Introduction
Lactic acid bacteria are naturally associated with mucosal surfaces, particularly the gastrointestinal tract, and are also indigenous to food related habitats, including plants, wine, milk and meat. Consumed for centuries, lactic acid bacteria have a long and safe association with humans [1]. Over the past decade, there has been increasing interest in the use of bacteria as mucosal delivery vehicles for vaccine antigens. There are a number of reports of oral vaccine candidates established from genetically modified pathogenic bacteria, such as Salmonella and Listeria [2], [3], [4], [5], [6] or commensal bacteria such as Lactococcus lactis and Lactobacillus species [7], [8], [9], [10]. While both pathogenic and commensal bacteria have advantages and disadvantages as mucosal delivery vehicles, lactic acid bacteria are preferable in terms of safety control and greater public acceptance [8], [11]. Thus, lactic acid bacteria are excellent candidates for the development of safe mucosal delivery vehicles for prophylactic and therapeutic molecules.
Of the lactobacilli strains previously used for vaccine delivery we chose Lactobacillus plantarum because there is evidence that this strain is better than other lactobacilli as a bacterial vector for mucosal vaccination due to its ability to deliver the expressed antigen and to its ability to persist in the gut [12], [13]. We have previously developed a protective oral vaccine for Lyme disease based in OspA-expressing L. plantarum [14]. In addition, we have recently reported that the immune response to OspA-expressing L. plantarum is modulated by the lipid modification of the antigen [15]. In order to determine if this technology can be applied to developing vaccines for other diseases we focused on the Class A select agent, Yersinia pestis. Low calcium response V antigen (LcrV) is a secreted virulence factor and parenteral immunization with recombinant protein protects mice from subcutaneous [16] and aerosol challenge with virulent Y. pestis [17]. The study reported here suggests that this system could be used as a platform technology to develop oral vaccines for multiple diseases.
Materials and Methods
Ethics statement
The procedures involving human blood were approved by the Institutional Review Board (IRB) of the University of Tennessee Health Science Center. The procedures involving mice were approved by the Institutional Animal Care and Use Committee (IACUC) at the University of Tennessee Health Science Center.
Bacterial strains, cell lines and culture conditions
L. plantarum was grown at 30°C in LM medium [1% proteose peptone (w/v), 1% beef extract (w/v), 0.5% yeast extract (w/v), 0.5% lactose (w/v), 9 mM ammonium citrate, 61 mM sodium acetate anhydrous, 0.4 mM magnesium sulfate, 0.3 mM manganese sulfate, 11.2 mM dipotassium phosphate, 0.5% Tween 20 (v/v)], supplemented with 10 μg/ml of chloramphenicol (Cm). T84 human colonic carcinoma epithelial cells were obtained from the American Type Culture Collection (ATCC, CCL-248, Manassas, VA). T84 cells were maintained at 37°C, 5% CO2 in DMEM-F12K medium modified by ATCC, containing 10% FCS, 100 U/ml penicillin and 100 μg/ml streptomycin.
Plasmid construction and characterization of expressed antigens
The wild type lcrV gene was PCR amplified from Yersinia pseudotuberculosis YpIII (pCD1) (kindly provided by James B. Bliska, Stony Brook University, Stony Brook, NY). This strain contains a plasmid with the Yersinia pestis lcrV gene serotype O:3 [18]. Additionally, we generated a synthetic sslcrV gene in which the lcrV gene was PCR amplified downstream of the nucleotide sequence encoding the leader peptide of OspA (Outer surface protein A) from Borrelia burgdorferi. Both wildtype lcrV and sslcrV recombinant genes where cloned into the Lactobacillus expression vector pLac613 to obtain pLac-V and pLac-ssV plasmids, respectively. Expression vectors were then transformed into Lactobacillus plantarum strain 256 to obtain the clones LpV and LpssV, that express the LcrV and ssLcrV antigens, respectively. Protein expression was checked by immunoblot as follows. Recombinant L. plantarum cells were disrupted with a French® press (Thermo Electron Corporation, Milford, MA), supernatants were analyzed on a 12% denaturing polyacrilamide gels and electrotransferred to a polyvinylidene difluoride membrane (PVDF, Millipore, Billerica, MA) for analysis with an LcrV-specific monoclonal antibody (mAb 40.1) [18].
Evaluation of the hydropathicity of antigens
The hydropathic character of LcrV and ssLcrV was predicted using an in silico approach representing a hydropathy plot of the LcrV and ssLcrV protein sequences. We used the FASTA program Kyte Doolittle Hydropathy Plot (http://fasta.bioch.virginia.edu/fasta_www2/fasta_www.cgi?rm=misc1), that is based on the parameters proposed by Kyte & Doolittle [19]. To assess the hydrophobic character of LcrV and ssLcrV expressed by recombinant Lactobacillus, we performed Triton X-114 phase partitioning [20]. L. plantarum cultures were grown overnight at 30 °C, harvested and resuspended to an OD600 of 1.0 in PBS. Bacteria were disrupted with a French® press and the insoluble material (membrane and cell wall) was separated from the cytosol fraction by centrifugation. This cell envelope fraction was suspended in 1 ml of ice-cold 2% Triton X-114 (v/v) in PBS. The fractions were rotated end over end at 4°C for 1 h and were phase-separated by warming the solution for 30 min in a water bath at 37°C followed by centrifugation for 15 min at 25°C. The separated detergent and aqueous phases were each washed three times. The solutions were then rewarmed and recentrifuged as described and the detergent and aqueous phases were collected. Ten (10) μl of each phase was analyzed on 15% denaturing polyacrylamide gels, electrotransferred to PVDF filters, and used for immunoblot analysis. LcrV-specific monoclonal antibody 40.1 (1:100) was used as primary antibody, goat anti-mouse IgG (H+L) conjugated to alkaline phosphatase (1:1,000; Pierce Rockford, IL) was used as secondary antibody and the immunoblot was developed by BCIP/NBT™ (KPL, Washington, DC). The protein bands corresponding to each LcrV antigen were quantified by densitometry using a Multi Image™ Light Cabinet and the AlphaEase™ software (Alpha Innotech Corporation, San Leandro, CA). The results were plotted as a percentage of the total LcrV content for each recombinant Lactobacillus.
Indirect immunofluorescence microscopy
Recombinant Lactobacillus were treated with and without 250 kU/ml of Lysozyme (Lyz) in TGF buffer [100 mM Tris-HCl pH.8, 50 mM glucose, 1% FBS (v/v) (Hyclone, South Logan, UT)] for 30 min. Cells were washed and resuspended in TGF buffer with mAb 40.1 (1:100) for 1 h at room temperature, washed three times with 500 μl TGF buffer and resuspended on 100 μl of the same buffer. Aliquots of 10 μl were placed on slides and air-dried at 37°C for 1 h. Slides were incubated with Alexa Fluor 488-labeled goat anti-mouse IgG antibody (1:250) (Molecular Probes, Invitrogen, Carlsbad, CA) in 100 μl TGF buffer at 23°C for 1 h with intermittent gentle mixing. After incubation, slides were washed three times with TGF buffer and fixed with 4% PBS–buffered formaldehyde (methanol free; Ted Pella Inc., Redding, CA) for an additional 15 min at room temperature. Labeled cells were mounted in VectaShield medium containing 4,6-diamidino-2-phenylindole (DAPI; Vector Laboratories, Burlingame, CA) and visualized using a Zeiss inverted Axiovert 200 motorized microscope and analyzed using the Axiovision 4.3 software.
