Abstract
FSH is produced by the pituitary gonadotrope to regulate gametogenesis. Steroid hormones, including androgens, progestins, and glucocorticoids, have all been shown to stimulate expression of the FSHβ subunit in primary pituitary cells and rodent models. Understanding the molecular mechanisms of steroid induction of FSHβ has been difficult due to the heterogeneity of the anterior pituitary. Immortalized LβT2 cells are a model of a mature gonadotrope cell and express the endogenous steroid receptor for each of the three hormones. Transient transfection of each receptor, along with ligand treatment, stimulates the mouse FSHβ promoter, but induction is severely diminished using receptors that lack the ability to bind DNA, indicating that induction is likely through direct DNA binding. All three steroid hormones act within the first 500 bp of the FSHβ promoter where six putative hormone response elements exist. The −381 site is critical for FSHβ induction by all three steroid hormones, whereas the −197 and −139 sites contribute to maximal induction. Interestingly, the −273 and −230 sites are also necessary for androgen and progestin induction of FSHβ, but not for glucocorticoid induction. Additionally, we find that all three receptors bind the endogenous FSHβ promoter, in vivo, and specifically bind the −381 site in vitro, suggesting that the binding of the receptors to this element is critical for the induction of FSHβ by these 3-keto steroid hormones. Our data indicate that androgens, glucocorticoids, and progestins act via their receptors to directly activate FSHβ gene expression in the pituitary gonadotrope.
FSH and LH are produced in the gonadotrope cells of the anterior pituitary. These hormones act on the gonads to regulate critical aspects of reproduction, including steroidogenesis, gametogenesis, and ovulation (1–3). FSH and LH are heterodimeric glycoproteins composed of a shared α-subunit and a unique β-subunit (4). The β-subunit confers the biological specificity of FSH and LH, and synthesis of this subunit appears to be the rate-limiting step for production of FSH and LH (5, 6). Both peptide and steroid hormones regulate FSH and LH synthesis to produce the hormonal pattern necessary for the estrous cycle and normal reproductive function. The hypothalamic neuropeptide, GnRH, mediates the synthesis and secretion of both FSH and LH (7). In addition, the modulation of FSHβ gene expression by the activin/inhibin/follistatin system has been well characterized (8, 9). Recent data show that activin can also regulate LHβ gene expression (10–14).
A fundamental concept in the study of reproduction is the regulation of the hypothalamic-pituitary-gonadal axis by steroid hormone feedback. In addition to exerting effects at the level of the hypothalamus, steroids control the transcription of FSHβ and LHβ subunit genes at the level of the pituitary, although their mechanisms of action have not been as well characterized as GnRH and activin. More specifically, androgens, progestins, and glucocorticoids have all been shown to induce FSHβ gene expression in the anterior pituitary [recently reviewed by Burger et al. (15)]. Although androgens and progestins are produced by the gonads, and glucocorticoids are produced by the adrenal glands, all of these 3-keto steroids possess a similar chemical structure and mechanism of action. Moreover, all three of their respective receptors, the androgen receptor (AR), progesterone receptor (PR), and glucocorticoid receptor (GR), are related members of the class I steroid receptor family (16, 17) and bind DNA directly at response elements containing the half-site TGTTCT organized as 15-bp inverted repeats with 3-bp spacers (18, 19). In the classical mechanism of action, the receptors homodimerize upon ligand binding and bind their response elements causing trans-activation of specific genes (20). More recently, it has been recognized that the steroid receptors can also function in a nonclassical manner to modulate transcription through indirect DNA binding via interactions with other transcription factors such as activation protein 1 (21–23).
Several lines of evidence indicate that androgens regulate the levels of FSHβ and LHβ mRNAs in the anterior pituitary. Studies in castrated, GnRH antagonist-treated rats have shown a selective increase in FSHβ mRNA upon treatment with testosterone (24– 27). Subsequent studies in primary rat pituitary cells confirmed that the activation of FSHβ expression by testosterone occurs at the level of the pituitary (28–30). In contrast to FSHβ, androgens repressed LHβ-subunit gene expression in both castrated, GnRH antagonist-treated rats (26, 27) and primary pituitary cell culture (29). Additionally, the effects of androgens on transcription of the LHβ subunit have been studied in gonadotrope-derived immortalized cell lines. Jorgensen and Nilson (31) found that androgens suppress bovine LHβ subunit gene expression through protein-protein interaction between ligand-bound AR and steroidogenic factor 1. Using a −617/+44 rat LHβ promoter, Curtin et al. (32) determined that androgen treatment suppressed GnRH-induced LHβ subunit gene transcription as well. However, they found that the suppression occurred primarily as a consequence of direct protein-protein interaction between AR and Sp1.
Progesterone also appears to mediate FSHβ gene expression at the level of the pituitary. FSHβ mRNA levels were increased in rats treated with estrogen and progesterone (33). The presence of estrogen and progesterone also further augmented the increase in FSHβ mRNA expression in response to GnRH stimulation (34). Furthermore, antiprogestins blocked FSH secretion and mRNA expression during the preovulatory FSH surge (35) as well as blocking the secondary FSH surge (36, 37). Both the rat and ovine FSHβ promoters have been examined for progesterone responsiveness. Reporter genes containing either the proximal rat or ovine FSHβ promoter responded to progestin treatment in primary rat or ovine pituitary cultures, respectively (38, 39). Within the ovine FSHβ promoter, six progesterone response elements (PREs) were shown to bind PR (38), whereas three PREs bound PR in the rat promoter (39), although the functional role of the individual elements was not determined. Less is known about the effects of progestins on LHβ mRNA expression, although no effect was reported on LHβ mRNA levels in ovariectomized rats treated with estrogen and progestin (34) or on LHβ mRNA levels in rat primary pituitary cells treated with both estrogen and progestin (40).
Similar to androgens and progestins, glucocorticoids affect FSHβ expression at the level of the pituitary. Several studies have demonstrated a selective increase in FSHβ gene expression in response to glucocorticoids in both intact animals (41, 42) as well as in primary pituitary cells (30, 43, 44). The effect of the glucocorticoids on FSHβ appears to be at the level of transcription as no effect on FSHβ mRNA half-life was detected (43). Unlike FSHβ, a direct effect of glucocorticoids on LHβ expression has not been observed (41–43), although Rosen et al. (45) did demonstrate that LHβ induction by GnRH was inhibited by glucocorticoids.
Given the importance of androgens, progestins, and glucocorticoids in the regulation of FSHβ gene expression, the purpose of this study was to investigate the molecular mechanisms of this regulation at the level of the gonadotrope. The identification of PREs in the proximal rat and ovine FSHβ promoters almost a decade ago by O’Conner et al. (39) and Webster et al. (38) suggested that there could be a direct mechanism of action. Additionally, because PR contains a DNA-binding domain (DBD) that is highly conserved with other members of the steroid receptor superfamily, including AR and GR, these researchers hypothesized that all of these receptors could bind to the FSHβ promoter and mediate its transcription. However, due to the fact that gonadotropes constitute only about 10% of the total secretory cells in the anterior pituitary (46) and that a majority of these cells express steroid receptors (47–50), the mechanism of action awaited the availability of an appropriate gonadotrope cell model system.
The development of the LβT2 gonadotrope-derived immortalized cell line provided a model system in which to study gonadotropin gene expression in a pure population of gonadotrope cells. The LβT2 cell line endogenously expresses many markers of a mature gonadotrope including FSHβ, LHβ, GnRH receptor (GnRH-R), activin, activin receptor, follistatin, and inhibin (13, 51, 52). It has also been shown to endogenously express the estrogen receptor (ER) (53) and AR (54). These properties make the LβT2 cell line an excellent model system for directly studying the regulation of gonadotropin gene expression by steroids.
Previously, LβT2 cells have been used to study how androgens repress the induction of LHβ gene transcription by GnRH (31, 32). More recently, Spady et al. (55) found that an ovine FSHβ reporter gene was activated in response to testosterone in the LβT2 cell line. In the current study, we used the LβT2 cell line to determine whether steroid hormones directly regulate the expression of the murine FSHβ gene at the level of the gonadotrope and whether this regulation occurs through binding of the steroid receptor to the FSHβ promoter. In particular, we used transient transfections with a FSHβ-luciferase reporter gene to examine the responsiveness of the proximal murine promoter to steroid regulation and to analyze the role of putative hormone response elements (HREs). We also used chromatin immunoprecipitation (ChIP) and gel-shift analysis to determine whether the steroid hormone receptors can bind to the proximal mouse FSHβ promoter in vivo and in vitro. Overall, we show that steroid hormone regulation of the FSHβ promoter can occur at the level of the gonadotrope through direct DNA binding of these steroid receptors to specific HREs.
RESULTS
Androgens, Progestins, and Glucocorticoids Mediate Transcription of the Murine FSHβ Gene
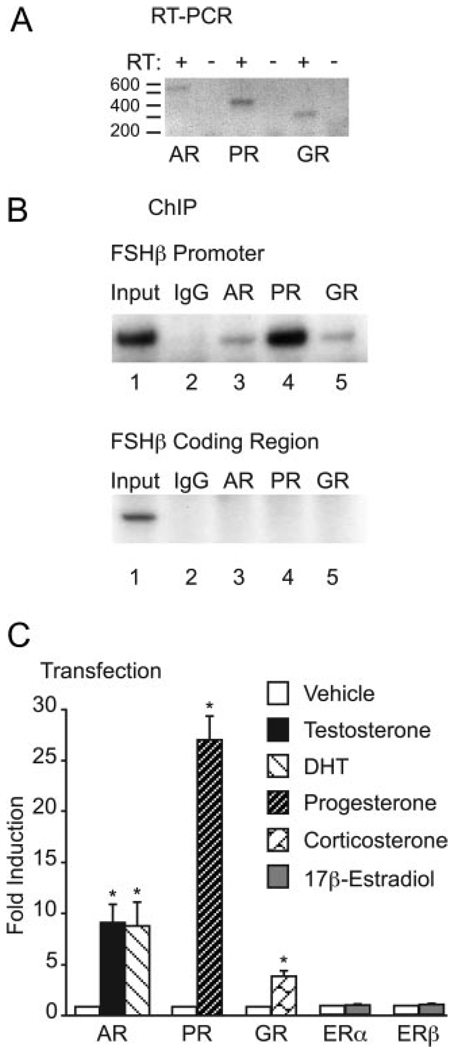
Gonadotrope cells in the anterior pituitary of rodents have been shown to express the receptors for androgens, progestins, and glucocorticoids (56–59), and the LβT2 cell line has been shown previously to express AR (54). We tested whether the LβT2 cells also express PR and GR to determine whether these cells constitute a relevant model system for studying the mechanisms of steroid responsiveness. Oligonucleotide primers encompassing 550 bp of AR, 406 bp of PR, and 298 bp of GR were used to amplify the respective receptors from cDNA generated by reverse transcription of mRNA from the LβT2 cell line. All three receptors were amplified by PCR at the expected sizes, and no bands were seen in the control lanes that lacked reverse transcriptase (Fig. 1A). Next, ChIP with antibodies specific to AR, PR, and GR was used to determine whether the endogenous steroid receptors could bind the mouse FSHβ promoter in vivo in LβT2 cells. The results shown in the upper panel of Fig. 1B demonstrate that all three ligand-bound receptors bind to the endogenous FSHβ promoter (Fig. 1B, upper panel; lanes 3–5). The strong signal for PR in the ChIP assay does not necessarily indicate that PR is more abundant than AR or GR in the LβT2 cells because quantitative PCR was not performed. Instead, it may reflect the affinity of the PR antibody for the receptor. In contrast, there was no precipitation of FSHβ promoter DNA with a nonspecific mouse IgG control (lane 2). The FSHβ promoter was also amplified from the input chromatin (lane 1) as a positive control for genomic DNA preparation and PCR conditions. As a control for specificity, primers encompassing part of the downstream coding region of the FSHβ gene were also used in PCR (Fig. 1B, lower panel). Although these primers amplified FSHβ from the input chromatin as expected (lane 1), no bands were amplified from the precipitated DNA (lanes 2–5).
Fig. 1. Androgens, Progestins, and Glucocorticoids Induce FSHβ Gene Expression in Immortalized Gonadotropes.
A, RT-PCR was used to detect expression of the steroid receptors in LβT2 cells. Amplified AR is visible at 550 bp, PR at 406 bp, and GR at 298 bp. In reverse transcription of total RNA isolated from LβT2 cells, + indicates the presence of reverse transcriptase, and − indicates no reverse transcriptase. B, ChIP was performed using cross-linked protein/chromatin from LβT2 cells and antibodies directed against AR, PR, and GR or, as a negative control, against nonspecific IgG. Upper panel, PCR primers encompassing the proximal promoter of FSHβ were used to detect precipitation of genomic DNA. Lower panel, PCR primers encompassing the downstream FSHβ coding region were used as a control for specificity. PCR amplification was performed on 0.2% chromatin input (lane 1), and chromatin was precipitated with either mouse IgG (lane 2), AR (lane 3), PR (lane 4), or GR (lane 5) antibodies. C, The −1000FSHβluc reporter gene was transiently transfected into LβT2 cells along with 200 ng of the respective steroid receptor expression vectors. After overnight starvation in serum-free media, the cells were treated with 100 nm testosterone, DHT, progesterone, corticosterone, or 17β-estradiol for 24 h. Luciferase activity was normalized to β-galactosidase activity and set relative to the empty reporter vector. The results represent the mean ± sem of at least three experiments performed in triplicate and are presented as fold induction of hormone treatment relative to the vehicle control (ethanol). For cells transfected with AR, and treated with testosterone or DHT, * indicates significantly different from the vehicle-treated control, using one-way ANOVA followed by Tukey’s post hoc test. For LβT2 cells transiently transfected with PR, GR, ERα, or ERβ and treated for 24 h with progesterone, corticosterone, or 17β-estradiol, respectively, * indicates significantly different from the respective vehicle-treated control using Student’s t test. RT, Reverse transcriptase.
