Abstract
This study investigated whether homeless men are a bridge group for transmission of HIV to the general population in India. A cross-sectional study design was used to measure subjects’ past and current sexual activities. We surveyed 493 of 606 homeless men aged 18–49 years who live in public places in Kolkata, India, who were invited to take part in a structured interview, using a CD player and earphones. Almost two-thirds of respondents had never attended school. Sex with commercial sex worker (CSWs), multiple sex partners, and inconsistent condom use were common. About 90% of married homeless men visited CSWs, but only 3.3% consistently used condoms. AIDS awareness and risk perception were very low. Less education and being married but not currently living with wife were associated with high-risk sexual behaviors. Homeless men should be considered a potential bridge for HIV transmission from CSWs to the general population. Appropriate non-written communication strategies targeted to homeless people are urgently needed. Community intervention programs targeting the homeless, such as the ‘Popular Opinion Leader’ model, should be designed and evaluated.
Keywords: Homeless, Risk group, Sexual behavior, HIV/AIDS, STDs, Condom use, India
Introduction
The 2006 estimates recently released by the National AIDS Control Organization (NACO) indicate that the national adult HIV prevalence in India is approximately 0.36%, which corresponds to an estimated 2–3.1 million people living with HIV in India. Although HIV prevalence is high among sex workers and drug users, the prevalence among its one billion-plus inhabitants is relatively low (NACO 2004). The majority of the cases come from urban areas, fuelled by heterosexual commercial sex workers (CSWs) and their clients, but an increasing number of cases are occurring among women with low risk behaviors. India stands at a critical point, with HIV poised to expand rapidly (Chandrasekharan et al. 2006).
Homeless in the United States and in other countries are considered to be at high risk for HIV because of their high-risk sexual and drug use behaviors. Several studies in the U.S. reported that homeless and runaway youth have higher rates of HIV infection (Bailey et al. 1998). These homeless youths are at elevated risk for HIV/AIDS in terms of high-risk sexual behavior, having large numbers of sexual partners, many casual sexual contacts, survival sex (in exchange for food), and infrequent condom use. Other studies in the U.S. have also demonstrated that HIV sero-prevalence is very high among migrant laborers and seasonal farm workers. In southern California, HIV screening at 15 labor camps revealed a 13% prevalence in 198 predominantly single migrant workers. In Florida, screening at 14 migrant farm worker labor camps during peak season identified a 5% prevalence of HIV among 310 subjects, predominantly of Latino and African-American ethnicity (Organista and Organista 1997).
Industrialization and rapid urbanization in India has resulted in massive migration of people from rural to urban areas, leading to a huge homeless population. According to the 2001 census, 285 million, or 28%, of Indians live in urban areas (Census of India 2001). The census also reports that there are 13.5 million households (household defined as a group of people who share a kitchen) without homes, with each household having an average of six members. The total homeless population has been estimated at 78 million. About 78% of these households without homes live in three major cities (Delhi, Kolkata, and Mumbai), where they live as street or pavement dwellers, due to their inability to afford accommodation in the cities. They live in public places such as church/temples, garages, or outdoor public places such as sidewalks, railway stations, under flyovers, but have no permanent housing structure. The majority are migrants looking for opportunities in the city, often fleeing rural poverty and, in many cases, natural calamities. Most but not all leave their family members in their home villages. They engage in temporary and odd jobs, such as rag picking, domestic service, hotel boys, porters, hand load carriers, and cart pullers. Their lifestyles and behaviors make them vulnerable for acquiring and transmitting sexually transmitted diseases (STDs) and HIV infection. Recent evidence of increasing transmission of HIV from urban to rural areas and to the general population, especially among married monogamous women in different parts of India, also points toward the role of rural to urban migrants in transmitting HIV to their spouses in rural areas.
Several studies have indicated that contrary to traditional beliefs, sexual promiscuity and other sexual risk behaviors are not uncommon in India. Multiple or non-regular sex partners have been found to be quite prevalent among younger adults (Brahme et al. 2005); the Behavioral Surveillance Survey across the country revealed that about 13% of urban males and 11.5% of rural males reported at least one non-regular sex partner (Hines and Caetano 1998). Premarital sex is also not uncommon. Condom use among sexually active individuals in India, however, remains very low. Infrequent condom use with CSWs (Dandona et al. 2005), non-regular sex partners (Brahme et al. 2005), or men having sex with men (Go et al. 2004) has been reported in almost all groups of sexually active persons, including married and unmarried men (NACO 2001b), urban slum dwellers (Sachdev 1998), rural men (Bhatia et al. 2005), and truck drivers (Ubaidullah 2004).
Little information has been collected about sexual behavior among homeless people in India. The National AIDS Control Organization has not yet considered homeless people to be a risk group for HIV (NACO 2001b). Thus, there is a need to study HIV transmission and risk behaviors among the homeless in India to learn about the role they may play in spreading the epidemic to the general population.
