Abstract
The expression of 5 markers associated with angiogenesis, proliferation, and apoptosis was studied in 26 canine simple mammary gland adenocarcinomas (SMGAs). The adenocarcinomas were graded histologically, and tissue sections were immunohistochemically stained for the expression of vascular endothelial growth factor (VEGF), VEGF receptor-2 (VEGFR-2), intra-tumor microvessel density, and tumor proliferation (PI) using antibodies against VEGF, VEGFR-2, von Willebrand factor, and Ki-67 antigen, respectively. Apoptotic indices (AI) were determined by an apoptosis assay. Markers VEGF and VEGFR-2 were detected in 96% and 100% of SMGAs, respectively. A high correlation between histologic grade and PI (r = 0.73), a moderate correlation between VEGF and histologic grade (r = 0.33), and between VEGF and PI (r = 0.42) were found. There was a significant difference in median PI among the 3 histologic grade groups (r < 0.05). Vascular endothelial growth factor may stimulate tumor cell proliferation through an autocrine loop, since VEGF and VEGFR-2 were expressed in most tumors.
Résumé
Expression immunohistochimique du récepteur-2 du facteur de croissance vasculaire endothélial dans les adénocarcinomes simples des glandes mammaires canines. L’expression des 5 marqueurs associés à l’angiogénèse, à la prolifération et à l’apoptose a été étudiée dans 26 adénocarcinomes simples des glandes mammaires canines (ASGM). Les adénocarcinomes ont été catégorisés par histologie et les sections des tissus ont été colorées par immunohistochimie pour l’expression du facteur de croissance endothélial vasculaire (FCEV), du récepteur-2 de FCEV (FCEV-2), de la densité des micro-vaisseaux dans la tumeur et de la prolifération de la tumeur en utilisant des anticorps contre FCEV, FCEV-2, le facteur von Willebrand et l’antigène Ki-67, respectivement. Des indices d’apoptose (IA) ont été déterminés à l’aide d’un essai d’apoptose. Des marqueurs FCEV et FCEV-2 ont été détectés dans 96 % et 100 % des ASGM, respectivement. Un haut niveau de corrélation entre le grade histologique et la prolifération de la tumeur (r = 0,73), une corrélation modérée entre le FCEV et le grade histologique (r = 0,33) et entre le FCEV et la prolifération de la tumeur (r = 0,42) ont été constatés. Il y avait une différence considérable entre la prolifération médiane parmi les 3 groupes de grades histologiques (r < 0,05). Le facteur de croissance endothélial vasculaire peut stimuler la prolifération des cellules des tumeurs par une boucle autocrine, vu que le FCEV et le FCEV-2 étaient exprimés dans la plupart des tumeurs.
(Traduit par Isabelle Vallières)
Introduction
The formation of new microvasculature in a process known as angiogenesis is critical for the growth and metastasis of malignant tumors (1). Vascular endothelial growth factor (VEGF) is a protein that plays a key role in tumor angiogenesis (2). Two VEGF receptors are present on endothelial cells, VEGF Receptor-1 (VEGFR-1) and VEGF-2 (VEGFR-2) (3). Both receptors bind to VEGF with high affinity (4,5); however, only VEGFR-2 is capable of mediating angiogenesis (6). Receptor VEGFR-1 is thought to play a regulatory role by decreasing the availability of VEGF to VEGFR-2 (6,7). Vascular endothelial growth factor and VEGFR-2 are associated with tumor cell proliferation (8–10). The simultaneous expression of both molecules on tumor cells may indicate that VEGF has an autocrine function, stimulating tumor cell growth (11); it may also decrease tumor apoptosis (12). In many human malignant tumors the increased expression of VEGF has been correlated with the histologic grade of malignancy (13–15). Moreover, the relationship between the degree of angiogenesis, often expressed as intra-tumor microvessel density (iMVD), and many parameters including tumor proliferation index (PI), an expression of tumor cell proliferation, and tumor apoptotic index (AI), an expression of tumor cell death by apoptosis, have been extensively studied in human cancer (8,10,16,17,18–24).
Mammary tumors comprise 52% of all neoplasms affecting female dogs (25), of which, 41% to 53% are malignant (26). Based on their histologic features, canine mammary tumors can be classified into several types including simple carcinoma, complex carcinoma, and carcinoma arising in a benign tumor (27).
In the veterinary literature, VEGF, VEGFR-2, iMVD, and PI have been evaluated in few canine tumors (16,28–35). However, the relationship between these parameters in canine mammary neoplasia is still unclear, and studying this relationship may aid in understanding their role in the progression of mammary neoplasia in dogs.
We previously evaluated the expression of these markers in canine cutaneous squamous cell carcinomas, trichoepitheliomas (16), and fibrosarcomas (36). The purpose of this study was to evaluate the expression of these markers in canine simple mammary gland adenocarcinomas.
