Abstract
Background
Current blood banking practices allow fresh frozen plasma (FFP) to be thawed and then stored for 5 days between 1-6°C. We hypothesized that aged plasma (Day 5 FFP) would be pro-inflammatory to the endothelium compared to fresh plasma (Day 0 FFP).
Materials and Methods
Human pulmonary endothelial cells (PECs) were treated with 1) media, 2) media + lipopolysaccharide (LPS), 3) lactated Ringer’s (LR), 4)LR + LPS, 5) Day 0 FFP, 6)Day 0 FFP + LPS, 7) Day 5 FFP, and 8) Day 5 FFP + LPS. After a 24 hour incubation, the PECs were stained with antibodies for I-CAM, V-CAM, P-selectin, and E-selectin. The cells were subsequently analyzed by flow cytometry.
Results
In both PEC groups treated with FFP and stimulated with LPS, I-CAM, V-CAM, P-selectin and E-selectin were significantly up regulated compared to LR when stimulated by LPS.
Conclusion
FFP at both ages significantly increased expression of four different adhesion molecules compared to LR in PECs. This may represent a possible mechanism for increased leukocyte binding on the endothelium as a result of FFP transfusion.
Background
The advent of damage control resuscitation (DCR) has dramatically changed the way trauma patients are treated.1,2,3 One of the central tenets of DCR is early use of fresh frozen plasma (FFP) in high ratios to packed red blood cells (PRBCs).4,5 While increased survival is associated with implementation of DCR, studies have also demonstrated some potential risks, including multiple organ failure and acute respiratory distress syndrome (ARDS). 6, 7 However, these risks are not demonstrated in some of the larger studies.3,8 Inflammatory complications may be related to the amount of time blood products remain in storage prior to transfusion. Other investigators have demonstrated increased inflammatory gene expression and death associated with stored blood products, especially PRBCs.9, 10 Current blood banking practice allows for thawed plasma to be stored between 1-6°C for up to five days, facilitating its early use. This is based on storage guidelines for PRBCs and preservation of coagulation factors in plasma.11, 12
Acute lung injury is mediated by leukocyte infiltration into alveoli and lung parenchyma. This infiltration is initiated at the endothelial level by interactions between endothelial cells and leukocytes. The first step in leukocyte migration is “rolling”, which occurs between endothelial adhesion molecules P-selectin and E-selectin and their ligands on leukocytes. Next is firm adherence to the endothelial cells, mediated by endothelial I-CAM-1 and V-CAM-1 and their respective ligands on leukocytes (LFA-1, and VLA-4). These adhesions molecules are increasingly expressed in response to various inflammatory stimuli, including tumor necrosis factor-α (TNF-α), iterleukin-1 (IL-1), and lipopolysaccharide (LPS). Considering the association of FFP with transfusion related lung injury (TRALI) and the current practices ongoing in blood banks, we hypothesized that thawed plasma stored for 5 days at 4°C would demonstrate increased pro-inflammatory properties on primary endothelial cells compared to Day 0 plasma or lactated ringers (LR).
Materials and Methods
This in vitro experiment utilized human pulmonary endothelial cells (PECs, PromoCell, Suttgart, Germany). Prior to the experiment the PECs were incubated in fully supplemented endothelial growth media-2 (Lonza, Basel, Switzerland). We defined plasma that is thawed the same day as transfusion as Day 0 FFP and plasma thawed 5 days before transfusion and stored at 4°C (as practiced by blood banks) as Day 5 FFP. FFP was purchased from Gulf Coast Regional Blood Bank Center in Houston, Texas, and the same donor was used for both Day 0 and Day 5 FFP. LR was obtained from Baxter (Deerfield, IL) and contained only the L-isomer. The groups were 1) unsupplemented media, 2) 30% LR, 3) 30% Day 0 FFP, and 4) 30% Day 5 FFP. LR and FFP were added to the same unsupplemented media as the media group. Ten units of Heparin per 1mL of media were also added to each group. These groups were further divided into subgroups that were either to be treated with LPS (Sigma-Aldrich, St. Louis) or not.