Live-cell ELISA (lcELISA)
To further investigate the localization of antigens on the Lactobacillus cell envelope, we used an indirect live-cell enzyme-linked immunosorbent assay (lcELISA). Lactobacillus cultures were grown overnight at 30°C, harvested and resuspended to an OD600 of 1.0 in TG buffer [100 mM Tris-HCl pH.8, 50 mM glucose]. For cell wall digestion, 1 ml aliquots were resuspended in TG buffer with or without Lyz (250 kU/ml) for 5 or 45 min at 37°C. Cells were washed twice with TG buffer, resuspended in the same buffer supplemented with 3% BSA (Bovine Serum Albumin, Sigma), and incubated with mAb 40.1 (1:500). Samples were washed twice and incubated for 30 min with goat anti-mouse IgG (H + L) antibodies conjugated to alkaline phosphatase (1:1,000). After an extensive wash, labeled cells were incubated with pNPP Microwell Substrate System (KPL). Microtiter plates were loaded with 100 μl of each cellular suspension, and optical densities were measured at 405 nm by a Spectra MAX plus ELISA reader (Molecular Devices, Sunnyvale, CA).
Intragastric inoculation of recombinant L. plantarum
L. plantarum expressing the target antigen was cultured in LM medium supplemented with 10 μg/ml Cm, and grown at 30°C to an OD600 of 1.0. That is the equivalent of 1×109 cells/ml corresponding to approximately 125 μg of total protein. The cells were harvested by centrifugation at 3000g for 10 min at 4°C and resuspended in 20% glycerol/phosphate buffered salt solution (Gibco, Grand Island, NY) in 1% of the initial volume. Cell suspensions in aliquots of 2 ml were frozen quickly in a dry ice bath and stored at −80°C. Aliquots were thawed at 4°C and 400 μl (4×1010 cells) were placed in a ball-tipped syringe for oral gavage inoculation. Groups of six female BALB/c mice (6–8 week old female, Charles River, Boston, MA) were immunized by intragastric inoculation of 4×1010 Lactobacillus expressing LcrV recombinant antigens. L. plantarum (Lp) was used as control. Mice received the first immunization, twice daily, for 8 days (days 1–4 and 8–11). The mice were bled on day 15 and after resting for two weeks the mice were bled again (day 30). On days 30–33 they received twice daily the 1st oral boost and rested for an additional 2 weeks. On day 50, the mice were bled. On days 51–54 they received twice daily the 2nd oral boost and rested for an additional 2 weeks. On day 70 mice were terminated, and blood, bronchoalveolar lavage (BAL) and vaginal lavage (VL) fluids were collected.
Humoral immune response
Serum, BAL and VL from orally inoculated mice were tested by indirect ELISA for the presence of IgG or IgA to LcrV. Purified recombinant LcrV was coated at 0.5 μg/ml on Nunc MaxiSorp™ flat-bottom ELISA plates (eBioscience, San Diego, CA) and indirect ELISA was performed using serum (1:100), BAL or VL. Anti-mouse IgG (1:1,600), anti-mouse IgG1 (1:2,000), anti-mouse IgG2a (1:2,000) or anti-mouse IgA (1:1,600) horseradish peroxidase-conjugated antibody (Jackson ImmunoResearch, West Grove, PA) was used as secondary antibody.
Generation of Bone Marrow Derived Dendritic Cells (BMDC) and stimulation for cytokine production
Cells were flushed from the femurs and tibias of euthanized BALB/c mice (6–8 week old female) with 10 ml RPMI 1640 (Gibco, Carlsbad, CA), depleted of red cells using the RBC Lysis Buffer (eBioscience Inc., San Diego, CA) and filtered through a 70-mm cell strainer. The cells were then plated in Petri dishes in RPMI 1640 supplemented with 10% FBS, 42.9 mM 2-mercaptoethanol, 100 U/ml penicillin, 100 μg/ml streptomycin, 200 mM L-glutamine, MEM non-essential amino acids (complete RPMI) and 20 ng/ml mouse recombinant GM-CSF (R&D) and were placed at 37°C in a 5% CO2 humidified incubator. On day 3 and 5 of culture, 10 ml of complete RPMI medium with 20 ng/ml GM-CSF was added to each dish. On day 7, nonadherent cells were harvested and washed with PBS at 4°C. Bone Marrow Derived Dendritic Cells (BMDC) were isolated using mouse CD11c MicroBeads (Miltenyi Biotech, Auburn, CA) according to the manufacturer's recommendations, yielding populations that were greater than 95% pure CD11c+ dendritic cells, as assessed by Flow Cytometry. Cell viability (greater than 95%) was determined by trypan blue exclusion. 1×106 BMDC/well were plated in 24-well tissue culture plates in 2 ml of complete RPMI supplemented with 20 ng/ml of mouse GM-CSF. Cells were co-cultured with UV-killed recombinant Lactobacillus at MOI 10:1 colony-forming units per cell for 48 h at 37°C. 100 ng/ml of LPS from Escherichia coli O111:B4 and L. plantarum were used as positive and negative control, respectively. Supernatants were collected and mouse TNFα, IL-12 p70, IFNγ and IL-10 cytokines, were quantified by ELISA (Quantikine, R&D Systems). The minimum detectable doses of TNFα, IL-12 p70, IFNγ and IL-10 were 5.1, 2.5, 2 and 4 pg/ml, respectively.
Generation of human Peripheral Blood Mononuclear Cells derived Dendritic Cells (PBMC/DC) and stimulation for cytokine production
Human peripheral blood was collected into heparin vacutainer tubes (BD Bioscience, Franklin Lakes, NJ). Peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll-Paque density gradient centrifugation (GE Healthcare, Uppsala, Sweden). A final suspension was made in RPMI 1640 (Hyclone), supplemented with 10% [v/v] FBS, 100 U/ml penicillin, 100 μg/ml streptomycin, 0.25 μg/ml and fungizone. Cell viability (greater than 95%) was determined by trypan blue exclusion. To derive the monocyte population of the PBMCs into dendritic cells (PBMC/DC) we cultured 1×106 cells/well in 24-well tissue culture plates for 5 days in 2 ml of complete RPMI 1640 supplemented with 10 ng/ml IL-4, and 100 ng/ml recombinant human granulocyte-macrophage colony-stimulating factor (GM-CSF) (R&D system, Minneapolis, MN). Cultures were placed at 37°C in a 5% CO2 humidified incubator. Every two days the medium was removed and 2 ml of fresh complete medium was added. On day 5, the cells were co-cultured with UV-killed recombinant Lactobacillus at MOI 10:1 colony-forming units per cell for 48 h at 37°C. 100 ng/ml of lipopolysaccharide (LPS) from Escherichia coli O111:B4 (LIST Biological Laboratories, Campbell, CA) and L. plantarum were used as positive and negative control, respectively. Supernatants were collected and human TNFα, IL-12, IFNγ, IL-6 and IL-10, were quantified by ELISA (Quantikine, R&D Systems). The minimum detectable doses of TNFα, IL-12, IFNγ, IL-10 and IL-6 were 1.6, 5, 8, 3.9 and 0.7 pg/ml, respectively.
