Abstract
This study examined associations between sleep onset latency and emotional eating in a minority sample of children. A cross-sectional school-based study of sleep, psychological constructs, diet and physical activity was conducted in 6 public and private schools in Los Angeles County. An ethnically diverse sample of 356 third through fifth graders completed confidential self-report surveys. Multilevel regression (MLM) analyses were conducted to study associations while controlling for gender, ethnicity, and the random effect of school. Girls made up 57% of the total sample, which was predominantly Latino (42.6%), followed by African Americans (21.6%) and Asians (19.2%). MLM revealed that there were significant associations between sleep onset latency and emotional eating (p=.030), depressive symptomology (p<.0001) and trait anxiety (p<.0001). Sobel's test for mediation showed that trait anxiety (p=.011) but not depressive symptomology (p=.141) was a mediator of the relationship between sleep onset latency and emotional eating. Thereby providing a mechanism through which sleep onset latency is related to emotional eating. These findings suggest that sleep onset latency is associated with increased anxiety, depressive symptoms, and emotional eating. Although causal inferences cannot be drawn from this cross-sectional data, future studies should examine the possibility that problems falling asleep could lead to emotional dysregulation that in turn leads to emotional eating. Emotional eating may be one avenue by which sleep disturbances lead to overweight and obesity.
Keywords: anxiety, depression, sleep onset latency, emotional eating, mediation
1. Introduction
Pediatric obesity continues to rise, despite public health prevention efforts. Further, minority children are at increased risk. This epidemic highlights the need to identify mechanisms to supplement the traditional prevention efforts that focus solely on energy intake and expenditure. Sleep duration has recently been identified as a novel risk factor for overweight and obesity in youth as well as adults.
Sleep onset latency (SOL)1, or the amount of time it takes to fall asleep, can lead to short sleep, unless one is able to make up for a long SOL by delaying wake-up time. Research suggests that short sleep can lead to increased dietary intake, which in turn can lead to obesity. This relationship has been demonstrated through laboratory studies that reported increases in ghrelin, a hormone that stimulates hunger, decreases in leptin, a hormone that induces satiation and increased snacking/hunger following short sleep. Imaki (2002) also found that irregular meal patterns and snacking were related to insufficient sleep.
Research also shows that various sleep disturbances can impact psychological health. Nearly 10 years ago, Roberts et al. (2000) reported that almost all studies in adolescents that assessed psychological outcomes of sleep problems had found associations to depression. However recent extant literature on this subject is sparse. A twin study of 8-year old children found a correlation between parent-reported sleep and child-reported depressive symptoms. Sleep disturbances have also been related to anxiety. In a prospective study, Gregory and colleagues showed that sleep problems in childhood were predictive of anxiety in adulthood (60% increased odds of being diagnosed with an anxiety disorder). A review of the literature reported substantial overlap in children reporting sleep disturbances, anxiety and depression. The study of these associations in minority youth may be particularly relevant, considering research reporting higher sleep deprivation in this group.
Thayer (2001) posits that emotional eating occurs due to a state of “tense tiredness.” Thus, short sleep and related negative affective states may lead to eating in response to negative affect, or emotional eating. Psychosomatic Theory of Obesity posits that emotional eating (eating in order to deal with negative affective states, in the absence of hunger) contributes to obesity. Therefore, this paper explores the inter-relationships among SOL, psychological functioning and emotional eating in minority children. We predict that SOL will be associated with negative affect and emotional eating.
2. Methods
2.1. Sample
Participants were 357 elementary school children from public and parochial schools in Los Angeles County. Third through fifth grade minority children provided cross-sectional data for the study. Student data for this study were taken from a larger study which aimed to validate the use of psychosocial scales developed for older, non-minority populations for minority children.
2.2. Recruitment and Procedures
School selection was based upon the ethnic make up of the school, in order to obtain a predominantly Latino & African American sample. Schools were contacted directly and asked for the ethnic breakdown of their student population. Elementary school principals were contacted to gauge interest in their school's participation. Interested principals presented the study to third through fifth grade teachers and asked if they would like their classes to participate in the survey. Study description letters were provided to principals and teachers. We contacted ten school principals. Two were unable to spare the time to participate and two did not respond after initial contact. Thus, a total of six schools participated in the present study.
