Abstract
Akt signaling plays a central role in T cell functions, such as proliferation, apoptosis, and regulatory T cell development. Phosphorylation at Ser473 in the hydrophobic motif, along with Thr308 in its activation loop, is considered necessary for Akt function. It is widely accepted that Phosphoinositide-dependent kinase 1 (PDK-1) phosphorylates Akt at Thr308, but the kinase(s) responsible for phosphorylating Akt at Ser473 (PDK-2) remains elusive. The existence of PDK-2 is considered to be specific to cell type and stimulus. PDK-2 in T cells in response to TCR stimulation has not been clearly defined. In this study, we found that conventional PKC positively regulated TCR-induced Akt Ser473 phosphorylation. PKC-alpha purified from T cells can phosphorylate Akt at Ser473 in vitro upon TCR stimulation. Knockdown of PKC-alpha in T cell line Jurkat cells reduced TCR-induced phosphorylation of Akt as well as its downstream targets. Thus our results suggest that PKC-alpha is a candidate for PDK-2 in T cells upon TCR stimulation.
Keywords: Akt, PKC-alpha, TCR, PDK-2
1. Introduction
Akt is a well-characterized effector of phosphoinositide 3-kinase (PI3-K), and has been shown to be involved in a number of biological functions including cell proliferation, differentiation, and survival [1]. Its dysregulation occurs in some human cancers [2–3]. In T cells, Akt can be activated by TCR and/or CD28 signaling, but the underlying mechanism is still unknown. The PI3K/Akt pathway is involved in T cell development, survival and migration, and has been recently implicated in the generation of regulatory T cells which play important roles in peripheral tolerance [4–15]. Understanding the mechanism of Akt regulation in T cells may provide new insights into the pathogenesis of autoimmune and inflammatory diseases.
Akt activation is regulated primarily by phosphorylation at two sites: a conserved threonine residue (Thr308) in the activation loop and a serine residue (Ser473) in the hydrophobic motif (HM) near the COOH terminus. Both residues are conserved among members of the AGC kinase (cAMP dependent, cGMP dependent, and protein kinase C) family [16–18]. Under physiological conditions, the phosphorylation of Thr308 appears to be coordinately regulated with the phosphorylation of Ser473 [19]. Phosphoinositide-dependent kinase 1 (PDK-1), the kinase that phosphorylates the activation loop site Thr308, has been unambiguously identified. However, PDK-2, the kinase that is hypothesized to phosphorylate Ser473, remains elusive. So far, at least 10 kinases have been suggested as an HM kinase or the so-called PDK-2, including mitogen-activated protein (MAP) kinase-activated protein kinase-2 (MK2), integrin-linked kinase (ILK), p38 MAP kinase, protein kinase C-α (PKC-α), PKC-β, the NIMA-related kinase-6 (NEK6), the mammalian target of rapamycin complex 2 (mTORC2), the double-stranded DNA-dependent protein kinase (DNK-PK), and the ataxia telangiectasia mutated (ATM) gene product [16][20–24]. It is generally accepted that PDK-2 is specific to cell type and stimulus. Whether any or all of these kinases act as a physiological Ser473 kinase in T cells remains to be established. Since PKC-β plays the role of PDK-2 in B cells downstream of the BAFF signal [25], we wondered whether PKC(s) plays similar roles in T cells.
In this study, we first found that conventional PKC but not PKC-θ positively regulated TCR-induced Akt phosphorylation. Then, using an in vitro kinase assay, we demonstrated that PKC-α from T cells could phosphorylate Akt in a TCR-dependent way. Finally, we discovered that knockdown of PKC-α in Jurkat cells decreased TCR-induced phosphorylation of Akt as well as its downstream target. Therefore, we domenstrate here that PKC-α serves as the PDK-2 in T cells upon TCR stimulation.
2. Materials and methods
2.1. Mice
All animal experimentation was carried out according to NIH guidelines and was approved by the animal care committee of the University of Chicago. C57BL/6 mice were purchased from The National Cancer Institute (Frederick, MD). PKC-θ−/− mice were purchased from The Jackson Laboratory (Bar Harbor, ME), and have been backcrossed onto the C57BL/6 background for 10 generations. All mice used for experiments were 6 to 10 weeks old.
