Abstract
Introduction
Little is known about ill-defined pain that persists following endodontic procedures, including an estimate of the problem’s magnitude. We conducted a systematic review of prospective studies that reported the frequency of non-odontogenic pain in patients who had undergone endodontic procedures.
Methods
Non-odontogenic pain was defined as dentoalveolar pain present for 6 months or more after endodontic treatment without evidence of dental pathology. Endodontic procedures reviewed were non-surgical root canal treatment, retreatment, and surgical root canal treatment. Studies were searched in four databases electronically, complemented by hand searching. A summary estimate of non-odontogenic tooth pain frequency was derived using random-effects meta-analysis.
Results
Of 770 articles retrieved and reviewed, 10 met inclusion criteria and 9 had data on both odontogenic and non-odontogenic causes of pain. A total of 3,343 teeth were included; 1,125 had follow-up information regarding pain status. We identified 48 teeth with non-odontogenic pain and estimated a 3.4% (95% CI: 1.4 to 5.5%) frequency of occurrence. In 9 articles containing data regarding both odontogenic and non-odontogenic causes of tooth pain, 56% (44/78) of all cases were thought to have a non-odontogenic cause.
Conclusions
Non-odontogenic pain is not an uncommon outcome following root canal therapy and may represent half of all cases of persistent tooth pain. These findings have implications for diagnosis and treatment of painful teeth that were previously root canal treated since therapy directed at the tooth in question would not be expected to resolve non-odontogenic pain.
Keywords: Tooth, Dentoalveolar, Pain, Root canal therapy, Systematic review
INTRODUCTION
Tooth pain, meaning pain of known pulpal or peri-radicular etiology, is not the only reason for pain perceived in the dentoalveolar regions (1). Non-odontogenic causes comprise varying etiologies, such as referred myofascial pain (2), headache (3), neuropathic disorders (4), and pain stemming from various pathological conditions (5). Quantifying the frequency of non-odontogenic pain following root canal therapy is important for dentists and patients, so patients can make educated decisions by knowing the risks and benefits associated with treatment. Determining the extent of this problem is the first step towards the long-term goal of reducing diagnostic errors that often lead to irreversible dental procedures in an attempt to alleviate the pain, such as root canal retreatments, surgical root canal treatments, and tooth extractions (6).
Several studies have investigated the component diagnoses, listed above, that comprise this group of non-odontogenic pain cases referred to tertiary care centers (5,7,8). Even though such pain is thought to be “rare” (9), the magnitude of this problem is not known to a degree that would allow for development of appropriate public health policy. Important subtypes of this pain are not quantified either, especially those pains thought to be neuropathic in nature. For patients and dentists alike, they represent a considerable challenge because they are known to respond less than favorably to treatment (10). Given the current situation, that is, multiple diagnoses comprising this group of non-odontogenic pain that have widely differing treatment needs, it is important to quantify this problem to inform clinicians so they can use this information in their daily practice. Therefore we sought to estimate the frequency of non-odontogenic dentoalveolar pain present at 6 months or greater following root canal therapy by performing a meta-analysis, which is a robust method of synthesizing published information (11).
MATERIALS & METHODS
Inclusion Criteria
Eligible for inclusion in this review were endodontic procedure articles published in any language before June 5, 2009 that reported on post-operative tooth pain after at least 6 months follow-up. Qualifying endodontic procedures included initial root canal treatment or retreatment, surgical or non-surgical, but not pulpotomy, partial pulpectomy, or pulp capping. The unit of observation considered was a human permanent tooth in vivo; primary teeth were excluded. The study outcome was presence of dentoalveolar pain that explicitly did not have an odontogenic etiology, such as a cracked tooth, missed canal or periapical pathosis. Pain could be spontaneous or provoked by biting, palpation, or percussion.
Another inclusion criterion for studies was that they reported baseline data of the population from which the follow up sample was drawn. This requirement, allowing frequency of occurrence to be calculated, limited study inclusion to case series, cohort and clinical trial studies, and excluded cross-sectional and case-control studies. Articles reporting randomized trials were included as a special type of prospective cohort study; however, the treatment arms were collapsed for our analysis. Unpublished research and studies reported only in abstract form were not considered.
