Abstract
Injury mortality was classically described with a trimodal distribution, with immediate deaths at the scene, early deaths due to hemorrhage, and late deaths from organ failure. We hypothesized that the development of trauma systems has improved prehospital care, early resuscitation, and critical care and altered this pattern. This population-based study of all trauma deaths in an urban county with a mature trauma system reviewed data for 678 patients (median age, 33 years; 81% male; 43% gunshot, 20% motor vehicle crashes). Deaths were classified as immediate (scene), early (in hospital, ≤4 hours from injury), or late (>4 hours after injury). Multinomial regression was used to identify independent predictors of immediate and early versus late deaths, adjusted for age, gender, race, intention, mechanism, toxicology, and cause of death. Results showed 416 (61%) immediate, 199 (29%) early, and 63 (10%) late deaths. Compared with the classical description, the percentage of immediate deaths remained unchanged, and early deaths occurred much earlier (median 52 vs 120 minutes). However, unlike the classic trimodal distribution, the late peak was greatly diminished. Intentional injuries, alcohol intoxication, asphyxia, and injuries to the head and chest were independent predictors of immediate death. Alcohol intoxication and injuries to the chest were predictors of early death, while pelvic fractures and blunt assaults were associated with late deaths. In conclusion, trauma deaths now have a predominantly bimodal distribution. Near elimination of the late peak likely represents advancements in resuscitation and critical care that have reduced organ failure. Further reductions in mortality will likely come from prevention of intentional injuries and injuries associated with alcohol intoxication.
Over a quarter century ago, Cowley described the “golden hour” for resuscitation of the severely injured, implying that patients who received definitive care soon after injury had better outcomes (1, 2). In a classic paper in 1983, Trunkey described a trimodal distribution of trauma deaths based upon the time interval from injury to death (3) (Table 1). Subsequently, comprehensive trauma systems were developed to reduce the burden of injuries and trauma deaths by devising interventions to reduce all three types of trauma deaths (4). Over the last three decades, these developments have included injury prevention, use of prehospital advanced life support interventions, rapid transport, widespread adoption of advanced trauma life support by prehospital providers and emergency departments, designated trauma centers with personnel and resources to care for the injured, evidence-based protocols for acute care of injuries, advances in critical care medicine, multidisciplinary care of the injured, and an emphasis on rehabilitation and reintegration into society.
Table 1.
Trunkey's 1983 classification of immediate, early, and late trauma deaths∗
| Deaths | Timing† | Location | Cause | Interventions‡ |
| Immediate | Minutes | Scene | Nonsurvivable injuries | Injury prevention |
| Early | Hours | Hospital | Severe injuries, potentially survivable with optimal care | Improved access to trauma care |
| Late | Weeks | Hospital | Multiple organ failure, sepsis | Improved resuscitation/critical care |
∗From Trunkey, 1983 (3).
†Timing of death after sustaining injuries.
‡Primary interventions with the most potential to reduce trauma deaths.
The impact of these developments in trauma systems on the outcome of trauma patients is not known. A single study published over a decade ago found a bimodal distribution of trauma deaths, with a persistent peak in immediate deaths and a second peak at 48 hours (5). However, the study population consisted of predominantly blunt injuries from a diverse geographical environment, with inconsistent access to prehospital care and trauma centers across the region. The purpose of the current study was to examine the time distribution of trauma deaths in an urban setting with a well-established and mature trauma system. We hypothesized that in a modern trauma system, there would be fewer immediate (at the scene) and early deaths (within hours of hospital arrival) and more delayed trauma deaths (multiple organ failure, sepsis).
METHODS
We undertook a population-based study of all trauma-related deaths in an urban county in 2005. Data were obtained from the office of the county medical examiner. Under article 49.25 of the state code of criminal procedure, the county medical examiner must be notified when any person dies an unnatural death or when the circumstances of death are unknown or lead to suspicion that the death was the result of unlawful means (6). The chief medical examiner for the county requires that all deaths that are the direct or indirect result of injury undergo a complete forensic postmortem examination. This requirement provides a unique opportunity in Dallas County to capture all injury-related deaths, including scene deaths, hospital deaths, and late deaths if they were in any way related to trauma. Data reviewed consisted of information obtained through scene investigations, police reports, prehospital and hospital records, and autopsy and toxicology findings.