This cross-sectional study documented the high prevalence and correlates of high-risk behaviors related to HIV among homeless men, and their potential to spread the HIV infection to the general population. Those who visited a CSW or had sex with a male partner and/or had multiple sexual partners were considered to be at high risk for HIV infection. We defined “bridge groups” as persons who have sex with both high- and low-risk individuals. The findings of this study are relevant to policy makers and program managers engaged in AIDS control programs in India and perhaps in other high-burden countries with comparable homeless populations.
Methods
Setting
This study was conducted in Kolkata, which is the capital of the Indian state of West Bengal, located in eastern India. The city has a population of almost five million, with an extended metropolitan population of over 14 million, making it the third largest urban agglomeration and the fourth largest city in India. The population density is 24,760/km2. HIV sentinel surveillance data revealed an HIV prevalence of 0.84% among antenatal clinic attendees (ANC) and 6.8% among CSWs (HIV Sentinel Surveillance Report 2005). The total number of HIV-infected individuals detected in West Bengal through 2005 was 9,852. There were 4,559 cumulative AIDS cases. Unprotected sex remains the major route of known HIV transmission, accounting for 89% of the infections in West Bengal (Health on the March 2005–2006).
This study was approved by the Institutional Review Board (IRB) of the University of California, Los Angeles, USA, and the IRB of National Institute of Cholera & Enteric Diseases, Kolkata, India.
Selection of Study Area
The Kolkata Municipal Corporation area is divided into 141 administrative wards. The present study was conducted in seven adjacent wards in central Kolkata (downtown area). The specific area was selected because it: (1) contains terminal railway stations, business places, and offices; (2) has thousands of homeless residents; and (3) is a center for drug dealing and commercial sex. Thus, this area is an appropriate setting for an in-depth study of the different kinds of interactions among many recognized groups at risk for acquiring and transmitting HIV and STDs, including the homeless.
Sample Selection
Across-sectional design was used tomeasure past and current sexual activities. The source population refers to all men aged 18–49 years who live in public places in central Kolkata, such as churches/temples, garages, or outdoor public places such as sidewalks, railway stations, under flyovers, and/or have no permanent housing structure for shelter in this area, and have been living in Kolkata for at least the past 30 days. Those who live in a rented home/motel/boarding/institution were not considered to be homeless.
The sample size was estimated for the objective of exploring predictors for ‘inconsistent condom use’. We used the algorithm of Ariawan and Frerichs (1996) for estimating sample size for this two-stage cluster survey. The entire study area was divided into 89 locations (clusters) after discussion with local key personnel. Using the CSurvey program, 26 clusters (locations) were randomly selected as study frames with probability proportionate to size (PPS) from the 89 locations within the study area. At the second stage, interviewers randomly selected the first eligible homeless men and then proceeded until 19 eligible subjects were sampled. Data were collected over a 4-month period starting in August 2005.
Questionnaire
An anonymous questionnaire was administered to each participant in a private location by a trained interviewer. The first part included less sensitive questions asked by the interviewer, such as socio-demographic characteristics, knowledge regarding HIV/STDs, attitude towards condom use, and substance abuse behavior. The sensitive questions relating to personal sexual behavior were included in the second part and administered by CD player and earphones (Liu et al. 1998). The questionnaire was piloted before being implemented in the main study (available upon request).
CD Player/Headphones Technique
Since sex is still a taboo subject in Indian culture, and people hesitate to discuss sexual issues with others, a CD player with earphones was used to ask sensitive questions. The questions were first recorded on a CD in the local dialect. The participants listened to the questions through earphones, and recorded their responses on an answer sheet with no identifying information, listing only codes for possible responses to each question. Questions were asked by a male voice, and possible answers were given by a female voice. The pilot study revealed that the majority of the respondents were illiterate or barely literate. For this reason, the answer sheet was coded with different colors for each question and different symbols for each option. Participants were asked to mark the symbols for their choices for each question.
Statistical Analysis
The two-stage cluster PPS sample rendered a self-weighted sample. Analyses were conducted with the SAS cluster survey program (SAS version 9.1.1, SAS Institute Inc. Cary, NC, USA). Descriptive analyses of all variables were done, using proportions and means where applicable. We then explored the association of important socio-demo-graphic factors with sexual risk behaviors. The Mantel–Haenzel χ2 test was used to compare proportions that were considered significant if the P-value was less than .05. Finally, logistic regression analyses were performed to detect predictors of high-risk sexual behavior, using the Wald statistic value.
Results
We approached 606 homeless men, of whom 494 (81.4%) agreed to participate. One subject chose to withdraw during the interview. The refusal rate was therefore 18.6%. Over three-quarters of the subjects who refused to participate stated that they were not willing to be involved in the study; the other one-quarter declined due to ‘lack of time’.