Information Sources and Search Strategy
We conducted an initial search in MEDLINE via the PubMed interface, covering the period from 1949 to June 5, 2009 and using the search terms specified in figure BOX 1. This search was then adapted for use and run in the Cochrane Library, TRIP database, and Google Scholar. We also hand searched the references of prominent articles, literature reviews, and textbook chapters (source list available upon request). Our intent was to be broad in scope to ensure inclusion of as much relevant existing data as reasonably possible. Training and reliability assessment of article selection, data abstraction of study variables, and assessment of reported study quality have been previously reported (12).
BOX . Electronic search strategy.
(pain OR quality of life OR hypersensitivit*) AND (root canal* OR endodont*) AND (cohort stud* OR prognos* OR treatment failure OR morbidity OR survival analysis OR disease susceptibility OR disease progression OR disease free survival OR time factor* OR recurrence OR clinical course OR inception cohort OR predict* OR outcome OR course OR postoperative OR longitudinal stud* OR treatment outcome OR follow-up stud* OR followup stud* OR prospective) NOT Review[Publication Type]
Statistical Methods
We used random-effects meta-analysis (13) to determine a summary estimate of non-odontogenic pain frequency. In a sensitivity analysis, we examined whether deletion of a single study substantially changed the meta-analysis summary estimate. To explore factors influencing the estimate, we performed meta-regression to investigate differences between studies with the following characteristics: 1) surgical versus non-surgical treatment, 2) follow-up rate of recall <50% versus ≥50%, 3) follow-up at 6 to 12 months versus at more than 12 months, 4) initial treatment versus re-treatment, and 5) above-median quality reporting score versus below-median score according to the STROBE criteria (12,14). We also estimated the proportion of non-odontogenic tooth pain amoung the subset of cases that had information on both “all-cause” and non-odontogenic pain.
All analyses were performed using the STATA software package (Stata Statistical Software: Release 10.1. College Station, TX: StataCorp LP) and the user-written metan and metareg commands.
RESULTS
Study Identification and Characteristics
We identified 770 articles (495 by electronic searching of databases and 275 by hand searching), the oldest published in 1921. Twenty-eight were published in a language other than English (7 French; 6 Chinese; 5 Japanese; 2 each in Italian, Russian, and Spanish; 1 each in Croatian, Danish, German, and Greek). Screening of titles and abstracts resulted in 306 articles being excluded. After full text review, another 464 articles were excluded, so 10 articles were included in the meta-analysis (Figure 1). All 10 articles were published in English and 6 of them were identified by hand searching.
Figure 1.
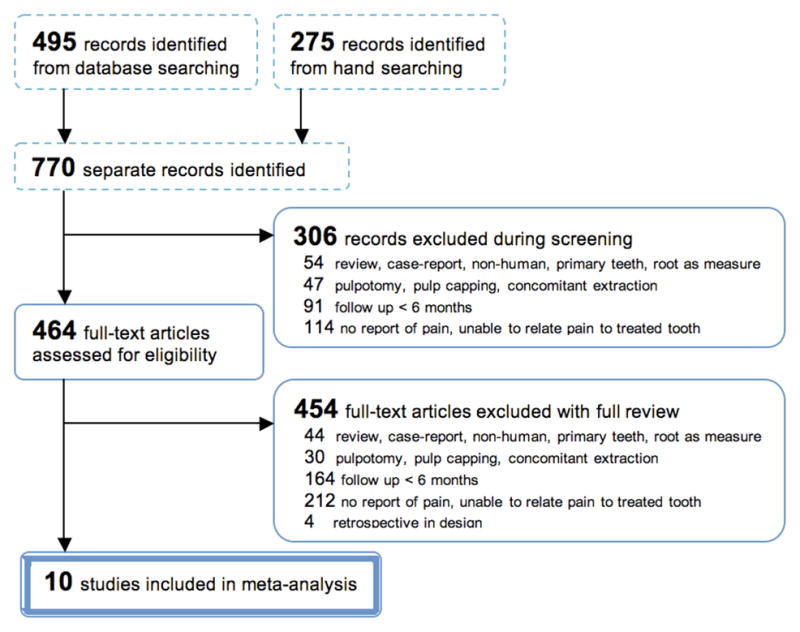
Flowchart of the systematic review process
The 10 included studies varied in the types of endodontic treatments provided, numbers of teeth treated (6 to 276), duration of follow-up (1 to 6 years), and percentage of teeth followed up (20 to 100%) (Table 1). From 3,343 teeth enrolled in the 10 studies, 1,125 teeth were followed up for at least 12 months. Among them, 48 teeth (4.3%) in 7 studies were reported to have pain without an identifiable odontogenic source. In these studies teeth were determined to have tooth-related disease when the tooth was present and “not properly restored”, “fractured”, periapical radiolucency present (15,16), sinus tract present (17), “root fracture associated with severe bone loss” (18), and “failure of coronal restoration” (19) could be identified with the root canal treated teeth. Variation in the quality of reporting (STROBE criteria) was observed (interquartile range = 8.5 to 20.5, range = 5 to 20.5), with median reporting quality score of 19.8 (possible scores ranging from 0 to 22). Furthermore, 9 studies contained details on both “all-cause” pain and non-odontogenic pain, making it possible to calculate the proportion of such pain outcomes.