Materials and methods
Tissue selection and histologic grading
Histologic sections previously diagnosed as canine simple mammary gland adenocarcinoma (SMGA), and submitted between 2002 to 2004 to the Prairie Diagnostic Services at the Western College of Veterinary Medicine, Saskatoon, Saskatchewan were evaluated independently by 2 of the authors (ANA and BAK). Twenty-six cases receiving consensus diagnosis were selected and each given a histologic grade from 1 to 3 based on the degree of tubular formation, the presence of mitotic figures, and nuclear pleomorphism according to established criteria (27). Histologic grading was performed independently by the same authors and tumors receiving different histologic grades were reevaluated and a consensus was established.
Immunohistochemical staining for VEGF, VEGFR-2, vWf, and Ki-67
An avidin-biotin-complex (ABC) immunohistochemical staining method was used on formalin-fixed paraffin-embedded tissues (37). Consecutive 5-μm tissue sections were cut from each paraffin block, and then mounted and dried on glass slides. Tissues were deparaffinized in Citrosolv (Fisher Scientific, Ottawa, Ontario), then dehydrated in graded alcohol solutions. Endogenous peroxidase activity was blocked with 3% hydrogen peroxide in absolute methanol for 12 min at room temperature. Antigen was retrieved by steaming the tissues in a vegetable steamer for 30 min using 0.01 M sodium citrate solution at pH 6.8. Non-specific protein binding was saturated using 4% horse serum (Invitrogen, Burlington, Ontario) in phosphate buffered saline (PBS) (Invitrogen) for 20 min at 42°C, except when staining for von Willebrand factor where 4% goat serum was used. Primary antibodies consisted of: monoclonal mouse anti-human VEGF121 isoform, 1/20 (NeoMarkers, Fremont, California, USA); monoclonal mouse anti-human VEGFR-2, 1/1000 (Santa Cruz Biotechnology, Santa Cruz, California, USA); polyclonal rabbit anti-human vWF, 1/2000 (Dakocytomation, Mississauga, Ontario); and prediluted monoclonal mouse anti-human Ki-67 (Zymed Laboratories, San Francisco, California, USA). The diluted primary antibodies were applied to tissue sections, and the slides incubated 14 to 18 h at 4°C. A biotinylated polyclonal secondary horse anti-mouse antiserum (Vector Laboratories, Burlington, Ontario) was applied to tissues for VEGF, VEGFR-2, and Ki-67 staining at a dilution of 1/400 for 20 min at 42°C. A 1/400 dilution of biotinylated polyclonal sheep anti-rabbit secondary antiserum was used to stain tissues for vWf. Reagent (ABC) was prepared according to the manufacturer’s directions (Vecastain Elite ABC kit; Vector Laboratories) and applied for 35 min at 42°C. Color development was achieved by applying a 3-3′-diaminobenzine-tetrahydrochloride (DAB) reagent (Sigma, Oakville, Ontario) for 5 min. Tissues were counterstained with hematoxylin (Sigma), rehydrated in graded alcohol, and mounted with coverslips.
When staining tissues for VEGF and VEGFR-2, serial sections of tissues were also stained with omission of the primary antibody and with an isotype matched irrelevant antibody (Neo Markers). Tissue from a canine splenic hemangiosarcoma was used as a positive control for VEGF. Tissue from a canine squamous cell carcinoma, previously known to express VEGFR-2 (16), was used as a positive control for VEGFR-2. Tissue from a normal canine lymph node was used as a positive control for Ki-67. Normal vessels in the surrounding tissue of each tumor were used as a positive control for vWf. Five normal canine skin tissues containing mammary glands were also stained for VEGF, VEGFR-2, and vWf.
Terminal deoxynucleotidyl transferase-mediated 2-deoxyuridine 5-triphosphate end-labeling assay for apoptosis
Apoptosis was detected using the ApopTag Peroxidase In Situ detection kit (Chemicon International, Temecula, California, USA). Briefly, 5-μm tissue sections were deparaffinized and rehydrated as described. Protein was digested with 20 μg/mL proteinase K solution (Invitrogen/VWR, Saskatoon, Saskatchewan) for 15 min at room temperature. Endogenous peroxidase activity was blocked with 3.0% hydrogen peroxide. An equilibration buffer supplied with the kit was applied for 15 s, followed by working strength terminal deoxynucleotidyl transferase enzyme for 1 h at 37°C. The slides were covered with an anti-digoxigenin conjugate and incubated in a humidified chamber for 30 min at room temperature. Color development and counterstaining were as described for immunohistochemical stains. Tissue from a canine lymphosarcoma was used as positive control for the TUNEL assay.
Immunohistochemical scoring for VEGF and VEGFR-2
A score ranging from 0 to 2 was assigned to each tumor section. Tumors were given a score of 0 if there was no staining, a score of 1 if there was pale brown staining and a score of 2 if there was dark brown staining. All tumors were evaluated independently by 2 of the authors (ANA and BAK). In instances of discordant scores, a score was established by consensus.