Demographic Characteristics of Study Participants
The socio-demographic information of the participants is presented in Table 1. The mean age of the participants was 28.2 years (range 18–45 years). Only 5% were older than 39 years. The mean duration in Kolkata was 4.7 years. Almost two-thirds (63.7%) had not attended school, but 30.4% were able to sign their name. The percentage of participants with no education is higher (30.8%) than observed in the total population in India (http://www.censusindia.net). Almost 80% were Hindu, and 21.3% were Muslim. About 28.8% of participants belonged to a scheduled caste, 1.8% to a scheduled tribe, 32% to the backward classes, and 32% to general castes. The study sample had a higher proportion of individuals in scheduled castes than the general population of West Bengal (5.5%).
Table 1.
Socio-demographic characteristics of study participants
| Characteristics | Number | % |
|---|---|---|
| Age (years) | ||
| 18–24 | 113 | 22.9 |
| 25–29 | 194 | 39.4 |
| 30–34 | 122 | 24.8 |
| 35–39 | 38 | 7.7 |
| 40–49 | 26 | 5.3 |
| Duration in Kolkata (years) | ||
| <4 | 223 | 45.2 |
| 4–6 | 207 | 42.0 |
| 7–10 | 39 | 7.9 |
| >10 | 24 | 4.9 |
| Education | ||
| Illiterate | 164 | 33.3 |
| Literate | 150 | 30.4 |
| Class IV | 86 | 17.4 |
| Class VIII | 55 | 11.2 |
| Class X | 29 | 5.9 |
| Above class X | 9 | 1.9 |
| Religion | ||
| Hindu | 380 | 77.1 |
| Muslim | 105 | 21.3 |
| Other | 8 | 1.6 |
| Race | ||
| Forward class | 158 | 32.0 |
| Backward class | 161 | 32.7 |
| Scheduled caste | 142 | 28.8 |
| Scheduled tribe | 9 | 1.8 |
| Others | 23 | 4.7 |
| Permanent residence | ||
| Bihar | 288 | 58.4 |
| Jharkhand | 104 | 21.1 |
| Orissa | 37 | 7.5 |
| Uttar Pradesh | 31 | 6.3 |
| West Bengal | 15 | 3.0 |
| Local | 12 | 2.4 |
| Others | 6 | 1.3 |
Almost 90% of the respondents were from the three states adjacent to Bihar, Jharkhand state, and 7.5% Orissa state. Only 3% were from rural West Bengal. The Census of India 2001 identifies Bihar as one of the poorest states in India, and as the largest source state for migrants to the rest of India.
Table 2 presents other socio-economic characteristics of the study participants. About 48% had lived on the streets in temporary structures or with friends, and 21% alone. Only 17% lived with their spouses and/or parents in these temporary arrangements. Another 13% lived with distant relatives. Forty-three percent were currently married, but 74% of them lived in Kolkata without their spouses. Almost all had some form of employment. Job types are categorized in Table 2. Their income from these menial jobs ranged from INR 150–600 (US $4–14), with an average of INR 368 (US $9).
Table 2.
Socio-demographic characteristics of study participants
| Characteristics | Number | % |
|---|---|---|
| Presently living with | ||
| Coworkers | 237 | 48.1 |
| Alone | 104 | 21.1 |
| Relatives | 49 | 9.9 |
| Family | 86 | 17.4 |
| Parents | 17 | 3.5 |
| Job | ||
| Rickshaw puller | 101 | 20.5 |
| Van puller | 127 | 25.8 |
| Street seller | 150 | 30.4 |
| Assistant | 79 | 16.0 |
| Labor | 27 | 5.5 |
| Rag picker | 9 | 1.8 |
| Marital status | ||
| Unmarried | 171 | 34.7 |
| Married | 212 | 43.0 |
| Divorced | 38 | 7.7 |
| Separated | 54 | 11.2 |
| Widowed | 18 | 3.6 |
| Frequency of visiting home town in past year | ||
| 1–2 Times | 224 | 45.4 |
| 3–4 Times | 169 | 34.3 |
| 5–6 Times | 59 | 12.0 |
| >6 Times | 13 | 2.6 |
| Never | 28 | 5.7 |
| Income (rupees/week) | ||
| 0–299 | 95 | 19.3 |
| 300–399 | 160 | 32.5 |
| 400–499 | 144 | 29.2 |
| 500 And above | 94 | 19.1 |
Forty-five percent of participants had visited their home town once or twice in the previous year. Another 34.3% had visited three or four times. Only 2.6% of participants reported that they went to their villages more than six times a year. Fifty-six percent of the married men whose families did not stay with them had visited their home villages more than twice in the past year.
Substance Abuse
Ninety-four percent of participants had used tobacco and/or alcohol during their lifetime. Older men were more addicted to tobacco and alcohol than younger men. Sixty-four percent of study participants had consumed alcohol. Twenty participants (4%) injected drugs regularly. Seventeen (85%) of the injecting drug users (IDUs) shared needles/syringes during drug use. We found IDUs in only six locations.