A total of 4318 deaths were reported to the county medical examiner during calendar year 2005. All were reviewed to identify deaths due to injuries. Patients were excluded if their death resulted from a drug overdose, poisoning, burn, or foreign-body aspiration and if they were not a resident of the county. The final study population consisted of 678 deaths, which constituted 16% of all deaths in the county. The estimated population of the county on July 1, 2005, was 2,308,527, and this was used to calculate trauma mortality rates (7). The time from injury to death and location of death were used to classify each death into one of three categories as described by Trunkey (3). Patients who were pronounced dead at the scene were considered “immediate” deaths, while those who were transported to the hospital were classified as “early” deaths (≤4 hours from injury) or “late” deaths (>4 hours from injury). Those who were transported to the hospital and were pronounced dead on arrival were classified as early deaths.
The distribution of deaths in this study was compared with the classical trimodal distribution by plotting the two together. Further statistical analysis was undertaken to identify independent predictors of each type of trauma death. Predictors explored included age, gender, mechanism of injury, intention, alcohol intoxication, and types of injuries. Correlations were performed to identify any interactions among the predictors. Variance inflation factor was calculated to measure the impact of collinearity among variables in the model. Any of the variables with a variance inflation factor ≥10 were considered to have a high degree of collinearity and were removed from the model. Multinomial regression analysis was used to identify independent predictors of immediate and early versus late deaths, adjusted for the confounders listed above. Odds ratios were calculated with their 95% confidence intervals. A P <0.05 was considered significant for all analyses.
RESULTS
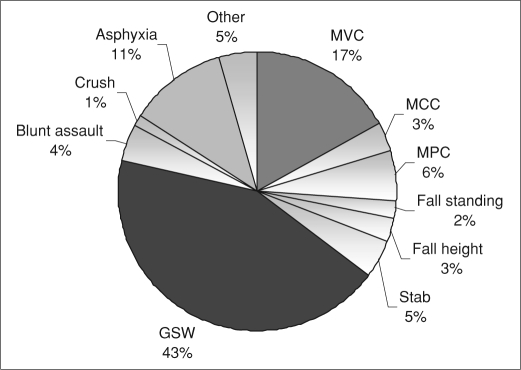
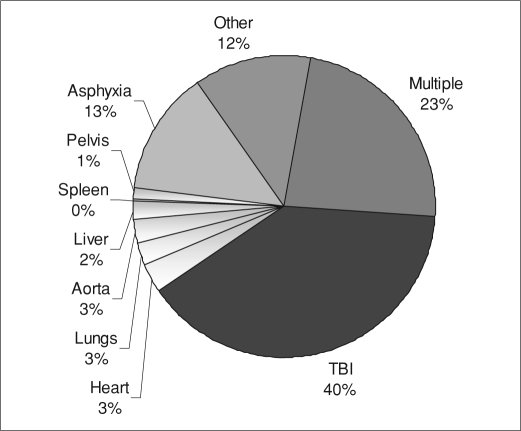
The trauma-specific mortality rate of the county was 29.4 deaths per 100,000 residents, while the national rate was 42.5 deaths. The median age of patients was 33 years, and 81% were male (Table 2). Almost half of all deaths were due to firearm injuries, while traffic-related deaths accounted for a quarter of all deaths (Figure 1). The most common injury leading to trauma deaths was isolated head injury followed by asphyxia, while a quarter of patients died from multiple injuries (Figure 2).
Table 2.
Description of trauma deaths in Dallas County, 2005
| All (n = 678) | Immediate (n = 416) | Early (n = 199) | Late (n = 63) | |
| Median age (years) | 33 | 35 | 28 | 33 |
| Gender: male | 81% | 80% | 87% | 70% |
| Race: white | 62% | 73% | 47% | 41% |
| Intentional | 62% | 73% | 47% | 27% |
| Alcohol related | 36% | 40% | 35% | 10% |
Figure 1.
