Abstract
Objective
With liberal use of computed tomography in the diagnostic management of trauma patients, incidental findings (IFs) are common and represent a major patient care and medical-legal concern. Consequently, we began an initiative to adequately capture, notify, and document IF events with a dedicated incidental finding (DIF) coordinator. We hypothesized a DIF coordinator would increase IF capture and promote notification, follow-up and documentation of IF events.
Methods
A quality improvement project to record and follow-up IFs post-injury was initiated at our level I trauma center (4/07-3/08, PRE-DIF). Due to concerns for inadequate documentation of identified IF events we implemented a DIF coordinator (4/08-3/09, POST-DIF). The DIF coordinator documented IFs daily from trauma admission radiology final reads. IFs were divided into 3 groups, Cat 1: attention prior to discharge, Cat 2: follow-up with primary doctor within 2 weeks, Cat 3: no specific follow-up. For Cat 1 IFs, in-hospital consultation of the appropriate service was verified. Upon discharge, patient notification, follow-up and documentation of events were confirmed. Certified mail or telephone contact was used to notify either the patient or primary doctor in those who lacked appropriate notification or documentation.
Results
Admission rates and IF Categories were similar across the two time periods. Implementation of a DIF coordinator resulted in over a 165% increase in IF capture (n=802 vs. n=302, p< 0.001). Patient notification was attempted and appropriate documentation of events was confirmed in 99.8% of patients. Patient notification was verified and follow-up was initiated in 95.8% of cases.
Conclusion
Implementation of a DIF coordinator resulted in over a 2.5-fold higher capture of IFs. Dedicated attention to IFs resulted in near complete initiation of patient notification, follow-up, and hospital record documentation of IF events. Inadequate patient notification and follow-up would delay appropriate care and potentially result in morbidity or even mortality. A dedicated incidental finding coordinator represents a potential solution to this patient care and medical-legal dilemma.
Introduction
Computed tomography (CT) imaging has become extremely common for the evaluation and characterization of injuries in the hemodynamically stable trauma patient.1-4 Recent evidence suggests whole-body CT or the ‘pan-CT’ is associated with a survival benefit and has been recommended as the standard diagnostic method during the early resuscitation phase for the injured patient with polytrauma.5 Incidental radiographic findings, those findings which are found on imaging studies performed for unrelated indications, have been shown to be relatively common throughout all of medicine as the sensitivity and quality of our radiographic techniques, particularly computerized tomography (CT) and magnetic resonance imaging (MRI), continues to improve.6-15 With the increasing liberal utilization of whole-body imaging in the management of the acutely injured patient, an increased frequency of these radiographic incidental findings (IFs) have been reported.16, 17 Clinically significant or serious IFs have been shown to be relatively common with increasing frequency in females and the elderly, while IF management has been touted as a significant challenge for busy trauma centers with medical-legal implications.18 The majority of the literature on this matter has revealed poor rates of patient notification, inadequate documentation of IF events that occur during a patient's hospital stay, and insufficient follow-up and treatment plans for those patients with clinically significant IFs.16, 18, 19
Although multiple analyses have documented that IFs and their management remain a patient care conundrum, few have provided any insight into a systematic approach or management solution that could address these potentially serious patient care and medical-legal issues. The main objective of this current analysis was to characterize the significance of dedicated attention to this IF problem by implementation of a dedicated incidental finding (DIF) coordinator at a busy, level I, trauma center. We hypothesized that committed attention to IFs via a dedicated coordinator would improve IF capture, improve notification and documentation of hospital IF events and promote appropriate follow-up arrangements either while the patient is admitted or following discharge.