Evaluation of microvessel density, Ki-67, and apoptosis
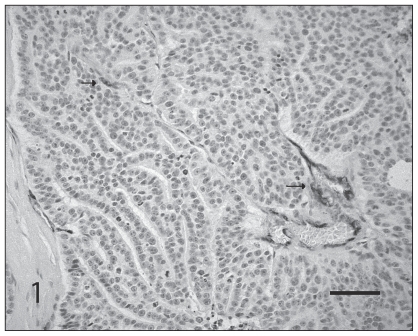
Intra-tumor microvessel density was evaluated with antibodies detecting vWf (Figure 1), using the “hot-spot method” (38). Slides were examined at low power (40×) to identify 10 areas with high vessel density followed by re-examination of each area at high-power (400×) and counting of all positively staining structures irrespective of whether or not a vessel lumen was identified. Continuous vessels were counted as one vessel. The average of the 10 fields was determined and was expressed as count per high-power field in each tumor.
Figure 1.
Immunohistochemical staining of endothelial cells for von Willebrand factor antigen in simple mammary gland adenocarcinoma. Note the density of labeled vessels (arrows). Avidin-Biotin-complex diaminobenzidine method, hematoxylin counterstain. Bar = 50 μm.
A similar method was used to evaluate sections stained with Ki-67 monoclonal antibody to demonstrate dividing tumor cells. The tissue sections were first examined at low power (40×) to identify 5 areas with high numbers of positive cells. Within each area, a high power field (400×) was selected and 200 cells were counted. A total of 1000 cells were counted in the 5 high power fields. The average number of the positive cells in the 5 fields represented the PI. The apoptotic index was similarly determined by counting 200 cells in 5 selected areas and averaging numbers of positive cells using the TUNEL assay in five 400× fields.
Statistical analysis
Statistical analysis was performed using Statistix 7 for Windows©2000 (Analytical Software, Tallahassee, Florida, USA). The strength of the association between the 6 variables evaluated (histologic grade, VEGF expression, VEGFR-2 expression, iMVD, PI, and AI) was assessed by Spearman Rank correlation coefficient. Correlation coefficients were interpreted as follows: r = 0, no correlation; 0 < r < 0.1, trivial correlation; 0.1 ≤ r < 0.3, slight correlation; 0.3 ≤ r < 0.5, moderate correlation; 0.5 ≤ r < 0.7, substantial or high correlation; and r ≥ 0.7 very high correlation (39).
The Kruskal-Wallis test was used to test for differences in the median iMVD, AI, and PI among the VEGF expression, VEGFR-2 expression, or histologic grade groups of SMGAs. This test was also used to evaluate the differences in VEGF or VEGFR-2 expression levels among the different histologic grades of SMGAs.
Results
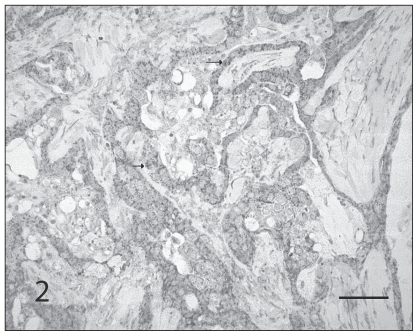
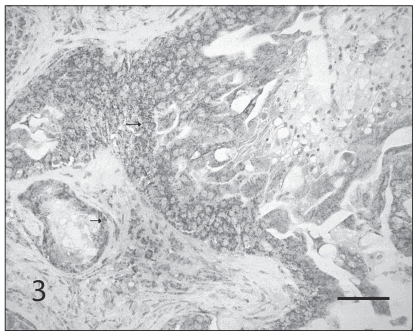
Of the 26 SMGAs, 11 (42.3%) were assigned a histologic grade of 1; 12 (46.2%), grade 2; and 3 (11.5%), grade 3. Vascular endothelial growth factor and VEGFR-2 antigens were detected in 96% and in 100% of the tumors, respectively (Figures 2 and 3). The results for each of the parameters evaluated are shown in Table 1. A high correlation between histologic grade and proliferation index (PI) (r = 0.73), a moderate correlation between VEGF expression and PI (r = 0.42), and a moderate correlation between VEGF and histologic grade (r = 0.33) were found (Spearman rank correlation test). Correlation coefficients between other variables were < 0.3.
Figure 2.
Immunohistochemical staining of tumor cells for VEGF antigen in simple mammary gland adenocarcinoma. Note the dark staining in the cytoplasm of tumor cells (arrows). Avidin-Biotin-complex diaminobenzidine method, hematoxylin counterstain. Bar = 50 μm.
Figure 3.
Immunohistochemical staining of tumor cells for VEGFR-2 antigen in simple mammary gland adenocarcinoma. Note the dark staining in the cytoplasm of tumor cells (arrows). Avidin-Biotin-complex diaminobenzidine method, hematoxylin counterstain. Bar = 50 μm.
Table 1.