Knowledge of HIV/AIDS
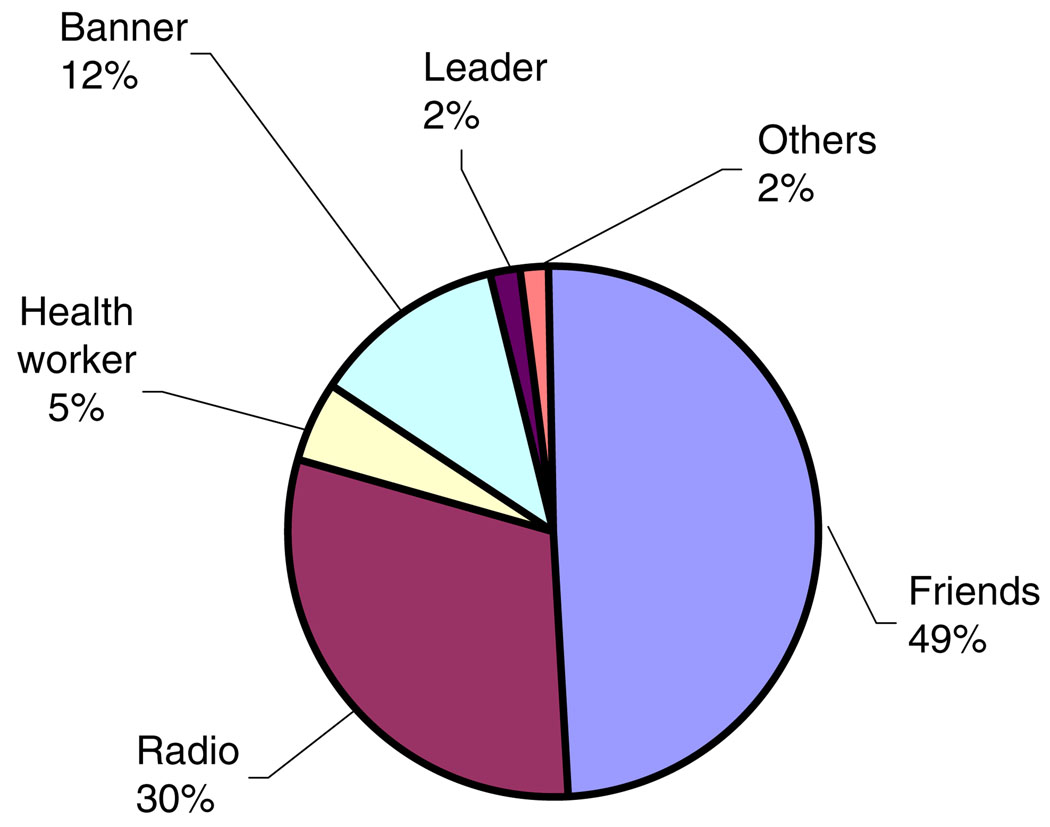
Self-perception of knowledge of HIV/AIDS was poor among the study participants. Only 1.6% of participants felt that they knew much about HIV/AIDS. About 45% of participants had never heard of it. Among those who had heard of HIV/AIDS, the highest proportion (49%) had received information about it from their friends (Fig. 1). The next most frequent source was radio (30.3%). The average duration since first hearing about HIV/AIDS was 3 years. Most had heard about it after coming to Kolkata.
Fig. 1.
Source of AIDS information (n = 493)
We asked six questions related to modes of HIV transmission. Responses were recorded as ‘agree’, ‘disagree’ and ‘do not know’. Most of the men had either no knowledge or incorrect information (Table 3).
Table 3.
Awareness about transmission of HIV infection among subjects (n = 493)
| Statements | Agree | Disagree | Do not know |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| AIDS is transmitted primarily through sexual relations | 77 (15.6) | 30 (6.1) | 386 (78.3) |
| AIDS can be transmitted by blood transfusions | 67 (13.6) | 60 (12.2) | 366 (74.2) |
| AIDS can be transmitted by mosquito bitesa | 104 (21.1) | 57 (11.6) | 332 (67.3) |
| AIDS can be transmitted from an infected mother to new born | 91 (18.5) | 41 (8.3) | 361 (73.2) |
| AIDS can be transmitted by sharing eating utensils with people infected with HIVa | 117 (23.7) | 37 (7.5) | 339 (68.8) |
| AIDS can be transmitted by sharing needles and syringes | 76 (15.4) | 30 (6.1) | 387 (78.5) |
Incorrect answers
Sexual Risk Behavior
Over 90% of participants had had sexual intercourse. The mean age at sexual debut was 19.5 years. Over 62% of sexually active men reported that they had heard about or seen a condom, but only 37% of those who had heard about or seen a condom had ever used one.
