Abstract
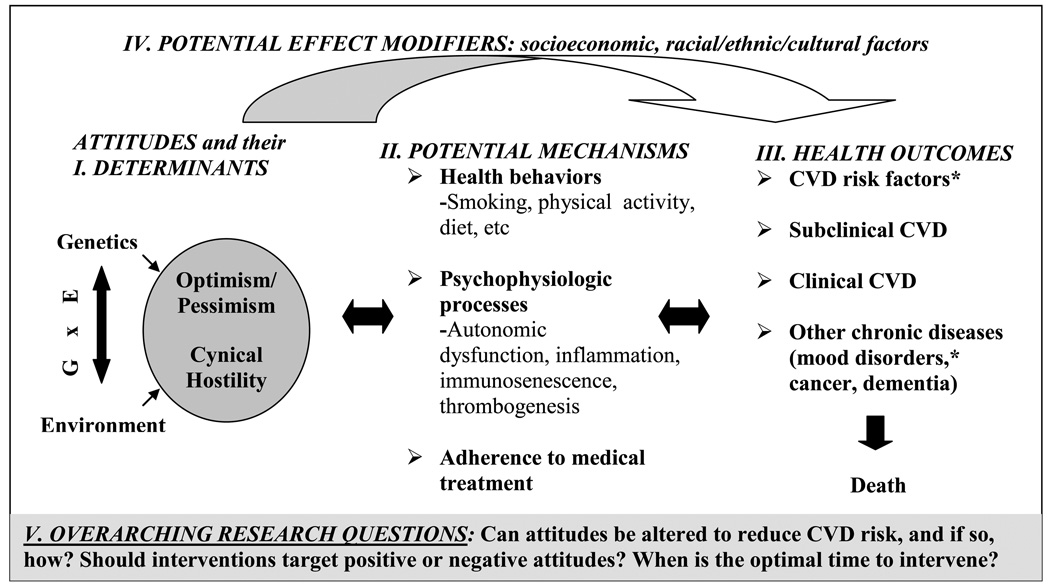
Psychological attitudes are prospectively related to cardiovascular disease (CVD), but a causal relationship has not been demonstrated. Trait optimism/pessimism (positive or negative future expectation, respectively), and cynical hostility (mistrust of people), are attitudes with features of personality traits. These attitudes may affect CVD risk in several ways, by influencing an individual’s 1) adoption of health behaviors, 2) maladaptive stress responding resulting in direct alteration of physiology (i.e., autonomic dysfunction, thrombosis, arrhythmias), 3) development of traditional CVD risk factors, and 4) lack of adherence to therapy in both primary and secondary prevention. More adaptive attitudes may favorably influence CVD risk at each of these critical junctures. The genetic and environmental (i.e., social, economic, racial/ethnic) determinants of attitudes have not been extensively studied. In addition, it is important to understand how some of these environmental determinants may also moderate the association between attitudes and CVD. Clinical trials to modify attitudes for CVD risk reduction (either by reducing negative attitudes or by increasing positive attitudes) are difficult to conduct, but are necessary to determine whether attitudes can indeed be modified, and if, so, to quantify any CVD-related benefits. To address these questions we present a broad, multidisciplinary research agenda utilizing mixed methods and integrating principles of epidemiology, genetics, psychophysiology, and behavioral medicine over the lifecourse (Figure 1). This overview focuses on attitudes and CVD, but has broader implications for understanding how psychological factors relate to chronic diseases of adulthood.
Keywords: attitudes, optimism, pessimism, cynical hostility, lifecourse, cardiovascular disease (CVD)
Introduction
Over the past few decades, our understanding of the health consequences of psychological factors has broadened to include both the detrimental associations of negative psychological factors (such as depression, anxiety, anger/hostility, acute and chronic stress)(1–5) and the beneficial associations with positive factors, including positive affect and positive attitudes.(6–13) Yet in spite of years of research linking psychological factors to cardiovascular disease (CVD), data on determinants of the relationship between attitudes and CVD remain sparse. This is a critical gap in knowledge, because psychological factors, which form early in life, may influence the pathogenesis of CVD throughout the lifecourse.(14)
Most studies of attitudes and CVD have not adopted a lifecourse approach, nor were they designed to establish a causal relationship. Determining a causal relationship requires a better understanding of the complex ways in which attitudes may directly or indirectly influence CVD pathogenesis. For example, attitudes may affect CVD risk in several ways, by influencing an individual’s 1) adoption of health behaviors, 2) maladaptive stress responding resulting in direct alteration of physiology (i.e., autonomic dysfunction, thrombosis, arrhythmias), 3) development of traditional CVD risk factors, and 4) lack of adherence to therapy in both primary and secondary prevention. We present in Figure 1 a novel, testable conceptual framework for examining the role of attitudes in the pathogenesis of CVD over the lifecourse. The framework integrates research questions and hypotheses from a broad range of disciplines and perspectives. The overarching hypothesis is that attitudes, which orginate in childhood and mature by early adulthood, may ultimately be responsible for a substantial portion of the burden of CVD. It is also conceivable that attitudes are important modifiable targets both for primary and secondary prevention of CVD. Clinical biobehavioral trials, which have been difficult to conduct, are needed to test interventions to change atittudes in an attempt to reduce CVD risk.