IL-8 production by human epithelial cells
T84 cells (human colon carcinoma epithelial cell line) were seeded in 24-well tissue culture plates (BD Biosciences, San Jose, CA) at a density of 1×106 cells/well and grown until they reached 90 to 95% confluence. L. plantarum cells were killed by exposure to UV light for 1 h and the lack of cell viability was confirmed by culture in MRS agar. T84 cells were co-cultured with UV-killed recombinant L. plantarum at a MOI 10:1 bacteria per cell (1×107 CFU/well), for 48 h. L. plantarum control and 0.5 μg/ml TNFα were used as negative and positive controls, respectively. Supernatants were collected and the human IL-8 production was measured by ELISA (Quantikine, R&D Systems, Minneapolis, MN).
Statistical Analysis
All data is represented as mean ± standard deviation. Statistical analyses were performed using Student's t-test. p<0.05 are considered statistically significant.
Results
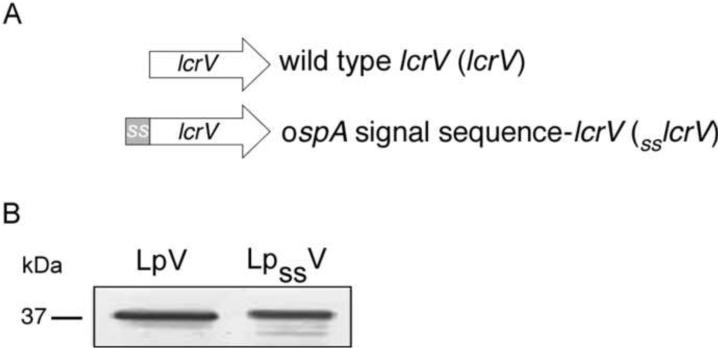
Construction of L. plantarum expressing LcrV. Evaluation of protein hydrophobicity and export
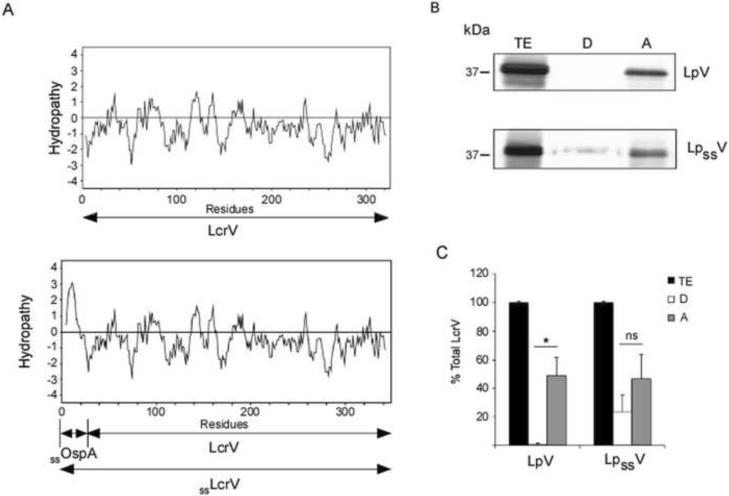
We have previously developed an effective oral vaccine for Lyme disease based on Lactobacillus plantarum expressing the outer surface protein A (OspA) of B. burgdorferi [14]. Recently, we reported that the immune response to Lactobacillus plantarum expressing OspA is modulated by the lipid modification of the antigen [15]. With the ultimate goal of proving that this system can be used as a platform technology to develop oral vaccines for multiple diseases, we focused on the category A select agent Yersinia pestis. We cloned into a Lactobacillus expression vector the Low calcium response V (lcrV) gene from Yersinia pestis downstream of the signal sequence of ospA, sslcrV. In addition, we generated a clone lacking the signal sequence of ospA, lcrV (Fig. 1A). Total extracts of L. plantarum expressing wildtype LcrV (LpV) or ssLcrV (LpssV) were analyzed by denaturing polyacrylamide gels and protein expression was confirmed using anti-LcrV monoclonal antibody mAb 40.1 (Fig.1B). As expected, LpssV migrates just slightly above LpV (37 kDa) given that it carries the leader peptide of OspA. We further analyzed protein hydrophobicity and evaluated the export of ssLcrV in comparison to the wildtype LcrV (Fig. 2). In silico analysis of LcrV and ssLcrV hydrophaty shows an increase in the hydrophobicity of ssLcrV compared to LcrV, that corresponds to the additional leader peptide of OspA present in the N-terminus of the protein (Fig. 2A). Using Triton X-114 phase partitioning of the cell envelope of Lactobacillus we observed that wildtype LcrV partitions only to the aqueous phase, suggesting that, in addition to being exported, wildtype LcrV is hydrophilic. In contrast, ssLcrV partitions equally between the detergent and aqueous phases, suggesting that the protein is also exported through the membrane and that, addition of the OspA leader peptide to LcrV (ssLcrV) increases the hydrophobicity of ssLcrV compared to wildtype LcrV. Differences between detergent and aqueous phases are significant for LpV (p=0.003) (Fig. 2B and 2C).
Figure 1. Characterization of recombinant Lactobacillus spp.
Schematic representation of the lcrV and ssLcrv recombinant genes (A), and immunoblot characterization of Lactobacillus expressing antigens (B). Whole-cell extract of wildtype LcrV- and ssLcrV- expressing L. plantarum (LpV and LpssV, respectively) were analyzed on a 12% SDS-PAGE, transferred to PVDF membrane and tested with LcrV-specific monoclonal antibody 40.1. Legend: ss: signal sequence of Borrelia burgdorferi ospA gene.
Figure 2. Evaluation of protein hydrophobicity and export.
(A) Hydropathy plot was performed for Lcrv and ssLcrV antigens, based on the parameters proposed by Kyte & Doolittle. (B) Wildtype LcrV- and ssLcrV-expressing L. plantarum were disrupted with a French® press, the insoluble material (cell envelope) was extracted with Triton X-114 and partitioned into detergent and aqueous phases. Protein fractions were analyzed on a SDS-PAGE and tested by immunoblot with LcrV-specific monoclonal antibody 40.1. (C) Protein was quantified by densitometry. The results were plotted as a percentage of the total LcrV content for each recombinant Lactobacillus. TE: total extract; D: detergent phase; A: aqueous phase; wild type LcrV-, and ssLcrV-expressing L. plantarum (LpV, and LpssV, respectively). *p=0.003; ns: not significant.
Localization of recombinant antigens in L. plantarum
Next, we wanted to analyze the localization of the recombinant proteins on the surface of L. plantarum. We incubated live recombinant L. plantarum with and without Lysozyme (Lyz) and we performed both immunofluorescence (IFA) and live-cell ELISA (lcELISA) assays. For immunofluorescence, we performed a 30 min incubation with Lyz after which the cells were washed, incubated with anti-LcrV mAb 40.1 followed by Alexa Fluor 488-labeled goat anti-mouse IgG (1:250). Staining was visualized using a Zeiss inverted Axiovert 200 microscope (Fig. 3A). For lcELISA, we incubated the recombinant L. plantarum with Lyz for 5 and 45 min, the cells were washed and incubated with anti-LcrV mAb 40.1 (Fig. 3B). In both assays, IFA and lcELISA, reactions without Lyz (No Lyz) detect protein that is exposed on the surface of the cell. Therefore, ssLcrV is surface exposed whereas wildtype LcrV is not (Fig. 3A and 3B). Reactions with Lyz digest peptidoglycan releasing the LcrV that is attached to the peptidoglycan layer of the cell wall and expose LcrV that is attached to the membrane (Lyz 30 min, Fig. 3A, or 5 and 45 min, Fig. 3B). Our results indicate that ssLcrV is associated with the peptidoglycan layer of the cell wall and is attached to the membrane whereas wildtype LcrV is not, further confirming that only ssLcrV is exported through the membrane.