2.2. Reagents
Purified anti-mouse CD3 (145-2C11), anti-human CD3 (OKT3) and all antibodies used in flow cytometry were purchased from BD PharMingen (San Diego, CA). Donkey anti-mouse secondary antibody was obtained from Sigma (St. Louis, MO). Protein G-Sepharose was purchased from GE Healthcare (Piscataway, NJ). Phospho-antibodies against Akt (Ser473 and Thr308), p70S6K and S6 were purchased from Cell Signaling, Inc. (Danvers, MA). Anti-PKC-α, anti-PKC-β and anti-Akt were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). HRP-conjugated goat anti-rabbit IgG or rabbit anti-mouse IgG were purchased from Kirkegaard & Perry Laboratories (Gaithersburg, MD). Recombinant inactive Akt was obtained from Upstate Biotechnology (Lake Placid, NY). The Cell Line Nucleofector kit V was obtained from Amaxa Biosystems (Cologne, Germany), and siRNAs were bought from Ambion (Austin, TX). Cell culture reagents were purchased from Invitrogen (San Diego, CA). Bisindolylmaleimide I and Gö6976 were bought from Calbiochem (San Diego, CA).
2.3. T cell isolation and activation
Spleen and lymph node T cells from WT (C57BL/6) or PKC-θ−/− mice were purified (purity >98% as determined by FACS analysis of CD3 cell surface expression) on T cell enrichment columns (R&D Systems, Minneapolis, MN). For in vitro acute stimulation, T cells were incubated with anti-CD3 (1 μg/ml) mAb for 30 min on ice, followed by cross-linking with rabbit anti-hamster IgG (5 μg/ml) for the indicated time periods, then lysed. T cell lysates were subjected to Western blot analysis or in vitro kinase assays. For chemical inhibition experiments, T cells were pretreated with pan-PKC inhibitor or selective PKC-α/β inhibitor for 1 hour at 37°C prior to anti-CD3 stimulation.
2.4. Cell culture, transfection and stimulation
Jurkat T cells were purchased from the American Type Culture Collection (Rockville, MD), and maintained in RPMI 1640 supplemented with 10% heat-inactivated fetal bovine serum (FBS), 100 U/ml penicillin-streptomycin, and 2 mM L-glutamine (C medium). Cells were cultured in a density between 0.5×106 to 1.5×106/ml and passaged every 2–3 days. A total of 1×106 Jurkat cells was transfected with 5μM nonsense siRNA or PKCα-siRNA. Nucleofection was carried out according to program X-001 with the Cell Line Nucleofector kit V. The transfected cells were incubated in C medium at 37°C for 48 h, then washed twice with RPMI 1640 and starved in RPMI 1640 at 37°C. After overnight serum starvation, the cells were harvested for stimulation with mouse anti-human anti-CD3 antibody (OKT3; 1μg/ml) followed by cross-linking with donkey anti-mouse secondary antibody (1μg/ml).
2.5. Western blotting
Cells were lysed in RIPA buffer [150 mM NaCl, 100 mM Tris (pH8.0), 0.5% Nonidet P-40, 1% deoxycholicacid, 0.1% SDS, 5 mM EDTA, 10 mM NaF, 1 mM Na3VO4, 2 mM leupeptin, 2 mM aprotinin and 1 mM phenylmethylsulfonylfluoride] and centrifuged at 13,200 rpm for 15 min. Bio-Rad protein assay reagent (Richmond, CA) was used to determine protein concentration. Equal quantities of proteins were separated by SDS-PAGE and transferred onto nitrocellulose membranes. The membranes were blocked for 1 h using 5% milk in Tris buffered saline with 0.1% Tween, then blotted with primary antibodies for 2 h at RT. The membranes were washed three times in TBST (10 min each) and incubated with HRP-conjugated secondary antibodies for 1 h at RT. The membranes were washed three times as above and the specific proteins were visualized with an enhanced chemiluminescence reagent (NEN, Boston, MA). The protein bands were then quantified with Image J software.
