just on walking speed but on aid-independent objective measures such as repeated chair stands.[18] The individuals who chose to use their device during testing may also be systematically different in other important ways. Though they are slower on average, it is unknown whether device use contributes to a poorer prognosis. Subsequent work to determine whether accounting for device use during testing improves the predictive power of SSWS may be fruitful.
In summary, this observational study of older women found no substantial evidence of loss of consistency nor increased measurement bias in self-selected walking speed recorded while using a cane compared to no assistive device.
What is new?
| Key finding: | -Self-selected walking speed (SSWS) recorded while an older person used a cane was consistent. |
| What this adds to what is known: |
-Among older women who used a cane in daily life, roughly half chose to use a cane during SSWS testing. |
| -Cane use was not associated with loss of consistency (neither substantially increased Coefficient of Variation nor decreased Intra-Class Correlation Coefficient). |
|
| Implications: | -Researchers and clinicians may permit people to use a customary cane while recording SSWS. |
Acknowledgements
The original study for this research was funded by NIA N01AG12112 and supported by NIH NCRR M01-RR00052. Dr. Weiss was funded by NIA T32AG00247. Drs. Seplaki and Weiss were funded by NIA P30 AG021334–04. We also thank Dr. Jack Guralnik for helpful comments on a draft and Dr. Qilu Yu for statistical advice.
References
- 1.Studenski S, Perera S, Wallace D, Chandler JM, Duncan PW, Rooney E, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322. doi: 10.1046/j.1532-5415.2003.51104.x. [DOI] [PubMed] [Google Scholar]
- 2.Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 3.Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, et al. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 4.Fisher SV, Gullickson G., Jr Energy cost of ambulation in health and disability: a literature review. Arch Phys Med Rehabil. 1978;59:124–133. [PubMed] [Google Scholar]
- 5.Freedman VA, Martin LG. Understanding trends in functional limitations among older Americans. Am J Public Health. 1998;88:1457–1462. doi: 10.2105/ajph.88.10.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kasper JD, Shapiro S, Guralnik JM, Bandeen-Roche KJ, Fried LP. Designing a community study of moderately to severely disabled older women: the Women's Health and Aging Study. Ann Epidemiol. 1999;9:498–507. doi: 10.1016/s1047-2797(99)00026-5. [DOI] [PubMed] [Google Scholar]
- 7.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov;:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 8.Simonsick EM, Kasper JD, Guralnik JM, Bandeen-Roche K, Ferrucci L, Hirsch R, et al. Severity of upper and lower extremity functional limitation: scale development and validation with self-report and performance-based measures of physical function. WHAS Research Group. Women's Health and Aging Study. J Gerontol B Psychol Sci Soc Sci. 2001;56 doi: 10.1093/geronb/56.1.s10. S10-9. [DOI] [PubMed] [Google Scholar]
- 9.Streiner DL, Norman GR. Reliability. In: Streiner DL, Norman GR, editors. Health Measurement Scales A Practical Guide to Their Development and Use. London: Oxford University Press; 2003. pp. 126–152. [Google Scholar]
- 10.Bland JM, Altman DG. Measurement error proportional to the mean. BMJ. 1996;313:106. doi: 10.1136/bmj.313.7049.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bland JM. [Accessed December 22, 2006];How should I calculate a within-subject coefficient of variation? [Online material] http://www-users.york.ac.uk/~mb55/meas/cv.htm.
- 12.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 13.StataCorp. Intercooled Stata Statistical Software. College Station, TX: 2005. [Google Scholar]
- 14.Bohannon RW. Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Ageing. 1997;26:15–19. doi: 10.1093/ageing/26.1.15. [DOI] [PubMed] [Google Scholar]
- 15.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54:743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 16.Ostir GV, Volpato S, Fried LP, Chaves P, Guralnik JM. Reliability and sensitivity to change assessed for a summary measure of lower body function: results from the Women's Health and Aging Study. J Clin Epidemiol. 2002;55:916–921. doi: 10.1016/s0895-4356(02)00436-5. [DOI] [PubMed] [Google Scholar]
- 17.Wolinsky FD, Miller DK, Andresen EM, Malmstrom TK, Miller JP. Reproducibility of physical performance and physiologic assessments. J Aging Health. 2005;17:111–124. doi: 10.1177/0898264304272784. [DOI] [PubMed] [Google Scholar]
- 18.Hoenig H, Ganesh SP, Taylor DH, Jr, Pieper C, Guralnik J, Fried LP. Lower extremity physical performance and use of compensatory strategies for mobility. J Am Geriatr Soc. 2006;54:262–269. doi: 10.1111/j.1532-5415.2005.00588.x. [DOI] [PubMed] [Google Scholar]