200,000 to 400,000 cells (between passages 4-7) were seeded with their respective media and incubated for 2 hours in 6 well plates. At that point the LPS groups were treated with 1 μg/mL of LPS. After a 24 hour incubation the PECs were collected and stained with fluorescent antibodies (BD Biosciences, San Jose, CA) for flow cytometry. Pulmonary cells were analyzed for I-CAM-1, V-CAM-1, p-selectin, and e-selectin. Flow cytometry was run on a BD LSR II (BD Biosciences, San Jose, CA). Data analysis was performed using one-way ANOVA with post hoc Bonferroni contrast on Analyse-it software (Leeds, UK). All cell culture experiments were performed in replicates of five and duplicated twice. P-values of ≤ 0.05 were considered significant.
Results
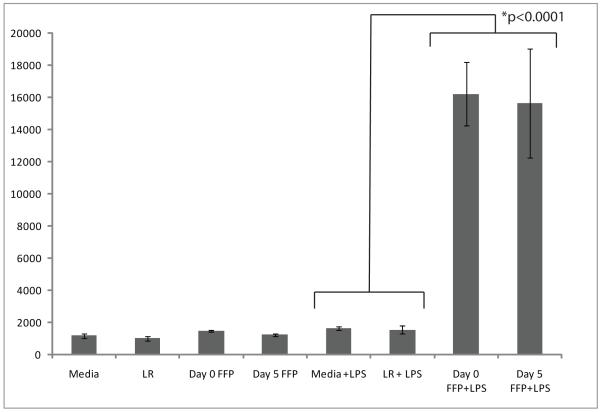
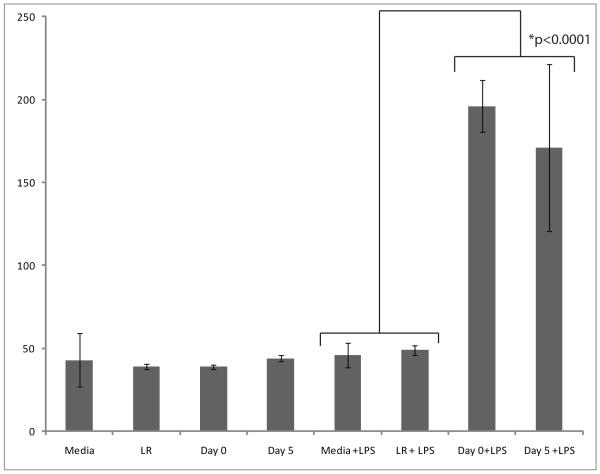
PECs that were incubated with FFP and stimulated with LPS demonstrated increased expression of all adhesion molecules examined when compared to LR and media. Numerical data is presented in Table 1. Expression of I-CAM-1 was increased 10.5 fold (p<0.0001) in the Day 0 FFP + LPS group compared to the LR + LPS group. There was no statistical difference between Day 0 FFP and Day 5 FFP when examining I-CAM-1 (Figure 1). V-CAM-1 was also found to be increased in PECs treated with plasma and LPS. There was a 4.3 fold increase in V-CAM-1 expression when comparing Day 0 FFP to media, and a 4 fold increase compared to LR (p<0.0001) (Figure 2). Again, no differences between the plasma groups were noted.
Table 1.
Median expression of adhesion molecules on PECs
| Media Median (range) |
LR Median (range) |
Day 0 FFP Median (range) |
Day 5 FFP Median (range) |
Media + LPS Median (range) |
LR + LPS Median (range) |
Day 0 FFP +LPS Median (range) |
Day 5 FFP + LPS Median (range) |
|
|---|---|---|---|---|---|---|---|---|
| I-CAM (n=5) | 1163 (946- 1315) |
998 (874- 1245) |
1466 (1374- 1524) |
1222 (1036- 1265) |
1613 (1570- 1825) |
1545 (1148- 1806) |
1624 (13488- 18641) |
15619 (12711- 20020) |
| V-CAM (n=5) | 43 (41-79) | 39 (38-42) | 39 (38-41) | 44 (41-46) | 46 (43-59) | 49 (44-52) | 196 (177- 219) |
171 (83-218) |
| P-selectin (n=5) |
6 (4-7) | 6 (4-6) | 15 (15-17) | 14 (12-17) | 8 (7-8) | 6 (5-6) | 27 (26-30) | 27 (26-32) |
| E-selectin (n=5) |
13 (12-68) | 20 (14-50) | 58 (34-142) | 61 (29-89) | 17 (14-43) | 40 (13-41) | 126 (106- 236) |
132 (91-273) |
Figure 1.
