Abstract
Purpose
Verbal memory decline is a frequent complication of left anterior temporal lobectomy (L-ATL). The goal of this study was to determine whether preoperative language mapping using functional magnetic resonance imaging (fMRI) is useful for predicting which patients are likely to experience verbal memory decline after L-ATL.
Methods
Sixty L-ATL patients underwent preoperative language mapping with fMRI, preoperative intracarotid amobarbital (Wada) testing for language and memory lateralization, and pre- and postoperative neuropsychological testing. Demographic, historical, neuropsychological, and imaging variables were examined for their ability to predict pre- to postoperative memory change.
Results
Verbal memory decline occurred in over 30% of patients. Good preoperative performance, late age at onset of epilepsy, left dominance on fMRI, and left dominance on the Wada test were each predictive of memory decline. Preoperative performance and age at onset together accounted for roughly 50% of the variance in memory outcome (p < .001), and fMRI explained an additional 10% of this variance (p ≤ .003). Neither Wada memory asymmetry nor Wada language asymmetry added additional predictive power beyond these noninvasive measures.
Discussion
Preoperative fMRI is useful for identifying patients at high risk for verbal memory decline prior to L-ATL surgery. Lateralization of language is correlated with lateralization of verbal memory, whereas Wada memory testing is either insufficiently reliable or insufficiently material-specific to accurately localize verbal memory processes.
Keywords: fMRI, memory, temporal lobectomy, language dominance, Wada test
Introduction
Brain surgery is an effective treatment for individuals who suffer from medically intractable epilepsy (Wiebe et al., 2001; Tellez-Zenteno et al., 2005). One common surgical procedure for epilepsy is anterior temporal lobectomy (ATL), which produces long-term cure rates of approximately 60–80% (McIntosh et al., 2001; Tellez-Zenteno et al., 2005). Common complications of ATL include upper quadrant visual field defects (Hughes et al., 1999; Barton et al., 2005), impairments on naming and other language tasks (Hermann et al., 1994; Langfitt & Rausch, 1996; Bell et al., 2000b; Sabsevitz et al., 2003), and declarative memory deficits. ATL typically involves removal of much of the anterior medial temporal lobe (MTL), including portions of the hippocampus and parahippocampus, which are known to be critical for encoding and retrieval of long-term episodic memories (Squire, 1992). Verbal memory decline after left ATL is a consistent finding in group studies (Chelune et al., 1991; Hermann et al., 1995; Kneebone et al., 1995; Loring et al., 1995b; Helmstaedter & Elger, 1996; Martin et al., 1998; Chiaravalloti & Glosser, 2001; Sabsevitz et al., 2001; Lee et al., 2002; Stroup et al., 2003; Baxendale et al., 2006; Lineweaver et al., 2006) and is much more frequent than non-verbal memory decline after right ATL (Lee et al., 2002). Studies using longitudinal neuropsychological methods that sensitively measure memory encoding processes show that significant verbal memory decline occurs in 30–60% of patients who undergo left ATL (Chelune et al., 1993; Martin et al., 1998; Sabsevitz et al., 2001; Stroup et al., 2003; Gleissner et al., 2004; Baxendale et al., 2006; Lineweaver et al., 2006). One principal goal of the preoperative evaluation in ATL candidates is, therefore, to estimate the risk of verbal memory decline.
Functional memory asymmetry during the intracarotid amobarbital, or Wada, test is predictive of verbal memory decline from left ATL, in that patients who show memory functions lateralized to the side of surgery are more likely to decline (Kneebone et al., 1995; Loring et al., 1995b; Bell et al., 2000a; Chiaravalloti & Glosser, 2001; Sabsevitz et al., 2001). Other studies have not found this test to be strongly predictive, however (Chelune & Najm, 2000; Stroup et al., 2003; Lacruz et al., 2004; Kirsch et al., 2005; Lineweaver et al., 2006), and many authors have raised concerns about its specificity and test-retest reliability (Novelly & Williamson, 1989; Loring et al., 1990; Lee et al., 1995; Kubu et al., 2000; Simkins-Bullock, 2000; Martin & Grote, 2002; Loddenkemper et al., 2007). Other presurgical tests of MTL functional or anatomical asymmetry are also modestly predictive of memory outcome, including structural MRI of the hippocampus (Trenerry et al., 1993; Chelune & Najm, 2000; Wendel et al., 2001; Stroup et al., 2003; Cohen-Gadol et al., 2004; Lineweaver et al., 2006) and inter-ictal positron emission tomography (Griffith et al., 2000). Preoperative neuropsychological testing also has predictive value, in that patients with good memory abilities prior to surgery are more likely to decline than patients with poor preoperative memory (Chelune et al., 1991; Hermann et al., 1995; Helmstaedter & Elger, 1996; Jokeit et al., 1997; Davies et al., 1998; Stroup et al., 2003; Gleissner et al., 2004; Baxendale et al., 2006; Lineweaver et al., 2006; Baxendale et al., 2007).
Our aim in the present study was to determine the value of preoperative functional magnetic resonance imaging (fMRI) for predicting verbal memory decline from left ATL. A previously published fMRI study demonstrated promising results in a small patient sample (Richardson et al., 2006). This prior study and two that examined nonverbal memory decline (Rabin et al., 2004; Janszky et al., 2005) focused on activation in the hippocampus and surrounding medial temporal lobe. Given the relative difficulty of measuring robust activation signals in the hippocampus with fMRI, we explored the possibility that a language lateralization test might provide information concerning verbal memory lateralization. The fMRI protocol we used provides a language lateralization measure that is strongly correlated with Wada language asymmetry (Binder et al., 1996) and predicts language outcome after left ATL (Sabsevitz et al., 2003). Here we assess the ability of this test to predict verbal memory decline after left ATL, and we compare its predictive power to other standard tests used for this purpose, including the Wada memory test.
Methods
Participants
Participants were 60 consecutively encountered patients with intractable left temporal lobe epilepsy, who were treated with left ATL (L-ATL) at the Medical College of Wisconsin Comprehensive Epilepsy Program between 1995 and 2006, and who met the following criteria: (a) preoperative fMRI language mapping performed, (b) preoperative and 6-month-postoperative neuropsychological evaluation performed, and (c) full scale IQ > 70. Three other L-ATL patients who otherwise met criteria were excluded because fMRI showed very low levels of activation. Wada data were not available for 4 of the 60 L-ATL patients included in the sample. Three of these patients were judged to have had either an invalid Wada memory test (2 patients) or an invalid Wada language test (1 patient), mainly due to excessive obtundation during anesthetization. Wada testing in the fourth patient was aborted because of a left hemisphere ischemic event. The patient was given intra-arterial tPA and had full recovery within 24 hours, with no infarction observed on MRI. Repeat neuropsychological testing in this patient prior to surgery showed no change from before the attempted Wada. These 4 patients were included in all of the fMRI analyses but excluded from all univariate and multivariate analyses involving the Wada asymmetry scores. Sixty-two consecutively encountered patients who underwent right ATL (R-ATL) with pre- and post-operative neuropsychological testing served as a comparison group to evaluate verbal memory changes in the L-ATL patients. One prior study showed that RATL patients are as likely to experience a verbal memory decline as they are a verbal memory improvement (Martin et al., 1998).
All patients underwent a standard ATL resection removing the anterior 3 to 4 cm of the temporal lobe, including lateral (middle temporal gyrus, inferior temporal gyrus, polar superior temporal gyrus) and medial (fusiform gyrus, parahippocampus, amygdala, anterior hippocampus) structures. The posterior extent of resection was tailored using electrocorticography in all patients and intra- or extraoperative stimulation mapping of language cortex when the language-dominant temporal lobe was resected. The same epilepsy surgeon performed all operations. FMRI data were collected for research purposes only and were not available to the surgeon before or after surgery. Informed consent was obtained from all patients prior to fMRI using a protocol approved by the Institutional Review Board of the Medical College of Wisconsin.
Patient demographic information is summarized in Table 1. The L-ATL and R-ATL groups did not differ on age, sex, years of education, handedness, age at onset of epilepsy (defined as the age at onset of recurring seizures), epilepsy duration, or measures of intelligence (all P values > 0.1).
TABLE 1.
Patient data.
| Left ATL | Right ATL | L vs. R | |
|---|---|---|---|
| Mean (SD) | Mean (SD) | p | |
| n | 60 | 62 | |
| Age at Surgery, y | 37.4 (10.0) | 40.3 (10.2) | n.s. |
| Sex, F/M | 29/31 | 39/23 | n.s. |
| Education, y | 13.2 (2.3) | 13.4 (2.7) | n.s. |
| Handedness, R/L/A | 48/11/1 | 49/9/4 | n.s. |
| Age at Epilepsy Onset, y | 15.1 (10.2) | 14.9 (11.3) | n.s. |
| Epilepsy Duration, y | 21.6 (13.0) | 24.5 (13.9) | n.s. |
| Full Scale IQ | 93.0 (12.4) | 93.3 (12.2) | n.s. |
| Verbal IQ | 91.9 (11.4) | 93.3 (12.8) | n.s. |
| Performance IQ | 95.8 (13.9) | 94.6 (12.6) | n.s. |
| Wada Language Asymmetry* | .548 (.531) | .825 (.249) | 0.0003 |
| Wada Memory Asymmetry* | −.251 (.446) | .634 (.310) | <0.0001 |
| FMRI Lateral Hemisphere LI** | .447 (.431) | .638 (.381) | 0.0125 |
F = female, M = male, R = right-handed, L = left-handed, A = ambidextrous, y = years
Wada data are based on 56 left ATL and 62 right ATL patients.
FMRI data are based on 60 left ATL and 57 right ATL patients
Neuropsychological Measures
All patients were administered a comprehensive neuropsychological examination both before and 6 months following ATL surgery. Testing at more time points was not considered practical given the other extensive testing requested of the patients. Existing data suggest that memory deficits measured in the first few months after left ATL surgery remain relatively stable at 1 year (Gleissner et al., 2004). Left ATL patients in one large study showed continued decline in verbal memory between 6 months and 2 years after surgery (Alpherts et al., 2006), a delayed effect that may or may not be attributable to the surgery. We thus selected the 6-month time point as the best index of performance change likely to be related to the surgery.
The 6-trial Selective Reminding Test (SRT) was used to assess verbal episodic memory (Buschke & Fuld, 1974). The SRT is a word list learning test with six recall trials. Patients are first presented with the full list of 12 words, and then receive “selective reminding” prior to each subsequent recall trial, consisting of presentation of only the items that were not recalled on the preceding trial. Multiple measures are computed during this learning phase of the test, including Long-Term Storage (LTS), an index of the ability to enter information into long-term storage (any word that is recalled on two consecutive trials), and Consistent Long-Term Recall (CLTR), an index of the ability to consistently retrieve information from long-term storage (words recalled on every subsequent trial). Free recall is tested without warning 30 minutes after the initial learning phase, yielding a Delayed Recall score. Finally, a recognition test is given after the free recall phase, in which patients hear the 12 list words mixed with 12 new words not on the list and indicate whether or not each item was on the list. Correct responses (hits and correct rejections) are summed to give a Recognition score.
Other memory measures administered at both testing sessions included the Logical Memory (LM) and Visual Reproduction (VR) subtests from the Wechsler Memory Scale Revised (WMS-R, 95 patients) or Wechsler Memory Scale III (WMS-III, 27 patients) (Wechsler, 1987, 1997), which measure immediate and delayed recall of prose passages and geometric designs respectively, and the 7/24 Spatial Recall Test (Rao et al., 1984). The 7/24 is a spatial pattern-learning test in which the patient is presented with an array of seven checkers on a 6 × 4 grid for 10 seconds over five learning trials. The patient is asked to reproduce the spatial pattern from memory after each exposure. Free recall is tested after a 30-minute delay. The total number of correctly placed checkers over the five learning trials constitutes the learning score. The number of correctly placed checkers after the delay period constitutes the delayed recall score.