Methods
A prospective analysis was performed using data derived from a quality improvement (QI) initiative at the University of Pittsburgh Medical Center, a busy level I trauma center with over 4,800 admission/year. The QI project occurred over a two year period (4/07- 3/09) and was initiated to characterize the incidence of IFs, patient notification rates, their subsequent management, and the appropriateness of follow-up and hospital documentation of IF related events. After a 12-month period of data collection (4/07-3/08, PRE-DIF), a concern arose for incomplete capture and inadequate patient notification and hospital record documentation of such events. During this initial time period, IF management was the responsibility of the resident house staff and rounding attendings on a daily basis which lacked consistency. IF capture (PRE-DIF) and documentation and notification rates for this initial period were determined by resident and attending communication. It was realized that a more aggressive and complete surveillance approach to this potential medical-legal problem was needed. On 4/08 we implemented a DIF coordinator as an integral part of our trauma program. Over the next 12 months (4/08-3/09, POST-DIF) The DIF coordinator identified IFs daily from final radiographic reads from the preceding 24 hour cohort of trauma admissions. Weekend and holiday admission IFs were documented on the subsequent Monday or next weekday, respectively. IFs were classified and divided into 3 categories based upon medical significance. Category 1: IF required attention prior to hospital discharge; Category 2: IF required follow-up with a patients primary medical doctor within two weeks following discharge; Category 3: IF required no follow-up, as described previously.18 For all Category 1 IFs, the DIF coordinator verified and assisted in coordinating the appropriate consult team needed during the trauma admission. Resident house-staff remained responsible for creation of a preformed electronic IF note which documented all in-house IF events. Following discharge, the hospital records of those patients with IFs (Category 2 and 3) were assessed for patient notification, recommended follow-up, and documentation of these events. For those patients where appropriate notification and documentation of IF management was lacking, certified mail or telephone contact was used to notify either the patient, the patient's family, a legal guardian or custodian, or the primary care physician followed by appropriate documentation of the communication. A copy of the radiographic IF along with follow-up recommendations was sent to each correspondent.
For the analysis, trauma admission demographics and injury characteristics over the two time periods (4/07-3/08, PRE-DIF) and (4/08-3/09, POST-DIF) were compared via univariate analysis. IF identification and capture and IF categories (Category 1,2 or 3 IFs) across the two time periods were then similarly compared. For the POST-DIF period, notification rates and method of notification were characterized. Data are summarized as mean ± SD, median [interquartile range], or percentage (%). Student-t or Mann-Whitney statistical tests were used to compare continuous variables, while Chi-Square or Fischer's Exact test were used for categorical variables. Statistical analyses were performed using SPSS 17 (SPSS, Chicago, IL).
Results
Over the two 12 month time periods (PRE-DIF, POST-DIF) trauma admission rates remained essentially unchanged with 4,810 admissions in the PRE-DIF period and 4,875 admission in the POST_DIF time period. There were no significant differences in age, gender, mechanism of injury (blunt or penetrating) or injury severity for trauma admissions across the two time periods. There was a significant difference across GCS scores for admissions over the two time periods, however these differences were clinically insignificant. (Table 1.) As female gender and, more importantly, older patients have been shown to be associated with a higher rate of IFs18, we further categorized the age of admissions for the two time periods to rule out any differences across age strata. This revealed no differences in age strata for the two time periods. (Table 2.)
Table 1. Group comparison for the PRE-DIF and POST-DIF time periods.
| PRE-DIF (n=4,810) |
POST-DIF (n=4,875) |
p-value | |
|---|---|---|---|
| Age (years) | 38.1±17 | 37.6±16 | 0.522 |
| Gender (%male) | 24.5% | 22.4% | 0.351 |
| Presenting GCS | 13.7±3 | 13.9±3 | 0.017 |
| Mechanism of Injury (Blunt%) | 91.6% | 91.8% | 0.390 |
| Injury Severity Score (ISS) | 28.2±14 | 28.1±15 | 0.893 |
Table 2. Age distribution comparison for the PRE-DIF and POST-DIF time periods.