One hundred twenty four of the never-married participants (73%) reported having had sexual activity. They reported three sexual partners on average during the past six months. Most sexually active participants (361/81.2%) had visited a CSW (Table 4), about 38% of whom had visited several times a week in the last three months. Two-thirds (67%) had never used a condom with a CSW. Only 12 participants (3.3%) reported using condoms consistently with CSWs within the last three months. Forty-eighty percent reported that they had drunk alcohol during their last visit to a CSW. Twenty-nine participants reported that they had a female sex partner other than their wives, girlfriends, or CSWs. Only four participants (14.2%) of those responding to the question had used condoms during their last sexual intercourse with other types of female sex partners.
Table 4.
Sexual behaviors and STD symptoms of study participants
| Characteristics | Na | % |
|---|---|---|
| Ever visited a commercial sex worker (CSW) | ||
| Yes | 363 | 81.2 |
| No | 84 | 18.8 |
| Frequency of visit to a CSW last 3 months | ||
| Everyday | 2 | 0.5 |
| Few times a week | 139 | 38.3 |
| Few times a month | 179 | 49.3 |
| Rarely | 43 | 11.8 |
| Use of condom during last visit to a CSW | ||
| Yes | 52 | 14.3 |
| No | 312 | 85.7 |
| Other female sex partner | ||
| Yes | 29 | 6.5 |
| No | 418 | 93.5 |
| Use of condom during last intercourse | ||
| Yes | 4 | 14.3 |
| No | 24 | 85.7 |
| Having any male sex partner | ||
| Yes | 68 | 15.2 |
| No | 379 | 84.8 |
| Condom use during last intercourse | ||
| Yes | 1 | 1.5 |
| No | 66 | 97.1 |
| Genital ulcer/discharge past 6 months | ||
| Yes | 121 | 24.5 |
| No | 372 | 75.5 |
N may not be equal for all variables due to missing values
Sex with men was also reported in the study. Sixty-eight participants (15%) reported that they had had a male partner. Seven reported having only male sex partners; the others were bisexual. Fifteen percent of married participants reported having also had sex with a male partner. None had used condoms consistently with their male partners. Only one participant had used a condom during their last sexual intercourse with a male partner.
One-quarter of participants (119/26.62%) reported that they had had a genital ulcer and/or urethral discharge during the past six months.
Association of Socio-demographic Factors with Visiting CSWs
We explored associations of socio-demographic characteristics with self-reported visits to CSWs among the 447 participants responding to all the questions. The data in Table 5 indicates that less education, fewer visits to one’s home town in the past year, not currently living with wife or relatives, being married, and shorter duration in Kolkata were significantly associated with visits to CSWs. About half of those who had more than 8 years of education had visited a CSW, compared to 90% of those who were illiterate and 86% of those barely literate. Most homeless who visited their home towns had also visited CSWs. In addition, 98.9% of participants who lived alone had visited a CSW. About one-third of participants who lived with their wives reported visiting a CSW, but 90% of currently married participants had a history of visiting CSWs. There was no association of age, income, or self-perception of one’s own knowledge of AIDS with visits to CSWs.
Table 5.
Association of socio-demographic characteristics with visiting commercial sex workers (n = 447)
| Characteristics | Category | No (%) | M-H χ2 |
|---|---|---|---|
| Age (years) | 18–24 | 56 (82.3) | 0.23 |
| 25–29 | 158 (81.9) | ||
| 30–34 | 96 (78.7) | ||
| 35–39 | 34 (89.5) | ||
| 40 and older | 19 (73.1) | ||
| Educational level | Illiterate | 133 (89.9) | 29.45* |
| Literate | 117 (86.0) | ||
| Class IV | 55 (72.3) | ||
| Class VIII | 41 (78.8) | ||
| Above class VIII | 17 (48.5) | ||
| Frequency of visiting hometown in the past year | Nil | 21 (77.8) | 36.84* |
| 1–2 times | 197 (97.5) | ||
| 3–4 times | 100 (64.5) | ||
| >4 times | 35 (67.3) | ||
| Income (Rs per week) | 0–299 | 56 (71.8) | 1.43 |
| 300–399 | 121(84.6) | ||
| 400–499 | 110 (82.7) | ||
| 500 and above | 76 (81.7) | ||
| Presently living with | Wife | 19 (35.2) | 149.89* |
| Relatives | 45 (51.4) | ||
| Friend | 207 (97.6) | ||
| Alone | 92 (98.9) | ||
| Marital status | Never Married | 160 (75.4) | 4.5* |
| Currently married | 99 (90.0) | ||
| Others | 104 (83.2) | ||
| Duration of stay in Kolkata (years) | 0–3 | 168 (87.5) | 12.45* |
| 4–6 | 152 (79.2) | ||
| >6 | 43 (68.2) | ||
| Self-perception of AIDS knowledge | A lot | 7 (87.5) | 0.01 |
| Something | 34 (85.0) | ||
| A little | 155 (79.1) | ||
| Nothing | 167 (82.3) |
P value < .01
We then attempted to explore any association of frequency of visits to CSWs with socio-demographic characteristics among those who reported a visit to a CSW. Frequency of visits to CSWs was significantly associated with younger age (P = .005). Almost half (46%) of the participants aged 18–24 years had visited CSWs several times a week, compared to 37% of the 25–29-year age group and 24% of the 30–34-year age group. Regular visits to CSWs were highest among those who had lived in Kolkata 4–7 years. We did not find any relationship between income and job type with frequency of visits to CSWs.
