Abstract
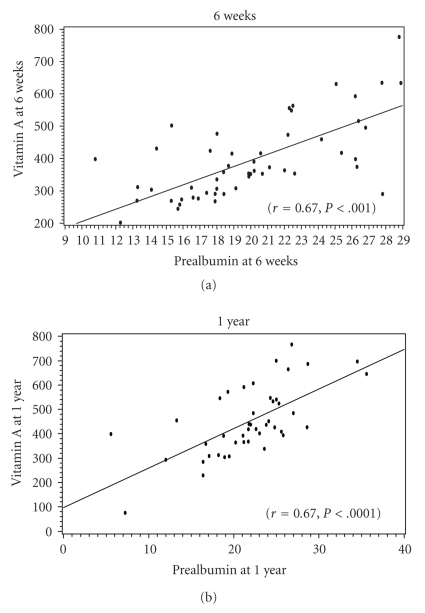
Introduction. Few data are available on vitamin A deficiency in the gastric bypass population. Methods. We performed a retrospective chart review of gastric bypass patients (n = 69, 74% female). The relationship between serum vitamin A concentration and markers of protein metabolism at 6-weeks and 1-year post-operative were assessed. Results. The average weight loss at 6-weeks and 1-year following surgery was 20.1 ± 9.1 kg and 44.1 ± 17.1 kg, respectively. At 6 weeks and 1 year after surgery, 35% and 18% of patients were vitamin A deficient, (<325 mcg/L). Similarly, 34% and 19% had low pre-albumin levels (<18 mg/dL), at these time intervals. Vitamin A directly correlated with pre-albumin levels at 6 weeks (r = 0.67, P < 0.001) and 1-year (r = 0.67, P < 0.0001). There was no correlation between the roux limb length measurement and pre-albumin or vitamin A serum concentrations at these post-operative follow-ups. Vitamin A levels and markers of liver function testing were also unrelated. Conclusion. Vitamin A deficiency is common after bariatric surgery and is associated with a low serum concentration of pre-albumin. This fat-soluble vitamin should be measured in patients who have undergone gastric bypass surgery and deficiency should be suspected in those with evidence of protein-calorie malnutrition.
1. Introduction
Obesity, defined as a body mass index (BMI) ≥ 30 kg/m2, is a chronic disease with major health and economic implications and is recognized as one of the greatest contributors of excessive morbidity and mortality in the 21st century. Approximately 30% of the American population is obese, making it the leading nutritional disorder in our society [1]. This trend has escalated to epidemic proportions with a disproportionate increase in persons with superobesity, defined as those with a BMI ≥ 50 kg/m2.
In 1991, the National Institutes of Health issued a consensus statement concluding that in the morbidly obese, bariatric surgery is the most successful intervention for long-term weight loss [2]. Significant weight loss following bariatric surgery reduces the inherent obesity-specific comorbidities, lowers cardiovascular risk, and provides a survival benefit in this escalating patient population [3, 4]. Weight loss surgery has become increasingly utilized, with greater than 225,000 procedures performed in the United States in 2008 according to the American Society of Metabolic and Bariatric Surgery [5].
Due to the malabsorption induced by the procedure, in conjunction with a reduced gastric volume and alterations in eating behaviors, there is an increased risk of developing certain mineral and vitamin deficiencies. Retinol deficiency is more commonly associated with malabsorptive weight loss surgical interventions, and fewer studies have reported this outcome with Roux-en-Y gastric bypass surgery [6, 7]. Routine postoperative laboratory surveillance at our institution identified a direct recurring coupling of deficiencies of serum retinol and prealbumin concentration; this association has not been previously described in the gastric bypass literature.
2. Methods
We performed a retrospective chart review of 122 obese patients (96 women, 26 men) who underwent Roux-en-Y gastric bypass surgery at William Beaumont Hospital in Royal Oak, Michigan, USA. Fifty-four charts had incomplete data and were excluded from analysis; the remaining 69 subjects served as our study population. The patient population was preapproved for surgery from a multidisciplinary perspective at the William Beaumont Hospital Weight Control Center. The surgeries were performed between October 2005 and July 2007 by two affiliated bariatric surgeons. Data were obtained from William Beaumont Hospital's electronic chart system (One Chart, EPIC systems Corporation) and operative reports.
Serum markers of nutrition were assessed including: prealbumin, albumin, total protein, and retinol. Roux limb measurements were analyzed as a potential mediator of malabsorption, and liver function studies were obtained. Patients were interviewed at baseline and follow-up intervals by our team of bariatric dietitians for nutritional compliance with dietary protein intake. Confidentiality was protected by assigning patients' anonymous numbers, and the study was approved by the hospital's Human Investigation Committee.