All children in the classrooms of interested teachers were invited to participate. The study coordinator explained the study and provided parent refusal forms to the students. Forms were available in both English and Spanish. Students were instructed to give the refusal forms, which included a description of the study, to their parents. Parents were asked to return the forms if they did not want their children to participate. Student assent forms were distributed to students that did not return parent refusal forms on the first day of data collection. Only students who did not have active parental refusal and provided written student assent were allowed to complete the survey. 73% of students participated in the study.
The paper-and-pencil confidential survey was administered at a time of day most convenient to the teacher. The survey included questions on sleep behaviors as well as psychosocial constructs, such as depression and anxiety. Time to complete the survey ranged from 30 minutes to 90 minutes, usually with younger students taking longer to complete the survey. Data collectors instructed participants on completing the survey and were available to answer questions. Bilingual education has been removed from public schools, therefore the surveys were in English language only, however Spanish speaking data collectors were available to answer questions. All procedures were approved by the Institutional Review Board, the school districts, and the Los Angeles Archdiocese.
2.3. Measures
2.3.1. Sleep onset latency (SOL)
The Sleep Habits Survey for adolescents was used to assess sleep onset latency. Students answered the question, “During the past month, how long has it usually taken you to fall asleep?” They reported their answers in hours and minutes. The Sleep Habits Survey has been shown to accurately represent actual sleep parameters in comparison with sleep diaries and actigraphy.
2.3.2. Trait anxiety
Trait Anxiety was measured using a modification of Zung's Self-rating Anxiety Scale (SAS; . The original 20-item measure has been shown to have good convergent and discriminant validity. The scale items and response options were simplified to increase child comprehension, based on qualitative feedback from this population (Cronbach α = .69).
2.3.3. Depression
A modified version of the Center for Epidemiological Studies Depression Scale (CES-D; was employed to measure depressive symptomology. The original 20-item scale has been used with adolescents and numerous studies support its validity and reliability. Items were simplified to increase understanding for younger children (Cronbach α = .79).
2.3.4. Emotional eating
A modified version of the emotional eating subscale (8-items) of the USA version of the Dutch Eating Behavior Questionnaire for Children (DEBQ-C) was employed to measure emotional eating. The DEBQ-C has been shown to have good psychometric qualities. With permission of the scale author, two items replaced one of the original items for which the English was unclear, thus the scale included on the survey included 8 items (Cronbach α = .84).
2.4. Data Analysis
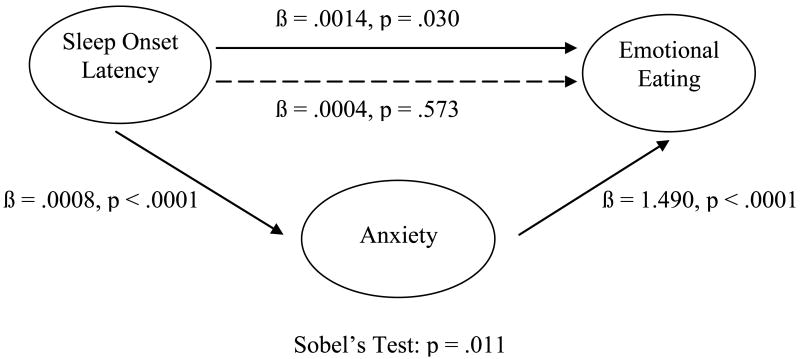
SAS v.9.1 software (Cary, NC) was used to conduct statistical analyses for the study. Descriptive statistics were calculated to present demographic data. Multilevel regression (MLM)2 analyses were conducted to study associations while controlling for gender, ethnicity, and the random effect of school. The Sobel Test for standard error was used to determine whether the influence of sleep onset latency on emotional eating was mediated by depression or anxiety (Figure 1). Steps for determining mediation based on Baron and Kenny's model were performed, followed by the Sobel Test for standard error to formally test if mediation was statistically significant.
Figure 1.
The Mediation Model
3. Results
Characteristics of the sample are reported in Table 1. The sample was of diverse ethnic background, with nearly 60% being female. Forty-one percent of students were in 5th grade, 34% in 3rd grade and 25% in 4th grade. There were no significant ethnic differences in any of the variables used in these analyses (data not shown).
Table 1.
