Abstract
Objective
The objective of this study was to test three hypotheses in a sample of individuals with COPD: 1) unsupportive family relationships are associated with psychological distress; 2) psychological distress is associated with smoking status; and 3) unsupportive family relationships are indirectly associated with smoking status via psychological distress.
Method
Cross-sectional data were collected via self-report questionnaires completed by 455 individuals with COPD who had at least a 10 pack-year smoking history. The hypotheses were tested with structural equation modeling.
Results
All three hypotheses were supported. Unsupportive family relationships were associated with psychological distress (β = .67, p < .001), psychological distress was associated with smoking status (β = .40, p < .001), and unsupportive family relationships were indirectly associated with smoking status via psychological distress (β = .27, p < .001).
Conclusion
Results of this study suggest that family relationships are an important factor to include in future longitudinal research that attempts to elucidate social and psychological influences on smoking behavior.
Keywords: depression, anxiety, smoking, chronic obstructive pulmonary disease
Approximately 85% of all cases of chronic obstructive pulmonary disease (COPD) are attributable to smoking. Smoking cessation is the most important behavioral intervention to alleviate symptoms and delay progression of COPD [1, 2]. Research is needed to understand modifiable social and psychological factors that influence smoking behavior among individuals with COPD. With a better understanding of these factors, there is a greater opportunity to develop comprehensive smoking cessation interventions to assist this population.
Social support is important for successful smoking cessation. In the Lung Health Study, support for quitting smoking predicted initial quitting and relapse rate within 24 months [3]. Support from family members may be particularly important. Prospective research indicates that partner support predicts success in quit attempts [4, 5]. In addition, negative behaviors of spouses (such as commenting that smoking is a dirty habit) predict relapse among individuals who are trying to quit smoking [6]. The association between family relationship quality and smoking behavior among individuals with COPD has not been studied, nor have potential mechanisms through which family relationships affect smoking behavior.
The influence of family relationships on smoking behavior may be mediated through psychological distress. Longitudinal research indicates that family relationships influence the onset [7] and course [8-10] of depression and anxiety. In turn, prospective studies indicate that symptoms of depression and anxiety predict the initiation and maintenance of smoking behavior [11, 12]. Depression also reduces smoking cessation rates and increases the risk of relapse among individuals who are trying to quit smoking [13, 14]. Psychological distress is especially important in COPD because there is a high prevalence of depression and anxiety among individuals with COPD [15, 16].
Although the independent influences of family relationships and psychological distress on smoking behavior have been established, no research to date has investigated the joint influence of both of these factors on smoking behavior. Such research is particularly important for individuals with COPD, as smoking behavior affects symptoms and progression of COPD. The aim of this study was to test the following hypotheses: 1) unsupportive family relationships are associated with psychological distress; 2) psychological distress is associated with smoking status; and 3) unsupportive family relationships are indirectly associated with smoking status via psychological distress.
METHODS
Sample and Procedures
Participants were studied under a protocol approved by the Institutional Review Board at National Jewish Health and the Colorado Multiple Institutional Review Board. This protocol was judged to be exempt by both review boards because the protocol solely involved the use of survey procedures which cannot be linked to subjects. Anonymous, cross-sectional data were collected from individuals with physician-diagnosed COPD by mailing questionnaires to people who had been assessed or treated for COPD at two medical centers in Denver selected to generate a diverse sample. One medical center was a tertiary-care respiratory hospital and the other was a university-affiliated public hospital. At the tertiary-care hospital, questionnaires were mailed to clinic patients who had consented to be contacted for research studies and patients who had registered with the clinical research unit. At the university-affiliated hospital, questionnaires were mailed to all patients with COPD at three internal medicine clinics associated with the hospital. Patients at these clinics with ICD-9 codes indicative of COPD were identified via a clinical database.