3. Postoperative Treatment
Our protocol at the William Beaumont Hospital Weight Loss Center involves regular follow-up outpatient visits at 6 weeks, 3, 6, 9, and 12 months with a multidisciplinary team that includes a dietitian, exercise physiologist, psychologist, and bariatrician. The dietitian works to optimize dietary intake and assess for food intolerances. A comprehensive nutritional intake routinely evaluates macronutrient composition. Routines recommendations include consuming a higher daily intake of lean protein (approximately 1.2 g/kg of ideal body weight), which generally corresponds to 55–80 and 70–110 grams for women and men, respectively. Other important dietary principles include avoidance of excessive sugars (>5 grams per serving), which can promote a Dumping Syndrome, and inclusion of <30% of daily intake from fat per day to avoid steatorrhea. Patients are also counseled to minimize the consumption of partially saturated and hydrogenated fats. We routinely recommend a chewable multivitamin twice daily, calcium citrate 500 mg three times daily with 400 IU of vitamin D, ferrous sulfate 30 mg daily separated by 2 hours from the calcium compound, and 1000 mcg of cyanocobalamin daily to prevent vitamin and mineral deficiencies. Laboratory surveillance of commonly reported mineral and vitamin deficiencies as well as protein levels prompted a tiered response of additional treatments as needed.
4. Statistical Analysis
Demographics and baseline characteristics are reported as means ± standard deviation (SD) or counts with percent frequencies as appropriate. Spearman correlations were completed between weight change and vitamin A levels with all the continuous variables at both 6 weeks and 1 year. Univariate comparisons between patients meeting their protein goal and those that did not were made using either a test for normally distributed data or Wilcoxon rank tests for the outliers. Categorical variables were examined using Pearson's chi-square as appropriate (expected frequency > 5; otherwise Fisher's Exact tests were used). These same tests were completed between patients with and without vitamin A deficiency. Statistical significance was chosen at P ≤ .05. All analyses used The SAS System for Windows version 9.2, Cary, NC.
5. Results
Baseline demographic information of our study population is in Table 1. Weight loss at 6 weeks and 1 year following surgery was 20.1 ± 9.1 kg and 44.1 ± 17.1 kg, respectively (Figure 1(a)). At 6 weeks and 1 year, 35% and 18% of patients were vitamin A deficient (<325 mcg/L). Similarly, 34% and 19% had low prealbumin levels (<18 mg/dL) at these time intervals (Figure 1(b)). Vitamin A directly correlated with prealbumin levels at 6 weeks (r = 0.67, P < .001), and 1-year (r = 0.67, P < .0001). There was no significant correlation between roux length measurement and serum vitamin A concentrations, at 6 weeks and 1 year (r = 0.008 and −0.008, resp.; P = .96 for both). Similarly, the correlations between the roux length and prealbumin concentrations at 6 weeks or 1 year were insignificant (r = −0.08; P = .55 and r = −0.001; P = .99). Achieving dietary protein intake goal, defined as average daily dietary protein intake within 5 grams of intake goal or greater on average, was also not associated with serum levels of vitamin A at 6 weeks or 1 year (P = .41; P = .24, resp.). No significant correlations between vitamin A levels and markers of liver function (aspartate aminotransferase and alanine aminotransferase) were observed at 6 weeks (P = .29, .98, resp.) or at 1 year (P = .34, .99, resp.). Vitamin K assessments were not included in the study methodology and cannot be commented on. We examined the associations between zinc, protein, and vitamin A in various forms and did not identify any significant relationships.
Table 1.
Baseline demographic variables.
| Baseline | |
|---|---|
| Mean age (yrs) | 48.8 ± 12.6 |
| Female (%) | 73.9 |
| Weight (kg) | 64.8 ± 13.2 |
| BMI (kg/m2) | 51.2 ± 9.4 |
| Roux limb length (cm) | 113.6 ± 33.1 |
Figure 1.
6. Discussion
Vitamin A is an essential fat-soluble vitamin absorbed through the small intestine as either retinol (animal derived) or carotene (plant and vegetable derived). Subsequently, it is converted to retinyl palmitate and hydrolyzed to bound retinyl binding protein that transports vitamin A to tissues. Several potential mechanisms may exacerbate vitamin A deficiency in a postoperative gastric bypass patient. First, the deficiency may arise from surgically bypassing the duodenum and first portion of the jejunum, promoting an iatrogenically induced malabsorption. Second, drastic decreases in the dietary intake of many micronutrients like carotenoids and retinol, especially in early recovery, are likely to occur. In addition, traditional dietary recommendations after gastric bypass include a low-fat diet which potentially limit the absorption of fat-soluble vitamins. This patient subset may also be at risk due to confounding nonalcoholic steatohepatitis, higher rates of cirrhosis, or both, which may interfere with maintaining vitamin A storage and production. Finally, higher levels of oxidative stress may also occur after gastric bypass surgery, which can interfere with vitamin A absorption and processing.
Vitamin A deficiency is rarely described in Western society; however, worldwide, it remains the most common etiology of visual disturbances, including blindness. Vitamin A deficiency has been ascribed to a wide variety of ophthalmologic complications including conjunctival and corneal xerosis, keratomalacia, retinopathy, visual loss, and nyctalopia. Moreover, retinol supports photosensitive pigmented cells of the retinal rods and cones that are necessary for optimal visual acuity.