Table 1.
Characteristics of the 10 studies included in the meta-analysis
| Authors, year | Endodontic procedure | Teeth enrolled | Follow up n (%) | Non-odontogenic tooth pain | Multiple procedures | Follow-up (years) | STROBE rating |
|---|---|---|---|---|---|---|---|
| Liu & Sidhu, 1995 | Initial NSRCT | 6 | 6 (100) | 0 | 0 | 1 – 3.5 | 5 |
| Danin et al, 1999 * | Periapical Surgery | 10 | 10 (100) | 0 | 0 | 1 – 1 | 10.7 |
| von Arx & Kurt, 1999 | Periapical Surgery | 50 | 43 (86) | 1 | 7 | 1 – 1 | 8 |
| Farzaneh et al, 2004a * | Re-Treatment NSRCT | 523 | 103 (20) | 0 | 79 | 4 – 6 | 20.5 |
| Farzaneh et al, 2004b * | Initial NSRCT | 442 | 122 (28) | 3 | 71 | 4 – 6 | 20.5 |
| Polycarpou et al, 2005 | Combined Treatments | 400† | 175 (44) | 21 | 0† | 1 – 1 | 20 |
| Marquis et al, 2006 * | Initial NSRCT | 532 | 131 (25) | 7 | 64 | 4 – 6 | 19.5 |
| de Chevigny et al, 2008a * | Initial NSRCT | 582 | 137 (24) | 6 | 71 | 4 – 6 | 20.5 |
| de Chevigny et al, 2008b * | Re-Treatment NSRCT | 477 | 122 (26) | 6 | 94 | 4 – 6 | 20.5 |
| Saunders et al, 2008 | Periapical Surgery | 321 | 276 (86) | 4 | 0 | 6 – 6 | 8.5 |
| Aggregate values: | 3,343 | 1,125 (37) | 48 | 386 | 1 – 6 | 19.8 | |
NSRCT = non-surgical root canal therapy; # = number
Reference found by hand searching
Assumed that each patient contributed only 1 tooth since not explicitly stated
Summary Estimate of Non-odontogenic Pain Frequency
The meta-analytical summary estimate of non-odontogenic pain frequency was 3.4% (95% CI: 1.4 to 5.5%, Figure 2). “Moderate” heterogeneity (i.e., inconsistency) (20) among study estimates was observed (I2=65%, p=0.002). When each study was eliminated in turn from the analysis and the meta-analysis was run with the nine remaining studies, the summary estimates ranged from 2.1% to 4.2%. Thus individual studies did not unduly influence the summary estimate even though one study identified 21 of the 48 cases (44%) of non-odontogenic pain.
Figure 2.