Mechanism of injury among 678 trauma deaths in Dallas County, 2005. GSW indicates gunshot wound; MVC, motor vehicle crash; MPC, motor vehicle vs pedestrian; MCC, motorcycle crash.
Figure 2.
Primary cause of death. TBI indicates traumatic brain injury.
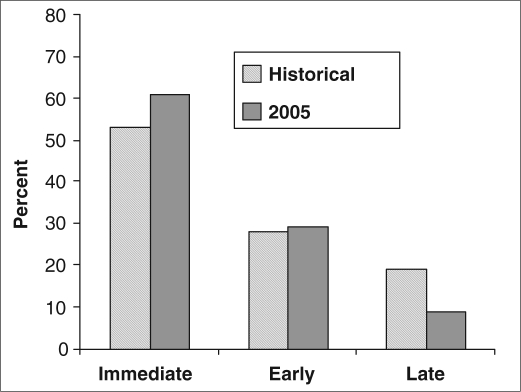
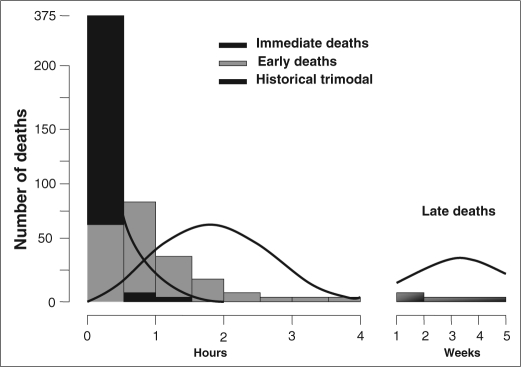
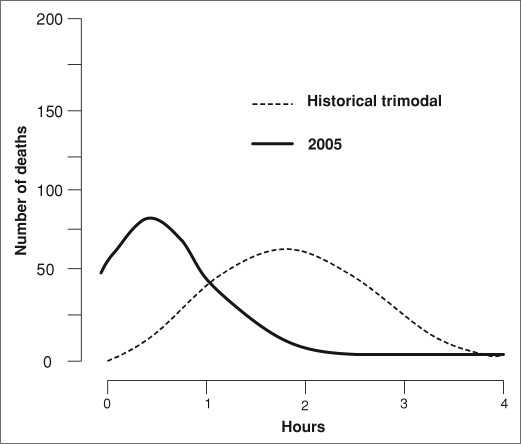
A majority of the deaths occurred immediately (416, 61%). Of the rest, 199 (29%) were early, and only 63 (9%) were late. Compared with the historical controls, this represented an increase in the percentage of immediate deaths, a decrease in late deaths, and no change in early deaths (Figure 3). Ninety-six percent of all deaths occurred within the first 24 hours. Of those who were transported to the hospital, 84% died within the first 12 hours and 89% in the first 24 hours. When the deaths were plotted against time, we found a persistent peak in immediate and early deaths (Figure 4). However, the early deaths occurred earlier (historical median 120 minutes vs 52 minutes in the present study), suggesting improvements in prehospital care resulting in earlier arrival of severely injured patients at the hospital (Figure 5). Most importantly, only 4% of deaths occurred after the first 24 hours, resulting in a markedly diminished late peak, suggesting improvements in resuscitation, critical care, and prevention and treatment of complications. Asphyxia, which was defined as strangulation, hanging, or drowning, may represent a different entity than other forms of trauma. However, when asphyxia was excluded from the analysis, the results were similar, as were the proportions of immediate, early, and late deaths (60%, 30%, and 10%, respectively).
Figure 3.
Timing of trauma deaths in the historical group from Trunkey's 1983 study (3) and in the group of 678 trauma deaths in Dallas County in 2005.
Figure 4.
Timing distribution of trauma deaths compared with the historical trimodal distribution. The black line represents the historical trimodal distribution; bars represent the present study.
Figure 5.
Time shift in early deaths in the group of 678 trauma deaths in Dallas County in 2005 compared with the historical group from Trunkey's 1983 study (3).