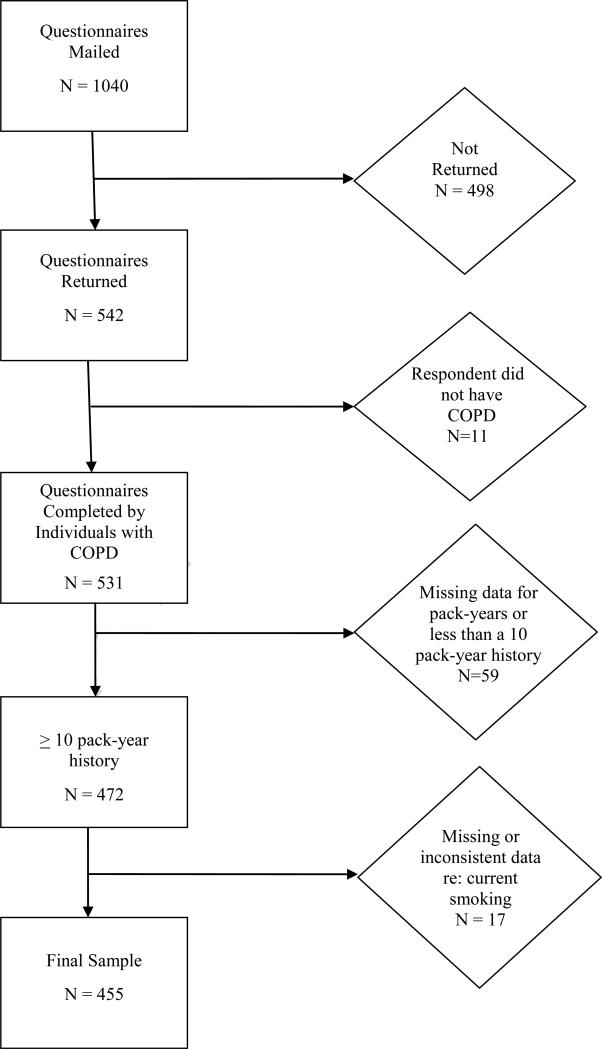
Questionnaires were mailed to 1040 individuals and returned by 542 people, a 52% response rate. The response rate was 67% at the tertiary-care hospital and 31% at the university-affiliated hospital. Eleven questionnaires were excluded from analyses because the respondent indicated that they did not have COPD. These respondents disagreed with their physician's diagnosis and were excluded because many of the items on the questionnaire are only applicable to individuals who self-identify as having COPD. We also required that respondents have at least a 10 pack-year smoking history. Fifty-nine respondents were excluded because they were missing data for smoking history or had less than a 10 pack-year smoking history. An additional 17 respondents were excluded because they were missing data about current smoking or gave inconsistent answers to the two questions used to assess current smoking. Thus, the final sample was 455 (see Figure 1).
Figure 1.
Recruitment Flow Diagram
Measures
Demographic, Health, and Disease Characteristics
Demographic, health, and disease characteristics were collected (see Tables 1 and 2). For number of comorbid conditions, respondents indicated whether they had the following health problems: arthritis, diabetes, heart disease or heart surgery, hypertension/high blood pressure, bone problems, cancer, and other. Number of comorbid conditions represents the total number of positive responses. The number of prescription medications for COPD was summed, with combination inhalers counted as two medications.
Table 1.