Figure 3. Localization of recombinant antigens in L. plantarum.
Localization of the recombinant antigens was studied by Immunofluorescence Assay (IFA) (A) and live-cell ELISA (lcELISA) (B). (A) Live recombinant L. plantarum were treated with or without Lyz for 30 min. After cell wall removal, the cells were incubated with mAb 40.1 followed by Alexa Fluor 488-labeled goat anti-mouse IgG (1:250) antibodies. Immunofluorescence staining was visualized using a Zeiss inverted Axiovert 200 microscope, and the images were acquired using AxioVision software. (B) Live recombinant L. plantarum were treated during 0, 5 or 45 min with Lyz and then subjected to lcELISA using mAb 40.1 and anti-mouse IgG secondary antibody labeled with alkaline phosphatase. The Optical Density at 405 nm (OD405) of the mean endpoint titer was determined. The average of triplicate samples per sample was determined and the error bar indicates standard deviation. *p=0.001. Results are representative of one of three independent experiments.
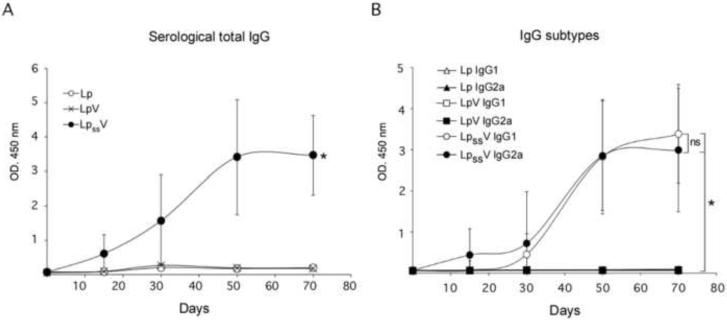
Antibody response to oral administration of recombinant L. plantarum
To assess the systemic and mucosal antibody immune response induced by the oral administration of recombinant L. plantarum, we immunized mice and tested serum levels of LcrV-specific IgG antibodies (Fig. 4), and the levels of mucosal LcrV-specifc IgA in bronchoalveolar lavage (BAL) and vaginal lavage (VL) (Fig. 5), by indirect ELISA.
Figure 4. Antibody response to oral administration of recombinant L. plantarum: serological IgG.
BALB/c mice were inoculated intragastrically with L. plantarum expressing wildtype LcrV (LpV) or ssLcrV (LpssV). Control mice were inoculated with L. plantarum (Lp). Serum samples were collected at days 0, 15, 30, 50 and 70, and specific serological anti-LcrV total IgG antibodies (A) and IgG subtypes IgG1 and IgG2a (B) were measured by indirect ELISA. The results are expressed as Optical Density at 450 nm (OD450). The average of triplicate samples per mouse was determined and the error bar indicates standard deviation. *p=0.001, ns: not significant. n=6 mice per group. Results are representative of one of three independent experiments.
Figure 5. Antibody response to oral administration of recombinant L. plantarum: mucosal IgA.
BALB/c mice were inoculated intragastrically with L. plantarum expressing wild type LcrV (LpV) or ssLcrV (LpssV). Control mice were inoculated with L. plantarum (Lp). Bronchoalveolar lavage (A) and vaginal lavage (B) were collected on day 70 and specific anti-LcrV IgA antibodies were measured by indirect ELISA. The results corresponding to each mouse are expressed as Optical Density at 450 nm (OD450) of the mean endpoint titer. n= 6 mice per group. Results are representative of one of three independent experiments. BAL, Bronchoalveolar Lavage; VL, Vaginal Lavage; ns, not significant. *p=0.008 **p=0.04
Mice orally administered with L. plantarum expressing ssLcrV (LpssV) developed LcrV-specific IgG antibody as early as 15 days after the first inoculation, reaching the highest titers 50 days later and a plateau by day 70. Mice that were inoculated with L. plantarum expressing wildtype LcrV (LpV) did not develop any LcrV-specific IgG antibodies resembling the response obtained by inoculating mice with empty L. plantarum. Differences are statistically significant, p=0.001 (Fig. 4A). In addition, isotyping of LcrV-specific IgG showed that only mice inoculated with L. plantarum expressing ssLcrV (LpssV) produced equivalent amounts of IgG1 and IgG2a (Fig. 4B).
As for determination of LcrV-specific IgA, we observed that mice inoculated with L. plantarum expressing ssLcrV (LpssV) produced significant amounts of LcrV-specific mucosal IgA in the lungs (BAL) and in the vagina (VL). In contrast, mice inoculated with L. plantarum expressing wildtype LcrV (LpV) or with empty L. plantarum (control) did not produce any LcrV-specific IgA antibodies in either the lungs or the vagina (Fig. 5A and 5B). Differences were statistically significant, (p=0.008 and p=0.04, respectively)
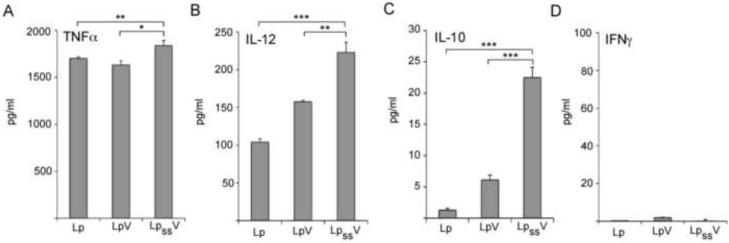
Production of cytokines in mouse Bone Marrow Derived Dendritic Cells co-cultured with recombinant L. plantarum
Dendritic cells (DCs) play a critical role in linking the innate and the adaptive immune responses, since they are specialized antigen-presenting cells capable of stimulating a primary T-lymphocyte response to specific antigen. Bone marrow derived dendritic cells (BMDC) were isolated using CD11c MicroBeads (Miltenyi) and cytokine production was analyzed after stimulation with UV-killed recombinant Lactobacillus. We determined that LpssV induced significantly higher production of proinflammatory cytokine TNFα as compared to LpV (p=0.006) and to the control (Lp, p=0.001); LpssV induced significantly higher production of proinflammatory cytokine IL-12 as compared to LpV (p=0.001) and to the control (Lp, p=0.0001); LpssV induced significantly higher production of anti-inflammatory cytokine IL-10 as compared to LpV (p=0.0001) and to the control (Lp, p=0.0001) (Fig. 6A, 6B and 6C). In contrast, there was no production of IFNγ by BMDC stimulated with either recombinant Lactobacillus or with the control (Fig. 6D).
Figure 6. Production of cytokines in mouse Bone Marrow Derived Dendritic Cells co-cultured with recombinant Lactobacillus.