Multinomial regression analyses demonstrated that intentional injuries, alcohol intoxication, asphyxia, and injuries to the head and chest were independent predictors of immediate death (Table 3). Alcohol intoxication and injuries to the chest were predictors of early death, while pelvic fractures and blunt assault were associated with late deaths. Early deaths were further analyzed to examine possible explanations for the shift to a shorter interval from injury to death. The median transport time was about 40 minutes (interquartile range, 31–48), indicating that most of these patients were pronounced dead within minutes of hospital arrival. Injuries resulting in early deaths were then categorized into nonsurvivable (traumatic brain injury, injury of heart or aorta) and potentially survivable (all other injuries). Of the early deaths, 76% of patients died of nonsurvivable injuries, suggesting that many patients who were transported to the hospital were moribund. Such patients may have been classified in the immediate category by Trunkey.
Table 3.
Predictors of immediate and early versus late deaths among 678 trauma deaths in Dallas County, 2005
| Odds ratios with 95% confidence intervals |
||
| Predictors | Immediate | Early |
| Age | 0.98 (0.97–1.01) | 1.02 (1.01–1.03)∗ |
| Intentional injury | 5.0 (2.7–9.5)∗ | 1.46 (0.8–2.8) |
| Alcohol intoxication | 7.0 (2.8–7.2)∗ | 4.8 (1.9–11.9)∗ |
| Head injury | 2.2 (1.2–4.2)∗ | 1.01 (0.53–1.9) |
| Chest injury | 3.6 (1.5–8.8)∗ | 4.3 (1.8–10.5)∗ |
| Asphyxia | 17.8 (2.3–14.2)∗ | 6.9 (0.85–55.5) |
| Pelvis injury | 0.21 (0.06–0.75)∗ | 0.31 (0.09–1.08) |
| Blunt assault | 0.16 (0.06–0.47)∗ | 0.17 (0.05–0.61) |
∗P < 0.05.
Substance abuse was prominent, as 56% of all deaths and 63% of immediate deaths had a positive toxicology screen on postmortem examination. Alcohol was the most frequent substance identified, comprising 35% of all deaths and 40% of immediate deaths. Furthermore, 54% of those who died from penetrating injuries had detectable levels of illicit drugs in their postmortem blood, most commonly marijuana (25%) and cocaine (16%).
DISCUSSION
The classical trimodal distribution of trauma deaths was described by Trunkey in 1983, based upon the distribution of deaths due to injuries in several counties of northern California (3). The findings of the current study show several important changes in the distribution of trauma deaths since then, as well as several similarities. With advances in trauma systems, the deaths have now assumed a largely bimodal distribution, with a vast majority of deaths occurring within the first few hours. Patients who survive beyond that are likely to live, with a dramatic decrease in the number of late deaths. At the same time, large numbers of immediate and early deaths emphasize a persistent need for ongoing efforts in injury prevention and control.
With development of prehospital and trauma systems, a large number of trauma patients are rapidly transported to trauma centers, where they are treated aggressively. Hence, when we undertook this study, we expected to see a reduction in the number of early deaths and an increase in the number of late deaths due to a larger number of patients surviving the initial insult. A late peak in deaths occurring days to weeks later has generally been attributed to the consequences of initial shock and crystalloid resuscitation (8, 9). The resulting ischemia-reperfusion injury leads to cellular damage, subsequently resulting in multiple organ dysfunction, such as acute respiratory distress syndrome, acute renal failure, cardiac dysfunction, infections, and sepsis (10–15). Near elimination of late deaths probably reflects improving outcomes of patients with multiple organ dysfunction. For example, recent critical care data suggest a reduction in mortality due to acute respiratory distress syndrome and acute renal failure (16, 17). These reductions have been attributed to improvements in critical care, such as intensivist-led units, evidence-based medicine (such as low-stretch ventilation), protocol-driven care, and minimization of errors (18, 19). Also, improvements in resuscitation methods, such as early use of blood products, utilization of massive transfusion protocols, and an emphasis on minimizing crystalloid resuscitation, may have contributed to reduction in late deaths (20).