Median I-CAM-1 expression on PECs as quantified by mean fluorescence intensity
Figure 2.
Median expression of V-CAM-1 on PECs as quantified by mean fluorescence intensity
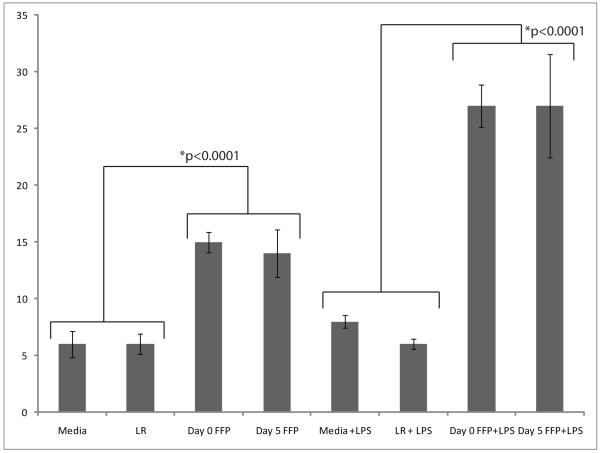
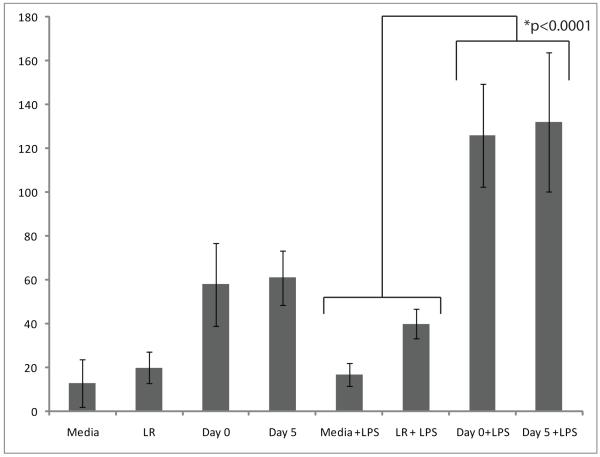
When examining P-selectin, the observed increase in expression of the LPS group was 3.4 fold greater in the Day 0 FFP group compared to media, and 4.5 times when compared to LR (p<0.0001). P-selectin was also increased by plasma (both Day 0 and Day 5) without LPS (p<0.0001). The fold increase in P-selectin expression after treatment with Day 0 FFP to LR and media was 2.5. No differences were observed between Day 0 and Day 5 FFP (Figure 3). Similarly, E-selectin was increased in PECs treated with FFP and stimulated with LPS. Expression of E-selectin was increased by 7.4 times when Day 0 FFP is compared to media, and by 3.15 times when compared to LR (p<0.0001). No differences between Day 0 and Day 5 FFP were observed when examining E-selectin (Figure 4). Though there was a trend of increased expression of E-selectin when contrasting plasma to LR and media without LPS, the differences did not reach statistical significance after ANOVA.
Figure 3.
Median expression of P-selectin on PECs as quantified by mean flourescence intensity
Figure 4.
Median E-selectin expression on PECs as quantified by mean flourescenc intensity.
Discussion
The increased and earlier use of FFP in resuscitation of seriously injured and massively transfused trauma patients has been associated with improved survival when used aggressively with PRBCs. However, some studies have demonstrated an association between multiple organ failure and ARDS and the use of FFP. While these observations have been made, the cellular mechanisms are not well understood.
Previous studies have demonstrated increased inflammation and infectious processes associated with blood product use.13, 14 In both human data and cell culture experiments, PRBCs have been implicated in inflammatory gene expression and increased infection rates.9,13,21 It has been shown that administration of only one unit of PRBCs can have a detrimental effect on surgical patients.15 On the other hand, there are no randomized control trials in trauma patients. While investigations in our laboratory demonstrate endothelial repair activity with Day 0 FPP, these effects diminish over time.16
This study looks to identify one possible mechanism for the observed increased incidence of inflammation amongst patients who receive high ratios of FFP. Our results show that treatment with plasma at both Day 0 and Day 5 time points increases adhesion molecule expression on PECs when compared to treatment with LR or media. Nevertheless, there is no significant difference between the two plasma groups. This suggests that endothelial cells are primed for adhesion of leukocytes and migration with subsequent inflammation irrespective of the age of the plasma transfused.