Demographic Characteristics of the Sample
| Combined Sample (n = 455) | Tertiary Care (n = 359) | Public Hospital (n = 96) | P Value for Comparison | |
|---|---|---|---|---|
| | ||||
| Variable | N (%) | N (%) | N (%) | |
| Gender | 0.44 | |||
| Male | 238 (52.4) | 191 (53.4) | 47 (49.0) | |
| Female | 216 (47.6) | 167 (46.6) | 49 (51.0) | |
| | ||||
| Age | 0.01 | |||
| Less than 60 | 96 (21.1) | 65 (18.1) | 31 (32.3) | |
| 60 to 64 | 82 (18.0) | 65 (18.1) | 17 (17.7) | |
| 65 to 69 | 104 (22.9) | 81 (22.6) | 23 (24.0) | |
| 70 to 74 | 85 (18.7) | 70 (19.5) | 15 (15.6) | |
| 75 or more | 88 (19.3) | 78 (21.7) | 10 (10.4) | |
| | ||||
| Race/ethnicity | <0.001 | |||
| Caucasian non-Hispanic | 394 (86.6) | 337 (93.9) | 57 (59.4) | |
| Black non-Hispanic | 22 (4.8) | 9 (2.5) | 13 (13.5) | |
| Hispanic | 32 (7.0) | 8 (2.2) | 24 (25.0) | |
| Other | 7 (1.5) | 5 (1.4) | 2 (2.1) | |
| | ||||
| Relationship Status | <0.001 | |||
| Married | 238 (52.3) | 221 (61.6) | 17 (17.7) | |
| Member of an unmarried couple | 11 (2.4) | 7 (1.9) | 4 (4.2) | |
| Divorced/separated | 124 (27.3) | 76 (21.2) | 48 (50.0) | |
| Widowed | 55 (12.1) | 42 (11.7) | 13 (13.5) | |
| Never married | 27 (5.9) | 13 (3.6) | 14 (14.6) | |
| | ||||
| Education | <0.001 | |||
| Some high school or less | 49 (10.9) | 23 (6.5) | 26 (27.1) | |
| High school graduate | 116 (25.7) | 89 (25.1) | 27 (28.1) | |
| Some college or technical school | 182 (40.4) | 145 (40.8) | 37 (38.5) | |
| College graduate | 104 (23.1) | 98 (27.6) | 6 (6.2) | |
| | ||||
| Income | <0.001 | |||
| Less than $15,000 | 134 (30.8) | 55 (16.1) | 79 (84.9) | |
| Between $15,001 and $25,000 | 58 (13.3) | 47 (13.7) | 11 (11.8) | |
| Between $25,001 and $35,000 | 74 (17.0) | 73 (21.3) | 1 (11) | |
| Between $35,001 and $50,000 | 55 (12.6) | 54 (15.8) | 1 (1.1) | |
| Between $50,001 and $75,000 | 57 (13.1) | 57 (16.7) | 0 (0.0) | |
| $75,001 or more | 57 (13.1) | 56 (16.4) | 1 (1.1) | |
Table 2.
Health and Disease Characteristics of the Sample
| Combined Sample (n = 455) | Tertiary Care (n = 359) | Public Hospital (n = 96) | P Value for Comparison | |
|---|---|---|---|---|
| | ||||
| Variable | M (SD) | M (SD) | M (SD) | |
| Pack-Years | 56.2 (28.8) | 56.4 (28.0) | 55.5 (32.1) | 0.78 |
| Number of Cigarettes per Day (among current smokers) | 11.0 (8.4) | 8.0 (6.7) | 13.3 (8.8) | <0.01 |
| Number of Years since Quit Smoking (among non-smokers) | 12.5 (9.8) | 12.9 (9.9) | 9.9 (9.4) | 0.05 |
| Body Mass Index | 26.9 (6.3) | 26.6 (5.9) | 28.1 (7.6) | 0.07 |
| Number of Comorbid Conditions | 1.7 (1.1) | 1.6 (1.1) | 2.0 (1.0) | <0.01 |
| Number of Years had COPD | 6.2 (5.0) | 6.3 (5.0) | 5.7 (4.7) | 0.34 |
| Number of Medications for COPD | 3.3 (1.9) | 3.4 (2.0) | 3.2 (1.7) | 0.41 |
| | ||||
| Variable | N (%) | N (%) | N (%) | |
| | ||||
| Current Smoker | <0.001 | |||
| No | 374 (82.2) | 324 (90.3) | 50 (52.1) | |
| Yes | 81 (17.8) | 35 (9.7) | 46 (47.9) | |
| Using oxygen for COPD | 0.08 | |||
| No | 161 (35.9) | 120 (33.8) | 41 (43.6) | |
| Yes | 288 (64.1) | 235 (66.2) | 53 (56.4) | |
Unsupportive Family Relationships
Criticism was measured by the perceived criticism subscale of the Family Emotional Involvement and Criticism Scale (FEICS) and the Perceived Criticism Measure (PCM). The FEICS is a 7-item scale that was developed to measure perceived criticism in medical patients [17]. The score for each item can range from 1 to 5. Responses to the 7 items are summed and the scale score ranges from 7 to 35. The PCM is a single item designed to measure the extent to which the respondent views family members as being critical on a scale ranging from 1 (not at all critical) to 10 (very critical) [9]. Blame was measured by an item developed for this study that was modeled on the PCM and was worded as follows: “To what extent do you think your family blames you for having COPD?” Responses range from 1 (not at all) to 10 (completely). General family functioning was assessed by the 12-item General Functioning subscale of the Family Assessment Device, which has been used in research on adjustment to medical illness [18]. The score for each item ranges from 1 to 4, and responses are averaged so the scale score also ranges from 1 to 4.