Cells were flushed from the femur and tibia of BALB/c mice, plated in Petri dishes in complete RPMI 1640 supplemented with 20 ng/ml mouse recombinant GM-CSF and cultured for 7 days. On day 7 non-adherent cells were harvested and Bone Marrow Derived Dendritic Cells (BMDC) were isolated using mouse CD11c MicroBeads (Miltenyi). 1×106 BMDC/well were plated in 24-well tissue culture plates and co-cultured with UV-killed recombinant Lactobacillus expressing wild type LcrV (LpV) or ssLcrV (LpssV) at MOI 10:1 colony-forming units per cell. 100 ng/ml of LPS from Escherichia coli O111:B4 and L. plantarum were used as positive and negative control, respectively. After 48 h supernatants were collected and TNFα (A), IL-12 p70 (B), IL-10 (C) and IFNγ (D) cytokine production was measured by sandwich ELISA (Quantikine). The average of triplicate samples was determined and the error bar indicates standard deviation. Results are representative of one of three independent experiments. *p=0.006, **p=0.001, ***p=0.0001
Production of cytokines in human Peripheral Blood Mononuclear Cells/Dendritic Cells co-cultured with recombinant L. plantarum
In order to further dissect this mechanism we isolated Human Peripheral Blood Mononuclear Cells (PBMCs) and treated with GM-CSF and IL-4 to derive the monocyte population into immature dentritic cells (PBMC/DCs). The treated cells were then co-cultured with UV-killed recombinant L. plantarum expressing either, wildtype LcrV (LpV), ssLcrV (LpssV) or the control (Lp) and the amount of pro-inflammatory cytokines TNFα, IL-12, IFNγ and IL-6, and anti-inflammatory cytokine IL-10 was quantified by ELISA (Fig. 7). As compared to L. plantarum expressing the wildtype LcrV (LpV) or the control, LpssV induced significant amounts of pro-inflammatory cytokines TNFα (p=0.001) IL-12 (p=0.0001), IFNγ (p=0.0001) and IL-6 (p=0.05) and anti-inflammatory cytokine IL-10 (p=0.001) (Fig. 7A, 7B, 7C, 7D and 7E, respectively). LPS was used as a positive control and upregulated secretion of all cytokines tested (data not shown).
Figure 7. Production of cytokines in human PBMC/DCs co-cultured with recombinant Lactobacillus.
Human Peripheral Blood Mononuclear Cells (PBMCs) were treated with 100 nM GM-CSF and 10 nM IL-4 during 5 days to derive monocytes into dendritic cells. 106 cells/well were seed in 24 well plates and co-cultured with UV-killed recombinant Lactobacillus expressing wild type LcrV (LpV) or ssLcrV (LpssV) at MOI 10:1 colony-forming units per cell. 100 ng/ml Escherichia coli O111:B4 lipopolysaccharide (LPS) and L. plantarum (Lp) were used as positive and negative control, respectively. After 48 h of stimulation, supernatants were collected and TNFα (A), IL-12 (B), IFNγ (C), IL-6 (D), and IL-10 (E) cytokine production was measured by sandwich ELISA (Quantikine). The average of triplicate samples was determined and the error bar indicates standard deviation. Results are representative of one of three independent experiments. *p=0.001, **p=0.0001, ***p=0.05
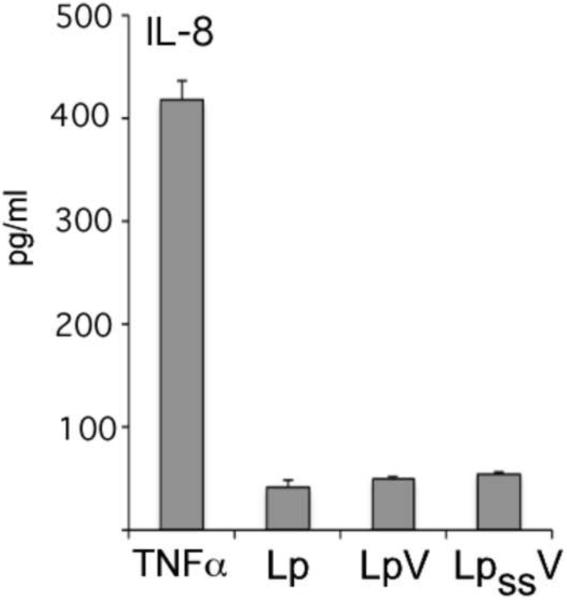
Production of IL-8 in human epithelial cells co-cultured with recombinant L. plantarum
In order to analyze the potential inflammatory response to the oral administration of L. plantarum expressing ssLcrV, we performed an assay using monolayer cultures of intestinal epithelial cells (T84), a human colon carcinoma cell line, stimulated with UV-killed, LpV, LpssV and control (Lp) and determined the production of IL-8 (Fig. 8). The co-culture of T84 cells with UV-killed LpV or LpssV did not induce significant production of the pro-inflammatory chemokine IL-8 in comparison to the negative control (Lp).
Figure 8. Production of IL-8 in human epithelial cells co-cultured with recombinant L. plantarum.
Human epithelial cells (T84) were seeded in 24-well plates (106 cells/well) and grown until they reached about 95% confluence. UV-killed L. plantarum expressing wild type LcrV (LpV) or ssLcrV (***Lp_V) were co-cultured with T84 cells at MOI 10:1 colony-forming units per cell for 48 h and culture supernatants were collected to determine IL-8 secretion by sandwich ELISA (Quantikine). TNFα (0.5 μg/ml) and UV-killed L. plantarum (Lp) were used as positive and negative control, respectively. The average of triplicate samples was determined and the error bar indicates standard deviation. Results are representative of one of three independent experiments.
Discussion
A mucosal delivery system for therapeutic or prophylactic molecules is needed to avoid degradation and promote uptake of the antigen in the gastrointestinal tract and stimulate adaptive immune responses, rather than the tolerogenic responses that are seen in studies done with feeding soluble antigens [1], [21]. In this study we report a second mucosal delivery vehicle using a platform technology previously developed in our laboratory. This novel oral vaccine was developed against Y. pestis and induces production of LcrV-specific systemic IgG as well as local and distant mucosal IgA. In addition, the vaccine polarizes T cells mainly to a Th1 type cellular response, with some involvement of Th2 immunity.
Using the Lyme disease mouse model we immunized mice via oral gavage inoculation with recombinant L. plantarum expressing B. burgdorferi outer surface protein A (OspA), and assessed vaccine efficacy after challenge with B. burgdorferi infected Ixodes ticks. Mice fed OspA-expressing lactobacilli developed a protective systemic IgG response as well as a mucosal local and distant IgA antibody response [14]. Furthermore, we found that recombinant L. plantarum expressing OspA lipoprotein breaks oral tolerance through a combined Th1/Th2 cell mediated immunity and that this delivery system does not induce secretion of pro-inflammatory chemokine IL-8 by epithelial cells [15]. From our initial observations in the Lyme disease mouse model it appears that an effective mucosal vaccine includes antigen expressed in a native form within a microorganism that remains viable and that will allow it to interact with specific components of the mucosal immune system. We assessed these factors by analyzing export and localization of LcrV in the cell envelope of L. plantarum and by evaluating induction of distant mucosal (BAL and VL) IgA production to the vaccine antigen. In addition, we analyzed the systemic IgG antibody and cellular immune responses induced by the vaccine antigen.
Numerous studies have addressed the effect of probiotic bacteria, such as lactobacilli, on immune function [22], [23], [24], [25], [26], [27], [28], [29] [30], [31]. Considering vaccine design, antigen presentation on the surface of lactobacilli is appealing because there is evidence that some strains have a favorable influence on physiologic and pathological processes of the host due to their health promoting characteristics associated with modulation of the immune system [32], [33], [29], [34], [35], [36], [37]. Our recent discovery that the leader peptide of OspA targets the protein to the cell envelope of Lactobacillus and that the Cys17 is recognized by the L. plantarum cell wall sorting machinery that lipidates OspA and releases the protein from the membrane to the outer layer of the cell wall [15], lead us to use this sequence as a signal at the N-terminus of LcrV to mark the protein for translocation across the cytoplasmic membrane of L. plantarum. We constructed two recombinant L. plantarum clones, LsspV expressing LcrV donwstream the leader peptide of OspA (ssLcrV) and LpV expressing LcrV without the OspA leader peptide (LcrV). Hydrophaty analysis and Triton X-114 extraction showed that the protein containing the OspA leader peptide (ssLcrV) is more hydrophobic than LcrV, and that the highly hydrophobic OspA leader peptide could be responsible for the association of the LcrV protein with the membrane. Furthermore, using live-cell ELISA and immunofluorescence assays we determined that only the LcrV that is associated with the leader peptide of OspA (ssLcrV) is presented on the surface of L. plantarum.