Figure 1.
Conceptual Model for Ongoing Research into Attitudes and Health over the Life-course
- *Note that some factors, such as traditional CVD risk factors and mood disorders (e.g., depression), are included under “Health Outcomes” but may also be in the causal pathway between attitudes and disease.
- Bidirectional arrows between sections underscore the potential for bidirectional relationships between attitudes, intermediate factors, and clinical disease.
We will first review a commonly-used definition of attitudes, and then address each domain illustrated in our research framework, including: 1) the genetic and environmental determinants of attitudes, 2) the potential mechanisms by which attitudes may affect CVD, 3) the CVD-related health outcomes (i.e., traditional CVD risk factors, subclinical disease, and clinical disease), 4) factors which may modify the observed associations between attitudes and CVD risk, and 5) research questions relating to whether attitudes can be modified for CVD risk reduction. We then conclude each section with a summary of relevant research opportunities.
Definition of Optimism/Pessimism and Cynical Hostility
Trait optimism/pessimism and cynical hostility are prospectively linked to incident CVD and total mortality. Among post-menopausal women, we found that optimism was associated with a favorable profile, and cynical hostility with an unfavorable profile, of baseline risk factors for CVD and mortality. The relationship between optimism/pessimism and cynical hostility and important health outcomes persisted even after adjustment for these baseline differences. Optimists (vs. pessimists) had a 9% lower risk of coronary heart disease and a 14% lower risk of mortality, while most (vs. least) cynical hostile women showed a trend toward increased incident coronary heart disease, as well as a 16% increased risk of mortality over eight years of follow up.(15)
Measurement of Attitudes
While there are several well-established questionnaires which capture the phenotype of optimism/pessimism and cynical hostility, this overview focuses on the Life Orientation Test-Revised(16) and the Cook Medley cynicism subscale.(17) These scales have been studied both separately and together in relation to CVD-related outcomes in men and women. The Life Orientation Test-Revised (LOT-R)(16) measures optimism/pessimism and contains six items. Item ratings are summed to yield a total score ranging from 6 to 30 (higher scores indicating greater optimism, lower scores indicating greater pessimism). The LOT-R also features subscales for optimism (higher scores indicate higher optimism) and pessimism (higher scores indicate higher pessimism). The cynicism subscale of the Cook-Medley Questionnaire(17) contains 13 true/false items (higher scores indicate greater cynical hostility.)
Conceptual Framework for Researching Attitudes and CVD over the Life-course
I. Genetic and Environmental Determinants of Attitudes
Debate still continues over the determinants of attitudes (Figure 1, Section I). Data from the study of twins suggest that the heritability for optimism and pessimism is moderate.(18) Plomin and colleagues investigated optimism and pessimism subscores (as assessed by the subscales of the LOT-R) among pairs of monozygotic and dizygotic twins reared together and apart. Averages of heritability estimates were 24% for optimism and 29% for pessimism. Genome-wide association studies(GWAS) of neuroticism(19, 20) and other personality traits in the five-dimension model of personality (extraversion, agreeableness, conscientiousness, neuroticism, and openness)(21) have revealed that the few areas of statistically significant genotypic variation (i.e., single nucleotide polymorphisms (SNPs)) explained only a small percentage of phenotypic variation in personality. Together, these findings suggest that multiple genetic loci may each contribute a small degree to personality, and underscore the need for large sample sizes in future studies.
Environmental factors, such as aspects of the physical and social environment, may also influence attitudes. For example, our qualitative work enabled us to examine in depth the familial, cultural, and societal contributions to negative attitudes surrounding obesity and weight loss among adult women. Women reported that many of these attitudes developed during childhood.(22) Heinonen et al found that higher pessimism (LOT-R subscale) was associated with childhood socioeconomic status (SES), while higher optimism (LOT-R subscale) was associated with adult SES.(23) Gene-by-environment (G × E) interactions have yielded clearer explanations of how psychological factors influence health outcomes, as in the case of greater vulnerability to depression observed among carriers of the short (s) allele of the serotonin transporter who also experienced early life adversity.(24) Further advances in behavior genetics now consider that determinants of psychological factors such as personality are best “conceptualized as dynamic systems of gene-environment interplay, p. 1485.” (25) Lifecourse studies are critical to understanding these complex interactions.
Research Opportunities
Future GWAS should not only attempt to identify SNPs associated with optimism/pessimism and cynical hostility, but must also investigate potential gene-by-environment interactions. Relevant environmental factors may include measures of socioeconomic status, education, exposure to environmental toxis (i.e., air pollution) and depressive symptoms. Both qualitative and quantitative studies are needed to investigate the relationship of physical, social and cultural environmental factors on the development of attitudes.