Simple mammary gland adenocarcinoma VEGF, VEGFR-2, iMVD, PI, AI, and histological grade scoresa
| Tumor identification | Histologic grade | VEGF score | VEGFR-2 score | iMVD count (s)b | PI (s) | AI (s) |
|---|---|---|---|---|---|---|
| 1 | 1 | 1 | 1 | 19.9 (6.5) | 15 (4.6) | 2.8 (1.5) |
| 2 | 1 | 1 | 2 | 8.3 (2.3) | 3.8 (1.6) | 2.6 (1.1) |
| 3 | 1 | 2 | 1 | 12.2 (3.7) | 20.2 (3.7) | 17.2 (5.9) |
| 4 | 1 | 1 | 2 | 6.4 (2.8) | 5.8 (3.3) | 4 (1) |
| 5 | 1 | 1 | 1 | 11.9 (6.7) | 32.4 (6) | 10.2 (2.6) |
| 6 | 1 | 1 | 1 | 10 (7) | 13.4 (5.3) | 22.2 (5.8) |
| 7 | 1 | 1 | 2 | 6.8 (2.8) | 18.8 (5.3) | 7 (1.2) |
| 8 | 1 | 1 | 2 | 15.6 (3.7) | 26.6 (5.1) | 7.4 (2.1) |
| 9 | 1 | 1 | 2 | 12.1 (5.7) | 7 (2.9) | 0 (0) |
| 10 | 1 | 1 | 2 | 11.2 (6.1) | 42.8 (8.6) | 0 (0) |
| 11 | 1 | 2 | 2 | 17.2 (7.6) | 38 (9.7) | 0 (0) |
| 12 | 2 | 1 | 2 | 16.2 (6.4) | 44.4 (8.8) | 11.8 (2.6) |
| 13 | 2 | 1 | 2 | 12.2 (6.4) | 16 (5.8) | 11.2 (4.4) |
| 14 | 2 | 1 | 2 | 9 (2.7) | 42 (10.4) | 3.8 (0.8) |
| 15 | 2 | 2 | 2 | 16.3 (12.1) | 23.4 (4) | 23.6 (5.4) |
| 16 | 2 | 1 | 1 | 10.5 (4.7) | 41.8 (6.1) | 6.4 (3.5) |
| 17 | 2 | 2 | 1 | 4.7 (1.7) | 54.4 (2.7) | 8.6 (2.9) |
| 18 | 2 | 1 | 1 | 7.5 (3.1) | 42 (4.1) | 4.8 (1.5) |
| 19 | 2 | 2 | 2 | 13.8 (5.3) | 46.4 (4.3) | 11.6 (1.9) |
| 20 | 2 | 1 | 1 | 16.2 (5.4) | 58.4 (9.1) | 12.6 (3) |
| 21 | 2 | 2 | 2 | 13 (5.9) | 44.8 (5.5) | 5.2 (1.3) |
| 22 | 2 | 1 | 2 | 16.2 (4.3) | 25 (4.9) | 2 (0.7) |
| 23 | 2 | 2 | 2 | 9.4 (3.3) | 59.6 (8.5) | 3.6 (1.1) |
| 24 | 3 | 2 | 1 | 28.5 (6.5) | 47.2 (5.2) | 1.8 (0.8) |
| 25 | 3 | 1 | 1 | 11.9 (2.6) | 66.6 (10.1) | 10.2 (1.9) |
| 26 | 3 | 2 | 1 | 8.8 (3.7) | 49.2 (8.4) | 0 (0) |
AI — apoptotic index, PI — proliferation index, VEGF — vascular endothelial growth factor, VEGFR-2 — VEGF receptor-2, iMVD — intra-tumor microvessel density.
s — standard deviation.
There was a significant difference (P = 0.0013) in median PI among the different tumor histologic grades (Kruskal-Wallis test). The median PI increased as the histologic grade increased; however, the difference in median PI was statistically significant only when grade 3 or 2 tumors were compared to grade 1 tumors. The median PI of grade 3 tumors was higher than the median PI of grade 2 tumors but the difference was not significant (see Table 2 for details).
Table 2.
Comparison of median PI, AI, and iMVD between the 3 histological grade groups in canine SMGAa
| Histologic grade | ||||
|---|---|---|---|---|
| Parameter | I | II | III | P-value |
| Median PI | 18.8 | 43.2 | 49.2 | 0.0013b |
| Median AI | 4.0 | 7.5 | 1.8 | 0.22 |
| Median iMVD | 11.9 | 12.6 | 11.9 | 0.89 |
SMGA — simple mammary gland adenocarcinoma, PI — roliferation index, AI — apoptotic index, iMVD — intra-tumor microvessel density.
Significant P-value. Grades III and II had a significantly higher median PI than grade I. The difference in median PI between grades II and III was not statistically significant.
There were no significant differences in median iMVD, PI, or AI among the different expression levels of VEGF, VEGFR-2, and no significant difference in median iMVD, or AI among the histologic grade groups (Kruskal-Wallis test). In normal skin tissues, VEGFR-2 expression was detected in normal mammary epithelium as well as dermal fibroblasts, while VEGF expression was weak or absent. Normal vessels within mammary tissue stained positive for VEGFR-2 and vWF.
Discussion
In this study, 26 canine simple mammary gland adenocarcinomas were histologicaly graded and immunohistochemically evaluated for the expression of VEGF and VEGFR-2, iMVD, PI, and AI.
We found a moderate correlation between VEGF and histologic grade. In agreement with this, a previous study found a significant difference in the number of VEGF positive cells among the different histologic grade groups of malignant canine mammary tumors (28). Only one study previously examined VEGFR-2 expression in canine mammary tumors (34). Several histologic subtypes were evaluated including malignant mixed tumors and tumors with squamous differentiation. Contrary to the present study, a significant difference in VEGFR-2 expression was found among the different histologic grades, with highest levels being found in less differentiated tumors (34). The absence of correlation between VEGFR-2 and histologic grade in SMGAs in this study may be related to sample size, or may indicate that VEGFR-2 is not related to histologic grade. Additional studies are needed to clarify the role of VEGF in mediating angiogenesis, and the relationship between VEGF and VEGFR-2, and histologic grade in canine SMGAs.