Dendritic cells control the delicate balance between Th1 and Th2 immunity, as well as tolerance (Th3) as they are the principal stimulators of naïve T cells [38], [39], [40], [31]. Therefore these cells are pivotal in the initiation of adaptive immune responses and can directly internalize intestinal bacteria [41], [42], [43], [23]. Given that dendritic cells are the front-line antigen presenting cells of the bowel mucosa, we and others [22], reasoned that the way in which these cells react to recombinant Lactobacillus would be pivotal in directing the nature of the adaptive immune response to the expressed antigen. When we stimulated mouse bone marrow derived dendritic (BMDC) cells with Lactobacillus expressing LcrV we observed that both clones induced significant production of the pro-inflammatory cytokine IL-12 as compared to the control, but did not induce any IFNγ. Although significant, production of the anti-inflammatory cytokine IL-10 was about 10 fold lower than that of IL-12. When we stimulated human peripheral blood derived dendritic cells (PBMC/DC) with recombinant Lactobacillus we observed that, in contrast to the control and Lactobacillus expressing wildtype LcrV (LpV), the clone ssLcrV (LpssV) induced significant amounts of pro-inflammatory cytokines TNFα, IL-12, IFNγ and IL-6. This clone also induced significant amounts of anti-inflammatory IL-10. Differences in detection of cytokines in both assays, namely IFNγ, can be explained by the fact that in the former (BMDC) we have a pure population of dendritic cells that do not express IFNγ, and in the later (PBMC/DC) we have a mixed population of monocyte derived dendritic cells, T cells, B cells and NK cells and we expect the production of IFNγ to come from T cells. These data indicate that the mechanism by which LcrV-expressing L. plantarum stimulates the immune response involves polarization to Th1 mediated immunity with some involvement of Th2. Furthermore, localization of the antigen at the cell envelope interface plays an essential role in directing the adaptive immune response that ensues.
Further, dendritic cells can receive tissue conditioning by intestinal epithelial cells that control the dendritic cell inflammatory potential [44], [45], [46], [23]. Therefore, lactobacilli can interact either directly with dendritic cells or indirectly via the action of epithelial cells. The absence of secretion of the pro-inflammatory chemokine IL-8 by human intestinal epithelial cells stimulated with L. plantarum expressing LcrV suggests that a vaccine composed of this agent would not induce local inflammation of the gut.
The ability to promote trafficking of primed cells to other mucosal sites is another important aspect of mucosal immunity. It has become clear that immunization at one mucosal site results in very specific immunity at distinct distant sites (i.e. nasal immunization results in active immunity in the rectum, respiratory and genito-urinary tract) and this process is described as compartmentalization of the mucosal immune system [47]. In our studies we observed that Lactobacillus expressing ssLcrV (LpssV) induced secretion of LcrV-specific IgAs in distant mucosal sites, such as in the lung (BAL) and vagina (VL). In contrast, Lactobacillus expressing wildtype LcrV (LpV) did not induce IgA secretion at these distant mucosal sites. The localization of the antigen in the cell envelope interface of the vaccine delivery vehicle (i. e. Lactobacillus) appears to play a role in this mechanism of compartmentalization.
It is recognized that the normal immune response at mucosal surfaces is one of non-response or tolerance. This is especially true of the intestine where tolerance to commensal flora (1012–1014 bacteria per gram of colonic issue) is the norm and a failure of this tolerant state results in disease [48], [49], [33]. Based on the assumption that a lack of counter-regulatory immune response favors the development of type I allergy, the induction of allergen-specific Th1 responses has been proposed as a promising concept for treatment of Th2-biased hyper-responsiveness [50]. Thus, it is exciting to presume that this technology could be expanded to deliver therapeutic molecules to treat diseases that involve failure of the tolerant states of the intestine, such as IBD, food allergies and celiac disease.
We developed a platform technology to express antigens in the cell envelope of bacteria in the probiotic bacterium Lactobacillus plantarum. We tested our mucosal delivery vehicle using two systems. First, we performed a thorough analysis of an oral vaccine using the Lyme disease mouse model. Expanding the application of our technology to Y. pestis, here we report cloning LcrV, a proven vaccine candidate for plague, in the same mucosal delivery vehicle and analysis of the LcrV-specific humoral and cellular immune response. In both systems, we determined production of systemic IgG and mucosal IgA antibody responses specific to either antigen. Furthermore, mouse and human dendritic cells stimulated with recombinant L. plantarum produced cytokines that polarize T cells to a Th1 type cellular response with some involvement of Th2 immunity. Here we provide evidence that our platform technology can be applied to deliver multiple prophylactic antigens and thus could also be expanded to deliver therapeutic molecules.
Acknowledgments
This study was supported by grants from NIH-NIAID, R44 AI074092 and R43 AI072810 to MGS. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Potential conflicts of interest: The corresponding author (MGS) has a relevant patent and is a major stockholder in Biopeptides, Corp.; RD has a relevant patent and is a major stockholder in Biopeptides, Corp.; JFMLS has a relevant patent and is a major stockholder in Lactrys Biopharmaceuticals BV; BD, JL and VN do not have any potential financial conflict of interest related to this manuscript.