II. Potential Mechanisms Linking Attitudes And Health
Available data suggest that multiple mechanisms underlie the relationship between attitudes and health (Figure 1, Section II). Optimism/pessimism and cynical hostility may influence physiology directly and indirectly. Direct mechanisms include activation of stress response systems with resulting alteration of neural, cardiac, endocrine, and immune physiology, which over time may accelerate CVD pathogenesis and/or increase the risk of sudden cardiac death.(26–31) Indirect mechanisms include the adoption and/or maintenance of health behaviors such as smoking, and adherence to medical advice and treatment regimens.(32)
Health Behaviors
Health behaviors (including smoking, diet, and physical activity) only partially explain how attitudes may influence CVD. Highly cynical and pessimistic adult individuals tend to report unhealthy behaviors such as smoking, while optimistic individuals tend to report healthy behaviors such as physical activity.(12, 15) Furthermore, structural equation modeling has shown that childhood personality traits influence smoking behavior, which in turn influences adult health status.(33) This powerful methodology has not yet been extended to include links with clinical CVD outcomes.
Psychophysiologic Processes
Autonomic Dysfunction/HPA Axis
Psychological factors have been shown to be associated with a number of measures of autonomic alterations, underscoring the relationship of optimism and cynical hostility to stress, coping, and social support. For example, compared to pessimists, optimists tend to have healthier social relationships(34) and to cope well with adversity. (35) By contrast, hostility may impair the stress-buffering effects of social support.(36) Over time, these psychophysiologic processes may result in more frequent and/or sustained cardiovascular activation. For example, during ambulatory blood pressure monitoring, optimists, as compared to pessimists, display fewer episodes of stress and negative affect, as well as fewer episodes of elevated blood pressure.(27) Similarly, neural imaging studies demonstrate differential activation of brain regions among optimists, as compared to pessimists,(37) and in hostile as compared to nonhostile individuals.(38) In addition, individuals reporting positive affect and optimism have a lower cortisol awakening response (a marker of HPA axis functioning)(10, 39, 40).
Many studies of risk factors focus on a single measurement in time. However, it is now shown that within-individual variability in physiologic indices (such as non-dipping of blood pressure in the evening, higher nonfasting triglyceride levels, and cardiac autonomic dysfunction), may independently contribute to risk. The association of this within-individual variation with attitudes in response to environmental stressors may be an independent determinant of disease.
Inflammation and Immunosenescence
Studies have demonstrated a link between pessimism and elevated titres of inflammatory markers in combination with shorter telomeres (termed immunosenescence). (41, 42) Such physiologic changes are important to CVD pathogenesis, as low grade chronic inflammation has been associated with increased insulin resistance, reduced pancreatic B-cell function, incident diabetes,(43) and overt CVD (independent of traditional CVD risk factors).(44, 45) (46, 47) Attitudes may also be related to the pathogenesis of CVD via alterations in thrombogenesis (i.e., platelet function, endothelial dysfunction, and activation of clotting factors).(41)
Adherence to Medical Advice
Optimists may adhere to medical advice more readily than pessimists. Tinker et al found that among post-menopausal women who were randomized to a low fat diet, optimists tended to adhere better than pessimists.(32) These findings of lower adherence among pessimists parallel research demonstrating the failure of some depressed individuals to adhere to medical advice and therapy.(48) Failure to adhere to treatment is partially mediated by health beliefs and expectations,(49) and has been described as an “unrecognized cardiac risk factor” leading to poor health outcomes and increased costs.(50) It should be noted that adherence to treatment is only as beneficial as a given treatment. In the age of “evidence-based medicine” it is often tempting to assume that the current standard of care represents the best care, which is not always the case. A classic example is the prescription of bedrest, which was widely recommended for a variety of ailments including acute myocardial infarction, until randomized trials demonstrated the benefit of early mobilization.(51, 52) As treatments evolve, evidence clearly demonstrates the health benefits of adherence to medical advice and therapy,(53) which has become a priority for the United States and other healthcare systems.(54)
Research Opportunities
Prospective qualitative and quantitative data are needed to understand how people with certain attitudes adopt and maintain health behaviors. One important research question would be whether optimists are more likely than pessimists to change behaviors, such as quitting smoking. Understanding the psychobiological mechanisms underlying the pathogenesis of CVD may be best accomplished through a combination of laboratory and “real life” settings combining self-reported and physiologic data. In addition, future research should address how attitudes may influence adherence to treatment and the associated costs.
III. Health Outcomes
Epidemiologic evidence to date supports a relationship between attitudes and health outcomes (Figure 1, Section III). In this framework, we broadly define health outcomes to incorporate traditional CVD risk factors and subclinical and overt CVD. Traditional CVD risk factors are included here to underscore the lifecourse perspective that attitudes may lead to the development of these risk factors during early adulthood and mid-life. Figure 1 also acknowledges the potential relationship of attitudes to other chronic diseases, such as depression, cancer, and dementia, which may be influenced by many of the same processes involved in the pathogenesis of CVD.