Ki-67 is a nuclear protein expressed in proliferating cells, which has been evaluated in many canine tumors (35,40–45). High index values of Ki-67 were positively correlated with metastasis, death from neoplasia, low disease-free survival rate and low overall survival rates in canine mammary tumors (45). Ki-67 expression is also a useful prognostic indicator in canine mast cell tumors (40). The finding, in the present study, of a significant difference in PI among the different histologic grade groups is in agreement with previous studies (40,45). The lack of a significant difference in PI between grade 3 and 2 tumors could be due to the small sample size.
The detection of VEGF and VEGFR-2 in most canine SMGAs, and the presence of a moderate correlation between VEGF expression and PI may indicate that VEGF promotes tumor growth through an autocrine loop. Similar to our finding in dogs, human breast cancer cells have been shown to have an autocrine VEGF activity (46). Such activity may provide a survival signal for tumor cells through the activation of the PI3/Akt pathway (47). Using a breast carcinoma cell line, the reduction of VEGF expression resulted in a significant decrease in the basal activity of PI3-kinase and, eventually, induced apoptosis (47). Vascular endothelial growth factor autocrine signaling may also result in the increased expression of the chemokine receptor CXCR4 on the surface of tumor cells (48). The binding of this receptor to its ligand, stromal-derived factor-1, stimulates tumor cell migration (49).
The development of angiogenesis in breast cancer is complex and depends on several angiogenic growth factors (50). The assessment of iMVD in breast cancer may relate to histologic grade and prognosis (51). Only 3 studies evaluated iMVD in canine mammary tumors (35,52,53), 2 of which found a correlation between iMVD and histologic grade (35,53). In the third study, iMVD was not correlated with patient age, sex, reproductive status, clinical tumor stage, or histologic type (52). The absence of correlation in this study may indicate that other angiogenic factors are more important than VEGF in promoting angiogenesis in this particular histologic subtype. The disparity between this study and other canine and human studies, however, may also relate to differences in markers used to evaluate iMVD (54), or could be due to the small sample size used herein.
Normal rodent mammary epithelial cells may express VEGF and VEGFR-2 (55). The expression of both molecules is important for the growth of mammary gland during pregnancy and lactation (55). Mammary stromal cells may also express VEGF (56). The expression of VEGFR-2 in normal mammary stromal cells is unknown. The normal mammary tissue used in this study belonged to a nonpregnant and nonlactating bitch. While VEGFR-2 expression was found in normal mammary epithelial and stromal cells, the expression of VEGF in these 2 cell populations was minimal or absent. This expression pattern may suggest that VEGF signaling may be important only during mammary development throughout pregnancy and lactation.
In conclusion, it was hypothesized that VEGF, VEGFR-2, iMVD, and PI would correlate with histologic grade and hence with malignancy of canine SMGAs. However, only VEGF expression and PI correlated with histologic grade. It was also concluded that VEGF may promote tumor growth through an autocrine loop. Since most tumors were positive for VEGF and VEGFR-2, these tumors may respond to therapy targeting these molecules.
Acknowledgments
The authors are grateful to Ms B. Trask and Dr. Cheryl Waldner for their technical and statistical assistance, respectively. This study was funded by a grant from the WCVM Companion Animal Health Fund, Saskatoon, Saskatchewan. CVJ
Footnotes
Reprints will not be available from the authors.
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office (hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
This study was funded by a grant from the Western College of Veterinary Medicine Companion Animal Health Fund, Saskatoon, Saskatchewan, Canada.