Univariate Analysis of Factors for High-Risk Sexual Behavior
Table 6 summarizes the factors associated with high-risk sexual behaviors. Most of the sexually active participants (393/93.3%) reported high-risk sexual behaviors. Education, marital status, duration in Kolkata, staying with a partner in Kolkata, perception of HIV risk, and alcohol consumption were found to be significantly associated with high-risk sexual behavior, whereas age and income were not.
Table 6.
Association of socio-demographic characteristics with high-risk sexual behavior (n = 447)
| Characteristics | Category | High-risk behavior number (%) | M-H χ2 |
|---|---|---|---|
| Age (years) | 18–24 | 63 (91.3) | 0.01 |
| 25–29 | 167 (86.5) | ||
| 30–34 | 105 (86) | ||
| 35–45 | 59 (92) | ||
| Educational level | Illiterate | 265 (93) | 17.29** |
| Class IV | 61 (80.3) | ||
| Above class IV | 68 (78.2) | ||
| Income (Rs per week) | 0–299 | 66 (83.5) | 4.14 |
| 300–499 | 241 (87.3) | ||
| 500 and above | 87 (93.5) | ||
| Presently living with | Wife | 29 (53.7) | 67.76** |
| Alone/others | 365 (92.6) | ||
| Marital status | Never married | 170 (80.2) | 14.99** |
| Others | 107 (97.3) | ||
| Currently married | 117 (92.9) | ||
| Duration of stay at Kolkata (years) | 0–3 | 180 (93.2) | 8.18** |
| >3 | 214 (83.9) | ||
| Perception of HIV risk | Yes | 43 (73) | 13.82 |
| No | 348 (90.4) | ||
| Drink alcohol | Yes | 255 (85.6) | 4.09* |
| No | 139 (92.7) |
P value < .05
P value < .01
Adjusted Logistic Regression Analysis
We compared the groups engaging in high-risk sexual behavior with those who did not. We included the factors listed in Table 7 as covariates, based on our findings and prior knowledge, as well as age of sexual debut. Factors significantly associated with high-risk behavior were education, staying with a partner in Kolkata, marital status, and self-perception of own HIV risk. The illiterate group had a 4.5-fold higher likelihood (95% C.I. 1.9–10.1) for engaging in high-risk behavior than participants with more than 4 years of education. Lack of perception of HIV risk was also strongly associated with high-risk behavior (AOR 3.9, 95% C.I. 1.6–9.6). Age, income, age at sexual debut, and duration in Kolkata were not found to be independent predictors of high-risk sexual behavior.
Table 7.
Adjusted logistic regression model of predictors for high-risk sexual behavior
| Characteristics | Category | AOR (95%CI) | Wald χ2 |
|---|---|---|---|
| Age (years) | 18–24 | 1.5 (0.3–8.4) | 1.48 |
| 25–29 | 0.5 (0.2–1.7) | 1.83 | |
| 30–34 | 0.5 (0.1–1.6) | 2.07 | |
| 35–45 | Reference | ||
| Educational level | Illiterate | 4.5 (1.9–10.8) | 13.63* |
| Class IV | 1.18 (0.4–3.2) | 1.79 | |
| Above class IV | Reference | ||
| Income (US$/week) | 0–7 | 0.5 (0.1–1.7) | 0.85 |
| 8–12 | 0.6 (0.2–1.8) | 0.2 | |
| 13 and above | Reference | ||
| Presently living with | Alone/others | 10.4 (4.6–23.8) | 31.04* |
| Wife | Reference | ||
| Marital status | Currently married | 3.1 (1.2–7.7) | 15.25* |
| Others | 3.84 (0.8–7.8) | 7.27 | |
| Never married | Reference | ||
| Duration of stay in Kolkata (years) | 0–3 | 2.3 (1.03–5.3) | 4.11 |
| >3 | Reference | ||
| Perception of HIV risk | No | 3.87 (1.6–9.6) | 8.58* |
| Yes | Reference | ||
| Alcohol consumption | Yes | 2.1 (0.9–4.7) | 2.88 |
| No | Reference | ||
| Age at first sex | 0.88 (0.8–1.1) | 3.62 |
P value < .01
Discussion
The HIV epidemic is concentrated in India among several high-risk groups. These groups have been included by NACO as sentinel groups, but homeless men are not included. This study has attempted to explore the vulnerability of homeless people for HIV infection.