CVD Risk Factors
Because most studies of attitudes and CVD have been conducted in older adults, less is known about how attitudes influence the development of CVD risk factors. For example, the association between depressive symptoms, life stress and the metabolic syndrome was only recently understood to be prospective. (55, 56) Hostility has been shown to predict incident hypertension among young adults. This relationship followed a dose-response increase with increasing quantiles of hostility, and was independent of other psychosocial factors. The most (vs. least) hostile adults demonstrated an 84% increased risk of incident hypertension over 15 years of follow up.(57)
Subclinical and Clinical CVD
Attitudes have also been prospectively related to subclinical and clinical CVD. In healthy middle aged women, hostility has been linked to accelerated carotid intima medial thickness (IMT) progression, and optimism to slower rates of IMT progression.(28, 29) Hostility also predicts coronary artery calcification in young adults.(58) These findings provide indirect evidence of a causal relationship between attitudes and subclincal CVD. The considerable evidence for an association between attitudes and overt clinical CVD outcomes has been discussed earlier. Much of the data has focused on coronary heart disease and mortality, with less emphasis on peripheral vascular disease or cerebrovascular disease.
Other Chronic Diseases
Many of the mechanisms proposed to explain CVD outcomes (health behaviors, biological processes, and adherence factors) may be applicable to other chronic health outcomes. For example, evidence suggests that psychological factors such as “distress-prone personalities” may affect the risk of incident cancer, recurrence, and cancer-related death.(5) In our own work in post-menopausal women, atttitudes were associated with cancer-related mortality. Among African-Americans, optimistic (vs. pessimistic) women had a 44% lower risk of dying from cancer. Conversely, the most (vs. least) cynical hostile women showed a 23% higher risk of cancer-related death.(15) Finally, optimism has been prospectively associated with decreased incidence of depression in older adults.(59)
Research Opportunities
More research is needed on how attitudes may influence development of additional CVD risk factors such as diabetes, hypercholesterolemia, and obesity, as well as other measures of subclinical CVD. Epidemiologic studies across the lifecourse are ideally suited to investigate how attitudes affect the multiple steps from CVD risk factors to clinical CVD. Lifecourse studies will also support investigation of possible causal links between attitudes and other chronic illnesses.
IV. Socioeconomic and Racial/ethnic/cultural Factors as Potential Effect Modifiers
Race/ethnicity appears to moderate the relationship between psychological factors and health outcomes. The cultural context in which racial and ethnic constructs exist and are influenced by socioeconomic factors make it easier to understand how cynical attitudes toward others may be both realistic and adaptive in some minority groups with a long history of exposure to discrimination. While hostile or pessimistic cognitions may be an appropriate coping response to an individual’s external reality,(60) there appears to be a physiological cost to such responses.(61–63)
Recently, we observed differences in the association of attitudes and health outcomes between African-American and white post-menopausal women.(15) At baseline, the prevalence of pessimism and cynical hostility was higher in African American as compared to white women. Over eight years of follow up, optimism and cynical hostility were associated with larger effects for total and cancer-related mortality in African-American women. However, the study sample was limited by few highly cynical, hostile white women. As noted above, overt clinical disease and mortality may be influenced heavily by health behaviors, which are themselves influenced by racial and ethnic differences. For example, we found that the cultural origins of negative attitudes surrounding obesity and weight loss experiences differed among African-American and white obese women.(22)
Research Opportunities
Physiological reactions to mental phenomena, such as hostile cognitions, may be more pronounced in African-American or minority individuals relative to whites, thus leading to greater amplitude or longer time course of physiologic responding, which over time facilitates greater disease burden. Psychophysiologic studies of attitudes and stress reactivity across racial/ethnic groups are needed to test this hypothesis. The lifecourse perspective is critical to understand the degree to which socioeconomic, racial/ethnic, and cultural factors shape the relationship between attitudes and health outcomes over time.
V. Conclusion and Future Research Directions
We have presented a research framework (Figure 1) for examining the role of attitudes in the pathogenesis of CVD over the lifecourse, and have proposed a number of research opportunities. Three central questions emerge from this framework: 1) Can attitudes be altered to reduce CVD risk, and if so, how? 2) Should interventions target positive or negative attitudes? 3) When is the optimal time to intervene? To effectively address these questions, lifecourse studies, clinical trials, and psychophysiologic studies should proceed in parallel.
Optimism and hostility, like other psychological factors, may be modifiable with cognitive behavioral therapy.(64, 65) Prior bio-behavioral studies have demonstrated success in treating psychological processes such as Type A behaviors(66) and mental stress(67, 68) with resulting improvements in cardiovascular health, but other bio-behavioral studies of depression and social support(69, 70) did not demonstrate clear improvements. Further research is needed to identify therapies to alter attitudes, and to determine which populations may maximally benefit. These studies urge a broader definition of “behavioral interventions”-- to not only target behaviors, but also the attitudes and beliefs which often preceed them and which may either sabotage or facilitate successful long term behavior change.(49)
Clinically, it is important to understand if adopting less negative attitudes (e.g., becoming less pessimistic) leads to greater risk reduction than adopting more positive ones. Knowing this will allow interventions to be tailored appropriately. Finally, it is unclear when the delivery of interventions to change attitudes may be most effective. For example, are attitudes malleable only up to a certain point in early adulthood? Or would adults who have already suffered CVD events be more receptive to change their attitudes?
In summary, attitudes may represent a largely untapped avenue to prevent and treat CVD. Decades after the introduction of the biopsychosocial model,(71) these attitudes (49) have yet to be integrated into prevention and treatment efforts. Our framework proposes to determine if such integration will ultimately ameliorate the vast public health burden of CVD.