Pre- to post-operative change scores on each of these tests were calculated by subtracting the pre-operative score from the post-operative score. Positive values thus indicate improvement, whereas negative values indicate a decline in performance. Change scores for the SRT and 7/24 measures were calculated from raw scores. Because raw scores from the WMS-R and WMS-III are not comparable, WMS scores were converted to standard scores using tables provided in the WMS manuals. WMS raw scores have also been provided in Table 2 for the subgroup of patients tested with the WMS-R. Some previous studies of cognitive outcome after epilepsy surgery have used regression-based change indices derived from test-retest changes observed in normative samples (Chelune et al., 1993; Hermann et al., 1996; Davies et al., 1998; Martin et al., 1998; Stroup et al., 2003; Baxendale et al., 2006; Lineweaver et al., 2006). Because subjects often show slight improvements on re-testing, due either to practice effects or regression toward the mean, this regression approach is a more sensitive method for detecting decline. In the current study, however, we focused on absolute change in performance, as these values may be more meaningful for clinicians and patients in formulating a pragmatic interpretation of the results. Furthermore, test-retest normative data necessary for computing regression-based change indices are not available for several of our key measures (e.g., SRT, 7/24).
TABLE 2.
Neuropsychological test scores.
| Left ATL | Right ATL | L vs. R | ||
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | p | ||
| SRT CLTR | Pre-op | 29.5 (13.5) | 33.2 (14.7) | n.s. |
| Post-op | 16.7 (12.4) | 38.7 (14.9) | <0.0001 | |
| Change | −12.8 (16.1)* | 5.5 (14.8) | <0.0001 | |
| Number (%) Declining | 20 (33%) | 3 (5%) | ||
| SRT LTS | Pre-op | 40.6 (12.2) | 43.8 (12.6) | n.s. |
| Post-op | 28.1 (13.6) | 49.3 (11.4) | <0.0001 | |
| Change | −12.5 (15.7)* | 5.5 (14.0) | <0.0001 | |
| Number (%) Declining | 27 (45%) | 3 (5%) | ||
| SRT Delayed Recall | Pre-op | 5.95 (2.96) | 7.25 (2.81) | 0.0186 |
| Post-op | 3.29 (2.55) | 8.04 (2.70) | <0.0001 | |
| Change | −2.66 (3.23)* | 0.79 (2.48) | <0.0001 | |
| Number (%) Declining | 31 (55%) | 3 (6%) | ||
| SRT Recognition | Pre-op | 21.91 (3.10) | 22.54 (2.42) | n.s. |
| Post-op | 20.21 (4.12) | 22.79 (2.22) | <0.0001 | |
| Change | −1.83 (3.89)* | 0.58 (2.44) | 0.0003 | |
| Number (%) Declining | 14 (26%) | 2 (4%) | ||
| WMS LM1 | Pre-op | 93.6 (15.2) | 95.7 (15.8) | n.s. |
| Post-op | 85.6 (11.9) | 96.5 (12.6) | <0.0001 | |
| Change | −8.0 (13.3)* | 0.8 (11.2) | 0.0001 | |
| Number (%) Declining | 16 (27%) | 5 (8%) | ||
| WMS LM2 | Pre-op | 89.0 (13.5) | 92.6 (14.2) | n.s. |
| Post-op | 83.3 (13.2) | 94.9 (13.2) | <0.0001 | |
| Change | −5.8 (12.9)* | 2.3 (11.7) | 0.0004 | |
| Number (%) Declining | 11 (18%) | 3 (5%) | ||
| (WMS-R LM1) | Pre-op | 21.8 (8.2) | 23.3 (7.8) | n.s. |
| Post-op | 17.1 (6.7) | 23.5 (6.2) | <0.0001 | |
| Change | −4.7 (6.7)* | 0.3 (5.3) | 0.0001 | |
| (WMS-R LM2) | Pre-op | 15.0 (8.4) | 17.0 (8.4) | n.s. |
| Post-op | 10.7 (7.3) | 17.7 (7.2) | <0.0001 | |
| Change | −4.3 (7.2)* | 1.1 (7.8) | 0.0008 | |
| WMS VR1 | Pre-op | 100.1 (17.1) | 100.6 (17.8) | n.s. |
| Post-op | 100.1 (18.3) | 99.4 (18.0) | n.s. | |
| Change | −0.0 (15.9) | −1.2 (16.5) | n.s. | |
| Number (%) Declining | 3 (5%) | 3 (5%) | ||
| WMS VR2 | Pre-op | 98.9 (15.9) | 94.6 (15.7) | n.s. |
| Post-op | 97.2 (15.7) | 96.6 (16.7) | n.s. | |
| Change | −1.5 (14.1) | 2.0 (16.8) | n.s. | |
| Number (%) Declining | 4 (7%) | 5 (8%) | ||
| 7/24 Total | Pre-op e | 29.9 (5.1) | 29.8 (5.7) | n.s. |
| Post-op | 29.9 (5.4) | 29.7 (5.8) | n.s. | |
| Change | 0.0 (5.6) | −0.1 (6.7) | n.s. | |
| Number (%) Declining | 3 (5%) | 5 (8%) | ||
| 7/24 Delayed Recall | Pre-op | 5.59 (1.73) | 5.07 (1.96) | n.s. |
| Post-op | 5.50 (1.64) | 4.83 (2.02) | n.s. | |
| Change | −0.09 (2.04) | −0.24 (2.74) | n.s. | |
| Number (%) Declining | 1 (2%) | 3 (5%) |
SRT CLTR = consistent long-term recall score from the Selective Reminding Test.
SRT LTS = long-term storage score from the Selective Reminding Test.
WMS LM1 = Logical Memory 1 standard scores from the WMS-R or WMS-III.
WMS LM2 = Logical Memory 2 standard scores from the WMS-R or WMS-III.
(WMS-R LM1) = LM 1 raw scores from a subgroup of patients who took the WMS-R.
(WMS-R LM2) = LM 2 raw scores from a subgroup of patients who took the WMS-R.
WMS VR1 = Visual Reproduction 1 standard scores from the WMS-R or WMS-III.
WMS VR2 = Visual Reproduction 2 standard scores from the WMS-R or WMS-III.
- SRT Delayed Recall based on 56 left and 53 right ATL patients,
- SRT Recognition based on 53 left and 52 right ATL patients,
- WMS-R raw scores based on 44 left and 51 right ATL patients,
- WMS VR2 based on 59 left and 62 right ATL patients,
- 7/24 Delayed Recall based on 58 left and 59 right ATL patients.
Mean change score significantly different from zero after Bonferroni correction for multiple comparisons (p < 0.002).
To calculate sensitivity and specificity measures, L-ATL patients were nominally classified as either showing or not showing decline on each test, defined as a negative change score of 1.5 standard deviations or more from the mean change score in the R-ATL group. The resulting cutoff values are somewhat conservative and represent substantial declines, generally in the range of 40–60% relative to pre-operative raw scores.
Wada Test Methods
Wada language and memory testing followed procedures described previously (Loring et al., 1992; Binder et al., 1996). Each hemisphere was tested separately for language and episodic memory competence by injecting 75 to 125 mg of amobarbital into the contralateral internal carotid artery. Return of motor function in the hemiplegic upper extremity was used as a gauge of the duration of hemisphere anesthesia. Multiple language functions were assessed during anesthesia, including counting, comprehension of commands, object naming, phrase repetition, and sentence reading. These tests were repeated until all functions returned to baseline levels. Resolution of anesthesia was determined by return of language, cessation of delta activity on EEG, return of full motor strength, and absence of contralateral asterixis. All language task performances were rated on a scale of 0 to 3, with higher scores reflecting better performance. Overall performance for each hemisphere was then calculated as the total score across all tests divided by the total score possible, yielding values ranging from 0 to 1. Immediately after recovery from the anesthetic, a 24-item object memory recognition test was administered. Eight target objects that had been presented in the visual field ipsilateral to the injection and named aloud by the examiner during the period of anesthesia and 16 novel foil objects were presented in a random order, and patients were required to indicate whether or not each object had been presented previously. A recognition memory score for each hemisphere, corrected for guessing, was calculated as the number of items correctly recognized minus half the number of false positive responses. These raw scores, which can range from 0 to 8, were divided by 8 to yield values ranging from 0 to 1.
Wada language asymmetry (WLA) was calculated as the difference between the performances of the left hemisphere (inject right) and the right hemisphere (inject left) (Binder et al., 1996). WLA values range from −1, reflecting strong language lateralization toward the right hemisphere, to +1, reflecting strong lateralization toward the left hemisphere.
Wada memory asymmetry (WMA) was calculated in an analogous manner by taking the difference between the recognition memory performances of the left hemisphere (inject right) and the right hemisphere (inject left), yielding values ranging from −1 (all memory capacity in the right hemisphere) to +1 (all memory capacity in the left hemisphere). As a check on the validity of this test as a measure of medial temporal lobe function, we compared WMA values in the left and right ATL groups. As shown in Table 1, WMA was lateralized to the right in the L-ATL group and strongly lateralized to the left in the R-ATL group. Using an optimal category boundary value of 0.3, the WMA correctly classified 89% of the patients as to side of seizure focus, consistent with previous reports (Kneebone et al., 1997; Alpherts et al., 2000; Cohen-Gadol et al., 2004).
MRI Acquisition
Imaging was conducted on either a 1.5 T GE Signa scanner (55 patients) or a 3 T GE Excite scanner (5 patients). High-resolution, T1-weighted anatomical reference images of the entire brain were acquired with a spoiled-gradient-echo (“SPGR”) sequence. Whole brain functional imaging used a T2*-weighted gradient-echo, echoplanar sequence with the following parameters at 1.5 T: TE = 40 ms, TR = 3000 ms, field of view = 240 mm, pixel matrix = 64 × 64, 19 sagittal slices, voxel size = 3.75 × 3.75 × 7 mm. Echoplanar imaging parameters at 3 T were as follows: TE = 25 ms, TR = 3000 ms, field of view = 224 mm, pixel matrix = 64 × 64, 34 axial slices, voxel size = 3.5 mm3.
FMRI Activation Tasks
Each functional imaging series consisted of multiple periods of baseline, in which patients performed a tone decision task, alternating with periods of language activation, in which patients performed a semantic decision task. The stimuli and activation tasks, their rationale, and the typical patterns of activation and lateralization observed in normal participants were described previously (Binder et al., 1997; Frost et al., 1999; Springer et al., 1999; Szaflarski et al., 2002). During the tone decision task, patients heard brief sequences of 3 to 7 tones of either low (500 Hz) or high (750 Hz) frequency and were instructed to press a button for any sequence containing two high tones. This task provides a control for low-level auditory processing in the superior temporal region and for nonlinguistic attentional and decision-making processes in the lateral frontal lobe (Binder et al., 1997). During the semantic decision task, patients were presented with spoken English nouns designating animals (i.e., “sheep”) and were instructed to press a button for animals they considered to be both “found in the United States” and “used by humans.” The contrast between semantic decision and tone decision tasks emphasizes additional demands on speech perception and lexical-semantic processes during the semantic decision task. This contrast produces highly reliable and strongly left-lateralized activation in areas previously implicated in language processing, including frontal, temporal, and parietal association cortices (Binder et al., 1997; Frost et al., 1999), and in the left hippocampus and surrounding medial temporal lobe (Binder et al., 1997; Bellgowan et al., 1998).