To monitor changes in promoter activity upon steroid treatment, LβT2 cells were transiently transfected with the proximal 1000 bp of the mouse FSHβ 5′-regulatory region linked to a luciferase reporter gene (−1000FSHβluc). Because the LβT2 cells are murine in origin, we investigated whether androgen regulation occurs in a similar manner on the murine promoter as it does on the ovine promoter (55). In previous studies, androgen induction of the ovine FSHβ promoter in the presence of endogenous AR resulted in a modest stimulation of transcription (1.5- to 1.9-fold) (55). Given this relatively weak induction, we amplified the steroid hormone response on the FSHβ promoter by transfecting the cells with 200 ng of rat AR.
Treatment of the cells with 100 nm testosterone for 24 h resulted in a 9-fold induction of the mouse FSHβ promoter (Fig. 1C). Dihydrotestosterone (DHT) was also tested to determine whether it could induce FSHβ because DHT cannot be aromatized to estrogen. Treatment with 100 nm DHT activated FSHβ to a similar extent as testosterone, implying that estrogenic activity does not play a role (Fig. 1C). To determine whether other 3-keto steroid hormones such as progestins or glucocorticoids could also regulate murine FSHβ gene expression, the cells were transfected with 200 ng of rat PRB or GR. Interestingly, progesterone and corticosterone also activated FSHβ transcription. Treatment of 100 nm progesterone resulted in a 27-fold induction, whereas 100 nm corticosterone activated FSHβ 4-fold (Fig. 1C).
To further ascertain whether estrogen can modulate transcription of FSHβ-subunit gene expression, the LβT2 cells were transfected with ERα or ERβ and treated with 100 nm 17β-estradiol for 24 h. Estrogen did not stimulate transcription of the −1000FSHβluc reporter gene compared with the vehicle control in the presence of either ERα or ERβ under these conditions (Fig. 1C). Moreover, estrogen did not positively regulate FSHβ gene expression in the presence of both ERs (data not shown). As a control, a luciferase reporter gene driven by a consensus estrogen response element inserted upstream of a minimal Herpes virus thymidine kinase promoter was induced under these conditions (data not shown). Our results agree with previous experiments in rats in which estrogen did not alter the expression of FSHβ mRNA in ovariectomized rats treated with a GnRH antagonist (60) or in female rat pituitary fragments (61).
Androgens, Progestins, and Glucocorticoids Stimulate FSHβ Gene Expression in a Receptor-and Dose-Dependent Manner
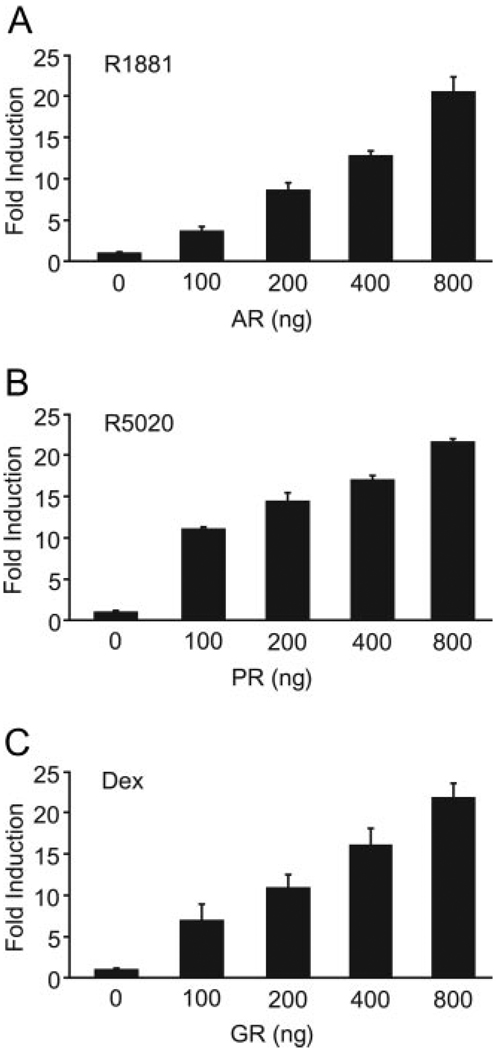
In addition to investigating hormone responsiveness, we examined whether the induction of FSHβ by androgens, progestins, and glucocorticoids was dependent upon receptor concentration. LβT2 cells were transfected with increasing concentrations of the receptor and then treated for 24 h with 100 nm of a synthetic analog of the relevant steroid hormones. There was a trend toward a positive induction with the endogenous receptors, and the addition of even 100 ng exogenous AR, PR, or GR all significantly induced FSHβ gene expression (Fig. 2). The small induction with the endogenous receptors likely reflects titration of the receptors by the transfected reporter genes. For each receptor, the level of FSHβ induction correlated with the amount of exogenous receptor, and the induction did not reach saturation even with the addition of 800 ng of receptor. These results indicate that the steroid receptors are necessary for transcriptional activation of FSHβ by androgens, progestins, and glucocorticoids and that the LβT2 cells are highly responsive to the presence of additional receptor. Furthermore, these data suggest that the steroid responsiveness is not likely due to an artificially high level of steroid receptors because the receptor is limiting in the cells.
Fig. 2. Androgens, Progestins, and Glucocorticoids Induce Transcription of FSHβ in a Receptor-Dependent Manner.
The −1000FSHβluc reporter gene was transiently transfected into LβT2 cells along with increasing receptor concentrations ranging from 0–800 ng/well, as indicated. After overnight starvation in serum-free media, the cells were treated for 24 h with the indicated hormone. The results represent the mean ± sem of at least three experiments performed in triplicate and are presented as fold induction relative to the vehicle control. A, LβT2 cells were transiently transfected with increasing amounts of AR and then treated with 100 nm R1881. B, LβT2 cells were transiently transfected with increasing amounts of PR and then treated with 100 nm R5020. C, LβT2 cells were transiently transfected with increasing amounts of GR and then treated with 100 nm dexamethasone (Dex).
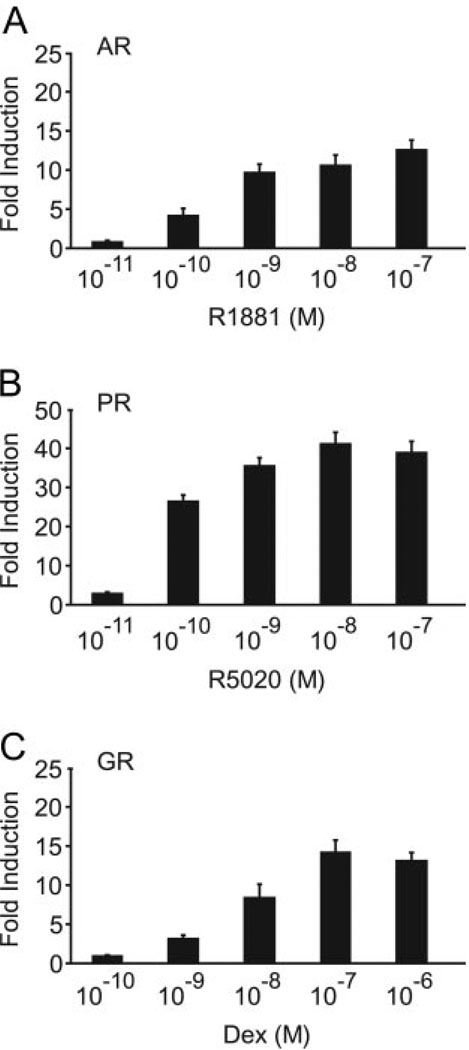
To test whether the induction of FSHβ occurs via a hormone-dependent mechanism, the LβT2 cells were transfected with AR, PR, or GR and then treated with increasing concentrations of the respective hormone. For each of the three hormones, treatment of the cells with a synthetic steroid analog stimulated FSHβ promoter activity in a dose-dependent manner (Fig. 3). Treatment with 100 pm of R1881, a synthetic androgen, activated FSHβ 4-fold, with a maximal induction of 12-fold at the 100 nm dose (Fig. 3A). Treatment with the synthetic progestin, R5020, resulted in activation of the FSHβ promoter at 100 pm with a maximal induction of 40-fold at 10 nm (Fig. 3B). Similarly, treatment with dexamethasone, a synthetic glucocorticoid, activated FSHβ with a concentration of 1 nm (3-fold) with saturation occurring at 100 nm (14-fold) (Fig. 3C), demonstrating that the steroid hormone regulation of FSHβ occurs in a saturable, dose-dependent manner and that physiological concentrations of hormone can activate the FSHβ gene promoter.
Fig. 3. Steroid Hormones Mediate Transcription of FSHβ in a Dose-Dependent Manner.
The −1000FSHβluc reporter gene was transiently transfected into LβT2 cells along with the respective receptor expression vector indicated on the graph. After overnight starvation in serum-free media, the cells were treated for 24 h with the indicated hormone concentrations. The results represent the mean ± sem of at least three experiments performed in triplicate and are presented as fold induction relative to the vehicle control. A, LβT2 cells were transiently transfected with the AR expression vector and then treated with R1881 concentrations ranging from 10 pm to 100 nm. B, LβT2 cells were transiently transfected with the PR expression vector and then treated for 24 h with 10 pm to 100 nm R5020. C, LβT2 cells were transiently transfected with the GR expression vector and then treated with 100 pm to 1 µm dexamethasone (Dex).
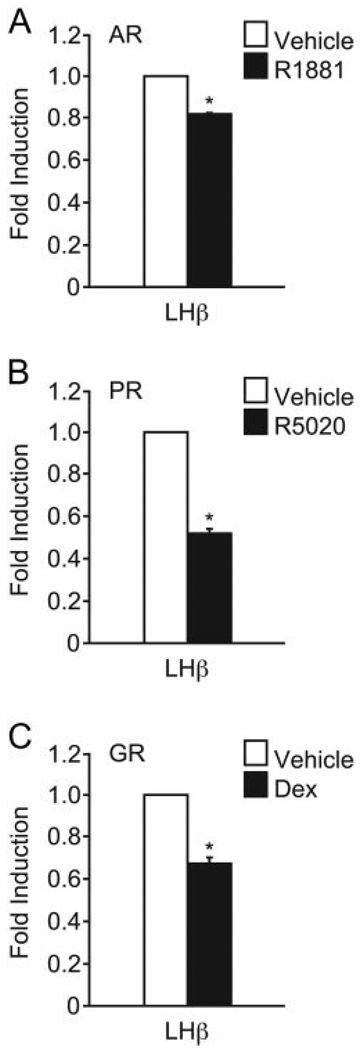
Induction by Steroid Hormone Receptors Is Gene Specific
To determine whether the transcriptional activation by the steroid hormone receptors is specific to the FSHβ gene, the effects of androgens, progestins, or glucocorticoids on the regulation of the LHβ-subunit gene were examined. In this set of experiments, the proximal 1.8 kb of the rat LHβ 5′-regulatory region linked to a luciferase reporter gene (1.8LHβluc) was transiently transfected into LβT2 cells. The cells were also transfected with 200 ng of AR, PR, or GR. Treatment of the cells with 100 nm R1881 repressed the LHβ promoter by 17% (Fig. 4A) whereas treatment with the progestin, R5020, caused a 48% decrease in LHβ gene expression (Fig. 4B). Treatment with dexamethasone also repressed LHβ by 32% (Fig. 4C). Thus, our results demonstrate that ligand-bound AR, PR, or GR can suppress LHβ gene transcription, whereas they induce FSHβ mRNA levels. This suggests that androgens, progestins, and glucocorticoids differentially regulate LHβ and FSHβ subunit gene expression at the level of the gonadotrope.
Fig. 4. Androgens, Progestins, and Glucocorticoids Down-Regulate LHβ Gene Expression.
The 1.8LHβluc reporter gene was transiently transfected into LβT2 cells along with the indicated receptor expression vector. After overnight starvation in serum-free media, the cells were treated for 24 h with hormone. The results represent the mean ± sem of at least three experiments performed in triplicate and are presented as fold induction relative to the vehicle control. *, Indicates that the hormone treatment was significantly different from the vehicle-treated control using Student’s t test. A, LβT2 cells were transiently transfected with the AR expression vector and then treated with 100 nm R1881. B, Cells were transiently transfected with the PR expression vector and then treated with 100 nm R5020. C, Cells were transiently transfected with the GR expression vector and then treated with 100 nm dexamethasone (Dex).