Acknowledgement
Dr. Hilary Tindle would like to acknowledge Drs. Karen Matthews and Michael Scheier for their mentorship in helping refine the conceptual model presented in this manuscript.
Funding
This publication was made possible by Grant Number KL2 RR024154 (Dr. Tindle) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflicts of interest.
Contributor Information
Hilary Tindle, Email: tindleha@upmc.edu, Division of General Internal Medicine, University of Pittsburgh, 230 McKee Place, Suite 600, Pittsburgh, PA 15213, 412-692-6929..
Esa Davis, Email: davism@upmc.edu, Division of General Internal Medicine, University of Pittsburgh, 230 McKee Place, Suite 600, Pittsburgh, PA 15213..
Lewis Kuller, Email: kullerl@edc.pitt.edu, Department of Epidemiology, Graduate School of Public Health, University of Pittsburgh, Pittsburgh, PA 15213..
References
- 1.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999 Apr 27;99(16):2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 2.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005 Mar 1;45(5):637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Matthews KA. Psychological perspectives on the development of coronary heart disease. Am Psychol. 2005 Nov;60(8):783–796. doi: 10.1037/0003-066X.60.8.783. [DOI] [PubMed] [Google Scholar]
- 4.Chida Y, Steptoe A. The Association of Anger and Hostility With Future Coronary Heart Disease: A Meta-Analytic Review of Prospective Evidence. J Am Coll Cardiol. 2009;53(11):936–946. doi: 10.1016/j.jacc.2008.11.044. [DOI] [PubMed] [Google Scholar]
- 5.Chida Y, Hamer M, Wardle J, Steptoe A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nature clinical practice Oncology. 2008 Aug;5(8):466–475. doi: 10.1038/ncponc1134. [DOI] [PubMed] [Google Scholar]
- 6.Tindle HA, Chang Y-F, Kuller LH, Manson JE, Robinson JG, Rosal MC, et al. Optimism, Cynical Hostility, and Incident Coronary Heart Disease and Mortality in the Women's Health Initiative. Circulation. 2009 August 10; doi: 10.1161/CIRCULATIONAHA.108.827642. 2009:CIRCULATIONAHA.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and Physical Health: A Meta-analytic Review. The Society of Behavioral Medicine. 2009 Aug 27;37:239–256. doi: 10.1007/s12160-009-9111-x. 09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008 Sep;70(7):741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 9.Steptoe A, Wardle J. Positive affect and biological function in everyday life. Neurobiol Aging. 2005;26(1) Supplement 1:108–112. doi: 10.1016/j.neurobiolaging.2005.08.016. [doi: DOI: 10.1016/j.neurobiolaging.2005.08.016] [DOI] [PubMed] [Google Scholar]
- 10.Steptoe A, Dockray S, Wardle J. Positive Affect and Psychobiological Processes Relevant to Health. J Pers. 2009:9999. doi: 10.1111/j.1467-6494.2009.00599.x. (9999) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steptoe A, Roux AVD. Happiness, social networks, and health. BMJ. 2008 December 4;:2008. doi: 10.1136/bmj.a2781. 337(dec04_2):a2781- [DOI] [PubMed] [Google Scholar]
- 12.Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S. Dispositional optimism and health behaviour in community-dwelling older people: associations with healthy ageing. Br J Health Psychol. 2006 Feb;11(Pt 1):71–84. doi: 10.1348/135910705X42850. [DOI] [PubMed] [Google Scholar]
- 13.Giltay EJ, Geleijnse JM, Zitman FG, Hoekstra T, Schouten EG. Dispositional Optimism and All-Cause and Cardiovascular Mortality in a Prospective Cohort of Elderly Dutch Men and Women. Arch Gen Psychiatry. 2004 November 1;61(11):1126–1135. doi: 10.1001/archpsyc.61.11.1126. 2004. [DOI] [PubMed] [Google Scholar]
- 14.Hampson SE, Friedman HS. Personality and Health A Lifespan Perspective. In: Oliver P, John RWR, Lawrence A, Pervin, editors. Handbook of Personality: Theory and Research. 3rd edition. New York: New York: Guilford Press; 2008. ed. [Google Scholar]
- 15.Tindle HA, Chang Y-F, Kuller LH, Manson JE, Robinson JG, Rosal MC, et al. Optimism, Cynical Hostility, and Incident Coronary Heart Disease and Mortality in the Women's Health Initiative. Circulation. 2009 August 25;120(8):656–662. doi: 10.1161/CIRCULATIONAHA.108.827642. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994 Dec;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 17.Cook W, Medley D. Proposed hostility and Pharisaic-virtue scales for the MMPI. J Appl Psychol. 1954;38(6):414–418. [Google Scholar]