| AGE: p = 0.377 | PRE-DIF (n=4,810) |
POST-DIF (n=4,875) |
|---|---|---|
| Less than 40 years (%) | 43.6% | 42.4% |
| 41-50 years (%) | 16.3% | 15.5% |
| 51-60 years (%) | 13.6% | 14.1% |
| 61-70 years (%) | 8.3% | 8.6% |
| 71-80 years (%) | 8.0% | 8.1% |
| > 80 years | 10.2% | 11.3% |
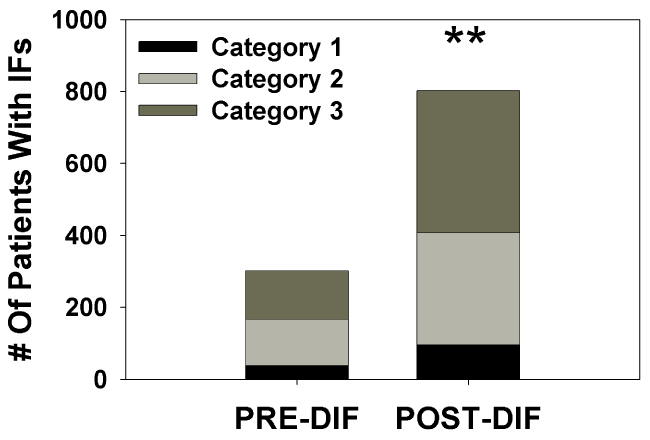
When the capture of IFs for the two time periods was compared, over a 165% higher capture of IFs was found following employment of a DIF coordinator (PRE-DIF: n=302; POST-DIF n=802; p < 0.001, Figure 1.). Importantly, there was no significant difference found for IF categories (category 1,2 or 3) across the two time periods (Table 3.). Patient notification was attempted and appropriate documentation of IF management was confirmed in 99.8% of patients in the POST-DIF time period. (Table 4.) For all Category 1 IFs (n=96) in the POST-DIF period, patient notification was verified, documented, and initiation of follow-up was verified during the hospital admission. There were 2 patients (0.2%) for whom no addresses, primary care physicians, or family members (or power of attorney) were able to be contacted by phone or registered mail. There were 32 patients (4.0%) with addresses or primary care physician contacts that were available but patients or physicians either refused to sign or accept the registered letter, phone service was disconnected or the addresses available were incorrect. The registered letters were returned and filed and phone contact attempts were documented in all 32 patients. Importantly, these 34 patients (4.2%) without verifiable patient notification all had IFs in Category 2 and 3. Of the 95.8% (n=768) of patients with verified patient notification in the POST-DIF period, 42.1% were notified with appropriate documentation while in the hospital prior to discharge, with Category 1 IFs having consultations initiated. In over 52% of cases, a registered letter to the patient, or post discharge contact with the family or primary physician was the main method of IF patient notification or method of documentation of such events. There was a 2.4% mortality rate in this IF cohort where no documentation was verified or required.
Figure 1. Incidental finding capture across comparison time periods, stratified by Category type. ** = statistically significant as compared to the PRE-DIF time period.
Table 3. Comparison of IF categories across time periods.
| IF Categories: p = 0.479 | PRE-DIF (n=302) | POST-DIF (n=802) |
|---|---|---|
| Category 1 | 12.9% | 12.0% |
| Category 2 | 42.1% | 38.9% |
| Category 3 | 45.0% | 49.1% |
Table 4. Distribution of notification attempt method for POST-DIF patients.