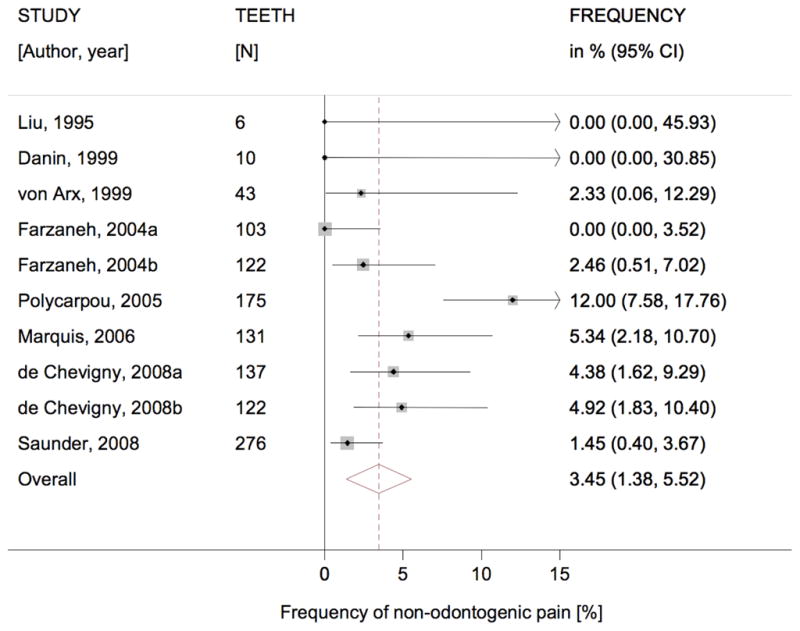
Random effects meta-analysis of the frequency of non-odontogenic tooth pain in 10 studies
Exploration of Study Heterogeneity
In meta-regression analyses (Table 2), follow-up duration was the factor that most differentiated pain frequency the most: the three studies with follow-up of 6–12 months had a frequency of persistent non-odontogenic pain higher by 4.5 percentage points than in the 7 studies with follow-up >12 months. Study reporting quality affected pain frequency the least: the five above-median STROBE criteria studies had a frequency of persistent non-odontogenic pain higher by 1.5 percentage points than in the five below-median studies. However, even when differences were substantial in magnitude, all were statistically non-significant due to small numbers of studies.
Table 2.
Assessment of study heterogeneity by meta-regression
| Comparison of Subgroups | Coefficient (standard error) | p-value |
|---|---|---|
| Surgical treatment vs. nonsurgical treatment | −2.7% (2.7) | 0.36 |
| ≥50% follow-up rate vs. <50% follow-up rate | −2.8% (2.7) | 0.34 |
| >12 months vs. 6–12 months follow-up duration | −4.5% (2.6) | 0.13 |
| Retreatment vs. initial treatment # | −2.3% (2.1) | 0.35 |
| Above-median vs. below-median reported study quality (STROBE criteria) | 1.5% (2.6) | 0.57 |
Four studies with missing data
Negative (−) sign indicates that first subgroup has higher pain frequency
Proportion of “all-cause” Pain that is Non-odontogenic
Nine studies had data for “all-cause” tooth pain, as previously reported (12), as well as for non-odontogenic pain, thus allowing an estimation of the proportion of such pain outcomes in each study population. In these 9 studies, 44 non-odontogenic pain cases (56%) of the 78 “all-cause” pain cases were identified.
DISCUSSION
This systematic review identified 10 prospective studies (3,343 enrolled teeth) and estimated the frequency of non-odontogenic pain at 6 months or more after root canal treatment to be 3.4% (95% CI: 1.4 to 5.5%). At this rate, with more than 16.4 million root canal treatments performed annually in the United States (21), each year over half a million endodontic patients would be at risk for non-odontogenic pain.
Non-odontogenic dentolalveolar pain is often difficult to diagnose (5,8) because it is poorly understood (22). Even defining and categorizing such persistent pain is challenging, but conceptually non-odontogenic pain in the dentoalveolar region can arise from 4 potential processes: 1) referred musculoskeletal pain disorder, 2) neuropathic pain disorder, 3) headache disorders presenting in the dentoalveolar region, and 4) a pathological process outside the immediate dentoalveolar region that refers pain to that area, such as sinus disease, salivary gland disorders, brain tumors, angina, throat cancer, and craniofacial vascular disorders (1).
In theory, our non-odontogenic pain frequency estimate is an estimate of the incidence of this condition. In practice, because the condition is challenging to diagnose, misclassification at baseline by failing to identify a non-odontogenic reason for pain results in the inclusion of such cases in the reported studies. Misclassified neuropathic pain cases at baseline would be expected to continue to be painful following endodontic treatment (9), or become more recalcitrant (23), while non-odontogenic cases of referred pain from distant tissues, such as musculoskeletal, pathological and headache disorders, would likely not be adequately addressed with endodontic treatment. The amount of misclassification is not known, since to our knowledge such research results have not been reported. Furthermore, since patients undergoing endodontic treatment commonly exhibit pre-existing dentoalveolar pain of inflammatory origin (24), this study cannot differentiate between patients whose non-odontogenic pain arose from pre-existing pathosis and patients whose pain arose from the procedure. Therefore, our estimate represents a mixture of truly incident and remissive cases, as well as maintenance of the condition in patients misclassified at baseline. For this reason we call this estimate a frequency of occurrence, which quantifies the burden of non-odontogenic pain – a condition with many clinical challenges.
