Abstract
Spontaneous intracranial epidural hematoma (EDH) due to dural metastasis of hepatocellular carcinoma is very rare. A 53-year-old male patient with hepatocellular carcinoma, who was admitted to the department of oncology, was referred to department of neurosurgery because of sudden mental deterioration to semicoma with papillary anisocoria and decerebrate rigidity after transarterial chemoembolization for hepatoma. Brain computed tomography (CT) revealed large amount of acute EDH with severe midline shifting. An emergent craniotomy and evacuation of EDH was performed. Active bleeding from middle cranial fossa floor was identified. There showed osteolytic change on the middle fossa floor with friable mass-like lesion spreading on the overlying dura suggesting metastasis. Pathological examination revealed anaplastic cells with sinusoidal arrangement which probably led to spontaneous hemorrhage and formation of EDH. As a rare cause of spontaneous EDH, dural metastasis from malignancy should be considered.
Keywords: Spontaneous epidural hematoma, Hepatocellular carcinoma, Dural metastasis
INTRODUCTION
Intracranial epidural hematoma (EDH) is usually a consequence of head injury. But, spontaneous intracranial EDHs can occur in patients with paracranial infections, bleeding or coagulation disorders, vascular malformation, and neoplastic condition7-9,11,18,19,21,27). Spontaneous intracranial EDH originating from a metastatic hepatocellular carcinoma is very rare. To the authors' knowledge, only 6 cases have been reported in the literature5,10,12,15-17). We describe a case of spontaneous intracranial acute EDH originating from a metastatic hepatocellular carcinoma of the skull and dura mater in the middle cranial fossa.
CASE REPORT
A 53-year-old male patient with hepatocellular carcinoma, who was admitted to the department of oncology, was referred to department of neurosurgery because of sudden mental deterioration to semicoma with papillary anisocoria and decerebrate rigidity after transarterial chemoembolization for hepatoma. Brain computed tomography (CT) revealed large amount of acute EDH with severe midline shifting (Fig. 1). He had no history of trauma and coagulopathy even though he had slightly prolonged prothrombin time (INR 1.36). An emergent craniotomy and evacuation of EDH was performed. There was no evidence of trauma on the scalp, subgaleal space and skull bone. Thick hematoma was seen on the epidural space, mostly on the temporal base displacing the brain. There showed an osteolytic change on the middle cranial fossa floor (Fig. 2). Active bleeding from the middle meningeal artery and osteolytic bone on the middle cranial fossa floor was controlled with bipolar cautery and application of bone wax. Curettage of friable mass-like lesions on the overlying dura and skull was performed, which suggested metastasis to the dura and skull. Pathological examination revealed anaplastic cells with sinusoidal arrangement which probably led to spontaneous hemorrhage and formation of EDH (Fig. 3). Despite of the rapid evacuation of EDH, he is in vegetative state after surgery.
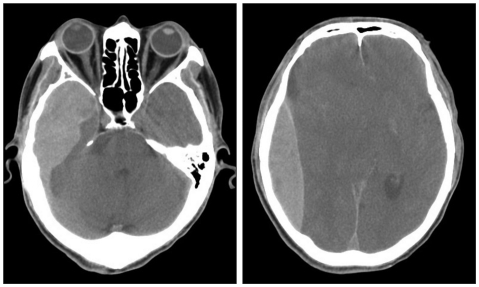
Fig. 1.
Brain CT scans showing a huge epidural hematoma from the right temporal base to the cerebral convexity with severe mass effect.
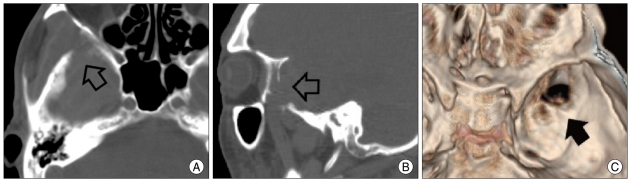
Fig. 2.
Brain CT scans showing osteolytic bone lesion on the middle cranial fossa floor. Axial (A) and sagittal (B) views of bone window level show eroded right temporal base (open arrows). Bony defect (black arrow) is well visualized on CT window image (C).