FMRI Data Analysis
Image processing and statistical analyses were conducted with AFNI (http://afni.nimh.nih.gov/afni). All analyses were performed at the individual subject level. Image alignment was used to reduce the effects of head movement. Task-related changes in MRI signal were identified using multiple regression. This method compares the time series of MRI signal values in each image voxel with an idealized hemodynamic response to the task alternation. The idealized response was modeled by convolving a gamma function with a time series of impulses representing each task trial. The regression model also included six movement vectors (computed during image registration) to further reduce any effects of head movement on estimation of the task response, and first- and second-order covariates to model any linear or quadratic baseline shifts. Significantly activated voxels were defined as those with a task effect beta coefficient corresponding to p < 0.001
Six region-of-interest (ROI) volumes were defined based on an average left hemisphere activation map from 80 normal, right-handed participants (Frost et al., 1999; Szaflarski et al., 2002). Mirror-image right hemisphere ROIs were created by reflecting these volumes symmetrically across the midline. The ROIs included left and right frontal lobe, left and right temporal lobe (including both medial and lateral temporal regions), and left and right lateral hemispheres. The latter included all activated regions in the lateral aspect of the frontal, temporal, and parietal lobes and excluded medial hemispheric regions. Significantly activated voxels were counted for each patient in each of the 6 ROIs. Laterality indexes (LI), reflecting the interhemispheric difference between voxel counts in left and right homologous ROIs, were calculated for each ROI using the formula: LI = [L−R]/[L+R] (Binder et al., 1996; Springer et al., 1999; Sabsevitz et al., 2003). As with the Wada asymmetry scores, the fMRI LIs range from −1 (all active voxels in the right hemisphere) to +1 (all active voxels in the left hemisphere).
Results
Pre- and Post-Operative Memory Performance
A variety of verbal and non-verbal episodic memory measures were obtained before and after ATL surgery. Table 2 shows the average pre-operative, post-operative, and pre-post change scores for each ATL group on these tests. The percentage of patients who declined is shown for each test.
As a group, the L-ATL patients showed significant decline on all verbal memory measures, most notably the CLTR, LTS, and Delayed Recall measures from the SRT. Change scores for the L-ATL group on these tests were all reliably below zero and differed from the R-ATL group, which showed slight improvements on these measures. The L-ATL group also declined, relative to change scores in the R-ATL group, on the Recognition subtest of the SRT and the Immediate and Delayed Logical Memory subtests (LM1 and LM2) from the Wechsler Memory Scale.
Change scores on all tests were highly variable, with some L-ATL patients showing marked decline and others showing modest improvements. Most notably, 45% of L-ATL patients declined on the LTS measure (i.e., showed at least a 16 point drop in raw score, or 39% relative to the pre-op average) and 55% declined on the Delayed Recall test (at least a 3 point, or ≥50%, drop) from the SRT. On the CLTR, 20 patients (33%) had an absolute decline of 17 points or more, a change that represents an absolute decrease of 57% relative to the mean pre-operative raw score of 29.8. Change scores on these three SRT subtests were moderately correlated: CLTR vs. LTS, r = .77; CLTR vs. Delayed Recall, r = .58; LTS vs. Delayed Recall, r = .49.
In contrast to these significant changes in verbal memory in the L-ATL group, neither the L-ATL nor the R-ATL group showed large changes on non-verbal memory tests such as the Visual Reproduction tests from the Wechsler Memory Scale or the 7/24 Spatial Recall Test. Analyses based solely on group means can miss even large declines occurring in a subset of patients. However, analysis of individual patients revealed only a small number (<8%) in either group with notable declines on these non-verbal memory measures, and no differences between the groups in the proportion showing a decline.
Predictors of Verbal Memory Decline
Table 3 shows the relationships, as measured by simple linear correlation, between a variety of potential predictors of memory decline and selected verbal memory change scores observed in the L-ATL patients. The strongest predictor for all the tests was the pre-operative score on that test. That is, patients with higher pre-operative scores tended to have larger declines, consistent with many prior studies (Chelune et al., 1991; Hermann et al., 1995; Jokeit et al., 1997; Davies et al., 1998; Stroup et al., 2003; Gleissner et al., 2004; Baxendale et al., 2006, 2007).
Table 3.
Correlation Values for Univariate Predictors of Memory Outcome in L-ATL Patients.
| Predictor Variable | CLTR | LTS | Delayed Recall | WMS LM1 | WMS LM2 |
|---|---|---|---|---|---|
| Pre-op Score | −.662**** | −.551**** | −.654**** | −.658**** | −.501**** |
| FMRI Lateral LI | −.432*** | −.438*** | −.316* | −.112 | −.211 |
| FMRI Frontal LI | −.396** | −.416*** | −.281* | −.053 | −.168 |
| FMRI Temporal LI | −.300* | −.233 | −.256* | −.305* | −.249 |
| Wada Memory Asymm. | −.331* | −.301* | −.135 | −.078 | −.104 |
| Wada Memory Left | −.231 | −.159 | −.168 | −.077 | −.111 |
| Wada Memory Right | .271* | .320* | .004 | .033 | .032 |
| Wada Language Asymm. | −.398** | −.411** | −.363** | −.214 | −.393** |
| Age at Epilepsy Onset | −.341** | −.324* | −.390** | −.282* | −.219 |
| Duration of Epilepsy | .194 | .125 | .215 | .157 | .192 |
| Age at Surgery | −.098 | −.171 | −.107 | −.059 | .054 |
p <0.0001
p <0.001
p <0.01
p <0.05
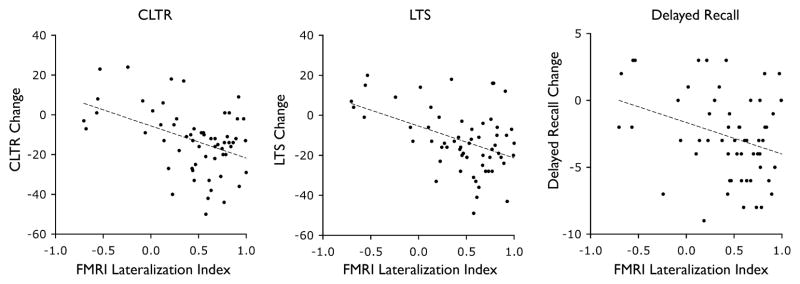
FMRI LIs were also significantly correlated with memory change scores on the SRT tests. The correlations were negative in each case, indicating that stronger lateralization of language-related activation on fMRI toward the left hemisphere was associated with greater decline in verbal memory performance following left ATL surgery. The lateral hemisphere and frontal fMRI LIs were the strongest predictors of the SRT outcomes. These LIs were robust predictors of the CLTR and LTS measures and were more modestly correlated with change on the Delayed Recall test. The temporal lobe fMRI LI showed correlations in the expected direction, but only the correlations with CLTR and Delayed Recall change were statistically reliable. Figure 1 shows scatter plots of the relationships between fMRI LI and these SRT change scores. FMRI LIs were less predictive of change on the WMS-R/III Logical Memory tests. In contrast to the SRT outcomes, the temporal lobe fMRI was the best predictor of change on the WMS LM1 and LM2.
Figure 1.
Relationships between fMRI lateralization indexes and individual memory change scores (CLTR, LTS, Delayed Recall) in the L-ATL patients.
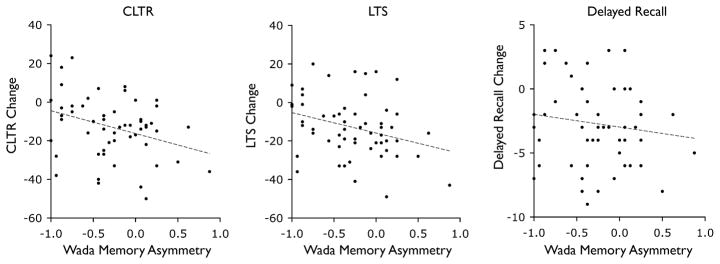
Wada memory testing was less predictive of memory outcome. WMA was only modestly predictive of CLTR and LTS change and was not correlated with Delayed Recall outcome or with either of the WMS-R/III verbal memory change scores. Figure 2 shows scatter plots of the relationships between WMA and the SRT change scores. Given previous evidence that memory outcome may be predicted by memory capacity in the left hemisphere or “functional reserve” capacity in the right hemisphere (Chelune, 1995; Kneebone et al., 1995; Jokeit et al., 1997; Davies et al., 1998; Bell et al., 2000a; Sabsevitz et al., 2001; Stroup et al., 2003), we also examined memory scores obtained by the left hemisphere during right-sided anesthetization (Wada Memory Left) and memory scores obtained by the right hemisphere during left-sided anesthetization (Wada Memory Right). The Wada Memory Right score (functional reserve) was modestly predictive of outcome on the LTS and CLTR measures, with better performance by the right hemisphere predicting better memory outcome. Wada Left memory scores were not predictive of outcome for any of the tests. In contrast, the Wada language asymmetry (WLA) was correlated with all outcome measures (with the exception of the WMS LM1) to approximately the same degree as the fMRI LIs. As with the fMRI measures, stronger lateralization of function toward the left hemisphere on the Wada language test was associated with proportionately greater decline in verbal memory.
Figure 2.
Relationships between Wada memory asymmetries and individual memory change scores (CLTR, LTS, Delayed Recall) in the L-ATL patients.
Age at onset of epilepsy (recurrent seizures) was correlated with change on all of the memory tests except WMS LM2. The negative sign of the correlations indicates that memory decline tends to be greater (change score more negative) with older age at onset, consistent with several prior reports (Saykin et al., 1989; Hermann et al., 1995; Jokeit et al., 1997; Gleissner et al., 2004). Neither age at the time of surgery nor duration of epilepsy was significantly correlated with memory outcome.
Multivariate Outcome Prediction
In applying these results to real clinical situations, the main questions to resolve are: which tests make a significant contribution to predicting outcome, and how should results from these tests be optimally combined? We addressed these questions in a series of stepwise multiple regression analyses combining the variables that predicted outcome in the univariate analyses. These analyses focused on three measures on which the L-ATL group showed the largest and most consistent verbal memory decline: the CLTR, LTS, and Delayed Recall measures from the SRT. Results of these analyses are shown in Table 4.
Table 4.
Multivariable Prediction Models of Memory Outcome After L-ATL.
| CLTR | R2 | p |
|---|---|---|
| Pre-op Score and Age at Epilepsy Onset | .489 | <0.001 |
| add FMRI Lateral Hemisphere LI | .591 | 0.001 |
| add Wada Memory and Wada Language | .616 | n.s. |
| LTS | R2 | p |
| Pre-op Score and Age at Epilepsy Onset | .366 | <0.001 |
| add FMRI Lateral Hemisphere LI | .481 | 0.001 |
| add Wada Memory and Wada Language | .510 | n.s. |
| Delayed Recall | R2 | p |
| Pre-op Score and Age at Epilepsy Onset | .535 | <0.001 |
| add FMRI Lateral Hemisphere LI | .610 | 0.003 |
| add Wada Memory and Wada Language | .627 | n.s. |
The first variables entered in all analyses were pre-operative test performance and age at onset of epilepsy. The rationale for including these variables first is that they can be obtained with relatively little expense and at no risk to the patient. Next, the fMRI lateral hemisphere LI was added, followed by simultaneous addition of both the WMA and WLA. Our rationale for adding fMRI in the second step is that fMRI is non-invasive and carries less risk than the Wada test. The WMA and WLA were added together in the final step because these measures are typically obtained together.
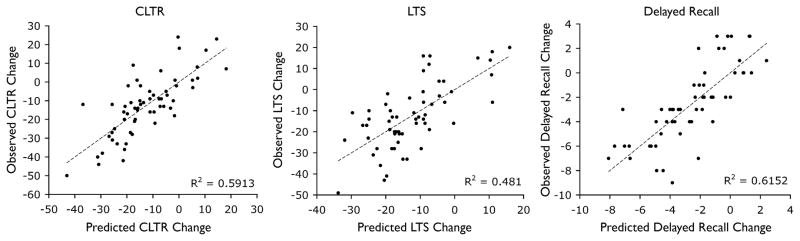
Preoperative score and age at onset of epilepsy together accounted for 49%, 37%, and 54% of the variance in outcome on the CLTR, LTS, and Delayed Recall measures, respectively. The fMRI LI added significantly to the predictive power of the model for all of the change scores, accounting for an additional 10% of the variance in CLTR change, 11% of the variance in LTS change, and 7% of the variance in Delayed Recall change. Together, pre-operative memory performance, age at onset of epilepsy, and fMRI LI accounted for roughly 59% of the variance in CLTR change, 48% of the variance in LTS change, and 61% of the variance in Delayed Recall change. When the Wada test language and memory data were entered in the equation after the fMRI LI already had been entered, there was no further significant increase in predictive power.