The meta-analytical approach allows aggregation of data to produce a robust estimate (11), but has known limitations based on the quality of the studies included (25,26). Therefore, we restricted our meta-analysis to prospective studies, which are thought to produce more accurate results in general (27) and to endodontic outcome studies in particular (12). Seven out of the 10 studies identified were published in the last decade, suggesting an increased interest in reporting patient-oriented outcomes and more design rigor in recent endodontic studies. Only one study assessed non-odontogenic pain as its primary outcome. This study found an incidence of 12% (21/175) (15), a number substantially higher than our meta-analysis summary, which may therefore suggest that our meta-analytic summary estimate is low.
In exploratory analyses, studies with shorter follow-up (6–12 months) had greater frequency of persistent non-odontogenic pain than those with longer follow up, which is an important finding (28) and may suggest that such persistent pain improves with time. Reduced frequency of persistent post-procedural pain over time has been observed by other studies investigating non-dental surgical models of human pain, such as Caesarean sections (29) and has been suggested to occur with orofacial pains (23), but has not been explored in relation to endodontic procedures.
A methodological problem of our review was that the reporting unit was the tooth, whereas the outcome of persistent dentoalveolar pain is a patient-based measure. Teeth within the same individual do not represent statistically independent observations, because they share the same environment, so confidence intervals for our point estimates should be larger than presented. However, we believe that this is not likely a major problem because even though 6 studies reported multiple observations per patient, the difference between the number of patients and the total number of teeth was low (12%; 386/3,343). Another important issue in this review was the large proportion of patients that were not followed (67%; 2,218/3,343), which allows ample opportunity for missing cases of non-odontogenic pain. This is potentially troubling because endodontic patients have been found not to inform their endodontist when persistent pain is present (30). This is not supported by our meta-regression, which found that studies with <50% follow-up rates had higher pain frequencies than those with ≥50% follow-up rates. This finding, though not statistically significant, is contrary to the common view. Caution needs to be used when interpreting such results since these assessments are exploratory and do not take into account that of the 6 studies having >50% follow-up rate, 4 had the lowest STROBE scores and the above-median STROBE criteria studies had higher frequencies compared to the below-median half.
Our meta-analysis provides some insight about the proportion of persistent pain after endodontic procedures that is non-odontogenic in nature. Combining the present study’s finding with our previous study that estimated the frequency of “all-cause” tooth pain to be 5.3% (12), non-odontogenic cases may account for 64% (3.4/5.3) of these teeth with pain. When comparing the proportion of patients exhibiting non-odontogenic pain among those determined to have all-cause pain in the 9 studies with available data, the proportion was 56% (44/78). When we use the best single study to assess this proportion, i.e., the study that used non-odontogenic pain as its primary outcome (15), this fraction was 57% (21/37). This suggests that at least half of all persistent tooth pain is of non-odontogenic nature, so these cases would best be managed without further endodontic therapy. This is contrary to current opinion (31–34) and practice (9) in dentistry, which advocates retreatment. Regardless of the recommended approach to pain after endodontic treatment, the large proportion of non-odontogenic pain has substantial implications for diagnoses and further treatment of these pain conditions.
In conclusion, 3.4% of patients experienced persistent pain of non-odontogenic origin following root canal therapy – a number that likely represents about half of all persistent “tooth” pains. Therefore, the outcome of non-odontogenic tooth pain is not as rare as commonly assumed. Given that non-odontogenic pain has diverse etiologies and successful treatment is often difficult, further research is needed to diagnose non-odontogenic pain subtypes, quantify the burden on the individual experiencing it, provide adequate treatment, and assess long-term outcomes. Also needed is research that differentiates cases of non-odontogenic pain from those of a local etiology, since tooth-based pathology is amenable to endodontic retreatment and non-odontogenic pain would be best treated if recognized.