Conversely, the effects of FFP are pleiotropic. The observed endothelial permeability caused by hypoxia and thrombin after HS may be initially beneficial, leading to the movement of interstitial fluid into the vascular space. However, the ongoing inducement of permeability with iatrogenic resuscitation fluids may contribute to vascular instability, edema, and other detrimental effects of injury and resuscitation. Since we have demonstrated in previous experiments that fresh (Day 0) plasma stabilizes the endothelium, the overall effect may be decreased permeability and an overall benefit, despite increased leukocyte-endothelial binding. The mechanisms and true incidence of potential complications remain obscured.
These observations are also supported by clinical data. Multiple retrospective studies have demonstrated increased survival associated with increased plasma to PRBC ratios. Holcomb et al demonstrated improved survival in 466 massively transfused patients (59.6% vs. 40.1%) for those patients that received high ratios of FFP to PRBCs, and no increased incidence of multiple organ failure or ARDS.3 In another large retrospective study Teixeira and colleagues demonstrated increased mortality (49%) amongst patients who received lower ratios of FFP to PRBCs compared to high ratios (25%).17 High ratios of FFP to PRBCs also were found to benefit patients in New Orleans, with the high ratio group at 87.5% survival and the low ratio group survival at 26%.18
Fewer articles demonstrate no benefit or risk. Scalea et al, demonstrate no survival benefit in their high FFP to PRBC ratio group, although their massive transfusion patients numbered only 81.19 Another paper, from Denver, demonstrated increased risk of multiple organ failure. Using Cox proportional hazard regression, the researchers found a 2.1% increased risk of MOF with every unit of FFP transfused. The risk of ARDS increased 2.5% with each unit of FFP. However, the group also reported that each unit of FFP decreased the risk of mortality by 2.9%.20
This study is limited by its dependence on in vitro experiments, without an in vivo model. Still, the use of LPS (a bacterial product) to induce stress is better suited to a septic model, rather than a HS or injury model. In spite of this, previous studies have used LPS in a two hit model of transfusion related lung injury.21 These in vitro studies are not representative of the complex milieu that exists after injury and hemorrhagic shock. Further cell culture, such as using PRBCs, and animal studies examining the balance between permeability and adhesion will help define this relationship. Other methods of examining variable expression would also increase the validity of these results. In addition, we recognize the rapidly changing activity involved in trauma response. Additional time point collections could elucidate appropriate pathways and associated genes.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Spinella PC, Perkins JG, Grathwol KW, et al. Effect of plasma and red blood cell transfusions on survival in patients with combat related traumatic injuries. J Trauma. 2008;64:S69–S78. doi: 10.1097/TA.0b013e318160ba2f. [DOI] [PubMed] [Google Scholar]
- 2.Borgman MA, Spinella PC, Perkins JG, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63:805–813. doi: 10.1097/TA.0b013e3181271ba3. [DOI] [PubMed] [Google Scholar]
- 3.Holcomb JB, Wade CE, Michalek JE, et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg. 2008;248:447–458. doi: 10.1097/SLA.0b013e318185a9ad. [DOI] [PubMed] [Google Scholar]
- 4.Beekley AC. Damage control resuscitation: a sensible approach to the exsanguinating surgical patient. Crit Care Med. 2008;36:S267–S274. doi: 10.1097/CCM.0b013e31817da7dc. [DOI] [PubMed] [Google Scholar]
- 5.Holcomb JB, Jenkins D, Rhee P, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62:307–310. doi: 10.1097/TA.0b013e3180324124. [DOI] [PubMed] [Google Scholar]