Change in CLTR was optimally predicted by the following formula:
| [1] |
Change in LTS was optimally predicted by the following formula:
| [2] |
Finally, change in Delayed Recall was best predicted by the following formula:
| [3] |
Figure 3 shows scatter plots of the predicted vs. observed change scores for each of the memory tests. Notably, none of the 60 patients had an unexpectedly large decline on any of the tests, i.e., there were no cases with a predicted change score greater than zero who nevertheless showed a large decline. Sensitivity and specificity of these prediction models can be ascertained by categorizing the cases nominally as showing Decline or No Decline. When Decline is defined as a negative change score 1.5 standard deviations or more from the mean change score in the RATL group, equation [1] showed sensitivity of 90%, specificity of 80%, and a positive predictive value of 69% for predicting Decline on the CLTR measure. Equation [2] showed sensitivity of 70%, specificity of 73%, and a positive predictive value of 68% for predicting Decline on the LTS measure. Finally, equation [3] showed sensitivity of 81%, specificity of 100%, and a positive predictive value of 100% for predicting Decline on the Delayed Recall measure.
Figure 3.
Predicted vs. observed individual memory change scores (CLTR, LTS, Delayed Recall) in the L-ATL patients.
Though not a focus of the present study, we also examined whether Wada testing contributes additional predictive power in the absence of fMRI data. This information may be of interest to clinicians who regularly perform the Wada test and do not have ready access to fMRI. When entered in the multivariate regression after preoperative score and age at onset, the combined Wada language and memory data did provide additional predictive value (CLTR R2 change = .096, p = .007; LTS R2 change = .111, p = .010; Delayed Recall R2 change = .071, p = .020). FMRI provided additional predictive value for the CLTR change scores even after inclusion of the Wada language and memory data (R2 change = .036, p = .042), and showed strong trends for adding predictive value with the other tests (LTS R2 change = .040, p = .056; Delayed Recall R2 change = .027, p = .074).
Because the WMS has been used frequently in prior studies of verbal memory outcome after ATL surgery, we also examined multivariate prediction models for the WMS-R/III LM1 and LM2 change scores. Preoperative scores and age at onset of epilepsy together accounted for 46% of LM1 change score variance and 26% of LM2 change score variance (both p < 0.001). Neither fMRI (lateral LI or temporal lobe LI) nor Wada data (combined language and memory) added significant predictive power to the models for these change scores.
Illustrative Cases
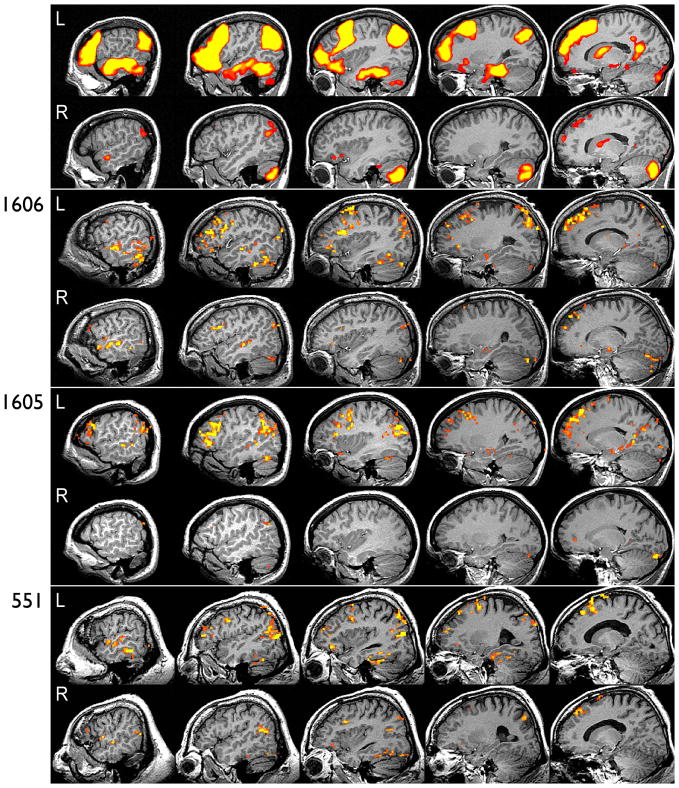
Selected patients are presented to demonstrate the fMRI activation patterns and to illustrate several typical outcomes and clinically important exceptions. Patient 1606 experienced one of the most severe verbal memory declines. This patient had high pre-operative test scores, late age of epilepsy onset, and a left-lateralized fMRI activation pattern (Figure 4). Predicted change scores, shown in parentheses in Table 5, closely matched the observed changes. WMA was also consistent with a poor outcome, with memory lateralized slightly toward the left hemisphere. Similar concordance between tests is illustrated by case 1605, who had strong left lateralization on both fMRI (Figure 4) and WMA. Patient 1605 illustrates that patients with strong left dominance for language and verbal memory can show severe decline even when the age at onset of seizures is early.
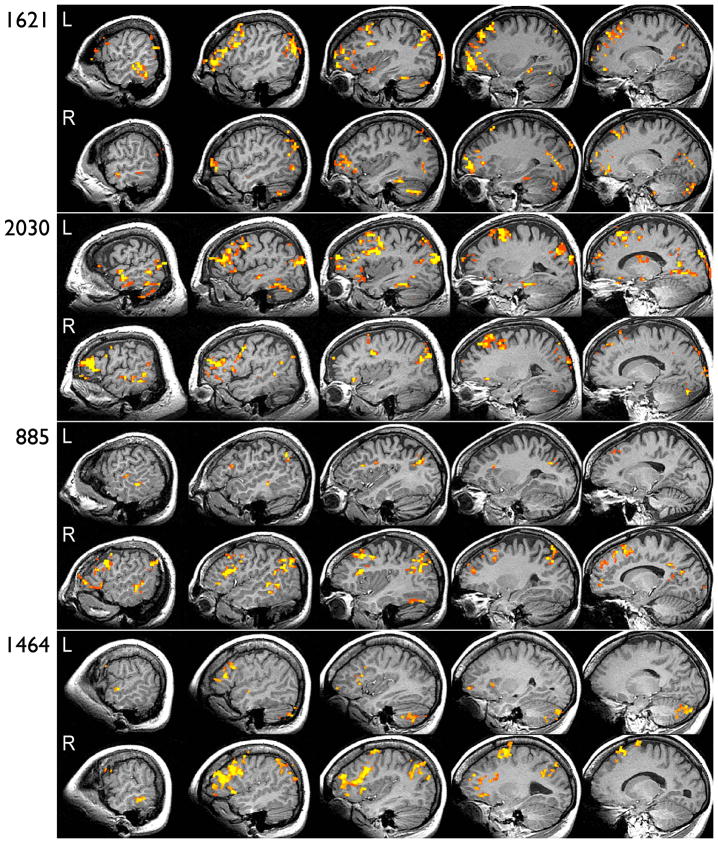
Figure 4.
Example fMRI activation maps are shown in serial sagittal sections through the left (L) and right (R) hemispheres at 10-mm intervals through standard stereotaxic space. All maps are thresholded at map-wise corrected p < 0.05 using a voxel-wise p < 0.001 and minimal cluster size of 300 μl. The top panel shows the average activation pattern for this task contrast obtained from 30 healthy adults (see (Binder et al., 1997) for details). The remaining panels show selected individuals described in Table 5, indicated by case number.
Table 5.
Illustrative L-ATL Cases (see Text)
| Pre-op SRT Scores |
Change Scores |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Sex | Age | AOE | WMA | FMRI | CLTR | LTS | DR | δCLTR | δLTS | δDR |
| 1606 | M | 40 | 36 | .13 | .58 | 62 | 62 | 10 | −50 (−43) | −49 (−34) | −6 (−8) |
| 1605 | F | 29 | 2 | .88 | .93 | 38 | 50 | 9 | −36 (−21) | −43 (−20) | −5 (−5) |
| 551 | M | 43 | 20 | −.94 | .63 | 48 | 49 | 8 | −38 (−29) | −36 (−22) | −6 (−5) |
| 1621 | F | 41 | 28 | −.38 | .47 | 41 | 44 | 10 | −25 (−24) | −19 (−18) | −6 (−7) |
| 1141 | F | 37 | 21 | −.25 | .61 | 35 | 46 | 4 | −33 (−20) | −41 (−20) | −3 (−2) |
| 1215 | F | 40 | 15 | −.94 | .44 | 37 | 50 | 6 | −28 (−18) | −28 (−18) | −4 (−3) |
| 2030 | M | 68 | 34 | −.44 | .23 | 52 | 56 | 6 | −40 (−31) | −23 (−25) | −3 (−4) |
| 765 | M | 30 | 11 | −.38 | .19 | 44 | 50 | 9 | −27 (−14) | −33 (−19) | −9 (−4) |
| 1539 | M | 43 | 17 | −1.00 | −.24 | 23 | 48 | 7 | 24 (0) | 9 (−9) | −7 (−2) |
| 885 | F | 28 | 12 | −.88 | −.70 | 25 | 28 | 6 | −3 (5) | 7 (11) | −2 (0) |
| 1464 | F | 25 | 12 | −.88 | −.68 | 46 | 52 | 9 | −7 (−10) | 4 (−5) | 2 (−2) |
Abbreviations: AOE = age at onset of epilepsy, WMA = Wada memory asymmetry, FMRI = fMRI lateralization index, DR = delayed recall subtest of the SRT. Numbers in parentheses in the change score columns indicate predicted change scores. All change scores represent the difference between postoperative and preoperative raw scores.
The limited predictive value of WMA is illustrated most clearly by a subgroup of patients with clear lateralization of memory to the right hemisphere, who nonetheless experienced severe verbal memory decline after L-ATL (see Figure 2). Patient 551, for example, showed one of the most severe declines despite a WMA indicating almost all memory function in the right hemisphere. Left-lateralized fMRI (Figure 4), late onset of epilepsy, and high pre-operative test scores, however, all predicted severe decline. Patients 1621 (Figure 5), 1141, and 1215 are examples of similar false negative predictions by WMA, all of whom also had left-lateralization of fMRI activation and relatively late onset of epilepsy.
Figure 5.
FMRI activation maps for four additional patients described in Table 5.
Patient 2030 represents another example of a false negative prediction by WMA. In this patient, the fMRI pattern was more symmetric (Figure 5), which taken in isolation is predictive of little or no decline (see Figure 1). However, when combined with the patient's late age of seizure onset and high pre-operative scores, the symmetric fMRI activation pattern is consistent with the patient's actual outcome. In contrast to the WMA, there were no cases in which the fMRI LI was strongly right-lateralized and the patient experienced a severe decline on the CLTR or LTS (see Figure 1). Two patients (765 and 1539) had relatively symmetric fMRI patterns and showed severe decline on the Delayed Recall measure. These declines would also have been unexpected on the basis of the WMA, which was right-lateralized in both patients. Decline on Delayed Recall was predicted from the multivariate model in both cases because of high preoperative performance and relatively late onset of epilepsy.
Patients who did not decline typically had low pre-operative test scores, earlier age at onset, or right-lateralized activation patterns on fMRI. Patients 885 and 1464 both had relatively late onset and good pre-op scores, but fMRI activation was lateralized strongly to the right hemisphere (Figure 5). These patients, both left-handed, likely represent cases of congenital right-hemisphere language dominance. In both cases WMA was also strongly lateralized to the right hemisphere. Three other patients showed similar right-lateralization on fMRI and WMA, preserved pre-operative function, and no evidence of decline.