- 18.Plomin R, Scheier MF, Bergeman CS, Pedersen NL, Nesselroade JR, McClearn GE. Optimism, pessimism and mental health: A twin/adoption analysis. Personality and Individual Differences. 1992;13(8):921–930. [Google Scholar]
- 19.Shifman S, Bhomra A, Smiley S, Wray NR, James MR, Martin NG, et al. A whole genome association study of neuroticism using DNA pooling. Mol Psychiatry. 2008 Mar;13(3):302–312. doi: 10.1038/sj.mp.4002048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wray NR, Middeldorp CM, Birley AJ, Gordon SD, Sullivan PF, Visscher PM, et al. Genome-wide linkage analysis of multiple measures of neuroticism of 2 large cohorts from Australia and the Netherlands. Arch Gen Psychiatry. 2008 Jun;65(6):649–658. doi: 10.1001/archpsyc.65.6.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Terracciano A, Sanna S, Uda M, Deiana B, Usala G, Busonero F, et al. Genome-wide association scan for five major dimensions of personality. Mol Psychiatry. 2008 Oct 28; doi: 10.1038/mp.2008.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis EM, Clark JM, Carrese JA, Gary TL, Cooper LA. Racial and Socioeconomic Differences in the Weight-Loss Experiences of Obese Women. Am J Public Health. 2005 September 1;95(9):1539–1543. doi: 10.2105/AJPH.2004.047050. 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heinonen K, Raikkonen K, Matthews KA, Scheier MF, Raitakari OT, Pulkki L, et al. Socioeconomic status in childhood and adulthood: associations with dispositional optimism and pessimism over a 21-year follow-up. J Pers. 2006 Aug;74(4):1111–1126. doi: 10.1111/j.1467-6494.2006.00404.x. [DOI] [PubMed] [Google Scholar]
- 24.Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003 Jul 18;301(5631):386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- 25.Krueger RF, South S, Johnson W, Iacono W. The Heritability of Personality Is Not Always 50%: Gene-Environment Interactions and Correlations Between Personality and Parenting. J Pers. 2008;76(6):1485–1522. doi: 10.1111/j.1467-6494.2008.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cottington E, Matthews K, Talbott E, Kuller L. Environmental events preceding sudden death in women. Psychosom Med. 1980 November 1;42(6):567–574. doi: 10.1097/00006842-198011000-00005. 1980. [DOI] [PubMed] [Google Scholar]
- 27.Raikkonen K, Matthews KA, Flory JD, Owens JF, Gump BB. Effects of optimism, pessimism, and trait anxiety on ambulatory blood pressure and mood during everyday life. J Pers Soc Psychol. 1999 Jan;76(1):104–113. doi: 10.1037//0022-3514.76.1.104. [DOI] [PubMed] [Google Scholar]
- 28.Matthews KA, Raikkonen K, Sutton-Tyrrell K, Kuller LH. Optimistic attitudes protect against progression of carotid atherosclerosis in healthy middle-aged women. Psychosom Med. 2004 Sep–Oct;66(5):640–644. doi: 10.1097/01.psy.0000139999.99756.a5. [DOI] [PubMed] [Google Scholar]
- 29.Matthews KA, Owens JF, Kuller LH, Sutton-Tyrrell K, Jansen-McWilliams L. Are hostility and anxiety associated with carotid atherosclerosis in healthy postmenopausal women? Psychosom Med. 1998 Sep–Oct;60(5):633–638. doi: 10.1097/00006842-199809000-00021. [DOI] [PubMed] [Google Scholar]
- 30.Demaree HA, Harrison DW. Physiological and neuropsychological correlates of hostility. Neuropsychologia. 1997 Oct;35(10):1405–1411. doi: 10.1016/s0028-3932(97)00053-5. [DOI] [PubMed] [Google Scholar]
- 31.Kuller LH, Talbott EO, Robinson C. Environmental and psychosocial determinants of sudden death. Circulation. 1987 Jul;76(1 Pt 2):I177–I185. [PubMed] [Google Scholar]
- 32.Tinker LF, Rosal MC, Young AF, Perri MG, Patterson RE, Van Horn L, et al. Predictors of dietary change and maintenance in the Women's Health Initiative Dietary Modification Trial. J Am Diet Assoc. 2007 Jul;107(7):1155–1166. doi: 10.1016/j.jada.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 33.Hampson SE, Goldberg LR, Vogt TM, Dubanoski JP. Mechanisms by which childhood personality traits influence adult health status: educational attainment and healthy behaviors. Health Psychol. 2007 Jan;26(1):121–125. doi: 10.1037/0278-6133.26.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Srivastava S, McGonigal KM, Richards JM, Butler EA, Gross JJ. Optimism in close relationships: How seeing things in a positive light makes them so. J Pers Soc Psychol. 2006 Jul;91(1):143–153. doi: 10.1037/0022-3514.91.1.143. [DOI] [PubMed] [Google Scholar]
- 35.Scheier MF, Weintraub JK, Carver CS. Coping with stress: divergent strategies of optimists and pessimists. J Pers Soc Psychol. 1986 Dec;51(6):1257–1264. doi: 10.1037//0022-3514.51.6.1257. [DOI] [PubMed] [Google Scholar]