Another important finding of this study was a change in the timing of early deaths. Again, with improvements in trauma systems, we expected that the peak in early deaths would shift to the right, i.e., patients with life-threatening but survivable injuries who made it to the hospital were being treated early and aggressively, and thus many deaths were prevented or prolonged. However, our data showed a shift to the left, suggesting that patients who made it to the hospital were actually dying earlier than historical controls. There are two possible explanations: either prehospital providers are bringing to the hospital sicker patients who are essentially dead upon arrival, or the initial resuscitation and management at the hospital are not as effective as they used to be. We believe that the former explanation is more plausible. Unfortunately, we were not able to determine which patients were pronounced dead upon arrival to the hospital. However, in our data, the median time from injury to hospital arrival was 42 minutes, while the median time from injury to death was 52 minutes. The short time interval between arrival at the hospital and time of death suggest that most of the patients in the early death group were moribund during transport. In a mature trauma system, prehospital times are probably much shorter now than they were before the trauma systems were developed, especially in an urban environment. This may also reflect a “scoop and run” approach by local paramedics. Hence, it is possible that many of the patients who would have previously been pronounced at the scene are now transported to hospitals. As such, it is likely that many of the deaths that we classified as early deaths in the current study were classified as immediate deaths in Trunkey's study. This logic is supported by the fact that a majority of early deaths were due to nonsurvivable injuries, such as an aortic transection, heart laceration, or severe brain injury.
In our study, the trauma-specific mortality rate was 29.4 per 100,000, significantly lower than the national rate of 42.5. The most plausible explanation for this discrepancy is access to trauma care. Dallas County is a large urban county with readily available ground and air medical transport throughout the region. In addition, there are two level 1 and one level 2 trauma centers in the county, and more than 80% of the patients were transported to these hospitals. The national rate includes patients from both urban and rural areas, a large portion of whom may not have direct access to trauma care. Furthermore, the mechanism and severity of injury may differ between urban and rural environments.
We believe that the most important finding of our study is a persistent need for injury prevention and control in our community. Our data show that a large majority of patients in Dallas County died of nonsurvivable injuries, suggesting that further reduction in trauma deaths may not be achieved with improvements in postinjury care. Even if all patients with potentially survivable injuries were salvaged with perfect therapies delivered in a flawless system of clinical care, the reduction in total number of trauma deaths would be rather small. Therefore, prevention of the injuries is likely to have the greatest impact on trauma mortality.
Multinomial analyses suggest potential targets for intervention, such as intentional injuries, primarily due to firearms, and injuries associated with alcohol intoxication. Substance abuse was a common finding on postmortem examination. While no direct causal relationship can be determined, the frequency of substance abuse among the trauma deaths suggests that it may be a significant contributing factor. Furthermore, the autopsy rates identifying substances of abuse may underestimate the actual frequency, as those who died later following their injuries may have eliminated the drugs or alcohol from their systems, resulting in a negative screen. Brief alcohol interventions and programs such as “Drive Alive,” which link alcohol consumption to injury, have demonstrated short-term success in reducing the number of recurrent injuries related to alcohol. However, those patients have already sustained and survived their injuries, and a long-term benefit from these programs has not yet been demonstrated (21–24). Additional prevention efforts should target the larger population at risk to modify behavior and attitudes towards alcohol and drug abuse. Unfortunately, the focus of trauma research continues to be finding the next best clinical therapy (25, 26). We strongly recommend that the trauma community support a similar emphasis on primary prevention of injuries through influencing the research agenda of the funding agencies.
This study has several potential limitations. It was a retrospective review of preexisting data and suffers from inherent limitations of such studies. Specifically, some data points may be subject to recall bias, such as the time of injury. However, we believe that the data were reliable, as they were obtained either from the report of a field investigator or from prehospital providers. The findings reflect the experience of a single, large urban county with three major trauma centers. Hence, the study may not be representative of all trauma deaths in the country. Also, a comparison of trauma system in Trunkey's study in 1983 to Dallas County in 2005 would be interesting. However, those descriptions were not available for analysis. In addition, we were not able to capture county residents who may have died of injuries outside the county jurisdiction, which may alter our estimate of the trauma-specific mortality rate. We assigned the cause of death based upon our assessment of all the injuries that were found at autopsy. Since many patients sustained multiple injuries, it is impossible to determine which injury directly led to the death of the patient. Finally, it should be recognized that comparison with historical controls was limited. This study was based on a visual comparison of recent data with a historical analysis, as we were not able to obtain the original historical data. Hence, a valid statistical comparative analysis of the two studies was not possible. Therefore, no definitive conclusions may be drawn from this analysis.