Discussion
Anterior temporal lobe resection is a very effective treatment for medically intractable temporal lobe epilepsy, yet this benefit must be weighed against the risk of cognitive decline, particularly in patients undergoing left ATL. Consistent with many prior studies (Chelune et al., 1993; Martin et al., 1998; Sabsevitz et al., 2001; Stroup et al., 2003; Gleissner et al., 2004; Baxendale et al., 2006; Lineweaver et al., 2006), we found a high incidence of verbal memory decline after left ATL. Depending on the specific measure used, 33–55% of L-ATL patients declined on a verbal learning test (SRT) relative to a right ATL control group. How clinically significant are such deficits? No patient in our series experienced the severe 'global amnesia' described in rare patients with bilateral MTL lesions (Scoville & Milner, 1957; Guerreiro et al., 2001; Di Gennaro et al., 2006), who are unable to form any new episodic memories. Moreover, it is unclear whether amnesia of this severity ever occurs after unilateral temporal lobe resection (Novelly & Williamson, 1989; Loring et al., 1990; Baxendale, 1998; Kubu et al., 2000; Simkins-Bullock, 2000; Kapur & Prevett, 2003). Instead, patients undergoing left ATL often show a relative decline from their baseline on standardized psychometric tests. In some cases these declines are proportionally quite large, as in the 33% of patients in our series who declined more than 17 points on the CLTR measure of the SRT. Relative to the average preoperative score of 30 on this test, a 17-point decline represents more than a 50% decrement in performance. Prior studies suggest that patients are aware of such memory deficits, and that these deficits adversely affect quality of life and employability (Perrine et al., 1995; Helmstaedter et al., 2003; Stroup et al., 2003; Lineweaver et al., 2004; Langfitt et al., 2007). A few patients in our series had declines of 40 or more points on the CLTR and LTS measures from the SRT (Figure 1). Such deficits may be comparable in severity to those of rare patients described in the literature as having 'amnesia' after unilateral temporal lobectomy (Loring et al., 1994a; Kapur & Prevett, 2003).
Also consistent with prior studies was the finding of relatively preserved verbal and nonverbal memory function after right ATL, and preserved nonverbal memory after left ATL (Lee et al., 2002; Stroup et al., 2003; Lineweaver et al., 2006). The nonverbal memory tests used here assessed single-trial memory for abstract visual figures and learning of spatial patterns. It is possible that other tests might be more sensitive for detecting post-operative deficits in right ATL patients, such as tests focusing on face or route learning (Bohbot et al., 1998; Chiaravalloti & Glosser, 2001). Nonetheless, the conclusion we draw from these data is that relative loss of verbal episodic memory ability after left ATL is by far the most prevalent and significant memory deficit associated with ATL surgery, and should, therefore, be the main focus of attempts to reduce memory decline after ATL.
Our aim in the present study was to determine whether preoperative fMRI predicts verbal memory decline. An equally important question is whether fMRI adds any predictive value over and above that available from other tests, particularly non-invasive measures like pre-operative test performance and medical history data. A third important issue is whether the Wada test contributes predictive value, and whether this relatively invasive test provides additional information over and above the non-invasive tests.
The most powerful predictor of verbal memory decline in our left ATL sample was pre-operative memory performance, which accounted for roughly 30–40% of the variance in outcome, depending on the specific outcome measure. Consistent with many prior studies (Chelune et al., 1991; Hermann et al., 1995; Helmstaedter & Elger, 1996; Jokeit et al., 1997; Davies et al., 1998; Stroup et al., 2003; Gleissner et al., 2004; Baxendale et al., 2006; Lineweaver et al., 2006; Baxendale et al., 2007), patients with higher pre-operative test scores tended to show larger declines. One possible explanation for this phenomenon is that the better pre-operative performers have more function to lose, i.e., that the poor performers show less decline due to a psychometric “floor effect”. While this may be part of the story, the data also suggest an inherent biological dependence of verbal memory on the left hemisphere. If it was possible for verbal memory to shift fully to the right temporal lobe in patients with long-standing left temporal epilepsy, such patients would show good pre-operative verbal memory and would be unaffected by left ATL. Evidence indicates, however, that more severe left MTL pathology is associated with worse pre-operative verbal memory (Sass et al., 1990; Rausch & Babb, 1993; Saling et al., 1993; Helmstaedter & Elger, 1996; Hermann et al., 1997), indicating that rightward shift of verbal memory in patients with left temporal lobe epilepsy, though protective, is associated with a lower level of baseline function. Pre-operative performance can thus be considered an indirect indicator of pathological status of the left MTL. Patients with better pre-operative performance typically have milder left MTL pathology, have maintained more of their verbal memory function in the left temporal lobe, and are at higher risk from left ATL (Hermann et al., 1992; Trenerry et al., 1993; Sass et al., 1994; Seidenberg et al., 1998; Chelune & Najm, 2000).
Language lateralization measured by fMRI was the second most powerful predictor of verbal memory decline, accounting for an additional 10% of the variance in outcome on the SRT tests. Moreover, fMRI added significant predictive power beyond that provided by pre-operative test scores and demographic variables like age at epilepsy onset. These other non-invasive measures and fMRI together accounted for 48–61% of the variance in specific outcome measures. This combination of tests also showed good accuracy for predicting categorical decline in individual patients, with sensitivity ranging from 70–90% and specificity ranging from 73–100%. Although these models predicted outcomes fairly well, there remain at least two potential sources for residual unexplained variance. First, although the ATL surgeries were relatively standardized, there was likely some variation in the posterior extent of resection, which may have affected outcomes. Whether extent of resection modifies memory outcome is controversial (Milner, 1970; Ojemann & Dodrill, 1985; Katz et al., 1989; Wolf et al., 1993; Wyler et al., 1995; Graydon et al., 2001) and should be explored in future studies using quantitative pre- and post-operative structural MRI in a multivariate model. A second source of variance is imperfect test-retest reliability. One normative study of the SRT, for example, showed a test-retest correlation of only 0.66 for the CLTR measure (Ruff et al., 1989). Though this result is not directly applicable to our study because the range of normal variation is likely to be small relative to the variation in change scores we studied, it nevertheless serves as a reminder that all psychometric tests are inherently imperfect measurements susceptible to uncontrolled, non-stationary factors.
The fMRI laterality indexes were less effective predictors of change scores on the WMS-R/III Logical Memory tests. In our sample of patients, these tests were less sensitive in detecting verbal memory decline compared to the SRT. For example, the proportion of patients showing decline on the WMS tests (18–27%) was substantially lower than on the SRT tests. The mean percent decline in raw scores on the WMS tests (i.e., change score/pre-op score) was roughly 20–30%, compared to 30–45% declines on the SRT measures. This difference could be due to an inherently greater effect of left ATL resections on learning processes (SRT) compared to single-trial encoding processes (WMS), as suggested by several authors (Rausch & Babb, 1993; Saling et al., 1993). In addition, the multiple trials used in the SRT procedure might simply provide a larger sample size and thus more statistically reliable observations (Lee et al., 2002). If the WMS changes are smaller or less reliable, they would be more difficult to predict, which could explain the lower correlations between these outcomes and the fMRI LIs. It is interesting, however, that among the fMRI indexes, the WMS change scores were best predicted by the temporal lobe LI. This pattern suggests that the WMS tests might be more selectively sensitive to processes carried out by the temporal lobe.
In contrast to the non-invasive measures, Wada memory asymmetry was only weakly correlated with verbal memory outcome. The Wada memory test was originally developed for the purpose of predicting global amnesia after ATL (Milner et al., 1962). Studies of its ability to predict relative verbal memory decline have been inconsistent, with several suggesting good predictive value (Kneebone et al., 1995; Loring et al., 1995b; Bell et al., 2000a; Chiaravalloti & Glosser, 2001; Sabsevitz et al., 2001) and others showing little or none, particularly when used in combination with non-invasive tests (Chelune & Najm, 2000; Stroup et al., 2003; Lacruz et al., 2004; Kirsch et al., 2005; Lineweaver et al., 2006). Some authors have questioned the general validity and reliability of Wada memory results (Novelly & Williamson, 1989; Loring et al., 1990; Lee et al., 1995; Kubu et al., 2000; Simkins-Bullock, 2000; Martin & Grote, 2002; Loddenkemper et al., 2007). Others have emphasized the sensitivity of the test to stimulus type, relative timing of stimulus presentation, procedures used for recall, and other methodological factors (Loring et al., 1994b; Loring et al., 1995a; Carpenter et al., 1996; Alpherts et al., 2000). A particular concern highlighted in our series is the relatively frequent occurrence of “false negative” Wada results, i.e., patients with memory lateralization to the right hemisphere who nevertheless show significant decline after left ATL (Figure 2, Table 5). Several prior reports have also raised concerns regarding such cases (Rausch et al., 1993; Kirsch et al., 2005).
We do not believe the weak predictive power of our Wada memory test can be attributed to procedural flaws. Our test used an object encoding procedure that has been shown to predict verbal memory decline after left ATL in several small series (Loring et al., 1995b; Sabsevitz et al., 2001). Patients were excluded from the analysis if they showed obtundation or bilateral poor memory performance. As direct evidence for the validity of the test, the left and right ATL groups showed markedly different memory asymmetry scores, suggesting that the test was sensitive to asymmetric MTL pathology. Thus, the Wada memory asymmetry score was only weakly related to memory decline despite its ability to detect MTL functional asymmetry.
Why is the Wada memory test not a stronger predictor of verbal memory decline? One possibility is that the Wada memory test as usually performed (and as performed here) employs a recognition procedure, whereas the tests used in neuropsychological assessment typically use free recall procedures. The SRT, however, also includes a Recognition subtest very similar to the procedure used for Wada memory evaluation. Significant predictors of change on this subtest included the preoperative score (r = −.308) and all of the fMRI LIs (e.g., r = −.408 for the Lateral ROI). In contrast, change on the Recognition subtest was not correlated with Wada memory asymmetry (r = −.110), thus offering no evidence that differences in memory test procedure account for the lack of correlation.
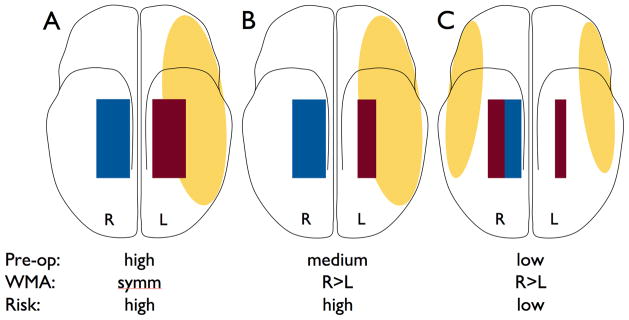
We believe a more viable explanation is that the Wada memory test is not sufficiently material-specific. The objects used in the test can be encoded either verbally, as object names, or non-verbally, as visual percepts. Patients with relatively weak verbal memory might show better memory performance using a non-verbal encoding strategy. If this non-verbal system is lateralized differently from the verbal memory system, the asymmetry of performance on the Wada test might mainly reflect lateralization of the non-verbal system rather than the verbal system (Figure 6). The verbal memory outcome tests, in contrast, are designed to assess strictly verbal memory functions. These verbal memory outcomes will not be accurately predicted in patients whose Wada memory asymmetry reflects mainly non-verbal memory lateralization. Thus the Wada object memory test is a good indicator of overall memory lateralization, and therefore a good indicator of seizure focus lateralization, but may not accurately reflect lateralization of verbal memory processes.
Figure 6.
Schematic diagram of a hypothetical model of memory and language representation in temporal lobe epilepsy (TLE). The yellow ovals represent language systems, red rectangles represent verbal episodic memory encoding systems in the medial temporal lobe (MTL), and blue rectangles represent non-verbal episodic memory encoding systems in the MTL. (A) Typical state in healthy subjects and patients with late-onset epilepsy. Language and verbal memory processes are strongly left-lateralized, placing the patient at high risk for verbal memory decline. (B) Chronic left TLE without shift. The left MTL is dysfunctional, causing Wada memory lateralization to the right, but verbal memory has not shifted, leaving the patient at high risk for verbal memory decline. (C) Chronic left TLE with shift. Both language and verbal memory functions have shifted partially to the right, lowering the risk for verbal memory decline. Note the relative lack of correspondence, across patient types, between Wada memory asymmetry and level of risk.