References
- 1.Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med. 1995;1:27–31. doi: 10.1038/nm0195-27. [DOI] [PubMed] [Google Scholar]
- 2.Hicklin DJ, Ellis LM. Role of the vascular endothelial growth factor pathway in tumor growth and angiogenesis. J Clin Oncol. 2005;23:1011–1027. doi: 10.1200/JCO.2005.06.081. [DOI] [PubMed] [Google Scholar]
- 3.Ferrara N. Vascular endothelial growth factor. Trends Cardiovasc Med. 1993;3:244–250. doi: 10.1016/1050-1738(93)90046-9. [DOI] [PubMed] [Google Scholar]
- 4.de Vries C, Escobedo JA, Ueno H, Houck K, Ferrara N, Williams LT. The fms-like tyrosine kinase, a receptor for vascular endothelial growth factor. Science. 1992;255:989–991. doi: 10.1126/science.1312256. [DOI] [PubMed] [Google Scholar]
- 5.Terman BI, Dougher-Vermazen M, Carrion ME, et al. Identification of the KDR tyrosine kinase as a receptor for vascular endothelial cell growth factor. Biochem Biophys Res Commun. 1992;187:1579–1586. doi: 10.1016/0006-291x(92)90483-2. [DOI] [PubMed] [Google Scholar]
- 6.Ferrara N. Role of vascular endothelial growth factor in regulation of physiological angiogenesis. Am J Physiol Cell Physiol. 2001;280:C1358–C1366. doi: 10.1152/ajpcell.2001.280.6.C1358. [DOI] [PubMed] [Google Scholar]
- 7.Fong GH, Rossant J, Gertsenstein M, Breitman ML. Role of the Flt-1 receptor tyrosine kinase in regulating the assembly of vascular endothelium. Nature. 1995;376:66–70. doi: 10.1038/376066a0. [DOI] [PubMed] [Google Scholar]
- 8.Dong P, Sakata K, Miyajima Y, Chijiwa K, Mori K, Nakashima T. The predictive value of p53, Ki-67 and angiogenetic factors in primary hypopharyngeal carcinoma. Kurume Med J. 2001;48:261–266. doi: 10.2739/kurumemedj.48.261. [DOI] [PubMed] [Google Scholar]
- 9.Nakopoulou L, Stefanaki K, Panayotopoulou E, et al. Expression of the vascular endothelial growth factor receptor-2/Flk-1 in breast carcinomas: Correlation with proliferation. Hum Pathol. 2002;33:863–870. doi: 10.1053/hupa.2002.126879. [DOI] [PubMed] [Google Scholar]
- 10.Kushlinskii NE, Orinovskii MB, Gurevich LE, et al. Expression of biomolecular markers (Ki-67, PCNA, Bcl-2, BAX, BclX, VEGF) in breast tumors. Bull Exp Biol Med. 2004;137:182–185. doi: 10.1023/b:bebm.0000028135.91289.e9. [DOI] [PubMed] [Google Scholar]
- 11.Erovic BM, Pelzmann M, Grasl MC, et al. Mcl-1, vascular endothelial growth factor-R2, and 14-3-3sigma expression might predict primary response against radiotherapy and chemotherapy in patients with locally advanced squamous cell carcinomas of the head and neck. Clin Cancer Res. 2005;11:8632–8636. doi: 10.1158/1078-0432.CCR-05-1170. [DOI] [PubMed] [Google Scholar]
- 12.Koide N, Nishio A, Kono T, et al. Histochemical study of vascular endothelial growth factor in squamous cell carcinoma of the esophagus. Hepatogastroenterology. 1999;46:952–958. [PubMed] [Google Scholar]
- 13.Dias PP, Azevedo M, Gartner F. Case of malignant biphasic mesothe-lioma in a dog. Vet Rec. 2001;149:680–681. doi: 10.1136/vr.149.22.680. [DOI] [PubMed] [Google Scholar]
- 14.Du JR, Jiang Y, Zhang YM, Fu H. Vascular endothelial growth factor and microvascular density in esophageal and gastric carcinomas. World J Gastroenterol. 2003;9:1604–1606. doi: 10.3748/wjg.v9.i7.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tse GM, Lui PC, Lee CS, et al. Stromal expression of vascular endothelial growth factor correlates with tumor grade and microvessel density in mammary phyllodes tumors: A multicenter study of 185 cases. Hum Pathol. 2004;35:1053–1057. doi: 10.1016/j.humpath.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 16.Al-Dissi AN, Haines DM, Singh B, Kidney BA. Immunohistochemical expression of vascular endothelial growth factor and vascular endothelial growth factor receptor associated with tumor cell proliferation in canine cutaneous squamous cell carcinomas and trichoepitheliomas. Vet Pathol. 2007;44:823–830. doi: 10.1354/vp.44-6-823. [DOI] [PubMed] [Google Scholar]
- 17.Bosari S, Lee AK, DeLellis RA, Wiley BD, Heatley GJ, Silverman ML. Microvessel quantitation and prognosis in invasive breast carcinoma. Hum Pathol. 1992;23:755–761. doi: 10.1016/0046-8177(92)90344-3. [DOI] [PubMed] [Google Scholar]
- 18.Macchiarini P, Fontanini G, Hardin MJ, Squartini F, Angeletti CA. Relation of neovascularisation to metastasis of non-small-cell lung cancer. Lancet. 1992;340:145–146. doi: 10.1016/0140-6736(92)93217-b. [DOI] [PubMed] [Google Scholar]
- 19.Wakui S, Furusato M, Itoh T, et al. Tumour angiogenesis in prostatic carcinoma with and without bone marrow metastasis: A morphometric study. J Pathol. 1992;168:257–262. doi: 10.1002/path.1711680303. [DOI] [PubMed] [Google Scholar]