In conclusion, we have shown that trauma-related deaths now have a largely bimodal, rather than a trimodal, distribution. The greatly diminished late peak in deaths likely implies improvements in resuscitation and critical care. The “golden hour” is real and remains relevant, as a majority of deaths occur rapidly following a severe injury. However, any further significant reduction in trauma deaths in Dallas County will come from primary prevention of intentional injuries and injuries associated with alcohol intoxication.
References
- 1.Cowley RA. The resuscitation and stabilization of major multiple trauma patients in a trauma center environment. Clin Med. 1976;83:16–22. [Google Scholar]
- 2.Cowley RA. A total emergency medical system for the state of Maryland. Md State Med J. 1975;24(7):37–45. [PubMed] [Google Scholar]
- 3.Trunkey DD. Trauma. Sci Am. 1983;249:28–35. [PubMed] [Google Scholar]
- 4.West JG, Trunkey DD, Lim RC. Systems of trauma care. A case of two counties. Arch Surg. 1979;114(4):455–460. doi: 10.1001/archsurg.1979.01370280109016. [DOI] [PubMed] [Google Scholar]
- 5.Meislin H, Criss EA, Judkins D, Berger R, Conroy C, Parks B, Spaite DW, Valenzuela TD. Fatal trauma: the modal distribution of time to death is a function of patient demographics and regional resources. J Trauma. 1997;43(3):433–440. doi: 10.1097/00005373-199709000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Forensic Sciences . Code of Criminal Procedure. Dallas, TX: Office of the Dallas County Medical Examiner; 2006. Chapter 49, Article 49.25. [Google Scholar]
- 7.Centers for Disease Control and Prevention. Injury Prevention & Control: Data & Statistics. Available at http://www.cdc.gov/ncipc/wisqars/default.htm; accessed March 26, 2010.
- 8.Cotton BA, Guy JS, Morris JA, Jr, Abumrad NN. The cellular, metabolic, and systemic consequences of aggressive fluid resuscitation strategies. Shock. 2006;26(2):115–121. doi: 10.1097/01.shk.0000209564.84822.f2. [DOI] [PubMed] [Google Scholar]
- 9.Weinstein PD, Doerfler ME. Systemic complications of fluid resuscitation. Crit Care Clin. 1992;8(2):439–448. [PubMed] [Google Scholar]
- 10.Navarrete-Navarro P, Ruiz-Bailén M, Rivera-Fernández R, Guerrero-López F, Pola-Gallego-de-Guzmán MD, Vázquez-Mata G. Acute respiratory distress syndrome in trauma patients: ICU mortality and prediction factors. Intensive Care Med. 2000;26(11):1624–1629. doi: 10.1007/s001340000683. [DOI] [PubMed] [Google Scholar]
- 11.Wang P, Chaudry IH. Crystalloid resuscitation restores but does not maintain cardiac output following severe hemorrhage. J Surg Res. 1991;50(2):163–169. doi: 10.1016/0022-4804(91)90241-d. [DOI] [PubMed] [Google Scholar]
- 12.Lang F, Busch GL, Ritter M, Völkl H, Waldegger S, Gulbins E, Häussinger D. Functional significance of cell volume regulatory mechanisms. Physiol Rev. 1998;78(1):247–306. doi: 10.1152/physrev.1998.78.1.247. [DOI] [PubMed] [Google Scholar]
- 13.Barak M, Rudin M, Vofsi O, Droyan A, Katz Y. Fluid administration during abdominal surgery influences on coagulation in the postoperative period. Curr Surg. 2004;61(5):459–462. doi: 10.1016/j.cursur.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 14.Ng KF, Lam CC, Chan LC. In vivo effect of haemodilution with saline on coagulation: a randomized controlled trial. Br J Anaesth. 2002;88(4):475–480. doi: 10.1093/bja/88.4.475. [DOI] [PubMed] [Google Scholar]