Why is language lateralization a stronger predictor of verbal memory decline, both when measured with fMRI and with the Wada test? Compared to Wada memory asymmetry, language asymmetry is more closely correlated with lateralization of verbal memory processes (Figure 6). When language is lateralized to the left side, as in the typical normal state, verbal memory processes are more likely to have remained left-lateralized, and the patient carries a higher risk for verbal memory decline (Figure 6A,B). Conversely, when language is represented bilaterally or predominantly on the right side, verbal memory is more likely to have shifted to the right, placing the patient at lower risk (Figure 6C). This model suggests that verbal or non-verbal material specificity of the MTL may be largely a function of the type of information the MTL receives from the ipsilateral neocortex. Only when the right MTL receives verbal information from the right hemisphere does it contribute to supporting verbal memory. As discussed above, however, it also appears that the right MTL may have intrinsic limitations in the verbal domain, in that patients who do not show verbal memory decline, and have presumably shifted some of their language and verbal memory functions to the right hemisphere, also tend to have lower pre-operative verbal memory scores. These lower pre-operative scores could also be partly explained in some cases by longer seizure duration and a tendency for lower general intellectual function in these patients.
Use of language lateralization to predict memory outcome is counterintuitive and has not, to our knowledge, been examined previously. No prior study to our knowledge has examined whether Wada language asymmetry predicts verbal memory outcome. Indeed, prior studies examining memory outcome have generally treated variation in language representation as a confound that interferes with assessment of other predictors, and most have excluded patients with atypical language dominance. In the only study relevant to this issue, researchers compared a “Montreal” Wada memory procedure similar to the one we used to a “Seattle” Wada procedure (Dodrill & Ojemann, 1997). In the Seattle procedure, short-term recall of objects is tested during anesthesia rather than after anesthesia when language and other functions have returned to normal. Compared to the Montreal procedure, the Seattle procedure was more likely to be abnormal when language was present on the side being tested, suggesting that it partly reflected language processes, particularly those involved in verbal short-term memory. Of note, the Seattle procedure predicted memory outcome (76% accuracy), whereas the Montreal procedure did not (48% accuracy).
One previous study assessed prediction of verbal memory outcome with preoperative fMRI. Richardson et al. (Richardson et al., 2006) used an fMRI word-encoding task to predict verbal memory outcome in 12 left ATL patients. Hippocampal activation on both sides predicted verbal memory decline on a delayed list-recall test (similar to the SRT Delayed Recall measure used in the present study), with left hippocampal activation slightly more predictive (r = .72) than right hippocampal activation (r = .71). Patients with higher activation levels experienced greater decline after left ATL surgery. The positive correlation between memory decline and right hippocampal activation was in a direction opposite to that predicted by the 'functional reserve' hypothesis, which predicts less decline with greater memory representation in the right MTL. The authors proposed that the right hippocampal activation observed by fMRI might represent a different, “dysfunctional” type of memory processing that “does not provide an adequate postoperative reserve to maintain memory function at the preoperative level” (Richardson et al., 2006). It is probably best to regard these results as preliminary, however, given the limited sample size used. This sample size also precluded the possibility of a multivariate analysis to determine the unique contribution of fMRI relative to other predictors. Compared to this earlier study, the current investigation included a larger number of patients and tested, for the first time, the clinical utility of fMRI in the context of several other variables known to predict memory outcome. Another important difference between the two studies is our use of a large region of interest that measures lateralization in a distributed language network, in contrast to the focused hippocampal ROI used by Richardson et al., which presumably isolates processes more specifically related to memory encoding. It could be argued, furthermore, that the fMRI activation tasks used in the two studies are fundamentally different, in that we used a language task whereas Richardson et al. used a memory task. We believe the difference in tasks is nominal more than actual, as semantic decision tasks are well known to result in incidental long-term encoding of the stimulus materials, often referred to as 'deep encoding' (Craik & Lockhart, 1972). Such tasks have been used by many researchers to activate the medial temporal lobe (Henke et al., 1999; Martin, 1999; Heckers et al., 2002; Daselaar et al., 2003), and the fMRI contrast used in the current study, though nominally a language task, produces strong activation in the left hippocampus and surrounding MTL at the group level (Binder et al., 1997; Bellgowan et al., 1998). We chose a large ROI to measure lateralization with this task in the expectation that this approach would provide the most reliable measurements in individual patients. In principle, however, specific identification of verbal memory encoding networks in the MTL could not only enable more accurate prediction of verbal memory outcome but might also provide a means of tailoring resections to reduce memory deficits. Development of robust methods for identifying these networks with fMRI should thus remain a goal of future research.
In conclusion, the present data suggest that verbal memory decline from left ATL surgery can be predicted with good accuracy using historical, neuropsychological, and fMRI language lateralization data. Wada language asymmetry is shown for the first time to be a better predictor of verbal memory outcome than Wada memory asymmetry, though this relatively invasive test does not provide additional predictive capability beyond fMRI and other non-invasive predictors. One question not addressed by the current study is how much more predictive power can be gained from volumetric analysis of the medial temporal lobe. Quantitative MRI can provide a sensitive index of hippocampal asymmetry that may account for some of the variance in memory outcome after left ATL (Trenerry et al., 1993; Chelune & Najm, 2000; Lineweaver et al., 2006). We plan to examine this variable in future studies. If the model presented in Figure 6 is correct, however, it is likely that hippocampal volume asymmetry will be highly correlated with Wada memory asymmetry and may not capture variance in outcome due to language representation. FMRI, on the other hand, appears to be a useful tool for providing this additional information.
Fast T2*-weighted imaging capabilities necessary for fMRI are a standard feature on currently marketed clinical MRI systems, and fMRI is now available in some form at most medical centers. Because it is non-invasive, clinical fMRI is likely to be considerably less costly than Wada testing. Implementation of cognitive fMRI protocols such as the one described here requires only installation of relatively low-cost audiovisual stimulation and response monitoring systems, together with expertise in cognitive training and testing provided by a neuropsychologist or cognitive neurologist. Auditory stimuli and presentation scripts used in the current study are available from the authors free of charge.
Acknowledgments
Our thanks to Linda Allen, Patrick Bellgowan, Kyle Capizzi, Julie Frost, Dongwook Lee, George Morris, Romila Mushtaq, Conrad Nievera, Edward Possing, Jane Springer, and Scott Winstanley for assistance with patient recruitment and collecting and coding the data. Supported by National Institute of Neurological Diseases and Stroke grant R01 NS35929, National Institutes of Health General Clinical Research Center grant M01 RR00058, National Research Service Award Fellowship F32 MH11921, and the Charles A. Dana Foundation. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines. None of the authors has any conflicts of interest to disclose.
References
- Alpherts WC, Vermeulen J, van Veelen CW. The Wada test: prediction of focus lateralization by asymmetric and symmetric recall. Epilepsy Res. 2000;39:239–249. doi: 10.1016/s0920-1211(00)00097-8. [DOI] [PubMed] [Google Scholar]
- Alpherts WC, Vermeulen J, van Rijen PC, Lopes da Silva FH, van Veelen CWM. Verbal memory decline after temporal epilepsy surgery? A 6-year multiple assessments follow-up study. Neurology. 2006;67:626–631. doi: 10.1212/01.wnl.0000230139.45304.eb. [DOI] [PubMed] [Google Scholar]
- Barton JS, Hefter R, Chang B, Schomer D, Drislane F. The field defects of anterior temporal lobectomy: a quantitative reassessment of Meyer's loop. Brain. 2005;128:2123–2133. doi: 10.1093/brain/awh544. [DOI] [PubMed] [Google Scholar]
- Baxendale S. Amnesia in temporal lobectomy patients: historical perspective and review. Seizure. 1998;7:15–24. doi: 10.1016/s1059-1311(98)90003-6. [DOI] [PubMed] [Google Scholar]
- Baxendale S, Thompson P, Harkness W, Duncan J. Predicting memory decline following epilepsy surgery: A multivariate approach. Epilepsia. 2006;47:1887–1894. doi: 10.1111/j.1528-1167.2006.00810.x. [DOI] [PubMed] [Google Scholar]
- Baxendale S, Thompson P, Harkness W, Duncan J. The role of the intracarotid amobarbital procedure in predicting verbal memory decline after temporal lobe resection. Epilepsia. 2007;48:546–552. doi: 10.1111/j.1528-1167.2006.00940.x. [DOI] [PubMed] [Google Scholar]
- Bell BD, Davies KG, Haltiner AM, Walters GL. Intracarotid amobarbital procedure and prediction of postoperative memory in patients with left temporal lobe epilepsy and hippocampal sclerosis. Epilepsia. 2000a;41:992–997. doi: 10.1111/j.1528-1157.2000.tb00284.x. [DOI] [PubMed] [Google Scholar]
- Bell BD, Davies KG, Hermann BP, Walters G. Confrontation naming after anterior temporal lobectomy is related to age of acquisition of the object names. Neuropsychologia. 2000b;38:83–92. doi: 10.1016/s0028-3932(99)00047-0. [DOI] [PubMed] [Google Scholar]
- Bellgowan PSF, Binder JR, Swanson SJ, Hammeke TA, Springer JA, Frost JA, Mueller WM, Morris GL. Side of seizure focus predicts left medial temporal lobe activation during verbal encoding. Neurology. 1998;51:479–484. doi: 10.1212/wnl.51.2.479. [DOI] [PubMed] [Google Scholar]