2.6. In vitro kinase assay of PKCα/β
T cells were isolated and activated as described above. Immunoprecipitation was performed as described previously [26–28]. In brief, cells were lysed in RIPA buffer and centrifuged at 13,200 rpm for 15 min, and supernatants were transferred to new tubes. Protein concentrations were determined by Bio-Rad protein assay reagent. 500 μg protein in 500μl RIPA buffer was incubated with 3 μg anti-PKCα/β antibody or isotype-matched control immunoglobulin with continuous agitation for 2 h at 4°C, followed by incubation with protein G-agarose for another 2 h at 4°C. Immunoprecipitates recovered by centrifugation were gently washed 3 times with RIPA buffer, then washed twice with PKCα/β kinase buffer containing 25 mM Tris-HCl pH 7.5, 10 mM MgCl2, 0.1 mM Na3VO4, 5 mM β-glycerophosphate, 2 mM dithiothreitol (DTT). Then the immunoprecipitated PKCα/β proteins were incubated with 0.5 μg recombinant inactive Akt and 500 μM ATP in a final volume of 15 μl kinase buffer for 30 min at 37°C. At the end of the reaction, 150 μl SDS loading buffer (×2) was added into each sample. The samples were boiled for 5 min, then resolved by SDS-PAGE, blotted with anti-phospho-Akt (Ser473), and reprobed with anti-PKCα/β as loading control.
3. Results
3.1. Conventional PKC positively regulates TCR-induced phosphorylation of Akt
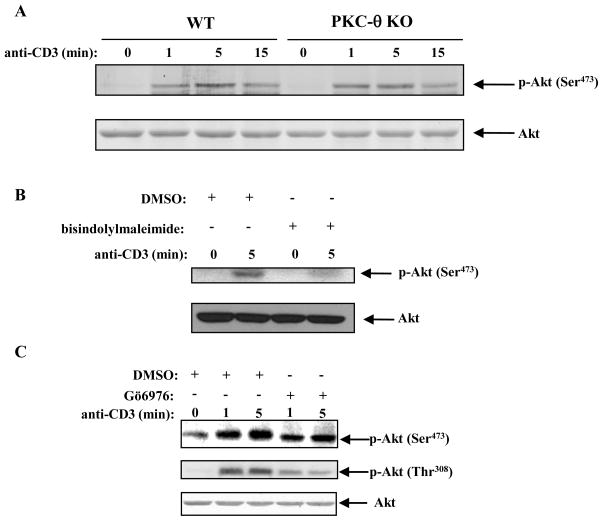
Since it has been shown that PKC-β phosphorylates Akt at Ser473 in B cells [25], we wondered whether PKC(s) played similar roles in T cells. PKC-θ is mainly expressed in T cells and is crucial for T cell activation [29,30], we first explored the possibility that it functioned as the PDK-2 in T cells. T cells isolated from wild-type (WT) or PKC-θ−/− mice were stimulated with anti-CD3, and lysed. The cell lysates were blotted with phospho-antibody against Akt at Ser473. The Western blot showed that PKC-θ deficiency did not impair TCR-induced Akt phosphorylation at Ser473, suggesting that PKC-θ is not the PDK-2 in T cells (Fig. 1A). To further determine whether other PKC isoform(s) function as the PDK-2 in T cells, we pretreated C57BL/6 splenic T cells with bisindolylmaleimide I (BIM), a pan-PKC inhibitor, and then stimulated them with anti-CD3. We found that inhibition of pan-PKC significantly suppressed TCR-induced Akt Ser473 phosphorylation (Fig. 1B). Therefore, our data suggest that other PKC isoform(s), but not PKC-θ, may function as the PDK-2 in T cells. In addition to PKC-θ, several other PKC isoforms are also expressed in T cells. PKC-α, which is highly expressed in T cells, together with PKC-θ, is involved in TCR down-regulation [31]. PKC-α and PKC-θ together have also been shown to activate NF-AT in T cells, which may account for the additive defect in adaptive immunity in PKC-α−/− PKC-θ−/− mice [32]. We next tested whether PKC-α was the PDK-2 in T cells. We employed the specific conventional PKC inhibitor Gö6976, which inhibits both PKC-α and PKC-β [33–35]. Primary T cells were pretreated with Gö6976, then stimulated with anti-CD3 and lysed. The cell lysates were resolved by immunoblotting. As seen in Fig. 1C, inhibition of PKC-α/β significantly inhibited TCR-induced Akt phosphorylation at both Ser473 and Thr308.