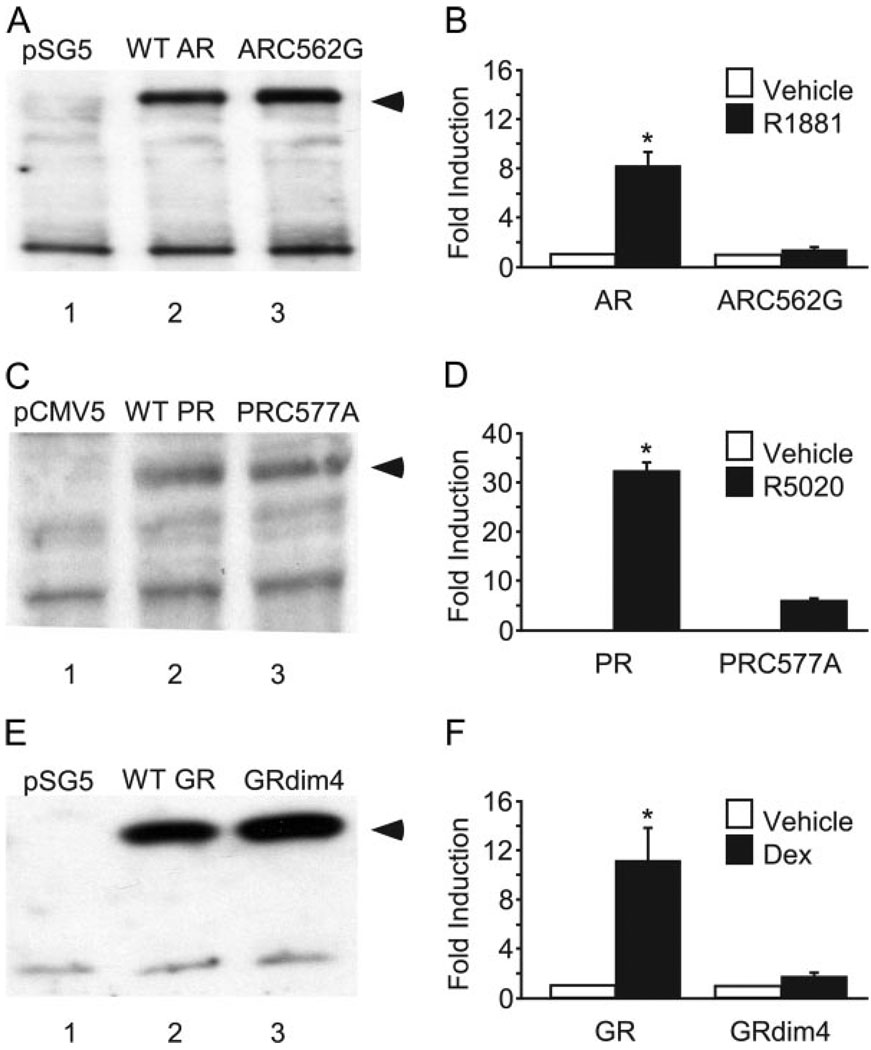
DNA Binding by Steroid Hormone Receptors Is Necessary for Transcriptional Activation of the FSHβ Gene Promoter
To determine whether direct DNA binding by AR, PR, or GR plays a critical role in the transactivation of FSHβ by steroid hormones, we transfected LβT2 cells with steroid receptor mutants deficient in DNA binding. These mutant receptors included an AR C562G mutation in the DNA binding domain (DBD) (62), a PR C577A mutation in the DBD (63), and a GRdim4 mutation containing the dim1 mutation, A458T, which has been previously described (22) as well as three other mutations (N454D, R460D, D462C) that further ensure loss of dimerization ability (21, 64), and thereby prevent DNA binding by the mutant receptor. To ensure that the mutant receptors were expressed at similar levels as the wild-type receptors, we overexpressed the mutant receptors in either LβT2 cells, in the case of mutant AR, or in Cos-1 cells, in the case of mutant PR and GR. For PR and GR, Cos-1 cells were used because overexpression of either wild-type or mutant receptors could not be detected by Western blot in LβT2 cell extracts, perhaps due to a lack of stability of the full-length receptor or lower transfection efficiency than Cos-1 cells. As demonstrated in Fig. 5, both wild-type and mutant receptors were expressed at similar levels (Fig. 5, A, C, and E, arrowhead). Equal amounts of protein were loaded as indicated by the similar level of expression of nonspecific bands in all three lanes of the gels. Although both wild-type and mutant receptors were expressed at similar levels, we observed no significant induction of the FSHβ promoter with the AR C562G mutant compared with the induction with the wild-type receptor upon treatment with 100 nm R1881 (Fig. 5B). Activation of the FSHβ promoter by the PR C577A mutant was also diminished after treatment with 100 nm R5020 (Fig. 5D). Additionally, no FSHβ induction with the GRdim4 mutation was seen upon treatment with 100 nm dexamethasone (Fig. 5F). These data indicate that AR, PR, and AR all need to bind DNA directly to stimulate transcription of the FSHβ gene in the presence of the appropriate steroid hormone.
Fig. 5. AR, PR, and GR Require DNA Binding to Facilitate FSHβ Gene Expression.
A, C, and E, Wild-type and mutant steroid receptors were overexpressed, and protein levels were analyzed by Western blot to ensure that wild-type and mutant receptors were expressed at a similar level. The arrowhead denotes the band specific for the respective steroid receptors, and the nonspecific bands demonstrate equal protein loading. A, WT AR, mutant AR (ARC562G), or empty vector control (pSG5) were overexpressed in LβT2 cells. B, WT PR, mutant PR (PRC577A) or empty vector control (pCMV5) were overexpressed in Cos-1 cells. C, WT GR, mutant GR (GRdim4) or empty vector control (pSG5) were overexpressed in Cos-1 cells. B, D, and F, −1000FSHβluc reporter gene was transiently transfected into LβT2 cells along with the wild-type or mutant receptor as indicated. After overnight starvation in serum-free media, the cells were treated for 24 h with hormone. The results represent the mean ± sem of at least three experiments performed in triplicate and are presented as fold induction relative to the vehicle control. *, Indicates that the hormone treatment was significantly different from the vehicle-treated control using Student’s t test. B, LβT2 cells were transiently transfected with the wild-type or mutant AR (ARC562G) expression vector and then treated with 100 nm R1881. D, Cells were transiently transfected with wild-type or mutant PR (PRC577A) expression vector and then treated with 100 nm R5020. F, Cells were transiently transfected with wild-type GR or GRdim4 mutant expression vector and then treated with 100 nm dexamethasone (Dex). WT, Wild type.
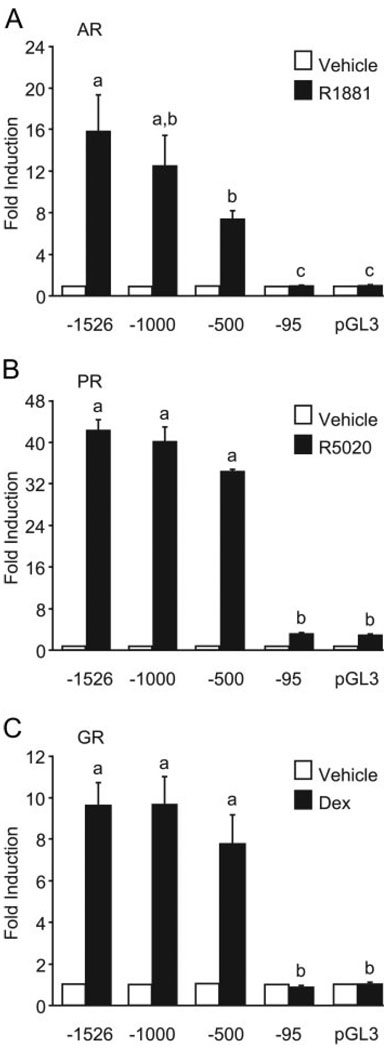
HREs in the Proximal Promoter Are Critical for FSHβ Induction by Androgens, Progestins, and Glucocorticoids
To map the promoter elements required for steroid hormone responsiveness in the mouse FSHβ gene promoter, truncation/deletion analysis was used. LβT2 cells were transiently transfected with truncations of the mouse FSHβ gene ranging from 1526 to 95 bp upstream of the transcription start site, and the ability of steroids to induce FSHβ was measured (Fig. 6). Truncation of the promoter to −95 resulted in a loss of responsiveness for each of the three hormones. Although some response to androgens was found in the upstream regions of the FSHβ promoter, a considerable degree of responsiveness was conferred in the first 500 bp of the FSHβ promoter (Fig. 6A). Interestingly, progestins and glucocorticoids did not appear to confer any additional response to FSHβ after the first 500 bp of the promoter (Fig. 6, B and C). Although differences in steroid responsiveness may exist on the FSHβ promoter, all three steroid receptors studied can act within the first 500 bp of the FSHβ promoter, implying that all three regulate the FSHβ promoter directly at the level of the gonadotrope.
Fig. 6. Induction of FSHβ by Steroid Hormone Receptors Maps to a Region Between −500 and −95 bp of the Proximal Promoter.
The −1526FSHβluc, −1000FSHβluc, −500FSHβluc, or −95FSHβluc reporter genes were transiently transfected into LβT2 cells along with the indicated receptor expression vector. After overnight starvation in serum-free media, the cells were treated for 24 h with hormone. The results represent the mean ± sem of at least three experiments performed in triplicate and are presented as fold induction relative to the vehicle control. Significantly different levels of hormone induction among truncations are indicated by differing letters, a, b, or c as determined by one-way ANOVA followed by Tukey’s post hoc test. A, LβT2 cells were transiently transfected with the reporter genes and the AR expression vector after which the cells were treated with 100 nm R1881. B, LβT2 cells were transiently transfected with the reporter genes and the PR expression vector and then the cells were treated with 100 nm R5020. C, LβT2 cells were transiently transfected with the reporter genes and the GR expression vector after which the cells were treated with 100 nm dexamethasone (Dex).
Because the responses to androgens, progestins, and glucocorticoids mapped to a proximal region of the FSHβ promoter and the responses also required a receptor capable of binding DNA, we examined the mouse promoter sequence in this region for putative HREs. This region contains putative HREs at −381/−367, −230/−216, and −139/−125 of the mouse promoter (see Fig. 7). These elements contain three or four of the G/C residues that have been shown to be critical for high-affinity binding of steroid receptors to DNA. These elements are also analogous to elements in the proximal rat and ovine FSHβ promoters that were identified as PR-binding sites, although the functional role of these sites in progesterone responsiveness was not previously determined (38, 39). Three additional elements were originally identified in the rat and ovine promoters. These correspond to putative HREs at −273/−259, −197/−183, and −175/−161 of the mouse promoter but are less conserved than the previous three elements.
Fig. 7. Conservation of Putative HREs in the Proximal FSHβ Promoter.
Putative HREs from the mouse, rat, ovine, and human FSHβ promoters are aligned 5′ to 3′. The 5′-start of the HRE in each respective species is given on the left. Bold letters indicate homology to the mouse sequence. Boxes highlight conserved G/C residues. References for the studies in which the respective HREs have been characterized are listed on the right.
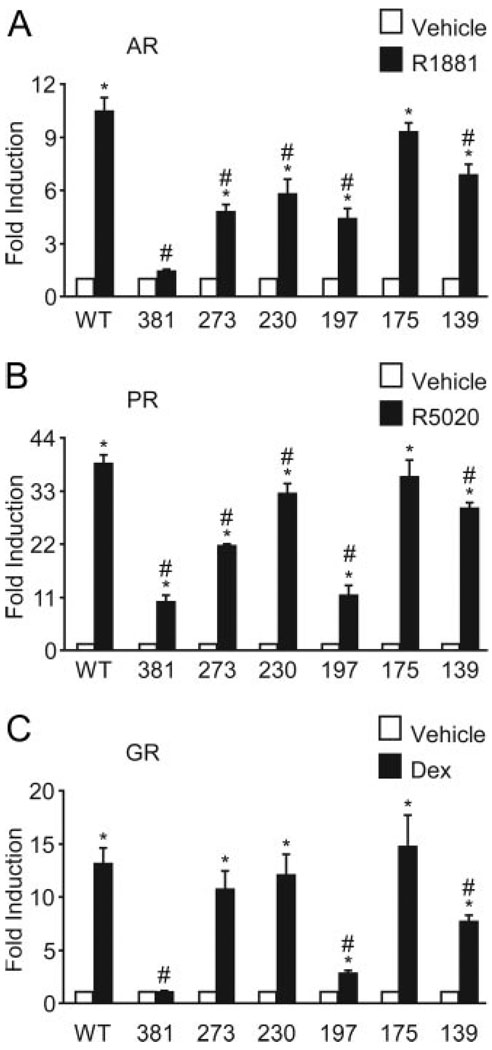
To investigate the importance of the individual elements, we created mutations in the six putative HREs by site-directed mutagenesis in the context of the −1000FSHβluc reporter gene. To disrupt binding of the steroid receptors to the putative HREs, mutations were made in the G/C residues critical for high-affinity binding (Fig. 7). Not surprisingly, none of the mutations affected basal expression of the FSHβ gene (data not shown). Mutation of the −381 site completely prevented the response to androgen (100 nm R1881), whereas the androgen responsiveness with mutations in the −273, −230, −197, and −139 HREs was diminished to approximately 46%, 55%, 42%, and 65%, respectively, of the wild-type FSHβ reporter gene (Fig. 8A). Interestingly, the −381 and −197 HRE mutations reduced the response to progesterone (100 nm R5020) to approximately 26% and 29%, respectively, whereas the −273, −230, and −139 HRE mutations decreased the response to progesterone to 55%, 83%, and 76%, respectively, of wild type (Fig. 8B). The −381 HRE mutation also completely abrogated responsiveness of the FSHβ reporter gene to glucocorticoid (100 nm dexamethasone). Induction by dexamethasone was inhibited with the −197 and −139 HRE mutations to approximately 21% and 59%, respectively, but, in contrast to the other two hormones, no significant inhibition was seen with mutation of the −273 and −230 HREs (Fig. 8C). Mutation of the −175 HRE had no functional effect on the androgen, progestin, or glucocorticoid responsiveness of the FSHβ promoter (Fig. 8). Clearly, the −381 and −197 HREs play a prominent role in the response to all three of the steroid hormones. The −139 element also appears to be necessary for induction by all three hormones and, whereas the −273 and −230 elements play a role in androgen and progesterone responsiveness, they do not appear to be necessary for glucocorticoid responsiveness.
Fig. 8. Multiple HREs Play Roles in the Induction of FSHβ by AR, PR, and GR.
The wild-type −1000FSHβluc reporter gene, or one of the six mutants, was transiently transfected into LβT2 cells along with the indicated receptor expression vector. After overnight starvation in serum-free media, the cells were treated for 24 h with hormone. The results represent the mean ± sem of at least three experiments performed in triplicate and are presented as fold induction relative to the vehicle control. *, Indicates that the hormone treatment was significantly different from the vehicle-treated control using Student’s t test. #, Indicates that the induction of the mutant reporter gene is significantly different from the induction of the wild-type reporter gene using one-way ANOVA followed by Tukey’s post hoc test. A, LβT2 cells were transiently transfected with the indicated reporter gene and the AR expression vector and then treated with 100 nm R1881. B, LβT2 cells were transiently transfected with the indicated reporter gene and the PR expression vector and then treated with 100 nm R5020.C, LβT2 cells were transiently transfected with the indicated reporter gene and the GR expression vector and then treated with 100 nm dexamethasone (Dex). WT, Wild type.