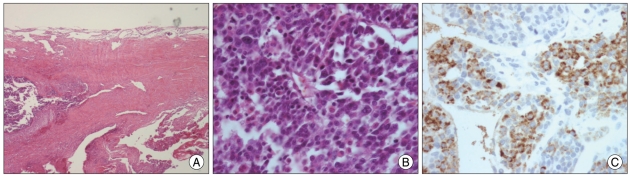
Fig. 3.
Photomicrographs obtained from the thickened dura matter showing metastatic hepatocellular carcinoma. A : Sinusoidal pattern of anaplastic cells is demonstrated in dural layer (H & E, ×100). B : Sinusoidal blood vessels (H & E, ×400). C : Hepatocyte antibody immunostain showing metastatic poorly differentiated hepatocyte with mitosis.
DISCUSSION
EDH is usually a consequence of head injury. In-bending of skull at the time of traumatic impact on the head makes the skull fracture, which can cause epidural bleeding from lacerated meningeal vessels, fractured edges, torn venous sinuses or diploic veins. But, spontaneous or non-traumatic intracranial EDHs are very rare. Main possible causes of this unusual phenomenon are infection from frontal sinusitis, maxillary sinusitis, otitis media and craniofacial infections, and coagulation disorders, vascular malformation of dura, and malignancy7-9,11,18,19,21,27).
Intracranial hemorrhage from distant metastasis of primary cancer is rare and its incidence accounts for 0.9-11%25). The location is usually intratumoral or intracerebral, and very rarely epidural. Spontaneous EDHs resulting from dural metastasis of primary malignancy have been reported only 16 cases9), which include lung cancer20,22,24), hepatocellular carcinoma5,10,12,15-17), ovarian cancer1), eosinophilic granuloma4,14), Ewing's sarcoma2,26), malignant fibrous histiocytoma13), and Langerhans' cell histiocytosis3). Spontaneous EDH due to dural metastasis of hepatocellular carcinoma is very rare and to the authors' knowledge, it has been reported only 6 cases in the literature5,10,12,15-17). It has been well known that hepatocellular carcinoma has a characteristic of high risk of bleeding tendency due to hepatic failure and formation of neoangiogenesis6). It usually spreads to regional lymph nodes around the porta hepatis via lymphatics, but it can also spread hematogenously via intrahepatic vein, portal vein, and hepatic artery. It commonly metastasizes to the lung, regional lymph nodes, peritoneum, and adrenal glands, but, rarely spread to the brain. Secondary intracranial hepatic carcinomas were 1.3-2.9% among intracranial metastatic tumors23). In most cases of spontaneous EDH of hepatocellular carcinoma, bleeding arise from middle meningeal artery, emissary vein, and venous sinus with regional bone invasion. Histological feature shows many sinusoid-like blood vessels. In our case, the bleeding had arisen from the eroded middle meningeal artery and osteolytic bone. Spontaneous EDHs of hepatocellular carcinoma may be spread via hematogenous route, but it is uncertain. Although dura acts as a barrier of tumor invasion, hepatocellular carcinoma has a high potency of dural invasion and destruction of neighboring bone.
To elucidate the cause of spontaneous EDH, it is necessary to examine the paranasal sinus and ear to rule out infection, chest X-ray for lung mass, abdominal sonography or CT scan for hepatocellular carcinoma, laboratory finding for coagulopathy and image studies for vascular abnormality9). In particular, the patient with hepatocellular carcinoma and lung metastasis should be evaluated for brain metastasis because intracranial metastasis of hepatocellular carcinoma often combined lung metastasis12). In addition, biopsy of dura mater and skull are needed during the operation.
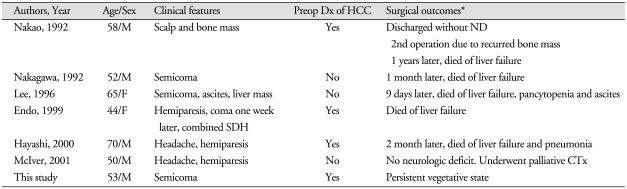
Clinical outcomes of spontaneous EDH with hepatocellular carcinoma were usually poor (Table 1). All of these patients (reported 6 and ours 1) underwent surgery. Five were dead because of liver failure, ascites, coagulopathy and pneumonia, one became vegetative state, and one survived. These poor outcomes might be caused by its own poor prognosis of terminal stage hepatocellular carcinoma, combined coagulopathy and liver failure, and high mortality rate of EDH.