Fig. 1.
Conventional PKC positively regulates TCR-induced phosphorylation of Akt. (A) T cells purified from C57BL/6 (B6) or PKC-θ−/− mice were stimulated with anti-CD3 (1μg/ml) for the indicated time points and lysed in RIPA buffer. Proteins were subjected to immunoblotting using a specific phospho-antibody against Akt Ser473. The membrane was stripped and reprobed with anti-Akt. (B) T cells from B6 mice were pretreated with pan-PKC inhibitor BIM (5 μM) for 1 h at 37 °C, then stimulated with anti-CD3 and lysed. Phospho-Akt (Ser473) and total Akt were detected as in (A). (C) T cells purified from B6 mice were pretreated with the selective conventional PKC inhibitor Gö6976 (1 μM) or an equal volume of DMSO at 37°C for 1 h, then stimulated and analyzed as in (A) and (B). Data shown represent one of three independent experiments.
3.2. PKC-α is the PDK-2 responsible for phosphorylating Akt at Ser473 upon TCR stimulation
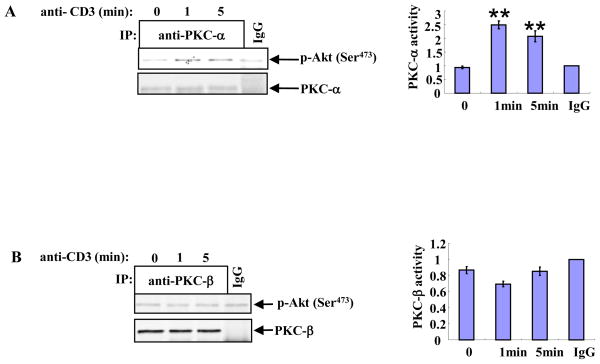
To further confirm the above result, we performed in vitro PKC kinase assays using recombinant Akt as a substrate. Splenic T cells isolated from B6 mice were stimulated with anti-CD3 and lysed. The cell lysates were immunoprecipitated with antibodies against PKC-α or PKC-β. The immunoprecipitated PKC-α or PKC-β proteins were incubated with recombinant inactive Akt in the presence of ATP, and the phosphorylation of Akt at Ser473 was determined. As shown in Fig. 2A, compared with the basal level of Akt Ser473 phosphorylation in the IgG well, PKC-α on its own did not lead to higher Akt phosphorylation. However, after 1 to 5 minutes of TCR stimulation, Akt Ser473 phosphorylation caused by PKC-α increased two-fold. In contrast, PKC-β wasn’t able to phosphorylate Akt at Ser473 in vitro even with TCR stimulation (Fig. 2B). Therefore, our data suggest that PKC-α may be the PDK-2 in T cells in the TCR signaling pathway.
Fig. 2.
PKC-α is the PDK-2 responsible for phosphorylating Akt at Ser473 upon TCR stimulation. T cells isolated from B6 mice were stimulated with anti-CD3 and lysed. PKC-α (A) or PKC-β (B) were immunoprecipitated and in vitro kinase assays were carried out as described in Methods. The phosphorylation of Akt at Ser473 was detected by immunoblotting as described above. The membranes were stripped and reprobed with anti-PKC-α (A) or PKC-β (B). Data shown represent one of four independent experiments. **P<0.01 with respect to the IgG basal level.