Literature
- [1].Wells JM, Mercenier A. Mucosal delivery of therapeutic and prophylactic molecules using lactic acid bacteria. Nat Rev Microbiol. 2008 May;6(5):349–62. doi: 10.1038/nrmicro1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Anderson R, Dougan G, Roberts M. Delivery of the Pertactin/P.69 polypeptide of Bordetella pertussis using an attenuated Salmonella typhimurium vaccine strain: expression levels and immune response. Vaccine. 1996 Oct;14(14):1384–90. doi: 10.1016/s0264-410x(96)00036-9. [DOI] [PubMed] [Google Scholar]
- [3].Ascon MA, Hone DM, Walters N, Pascual DW. Oral immunization with a Salmonella typhimurium vaccine vector expressing recombinant enterotoxigenic Escherichia coli K99 fimbriae elicits elevated antibody titers for protective immunity. Infect Immun. 1998 Nov;66(11):5470–6. doi: 10.1128/iai.66.11.5470-5476.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kohler JJ, Pathangey L, Hasona A, Progulske-Fox A, Brown TA. Long-term immunological memory induced by recombinant oral Salmonella vaccine vectors. Infect Immun. 2000 Jul;68(7):4370–3. doi: 10.1128/iai.68.7.4370-4373.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Peters C, Peng X, Douven D, Pan ZK, Paterson Y. The induction of HIV Gag-specific CD8+ T cells in the spleen and gut-associated lymphoid tissue by parenteral or mucosal immunization with recombinant Listeria monocytogenes HIV Gag. J Immunol. 2003 May 15;170(10):5176–87. doi: 10.4049/jimmunol.170.10.5176. [DOI] [PubMed] [Google Scholar]
- [6].Shata MT, Reitz MS, Jr., DeVico AL, Lewis GK, Hone DM. Mucosal and systemic HIV-1 Env-specific CD8(+) T-cells develop after intragastric vaccination with a Salmonella Env DNA vaccine vector. Vaccine. 2001 Nov 12;20(3–4):623–9. doi: 10.1016/s0264-410x(01)00330-9. [DOI] [PubMed] [Google Scholar]
- [7].Wu CM, Chung TC. Mice protected by oral immunization with Lactobacillus reuteri secreting fusion protein of Escherichia coli enterotoxin subunit protein. FEMS Immunol Med Microbiol. 2007 Aug;50(3):354–65. doi: 10.1111/j.1574-695X.2007.00255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kajikawa A, Satoh E, Leer RJ, Yamamoto S, Igimi S. Intragastric immunization with recombinant Lactobacillus casei expressing flagellar antigen confers antibody-independent protective immunity against Salmonella enterica serovar Enteritidis. Vaccine. 2007 May 4;25(18):3599–605. doi: 10.1016/j.vaccine.2007.01.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Li YG, Tian FL, Gao FS, Tang XS, Xia C. Immune responses generated by Lactobacillus as a carrier in DNA immunization against foot-and-mouth disease virus. Vaccine. 2007 Jan 15;25(5):902–11. doi: 10.1016/j.vaccine.2006.09.034. [DOI] [PubMed] [Google Scholar]
- [10].Lee JS, Poo H, Han DP, Hong SP, Kim K, Cho MW, et al. Mucosal immunization with surface-displayed severe acute respiratory syndrome coronavirus spike protein on Lactobacillus casei induces neutralizing antibodies in mice. J Virol. 2006 Apr;80(8):4079–87. doi: 10.1128/JVI.80.8.4079-4087.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Pouwels PH, Vriesema A, Martinez B, Tielen FJ, Seegers JF, Leer RJ, et al. Lactobacilli as vehicles for targeting antigens to mucosal tissues by surface exposition of foreign antigens. Methods Enzymol. 2001;336:369–89. doi: 10.1016/s0076-6879(01)36602-8. [DOI] [PubMed] [Google Scholar]
- [12].Shaw DM, Gaerthe B, Leer RJ, Van Der Stap JG, Smittenaar C, Heijne Den Bak-Glashouwer M, et al. Engineering the microflora to vaccinate the mucosa: serum immunoglobulin G responses and activated draining cervical lymph nodes following mucosal application of tetanus toxin fragment C-expressing lactobacilli. Immunology. 2000 Aug;100(4):510–8. doi: 10.1046/j.1365-2567.2000.00069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Grangette C, Muller-Alouf H, Geoffroy M, Goudercourt D, Turneer M, Mercenier A. Protection against tetanus toxin after intragastric administration of two recombinant lactic acid bacteria: impact of strain viability and in vivo persistence. Vaccine. 2002 Sep 10;20(27–28):3304–9. doi: 10.1016/s0264-410x(02)00301-8. [DOI] [PubMed] [Google Scholar]
- [14].del Rio B, Dattwyler RJ, Aroso M, Neves V, Meirelles L, Seegers JF, et al. Oral immunization with recombinant lactobacillus plantarum induces a protective immune response in mice with Lyme disease. Clin Vaccine Immunol. 2008 Sep;15(9):1429–35. doi: 10.1128/CVI.00169-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Del Rio B, Seegers JFML, Gomes-Solecki, M. Immune response to Lactobacillus plantarum expressing Borrelia burgdorferi OspA is modulated by the lipid modification of the antigen. PloS One. 2010 Jun;5(6):e11199. doi: 10.1371/journal.pone.0011199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Leary SE, Williamson ED, Griffin KF, Russell P, Eley SM, Titball RW. Active immunization with recombinant V antigen from Yersinia pestis protects mice against plague. Infect Immun. 1995 Aug;63(8):2854–8. doi: 10.1128/iai.63.8.2854-2858.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Alpar HO, Eyles JE, Williamson ED, Somavarapu S. Intranasal vaccination against plague, tetanus and diphtheria. Adv Drug Deliv Rev. 2001 Sep 23;51(1–3):173–201. doi: 10.1016/s0169-409x(01)00166-1. [DOI] [PubMed] [Google Scholar]
- [18].Gomes-Solecki MJ, Savitt AG, Rowehl R, Glass JD, Bliska JB, Dattwyler RJ. LcrV capture enzyme-linked immunosorbent assay for detection of Yersinia pestis from human samples. Clin Diagn Lab Immunol. 2005 Feb;12(2):339–46. doi: 10.1128/CDLI.12.2.339-346.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kyte J, Doolittle RF. A simple method for displaying the hydropathic character of a protein. J Mol Biol. 1982 May 5;157(1):105–32. doi: 10.1016/0022-2836(82)90515-0. [DOI] [PubMed] [Google Scholar]
- [20].Radolf JD, Chamberlain NR, Clausell A, Norgard MV. Identification and localization of integral membrane proteins of virulent Treponema pallidum subsp. pallidum by phase partitioning with the nonionic detergent triton X-114. Infect Immun. 1988 Feb;56(2):490–8. doi: 10.1128/iai.56.2.490-498.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Neutra MR, Kozlowski PA. Mucosal vaccines: the promise and the challenge. Nat Rev Immunol. 2006 Feb;6(2):148–58. doi: 10.1038/nri1777. [DOI] [PubMed] [Google Scholar]
- [22].Livingston M, Loach D, Wilson M, Tannock GW, Baird M. Gut commensal Lactobacillus reuteri 100-23 stimulates an immunoregulatory response. Immunol Cell Biol. Jan;88(1):99–102. doi: 10.1038/icb.2009.71. [DOI] [PubMed] [Google Scholar]
- [23].Mileti E, Matteoli G, Iliev ID, Rescigno M. Comparison of the immunomodulatory properties of three probiotic strains of Lactobacilli using complex culture systems: prediction for in vivo efficacy. PLoS One. 2009;4(9):e7056. doi: 10.1371/journal.pone.0007056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Mohamadzadeh M, Duong T, Hoover T, Klaenhammer TR. Targeting mucosal dendritic cells with microbial antigens from probiotic lactic acid bacteria. Expert Rev Vaccines. 2008 Mar;7(2):163–74. doi: 10.1586/14760584.7.2.163. [DOI] [PubMed] [Google Scholar]