Characteristics of the sample (n = 356)
| Variable | Mean (SD) | Range |
|---|---|---|
| Age (yrs) | 9.56 (1.03) | 8 – 12 |
| Femalea | 195 (57.4) | |
| Ethnicitya | ||
| African American | 72 (21.6) | |
| Asian | 64 (19.2) | |
| Latino | 142 (42.6) | |
| Mixed | 37 (11.1) | |
| Other | 18 (5.4) | |
| Sleep Onset Latency (mins) | 56.30 (59.90) | 0 - 210 |
| Anxiety | 0.5093 (0.10) | 0.27 – 0.89 |
| Depression | 19.29 (9.55) | 0 - 46 |
| Emotional Eating | 1.48 (0.47) | 1 - 3 |
n (%)
Multi-level regression analyses revealed associations among sleep onset latency, anxiety, depression, and emotional eating (Figures 1 and 2). Specifically, SOL showed statistically significant relationships with emotional eating (ß = .0014, p = .0298), anxiety (ß = .0008, p < .0001), and depression (ß = .0752, p < .0001). Further analyses revealed that anxiety (ß = 1.485, p < .0001) and depression (ß = .0108, p = .0017) were also significantly associated with emotional eating. Thus, additional regression analyses, including the same covariates and random effect of school, tested for the mediating effect of anxiety and depression (in separate models) in the relationship between SOL and emotional eating.
Results showed that when anxiety was included in the model regressing SOL on emotional eating, the association between these two variables became non-significant (p = .5727). The same was found when depression was included in the model (p = .2213), however in this model, the path between depression and emotional eating also become non-significant (p = .1250). Sobel's Test of the indirect effect indicated that there was a significant mediating effect for anxiety (p = .0116), but not for depression (p = .1412), in the association between SOL and emotional eating (Figures 1 and 2).
4. Discussion
The present study aimed to test relationships among sleep onset latency, psychological constructs and emotional eating. As hypothesized, and consistent with the literature that shows sleep disturbance is associated with anxiety and depression (e.g. Gregory 2005, 2006), we found a positive association between SOL and both negative affect (anxiety and depression) and emotional eating. Further analyses revealed that anxiety fully mediated the relationship between SOL and emotional eating. These findings provide a possible mechanism through which sleep problems, namely short sleep, can lead to obesity. Taking a long time to fall asleep may lead to increased anxiety; this anxiety can then result in emotional eating. If one is overeating due to emotional arousal rather than in response to physiological hunger, this has the potential to lead to overweight and obesity.
These data relied on self-reported data for all measures, which may bring into question the accuracy of the data. Although, studies have shown child reports of sleep behavior to be more accurate than parent report, replication of findings using objective measures of sleep such as actigraphy or polysomnography would enhance the validity of findings.
Reducing SOL could result in sleep extension and reduced risk for overeating. Therefore, reduction of SOL might provide a novel obesity intervention component for minority youth, a population in which obesity prevention and treatment efforts have been predominantly unsuccessful. The modifiable nature of sleep behaviors holds promise as a potential means for obesity prevention. At minimum, improving sleep in our youth may improve psychological well-being, which is certainly as important as physical well-being.
Acknowledgments
We would like to thank the LAUSD, AUSD & the Roman Catholic Archdiocese for their continued support of our research. Special thanks to all of our participants and to our fellow lab members who volunteered to assist in data collection as well as our data entry staff.
Footnotes
SOL = Sleep onset latency
MLM = Multilevel regression
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Arianna D. McClain, Email: admcclai@usc.edu.
Donna Spruijt-Metz, Email: dmetz@usc.edu.