Serum retinol levels and protein-calorie malnutrition have been correlated among children and infants in developing nations. Vitamin A deficient children treated with an augmented dietary protein intake demonstrated an increase in serum protein markers as well as serum retinol levels [8]. In this extreme clinical scenario, retinol deficiency was successfully managed through this dietary intervention alone, without the addition of vitamin A rich foods or vitamin A supplementation [9]. The present findings support the intimate interaction that serum retinol levels have to carrier proteins which determine the bioavailability of serum retinol concentration and reinforce the interdependent relationship of these nutritional markers. As such, total body stores of vitamin A may not be truly deficient; in reality, limited access to nutritional protein binding and transport capacity may underlie these serum retinol findings. These data suggest that addressing the nutritional protein levels is necessary in conjunction with deficient serum retinol concentrations.
There are several case series describing vitamin A deficiency with visual disturbances involving patients who have had gastric or intestinal surgery [6, 7, 10]. None of our patients complained of visual disturbance; however, ocular complaints may have been underreported in the scope of this paper because many clinical features especially early in the course of retinol deficiency can be vague or nonspecific and may not have been recognized as clinically relevant. Additionally, these variables were assessed over a relatively short follow-up interval. It is important to acknowledge this potential complication after bariatric surgery in patients who undergo longstanding iatrogenic malabsorption with limited nutritional protein stores [10] and consider appropriate diagnostic testing and referral for ophthalmologic assessment, when appropriate.
7. Limitations
Our investigation has all the limitations of a small retrospective study. The study cohort was obtained via available data. Accordingly, our population was limited to those patients who were compliant with their baseline evaluation, 1-year follow-up exam and serial laboratory testing. Subjects with missing preoperative or postoperative lab values were excluded from the analysis, which may have biased our study in representing a more compliant subset of patients. Because we captured these data in the scope of clinical management, multivitamin brands and additional retinol supplementation may have varied according to patient preference and our treatment methodology. We also did not account for other potential confounding variables, including physical activity, nutritional compliance, or the duration of supplementation. Accordingly, we are not able to make treatment recommendations for these deficiencies. Nevertheless, vitamin A deficiency is of escalating interest in clinical centers and will likely be the focus of future research. Finally, baseline vitamin A levels were not obtained.
8. Conclusion
We noted a striking, direct relationship between postoperative nutritional protein levels and vitamin A concentrations in our gastric bypass populations. Vitamin A deficiency is common after gastric bypass and is directly associated with a low serum prealbumin concentration, a measure of protein-calorie malnutrition. This fat-soluble vitamin deficiency should be considered in postoperative patients and deficiency should be strongly suspected in those with evidence of protein calorie malnutrition. Improving awareness and understanding of total body vitamin A utilization is of paramount importance in the ongoing medical management of this at-risk population.
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of the American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Gastrointestinal surgery for severe obesity. NIH Consensus Development Conference. 1991;9(1):1–20. [PubMed] [Google Scholar]
- 3.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. Journal of the American Medical Association. 2004;292(14):1724–1737. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 4.Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. New England Journal of Medicine. 2007;357(8):753–761. doi: 10.1056/NEJMoa066603. [DOI] [PubMed] [Google Scholar]
- 5. American Society for Metabolic and Bariatric Surgery (ASMBS) Fact sheet, http://www.asbs.org/Newsite07/media/asmbs_fs_surgery.pdf.
- 6.Chae T, Foroozan R. Vitamin A deficiency in patients with a remote history of intestinal surgery. British Journal of Ophthalmology. 2006;90(8):955–956. doi: 10.1136/bjo.2006.092502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee BW, Hamilton SM, Harris JP, Schwab IR. Occular complications of hypovitaminosis A after bariatric surgery. Ophthalmology. 2005;112:1031–1034. doi: 10.1016/j.ophtha.2004.12.045. [DOI] [PubMed] [Google Scholar]
- 8.Zaklama MS, Gabr MK, El Maraghy S, Patwardhan VN. Serum vitamin A in protein—calorie malnutrition. American Journal of Clinical Nutrition. 1973;26(11):1202–1206. doi: 10.1093/ajcn/26.11.1202. [DOI] [PubMed] [Google Scholar]
- 9.Smith R, Goodman DS, Zaklama MS. Serum vitamin A, retinol binding protein, and prealbumin concentrations in protein calorie malnutrition. I. A functional defect in hepatic retinol release. American Journal of Clinical Nutrition. 1973;26(9):973–981. doi: 10.1093/ajcn/26.9.973. [DOI] [PubMed] [Google Scholar]
- 10.Scopinaro N, Gianetta E, Adami GF, et al. Biliopancreatic diversion for obesity at eighteen years. Surgery. 1996;119(3):261–268. doi: 10.1016/s0039-6060(96)80111-5. [DOI] [PubMed] [Google Scholar]