- 36.Chen YY, Gilligan S, Coups EJ, Contrada RJ. Hostility and perceived social support: interactive effects on cardiovascular reactivity to laboratory stressors. Ann Behav Med. 2005 Feb;29(1):37–43. doi: 10.1207/s15324796abm2901_6. [DOI] [PubMed] [Google Scholar]
- 37.Sharot T, Riccardi AM, Raio CM, Phelps EA. Neural mechanisms mediating optimism bias. Nature. 2007;450(7166):102–105. doi: 10.1038/nature06280. [DOI] [PubMed] [Google Scholar]
- 38.Shapiro PA, Sloan RP, Bagiella E, Kuhl JP, Anjilvel S, Mann JJ. Cerebral activation, hostility, and cardiovascular control during mental stress. J Psychosom Res. 2000 Apr–May;48(4–5):485–491. doi: 10.1016/s0022-3999(00)00100-8. [DOI] [PubMed] [Google Scholar]
- 39.Chida Y, Steptoe A. Cortisol awakening response and psychosocial factors: A systematic review and meta-analysis. Biol Psychol. 2008 Oct 30; doi: 10.1016/j.biopsycho.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 40.Lai JC, Evans PD, Ng SH, Chong AM, Siu OT, Chan CL, et al. Optimism, positive affectivity, and salivary cortisol. Br J Health Psychol. 2005 Nov;10(Pt 4):467–484. doi: 10.1348/135910705X26083. [DOI] [PubMed] [Google Scholar]
- 41.Roy B, Diez-Roux AV, Seeman T, Ranjit N, Shea S, Cushman M. Association of Optimism and Pessimism With Inflammation and Hemostasis in the Multi-Ethnic Study of Atherosclerosis (MESA) Psychosom Med. 2010 February 1;72(2):134–140. doi: 10.1097/PSY.0b013e3181cb981b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O'Donovan A, Lin J, Dhabhar FS, Wolkowitz O, Tillie JM, Blackburn E, et al. Pessimism correlates with leukocyte telomere shortness and elevated interleukin-6 in post-menopausal women. Brain Behav Immun. 2009;23(4):446–449. doi: 10.1016/j.bbi.2008.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu S, Tinker L, Song Y, Rifai N, Bonds DE, Cook NR, et al. A prospective study of inflammatory cytokines and diabetes mellitus in a multiethnic cohort of postmenopausal women. Arch Intern Med. 2007 Aug 13–27;167(15):1676–1685. doi: 10.1001/archinte.167.15.1676. [DOI] [PubMed] [Google Scholar]
- 44.Rutter MK, Meigs JB, Sullivan LM, D'Agostino RB, Sr, Wilson PWF. C-Reactive Protein, the Metabolic Syndrome, and Prediction of Cardiovascular Events in the Framingham Offspring Study. Circulation. 2004 July 27;110(4):380–385. doi: 10.1161/01.CIR.0000136581.59584.0E. 2004. [DOI] [PubMed] [Google Scholar]
- 45.Ridker PM, Buring JE, Cook NR, Rifai N. C-Reactive Protein, the Metabolic Syndrome, and Risk of Incident Cardiovascular Events: An 8-Year Follow-Up of 14 719 Initially Healthy American Women. Circulation. 2003 January 28;107(3):391–397. doi: 10.1161/01.cir.0000055014.62083.05. 2003. [DOI] [PubMed] [Google Scholar]
- 46.Pai JK, Pischon T, Ma J, Manson JE, Hankinson SE, Joshipura K, et al. Inflammatory markers and the risk of coronary heart disease in men and women. N Engl J Med. 2004 Dec 16;351(25):2599–2610. doi: 10.1056/NEJMoa040967. [DOI] [PubMed] [Google Scholar]
- 47.Cesari M, Penninx BW, Newman AB, Kritchevsky SB, Nicklas BJ, Sutton-Tyrrell K, et al. Inflammatory markers and onset of cardiovascular events: results from the Health ABC study. Circulation. 2003 Nov 11;108(19):2317–2322. doi: 10.1161/01.CIR.0000097109.90783.FC. [DOI] [PubMed] [Google Scholar]
- 48.DiMatteo MR, Lepper HS, Croghan TW. Depression Is a Risk Factor for Noncompliance With Medical Treatment: Meta-analysis of the Effects of Anxiety and Depression on Patient Adherence. Arch Intern Med. 2000 July 24;160(14):2101–2107. doi: 10.1001/archinte.160.14.2101. 2000. [DOI] [PubMed] [Google Scholar]
- 49.Glanz K, Rimer BK, FM L. Theory, Research and Practice. WIley & Sons: San Francisco; 2002. Health Behavior and Health Education. [Google Scholar]
- 50.Munger MA, Van Tassell BW, LaFleur J. Medication nonadherence: an unrecognized cardiovascular risk factor. MedGenMed. 2007;9(3):58. [PMC free article] [PubMed] [Google Scholar]
- 51.Abraham AS, Sever Y, Weinstein M, Dollberg M, Menczel J. Value of early ambulation in patients with and without complications after acute myocardial infarction. N Engl J Med. 1975 Apr 3;292(14):719–722. doi: 10.1056/NEJM197504032921403. [DOI] [PubMed] [Google Scholar]
- 52.EARLY MOBILISATION AFTER UNCOMPLICATED MYOCARDIAL INFARCTION. Prospective Study of 538 Patients. The Lancet. 1973;302(7825):346–349. [PubMed] [Google Scholar]