- 6.Watson GA, Sperry JL, Rosengart MR, et al. Fresh frozen plasma is independently associated with a higher risk of multiple organ failure and acute respiratory distress syndrome. J Trauma. 2009;67:221–230. doi: 10.1097/TA.0b013e3181ad5957. [DOI] [PubMed] [Google Scholar]
- 7.Bochicchio GV, Napolitano L, Joshi M, et al. Outcome analysis of blood product transfusion in trauma patients: a prospective, risk-adjusted study. World J Surg. 2008;32:2185–2189. doi: 10.1007/s00268-008-9655-0. [DOI] [PubMed] [Google Scholar]
- 8.Cotton BA, Au BK, Nunez TC, et al. Predefined massive transfusion protocols are associated with a reduction in organ failure and postinjury complications. J Trauma. 2009;66:41–48. doi: 10.1097/TA.0b013e31819313bb. [DOI] [PubMed] [Google Scholar]
- 9.Escobar GA, Cheng AM, Moore EE, et al. Stored packed red blood cell transfusion up-regulates inflammatory gene expression in circulating leukocytes. Ann Surg. 2007;246:129–134. doi: 10.1097/01.sla.0000264507.79859.f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spinella PC, Carroll CL, Staff I, et al. Duration of red blood cell storage is associated with increased incidence of deep vein thrombosis and in hospital mortality in patients with traumatic injuries. Critical Care. 2009;13:R151. doi: 10.1186/cc8050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lamboo M, Poland DC, Eikenboom JC, et al. Coagulation parameters of thawed fresh-frozen plasma during storage at different temperatures. Transfus Med. 2007;17:182–186. doi: 10.1111/j.1365-3148.2007.00729.x. [DOI] [PubMed] [Google Scholar]
- 12.Spinella PC, Holcomb JB. Resuscitation and transfusion principles for traumatic hemorrhagic shock. Blood Rev. 2009 Aug 18; doi: 10.1016/j.blre.2009.07.003. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murrell Z, Haukoos JS, Putnam B, et al. The effect of older blood on mortality, need for ICU care, and the length of ICU stay after major trauma. Am Surg. 2005:71-781–785. doi: 10.1177/000313480507100918. [DOI] [PubMed] [Google Scholar]
- 14.Taylor RW, Manganaro L, O’Brien J, et al. Impact of allogenic packed red blood cell transfusion on nosocomial infection rates in the critically ill patient. Crit Care Med. 2002;30:2249–2254. doi: 10.1097/00003246-200210000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Bernard AC, Davenport DL, Chang PK, et al. Intraoperative transfusion of 1 U to 2 U packed red blood cells is associated with increased 30-day mortality, surgical site infection, pneumonia, and sepsis in general surgery patients. J Am Coll Surg. 2009;208:931–937. doi: 10.1016/j.jamcollsurg.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 16.Pati S, Matijevic N, Doursout MF, et al. The protective effects of day 0 fresh frozen plasma (FFP) on vascular endothelial permeability, coagulation, and resuscitation after hemorrhagic shock are time dependent and diminish between day 0 and day 5. Unpublished results. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teixeira P, Inaba K, Shulman I, et al. Impact of plasma transfusion in massively transfused trauma patients. J Trauma. 2009;66:693–697. doi: 10.1097/TA.0b013e31817e5c77. [DOI] [PubMed] [Google Scholar]
- 18.Duchesne JC, Hunt JP, Wahl G, et al. Review of current blood transfusions strategies in a mature level I trauma center: were we wrong for the last 60 years? J Trauma. 2008;65:272–278. doi: 10.1097/TA.0b013e31817e5166. [DOI] [PubMed] [Google Scholar]
- 19.Scalea TM, Bochicchio KM, Lumpkins K, et al. Early aggressive use of fresh frozen plasma does not improve outcome in critically injured trauma patients. Ann Surg. 2008;248:578–584. doi: 10.1097/SLA.0b013e31818990ed. [DOI] [PubMed] [Google Scholar]
- 20.Kasuk JL, Moore EE, Johnson JL, et al. Postinjury life threatening coagulopathy: Is 1:1 fresh frozen plasma the answer? J Trauma. 2008;65:261–271. doi: 10.1097/TA.0b013e31817de3e1. [DOI] [PubMed] [Google Scholar]
- 21.Kelher MR, Masuno T, Moore EE, et al. Plasma from stored packed red blood cells and MHC class I antibodies causes acute lung injury in a 2-event in vivo rat model. Blood. 2009;113:2079–2087. doi: 10.1182/blood-2008-09-177857. [DOI] [PMC free article] [PubMed] [Google Scholar]