3.3. Knockdown of PKC-α in Jurkat cells decreases TCR-induced Akt phosphorylation
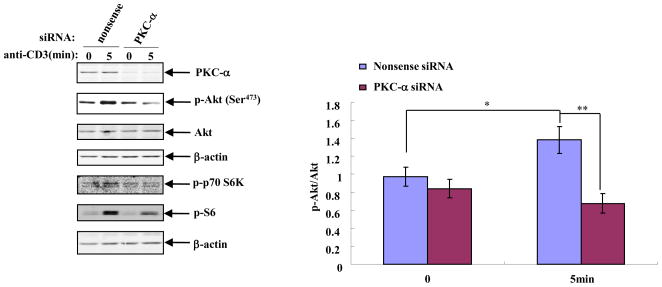
To verify the role of PKC-α in phosphorylating Akt at Ser473 in a more physiological setting, we employed commercial siRNA to decrease the expression level of PKC-α in T-cell-line Jurkat cells. Jurkat cells were transfected with PKC-α or nonsense siRNA, cultured for 3 days, then stimulated with human anti-CD3 for 5 min in vitro. Phospho-Akt was determined by Western blot. TCR-induced Akt phosphorylation was significantly decreased in Jurkat cells expressing lower levels of PKC-α (Fig. 3).
Fig. 3.
Knockdown of PKC-α in Jurkat cells decreases TCR-induced Akt phosphorylation. Jurkat cells were transfected with PKC-α or nonsense siRNA as described in Methods. Forty-eight hours later, the transfected cells were starved in RPMI 1640 overnight, then harvested for stimulation. The cell lysates were resolved by SDS-PAGE, blotted with phospho-antibodies against Akt (Ser473), p70S6K and S6, then reprobed with a loading control. Data shown represent one of four independent experiments. *P<0.05, **P<0.01.
p70S6K is a downstream target of Akt. Activation of Akt leads to the phosphorylation of p70S6K, which participates in the regulation of cell growth and proliferation by phosphorylating and activating its further downstream substrate, S6. As shown in Fig. 3, TCR stimulation increased the phosphorylation of both p70S6K and S6, but reduced PKC-α expression significantly decreased such phosphorylation.
4. Discussion
It has been well documented that Akt phosphorylation at both Ser473 and Thr308 are essential for its full activation [16,36]. The Thr308 kinase PDK-1 has been well defined, but the Ser473 kinase PDK-2 is still controversial and is considered to be specific to cell type and stimulus.
Although it has been suggested that PKC-α acts as the PDK-2 in other cell types [21], its role in Akt Ser473 phosphorylation in T cells is unknown. We tested the role of PKC-α in the phosphorylation of Akt at Ser473 using several approaches. First, using the pan-PKC inhibitor BIM in combination with PKC-θ−/− T cells, we found that other isoform(s) of PKC but not PKC-θ were involved in the regulation of TCR-induced Akt Ser473 phosphorylation (Fig. 1A and 1B). Consistent with this finding, the selective PKC-α/β inhibitor Gö6976 inhibited TCR-induced Akt phosphorylation at Ser473 and Thr308 (Fig. 1C). Further confirmation of the involvement of PKC-α in the regulation of Akt Ser473 phosphorylation came from the in vitro PKC kinase assays using recombinant inactive Akt as a substrate. With this approach, we demonstrated that PKC-α but not PKC-β could phosphorylate Akt at Ser473 in a TCR-dependent manner (Fig. 2A and 2B), which is consistent with other publications [22]. Furthermore, we found that Jurkat cells expressing lower levels of PKC-α displayed defective phosphorylation of Akt at Ser473 upon TCR stimulation (Fig. 3). These data not only indicate that PKC-α is the potential PDK-2 in T cells downstream of TCR stimulation, but also support the notion that phosphorylation of Akt at Ser473 can facilitate the phosphorylation of Akt at Thr308 (Fig. 1C) [16,37].
In conclusion, our data collectively indicate that PKC-α is responsible for TCR-induced phosphorylation of Akt at Ser473. Therefore, PKC-α functions as the PDK-2 in T cells.
Acknowledgments
The project described was supported by the National Natural Science Foundation of China (30872790/H0908 to FY), as well as grants from the National Institutes of Health (NIH) (R01 AI090901-07 to JZ) and from the American Heart Association (09GRNT2010084 to JZ). LY was supported by a Scholarship from the China Scholarship Council of the Ministry of Education of P.R. China ([2007] 3020). JZ is an American Lung Association Career Investigator.