- 20.Saclarides TJ, Speziale NJ, Drab E, Szeluga DJ, Rubin DB. Tumor angiogenesis and rectal carcinoma. Dis Colon Rectum. 1994;37:921–926. doi: 10.1007/BF02052599. [DOI] [PubMed] [Google Scholar]
- 21.Olivarez D, Ulbright T, DeRiese W, et al. Neovascularization in clinical stage A testicular germ cell tumor: Prediction of metastatic disease. Cancer Res. 1994;54:2800–2802. [PubMed] [Google Scholar]
- 22.Bartoletti R, Cai T, Nesi G, Sardi I, Rizzo M. Qualitative and quantitative analysis of angiogenetic factors in transitional cell bladder carcinoma: Relationship with clinical course at 10 years follow-up. Oncol Rep. 2005;14:251–255. [PubMed] [Google Scholar]
- 23.Li VW, Folkerth RD, Watanabe H, et al. Microvessel count and cerebrospinal fluid basic fibroblast growth factor in children with brain tumours. Lancet. 1994;344:82–86. doi: 10.1016/s0140-6736(94)91280-7. [DOI] [PubMed] [Google Scholar]
- 24.Vacca A, Ribatti D, Roncali L, et al. Bone marrow angiogenesis and progression in multiple myeloma. Br J Haematol. 1994;87:503–508. doi: 10.1111/j.1365-2141.1994.tb08304.x. [DOI] [PubMed] [Google Scholar]
- 25.Brody RS, Goldschmidt MH, Roszel J. Canine mammary gland neoplasia. J Am Anim Hosp Assoc. 1985;19:61–90. [Google Scholar]
- 26.Rutteman GR, Withrow SJ, MacEwen EG. Tumors of the mammary gland. In: Withrow SJ, MacEwen EG, editors. Small Animal Clinical Oncology. 3rd ed. Philadelphia: WB Saunders; 2000. pp. 450–467. [Google Scholar]
- 27.Misdorp W. Tumors of the mammary gland. In: Meuten DJ, editor. Tumors in Domestic Animals. 4th ed. Ames, Iowa: Iowa State Univer Pr; 2003. pp. 575–606. [Google Scholar]
- 28.Restucci B, Papparella S, Maiolino P, De Vico G. Expression of vascular endothelial growth factor in canine mammary tumors. Vet Pathol. 2002;39:488–493. doi: 10.1354/vp.39-4-488. [DOI] [PubMed] [Google Scholar]
- 29.Maiolino P, De Vico G, Restucci B. Expression of vascular endothelial growth factor in basal cell tumours and in squamous cell carcinomas of canine skin. J Comp Pathol. 2000;123:141–145. doi: 10.1053/jcpa.2000.0404. [DOI] [PubMed] [Google Scholar]
- 30.Rawlings NG, Simko E, Bebchuk T, Caldwell SJ, Singh B. Localization of integrin alpha(v)beta3 and vascular endothelial growth factor receptor-2 (KDR/Flk-1) in cutaneous and oral melanomas of dog. Histol Histopathol. 2003;18:819–826. doi: 10.14670/HH-18.819. [DOI] [PubMed] [Google Scholar]
- 31.Maiolino P, Papparella S, Restucci B, De Vico G. Angiogenesis in squamous cell carcinomas of canine skin: An immunohistochemical and quantitative analysis. J Comp Pathol. 2001;125:117–121. doi: 10.1053/jcpa.2001.0485. [DOI] [PubMed] [Google Scholar]
- 32.Restucci B, De Vico G, Maiolino P. Evaluation of angiogenesis in canine mammary tumors by quantitative platelet endothelial cell adhesion molecule immunohistochemistry. Vet Pathol. 2000;37:297–301. doi: 10.1354/vp.37-4-297. [DOI] [PubMed] [Google Scholar]
- 33.Restucci B, Maiolino P, Paciello O, Martano M, De Vico G, Papparella S. Evaluation of angiogenesis in canine seminomas by quantitative immunohistochemistry. J Comp Pathol. 2003;128:252–259. doi: 10.1053/jcpa.2002.0630. [DOI] [PubMed] [Google Scholar]
- 34.Restucci B, Borzacchiello G, Maiolino P, Martano M, Paciello O, Papparella S. Expression of vascular endothelial growth factor receptor Flk-1 in canine mammary tumours. J Comp Pathol. 2004;130:99–104. doi: 10.1016/j.jcpa.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 35.Martin De Las MJ, Millan Y, Ruiz-Villamor E, Bautista MJ, Rollon E, Espinosa De Los MA. Apoptosis and mitosis in tumours of the skin and subcutaneous tissues of the dog. Res Vet Sci. 1999;66:139–146. doi: 10.1053/rvsc.1998.0260. [DOI] [PubMed] [Google Scholar]
- 36.Al-Dissi AN, Haines DM, Singh B, Kidney BA. Immunohistochemical expression of vascular endothelial growth factor and vascular endothelial growth factor receptor in canine cutaneous fibrosarcomas. J Comp Pathol. 2009;141:229–236. doi: 10.1016/j.jcpa.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 37.Haines DM, Chelack BJ. Technical considerations for developing enzyme immunohistochemical staining procedures on formalin-fixed paraffin-embedded tissues for diagnostic pathology. J Vet Diagn Invest. 1991;3:101–112. doi: 10.1177/104063879100300128. [DOI] [PubMed] [Google Scholar]