Very few participants considered themselves to be a risk for HIV infection. In spite of living in Kolkata, their awareness level is as low as those of rural residents of India. These misconceptions often cause people to discriminate against people living with HIV/AIDS, and to be reluctant to socialize with them. The extremely low awareness of their own risk for HIV, coupled with low awareness about HIV/AIDS, underscores the need for targeting the homeless to receive information. We found that half of participants got information about HIV from their friends/coworkers. Communication through peers is therefore one possible strategy to increase HIV/AIDS knowledge levels in this group. Thus, the ‘Popular Opinion Leader’ (POL) model community intervention strategy might be effective in this group (Kelly 2004). This POL model has been well adapted to different groups of people in several countries.
Having multiple sex partners is associated with increased risk for HIV/STDs, as observed in several studies (NACO 2006; Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat 2003). We found that more than two-thirds of never married participants were sexually active, and almost all sexually active participants had more than one sexual partner. Younger men were more likely to report multiple sex partners than older men. Our data indicate that this group is more sexually active than the general population.
Another important consideration would be the potential for transmission of HIV/STD by these homeless men to their usual sex partners. We observed that 80% of study participants had visited a CSW. Fifteen percent of homeless men had engaged in sex with male partners. Condom use with sex partners was minimal. Moreover, 79% of currently married participants reported extramarital sex. The HIV prevalence among CSWs in Kolkata was 10.8% in 2005 (National AIDS control organization 2005). Clearly, sexual mixing among CSWs, homeless men, and their spouses was common among the homeless. Thus, there is a high likelihood of homeless men transmitting HIV to their spouses living in rural areas, as well as to their other partners.
We explored the underlying causes of high-risk behaviors in this population. Several studies have found that acculturation among migrants is a complex issue and influences many of migrants’ behaviors, including HIV risk behaviors (NACO 2001a). This study showed that those who were illiterate, recently migrated to Kolkata, ever married, stayed with friends or alone, drank alcohol, and perceived themselves to be risk-free were more likely to engage in high-risk sexual behaviors. Those young married men not staying with their wives were more likely to engage in risk-taking behavior than those married and staying with their spouses. Weaker family ties, lack of social inhibitions in a new place, and peer pressure promoted sexual mixing.
Several limitations in our study need to be mentioned. First, there was an 18% refusal rate in this study. Participation was voluntary and anonymous. We have no data about those who refused participation. However, we suspect that those who knew their risk status were more likely to refuse to participate, so our estimates are probably conservative. Second, all variables were self-reported. Respondents may have under-reported some sexual behaviors because of conservative social norms. Although some studies re-interview a randomly selected subset of participants to test reliability of responses, this was not possible in our case. We recorded all information anonymously, so that we had no way to recall our participants. Rather, we adopted a cross-checking procedure during the interview session.
Implications and Recommendations
This study demonstrates that a significant proportion of homeless men are engaging in high-risk sexual behaviors that make them vulnerable to acquiring HIV and transmitting it to their regular partners. More alarming, this study provides evidence that condom use is minimal with sex partners. Married men not staying with spouses were strongly associated with high-risk behavior. NACO has identified several groups as ‘high-risk groups’ and ‘bridge risk groups’. Targeted intervention projects are now being conducted among these identified groups to reduce the spread of HIV transmission to the huge general population. Immediate steps should be taken by NACO to recognize that homeless people engage in high-risk activities, and therefore are a ‘bridge group’. Education about risks involved with multiple partners, extramarital sex, and not using of condoms are also needed, especially among the younger homeless men. Non-written communication strategies need to be adopted in order to reach this population. Strategies should include pictographic posters, story groups, street drama, and radio spots that reach those who are illiterate. There is a need to convince them that they are at risk. One strategy could be the POL model to approach community intervention. Core elements of the POL strategy would be: (1) identify and enlist the support of popular and well-linked opinion leaders to take on risk reduction advocacy roles; (2) train cadres of opinion leaders to disseminate risk reduction messages in conversations within their own natural social networks; (3) support and reinforce successive waves of opinion leaders to help reshape social norms to encourage safer sex. All the major findings from this study are likely to be relevant not only to homeless people of Kolkata, but also to homeless men in other cities in India and other countries. Given the current low population prevalence of HIV in India, now is the time to act before homeless men become a major driver of the epidemic.
Acknowledgements
We thank Wendy Aft for editorial assistance. We also thank Mitun Bose for assistance throughout the entire research. The views expressed in this article are solely those of the authors and do not necessarily reflect official views of the Government of West Bengal, India. This work was supported by NIH Fogarty International Center grant D43 TW000013.
Contributor Information
Arunansu Talukdar, Medicine Department, Calcutta National Medical College, Kolkata, India.
Krishnendu Roy, Medicine Department, Calcutta National Medical College, Kolkata, India.
Indrajit Saha, Community Medicine, R.G. Kar Medical College, Kolkata, India.
Jayashree Mitra, Department of Health & Family Welfare, Kolkata, West Bengal, India.
Roger Detels, Email: detels@ucla.edu, School of Public Health, University of California Los Angeles, Los Angeles, CA 90095-1772, USA.