Table 1.
Summary of patients in the literature who were diagnosed as spontaneous epidural hematoma from hepatocellular carcinoma metastasis
*All patients underwent surgery. CTx : chemotherapy, Dx : diagnosis, F : female, HCC : hepatocellular carcinoma, M : male, ND : neurologic deficit, Preop : preoperative, SDH : subdural hematoma
CONCLUSION
The authors report a rare case of spontaneous intracranial EDH originating from a metastatic hepatocellular carcinoma of the skull and dura mater on the middle cranial fossa. In patients who have spontaneous EDH, metastatic hepatocellular carcinoma should be included in the differential diagnosis as a rare cause of spontaneous EDH.
References
- 1.Anegawa S, Hirohata S, Tokutomi T, Kuramoto S. Spontaneous epidural hematoma secondary to dural metastasis from an ovarian carcinoma--case report. Neurol Med Chir (Tokyo) 1989;29:854–856. doi: 10.2176/nmc.29.854. [DOI] [PubMed] [Google Scholar]
- 2.Aslam E, Imran M, Faridi NM. Bilateral parietal extradural metastatic Ewing's sarcoma simulating acute epidural hematoma. J Coll Physicians Surg Pak. 2006;16:543–544. [PubMed] [Google Scholar]
- 3.Chen HC, Shen WC, Chou DY, Chiang IP. Langerhans cell histiocytosis of the skull complicated with an epidural hematoma. AJNR Am J Neuroradiol. 2002;23:493–495. [PMC free article] [PubMed] [Google Scholar]
- 4.Cho DY, Liau WR, Chiang IP. Eosinophilic granuloma with acute epidural hematoma : a case report. Pediatr Neurosurg. 2001;35:266–269. doi: 10.1159/000050434. [DOI] [PubMed] [Google Scholar]
- 5.Endo M, Hamano M, Watanabe K, Wakai S. [Combined chronic subdural and acute epidural hematoma secondary to metastatic hepatocellular cancer : case report.] No Shinkei Geka. 1999;27:331–334. [PubMed] [Google Scholar]
- 6.Friedman HD. Hepatocellular carcinoma with central nervous system metastasis : a case report and literature review. Med Pediatr Oncol. 1991;19:139–144. doi: 10.1002/mpo.2950190215. [DOI] [PubMed] [Google Scholar]
- 7.Gordon AG. Extradural hematoma and homolateral otitis media. J Neurosurg. 1978;49:942–943. doi: 10.3171/jns.1978.49.6.0942a. [DOI] [PubMed] [Google Scholar]
- 8.Griffiths SJ, Jatavallabhula NS, Mitchell RD. Spontaneous extradural haematoma associated with craniofacial infections: case report and review of the literature. Br J Neurosurg. 2002;16:188–191. doi: 10.1080/026886902317384553. [DOI] [PubMed] [Google Scholar]
- 9.Hassan MF, Dhamija B, Palmer JD, Hilton D, Adams W. Spontaneous cranial extradural hematoma : case report and review of literature. Neuropathology. 2009;29:480–484. doi: 10.1111/j.1440-1789.2008.00977.x. [DOI] [PubMed] [Google Scholar]
- 10.Hayashi K, Matsuo T, Kurihara M, Daikoku M, Kitange G, Shibata S. Skull metastasis of hepatocellular carcinoma associated with acute epidural hematoma : a case report. Surg Neurol. 2000;53:379–382. doi: 10.1016/s0090-3019(00)00208-1. [DOI] [PubMed] [Google Scholar]
- 11.Kelly DL, Jr, Smith JM. Epidural hematoma secondary to frontal sinusitis. Case report. J Neurosurg. 1968;28:67–69. doi: 10.3171/jns.1968.28.1.0067. [DOI] [PubMed] [Google Scholar]
- 12.Lee KW, Chung DS, Huh PW, Hong YK, Rha HK, Kang JK. Intracranial metastasis of hepatocellular carcinoma associated with epidural hematoma : a case report. J Korean Neurosurg Soc. 1996;25:1738–1742. [Google Scholar]