Psychological Distress
Psychological distress was measured by the depression and anxiety subscales of the Hospital Anxiety and Depression Scale, which was designed to measure symptoms of depression and anxiety in medical outpatients [19] and has frequently been used in studies of COPD [20, 21]. Each subscale has 7 items with scores that range from 1 to 3. Responses are summed and each subscale score can range from 0 to 21.
Current Smoking Status
Current smoking status was assessed via two questions: 1) On average, how many cigarettes do you now smoke a day; and 2) How long ago did you quit smoking? For the first question, a response of zero cigarettes was used to indicate that the respondent was a non-smoker. Any response greater than zero indicated that the respondent was a current smoker. For the second question, if the respondent checked the response “not applicable—I still smoke,” they were considered a current smoker. If the respondent wrote a response for how long ago they quit, they were considered a non-smoker. Respondents had to answer both questions and provide consistent answers to be classified as either a current smoker or a non-smoker.
Analyses
PASW version 17.0 was used to calculate t-tests and chi-square tests to compare the tertiary-care with the university-affiliated hospital with regard to demographic, health and disease, and family and psychological characteristics.
Mplus 5.0 was used to test all hypotheses via a single structural equation model. Structural equation modeling (SEM) was used because SEM accounts for measurement error by utilizing multiple indicators of a construct [22]. For example, multiple measures of family relationships were used as indicators of unsupportive family relationships. SEM was also used because it can simultaneously test an entire model rather than separately testing each of the components of the model. The following three associations were tested: 1) family relationship quality with psychological distress; 2) psychological distress with smoking status; and, 3) the indirect path from relationship quality to smoking status via psychological distress. These associations were evaluated both for statistical significance and effect size. Effect size is not affected by the sample size, whereas statistical significance is highly related to sample size. In SEM a standardized path coefficient of at least .30 is considered a medium effect size, and a coefficient of .50 or larger a large effect size [22].
Potential moderators were examined to determine whether hypotheses needed to be tested separately by hospital, gender, socioeconomic status, oxygen use, or relationship status (coupled versus single). For example, the moderating effect of hospital was tested by comparing a model in which all path coefficients were constrained to be identical for the two hospitals with a series of models that allowed path coefficients to differ by hospital. The constrained model was compared to: 1) a model in which the path from family to psychological distress was allowed to differ by hospital, 2) a model in which the path from psychological distress to smoking status was allowed to differ by hospital, and 3) a model in which the path from family to smoking status was allowed to differ by hospital. The goal was to determine whether the value of the path coefficient being tested differed by hospital at p < .05.
RESULTS
Preliminary Analyses
Table 1 presents demographic characteristics of the sample. Participants from the two hospitals differed with regard to age, race/ethnicity, relationship status, education, and income. Table 2 presents health and disease characteristics of the sample. Of note, 90% of participants from the tertiary-care hospital had quit smoking, while only 52% of participants from the university-affiliated hospital had quit smoking. Among current smokers, participants from the university-affiliated hospital smoked significantly more cigarettes per day. Table 3 presents means and standard deviations for the family and psychological variables used in the structural equation model. Participants from the university-affiliated hospital reported more unsupportive family relationships and more psychological distress.
Table 3.