Footnotes
Conflict of interest
The authors declare that we do not have any financial interest related to the work described in this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Manning BD, Cantley LC. AKT/PKB signaling: navigating downstream. Cell. 2007;129:1261–1274. doi: 10.1016/j.cell.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martelli AM, Nyakern M, Tabellini G, Bortul R, Tazzari PL, Evangelisti C, Cocco L. Phosphoinositide 3-kinase/Akt signaling pathway and its therapeutical implications for human acute myeloid leukemia. Leukemia. 2006;20:911–928. doi: 10.1038/sj.leu.2404245. [DOI] [PubMed] [Google Scholar]
- 3.Carnero A, Blanco-Aparicio C, Renner O, Link W, Leal JF. The PTEN/PI3K/AKT signalling pathway in cancer, therapeutic implications. Curr Cancer Drug Targets. 2008;8:187–198. doi: 10.2174/156800908784293659. [DOI] [PubMed] [Google Scholar]
- 4.Webb LM, Vigorito E, Wymann MP, Hirsch E, Turner M. Cutting edge: T cell development requires the combined activities of the p110gamma and p110delta catalytic isoforms of phosphatidylinositol 3-kinase. J Immunol. 2005;175:2783–2787. doi: 10.4049/jimmunol.175.5.2783. [DOI] [PubMed] [Google Scholar]
- 5.Swat W, Montgrain V, Doggett TA, Douangpanya J, Puri K, Vermi W, Diacovo TG. Essential role of PI3Kdelta and PI3Kgamma in thymocyte survival. Blood. 2006;107:2415–2422. doi: 10.1182/blood-2005-08-3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones RG, Parsons M, Bonnard M, Chan VS, Yeh WC, Woodgett JR, Ohashi PS. Protein kinase B regulates T lymphocyte survival, nuclear factor kappaB activation, and Bcl-X(L) levels in vivo. J Exp Med. 2000;191:1721–1734. doi: 10.1084/jem.191.10.1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Juntilla MM, Wofford JA, Birnbaum MJ, Rathmell JC, Koretzky GA. Akt1 and Akt2 are required for alphabeta thymocyte survival and differentiation. Proc Natl Acad Sci USA. 2007;104:12105–12110. doi: 10.1073/pnas.0705285104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fayard E, Gill J, Paolino M, Hynx D, Hollander GA, Hemmings BA. Deletion of PKBalpha/Akt1 affects thymic development. PLoS One. 2007;2:e992. doi: 10.1371/journal.pone.0000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mao C, Tili EG, Dose M, Haks MC, Bear SE, Maroulakou I, Horie K, Gaitanaris GA, Fidanza V, Ludwig T, Wiest DL, Gounari F, Tsichlis PN. Unequal contribution of Akt isoforms in the double-negative to double-positive thymocyte transition. J Immunol. 2007;178:5443–5453. doi: 10.4049/jimmunol.178.9.5443. [DOI] [PubMed] [Google Scholar]
- 10.Fabre S, Carrette F, Chen J, Lang V, Semichon M, Denoyelle C, Lazar V, Cagnard N, Dubart-Kupperschmitt A, Mangeney M, Fruman DA, Bismuth G. FOXO1 regulates L-Selectin and a network of human T cell homing molecules downstream of phosphatidylinositol 3-kinase. J Immunol. 2008;181:2980–2989. doi: 10.4049/jimmunol.181.5.2980. [DOI] [PubMed] [Google Scholar]
- 11.Sinclair LV, Finlay D, Feijoo C, Cornish GH, Gray A, Ager A, Okkenhaug K, Hagenbeek TJ, Spits H, Cantrell DA. Phosphatidylinositol-3-OH kinase and nutrient-sensing mTOR pathways control T lymphocyte trafficking. Nat Immunol. 2008;9:513–521. doi: 10.1038/ni.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carlson CM, Endrizzi BT, Wu J, Ding X, Weinreich MA, Walsh ER, Wani MA, Lingrel JB, Hogquist KA, Jameson SC. Kruppel-like factor 2 regulates thymocyte and T-cell migration. Nature. 2006;442:299–302. doi: 10.1038/nature04882. [DOI] [PubMed] [Google Scholar]