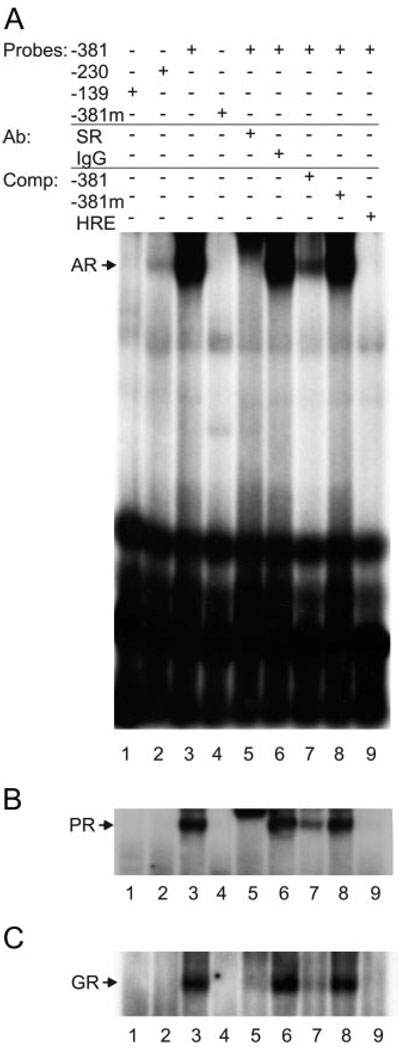
AR, PR, and GR Bind to the −381 HRE in the Mouse FSHβ Promoter
We used an EMSA to assess whether AR, GR, and PR can bind to the HREs in the proximal mouse FSHβ promoter. Although we did not detect steroid receptor binding using LβT2 nuclear extracts, we observed binding of AR, PR, and GR from baculovirus-infected insect whole-cell extracts to the wild-type −381 element (Fig. 9, lane 3), whereas no binding to the −381 HRE mutant was seen (lane 4). For each of the receptors, the resulting complex on the −381 oligonucleotide was supershifted by a receptor-specific antibody (lane 5) but not by IgG (lane 6). The complexes also showed self-competition (lane 7), failed to compete with a mutant probe (lane 8), and showed evidence of competition with a consensus HRE (lane 9). These results confirm that AR, PR, and GR can all bind directly and specifically to the −381 HRE in the mouse FSHβ-subunit gene. In agreement with the results obtained by Spady et al. (55), using the ovine FSHβ promoter, AR also bound to the −230 element (Fig. 9A, lane 2) albeit to a much lesser degree than the −381 element.
Fig. 9. Ligand-Bound AR, PR, and GR All Bind Specifically to the −381 HRE.
Whole-cell extracts containing overexpressed AR, PR, or GR from baculovirus-infected insect cells were incubated with the −139, −230, or −381 probe and tested for complex formation in EMSA. The relevant steroid receptor-DNA complex on the −381 element is shown in lane 3 and on the mutated −381 element (mutation as in Fig. 8), whereas the antibody supershift is shown in lane 5, IgG control (lane 6), self-competition (lane 7), mutant competition (lane 8), and competition with a consensus HRE (HRE) (lane 9). A, Probes were incubated with overexpressed AR. B, Probes were incubated with overexpressed PR. C, Probes were incubated with overexpressed GR. Ab, Antibody; Comp, competition.
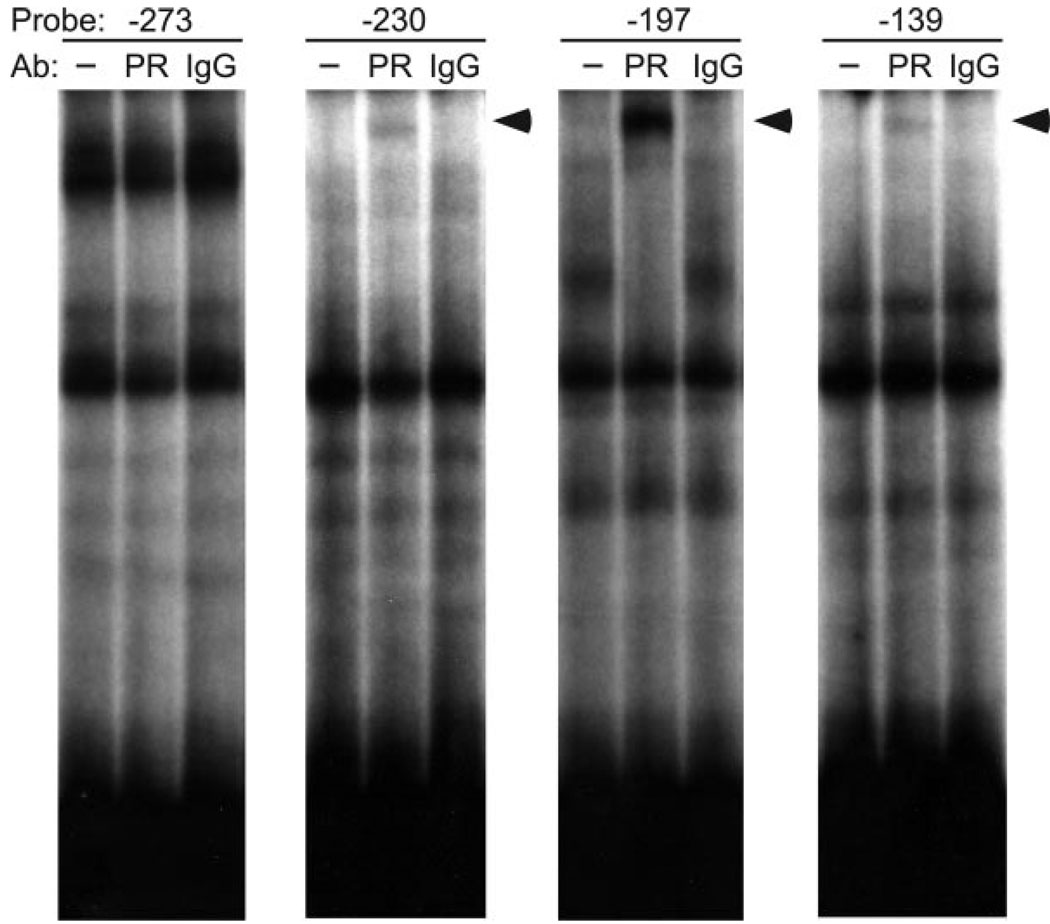
To determine whether AR, PR, or GR could bind the other functional HREs, the EMSA was repeated with probes encompassing the −273 and −197 sites as well as the −230 and −139 sites. As seen in Fig. 10, an antibody specific for PR produced a supershift when the −197 probe was incubated with baculovirus-infected insect whole-cell extracts overexpressing PR (arrowhead), whereas no shift was seen with the negative nonspecific IgG control. This supershift was detectable after a much longer exposure than the EMSA in Fig. 9B. These results show that PR binds weakly to the −197 HRE compared with the −381 site and contrast with previous gel shifts that used HREs from the rat and ovine promoters (38, 39). In addition, we saw a very weak supershift on the −230 and −139 sites that could indicate potential binding at these sites by PR as well. We did not observe binding to the other functional HREs by AR or GR under these EMSA conditions (data not shown) with the exception of the binding of AR to the −230 HRE as shown in Fig. 9. These results indicate that, although these HREs play a functional role in hormone responsiveness, they do not bind steroid receptors with high affinity on their own.
Fig. 10. PR Binds the −197 HRE.
Whole-cell extracts containing overexpressed PR from baculovirus-infected insect cells were incubated with the −273, −230, −197, or −139 probes and tested for complex formation in EMSA. Antibodies (Ab) are indicated with the left lane containing no antibody (−), the middle lane containing PR antibody (PR), and the right lane containing a nonspecific IgG control antibody (IgG). The antibody supershift is marked with an arrowhead.
Because AR, PR, and GR did not bind to the other functional HREs in a convincing fashion (except PR binding to the −197 site), we tested whether other proteins from LβT2 nuclear extracts bound the −273, −230, −197, or −139 sites. Although no difference was seen between vehicle-treated and hormone-treated LβT2 nuclear extracts (data not shown), basal protein complexes bound all four probes (Fig. 11). Arrows denote specific complexes that were competed by unlabeled-self but not by unlabeled-mutant, competitor, using the −273 probe (Fig. 11A), the −230 probe (Fig. 11B), the −197 probe (Fig. 11C), and the −139 probe (Fig. 11D). Competition with mutant probes containing the same mutations used in the transient transfection experiments was used to determine whether any of the basal complexes were sensitive to those specific mutations. As can be seen, each of the gel shifts contained at least one complex that was sensitive to a mutation in the functional HRE, indicating that these basal proteins may also contribute to steroid binding or induction although, as mentioned previously, mutation of any of the HREs did not alter basal activity of the FSHβ promoter (data not shown) nor did steroid treatment alter these EMSA complexes.
Fig. 11. Specific Protein Complexes from LβT2 Nuclear Extracts Bind the −273, −230, −197, and −139 HREs.
Nuclear extracts prepared from LβT2 cells were incubated with the −273, −230, −197, or −139 probes and tested for specific complex formation in EMSA. Unlabeled competitors (500×) (Comp) were added to test the specificity of complex formation as indicated. A, −273 probe with no competition (−), self-competition (273), or mutant competition (273m). B, −230 probe with no competition (−), self-competition (230), or mutant competition (230m). C, −197 probe with no competition (−), self-competition (197), or mutant competition (197m). D, −139 probe with no competition (−), self-competition (139), or mutant competition (139m). Complexes competed by self-competition, but not by mutant competition, are indicated with arrows.
DISCUSSION
Gonadal steroid hormone feedback is a crucial component of the control of gonadotropin synthesis in the pituitary gonadotrope (15). In addition, although exposure to stress hormones such as corticosterone or dexamethasone can inhibit ovulation in primates and rodents (45, 65–70), there is evidence that glucocorticoids play a physiological role in activating FSHβ gene expression. For instance, both progestin and glucocorticoid levels peak during proestrus (71, 72), and this coincides with increased FSHβ mRNA expression and the secondary FSHβ surge that occurs in the morning of estrus in rodents (73). Furthermore, glucocorticoids, as well as progestins, appear to be necessary for the secondary FSHβ surge (37, 74). These studies complement the numerous experiments in rats and mixed rat pituitary cells that found induction of FSHβ mRNA after treatment with androgens, progestins, or glucocorticoids (24, 26, 28, 29, 33, 34, 41–43).
In the current study, we characterized the specific molecular mechanisms of steroid hormone regulation of the FSHβ gene in LβT2 cells. Our results demonstrate that the proximal murine FSHβ promoter is activated by androgens, progestins, and glucocorticoids (as well as their synthetic analogs) in the context of immortalized gonadotropes in culture (Figs. 1 and 3) in contrast to the lack of estrogen responsiveness on the murine FSHβ promoter (Fig. 1). We also show, for the first time, that progestins and glucocorticoids, like androgens, can suppress transcription of the LHβ-subunit gene at the level of the gonadotrope (Fig. 4), although glucocorticoids have previously been shown to inhibit GnRH induction of LHβ (45). However, because no obvious HREs exist in the LHβ promoter, it is likely that the mechanism(s) of action are indirect, similar to the aforementioned studies concerning the suppression of LHβ by androgens. The study of the mechanism(s) of LHβ suppression by progestins and glucocorticoids is currently ongoing in our laboratory. Although FSH and LH are produced in the same cell type and both of their β-subunits are positively regulated by GnRH and activin (10, 75–77), the expression profiles of FSHβ and LHβ have been shown to differ over the menstrual cycle (73, 78). It is intriguing to postulate that some of the observed differential regulation of the gonadotropin β-subunits may be due to these three 3-keto steroid hormones.
Androgens, progestins, and glucocorticoids could affect FSHβ synthesis directly or by indirect means such as altering the balance of the autocrine activin/inhibin/follistatin system (30, 79). Our data indicate that induction of FSHβ by androgens, progestins, and glucocorticoids is dependent on the presence of the appropriate hormone-bound steroid receptor because expression of the murine FSHβluc reporter gene depends on the receptor levels (Fig. 2) and hormone concentration (Fig. 3). We also provide evidence that the murine FSHβ promoter is directly bound and regulated by all three steroid hormone receptors. Using ChIP, we show that the endogenous AR, PR, and GR can bind the FSHβ promoter in vivo in LβT2 cells (Fig. 1B). Moreover, the use of mutant steroid receptors lacking the ability to bind DNA demonstrated that the steroid hormone receptors must bind DNA directly to modulate FSHβ gene expression (Fig. 5). We also show that all three of the steroid hormone receptors can bind to specific sites within the FSHβ promoter in vitro using gel-shift analysis (Figs. 9 and 10). Furthermore, mutation of putative HREs in the context of the −1000FSHβluc reporter gene abolished the responsiveness of FSHβ to androgens, progestins, and glucocorticoids (Fig. 8). Thus, this is the first demonstration that AR, PR, and GR can all directly induce murine FSHβ gene expression.
It has been suggested previously that steroids (androgens in particular) can induce the expression of the GnRH-R (32,55) and that this regulation may be one of the contributing factors to induction of FSHβ by steroids. However, our results demonstrating the suppression of the LHβ gene by steroids would argue against a role of the GnRH-R. Furthermore, Bedecarrats and Kaiser (80) have shown that up-regulation of GnRH-R by overexpression or a higher-pulse frequency of GnRH inhibits FSHβ expression. These results all point to direct regulation of the gonadotropin β-subunit genes by steroid hormones.