Acknowledgments
Thanks to those who translated articles: Estelle Arnaud-Battandier, David Bereiter, Dino Bilankov, Zheng Chang, Wenjung Kang, Sergey Khasabov, Thomas List, Keiichiro Okamoto, Akimasa Tashiro, and Ana Velly.
Supported by National Institutes of Health grants: K12-RR023247, U01-DE016746 and U01-DE016747 (DR Nixdorf).
Footnotes
The authors deny any conflicts of interest related to this study
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mattscheck D, Law AS, Nixdorf DR. Diagnosis of non-odonogentic toothache. In: Hargreaves KM, Cohen S, editors. Cohen’s pathways of the pulp. 10. St. Louis, MO: Mosby Inc; 2011. pp. 49–70. [Google Scholar]
- 2.Wright EF. Referred craniofacial pain patterns in patients with temporomandibular disorder. J Am Dent Assoc. 2000;131:1307–15. doi: 10.14219/jada.archive.2000.0384. [DOI] [PubMed] [Google Scholar]
- 3.Alonso AA, Nixdorf DR. Case series of four different headache types presenting as tooth pain. J Endod. 2006;32:1110–3. doi: 10.1016/j.joen.2006.02.033. [DOI] [PubMed] [Google Scholar]
- 4.Baad-Hansen L. Atypical odontalgia - pathophysiology and clinical management. J Oral Rehabil. 2008;35:1–11. doi: 10.1111/j.1365-2842.2007.01813.x. [DOI] [PubMed] [Google Scholar]
- 5.Israel HA, Ward JD, Horrell B, Scrivani SJ. Oral and maxillofacial surgery in patients with chronic orofacial pain. J Oral Maxillofac Surg. 2003;61:662–7. doi: 10.1053/joms.2003.50133. [DOI] [PubMed] [Google Scholar]
- 6.Linn J, Trantor I, Teo N, Thanigaivel R, Goss AN. The differential diagnosis of toothache from other orofacial pains in clinical practice. Aust Dent J. 2007;52:S100–4. doi: 10.1111/j.1834-7819.2007.tb00518.x. [DOI] [PubMed] [Google Scholar]
- 7.Fricton JR. Critical commentary 1 - A unified concept of idiopathic pain: Clinical features. J Orofac Pain. 1999;13:185–9. [PubMed] [Google Scholar]
- 8.de Siqueira SRDT, Nobrega JCM, Valle LBS, Teixeira MJ, de Siqueira JTT. Idiopathic trigeminal neuralgia: Clinical aspects and dental procedures. Oral Surg Oral Med Oral Path Oral Rad Endod. 2004;98:311–5. doi: 10.1016/S1079210404003191. [DOI] [PubMed] [Google Scholar]
- 9.Oshima K, Ishii T, Ogura Y, Aoyama Y, Katsuumi I. Clinical investigation of patients who develop neuropathic tooth pain after endodontic procedures. J Endod. 2009;35:958–61. doi: 10.1016/j.joen.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 10.Lewis MAO, Sankar V, De Laat A, Benoliel R. Management of neuropathic orofacial pain. Oral Surg Oral Med Oral Path Oral Rad and Endod. 2007;103(suppl 1):S32.e1, S32.e24. doi: 10.1016/j.tripleo.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 11.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Padstow, UK: John Wiley & Sons, Ltd; 2009. [Google Scholar]
- 12.Nixdorf DR, Moana-Filho EJ, Law AS, McGuire LA, Hodges JS, John MT. Frequency of persistent tooth pain after root canal therapy: A systematic review and meta-analysis. J Endod. 2010;36:224–30. doi: 10.1016/j.joen.2009.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 14.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. Ann Intern Med. 2007;147:W163–94. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. [DOI] [PubMed] [Google Scholar]
- 15.Polycarpou N, Ng YL, Canavan D, Moles DR, Gulabivala K. Prevalence of persistent pain after endodontic treatment and factors affecting its occurrence in cases with complete radiographic healing. Int Endod J. 2005;38:169–78. doi: 10.1111/j.1365-2591.2004.00923.x. [DOI] [PubMed] [Google Scholar]