| POST-DIF period (n=802) | N (%) |
|---|---|
| Patient notification unable to be documented or verified | 2 (0.2%) |
| Patient notification event documented via return of registered letter but not verified | 32 (4.0%) |
| Inpatient notification of IF and/or Inpatient Consultation | 338 (42.1%) |
| Registered letter to patient accepted | 384 (47.9%) |
| Letter/fax to primary care physician accepted | 24 (3.0%) |
| Letter to family accepted | 3 (0.4%) |
| Patient Expired (no IF notification required) | 19 (2.4%) |
Discussion
As the use of whole-body CT imaging for the diagnostic management of the acutely injured patient continues to increase, if not already the ‘gold standard’ in the hemodynamically stable patient, IFs will continue to pose a significant challenge for all trauma centers.5, 18 Appropriate patient notification and initiation of follow-up for even serious findings, including suspected malignancies and aortic aneurysms have been historically poor.18, 19 Importantly, IFs have been shown to be significantly more common in patients older than 40 years of age.18 As the average age of U.S. population continues to increase, (www.asaging.org/nchs) and a corresponding increase in the average age of the injured patient occurs, IFs will become even more common and a greater patient care and medical-legal dilemma. The results of the current prospective analysis, characterizing a quality improvement initiative with the aim to provide focused attention to IFs by incorporation of a dedicated incidental finding coordinator into the trauma service, provides a potential organized approach or management pathway that can help address these difficult incidental radiographic issues. Dedicated attention to IFs in an injured cohort resulted in over a 165% increase in IF identification and capture. For all potentially serious IFs, (Category 1) in hospital patient notification and consultation was initiated and verified with the assistance of a DIF coordinator. Following initiation of the DIF coordinator, 95.8% of patients with IFs were notified of their radiographic abnormalities, with appropriate initiation of follow-up, all with adequate documentation of such events.
The magnitude of improved capture by dedicated attention to IFs was both unexpected and surprising. In the PRE-DIF time period, IFs were addressed as they were found on rounds when final radiographic reads were completed with reliance on house staff and rounding attendings to notify the patients and arrange or plan for appropriate follow-up. IF management was characterized and tallied based upon these actions. Although this may have been performed adequately, without a consistent provider or coordinator focusing on this problem, IFs were likely being missed. If not as equally important, documentation of IF events that occurred in the hospital were inadequate with potential medical-legal implications for those patients where in hospital notification or documentation was lacking. This analysis suggests that without dedicated attention as occurred in the POST-DIF period, many IFs may be going unrecognized or inadequately addressed with the potential for delay in appropriate care and subsequent morbidity or even mortality. Similarly, without dedicated IF attention, documentation of notification and follow-up arrangements may be inadequate, even if IF events were appropriately performed and arranged.
Prior literature regarding the management of IFs have looked at the use of midlevel providers to perform tertiary trauma surveys once admitted and to notify those patients at that time prior to discharge with appropriate follow-up plans.20 Although this prior study was descriptive in nature with no comparison group or method of verifying their IF capture completeness, their conclusions are similar to the conclusions of this current analysis. A dedicated IF management scheme with continuity over time can result in appropriate IF capture, notification, follow-up planning and documentation of such events, with a minimization of legal risks inherent to these type of radiographic findings following injury.
Although there was an overall 95.8% rate of patient notification with initiation of follow-up and with proper documentation, despite dedicated attention, only 42% of patients were appropriately notified while in the hospital or had adequate documentation of any in-hospital events. All Category 1 IFs had verified in-hospital follow-up arranged, however, over 52% of patients with IFs lacked appropriate documentation of notification and planned follow-up, if needed, and required registered letters or phone notification post-discharge. Currently in our trauma program the residents or rounding attendings remain responsible for notification of IFs and documentation of such events using an electronic IF note. The DIF coordinator participates with Category 1 IFs and verifies in-house consultation has been arranged, however, significant room for improvement for those Category 2 and 3 IFs still exists, with the most common insufficiency being IF documentation. With increasing patient volumes and workloads and resident work hour restrictions, it may be that additional management pathways and practices that go beyond or above standard patient care may require dedicated attention by midlevel providers who offer continuity and familiarity to such practices.