- Binder JR, Swanson SJ, Hammeke TA, Morris GL, Mueller WM, Fischer M, Benbadis S, Frost JA, Rao SM, Haughton VM. Determination of language dominance using functional MRI: A comparison with the Wada test. Neurology. 1996;46:978–984. doi: 10.1212/wnl.46.4.978. [DOI] [PubMed] [Google Scholar]
- Binder JR, Frost JA, Hammeke TA, Cox RW, Rao SM, Prieto T. Human brain language areas identified by functional MRI. J Neurosci. 1997;17:353–362. doi: 10.1523/JNEUROSCI.17-01-00353.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohbot VD, Kalina M, Stepankova K, Spackova N, Petrides M, Nadel L. Spatial memory deficits in patients with lesions to the right hippocampus and to the right parahippocampus. Neuropsychologia. 1998;36:1217–1238. doi: 10.1016/s0028-3932(97)00161-9. [DOI] [PubMed] [Google Scholar]
- Buschke H, Fuld PA. Evaluating storage, retention, and retrieval in disordered memory and learning. Neurology. 1974;24:1019–1025. doi: 10.1212/wnl.24.11.1019. [DOI] [PubMed] [Google Scholar]
- Carpenter K, Oxbury JM, Oxbury S, Wright GD. Memory for objects presented after intracarotid sodium amytal: a sensitive clinical neuropsychological indicator of temporal lobe pathology. Seizure. 1996;5:103–108. doi: 10.1016/s1059-1311(96)80102-6. [DOI] [PubMed] [Google Scholar]
- Chelune GC. Hippocampal adequacy versus functional reserve: predicting memory functions following temporal lobectomy. Arch Clin Neuropsychol. 1995;10:413–432. [PubMed] [Google Scholar]
- Chelune GJ, Naugle RI, Lüders H, Awad IA. Prediction of cognitive change as a function of preoperative ability level among temporal lobectomy patients at six months follow-up. Neurology. 1991;41:399–404. doi: 10.1212/wnl.41.3.399. [DOI] [PubMed] [Google Scholar]
- Chelune GJ, Naugle RI, Lüders H, Sedlak J, Awad IA. Individual change after epilepsy surgery: Practice effects and base-rate information. Neuropsychology. 1993;7:41–52. [Google Scholar]
- Chelune GJ, Najm IM. Risk factors associated with postsurgical decrements in memory. In: Luders HO, Comair Y, editors. Epilepsy surgery. 2. Lippincott; Philadelphia: 2000. pp. 497–504. [Google Scholar]
- Chiaravalloti ND, Glosser G. Material-specific memory changes after anterior temporal lobectomy as predicted by the intracarotid amobarbital test. Epilepsia. 2001;42:902–911. doi: 10.1046/j.1528-1157.2001.02500.x. [DOI] [PubMed] [Google Scholar]
- Cohen-Gadol AA, Westerveld M, Alvarez-Carilles J, Spencer DD. Intracarotid amytal memory test and hippocampal magnetic resonance imaging volumetry: validity of the Wada test as an indicator of hippocampal integrity among candidates for epilepsy surgery. J Neurosurg. 2004;101:926–931. doi: 10.3171/jns.2004.101.6.0926. [DOI] [PubMed] [Google Scholar]
- Craik FIM, Lockhart RS. Levels of processing: a framework for memory research. J Verb Learn Verb Behav. 1972;11:671–684. [Google Scholar]
- Daselaar SM, Veltman DJ, Rombouts SA, Raaijmakers JG, Jonker C. Deep processing activates the medial temporal lobe in young but not in old adults. Neurobiol Aging. 2003;24:1005–1011. doi: 10.1016/s0197-4580(03)00032-0. [DOI] [PubMed] [Google Scholar]
- Davies KG, Bell BD, Bush AJ, Wyler AR. Prediction of verbal memory loss in individuals after anterior temporal lobectomy. Epilepsia. 1998;39:820–828. doi: 10.1111/j.1528-1157.1998.tb01175.x. [DOI] [PubMed] [Google Scholar]
- Di Gennaro G, Grammaldo LG, Quarato PP, Esposito V, Mascia A, Sparano A, Meldolesi GN, Picardi A. Severe amnesia following bilateral medial temporal lobe damage occurring on two distinct occasions. Neurol Sci. 2006;27:129–133. doi: 10.1007/s10072-006-0614-y. [DOI] [PubMed] [Google Scholar]
- Dodrill CB, Ojemann GA. An exporatory comparison of three methods of memory assessment with the intracarotid amobarbital procedure. Brain Cogn. 1997;33:210–223. doi: 10.1006/brcg.1997.0893. [DOI] [PubMed] [Google Scholar]
- Frost JA, Binder JR, Springer JA, Hammeke TA, Bellgowan PSF, Rao SM, Cox RW. Language processing is strongly left lateralized in both sexes: Evidence from FMRI. Brain. 1999;122:199–208. doi: 10.1093/brain/122.2.199. [DOI] [PubMed] [Google Scholar]
- Gleissner U, Helmstaedter C, Schramm J, Elger CE. Memory outcome after selective amygdalohippocampectomy in patients with temporal lobe epilepsy: One-year follow-up. Epilepsia. 2004;45:960–962. doi: 10.1111/j.0013-9580.2004.42203.x. [DOI] [PubMed] [Google Scholar]
- Graydon FJ, Nunn JA, Polkey CE, Morris RG. Neuropsychological outcome and extent of resection in unilateral temporal lobectomy. Epil Behav. 2001;2:140–151. doi: 10.1006/ebeh.2001.0163. [DOI] [PubMed] [Google Scholar]
- Griffith HR, Perlman SB, Woodard AR, Rutecki PA, Jones JC, Ramirez LF, DeLaPena R, Seidenberg M, Hermann BP. Preoperative FDG-PET temporal lobe hypometabolism and verbal memory after temporal lobectomy. Neurology. 2000;54:1161–1165. doi: 10.1212/wnl.54.5.1161. [DOI] [PubMed] [Google Scholar]
- Guerreiro CAM, Jones-Gotman M, Andermann F, Cendes F. Severe amnesia in epilepsy: Causes, anatomopsychological considerations, and treatment. Epil Behav. 2001;2:224–246. doi: 10.1006/ebeh.2001.0167. [DOI] [PubMed] [Google Scholar]
- Heckers S, Weiss AP, Alpert NM, Schacter DL. Hippocampal and brain stem activation during word retrieval after repeated and semantic encoding. Cereb Cortex. 2002;12:900–907. doi: 10.1093/cercor/12.9.900. [DOI] [PubMed] [Google Scholar]
- Helmstaedter C, Elger CE. Cognitive consequences of two-thirds anterior temporal lobectomy on verbal memory in 144 patients: a three-month follow-up study. Epilepsia. 1996;37:171–180. doi: 10.1111/j.1528-1157.1996.tb00009.x. [DOI] [PubMed] [Google Scholar]
- Helmstaedter C, Kurthen M, Lux S, Reuber M, Elger CE. Chronic epilepsy and cognition: a longitudinal study in temporal lobe epilepsy. Ann Neurol. 2003;54:425–432. doi: 10.1002/ana.10692. [DOI] [PubMed] [Google Scholar]
- Henke K, Weber B, Kneifel S, Wieser HG, Buck A. Human hippocampus associates information in memory. PNAS. 1999;96:5884–5889. doi: 10.1073/pnas.96.10.5884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermann BP, Wyler AR, Somes G, Berry AD, Dohan FC. Pathological status of the mesial temporal lobe predicts memory outcome from left anterior temporal lobectomy. Neurosurgery. 1992;31:652–657. doi: 10.1227/00006123-199210000-00006. [DOI] [PubMed] [Google Scholar]
- Hermann BP, Wyler AR, Somes G, Clement L. Dysnomia after left anterior temporal lobectomy without functional mapping: frequency and correlates. Neurosurgery. 1994;35:52–57. doi: 10.1227/00006123-199407000-00008. [DOI] [PubMed] [Google Scholar]
- Hermann BP, Seidenberg M, Haltiner A, Wyler AR. Relationship of age at onset, chronologic age, and adequacy of preoperative performance to verbal memory change after anterior temporal lobectomy. Epilepsia. 1995;36:137–145. doi: 10.1111/j.1528-1157.1995.tb00972.x. [DOI] [PubMed] [Google Scholar]
- Hermann BP, Seidenberg M, Schoenfeld J, Peterson J, Leveroni C, Wyler AR. Empirical techniques for determining the reliability, magnitude, and pattern of neuropsychological change after epilepsy surgery. Epilepsia. 1996;37:942–950. doi: 10.1111/j.1528-1157.1996.tb00531.x. [DOI] [PubMed] [Google Scholar]
- Hermann BP, Seidenberg M, Schoenfeld J, Davies K. Neuropsychological characteristics of the syndrome of mesial temporal lobe epilepsy. Arch Neurol. 1997;54:369–376. doi: 10.1001/archneur.1997.00550160019010. [DOI] [PubMed] [Google Scholar]
- Hughes TS, Abou-Khalil B, Lavin PJ, Fakhoury T, Blumenkopf B, Donahue SP. Visual field defects after temporal lobe resection: a prospective quantitative analysis. Neurology. 1999;53:167–172. doi: 10.1212/wnl.53.1.167. [DOI] [PubMed] [Google Scholar]
- Janszky J, Jokeit H, Kontopoulou K, Mertens M, Ebner A, Pohlmann-Eden B, Woermann FG. Functional MRI predicts memory performance after right mesiotemporal epilepsy surgery. Epilepsia. 2005;46:244–250. doi: 10.1111/j.0013-9580.2005.10804.x. [DOI] [PubMed] [Google Scholar]
- Jokeit H, Ebner A, Holthausen H, Markowitsch HJ, Moch A, Pannek H, Schulz R, Tuxhorn I. Individual prediction of change in delayed recall of prose passages after left-sided anterior temporal lobectomy. Neurology. 1997;49:481–487. doi: 10.1212/wnl.49.2.481. [DOI] [PubMed] [Google Scholar]
- Kapur N, Prevett M. Unexpected amnesia: are there lessons to be learned from cases of amnesia following unilateral temporal lobe surgery? Brain. 2003;126:2573–2585. doi: 10.1093/brain/awg275. [DOI] [PubMed] [Google Scholar]
- Katz A, Awad I, Kong A, Chelune G, Naugle R, Wyllie E, Beauchamp G, Lüders H. Extent of resection in temporal lobectomy for epilepsy: II. memory changes and neurologic complications. Epilepsia. 1989;30:763–771. doi: 10.1111/j.1528-1157.1989.tb05336.x. [DOI] [PubMed] [Google Scholar]
- Kirsch HE, Walker JA, Winstanley FS, Hendrickson R, Wong ST, Barbaro NM, Laxer KD, Garcia PA. Limitations of Wada memory asymmetry as a predictor of outcomes after temporal lobectomy. Neurology. 2005;65:676–680. doi: 10.1212/01.wnl.0000174440.31387.65. [DOI] [PubMed] [Google Scholar]
- Kneebone AC, Chelune GJ, Dinner DS, Naugle RI, Awad IA. Intracarotid amobarbital procedure as a predictor of material-specific memory change after anterior temporal lobectomy. Epilepsia. 1995;36:857–865. doi: 10.1111/j.1528-1157.1995.tb01628.x. [DOI] [PubMed] [Google Scholar]
- Kneebone AC, Chelune GJ, Dinner DS, et al. Individual patient prediction of seizure lateralization in temporal lobe epilepsy: a comparison between neuropsychological memory measures and the intracarotid amobarbital procedure. J Int Neuropsychol Soc. 1997;3:159–168. [PubMed] [Google Scholar]
- Kubu CS, Girvin JP, McLachlan RS, Pavol M, Harnadek MC. Does the intracarotid amobarbital procedure predict global amnesia after temporal lobectomy? Epilepsia. 2000;41:1321–1329. doi: 10.1111/j.1528-1157.2000.tb04612.x. [DOI] [PubMed] [Google Scholar]
- Lacruz ME, Alarcon G, Akanuma N, Lum FC, Kissani N, Koutroumanidis M, Adachi N, Binnie CD, Polkey CE, Morris RG. Neuropsychological effects associated with temporal lobectomy and amygdalohippocampectomy depending on Wada test failure. J Neurol Neurosurg Psychiatry. 2004;75:600–607. doi: 10.1136/jnnp.2003.020248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langfitt JT, Rausch R. Word-finding deficits persist after left anterotemporal lobectomy. Arch Neurol. 1996;53:72–76. doi: 10.1001/archneur.1996.00550010090021. [DOI] [PubMed] [Google Scholar]
- Langfitt JT, Westerveld M, Hamberger MJ, Walczak TS, Cicchetti DV, Berg AT, Vickrey BG, Barr WB, Sperling MR, Masur D, Spencer SS. Worsening of quality of life after epilepsy surgery: effect of seizures and memory decline. Neurology. 2007;68:1988–1994. doi: 10.1212/01.wnl.0000264000.11511.30. [DOI] [PubMed] [Google Scholar]
- Lee GP, Loring DW, Smith JR, Flanigin HF. Intraoperative hippocampal cooling and Wada memory testing in the evaluation of amnesia risk following anterior temporal lobectomy. Arch Neurol. 1995;52:857–861. doi: 10.1001/archneur.1995.00540330035011. [DOI] [PubMed] [Google Scholar]