References
- Ariawan I, Frerichs RR. CSurvey 1.5.A cluster sampling utility program for IBM-compatible microcomputers. Los Angeles: University of California, Los Angeles; 1996. [Google Scholar]
- Bailey SL, Camlin CS, Ennett ST. Substance abuse and risky sexual behavior among homeless runaway youth. Journal of Adolescent Health. 1998;23:377–388. doi: 10.1016/s1054-139x(98)00033-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatia V, Swami HM, Parashar A, Justin TR. Condom-promotion programme among slum-dwellers in Chandigarh, India. Public Health. 2005;119(5):382–384. doi: 10.1016/j.puhe.2004.07.004. [DOI] [PubMed] [Google Scholar]
- Brahme RG, Sahay S, Malhotra-Kohli R, Divekar AD, Gangakhedkar RR, Parkhe AP, Kharat MP, Risbud AR, Bollinger RC, Mehendale SM, Paranjape RS. High-risk behaviour in young men attending sexually transmitted disease clinics in Pune, India. AIDS Care. 2005;17(3):377–385. doi: 10.1080/09540120412331299771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census of India. New Delhi, India: Office of the Registrar General. 2001 Retrieved from http://www.censusindia.net (December 7, 2006)
- Chandrasekharan P, Dallabetta G, Loo V, Rao S, Gayal H, Alexandar A. Containing HIV/AIDS in India: The unfinished agenda. Lancet Infectious Diseases. 2006;6(8):508–521. doi: 10.1016/S1473-3099(06)70551-5. [DOI] [PubMed] [Google Scholar]
- Dandona R, Dandona L, Gutierrez JP, Kumar AG, McPherson S, Samuels F, Bertozzi SM ASCI FPP Study Team. High risk of HIV in non-brothel based female sex workers in India. BMC Public Health. 2005;5:87. doi: 10.1186/1471-2458-5-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go VF, Srikrishnan AK, Sivaram S, Murugavel GK, Galai N, Johnson SC, Sripaipan T, Solomon S, Celentano DD. High HIV prevalence and risk behaviors in men who have sex with men in Chennai, India. Journal of Acquired Immune Deficiency Syndrome. 2004;35(3):314–319. doi: 10.1097/00126334-200403010-00014. [DOI] [PubMed] [Google Scholar]
- Government of West Bengal, India. Health on the March, West Bengal. 2005–2006
- Hines AM, Caetano R. Alcohol and AIDS-related sexual behavior among Hispanics: Acculturation and gender differences. AIDS Education and Prevention. 1998;10(6):533–547. [PubMed] [Google Scholar]
- Kelly JA. Popular opinion leaders and HIV prevention peer education: Resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care. 2004;16(2):139–150. doi: 10.1080/09540120410001640986. [DOI] [PubMed] [Google Scholar]
- Liu H, Xie J, Yu W, Song W, Gao Z, Ma Z, Detels R. A study of sexual behavior among rural residents of China. Journal of Acquired Immune Deficiency Syndrome and Human Retrovirology. 1998;19(1):80–88. doi: 10.1097/00042560-199809010-00013. [DOI] [PubMed] [Google Scholar]
- National AIDS Control Organization (NACO) Combating HIV/AIDS in India 2000–2001. 2001a Retrieved from http://www.naco.nic.in/vsnaco/indianscene/country.htm 25 October, 2006.
- National AIDS Control Organization (NACO) National baseline general population behavior surveillance survey, India. 2001b
- National AIDS Control Organization (NACO) HIV/AIDS Indian scenario. Current status and trend of the HIV/AIDS epidemic in India. 2004
- National AIDS Control Organization (NACO) HIV/AIDS epidemiological surveillance and estimation report for the year 2005. 2005 Retrieved from http://www.nacoonline.org 25 October, 2006.
- National AIDS Control Organization (NACO) Monthly updates on AIDS. 2006 (31st August, 2006). Retrieved from http://www.nacoonline.org/facts_reportjuly.htm 25 October, 2006.
- Organista KC, Organista PB. Migrant laborers and AIDS in United States: A review of literature. AIDS Education and Prevention. 1997;9(1):83–93. [PubMed] [Google Scholar]
- World population prospects: The 2002 revision. New York: United Nations; 2003. Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat. [Google Scholar]
- Sachdev P. Sex on campus: A preliminary study of knowledge, attitudes and behaviour of university students in Delhi, India. Journal of Biosocial Science. 1998;30(1):95–105. doi: 10.1017/s0021932098000959. [DOI] [PubMed] [Google Scholar]
- Ubaidullah M. Social vaccine for HIV prevention: A study on truck drivers in South India. Social Work in Health Care. 2004;39(3–4):399–414. doi: 10.1300/j010v39n03_11. [DOI] [PubMed]
- West Bengal State AIDS Prevention & Control Society, India. HIV sentinel surveillance report. 2005