- 13.Leung G, Yip P, Fan YW. Spontaneous epidural haematoma associated with radiation-induced malignant fibrous histiocytoma. J R Coll Surg Edinb. 1999;44:404–406. [PubMed] [Google Scholar]
- 14.Martínez-Lage JF, Bermüdez M, Martínez-Barba E, Fuster JL, Poza M. Epidural hematoma from a cranial eosinophilic granuloma. Childs Nerv Syst. 2002;18:74–76. doi: 10.1007/s003810100491. [DOI] [PubMed] [Google Scholar]
- 15.McIver JI, Scheithauer BW, Rydberg CH, Atkinson JL. Metastatic hepatocellular carcinoma presenting as epidural hematoma : case report. Neurosurgery. 2001;49:447–449. doi: 10.1097/00006123-200108000-00034. [DOI] [PubMed] [Google Scholar]
- 16.Nakagawa Y, Yoshino E, Suzuki K, Tatebe A, Andachi H. Spontaneous epidural hematoma from a hepatocellular carcinoma metastasis to the skull--case report. Neurol Med Chir (Tokyo) 1992;32:300–302. doi: 10.2176/nmc.32.300. [DOI] [PubMed] [Google Scholar]
- 17.Nakao N, Kubo K, Moriwaki H. Cranial metastasis of hepatocellular carcinoma associated with chronic epidural hematoma--case report. Neurol Med Chir (Tokyo) 1992;32:100–103. doi: 10.2176/nmc.32.100. [DOI] [PubMed] [Google Scholar]
- 18.Ng WH, Yeo TT, Seow WT. Non-traumatic spontaneous acute epidural haematoma--report of two cases and review of the literature. J Clin Neurosci. 2004;11:791–793. doi: 10.1016/j.jocn.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Sanchis JF, Orozco M, Cabanes J. Spontaneous extradural haematomas. J Neurol Neurosurg Psychiatry. 1975;38:577–580. doi: 10.1136/jnnp.38.6.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sato N, Tsurushima H, Matsumura A, Meguro K, Doi M. [A case of epidural hematoma due to dural metastasis.] No Shinkei Geka. 1991;19:447–450. [PubMed] [Google Scholar]
- 21.Sekimoto T, Nakagawa Y, Ueda S, Hirakawa K, Fukuma S, Taketomo S. [Spontaneous epidural hematoma--report of two cases.] No Shinkei Geka. 1985;13:1253–1257. [PubMed] [Google Scholar]
- 22.Shamim MS, Bari ME, Enam SA. Dural metastases presenting as an extradural hematoma : a rare presentation. J Pak Med Assoc. 2005;55:509–510. [PubMed] [Google Scholar]
- 23.Shuangshoti S, Rungruxsirivorn S, Panyathanya R. Intracranial metastasis of hepatic carcinomas : a study of 9 cases within 28 years. J Med Assoc Thai. 1989;72:307–313. [PubMed] [Google Scholar]
- 24.Simmons NE, Elias WJ, Henson SL, Laws ER. Small cell lung carcinoma causing epidural hematoma : case report. Surg Neurol. 1999;51:56–59. doi: 10.1016/s0090-3019(97)00450-3. [DOI] [PubMed] [Google Scholar]
- 25.Wakai S, Yamakawa K, Manaka S, Takakura K. Spontaneous intracranial hemorrhage caused by brain tumor : its incidence and clinical significance. Neurosurgery. 1982;10:437–444. doi: 10.1227/00006123-198204000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Yamashita Y, Kumabe T, Kobayashi T, Abiko H, Seki H, Yoshimoto T. [Ewing's sarcoma at the occipital bone presenting as acute epidural hematoma: a case report.] No Shinkei Geka. 1997;25:567–571. [PubMed] [Google Scholar]
- 27.Zheng FX, Chao Y. Spontaneous intracranial extradural hematoma : case report and literature review. Neurol India. 2009;57:324–326. doi: 10.4103/0028-3886.53288. [DOI] [PubMed] [Google Scholar]