In addition to establishing that androgens, progestins, and glucocorticoids directly modulate FSHβ transcription, we characterized the roles played by the HREs contained within the FSHβ promoter. Because the responsiveness to steroid hormones mapped within the first 500 bp of the murine FSHβ promoter (Fig. 6), we concentrated on the putative HREs in this region of the promoter. The six elements characterized had all been shown to bind PR in earlier studies using the rat and ovine promoters (38, 39), although the relative importance of these sites had not been evaluated previously. In agreement with the data obtained using the rat promoter, the −381 HRE specifically bound PR as well as binding AR and GR (Fig. 9). Our gel-shift experiments suggest that the −381 HRE may be critical for direct regulation of the murine FSHβ promoter. This hypothesis is further substantiated by the fact that mutation of this site greatly reduced or abolished FSHβ responsiveness to androgens, progestins, and glucocorticoids (Fig. 8). Interestingly, the −381 HRE is an 11/12 match for a direct repeat element as opposed to a classical palindromic inverted repeat. This type of element has been reported to selectively confer specificity to AR on several enhancers and promoters [recently reviewed by Verrijdt et al. (81)]. However, in the context of the FSHβ promoter, this sequence appears to be recognized by all three steroid receptors.
This raises the question of whether there is a specific response to these 3-keto steroid hormones on the murine FSHβ promoter because androgens, progestins, and glucocorticoids have such different physiological effects. Much of the specificity may be provided by different levels of the steroid hormones. For instance, there is a circadian variation in glucocorticoid levels that can be affected by internal or external stress. Additionally, progesterone levels vary dramatically over the estrous cycle, and high levels are produced during pregnancy. Testosterone levels also increase in the male at puberty and, after peaking over the following decade, progressively decline with age. Factors such as temporal expression of the steroid receptors or subtle sequence preferences in the multiple HREs present in the FSHβ promoter or in residues flanking the HREs, which result in different conformational changes in the receptors and, thus, differential cofactor recruitment or protein-protein interactions with adjacent DNA-binding proteins, could also have an effect on specificity.
Because the magnitude of steroid hormone response imparted by each HRE is often weak, multiple HREs are often found in close proximity in the promoters of steroid-responsive genes (82). This situation also appears to apply to the murine FSHβ promoter because mutation of the −273, −230, −197, and −139 HREs all reduce induction of FSHβ by both androgens and progestins, suggesting that they are needed for the full induction. Glucocorticoid responsiveness seems to be less sensitive to mutation of the HREs although mutation of the −197 and −139 HREs did have a considerable effect. In addition to binding of AR, PR, and GR to the −381 HRE, we observed weak binding by PR to the −197 HRE and AR to the −230 site (Figs. 9 and 10). These data suggest several possibilities. First, these elements (with the exception of the −381 HRE) may have a low affinity for steroid receptors, and binding is difficult to detect using gelshift analysis although binding could be aided by high-affinity binding at the −381 site. Second, nuclear proteins present in the LβT2 cells may be necessary for the steroid receptors to bind to these elements. Finally, these sites could be required for the binding of other transcription factors that would alter steroid hormone responsiveness. In support of the last two possibilities, we observed basal protein complex formation on the −297, −230, −197, and −139 elements using LβT2 nuclear extracts that were sensitive to mutations in these HREs (Fig. 11) although mutations in the HREs did not affect basal activity of the FSHβ promoter nor did steroid treatment of the cells alter the complexes (data not shown).
All of the functional HREs we characterized in the mouse promoter have a degree of conservation across multiple species, suggesting that they may play roles in steroid regulation of other mammalian species (Fig. 7). Not surprisingly, the putative HRE with the least conservation, the −175 element, had no functional effect in androgen, progestin, or glucocorticoid responsiveness of the murine FSHβ promoter (Fig. 8). Although the HREs in the proximal FSHβ promoter are well conserved in mammals, there appear to be species-specific differences in the regulation of the FSHβ promoter by steroids. Our experiments with the murine FSHβ promoter in LβT2 cells and previous studies examining endogenous FSHβ expression in rodents and in rat pituitary cells contrast with the regulation of FSHβ by androgen and progestins observed in sheep and primates. In particular, androgens have been shown to repress FSH secretion at the level of the pituitary in rams and male rhesus monkeys (83, 84) as well as in mixed pituitary cell cultures from transgenic mice containing 10 kb of the human FSHβ promoter (85). Moreover, FSHβ mRNA levels have been shown to decrease after progestin treatment in ovine mixed pituitary cell cultures (86) and in ovariectomized ewes pretreated with estrogen and treated with progesterone that received a hypothalamic-pituitary disconnection (87). Progesterone treatment also repressed the luciferase activity in pituitary cells derived from a transgenic mouse containing 4.7 kb of the ovine FSHβ promoter linked to a luciferase reporter gene (88). Curiously, this same FSHβluc reporter gene was activated by progestins when transiently transfected into ovine mixed pituitary culture (38) and induced by androgens when transfected into LβT2 cells (55).
One possibility is that the results obtained in rodents, as compared with sheep and primates, differ due to species-specific steroid effects on the FSHβ promoter. For instance, the −381 HRE that we found to be essential for hormone responsiveness on the murine FSHβ promoter is conserved between mice and rats but not present in sheep. However, species-specific differences would not explain why the ovine FSHβluc reporter gene was activated by progestins (38) whereas the endogenous gene was repressed (86). It is also plausible that a factor present in sheep and primate gonadotropes is necessary for the negative regulation; however, this is difficult to address because the available immortalized gonadotrope-derived cell lines and transgenic animal models are based on the mouse. Finally, it is credible that paracrine influences from other secretory cell types present in the anterior pituitary could be responsible for the negative regulation observed with the ovine and primate promoters. For example, androgens have been shown to regulate follistatin mRNA levels (27, 30, 89) and thus could indirectly mediate transcription of FSHβ mRNA by impacting the autocrine/paracrine activity of activin in the gonadotrope. In addition, folliculostellate cells in the pituitary have been shown to secrete follistatin and overgrow mixed pituitary cell cultures (89). Clearly, further investigation is needed to discern whether steroids play distinct roles in the regulation of FSHβ mRNA levels in different mammalian species.
In summary, we have demonstrated that androgens, progestins, and glucocorticoids via their receptors directly induce expression of the murine FSHβ-subunit gene at the level of the gonadotrope and that this regulation occurs through binding of the receptors to the −381 HRE in the proximal FSHβ promoter. Additionally, this activation is specific for FSHβ, because LHβ gene expression is repressed by androgens, progestins, and glucocorticoids. Although our studies do not exclude the possibility of steroidal regulation of GnRH synthesis as a central regulator of gonadotropin production, they do suggest that in endocrine disorders, such as polycystic ovary syndrome and Cushing’s disease with excess androgens and glucocorticoids, respectively, fertility could be impacted by altered FSHβ and LHβ gene expression directly at the level of the gonadotrope, as well as the hypothalamus. Further examination of androgen, progesterone, and glucocorticoid regulation of the gonadotropin genes in the anterior pituitary is needed to better understand the physiological role these steroid hormones play in the maintenance of reproductive fitness. To begin to address their roles, selective ablation of the individual steroid hormone receptors in the gonadotrope cells needs to be performed using the Cre-LoxP system in mice. These conditional knockouts will determine whether AR, PR, and GR are necessary for gonadotropin regulation or whether there is a more dominant steroid regulation of the gonadotrope through afferent communication with the GnRH neuron. Evidence suggests that, individually, each of these steroids contributes to reproductive fitness through their cognate receptors. However, it is likely that complex interactions among them and other regulators of the hypothalamic-pituitary-gonadal axis such as GnRH and activin exist and are also critical for reproduction.
MATERIALS AND METHODS
Hormones
Testosterone, dihydrotestosterone, 17β-estradiol, progesterone, corticosterone, and dexamethasone were obtained from Sigma-Aldrich (St. Louis, MO). Promegestone (R5020) and methyltrienolone (R1881) were purchased from NEN Life Sciences (Boston, MA).
Construction of Reporter Plasmids
Three luciferase reporter gene plasmids were generated by PCR amplification of the mouse FSHβ promoter from a genomic clone kindly provided by Malcolm Low. Each PCR product was ligated into a pGL3 luciferase reporter plasmid (Promega Corp., Madison, WI) that had been digested with KpnI and HindIII. Initially, a luciferase reporter plasmid driven by 1526 bp of the mouse FSHβ promoter (−1526FSHβluc) was constructed. Two other reporter plasmids, −1000FSHβluc and −500FSHβluc were generated in a similar manner. Construction of the −95FSHβluc plasmid was described previously (90). We confirmed the sequences of all promoter fragments with dideoxynucleotide sequencing by the DNA Sequencing Shared Resource, University of California San Diego Cancer Center.
The steroid receptor expression vectors used in these studies all contained rat cDNAs and were: AR, pSG5-rAR (62); PR, pCMV5-rPRB (provided by Benita Katzenellenbogen); GR, pSG5-rGR (provided by Keith Yamamoto); and ER, pcDNA3.1-rERα, and ERβ (91).
Mutagenesis
We used the QuikChange Site-Directed Mutagenesis Kit (Stratagene, La Jolla, CA) to generate mutations in six putative HREs in the proximal FSHβ promoter. The mutagenesis was performed using the −1000FSHβluc plasmid and the appropriate oligonucleotides according to the manufacturer’s protocol. The following oligonucleotides were used for mutagenesis: −139HREmut [5′-CATTTAGACTGCTTTGCCGAGGCTTCATGTCCCTGTCCGT-3′], −175HREmut [5′-AAACCATCATCACTGATAGGATTTTCTGGTCTGTGGCATTTAGAC-3′], −197HREmut [5′-ATATCAGATTCGGTTTCTAGAGAAACCATCATCACTGATAGCATTTTC-3′], −230HREmut [5′-TAATTTACAAGGTGAGCGAGTGGGTCTGGTGCCATATCAGATTCG-3′], −273HREmut [5′-AAGATCAGAAACAATAGTCTAGAGTCTAGAGTCACATTTAATTTAC-3′], and −381-HREmut [5′-TTCATACACTTGGAGTCTTGAGTCTCTTGTTGGATCAATTAAGAC-3′]. The mutated residues are underlined.
We also used the QuikChange Site-Directed Mutagenesis Kit to generate mutant PRs and GRs unable to bind to DNA. The PRC577A mutant is analogous to a C587A mutation in the human PRB that prevents DNA binding (63). The GRdim4 mutant contains four point mutations that prevent dimerization of the receptor and thus DNA binding: N454D, A458T, R460D, and D462C (64). The mutagenesis was performed using the pCMV5-rPRB or the pSG5-rGR plasmid, respectively, and the appropriate oligonucleotides according to the manufacturer’s protocol. The following oligonucleotides were used for mutagenesis: PRC577Amut [5′-TCACTATGGTGTGCTTACCTGTGGGAGCGCCAAGGTCTTCTTTAAGAGGG-3′] and GRdim4mut [5′-AAGGACAGCACGATTACCTTTGTACTGGAGATAACTGTTGCATCAT-3′]. As with the reporter plasmids, all mutations were confirmed by dideoxynucleotide sequencing. Construction of the pSG5-rARC562G mutant was described previously (62).
Cell Culture and Transient Transfection
All of the transient transfection experiments were performed with the LβT2 cell line (13). LβT2 cells were maintained in 10-cm diameter dishes in DMEM (Cellgro, Mediatech, Herndon, VA) supplemented with 10% fetal bovine serum (Omega Scientific, Inc., Tarzana, CA) at 37 C with 5% CO2. One day before transfection, 3 × 105 cells per well were plated into 12-well plates. Transient transfection was performed using Fugene 6 reagent (Roche Molecular Biochemicals, Indianapolis, IN) following the manufacturer’s instructions. Each well was transfected with 0.4 µg of reporter plasmid. Additionally, the cells were transfected with 0.2 µg of the appropriate steroid receptor (unless otherwise noted). As an internal control for transfection efficiency, we transfected the LβT2 cells with 0.2 µg of a reporter plasmid containing β-galactosidase driven by the Herpes virus thymidine kinase promoter (tk-β-gal) or the Rous sarcoma virus promoter (RSV-β-gal). The cells were switched to serum-free DMEM supplemented with 0.1% BSA, 5 mg/liter transferrin, and 50 nm sodium selenite 6 h after transfection. The following day, the cells were treated with ethanol (vehicle control) or hormone for 24 h. The cells were washed once with 1 × PBS and then lysed with 0.1 m K-phosphate buffer, pH 7.8, containing 0.2% Triton X-100. After lysing the cells, we assayed the luciferase activity using a buffer containing 100 mm Tris-HCl, pH 7.8, 15 mm MgSO4, 10 mm ATP, and 65 µm luciferin. β-Galactosidase activity was measured using the Galacto-light assay (Tropix, Bedford, MA) according to the manufacturer’s protocol. Both luciferase and β-galactosidase activities were measured using an EG&G Berthold Microplate Luminometer (PerkinElmer Corp., Norwalk, CT).
RT-PCR
LβT2 cells were grown to 80% confluency on 6-cm plates, and total RNA was extracted from LβT2 cells with TRIzol Reagent (Invitrogen, Carlsbad, CA) following the manufacturer’s protocol. Contaminating DNA was removed with DNA-free reagent (Ambion, Inc., Austin, TX). RNA (2.5 µg) was reverse-transcribed using the SuperScript III First-Strand Synthesis System (Invitrogen) according to the manufacturer’s protocol. The following oligonucleotides were used for PCR: AR sense [5′-GAGAACCCATTGGACTACG-3′] and AR antisense [5′-TGAAGAAGACCTTGCAGC-3′]; PR sense [5′-CTAAATGAGCAGAGGATGAAGGAG-3′] and PR antisense [5′-TGGGGCAACTGGGGCAGCAATAAC-3′]; GR sense [5′-TGCTATGCTTTGCTCCTGATCTG-3′] and GR antisense [5′-TGTCAGTTGATAAAACCGCTGCC-3′] under the following conditions: 95 C for 2 min followed by 32 cycles of 95 C for 45 sec, 52 C for 1 min, and 72 C for 1 min. The PCR contained either 2 µl of reverse-transcribed LβT2 RNA or, as a negative control, 2 µl of LβT2 RNA that was not reverse-transcribed. PCR products were run on a 1% acrylamide gel stained with ethidium bromide.