- 13.Sebzda E, Zou Z, Lee JS, Wang T, Kahn ML. Transcription factor KLF2 regulates the migration of naive T cells by restricting chemokine receptor expression patterns. Nat Immunol. 2008;9:292–300. doi: 10.1038/ni1565. [DOI] [PubMed] [Google Scholar]
- 14.Haxhinasto S, Mathis D, Benoist C. The AKT-mTOR axis regulates de novo differentiation of CD4+Foxp3+ cells. J Exp Med. 2008;205:565–574. doi: 10.1084/jem.20071477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sauer S, Bruno L, Hertweck A, Finlay D, Leleu M, Spivakov M, Knight ZA, Cobb BS, Cantrell D, O’Connor E, Shokat KM, Fisher AG, Merkenschlager M. T cell receptor signaling controls Foxp3 expression via PI3K, Akt, and mTOR. Proc Natl Acad Sci USA. 2008;105:7797–7802. doi: 10.1073/pnas.0800928105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dong LQ, Liu F. PDK2: the missing piece in the receptor tyrosine kinase signaling pathway puzzle. Am J Physiol Endocrinol Metab. 2005;289:E187–E196. doi: 10.1152/ajpendo.00011.2005. [DOI] [PubMed] [Google Scholar]
- 17.Bozulic L, Hemmings BA. PIKKing on PKB: regulation of PKB activity by phosphorylation. Curr Opin Cell Biol. 2009;21:256–261. doi: 10.1016/j.ceb.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 18.Fayard E, Tintignac LA, Baudry A, Hemmings BA. Protein kinase B/Akt at a glance. J Cell Sci. 2005;118:5675–5678. doi: 10.1242/jcs.02724. [DOI] [PubMed] [Google Scholar]
- 19.Chan TO, Tsichlis PN. PDK2: a complex tail in one Akt. Sci STKE. 2001;2001:e1. doi: 10.1126/stke.2001.66.pe1. [DOI] [PubMed] [Google Scholar]
- 20.Persad S, Attwell S, Gray V, Mawji N, Deng JT, Leung D, Yan J, Sanghera J, Walsh MP, Dedhar S. Regulation of protein kinase B/Akt-serine 473 phosphorylation by integrin-linked kinase: critical roles for kinase activity and amino acids arginine 211 and serine 343. J Biol Chem. 2001;276:27462–27469. doi: 10.1074/jbc.M102940200. [DOI] [PubMed] [Google Scholar]
- 21.Partovian C, Simons M. Regulation of protein kinase B/Akt activity and Ser473 phosphorylation by protein kinase Calpha in endothelial cells. Cell Signal. 2004;16:951–957. doi: 10.1016/j.cellsig.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Kawakami Y, Nishimoto H, Kitaura J, Maeda-Yamamoto M, Kato RM, Littman DR, Leitges M, Rawlings DJ, Kawakami T. Protein kinase C betaII regulates Akt phosphorylation on Ser-473 in a cell type- and stimulus-specific fashion. J Biol Chem. 2004;279:47720–47725. doi: 10.1074/jbc.M408797200. [DOI] [PubMed] [Google Scholar]
- 23.Sarbassov DD, Guertin DA, Ali SM, Sabatini DM. Phosphorylation and regulation of Akt/PKB by the rictor-mTOR complex. Science. 2005;307:1098–1101. doi: 10.1126/science.1106148. [DOI] [PubMed] [Google Scholar]
- 24.Dragoi AM, Fu X, Ivanov S, Zhang P, Sheng L, Wu D, Li GC, Chu WM. DNA-PKcs, but not TLR9, is required for activation of Akt by CpG-DNA. EMBO J. 2005;24:779–789. doi: 10.1038/sj.emboj.7600539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patke A, Mecklenbrauker I, Erdjument-Bromage H, Tempst P, Tarakhovsky A. BAFF controls B cell metabolic fitness through a PKC{beta}- and Akt-dependent mechanism. J Exp Med. 2006;203:2551–2562. doi: 10.1084/jem.20060990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang J, Bardos T, Li DD, Gal I, Vermes C, Xu JY, Mikecz K, Finnegan A, Lipkowitz S, Glant TT. Cutting Edge:Regulation of T cell activation threshold by CD28 costimulation by targeting Cbl-b for ubiquitination. J Immunol. 2002;169:2236–2240. doi: 10.4049/jimmunol.169.5.2236. [DOI] [PubMed] [Google Scholar]