Family and Psychological Characteristics of the Sample
| Combined Sample (n = 455) | Tertiary Care (n = 359) | Public Hospital (n = 96) | P Value for Comparison | |
|---|---|---|---|---|
| | ||||
| Variable | M (SD) | M (SD) | M (SD) | |
| Family Characteristics | ||||
| Criticism (measured by FEICS) | 11.3 (4.9) | 10.7 (4.3) | 13.7 (6.3) | <0.001 |
| Criticism (measured by PCM) | 2.8 (2.4) | 2.6 (2.2) | 3.3 (2.8) | 0.06 |
| Blame | 3.9 (3.4) | 3.8 (3.3) | 4.3 (3.7) | 0.29 |
| General Family Functioning | 1.9 (0.6) | 1.8 (0.5) | 2.0 (0.7) | 0.02 |
| Psychological Characteristics | ||||
| Symptoms of Depression | 6.0 (3.8) | 5.7 (3.7) | 7.3 (3.9) | <0.001 |
| Symptoms of Anxiety | 6.9 (4.4) | 6.3 (4.1) | 9.0 (4.7) | <0.001 |
Testing for Potential Moderators
Hospital, gender, socioeconomic status, and relationship status did not moderate any of the paths. However, the path from family relationships to psychological distress differed by oxygen use. Individuals who were not on oxygen had a standardized path coefficient of .75, while individuals who were on oxygen had a standardized path coefficient of .61. Both path coefficients had a large effect size and were statistically significant. Thus, the link from family relationships to psychological distress was stronger among individuals who are not on oxygen than among individuals who are on oxygen; however, this path had a large effect size for both groups. All hypotheses were tested for the entire sample rather than splitting the sample according to oxygen use because the moderating effect of oxygen use was simply a matter of degree and did not alter substantive conclusions.
Hypothesis Testing
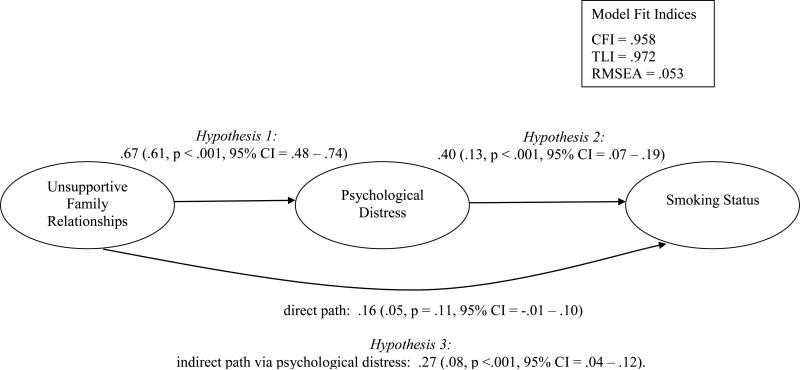
Model fit indices indicating how well the model fits the actual data were calculated. The scores (see Figure 2) were all within the published guidelines of >.95 for the Comparative Fit Index (CFI) and the Tucker-Lewis Index (TLI) [23] and <.08 for the Root Mean Square Error of Approximation (RMSEA) [24].
Figure 2.
Maximum Likelihood Estimates of the Associations among Family Relationships, Psychological Distress, and Smoking Status
Note: Standardized path coefficients outside parenthesis, unstandardized within parentheses
Hypothesis 1
Hypothesis 1 states that unsupportive family relationships are associated with psychological distress. The path from family relationships to psychological distress was highly significant (p < .001) and the standardized path coefficient was .67, indicating a large effect size.
Hypothesis 2
Hypothesis 2 states that psychological distress is associated with smoking status. The path from psychological distress to smoking status was highly significant (p < .001) and the standardized path coefficient was .40, indicating a medium effect size.
Hypothesis 3
Hypothesis 3 states that unsupportive family relationships are indirectly associated with smoking status via psychological distress. This hypothesis was tested by the strength of the indirect path from family relationships to smoking status via psychological distress. This indirect path was highly significant (p < .001), with a standardized path coefficient of .27 falling just short of the cutoff of .30 that is considered a medium effect size [22]. The direct path from family relationships to smoking status was not statistically significant, suggesting that the association between family relationships and smoking status is fully mediated by psychological distress.