This analysis does have several limitations that deserve discussion. First, this study was performed at a single, busy, level I trauma center and may not be generalizable or pertinent to other centers with differing admission demographics or injury characteristics. IF categories (1,2 and 3) were based upon prior literature classification18, however, some judgment was required mostly between categories 2 and 3 depending on a patient's known pre-existing chronic disease versus a previously unknown condition or finding. It is interesting that the distribution of Category 1, Category 2 and Category 3 IFs in this analysis was similar to prior analyses.16, 18, 19 Although Category 3 IFs were considered not to require any medical follow-up and included findings such as renal cysts, small hiatal hernias or benign anatomical variants, it was felt that patient notification was still necessary for both patient care and medical-legal concerns. An important limitation of the conclusions formulated from this analysis is based upon the fact that IF capture and management from the PRE-DIF period was based upon resident house staff and attending documentation and no retrospective review of all PRE-DIF trauma admissions was performed to document and verify IFs that were actually missed. An assumption is required when the two time periods are actually compared due to this limitation, however, this assumption is minimized by the similarity of trauma admissions and demographics across the two time periods. Follow-up for Category 1 IFs was verified during a patient's admission, however, no follow-up of outpatient care or further evaluation for Category 1 IFs was performed. Similarly, only initiation of follow-up via verbal recommendation to the patient or by registered letter occurred for Category 2 and 3 IFs. No investigation into the subsequent care which was performed or arranged by the primary care physician, if any, was carried out. These represent significant limitations to the current analysis, but would likely represent a logistically difficult requirement for any busy trauma center. Finally, the above limitations of this quality improvement initiative do not allow documentation or quantification of any real health benefit or medical-legal risk reduction over the two time periods. Patient care and medical-legal benefits can only be inferred by proxy, secondary to improved IF capture, patient notification and appropriate document of such events.
In conclusion, IFs represent a significant challenge for trauma centers that will likely continue to increase in frequency. An organized, consistent approach is required to achieve adequate capture, notification, initiation of follow-up and documentation of such events. Implementation of a dedicated incidental finding coordinator was associated with a significant increase in IF capture and an acceptably high rate of patient notification, follow-up initiation and appropriate documentation of IF events. Dedicated attention with an organized, consistent approach is required for successful follow-up and management and represents a potential solution to this patient care and medical-legal problem following injury.
Acknowledgments
The project described was supported by Grant Number NIH KL2 RR024154-03 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research, and its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp
Footnotes
This paper was presented as an oral presentation at the annual meeting of the Central Surgical Association in Chicago, Illinois, Mar 10-Mar 13, 2010.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Bibliography
- 1.Deunk J, Brink M, Dekker HM, et al. Routine versus selective multidetector-row computed tomography (MDCT) in blunt trauma patients: level of agreement on the influence of additional findings on management. J Trauma. 2009 Nov;67(5):1080–1086. doi: 10.1097/TA.0b013e318189371d. [DOI] [PubMed] [Google Scholar]
- 2.Deunk J, Brink M, Dekker HM, et al. Routine versus selective computed tomography of the abdomen, pelvis, and lumbar spine in blunt trauma: a prospective evaluation. J Trauma. 2009 Apr;66(4):1108–1117. doi: 10.1097/TA.0b013e31817e55c3. [DOI] [PubMed] [Google Scholar]
- 3.Ramirez RM, Cureton EL, Ereso AQ, et al. Single-contrast computed tomography for the triage of patients with penetrating torso trauma. J Trauma. 2009 Sep;67(3):583–588. doi: 10.1097/TA.0b013e3181a39330. [DOI] [PubMed] [Google Scholar]