- 27.Li D, Gal I, Vermes C, Alegre ML, Chong AS, Chen L, Shao Q, Adarichev V, Xu X, Koreny T, Mikecz K, Finnegan A, Glant TT, Zhang J. Cutting Edge: Cbl-b: One of the key molecules tuning CD28- and CTLA-4-mediated T cell costimulation. J Immunol. 2004;173:7135–7139. doi: 10.4049/jimmunol.173.12.7135. [DOI] [PubMed] [Google Scholar]
- 28.qiao G, Li Z, Molinero L, Alegre ML, Ying H, Sun Z, Penninger JM, Zhang J. T Cell Receptor-induced NF-{kappa}B Activation Is Negatively Regulated by E3 Ubiquitin Ligase Cbl-b. Mol Cell Biol. 2008;28:2470–2480. doi: 10.1128/MCB.01505-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baier G, Telford D, Giampa L, Coggeshall KM, Baier-Bitterlich G, Isakov N, Altman A. Molecular cloning and characterization of PKC theta, a novel member of the protein kinase C (PKC) gene family expressed predominantly in hematopoietic cells. J Biol Chem. 1993;268:4997–5004. [PubMed] [Google Scholar]
- 30.Altman A, Villalba M. Protein kinase C-theta (PKCtheta): it’s all about location, location. location Immunol Rev. 2003;192:53–63. doi: 10.1034/j.1600-065x.2003.00027.x. [DOI] [PubMed] [Google Scholar]
- 31.von EM, Nielsen MW, Bonefeld CM, Boding L, Larsen JM, Leitges M, Baier G, Odum N, Geisler C. Protein kinase C (PKC) alpha and PKC theta are the major PKC isotypes involved in TCR down-regulation. J Immunol. 2006;176:7502–7510. doi: 10.4049/jimmunol.176.12.7502. [DOI] [PubMed] [Google Scholar]
- 32.Gruber T, Hermann-Kleiter N, Pfeifhofer-Obermair C, Lutz-Nicoladoni C, Thuille N, Letschka T, Barsig J, Baudler M, Li J, Metzler B, Nusslein-Hildesheim B, Wagner J, Leitges M, Baier G. PKC theta cooperates with PKC alpha in alloimmune responses of T cells in vivo. Mol Immunol. 2009;46:2071–2079. doi: 10.1016/j.molimm.2009.02.030. [DOI] [PubMed] [Google Scholar]
- 33.Bedoya LM, Marquez N, Martinez N, Gutierrez-Eisman S, Alvarez A, Calzado MA, Rojas JM, Appendino G, Munoz E, Alcami J. SJ23B, a jatrophane diterpene activates classical PKCs and displays strong activity against HIV in vitro. Biochem Pharmacol. 2009;77:965–978. doi: 10.1016/j.bcp.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 34.Fehrenbach K, Lessmann E, Zorn CN, Kuhny M, Grochowy G, Krystal G, Leitges M, Huber M. Steel factor enhances supraoptimal antigen-induced IL-6 production from mast cells via activation of protein kinase C-beta. J Immunol. 2009;182:7897–7905. doi: 10.4049/jimmunol.0801773. [DOI] [PubMed] [Google Scholar]
- 35.Gschwendt M, Dieterich S, Rennecke J, Kittstein W, Mueller HJ, Johannes FJ. Inhibition of protein kinase C mu by various inhibitors. Differentiation from protein kinase c isoenzymes. FEBS Lett. 1996;392:77–80. doi: 10.1016/0014-5793(96)00785-5. [DOI] [PubMed] [Google Scholar]
- 36.Woodgett JR. Recent advances in the protein kinase B signaling pathway. Curr Opin Cell Biol. 2005;17:150–157. doi: 10.1016/j.ceb.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 37.Scheid MP, Marignani PA, Woodgett JR. Multiple phosphoinositide 3-kinase-dependent steps in activation of protein kinase B. Mol Cell Biol. 2002;22:6247–6260. doi: 10.1128/MCB.22.17.6247-6260.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]