DISCUSSION
This study extends the research on social and psychological factors that influence smoking behavior by considering a model of the joint influence of family relationships and psychological distress on smoking status of individuals with COPD. Results support the premise that unsupportive family relationships lead to psychological distress, which in turn affects smoking status. Since the data in the present study were cross-sectional, the direction of causality cannot be inferred solely from these data. However, the hypothesized direction of effect is consistent with prospective research demonstrating that family relationship quality influences the onset and course of depression and anxiety [7-10], and both family relationship quality [4-6] and depression and anxiety [11-14] influence smoking behavior. Nonetheless, it is likely that the associations among family relationships, psychological distress, and smoking behavior are very complex and possibly circular. For example, research indicates that smoking behavior influences psychological distress [25] and that genetic factors influence both smoking behavior and psychological distress [26].
The present study is important because it is the first study to link family relationship quality with psychological distress and smoking status among individuals with COPD. Results suggest that smoking cessation interventions for individuals with COPD may be most effective if they incorporate a focus on both family relationships and psychological distress. Family and relational treatments have already demonstrated effectiveness in treating depressive and anxiety disorders [10, 27]. Further, couple and family therapy have demonstrated utility as an intervention for multiple forms of drug addiction [28], including alcohol abuse [29]. A meta-analysis of treatments for drug abuse found that family therapy was more effective than individual therapy [30]. It is surprising that family members have not routinely been involved in smoking cessation interventions. In fact, both social and psychological factors are largely overlooked in treatment guidelines for smoking cessation among individuals with COPD.
Limitations of the study should be considered. As discussed above, analyses are based on cross-sectional data. Longitudinal studies are needed to establish the direction of causality. A second limitation is that 52% of the individuals who received a survey returned it and the response rate differed by medical center. This may limit generalizability of findings, and data from the university-affiliated hospital should be interpreted with more caution because there were fewer participants and a lower response rate from this hospital. Given the lower response rate from the university-affiliated hospital, it is more likely that responses are from a biased sample from this hospital than from the tertiary-care hospital. It would be informative to replicate this study in a university-affiliated hospital. A third limitation is that current smoking status was not biologically confirmed. Fourth, information regarding actual diagnosis of depression or anxiety was not gathered. Fifth, spirometry was not available to characterize COPD severity in this sample.
Strengths of this study include the fact that participants were recruited from two hospitals with very different patient populations. Despite the fact that patients from the tertiary-care hospital and the university-affiliated hospital differed so much from each other, the observed associations did not differ by hospital. This diverse sample also made it possible to test for moderating effects of gender, socioeconomic status, oxygen use, and relationship status. The overwhelmingly non-significant findings of the tests for moderators suggest that the model tested is relevant to a broad range of patients with COPD. Prior analyses based on this sample indicate that family relationship quality is associated with psychological distress, which in turn is associated with clinical features of COPD (i.e., breathlessness and quality of life) [31]. The present study focused on smoking—a key health behavior for individuals with COPD. It appears that a similar process may influence both health behaviors and clinical features of COPD.
Given the demographic differences between the two hospitals, it is not surprising that 90% of participants from the tertiary-care hospital had quit smoking while only 52% of participants from the university-affiliated hospital had quit smoking. Individuals with lower socioeconomic status are less likely to quit smoking [32, 33], and participants from the university-affiliated hospital had less education and lower incomes than participants from the tertiary-care hospital. Given the disparate rates of current smoking in the two hospitals, replication of this study with a different sample would be informative.
Results of this study suggest that family relationships are an important factor to include in future longitudinal research that attempts to elucidate social and psychological influences on smoking behavior. Exactly which aspects of family relationships are most influential needs to be further investigated. Criticism, blame, and nagging behaviors are likely to be important, as are more general aspects of family functioning such as marital satisfaction and problem-solving. More effective interventions to help individuals with COPD quit smoking are needed, and incorporating family and relational factors into treatment may lead to improvements in smoking cessation interventions.