- 16.de Chevigny C, Dao TT, Basrani BR, et al. Treatment outcomes in endodontics: The Toronto study--phases 3 and 4: Orthograde retreatment. J Endod. 2008;34:131–7. doi: 10.1016/j.joen.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 17.Farzaneh M, Abitbol S, Lawrence HP, Friedman S Toronto Study. Treatment outcome in endodontics-the Toronto study. Phase II: Initial treatment. J Endod. 2004;30:302–9. doi: 10.1097/00004770-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Marquis VL, Dao T, Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: The Toronto study. Phase III: Initial treatment. J Endod. 2006;32:299–306. doi: 10.1016/j.joen.2005.10.050. [DOI] [PubMed] [Google Scholar]
- 19.Sanders A, Slade GD, Lim S, Reisine ST. Impact of oral disease on quality of life in the US and Australian populations. Community Dent Oral Epidemiol. 2009;37:171–81. doi: 10.1111/j.1600-0528.2008.00457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Dental Association. Survey of dental services rendered and distribution of dentists in the United States by region and state, 1999. 2002 [Google Scholar]
- 22.Quail G. Atypical facial pain--a diagnostic challenge. Aust Fam Physician. 2005;34:641–5. [PubMed] [Google Scholar]
- 23.Allerbring M, Haegerstam G. Chronic idiopathic orofacial pain. A long-term follow-up study. Acta Odontol Scand. 2004;62:66–9. doi: 10.1080/00016350310008517. [DOI] [PubMed] [Google Scholar]
- 24.Fouad A, Levin L. Pupal reactions to caries and dental procedures. In: Hargreaves KM, Cohen S, editors. Cohen’s pathways of the pulp. 10. St. Louis, MO: Mosby, Inc; 2011. pp. 504–28. [Google Scholar]
- 25.Moles DR, Needleman IG, Niederman R, Lau J. Introduction to cumulative meta-analysis in dentistry: Lessons learned from undertaking a cumulative meta-analysis in periodontology. J Dent Res. 2005;84:345–9. doi: 10.1177/154405910508400410. [DOI] [PubMed] [Google Scholar]
- 26.Spangberg LSW. Systematic reviews in endodontics - examples of GIGO? Oral Surg Oral Med Oral Path Oral Rad Endod. 2007;103:723–4. doi: 10.1016/j.tripleo.2007.03.032. [DOI] [PubMed] [Google Scholar]
- 27.Cummings SR, Newman TB, Hulley SB. Designing a cohort study. In: Cummings SR, Newman TB, Hulley SB, editors. Designing Clinical Research. 3. Philadelphia, PA: Lippincott, Williams & Wilkins; 2007. pp. 97–107. [Google Scholar]
- 28.Savitz DA. Interpreting epidemiological evidence: strategies for study design and analysis. New York, NY: Oxford University Press; 2003. Integration of evidence across studies; pp. 261–83. [Google Scholar]
- 29.Nikolajsen L, Sorensen HC, Jensen TS, Kehlet H. Chronic pain following Caesarean section. Acta Anaesthesiol Scand. 2004;48:111–6. doi: 10.1111/j.1399-6576.2004.00271.x. [DOI] [PubMed] [Google Scholar]
- 30.Lobb WK, Zakariasen KL, McGrath PJ. Endodontic treatment outcomes: Do patients perceive problems? J Am Dent Assoc. 1996;127:597–600. doi: 10.14219/jada.archive.1996.0271. [DOI] [PubMed] [Google Scholar]
- 31.Abbott PV. Factors associated with continuing pain in endodontics. Aust Dent J. 1994;39:157–61. doi: 10.1111/j.1834-7819.1994.tb03084.x. [DOI] [PubMed] [Google Scholar]
- 32.Cohn SA. Clinical update--the teeth and the maxillary sinus: The mutual impact of clinical procedures, disease conditions and their treatment implications. Part 1. The differential diagnosis of tooth sinus pain--the dentist’s view. Aust Endod J. 1999;25:29–31. doi: 10.1111/j.1747-4477.1999.tb00067.x. [DOI] [PubMed] [Google Scholar]
- 33.Boucher Y, Sobel M, Sauveur G. Persistent pain related to root canal filling and apical fenestration: A case report. J Endod. 2000;26:242–4. doi: 10.1097/00004770-200004000-00013. [DOI] [PubMed] [Google Scholar]
- 34.Kim S, Kratchman S. Modern endodontic surgery concepts and practice: A review. J Endod. 2006;32:601–23. doi: 10.1016/j.joen.2005.12.010. [DOI] [PubMed] [Google Scholar]