- [25].Kanzato H, Fujiwara S, Ise W, Kaminogawa S, Sato R, Hachimura S. Lactobacillus acidophilus strain L-92 induces apoptosis of antigen-stimulated T cells by modulating dendritic cell function. Immunobiology. 2008;213(5):399–408. doi: 10.1016/j.imbio.2007.10.001. [DOI] [PubMed] [Google Scholar]
- [26].Chuang L, Wu KG, Pai C, Hsieh PS, Tsai JJ, Yen JH, et al. Heat-killed cells of lactobacilli skew the immune response toward T helper 1 polarization in mouse splenocytes and dendritic cell-treated T cells. J Agric Food Chem. 2007 Dec 26;55(26):11080–6. doi: 10.1021/jf071786o. [DOI] [PubMed] [Google Scholar]
- [27].O'Mahony L, O'Callaghan L, McCarthy J, Shilling D, Scully P, Sibartie S, et al. Differential cytokine response from dendritic cells to commensal and pathogenic bacteria in different lymphoid compartments in humans. Am J Physiol Gastrointest Liver Physiol. 2006 Apr;290(4):G839–45. doi: 10.1152/ajpgi.00112.2005. [DOI] [PubMed] [Google Scholar]
- [28].Smits HH, Engering A, van der Kleij D, de Jong EC, Schipper K, van Capel TM, et al. Selective probiotic bacteria induce IL-10-producing regulatory T cells in vitro by modulating dendritic cell function through dendritic cell-specific intercellular adhesion molecule 3-grabbing nonintegrin. J Allergy Clin Immunol. 2005 Jun;115(6):1260–7. doi: 10.1016/j.jaci.2005.03.036. [DOI] [PubMed] [Google Scholar]
- [29].Mohamadzadeh M, Olson S, Kalina WV, Ruthel G, Demmin GL, Warfield KL, et al. Lactobacilli activate human dendritic cells that skew T cells toward T helper 1 polarization. Proc Natl Acad Sci U S A. 2005 Feb 22;102(8):2880–5. doi: 10.1073/pnas.0500098102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hart AL, Lammers K, Brigidi P, Vitali B, Rizzello F, Gionchetti P, et al. Modulation of human dendritic cell phenotype and function by probiotic bacteria. Gut. 2004 Nov;53(11):1602–9. doi: 10.1136/gut.2003.037325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Christensen HR, Frokiaer H, Pestka JJ. Lactobacilli differentially modulate expression of cytokines and maturation surface markers in murine dendritic cells. J Immunol. 2002 Jan 1;168(1):171–8. doi: 10.4049/jimmunol.168.1.171. [DOI] [PubMed] [Google Scholar]
- [32].Erickson KL, Hubbard NE. Probiotic immunomodulation in health and disease. J Nutr. 2000 Feb;130(2S Suppl):403S–9S. doi: 10.1093/jn/130.2.403S. [DOI] [PubMed] [Google Scholar]
- [33].Macpherson AJ, Harris NL. Interactions between commensal intestinal bacteria and the immune system. Nat Rev Immunol. 2004 Jun;4(6):478–85. doi: 10.1038/nri1373. [DOI] [PubMed] [Google Scholar]
- [34].Perdigon G, Alvarez S, Pesce de Ruiz Holgado A. Immunoadjuvant activity of oral Lactobacillus casei: influence of dose on the secretory immune response and protective capacity in intestinal infections. J Dairy Res. 1991 Nov;58(4):485–96. doi: 10.1017/s0022029900030090. [DOI] [PubMed] [Google Scholar]
- [35].Link-Amster H, Rochat F, Saudan KY, Mignot O, Aeschlimann JM. Modulation of a specific humoral immune response and changes in intestinal flora mediated through fermented milk intake. FEMS Immunol Med Microbiol. 1994 Nov;10(1):55–63. doi: 10.1111/j.1574-695X.1994.tb00011.x. [DOI] [PubMed] [Google Scholar]
- [36].Pouwels PH, Leer RJ, Boersma WJ. The potential of Lactobacillus as a carrier for oral immunization: development and preliminary characterization of vector systems for targeted delivery of antigens. J Biotechnol. 1996 Jan 26;44(1–3):183–92. doi: 10.1016/0168-1656(95)00140-9. [DOI] [PubMed] [Google Scholar]
- [37].Maassen CB, Laman JD, den Bak-Glashouwer MJ, Tielen FJ, van Holten-Neelen JC, Hoogteijling L, et al. Instruments for oral disease-intervention strategies: recombinant Lactobacillus casei expressing tetanus toxin fragment C for vaccination or myelin proteins for oral tolerance induction in multiple sclerosis. Vaccine. 1999 Apr 23;17(17):2117–28. doi: 10.1016/s0264-410x(99)00010-9. [DOI] [PubMed] [Google Scholar]
- [38].Kalinski P, Hilkens CM, Wierenga EA, Kapsenberg ML. T-cell priming by type-1 and type-2 polarized dendritic cells: the concept of a third signal. Immunol Today. 1999 Dec;20(12):561–7. doi: 10.1016/s0167-5699(99)01547-9. [DOI] [PubMed] [Google Scholar]
- [39].Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998 Mar 19;392(6673):245–52. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- [40].Kronin V, Hochrein H, Shortman K, Kelso A. Regulation of T cell cytokine production by dendritic cells. Immunol Cell Biol. 2000 Jun;78(3):214–23. doi: 10.1046/j.1440-1711.2000.00902.x. [DOI] [PubMed] [Google Scholar]
- [41].Rescigno M, Urbano M, Valzasina B, Francolini M, Rotta G, Bonasio R, et al. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol. 2001 Apr;2(4):361–7. doi: 10.1038/86373. [DOI] [PubMed] [Google Scholar]
- [42].Chieppa M, Rescigno M, Huang AY, Germain RN. Dynamic imaging of dendritic cell extension into the small bowel lumen in response to epithelial cell TLR engagement. J Exp Med. 2006 Dec 25;203(13):2841–52. doi: 10.1084/jem.20061884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Niess JH, Brand S, Gu X, Landsman L, Jung S, McCormick BA, et al. CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science. 2005 Jan 14;307(5707):254–8. doi: 10.1126/science.1102901. [DOI] [PubMed] [Google Scholar]
- [44].Rimoldi M, Chieppa M, Salucci V, Avogadri F, Sonzogni A, Sampietro GM, et al. Intestinal immune homeostasis is regulated by the crosstalk between epithelial cells and dendritic cells. Nat Immunol. 2005 May;6(5):507–14. doi: 10.1038/ni1192. [DOI] [PubMed] [Google Scholar]
- [45].Iliev ID, Mileti E, Matteoli G, Chieppa M, Rescigno M. Intestinal epithelial cells promote colitis-protective regulatory T-cell differentiation through dendritic cell conditioning. Mucosal Immunol. 2009 Jul;2(4):340–50. doi: 10.1038/mi.2009.13. [DOI] [PubMed] [Google Scholar]
- [46].Iliev ID, Spadoni I, Mileti E, Matteoli G, Sonzogni A, Sampietro GM, et al. Human intestinal epithelial cells promote the differentiation of tolerogenic dendritic cells. Gut. 2009 Nov;58(11):1481–9. doi: 10.1136/gut.2008.175166. [DOI] [PubMed] [Google Scholar]
- [47].Macpherson AJ, Uhr T. Compartmentalization of the mucosal immune responses to commensal intestinal bacteria. Ann N Y Acad Sci. 2004 Dec;1029:36–43. doi: 10.1196/annals.1309.005. [DOI] [PubMed] [Google Scholar]
- [48].Mowat AM. Anatomical basis of tolerance and immunity to intestinal antigens. Nat Rev Immunol. 2003 Apr;3(4):331–41. doi: 10.1038/nri1057. [DOI] [PubMed] [Google Scholar]
- [49].Sansonetti PJ. War and peace at mucosal surfaces. Nat Rev Immunol. 2004 Dec;4(12):953–64. doi: 10.1038/nri1499. [DOI] [PubMed] [Google Scholar]
- [50].Daniel C, Repa A, Wild C, Pollak A, Pot B, Breiteneder H, et al. Modulation of allergic immune responses by mucosal application of recombinant lactic acid bacteria producing the major birch pollen allergen Bet v 1. Allergy. 2006 Jul;61(7):812–9. doi: 10.1111/j.1398-9995.2006.01071.x. [DOI] [PubMed] [Google Scholar]