Acknowledgments
We thank Richard Albert, MD; Thomas MacKenzie, MD, MSPH; Holly Batal, MD, MBA; Rebecca Hanratty, MD; and Jeanne Rozwadowski, MD; for their help recruiting participants for this study.
Funding/Support
This project was supported by funding from the National Institutes of Health [grants F32 HL083687, K23 HL091049], a Postdoctoral Research Fellowship Grant from the Alpha-1 Foundation, and the Flight Attendant Medical Research Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Clini E, Costi S, Lodi S, Rossi G. Non-pharmacological treatment for chronic obstructive pulmonary disease. Medical Science Monitor. 2003;9(12):RA300–5. [PubMed] [Google Scholar]
- 2.Rennard SI. Treatment of stable chronic obstructive pulmonary disease. Lancet. 2004;364(9436):791–802. doi: 10.1016/S0140-6736(04)16941-9. [DOI] [PubMed] [Google Scholar]
- 3.Nides MA, Rakos RF, Gonzales D, et al. Predictors of initial smoking cessation and relapse through the first 2 years of the Lung Health Study. J Consult Clin Psychol. 1995;63(1):60–9. doi: 10.1037//0022-006x.63.1.60. [DOI] [PubMed] [Google Scholar]
- 4.Gulliver SB, Hughes JR, Solomon LJ, Dey AN. An investigation of self-efficacy, partner support and daily stresses as predictors of relapse to smoking in self-quitters. Addiction. 1995;90(6):767–72. doi: 10.1046/j.1360-0443.1995.9067673.x. [DOI] [PubMed] [Google Scholar]
- 5.Key JD, Marsh LD, Carter CL, Malcolm RJ, Sinha D. Family-focused smoking cessation:enhanced efficacy by the addition of partner support and group therapy. Subst Abus. 2004;25(1):37–41. doi: 10.1300/J465v25n01_06. [DOI] [PubMed] [Google Scholar]
- 6.Roski J, Schmid LA, Lando HA. Long-term associations of helpful and harmful spousal behaviors with smoking cessation. Addict Behav. 1996;21(2):173–85. doi: 10.1016/0306-4603(95)00047-x. [DOI] [PubMed] [Google Scholar]
- 7.Whisman MA, Bruce ML. Marital dissatisfaction and incidence of major depressive episode in a community sample. J Abnorm Psychol. 1999;108(4):674–8. doi: 10.1037//0021-843x.108.4.674. [DOI] [PubMed] [Google Scholar]
- 8.Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry. 1998;55(6):547–52. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- 9.Hooley JM, Teasdale JD. Predictors of relapse in unipolar depressives: expressed emotion, marital distress, and perceived criticism. J Abnorm Psychol. 1989;98(3):229–35. doi: 10.1037//0021-843x.98.3.229. [DOI] [PubMed] [Google Scholar]
- 10.Marcaurelle R, Belanger C, Marchand A. Marital relationship and the treatment of panic disorder with agoraphobia: a critical review. Clin Psychol Rev. 2003;23(2):247–76. doi: 10.1016/s0272-7358(02)00207-6. [DOI] [PubMed] [Google Scholar]
- 11.Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, Bowes G. Depression, anxiety, and smoking initiation: a prospective study over 3 years. Am J Public Health. 1998;88(10):1518–22. doi: 10.2105/ajph.88.10.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Breslau N, Peterson EL, Schultz LR, Chilcoat HD, Andreski P. Major depression and stages of smoking. A longitudinal investigation. Arch Gen Psychiatry. 1998;55(2):161–6. doi: 10.1001/archpsyc.55.2.161. [DOI] [PubMed] [Google Scholar]
- 13.Anda RF, Williamson DF, Escobedo LG, Mast EE, Giovino GA, Remington PL. Depression and the dynamics of smoking. A national perspective. Jama. 1990;264(12):1541–5. [PubMed] [Google Scholar]
- 14.Glassman AH, Stetner F, Walsh BT, et al. Heavy smokers, smoking cessation, and clonidine. Results of a double-blind, randomized trial. Jama. 1988;259(19):2863–6. [PubMed] [Google Scholar]
- 15.Kunik ME, Roundy K, Veazey C, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127(4):1205–11. doi: 10.1378/chest.127.4.1205. [DOI] [PubMed] [Google Scholar]