- 38.Hasan J, Byers R, Jayson GC. Intra-tumoural microvessel density in human solid tumours. Br J Cancer. 2002;86:1566–1577. doi: 10.1038/sj.bjc.6600315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Mahwah, New Jersey: Lawrence Erlbaum; 1988. Differences between correlation coefficients; pp. 109–139. [Google Scholar]
- 40.Scase TJ, Edwards D, Miller J, et al. Canine mast cell tumors: Correlation of apoptosis and proliferation markers with prognosis. J Vet Intern Med. 2006;20:151–158. doi: 10.1892/0891-6640(2006)20[151:cmctco]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 41.Zacchetti A, van Garderen E, Teske E, Nederbragt H, Dierendonck JH, Rutteman GR. Validation of the use of proliferation markers in canine neoplastic and non-neoplastic tissues: Comparison of KI-67 and proliferating cell nuclear antigen (PCNA) expression versus in vivo bromodeoxyuridine labelling by immunohistochemistry. APMIS. 2003;111:430–438. doi: 10.1034/j.1600-0463.2003.t01-1-1110208.x. [DOI] [PubMed] [Google Scholar]
- 42.Phillips BS, Kass PH, Naydan DK, Winthrop MD, Griffey SM, Madewell BR. Apoptotic and proliferation indexes in canine lymphoma. J Vet Diagn Invest. 2000;12:111–117. doi: 10.1177/104063870001200202. [DOI] [PubMed] [Google Scholar]
- 43.Roels S, Tilmant K, Ducatelle R. PCNA and Ki67 proliferation markers as criteria for prediction of clinical behaviour of melanocytic tumours in cats and dogs. J Comp Pathol. 1999;121:13–24. doi: 10.1053/jcpa.1998.0291. [DOI] [PubMed] [Google Scholar]
- 44.Griffey SM, Kraegel SA, Madewell BR. Proliferation indices in spontaneous canine lung cancer: Proliferating cell nuclear antigen (PCNA), Ki-67 (MIB1) and mitotic counts. J Comp Pathol. 1999;120:321–132. doi: 10.1053/jcpa.1998.0281. [DOI] [PubMed] [Google Scholar]
- 45.Pena LL, Nieto AI, Perez-Alenza D, Cuesta P, Castano M. Immunohistochemical detection of Ki-67 and PCNA in canine mammary tumors: Relationship to clinical and pathologic variables. J Vet Diagn Invest. 1998;10:237–246. doi: 10.1177/104063879801000303. [DOI] [PubMed] [Google Scholar]
- 46.Weigand M, Hantel P, Kreienberg R, Waltenberger J. Autocrine vascular endothelial growth factor signalling in breast cancer. Evidence from cell lines and primary breast cancer cultures in vitro. Angiogenesis. 2005;8:197–204. doi: 10.1007/s10456-005-9010-0. [DOI] [PubMed] [Google Scholar]
- 47.Bachelder RE, Crago A, Chung J, et al. Vascular endothelial growth factor is an autocrine survival factor for neuropilin-expressing breast carcinoma cells. Cancer Res. 2001;61:5736–540. [PubMed] [Google Scholar]
- 48.Bachelder RE, Wendt MA, Mercurio AM. Vascular endothelial growth factor promotes breast carcinoma invasion in an autocrine manner by regulating the chemokine receptor CXCR4. Cancer Res. 2002;62:7203–7206. [PubMed] [Google Scholar]
- 49.Muller A, Homey B, Soto H, et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410:50–56. doi: 10.1038/35065016. [DOI] [PubMed] [Google Scholar]
- 50.Fox SB, Generali DG, Harris AL. Breast tumour angiogenesis. Breast Cancer Res. 2007;9:216. doi: 10.1186/bcr1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kato T, Steers G, Campo L, et al. Prognostic significance of microvessel density and other variables in Japanese and British patients with primary invasive breast cancer. Br J Cancer. 2007;97:1277–1286. doi: 10.1038/sj.bjc.6604015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Griffey SM, Verstraete FJ, Kraegel SA, Lucroy MD, Madewell BR. Computer-assisted image analysis of intratumoral vessel density in mammary tumors from dogs. Am J Vet Res. 1998;59:1238–1242. [PubMed] [Google Scholar]
- 53.Jakab C, Halasz J, Kiss A, et al. Evaluation of microvessel density (MVD) in canine mammary tumours by quantitative immunohistochemistry of the claudin-5 molecule. Acta Vet Hung. 2008;56:495–510. doi: 10.1556/AVet.56.2008.4.7. [DOI] [PubMed] [Google Scholar]
- 54.Ferrer L, Fondevila D, Rabanal RM, Vilafranca M. Immunohistochemical detection of CD31 antigen in normal and neoplastic canine endothelial cells. J Comp Pathol. 1995;112:319–326. doi: 10.1016/s0021-9975(05)80013-1. [DOI] [PubMed] [Google Scholar]
- 55.Pepper MS, Baetens D, Mandriota SJ, et al. Regulation of VEGF and VEGF receptor expression in the rodent mammary gland during pregnancy, lactation, and involution. Dev Dyn. 2000;218:507–524. doi: 10.1002/1097-0177(200007)218:3<507::AID-DVDY1012>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 56.Senger DR, Van De Water L. VEGF expression by epithelial and stromal cell compartments: Resolving a controversy. Am J Pathol. 2000;157:1–3. doi: 10.1016/S0002-9440(10)64508-7. [DOI] [PMC free article] [PubMed] [Google Scholar]