- 15.Watters JM, Tieu BH, Todd SR, Jackson T, Muller PJ, Malinoski D, Schreiber MA. Fluid resuscitation increases inflammatory gene transcription after traumatic injury. J Trauma. 2006;61(2):300–308. doi: 10.1097/01.ta.0000224211.36154.44. [DOI] [PubMed] [Google Scholar]
- 16.Zambon M, Vincent JL. Mortality rates for patients with acute lung injury/ARDS have decreased over time. Chest. 2008;133(5):1120–1127. doi: 10.1378/chest.07-2134. [DOI] [PubMed] [Google Scholar]
- 17.Ciesla DJ, Moore EE, Johnson JL, Cothren CC, Banerjee A, Burch JM, Sauaia A. Decreased progression of postinjury lung dysfunction to the acute respiratory distress syndrome and multiple organ failure. Surgery. 2006;140(4):640–647. doi: 10.1016/j.surg.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 18.The Acute Respiratory Distress Syndrome Network Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 19.van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345(19):1359–1367. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 20.Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, Sebesta J, Jenkins D, Wade CE, Holcomb JB. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63(4):805–813. doi: 10.1097/TA.0b013e3181271ba3. [DOI] [PubMed] [Google Scholar]
- 21.Ekeh AP, Hamilton SB, Demko D, McCarthy MC. The effect of a trauma center-based intervention program on recidivism among adolescent driving offenders. J Trauma. 2008;65(5):1117–1120. doi: 10.1097/TA.0b013e318187cfe3. [DOI] [PubMed] [Google Scholar]
- 22.Walton MA, Goldstein AL, Chermack ST, McCammon RJ, Cunningham RM, Barry KL, Blow FC. Brief alcohol intervention in the emergency department: moderators of effectiveness. J Stud Alcohol Drugs. 2008;69(4):550–560. doi: 10.15288/jsad.2008.69.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daeppen JB, Gaume J, Bady P, Yersin B, Calmes JM, Givel JC, Gmel G. Brief alcohol intervention and alcohol assessment do not influence alcohol use in injured patients treated in the emergency department: a randomized controlled clinical trial. Addiction. 2007;102(8):1224–1233. doi: 10.1111/j.1360-0443.2007.01869.x. [DOI] [PubMed] [Google Scholar]
- 24.Soderstrom CA, DiClemente CC, Dischinger PC, Hebel JR, McDuff DR, Auman KM, Kufera JA. A controlled trial of brief intervention versus brief advice for at-risk drinking trauma center patients. J Trauma. 2007;62(5):1102–1111. doi: 10.1097/TA.0b013e31804bdb26. [DOI] [PubMed] [Google Scholar]
- 25.West MA, Shapiro MB, Nathens AB, Johnson JL, Moore EE, Minei JP, Bankey PE, Freeman B, Harbrecht BG, McKinley BA, Moore FA, Maier RV, the Inflammation and the Host Response to Injury Collaborative Research Program Inflammation and the host response to injury, a large-scale collaborative project: patient-oriented research core-standard operating procedures for clinical care. IV. Guidelines for transfusion in the trauma patient. J Trauma. 2006;61(2):436–439. doi: 10.1097/01.ta.0000232517.83039.c4. [DOI] [PubMed] [Google Scholar]
- 26.Brasel KJ, Bulger E, Cook AJ, Morrison LJ, Newgard CD, Tisherman SA, Kerby JD, Coimbra R, Hata JS, Hoyt DB, Resuscitation Outcomes Consortium Investigators Hypertonic resuscitation: design and implementation of a prehospital intervention trial. J Am Coll Surg. 2008;206(2):220–232. doi: 10.1016/j.jamcollsurg.2007.07.020. [DOI] [PubMed] [Google Scholar]