- Lee TMC, Yip JTH, Jones-Gotman M. Memory deficits after resection of left or right anterior temporal lobe in humans: A meta-analytic review. Epilepsia. 2002;43:283–291. doi: 10.1046/j.1528-1157.2002.09901.x. [DOI] [PubMed] [Google Scholar]
- Lineweaver TT, Naugle RI, Cafaro AM, Bingaman W, Luders HO. Patients' perceptions of memory functioning before and after surgical intervention to treat medically refractory epilepsy. Epilepsia. 2004;45:1604–1612. doi: 10.1111/j.0013-9580.2004.54503.x. [DOI] [PubMed] [Google Scholar]
- Lineweaver TT, Morris HH, Naugle RI, Najm IM, Diehl B, Bingaman W. Evaluating the contributions of state-of-the-art assessment techniques to predicting memory outcome after unilateral anterior temporal lobectomy. Epilepsia. 2006;47:1895–1903. doi: 10.1111/j.1528-1167.2006.00807.x. [DOI] [PubMed] [Google Scholar]
- Loddenkemper T, Morris HH, Lineweaver TT, Kellinghaus C. Repeated intracarotid amobarbital tests. Epilepsia. 2007;48:553–558. doi: 10.1111/j.1528-1167.2007.00982.x. [DOI] [PubMed] [Google Scholar]
- Loring DW, Lee GP, Meador KJ, Flanigin HF, Figueroa RE, Martin RC. The intracarotid amobarbital procedure as a predictor of memory failure following unilateral temporal lobectomy. Neurology. 1990;40:605–610. doi: 10.1212/wnl.40.4.605. [DOI] [PubMed] [Google Scholar]
- Loring DW, Meador KJ, Lee GP, King DW. Amobarbital Effects and Lateralized Brain Function: The Wada Test. Springer-Verlag; New York: 1992. [Google Scholar]
- Loring DW, Hermann BP, Meador KJ, Lee GP, Gallagher BB, King DW, Murro AM, Smith JR, Wyler AR. Amnesia after unilateral temporal lobectomy: a case report. Epilepsia. 1994a;35:757–763. doi: 10.1111/j.1528-1157.1994.tb02507.x. [DOI] [PubMed] [Google Scholar]
- Loring DW, Meador KJ, Lee GP, King DW, Gallagher BB, Murro AM, Smith JR. Stimulus timing effects on Wada memory testing. Arch Neurol. 1994b;51:806–810. doi: 10.1001/archneur.1994.00540200086020. [DOI] [PubMed] [Google Scholar]
- Loring DW, Hermann BP, Perrine K, Plenger PM, Lee GP, Nichols ME, Meador KJ. Memory for real objects is superior to line drawing recognition in discrimination of lateralized temporal lobe impairment during the Wada test. J Int Neuropsychol Soc. 1995a;1:134. [Google Scholar]
- Loring DW, Meador KJ, Lee GP, King DW, Nichols ME, Park YD, Murro AM, Gallagher BB, Smith JR. Wada memory asymmetries predict verbal memory decline after anterior temporal lobectomy. Neurology. 1995b;45:1329–1333. doi: 10.1212/wnl.45.7.1329. [DOI] [PubMed] [Google Scholar]
- Martin A. Automatic activation of the medial temporal lobe during encoding: Lateralized influences of meaning and novelty. Hippocampus. 1999;9:62–70. doi: 10.1002/(SICI)1098-1063(1999)9:1<62::AID-HIPO7>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Martin RC, Sawrie SM, Roth DL, Giliam FG, Faught E, Morawetz RB, Kuzniecky R. Individual memory change after anterior temporal lobectomy: a base rate analysis using regression-based outcome methodology. Epilepsia. 1998;39:1075–1082. doi: 10.1111/j.1528-1157.1998.tb01293.x. [DOI] [PubMed] [Google Scholar]
- Martin RC, Grote CL. Does the Wada test predict memory decline following epilepsy surgery. Epil Behav. 2002;3:4–15. [Google Scholar]
- McIntosh AM, Wilson SJ, Berkovic SF. Seizure outcome after temporal lobectomy: current research practice and findings. Epilepsia. 2001;42:1288–1307. doi: 10.1046/j.1528-1157.2001.02001.x. [DOI] [PubMed] [Google Scholar]
- Milner B, Branch C, Rasmussen T. Study of short-term memory after intracarotid injection of sodium amytal. Trans Am Neurol Assoc. 1962;87:224–226. [Google Scholar]
- Milner B. Memory and the medial temporal regions of the brain. In: Pribram KH, Broadbent DE, editors. Biology of Memory. Academic Press; New York: 1970. pp. 29–50. [Google Scholar]
- Novelly RA, Williamson PD. Incidence of false-positive memory impairment in the intracarotid Amytal procedure. Epilepsia. 1989;30:711. [Google Scholar]
- Ojemann GA, Dodrill CB. Verbal memory deficits after left temporal lobectomy for epilepsy. J Neurosurg. 1985;62:101–107. doi: 10.3171/jns.1985.62.1.0101. [DOI] [PubMed] [Google Scholar]
- Perrine K, Hermann BP, Meador KJ, Vickrey BG, Cramer JA, Hays RD, Devinsky O. The relationship of neuropsychological functioning to quality of life in epilepsy. Arch Neurol. 1995;52:997–1003. doi: 10.1001/archneur.1995.00540340089017. [DOI] [PubMed] [Google Scholar]
- Rabin ML, Narayan VM, Kimberg DY, Casasanto DJ, Glosser G, Tracy JI, French JA, Sperling MR, Detre JA. Functional MRI predicts post-surgical memory following temporal lobectomy. Brain. 2004;127:2286–2298. doi: 10.1093/brain/awh281. [DOI] [PubMed] [Google Scholar]
- Rao SM, Hammeke TA, McQuillen MP, Khatri BO, Lloyd D. Memory disturbance in chronic progressive multiple sclerosis. Arch Neurol. 1984;41:625–631. doi: 10.1001/archneur.1984.04210080033010. [DOI] [PubMed] [Google Scholar]
- Rausch R, Babb TL. Hippocampal neuron loss and memory scores before and after temporal lobe surgery for epilepsy. Arch Neurol. 1993;50:812–817. doi: 10.1001/archneur.1993.00540080023008. [DOI] [PubMed] [Google Scholar]
- Rausch R, Silfvenius H, Wieser H-G, Dodrill CB, Meador KJ, Jones-Gotman M. Intraarterial amobarbital procedures. In: Engel J, editor. Surgical treatment of the epilepsies. 2. Raven Press; New York: 1993. pp. 341–357. [Google Scholar]
- Richardson MP, Strange BA, Duncan JS, Dolan RJ. Memory fMRI in left hippocampal sclerosis. Optimizing the approach to predicting postsurgical memory. Neurology. 2006;66:699–705. doi: 10.1212/01.wnl.0000201186.07716.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruff RM, Light RH, Quayhagen M. Selective reminding tests: a normative study of verbal learning in adults. J Clin Exp Neuropsychol. 1989;11:539–550. doi: 10.1080/01688638908400912. [DOI] [PubMed] [Google Scholar]
- Sabsevitz DS, Swanson SJ, Morris GL, Mueller WM, Seidenberg M. Memory outcome after left anterior temporal lobectomy in patients with expected and reversed Wada memory asymmetry scores. Epilepsia. 2001;42:1408–1415. doi: 10.1046/j.1528-1157.2001.38500.x. [DOI] [PubMed] [Google Scholar]
- Sabsevitz DS, Swanson SJ, Hammeke TA, Spanaki MV, Possing ET, Morris GL, Mueller WM, Binder JR. Use of preoperative functional neuroimaging to predict language deficits from epilepsy surgery. Neurology. 2003;60:1788–1792. doi: 10.1212/01.wnl.0000068022.05644.01. [DOI] [PubMed] [Google Scholar]
- Saling MM, Berkovic SF, O'Shea MF, Kalnins RM, Darby DG, Bladin PF. Lateralization of verbal memory and unilateral hippocampal sclerosis: evidence of task-specific effects. J Clin Exp Neuropsychol. 1993;15:608–618. doi: 10.1080/01688639308402582. [DOI] [PubMed] [Google Scholar]
- Sass KJ, Spencer SS, JHK, Westerveld M, Novelly RA, Lencz T. Verbal memory impairment correlates with hippocampal pyramidal cell density. Neurology. 1990;40:1694–1697. doi: 10.1212/wnl.40.11.1694. [DOI] [PubMed] [Google Scholar]
- Sass KJ, Westerveld M, Buchanan CP, Spencer SS, Kim JH, Spencer DP. Degree of hippocampal neuron loss determines severity of verbal memory decrease after left anteromesiotemporal lobectomy. Epilepsia. 1994;35:1179–1186. doi: 10.1111/j.1528-1157.1994.tb01786.x. [DOI] [PubMed] [Google Scholar]
- Saykin AJ, Gur RC, Sussman NM, Gur RE, O'Connor MJ. Memory before and after temporal lobectomy: effects of laterality and age of onset. Brain Cogn. 1989;9:191–200. doi: 10.1016/0278-2626(89)90029-8. [DOI] [PubMed] [Google Scholar]
- Scoville WB, Milner B. Loss of recent memory after bilateral hippocampal lesions. J Neurol Neurosurg Psychiatry. 1957;20:11–21. doi: 10.1136/jnnp.20.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidenberg M, Hermann B, Wyler AR, Davies K, Dohan FC, Leveroni C. Neuropsychological outcome following anterior temporal lobectomy in patients with and without the syndrome of mesial temporal lobe epilepsy. Neuropsychology. 1998;12:303–316. doi: 10.1037//0894-4105.12.2.303. [DOI] [PubMed] [Google Scholar]
- Simkins-Bullock J. Beyond speech lateralization: a review of the variability, reliability, and validity of the intracarotid amobarbital procedure and its nonlanguage uses in epilepsy surgery candidates. Neuropsychol Rev. 2000;10:41–74. doi: 10.1023/a:1009044630227. [DOI] [PubMed] [Google Scholar]
- Springer JA, Binder JR, Hammeke TA, Swanson SJ, Frost JA, Bellgowan PSF, Brewer CC, Perry HM, Morris GL, Mueller WM. Language dominance in neurologically normal and epilepsy subjects: a functional MRI study. Brain. 1999;122:2033–2045. doi: 10.1093/brain/122.11.2033. [DOI] [PubMed] [Google Scholar]
- Squire LR. Memory and the hippocampus: a synthesis from findings with rats, monkeys, and humans. Psychol Rev. 1992;99:195–231. doi: 10.1037/0033-295x.99.2.195. [DOI] [PubMed] [Google Scholar]
- Stroup E, Langfitt JT, Berg M, McDrmott M, Pilcher W, Como P. Predicting verbal memory decline following anterior temporal lobectomy (ATL) Neurology. 2003;60:1266–1273. doi: 10.1212/01.wnl.0000058765.33878.0d. [DOI] [PubMed] [Google Scholar]
- Szaflarski JP, Binder JR, Possing ET, McKiernan KA, Ward DB, Hammeke TA. Language lateralization in left-handed and ambidextrous people: fMRI data. Neurology. 2002;59:238–244. doi: 10.1212/wnl.59.2.238. [DOI] [PubMed] [Google Scholar]
- Tellez-Zenteno JF, Dhar R, Wiebe S. Long-term seizure outcomes following epilepsy surgery: a systematic review and meta-analysis. Brain. 2005;128:1188–1198. doi: 10.1093/brain/awh449. [DOI] [PubMed] [Google Scholar]
- Trenerry MR, Jack CRJ, Ivnik RJ, Sharbrough FW, Cascino GD, Hirschorn KA, Marsh WR, Kelly PJ, Meyer FB. MRI hippocampal volumes and memory function before and after temporal lobectomy. Neurology. 1993;43:1800–1805. doi: 10.1212/wnl.43.9.1800. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Memory Scale - Revised. Psychological Corporation; San Antonio, TX: 1987. [Google Scholar]
- Wechsler D. Wechsler Memory Scale - Third Edition. Psychological Corporation; San Antonio, TX: 1997. [Google Scholar]
- Wendel JD, Trenerry MR, Xu YC, Sencakova D, Cascino GD, Britton JW, Lagerlund TD, Shin C, So EL, Sharbrough FW, Jack CR. The relationship between quantitative T2 relaxometry and memory in nonlesional temporal lobe epilepsy. Epilepsia. 2001;42:863–869. doi: 10.1046/j.1528-1157.2001.042007863.x. [DOI] [PubMed] [Google Scholar]
- Wiebe S, Blume W, Girvin JP, Eliasziw M. A randomized, controlled trial of surgery for temporal-lobe epilepsy. NEJM. 2001;345:311–318. doi: 10.1056/NEJM200108023450501. [DOI] [PubMed] [Google Scholar]
- Wolf RL, Ivnik RJ, Hirschorn KA, Sharbrough FW, Cascino GF, Marsh WR. Neurocognitive efficiency following left temporal lobectomy: standard versus limited resection. J Neurosurg. 1993;79:76–83. doi: 10.3171/jns.1993.79.1.0076. [DOI] [PubMed] [Google Scholar]
- Wyler AR, Hermann BP, Somes G. Extent of medial temporal resection and outcome from anterior temporal lobectomy: a randomized prospective study. Neurosurgery. 1995;37:982–991. doi: 10.1227/00006123-199511000-00019. [DOI] [PubMed] [Google Scholar]