ChIP
LβT2 cells were grown to confluency in 15-cm plates, treated with 100 nm hormone, and proteins were cross-linked to DNA by the direct addition of 1% formaldehyde to the cell medium. The nuclear fraction was obtained, and chromatin was sonicated to an average length of 1 kb in sonication buffer [50 mm HEPES, 140 mm NaCl, 1 mm EDTA, 1% Triton X-100, 0.1% Na-deoxycholate, and 0.1% sodium dodecyl sulfate (SDS)]. The lysate was diluted with ChIP dilution buffer (0.01% SDS, 1.1% Triton, 1.2 mm EDTA, 16.7 mm Tris pH 8, 167 mm NaCl) to a total of 3.5 ml and precleared with 100 µl Protein A/G PLUS-Agarose beads (Santa-Cruz Biotechnology, Inc., Santa Cruz, CA). Protein-DNA complexes were incubated overnight with the C-19x AR polyclonal antibody (Santa Cruz Biotechnology, Inc.), the 1294 PR mouse monoclonal antibody (provided by Dean Edwards), the N499 GR rabbit polyclonal antibody (donated by Keith Yamamoto), or a nonspecific IgG control (Santa Cruz) and precipitated with Protein A/G beads (Santa Cruz). A fraction of the protein-DNA was not precipitated but set aside as the input. The agarose beads were washed in the following order: low-salt wash buffer [0.1% SDS, 1% Triton X-100, 2 mm EDTA, 20 mm Tris (pH 8), 150 mm NaCl], high-salt wash buffer [0.1% SDS, 1% Triton X-100, 2 mm EDTA, 20 mm Tris (pH 8), 500 mm NaCl], LiCl wash buffer [250 mm LiCl, 1% Nonidet P-40, 1% Nadeoxycholate, 1 mm EDTA, 10 mm Tris (pH 8)] and twice with Tris-EDTA buffer. The protein-DNA complexes were eluted with elution buffer (1% SDS, 0.1 m NaHCO3), and the crosslinks were reversed with the addition of 200 mm NaCl and incubation at 65 C for 4 h. The DNA was phenol-chloroform extracted, precipitated, and then resuspended in 50 µl of water. The primers used in PCR for the FSHβ promoter were 5′-GGTGTGCTGCCATATCAGATTCGG-3′ and 5′-GCATCAAGTGCTGCTACTCACCTGTG-3′ and spanned the 280-bp sequence in the mouse FSHβ gene from −223 to +57. The primers for the FSHβ coding region were 5′-GCCGTTTCTGCATAAGC-3′ and 5′-CAATCTTACGGTCTCGTATACC-3′. The following PCR conditions were used: 4 min at 95 C, followed by 26 cycles consisting of 1 min at 95 C, 1 min at 60 C, and 1 min at 72 C, and an extension of 10 min at 72 C. The PCR product was labeled by including [α-32P]dATP in the nucleotide mix and run on a 5% acrylamide gel in 0.5× Tris-borate-EDTA buffer. The gels were dried and subjected to autoradiography.
Preparation of Protein Extracts
Full-length, human AR containing a Flag epitope tag (92), human Flag-PRB (93), or Flag-GR (kindly provided by Steve Nordeen) was overexpressed in Sf9 insect cells via a bacu-lovirus expression system by the University of Colorado Cancer Center Tissue Culture Core Facility. The Sf9 cells were inoculated with virus at a multiplicity of infection of 1.0 and grown for an additional 48 h at 27 C. Cells containing AR, PR, or GR were treated for the last 24 h before harvest with 1 µm DHT, 200 nm R5020, or 500 nm triamcinolone acetonide (final concentration), respectively. The cells were harvested by centrifugation at 1500 rpm for 15 min, washed once in TG buffer (10 mm Tris-HCl, pH 8.0; and 10% glycerol) and frozen as a pellet at −80 C. We lysed the Sf9 cells in a homogenization buffer [20 mm Tris-HCl (pH 7.5), 350 mm NaCl, 1 mm dithiothreitol, 10% glycerol, 0.5 µg/ml leupeptin, 10 µg/ml bacitracin, 2 µg/ml aprotinin, 1 µg/ml pepstatin]. All procedures were done at 0–4 C. The cell lysate was centrifuged at 40,000 rpm for 30 min, and the supernatant was taken as a soluble whole-cell extract.
Nuclear extracts were prepared from LβT2 and Cos-1 cells as previously described (94).
Western Blot Analysis
Wild-type and mutant steroid receptors, as well as their respective empty vector controls, were overexpressed in LβT2 cells (AR, ARC562G, and pSG5) or Cos-1 cells (PR, PRC577A, pCMV5 and GR, GRdim4, pSG5) by transiently transfecting 10 µg of DNA using Fugene 6 into 10-cm plates of cells and treating the cells with 100 nm R1881, R5020, or dexamethasone, respectively. Cells were harvested 24 h later by incubating cells in a lysis buffer [20 mm Tris-HCl (pH 7.4), 140 mm NaCl, 0.5% Nonidet P-40, 0.5 mm EDTA, 10 µg/ml aprotinin, 10 µg/ml pepstatin, 10 µg/ml leupeptin, and 1 mm phenylmethylsulfonyl fluoride] for 30 min. The protein concentration was determined with Bradford reagent (Bio-Rad Laboratories, Inc., Hercules, CA), and an equal amount of protein per sample was loaded on a SDS-PAGE gel. After the proteins were resolved by electrophoresis and transferred to a polyvinylidene fluoride membrane, they were probed with specific antibodies for AR, PR, and GR. Specifically, the C-19x AR polyclonal antibody (Santa Cruz Biotechnology, Inc.), the 1294 PR mouse monoclonal antibody (provided by Dean Edwards), or the N499 GR rabbit polyclonal antibody (donated by Keith Yamamoto) were used. The bands were detected with secondary antibodies linked to horseradish peroxidase and enhanced chemiluminescence reagent (Amersham Biosciences, Piscataway, NJ).
EMSA
To determine whether 3-keto steroid hormone receptors could bind to HREs in the proximal mouse FSHβ promoter, whole-cell extracts containing either AR, PR, or GR were incubated with 1 fmol of 32P-labeled oligonucleotide at 4 C for 30 min in a DNA-binding buffer [10 mm HEPES(pH 7.8), 50 mm KCl, 5 mm MgCl2,0.1% Nonidet P-40,1 mm dithiothreitol, 2 µg polydeoxyinosinic deoxycytidylic acid, and 10% glycerol]. The oligonucleotides were end-labeled with T4 DNA polymerase and [γ-32P]ATP. After 30 min, the DNA binding reactions were run on a 5% polyacrylamide gel (30:1 acrylamide-bisacrylamide) containing 2.5% glycerol in a 0.5× Tris-acetate-EDTA buffer. The C-19x AR polyclonal antibody, the 1294 PR mouse monoclonal antibody, and the N499 GR rabbit polyclonal antibody were used to supershift AR, PR, and GR, respectively. We used rabbit IgG or mouse IgG as a control for nonspecific binding. A 500-fold excess of the relevant oligonucleotide was used for competition. The following oligonucleotides were used for EMSA: −139HRE, 5′-AGACTGCTTTGGCGAGGCTTGATCTCCCTGTCCGT-3′; −197HRE, 5′-AGATTCGGTTTGTACAGAAACCATCATCACTGATA-3′; −230HRE, 5′-TACAAGGTGAGGGAGTGGGTGTGCTGCCATATCAG-3′; −273HRE, 5′-AAGATCAGAAAGAATAGTCTAGACTCTAGAGTCAC-3′; −381HRE, 5′-ACACTTGGAGTGTTCAGTCTGTTCTTGGATCAATT-3′; −139mut, 5′-AGACTGCTTTGCCGAGCTTCATGTCCCTGTCCGT-3′; −197mut, 5′-AGATTCGGTTTCTAGAGAAACCATCATCACTGATA-3′; −230mut, 5′-TACAAGGTGAGCGAGTGGGTCTGGTGCCATATCAG-3′; −273mut, 5′-AAGATCAGAAACAATAGTCTAGAGTCTAGAGTCAC-3′; −381mut, 5′-ACACTTGGAGTCTTGAGTCTCTTGTTGGATCAATT-3′; and the consensus HRE, 5’-ACGGGTGGAACGCGGTGTTCTTTTGGC-3′.
Statistical Analyses
Transient transfections were performed in triplicate, and each experiment was repeated at least three times. The data were normalized for transfection efficiency by expressing luciferase activity relative to β-galactosidase activity and relative to the empty pGL3 plasmid to control for hormone effects on the vector DNA. The data were analyzed by Student’s t test for independent samples or one-way ANOVA followed by post hoc comparisons with the Tukey-Kramer honestly significant difference (HSD) test using the statistical package JMP 5.0 (SAS Institute, Inc., Cary, NC). Significant differences were designated as P < 0.05.
Acknowledgments
We thank Djurdjica Coss, Janice Sue Bailey, and other members of the Mellon lab for helpful discussions and comments; Scott Kelley for his suggestions and critical reading of the manuscript; Malcolm Low for providing the mouse FSHβ genomic clone; Jorma Palvimo for the pSG5-rAR and pSG5-rARC562G plasmids; Benita Katzenellenbogen for the pCMV5-rPRB plasmid; and Keith Yamamoto for the pSG5-rGR plasmid and the N499 GR rabbit polyclonal antibody. We also thank Margaret Shupnik for providing the pcDNA3.1-rERα and ERβ plasmids; Mark Lawson and Marit Kreidel for the 1.8LHβluc plasmid; Elizabeth Wilson for the Flag-AR baculovirus; Steve Nordeen for the Flag-PRB and Flag-GR baculoviruses; and Dean Edwards for the 1294 PR mouse monoclonal antibody. We also thank the University of Colorado Cancer Center Tissue Culture Core Facility for baculovirus production and the University of California San Diego Cancer Center DNA Sequencing Shared Resource for dideoxynucleotide sequencing.
This work was supported by National Institute of Child Health and Human Development/National Institutes of Health (NIH) through a cooperative agreement (U54 HD012303) as part of the Specialized Cooperative Centers Program in Reproduction Research (to P.L.M.). This work was also supported by NIH Grant R37 HD020377 (to P.L.M.). V.G.T. was supported by NIH Grants F32 DK065437 and T32 HD007203. S.M.M. was partially supported by NIH Grant T32 DK07541.
Abbreviations
- AR
Androgen receptor
- ChIP
chromatin immunoprecipitation
- DHT
dihydrotestosterone
- ER
estrogen receptor
- GnRH-R
GnRH receptor
- GR
glucocorticoid receptor
- HRE
hormone response element
- PR
progesterone receptor
- PRE
progesterone response element
- SDS
sodium dodecyl sulfate
Footnotes
Disclosure statement: The authors have nothing to disclose.