- 4.Tillou A, Gupta M, Baraff LJ, et al. Is the use of pan-computed tomography for blunt trauma justified? A prospective evaluation. J Trauma. 2009 Oct;67(4):779–787. doi: 10.1097/TA.0b013e3181b5f2eb. [DOI] [PubMed] [Google Scholar]
- 5.Huber-Wagner S, Lefering R, Qvick LM, et al. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet. 2009 Apr 25;373(9673):1455–1461. doi: 10.1016/S0140-6736(09)60232-4. [DOI] [PubMed] [Google Scholar]
- 6.Horton KM, Post WS, Blumenthal RS, Fishman EK. Prevalence of significant noncardiac findings on electron-beam computed tomography coronary artery calcium screening examinations. Circulation. 2002 Jul 30;106(5):532–534. doi: 10.1161/01.cir.0000027136.56615.de. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs PC, Mali WP, Grobbee DE, van der Graaf Y. Prevalence of incidental findings in computed tomographic screening of the chest: a systematic review. J Comput Assist Tomogr. 2008 Mar-Apr;32(2):214–221. doi: 10.1097/RCT.0b013e3181585ff2. [DOI] [PubMed] [Google Scholar]
- 8.Machaalany J, Yam Y, Ruddy TD, et al. Potential clinical and economic consequences of noncardiac incidental findings on cardiac computed tomography. J Am Coll Cardiol. 2009 Oct 13;54(16):1533–1541. doi: 10.1016/j.jacc.2009.06.026. [DOI] [PubMed] [Google Scholar]
- 9.Molitch ME. Pituitary tumours: pituitary incidentalomas. Best Pract Res Clin Endocrinol Metab. 2009 Oct;23(5):667–675. doi: 10.1016/j.beem.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 10.Singh PK, Buch HN. Adrenal incidentaloma: evaluation and management. J Clin Pathol. 2008 Nov;61(11):1168–1173. doi: 10.1136/jcp.2006.044313. [DOI] [PubMed] [Google Scholar]
- 11.Illes J, Kirschen MP, Edwards E, et al. Ethics. Incidental findings in brain imaging research. Science. 2006 Feb 10;311(5762):783–784. doi: 10.1126/science.1124665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vernooij MW, Ikram MA, Tanghe HL, et al. Incidental findings on brain MRI in the general population. N Engl J Med. 2007 Nov 1;357(18):1821–1828. doi: 10.1056/NEJMoa070972. [DOI] [PubMed] [Google Scholar]
- 13.Awad IA, Spetzler RF, Hodak JA, Awad CA, Carey R. Incidental subcortical lesions identified on magnetic resonance imaging in the elderly. I. Correlation with age and cerebrovascular risk factors. Stroke. 1986 Nov-Dec;17(6):1084–1089. doi: 10.1161/01.str.17.6.1084. [DOI] [PubMed] [Google Scholar]
- 14.Messersmith WA, Brown DF, Barry MJ. The prevalence and implications of incidental findings on ED abdominal CT scans. Am J Emerg Med. 2001 Oct;19(6):479–481. doi: 10.1053/ajem.2001.27137. [DOI] [PubMed] [Google Scholar]
- 15.Richman PB, Courtney DM, Friese J, et al. Prevalence and significance of nonthromboembolic findings on chest computed tomography angiography performed to rule out pulmonary embolism: a multicenter study of 1,025 emergency department patients. Acad Emerg Med. 2004 Jun;11(6):642–647. [PubMed] [Google Scholar]
- 16.Barrett TW, Schierling M, Zhou C, et al. Prevalence of incidental findings in trauma patients detected by computed tomography imaging. Am J Emerg Med. 2009 May;27(4):428–435. doi: 10.1016/j.ajem.2008.03.025. [DOI] [PubMed] [Google Scholar]
- 17.Eskandary H, Sabba M, Khajehpour F, Eskandari M. Incidental findings in brain computed tomography scans of 3000 head trauma patients. Surg Neurol. 2005 Jun;63(6):550–553. doi: 10.1016/j.surneu.2004.07.049. discussion 553. [DOI] [PubMed] [Google Scholar]
- 18.Paluska TR, Sise MJ, Sack DI, Sise CB, Egan MC, Biondi M. Incidental CT findings in trauma patients: incidence and implications for care of the injured. J Trauma. 2007 Jan;62(1):157–161. doi: 10.1097/01.ta.0000249129.63550.cc. [DOI] [PubMed] [Google Scholar]
- 19.Munk MD, Peitzman AB, Hostler DP, Wolfson AB. Frequency and follow-up of incidental findings on trauma computed tomography scans: Experience at a level one trauma center. J Emerg Med. 2008 sep 18; doi: 10.1016/j.jemermed.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 20.Huynh TT, Moran KR, Blackburn AH, Jacobs DG, Thomason MH, Sing RF. Optimal management strategy for incidental findings in trauma patients: an initiative for midlevel providers. J Trauma. 2008 Aug;65(2):331–334. doi: 10.1097/TA.0b013e31817e5153. discussion 335-336. [DOI] [PubMed] [Google Scholar]