- 53.Osterberg L, Blaschke T. Adherence to Medication. N Engl J Med. 2005 August 4;353(5):487–497. doi: 10.1056/NEJMra050100. 2005. [DOI] [PubMed] [Google Scholar]
- 54.Cutler DM, Everett W. Thinking Outside the Pillbox -- Medication Adherence as a Priority for Health Care Reform. N Engl J Med. 2010 April 7; doi: 10.1056/NEJMp1002305. NEJMp1002305. [DOI] [PubMed] [Google Scholar]
- 55.Raikkonen K, Matthews KA, Kuller LH. Depressive Symptoms and Stressful Life Events Predict Metabolic Syndrome Among Middle-Aged Women. Diabetes Care. 2007 April;30(4):872–877. doi: 10.2337/dc06-1857. 2007. [DOI] [PubMed] [Google Scholar]
- 56.Raikkonen K, Matthews KA, Kuller LH. The relationship between psychological risk attributes and the metabolic syndrome in healthy women: Antecedent or consequence? Metabolism. 2002;51(12):1573–1577. doi: 10.1053/meta.2002.36301. [DOI] [PubMed] [Google Scholar]
- 57.Yan LL, Liu K, Matthews KA, Daviglus ML, Ferguson TF, Kiefe CI. Psychosocial factors and risk of hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) study. JAMA. 2003 Oct 22;290(16):2138–2148. doi: 10.1001/jama.290.16.2138. [DOI] [PubMed] [Google Scholar]
- 58.Iribarren C, Sidney S, Bild DE, Liu K, Markovitz JH, Roseman JM, et al. Association of Hostility With Coronary Artery Calcification in Young Adults: The CARDIA Study. JAMA. 2000 May 17;283(19):2546–2551. doi: 10.1001/jama.283.19.2546. 2000. [DOI] [PubMed] [Google Scholar]
- 59.Giltay EJ, Zitman FG, Kromhout D. Dispositional optimism and the risk of depressive symptoms during 15 years of follow-up: the Zutphen Elderly Study. J Affect Disord. 2006 Mar;91(1):45–52. doi: 10.1016/j.jad.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 60.Thomas SA, González-Prendes AA. Powerlessness, Anger, and Stress in African American Women: Implications for Physical and Emotional Health. Health Care Women Int. 2009;30(1):93–113. doi: 10.1080/07399330802523709. [DOI] [PubMed] [Google Scholar]
- 61.McEwen B, Lasley EN. Allostatic load: when protection gives way to damage. Adv Mind Body Med. 2003 Spring;19(1):28–33. [PubMed] [Google Scholar]
- 62.McEwen BS, Mirsky AE. How socioeconomic status may "get under the skin" and affect the heart. Eur Heart J. 2002 Nov;23(22):1727–1728. doi: 10.1053/euhj.2002.3283. [DOI] [PubMed] [Google Scholar]
- 63.McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Horm Behav. 2003 Jan;43(1):2–15. doi: 10.1016/s0018-506x(02)00024-7. [DOI] [PubMed] [Google Scholar]
- 64.Seligman ME, Steen TA, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. Am Psychol. 2005 Jul–Aug;60(5):410–421. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- 65.Seligman ME, Castellon C, Cacciola J, Schulman P, Luborsky L, Ollove M, et al. Explanatory style change during cognitive therapy for unipolar depression. J Abnorm Psychol. 1988;97(1):13–18. doi: 10.1037//0021-843x.97.1.13. [DOI] [PubMed] [Google Scholar]
- 66.Friedman M, Thoresen CE, Gill JJ, Ulmer D, Thompson L, Powell L, et al. Feasibility of altering type A behavior pattern after myocardial infarction. Recurrent Coronary Prevention Project Study: methods, baseline results and preliminary findings. Circulation. 1982 July 1;66(1):83–92. doi: 10.1161/01.cir.66.1.83. 1982. [DOI] [PubMed] [Google Scholar]
- 67.Blumenthal JA, Babyak M, Wei J, O'Connor C, Waugh R, Eisenstein E, et al. Usefulness of psychosocial treatment of mental stress-induced myocardial ischemia in men. Am J Cardiol. 2002 Jan 15;89(2):164–168. doi: 10.1016/s0002-9149(01)02194-4. [DOI] [PubMed] [Google Scholar]
- 68.Blumenthal JA, Sherwood A, Babyak MA, Watkins LL, Waugh R, Georgiades A, et al. Effects of exercise and stress management training on markers of cardiovascular risk in patients with ischemic heart disease: a randomized controlled trial. JAMA. 2005 Apr 6;293(13):1626–1634. doi: 10.1001/jama.293.13.1626. [DOI] [PubMed] [Google Scholar]
- 69.Glassman AH, O'Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT, Jr, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002 Aug 14;288(6):701–709. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 70.Writing Committee for the ENRICHD Investigators. Effects of Treating Depression and Low Perceived Social Support on Clinical Events After Myocardial Infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 2003 June 18;289(23):3106–3116. doi: 10.1001/jama.289.23.3106. 2003. [DOI] [PubMed] [Google Scholar]
- 71.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977 Apr 8;196(4286):129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]