REFERENCES
- 1.Kumar TR, Wang Y, Lu N, Matzuk MM. Follicle stimulating hormone is required for ovarian follicle maturation but not male fertility. Nat Genet. 1997;15:201–204. doi: 10.1038/ng0297-201. [DOI] [PubMed] [Google Scholar]
- 2.Ma X, Dong Y, Matzuk MM, Kumar TR. Targeted disruption of luteinizing hormone β-subunit leads to hypogonadism, defects in gonadal steroidogenesis, and infertility. Proc Natl Acad Sci USA. 2004;101:17294–17299. doi: 10.1073/pnas.0404743101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burns KH, Matzuk MM. Minireview: genetic models for the study of gonadotropin actions. Endocrinology. 2002;143:2823–2835. doi: 10.1210/endo.143.8.8928. [DOI] [PubMed] [Google Scholar]
- 4.Pierce JG, Parsons TF. Glycoprotein hormones: structure and function. Annu Rev Biochem. 1981;50:465–495. doi: 10.1146/annurev.bi.50.070181.002341. [DOI] [PubMed] [Google Scholar]
- 5.Kaiser UB, Jakubowiak A, Steinberger A, Chin WW. Differential effects of gonadotropin-releasing hormone (GnRH) pulse frequency on gonadotropin subunit and GnRH receptor messenger ribonucleic acid levels in vitro. Endocrinology. 1997;138:1224–1231. doi: 10.1210/endo.138.3.4968. [DOI] [PubMed] [Google Scholar]
- 6.Papavasiliou SS, Zmeili S, Khoury S, Landefeld TD, Chin WW, Marshall JC. Gonadotropin-releasing hormone differentially regulates expression of the genes for luteinizing hormone α and β subunits in male rats. Proc Natl Acad Sci USA. 1986;83:4026–4029. doi: 10.1073/pnas.83.11.4026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vale W, Rivier C, Brown M. Regulatory peptides of the hypothalamus. Annu Rev Physiol. 1977;39:473–527. doi: 10.1146/annurev.ph.39.030177.002353. [DOI] [PubMed] [Google Scholar]
- 8.Ying SY. Inhibins, activins, and follistatins: gonadal proteins modulating the secretion of follicle-stimulating hormone. Endocr Rev. 1988;9:267–293. doi: 10.1210/edrv-9-2-267. [DOI] [PubMed] [Google Scholar]
- 9.Carroll RS, Corrigan AZ, Gharib SD, Vale W, Chin WW. Inhibin, activin, and follistatin: regulation of follicle-stimulating hormone messenger ribonucleic acid levels. Mol Endocrinol. 1989;3:1969–1976. doi: 10.1210/mend-3-12-1969. [DOI] [PubMed] [Google Scholar]
- 10.Coss D, Thackray VG, Deng CX, Mellon PL. Activin regulates luteinizing hormone β-subunit gene expression through smad-binding and homeobox elements. Mol Endocrinol. 2005;19:2610–2623. doi: 10.1210/me.2005-0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Attardi B, Miklos J. Rapid stimulatory effect of activin-A on messenger RNA encoding the follicle-stimulating hormone β-subunit in rat pituitary cell cultures. Mol Endocrinol. 1990;4:721–726. doi: 10.1210/mend-4-5-721. [DOI] [PubMed] [Google Scholar]
- 12.Blumenfeld Z, Ritter M. Inhibin, activin, and follistatin in human fetal pituitary and gonadal physiology. Ann NY Acad Sci. 2001;943:34–48. doi: 10.1111/j.1749-6632.2001.tb03788.x. [DOI] [PubMed] [Google Scholar]
- 13.Pernasetti F, Vasilyev VV, Rosenberg SB, Bailey JS, Huang H-J, Miller WL, Mellon PL. Cell-specific transcriptional regulation of FSHβ by activin and GnRH in the LβT2 pituitary gonadotrope cell model. Endocrinology. 2001;142:2284–2295. doi: 10.1210/endo.142.6.8185. [DOI] [PubMed] [Google Scholar]
- 14.Yamada Y, Yamamoto H, Yonehara T, Kanasaki H, Nakanishi H, Miyamoto E, Miyazaki K. Differential activation of the luteinizing hormone β-subunit promoter by activin and gonadotropin-releasing hormone: a role for the mitogen-activated protein kinase signaling pathway in LβT2 gonadotrophs. Biol Reprod. 2004;70:236–243. doi: 10.1095/biolreprod.103.019588. [DOI] [PubMed] [Google Scholar]
- 15.Burger LL, Haisenleder DJ, Dalkin AC, Marshall JC. Regulation of gonadotropin subunit gene transcription. J Mol Endocrinol. 2004;33:559–584. doi: 10.1677/jme.1.01600. [DOI] [PubMed] [Google Scholar]
- 16.Mangelsdorf DJ, Thummel C, Beato M, Herrlich P, Schutz G, Umesono K, Blumberg B, Kastner P, Mark M, Chambon P, Evans RM. The nuclear receptor superfamily: the second decade. Cell. 1995;83:835–839. doi: 10.1016/0092-8674(95)90199-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thornton JW. Evolution of vertebrate steroid receptors from an ancestral estrogen receptor by ligand exploitation and serial genome expansions. Proc Natl Acad Sci USA. 2001;98:5671–5676. doi: 10.1073/pnas.091553298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ham J, Thomson A, Needham M, Webb P, Parker M. Characterization of response elements for androgens, glucocorticoids and progestins in mouse mammary tumour virus. Nucleic Acids Res. 1988;16:5263–5276. doi: 10.1093/nar/16.12.5263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beato M. Gene regulation by steroid hormones. Cell. 1989;56:335–344. doi: 10.1016/0092-8674(89)90237-7. [DOI] [PubMed] [Google Scholar]
- 20.Tsai MJ, O’Malley BW. Molecular mechanisms of action of steroid/thyroid receptor superfamily members. Annu Rev Biochem. 1994;63:451–486. doi: 10.1146/annurev.bi.63.070194.002315. [DOI] [PubMed] [Google Scholar]
- 21.Heck S, Kullmann M, Gast A, Ponta H, Rahmsdorf HJ, Herrlich P, Cato AC. A distinct modulating domain in glucocorticoid receptor monomers in the repression of activity of the transcription factor AP-1. EMBO J. 1994;13:4087–4095. doi: 10.1002/j.1460-2075.1994.tb06726.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reichardt HM, Kaestner KH, Tuckermann J, Kretz O, Wessely O, Bock R, Gass P, Schmid W, Herrlich P, Angel P, Schutz G. DNA binding of the glucocorticoid receptor is not essential for survival. Cell. 1998;93:531–541. doi: 10.1016/s0092-8674(00)81183-6. [DOI] [PubMed] [Google Scholar]
- 23.Kallio PJ, Poukka H, Moilanen A, Janne OA, Palvimo JJ. Androgen receptor-mediated transcriptional regulation in the absence of direct interaction with a specific DNA element. Mol Endocrinol. 1995;9:1017–1028. doi: 10.1210/mend.9.8.7476976. [DOI] [PubMed] [Google Scholar]
- 24.Paul SJ, Ortolano GA, Haisenleder DJ, Stewart JM, Shupnik MA, Marshall JC. Gonadotropin subunit messenger RNA concentrations after blockade of gonadotropin-releasing hormone action: testosterone selectively increases follicle-stimulating hormone β-subunit messenger RNA by posttranscriptional mechanisms. Mol Endocrinol. 1990;4:1943–1955. doi: 10.1210/mend-4-12-1943. [DOI] [PubMed] [Google Scholar]
- 25.Dalkin AC, Paul SJ, Haisenleder DJ, Ortolano GA, Yasin M, Marshall JC. Gonadal steroids effect similar regulation of gonadotrophin subunit mRNA expression in both male and female rats. J Endocrinol. 1992;132:39–45. doi: 10.1677/joe.0.1320039. [DOI] [PubMed] [Google Scholar]
- 26.Wierman ME, Wang C. Androgen selectively stimulates follicle-stimulating hormone-β mRNA levels after gonadotropin-releasing hormone antagonist administration. Biol Reprod. 1990;42:563–571. doi: 10.1095/biolreprod42.3.563. [DOI] [PubMed] [Google Scholar]
- 27.Burger LL, Haisenleder DJ, Aylor KW, Dalkin AC, Prendergast KA, Marshall JC. Regulation of luteinizing hormone-β and follicle-stimulating hormone (FSH)-β gene transcription by androgens: testosterone directly stimulates FSH-β transcription independent from its role on follistatin gene expression. Endocrinology. 2004;145:71–78. doi: 10.1210/en.2003-1047. [DOI] [PubMed] [Google Scholar]
- 28.Gharib SD, Leung PC, Carroll RS, Chin WW. Androgens positively regulate follicle-stimulating hormone β-subunit mRNA levels in rat pituitary cells. Mol Endocrinol. 1990;4:1620–1626. doi: 10.1210/mend-4-11-1620. [DOI] [PubMed] [Google Scholar]
- 29.Winters SJ, Ishizaka K, Kitahara S, Troen P, Attardi B. Effects of testosterone on gonadotropin subunit messenger ribonucleic acids in the presence or absence of gonadotropin-releasing hormone. Endocrinology. 1992;130:726–734. doi: 10.1210/endo.130.2.1370794. [DOI] [PubMed] [Google Scholar]
- 30.Leal AM, Blount AL, Donaldson CJ, Bilezikjian LM, Vale WW. Regulation of follicle-stimulating hormone secretion by the interactions of activin-A, dexamethasone and testosterone in anterior pituitary cell cultures of male rats. Neuroendocrinology. 2003;77:298–304. doi: 10.1159/000070896. [DOI] [PubMed] [Google Scholar]
- 31.Jorgensen JS, Nilson JH. AR suppresses transcription of the LHβ subunit by interacting with steroidogenic factor-1. Mol Endocrinol. 2001;15:1505–1516. doi: 10.1210/mend.15.9.0691. [DOI] [PubMed] [Google Scholar]
- 32.Curtin D, Jenkins S, Farmer N, Anderson AC, Haisenleder DJ, Rissman E, Wilson EM, Shupnik MA. Androgen suppression of GnRH-stimulated rat LHβ gene transcription occurs through Sp1 sites in the distal GnRH-responsive promoter region. Mol Endocrinol. 2001;15:1906–1917. doi: 10.1210/mend.15.11.0723. [DOI] [PubMed] [Google Scholar]
- 33.Attardi B, Fitzgerald T. Effects of progesterone on the estradiol-induced follicle-stimulating hormone (FSH) surge and FSH β messenger ribonucleic acid in the rat. Endocrinology. 1990;126:2281–2287. doi: 10.1210/endo-126-5-2281. [DOI] [PubMed] [Google Scholar]
- 34.Kerrigan JR, Dalkin AC, Haisenleder DJ, Yasin M, Marshall JC. Failure of gonadotropin-releasing hormone (GnRH) pulses to increase luteinizing hormone β messenger ribonucleic acid in GnRH-deficient female rats. Endocrinology. 1993;133:2071–2079. doi: 10.1210/endo.133.5.8404655. [DOI] [PubMed] [Google Scholar]
- 35.Ringstrom SJ, Szabo M, Kilen SM, Saberi S, Knox KL, Schwartz NB. The antiprogestins RU486 and ZK98299 affect follicle-stimulating hormone secretion differentially on estrus, but not on proestrus. Endocrinology. 1997;138:2286–2290. doi: 10.1210/endo.138.6.5161. [DOI] [PubMed] [Google Scholar]
- 36.Knox KL, Schwartz NB. RU486 blocks the secondary surge of follicle-stimulating hormone in the rat without blocking the drop in serum inhibin. Biol Reprod. 1992;46:220–225. doi: 10.1095/biolreprod46.2.220. [DOI] [PubMed] [Google Scholar]
- 37.Szabo M, Kilen SM, Saberi S, Ringstrom SJ, Schwartz NB. Antiprogestins suppress basal and activin-stimulated follicle-stimulating hormone secretion in an estrogen-dependent manner. Endocrinology. 1998;139:2223–2228. doi: 10.1210/endo.139.5.6015. [DOI] [PubMed] [Google Scholar]
- 38.Webster JC, Pedersen NR, Edwards DP, Beck CA, Miller WL. The 5′-flanking region of the ovine follicle-stimulating hormone-β gene contains six progesterone response elements: three proximal elements are sufficient to increase transcription in the presence of progesterone. Endocrinology. 1995;136:1049–1058. doi: 10.1210/endo.136.3.7867558. [DOI] [PubMed] [Google Scholar]
- 39.O’Conner JL, Wade MF, Prendergast P, Edwards DP, Boonyaratanakornkit V, Mahesh VB. A 361 base pair region of the rat FSH-β promoter contains multiple progesterone receptor-binding sequences and confers progesterone responsiveness. Mol Cell Endocrinol. 1997;136:67–78. doi: 10.1016/s0303-7207(97)00216-5. [DOI] [PubMed] [Google Scholar]
- 40.Park D, Cheon M, Kim C, Kim K, Ryu K. Progesterone together with estradiol promotes luteinizing hormone β-subunit mRNA stability in rat pituitary cells cultured in vitro. Eur J Endocrinol. 1996;134:236–242. doi: 10.1530/eje.0.1340236. [DOI] [PubMed] [Google Scholar]
- 41.Ringstrom SJ, McAndrews JM, Rahal JO, Schwartz NB. Cortisol in vivo increases FSH β mRNA selectively in pituitaries of male rats. Endocrinology. 1991;129:2793–2795. doi: 10.1210/endo-129-5-2793. [DOI] [PubMed] [Google Scholar]
- 42.McAndrews JM, Ringstrom SJ, Dahl KD, Schwartz NB. Corticosterone in vivo increases pituitary follicle-stimulating hormone (FSH)-β messenger ribonucleic acid content and serum FSH bioactivity selectively in female rats. Endocrinology. 1994;134:158–163. doi: 10.1210/endo.134.1.8275929. [DOI] [PubMed] [Google Scholar]
- 43.Kilen SM, Szabo M, Strasser GA, McAndrews JM, Ringstrom SJ, Schwartz NB. Corticosterone selectively increases follicle-stimulating hormone β-subunit messenger ribonucleic acid in primary anterior pituitary cell culture without affecting its half-life. Endocrinology. 1996;137:3802–3807. doi: 10.1210/endo.137.9.8756550. [DOI] [PubMed] [Google Scholar]
- 44.Bohnsack BL, Szabo M, Kilen SM, Tam DH, Schwartz NB. Follistatin suppresses steroid-enhanced follicle-stimulating hormone release in vitro in rats. Biol Reprod. 2000;62:636–641. doi: 10.1095/biolreprod62.3.636. [DOI] [PubMed] [Google Scholar]
- 45.Rosen H, Dalkin A, Haisenleder D, Friberg RD, Ortolano G, Barkan A Dexamethasone alters responses of pituitary gonadotropin-releasing hormone (GnRH) receptors, gonadotropin subunit messenger ribonucleic acids, and gonadotropins to pulsatile GnRH in male rats. Endocrinology. 1991;128:654–660. doi: 10.1210/endo-128-2-654. [DOI] [PubMed] [Google Scholar]
- 46.Ibrahim SN, Moussa SM, Childs GV. Morphometric studies of rat anterior pituitary cells after gonadectomy: correlation of changes in gonadotropes with the serum levels of gonadotropins. Endocrinology. 1986;119:629–637. doi: 10.1210/endo-119-2-629. [DOI] [PubMed] [Google Scholar]