References
- Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk factors for childhood overweight: a prospective study from birth to 9.5 years. The Journal of Pediatrics. 2004;145:20–25. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Chorney D, Detweiler M, Morris T, Kuhn B. The interplay of sleep disturbance, anxiety, and depression in children. Journal of Pediatric Psychology. 2007;33(4):339–348. doi: 10.1093/jpepsy/jsm105. [DOI] [PubMed] [Google Scholar]
- Davis JN, Kelly LA, Lane CJ, Ventura EE, Byrd-Williams CE, Alexandar KA, et al. Randomized control trial to improve adiposity and insulin resistance in overweight Latino adolescents. Obesity. 2009;17:1542–15488. doi: 10.1038/oby.2009.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory A, Caspi A, Eley T, Moffitt T, O’Connor T, Poulton R. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. Journal of Abnormal Child Psychology. 2005;33:157–163. doi: 10.1007/s10802-005-1824-0. [DOI] [PubMed] [Google Scholar]
- Gregory A, Rijsdijk F, Dahl R, McGuffin P, Eley T. Associations between sleep problems, anxiety, and depression in twins at 8 years of age. Pediatrics. 2006;118:1124–1132. doi: 10.1542/peds.2005-3118. [DOI] [PubMed] [Google Scholar]
- Gruber R, Sadeh A, Raviv A. Sleep of school-age children: objective and subjective measures. Sleep Research. 1997;26:158. [Google Scholar]
- Ievers-Landis CE, Storfer-Isser A, Rosen C, Johnson NL, Redline S. Relationship of sleep parameters, child psychological functioning, and parenting stress to obesity status among preadolescent children. Journal of Developmental & Behavioral Pediatrics. 2008;29:243–252. doi: 10.1097/DBP.0b013e31816d923d. [DOI] [PubMed] [Google Scholar]
- Imaki M, Hatanaka Y, Ogawa Y, Yoshida Y, Tanada S. An epidemiological study on relationship between the hours of sleep and life style factors in Japanese factory workers. Journal of physiological anthropology and applied human science. 2002;21:115–120. doi: 10.2114/jpa.21.115. [DOI] [PubMed] [Google Scholar]
- Kaplan HI, Kaplan H. The psychosomatic concept of obesity. Journal of Nervous & Mental Disease. 1957;125:181–200. doi: 10.1097/00005053-195704000-00004. [DOI] [PubMed] [Google Scholar]
- Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- Levi J, Gadola E, Segal LM. F as in fat: How obesity policies are failing in America. Washington, DC: Trust for America's Health; 2006. [Google Scholar]
- Ogden CL, Carroll MD, Flegal KM. High Body Mass Index for Age Among US Children and Adolescents, 2003-2006. JAMA. 2008;299:2401. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- Owens J, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. Journal of Developmental & Behavioral Pediatrics. 2000;21:27–36. doi: 10.1097/00004703-200002000-00005. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general oopulation. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, et al. Early life risk factors for obesity in childhood: cohort study. British Medical Journal. 2005;330:1357. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts R, Shema S, Kaplan G, Strawbridge W. Sleep complaints and depression in an aging cohort: a prospective perspective. The American Journal of Psychiatry. 2000;157:81–88. doi: 10.1176/ajp.157.1.81. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Washington DC: American Sociological Association; 1982. [Google Scholar]
- Spiegel K, Leproult R, L'Hermite-Baleriaux M, Copinschi G, Penev PD, Van Cauter E. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. Journal of Clinical Endocrinology & Metabolism. 2004;89:5762–5771. doi: 10.1210/jc.2004-1003. [DOI] [PubMed] [Google Scholar]
- Spiegel K, Leproult R, Tasali E, Penev P, Van Cauter E. Sleep curtailment results in decreased leptin levels and increased hunger and appetite. Sleep. 2003;26:A174. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine. 2004;141:846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- Spilsbury JC, Storfer-Isser A, Drotar D, Rosen CL, Kirchner LH, Benham H, et al. Sleep behavior in an urban US sample of school-aged children. Archives of Pediatrics & Adolescent Medicine. 2004;158:988–994. doi: 10.1001/archpedi.158.10.988. [DOI] [PubMed] [Google Scholar]
- Spruijt-Metz D, Nguyen-Michel ST, Goran MI, Chou CP, Huang TT. Reducing sedentary behavior in minority girls via a theory-based, tailored classroom media intervention. Int J Pediatr Obes. 2008;3:240–248. doi: 10.1080/17477160802113415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:210. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer R. Calm Energy: How people regulate mood with food and exercise. Oxford; Oxford University Press; 2001. [Google Scholar]
- van Strien T, Oosterveld P. The children's DEBQ for assessment of restrained, emotional, and external eating in 7- to 12-year-old children. Int J Eat Disord. 2008;41:72–81. doi: 10.1002/eat.20424. [DOI] [PubMed] [Google Scholar]
- Vioque J, Torres A, Quiles J. Time spent watching television, sleep duration and obesity in adults living in Valencia, Spain. International Journal of Obesity. 2000;24:1683–1688. doi: 10.1038/sj.ijo.0801434. [DOI] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26:213–216. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]