- 16.Putman-Casdorph H, McCrone S. Chronic obstructive pulmonary disease, anxiety, and depression: state of the science. Heart Lung. 2009;38(1):34–47. doi: 10.1016/j.hrtlng.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Shields CG, Franks P, Harp JJ, McDaniel SH, Campbell TL. Development of the Family Emotional Involvement and Criticism Scale (FEICS): a self-report scale to measure expressed emotion. J Marital Fam Ther. 1992;18(4):395–407. [Google Scholar]
- 18.Evans RL, Bishop DS, Matlock AL, Stranahan S, Halar EM, Noonan WC. Prestroke family interaction as a predictor of stroke outcome. Arch Phys Med Rehabil. 1987;68(8):508–12. [PubMed] [Google Scholar]
- 19.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 20.Hajiro T, Nishimura K, Tsukino M, Ikeda A, Koyama H, Izumi T. Comparison of discriminative properties among disease-specific questionnaires for measuring health-related quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(3 Pt 1):785–90. doi: 10.1164/ajrccm.157.3.9703055. [DOI] [PubMed] [Google Scholar]
- 21.Dahlen I, Janson C. Anxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary disease. Chest. 2002;122(5):1633–7. doi: 10.1378/chest.122.5.1633. [DOI] [PubMed] [Google Scholar]
- 22.Kline RB. Principles and practice of structural equation modeling. Guilford Press; New York: 1998. [Google Scholar]
- 23.Hu L, Bentler PM. Cutoff criteria in fix indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- 24.Browne M, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long J, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–62. [Google Scholar]
- 25.Pedersen W, von Soest T. Smoking, nicotine dependence and mental health among young adults: a 13-year population-based longitudinal study. Addiction. 2009;104(1):129–37. doi: 10.1111/j.1360-0443.2008.02395.x. [DOI] [PubMed] [Google Scholar]
- 26.Kendler KS, Neale MC, MacLean CJ, Heath AC, Eaves LJ, Kessler RC. Smoking and major depression. A causal analysis. Arch Gen Psychiatry. 1993;50(1):36–43. doi: 10.1001/archpsyc.1993.01820130038007. [DOI] [PubMed] [Google Scholar]
- 27.Beach S. Affective disorders. J Marital Fam Ther. 2003;29:247–61. doi: 10.1111/j.1752-0606.2003.tb01203.x. [DOI] [PubMed] [Google Scholar]
- 28.Carroll KM, Onken LS. Behavioral therapies for drug abuse. Am J Psychiatry. 2005;162(8):1452–60. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Farrell TJ, Fals-Stewart W. Alcohol abuse. J Marital Fam Ther. 2003;29(1):121–46. doi: 10.1111/j.1752-0606.2003.tb00387.x. [DOI] [PubMed] [Google Scholar]
- 30.Stanton MD, Shadish WR. Outcome, attrition, and family-couples treatment for drug abuse: a meta-analysis and review of the controlled, comparative studies. Psychol Bull. 1997;122(2):170–91. doi: 10.1037/0033-2909.122.2.170. [DOI] [PubMed] [Google Scholar]
- 31.Holm KE, Bowler RP, Make BJ, Wamboldt FS. Family relationship quality is associated with psychological distress, dyspnea, and quality of life in COPD. COPD. 2009;6(5):359–68. doi: 10.1080/15412550903143919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Businelle MS, Kendzor DE, Reitzel LR, et al. Mechanisms linking socioeconomic status to smoking cessation: a structural equation modeling approach. Health Psychol. 2010;23(3):262–73. doi: 10.1037/a0019285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Broms U, Silventoinen K, Lahelma E, Koskenvuo M, Kaprio J. Smoking cessation by socioeconomic status and marital status: the contribution of smoking behavior and family background. Nicotine Tob Res. 2004;6(3):447–55. doi: 10.1080/14622200410001696637. [DOI] [PubMed] [Google Scholar]