- 47.Stefaneanu L. Pituitary sex steroid receptors: localization and function. Endocr Pathol. 1997;8:91–108. doi: 10.1007/BF02739938. [DOI] [PubMed] [Google Scholar]
- 48.Pelletier G, Labrie C, Labrie F. Localization of oestrogen receptor α, oestrogen receptor β and androgen receptors in the rat reproductive organs. J Endocrinol. 2000;165:359–370. doi: 10.1677/joe.0.1650359. [DOI] [PubMed] [Google Scholar]
- 49.Turgeon JL, Waring DW. Progesterone regulation of the progesterone receptor in rat gonadotropes. Endocrinology. 2000;141:3422–3429. doi: 10.1210/endo.141.9.7688. [DOI] [PubMed] [Google Scholar]
- 50.Ozawa H, Ito T, Ochiai I, Kawata M. Cellular localization and distribution of glucocorticoid receptor immunoreactivity and the expression of glucocorticoid receptor messenger RNA in rat pituitary gland. A combined double immunohistochemistry study and in situ hybridization histochemical analysis. Cell Tissue Res. 1999;295:207–214. doi: 10.1007/s004410051226. [DOI] [PubMed] [Google Scholar]
- 51.Graham KE, Nusser KD, Low MJ. LβT2 gonadotroph cells secrete follicle stimulating hormone (FSH) in response to activin A. J Endocrinol. 1999;162:R1–R5. doi: 10.1677/joe.0.162r001. [DOI] [PubMed] [Google Scholar]
- 52.Lewis KA, Gray PC, Blount AL, MacConell LA, Wiater E, Bilezikjian LM, Vale W. Betaglycan binds inhibin and can mediate functional antagonism of activin signalling. Nature. 2000;404:411–414. doi: 10.1038/35006129. [DOI] [PubMed] [Google Scholar]
- 53.Schreihofer DA, Stoler MH, Shupnik MA. Differential expression and regulation of estrogen receptors (ERs) in rat pituitary and cell lines: estrogen decreases ERα protein and estrogen responsiveness. Endocrinology. 2000;141:2174–2184. doi: 10.1210/endo.141.6.7505. [DOI] [PubMed] [Google Scholar]
- 54.Lawson MA, Li D, Glidewell-Kenney CA, Lopez FJ. Androgen responsiveness of the pituitary gonadotrope cell line LβT2. J Endocrinol. 2001;170:601–607. doi: 10.1677/joe.0.1700601. [DOI] [PubMed] [Google Scholar]
- 55.Spady TJ, Shayya R, Thackray VG, Ehrensberger L, Bailey JS, Mellon PL. Androgen regulates FSHβ gene expression in an activin-dependent manner in immortalized gonadotropes. Mol Endocrinol. 2004;18:925–940. doi: 10.1210/me.2003-0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Okada Y, Fujii Y, Moore JP, Jr, Winters SJ. Androgen receptors in gonadotrophs in pituitary cultures from adult male monkeys and rats. Endocrinology. 2003;144:267–273. doi: 10.1210/en.2002-220770. [DOI] [PubMed] [Google Scholar]
- 57.Fox SR, Harlan RE, Shivers BD, Pfaff DW. Chemical characterization of neuroendocrine targets for progesterone in the female rat brain and pituitary. Neuroendocrinology. 1990;51:276–283. doi: 10.1159/000125350. [DOI] [PubMed] [Google Scholar]
- 58.Turgeon JL, Van Patten SM, Shyamala G, Waring DW. Steroid regulation of progesterone receptor expression in cultured rat gonadotropes. Endocrinology. 1999;140:2318–2325. doi: 10.1210/endo.140.5.6709. [DOI] [PubMed] [Google Scholar]
- 59.Kononen J, Honkaniemi J, Gustafsson JA, Pelto-Huikko M. Glucocorticoid receptor colocalization with pituitary hormones in the rat pituitary gland. Mol Cell Endocrinol. 1993;93:97–103. doi: 10.1016/0303-7207(93)90144-9. [DOI] [PubMed] [Google Scholar]
- 60.Shupnik MA, Gharib SD, Chin WW. Divergent effects of estradiol on gonadotropin gene transcription in pituitary fragments. Mol Endocrinol. 1989;3:474–480. doi: 10.1210/mend-3-3-474. [DOI] [PubMed] [Google Scholar]
- 61.Shupnik MA, Fallest PC. Pulsatile GnRH regulation of gonadotropin subunit gene transcription. Neurosci Biobehav Rev. 1994;18:597–599. doi: 10.1016/0149-7634(94)90017-5. [DOI] [PubMed] [Google Scholar]
- 62.Ikonen T, Palvimo JJ, Janne OA. Heterodimerization is mainly responsible for the dominant negative activity of amino-terminally truncated rat androgen receptor forms. FEBS Lett. 1998;430:393–396. doi: 10.1016/s0014-5793(98)00701-7. [DOI] [PubMed] [Google Scholar]
- 63.Takimoto GS, Tasset DM, Eppert AC, Horwitz KB. Hormone-induced progesterone receptor phosphorylation consists of sequential DNA-independent and DNA-dependent stages: analysis with zinc finger mutants and the progesterone antagonist ZK98299. Proc Natl Acad Sci USA. 1992;89:3050–3054. doi: 10.1073/pnas.89.7.3050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rogers SL, Nabozny G, McFarland M, Pantages-Torok L, Archer J, Kalkbrenner F, Zuvela-Jelaska L, Haynes N, Jiang H. Four mutations in the GR dimerization domain result in perinatal lethal mice; Keystone Symposia Nuclear Receptors; Keystone, CO: Steroid Sisters; 2004. [Google Scholar]
- 65.Hagino N, Watanabe M, Goldzieher JW. Inhibition by adrenocorticotrophin of gonadotrophin-induced ovulation in immature female rats. Endocrinology. 1969;84:308–314. doi: 10.1210/endo-84-2-308. [DOI] [PubMed] [Google Scholar]
- 66.Smith ER, Johnson J, Weick RF, Levine S, Davidson JM. Inhibition of the reproductive system in immature rats by intracerebral implantation of cortisol. Neuroendocrinology. 1971;8:94–106. doi: 10.1159/000121997. [DOI] [PubMed] [Google Scholar]
- 67.Rivier C, Rivier J, Vale W. Stress-induced inhibition of reproductive functions: role of endogenous corticotropin-releasing factor. Science. 1986;231:607–609. doi: 10.1126/science.3003907. [DOI] [PubMed] [Google Scholar]
- 68.Dubey AK, Plant TM. A suppression of gonadotropin secretion by cortisol in castrated male rhesus monkeys (Macaca mulatta) mediated by the interruption of hypothalamic gonadotropin-releasing hormone release. Biol Reprod. 1985;33:423–431. doi: 10.1095/biolreprod33.2.423. [DOI] [PubMed] [Google Scholar]
- 69.Ringstrom SJ, Schwartz NB. Cortisol suppresses the LH, but not the FSH, response to gonadotropin-releasing hormone after orchidectomy. Endocrinology. 1985;116:472–474. doi: 10.1210/endo-116-1-472. [DOI] [PubMed] [Google Scholar]
- 70.Ringstrom SJ, Suter DE, Hostetler JP, Schwartz NB. Cortisol regulates secretion and pituitary content of the two gonadotropins differentially in female rats: effects of gonadotropin-releasing hormone antagonist. Endocrinology. 1992;130:3122–3128. doi: 10.1210/endo.130.6.1597133. [DOI] [PubMed] [Google Scholar]
- 71.Buckingham JC, Dohler KD, Wilson CA. Activity of the pituitary-adrenocortical system and thyroid gland during the oestrous cycle of the rat. J Endocrinol. 1978;78:359–366. doi: 10.1677/joe.0.0780359. [DOI] [PubMed] [Google Scholar]
- 72.Nichols DJ, Chevins PF. Plasma corticosterone fluctuations during the oestrous cycle of the house mouse. Experientia. 1981;37:319–320. doi: 10.1007/BF01991678. [DOI] [PubMed] [Google Scholar]
- 73.Ortolano GA, Haisenleder DJ, Dalkin AC, Iliff-Sizemore SA, Landefeld TD, Maurer RA, Marshall JC. Follicle-stimulating hormone β subunit messenger ribonucleic acid concentrations during the rat estrous cycle. Endocrinology. 1988;123:2946–2948. doi: 10.1210/endo-123-6-2946. [DOI] [PubMed] [Google Scholar]
- 74.Tebar M, Uilenbroek JT, Kramer P, van Schaik RH, Wierikx CD, Ruiz A, de Jong FH, Sanchez-Criado JE. Effects of progesterone on the secondary surge of follicle-stimulating hormone in the rat. Biol Reprod. 1997;57:77–84. doi: 10.1095/biolreprod57.1.77. [DOI] [PubMed] [Google Scholar]
- 75.Kaiser UB, Conn PM, Chin WW. Studies of gonadotropin-releasing hormone (GnRH) action using GnRH receptor-expressing pituitary cell lines. Endocr Rev. 1997;18:46–70. doi: 10.1210/edrv.18.1.0289. [DOI] [PubMed] [Google Scholar]
- 76.Weiss J, Crowley WF, Jr, Halvorson LM, Jameson JL. Perifusion of rat pituitary cells with gonadotropin-releasing hormone, activin, and inhibin reveals distinct effects on gonadotropin gene expression and secretion. Endocrinology. 1993;132:2307–2311. doi: 10.1210/endo.132.6.8504735. [DOI] [PubMed] [Google Scholar]
- 77.Jorgensen JS, Quirk CC, Nilson JH. Multiple and overlapping combinatorial codes orchestrate hormonal responsiveness and dictate cell-specific expression of the genes encoding luteinizing hormone. Endocr Rev. 2004;25:521–542. doi: 10.1210/er.2003-0029. [DOI] [PubMed] [Google Scholar]
- 78.Zmeili SM, Papavasiliou SS, Thorner MO, Evans WS, Marshall JC, Landefeld TD. α and Luteinizing hormone β subunit messenger ribonucleic acids during the rat estrous cycle. Endocrinology. 1986;119:1867–1869. doi: 10.1210/endo-119-4-1867. [DOI] [PubMed] [Google Scholar]
- 79.Tebar M, de Jong FH, Sanchez-Criado JE. Regulation of inhibin/activin subunits and follistatin mRNA expression in the rat pituitary at early estrus. Life Sci. 2000;67:2549–2562. doi: 10.1016/s0024-3205(00)00839-0. [DOI] [PubMed] [Google Scholar]
- 80.Bedecarrats GY, Kaiser UB. Differential regulation of gonadotropin subunit gene promoter activity by pulsatile gonadotropin-releasing hormone (GnRH) in perifused L β T2 cells: role of GnRH receptor concentration. Endocrinology. 2003;144:1802–1811. doi: 10.1210/en.2002-221140. [DOI] [PubMed] [Google Scholar]
- 81.Verrijdt G, Haelens A, Claessens F. Selective DNA recognition by the androgen receptor as a mechanism for hormone-specific regulation of gene expression. Mol Genet Metab. 2003;78:175–185. doi: 10.1016/s1096-7192(03)00003-9. [DOI] [PubMed] [Google Scholar]
- 82.Geserick C, Meyer HA, Haendler B. The role of DNA response elements as allosteric modulators of steroid receptor function. Mol Cell Endocrinol. 2005;236:1–7. doi: 10.1016/j.mce.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 83.Tilbrook AJ, Turner AI, Clarke IJ. Stress and reproduction: central mechanisms and sex differences in non-rodent species. Stress. 2002;5:83–100. doi: 10.1080/10253890290027912. [DOI] [PubMed] [Google Scholar]
- 84.Majumdar SS, Mikuma N, Ishwad PC, Winters SJ, Attardi BJ, Perera AD, Plant TM. Replacement with recombinant human inhibin immediately after orchidectomy in the hypophysiotropically clamped male rhesus monkey (Macaca mulatta) maintains follicle-stimulating hormone (FSH) secretion and FSH β messenger ribonucleic acid levels at precastration values. Endocrinology. 1995;136:1969–1977. doi: 10.1210/endo.136.5.7720645. [DOI] [PubMed] [Google Scholar]
- 85.Kumar TR, Huntress VF, Low MJ. Gonadotrope-specific expression of the human follicle-stimulating hormone β-subunit gene in pituitaries of transgenic mice. Mol Endocrinol. 1992;6:81–90. doi: 10.1210/mend.6.1.1738375. [DOI] [PubMed] [Google Scholar]
- 86.Phillips CL, Lin LW, Wu JC, Guzman K, Milsted A, Miller WL. 17 β-estradiol and progesterone inhibit transcription of the genes encoding the subunits of ovine follicle-stimulating hormone. Mol Endocrinol. 1988;2:641–649. doi: 10.1210/mend-2-7-641. [DOI] [PubMed] [Google Scholar]
- 87.Turzillo AM, DiGregorio GB, Nett TM. Messenger ribonucleic acid for gonadotropin-releasing hormone receptor and numbers of gonadotropin-releasing hormone receptors in ovariectomized ewes after hypothalamic-pituitary disconnection and treatment with estradiol. J Anim Sci. 1995;73:1784–1788. doi: 10.2527/1995.7361784x. [DOI] [PubMed] [Google Scholar]
- 88.Huang HJ, Sebastian J, Strahl BD, Wu JC, Miller WL. The promoter for the ovine follicle-stimulating hormone-β gene (FSHβ) confers FSHβ-like expression on luciferase in transgenic mice: regulatory studies in vivo and in vitro. Endocrinology. 2001;142:2260–2266. doi: 10.1210/endo.142.6.8202. [DOI] [PubMed] [Google Scholar]
- 89.Kawakami S, Fujii Y, Okada Y, Winters SJ. Paracrine regulation of FSH by follistatin in folliculostellate cell-enriched primate pituitary cell cultures. Endocrinology. 2002;143:2250–2258. doi: 10.1210/endo.143.6.8857. [DOI] [PubMed] [Google Scholar]
- 90.Jacobs SBR, Coss D, McGillivray SM, Mellon PL. Nuclear factor-Y and steroidogenic factor-1 physically and functionally interact to contribute to cell-specific expression of the mouse follicle-stimulating hormone-β gene. Mol Endocrinol. 2003;17:1470–1483. doi: 10.1210/me.2002-0286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Resnick EM, Schreihofer DA, Periasamy A, Shupnik MA. Truncated estrogen receptor product-1 suppresses estrogen receptor transactivation by dimerization with estrogen receptors α and β. J Biol Chem. 2000;275:7158–7166. doi: 10.1074/jbc.275.10.7158. [DOI] [PubMed] [Google Scholar]
- 92.Liao M, Zhou Z, Wilson EM. Redox-dependent DNA binding of the purified androgen receptor: evidence for disulfide-linked androgen receptor dimers. Biochemistry. 1999;38:9718–9727. doi: 10.1021/bi990589i. [DOI] [PubMed] [Google Scholar]
- 93.Thackray VG, Toft DO, Nordeen SK. Novel activation step required for transcriptional competence of progesterone receptor on chromatin templates. Mol Endocrinol. 2003;17:2543–2553. doi: 10.1210/me.2003-0200. [DOI] [PubMed] [Google Scholar]
- 94.Rosenberg SB, Mellon PL. An Otx-related homeodomain protein binds an LHβ promoter element important for activation during gonadotrope maturation. Mol Endocrinol. 2002;16:1280–1298. doi: 10.1210/mend.16.6.0841. [DOI] [PMC free article] [PubMed] [Google Scholar]