Abstract
This paper reviews systems and techniques to deliver simultaneous thermoradiotherapy of breast cancer. It first covers the clinical implementation of simultaneous delivery of superficial (microwave or ultrasound) hyperthermia and external photon beam radiotherapy, first using a Co-60 teletherapy unit and later medical linear accelerators. The parallel development and related studies of the SURLAS, an advanced system specifically designed and developed for simultaneous thermoradiotherapy, follows. The performance characteristics of the SURLAS are reviewed and power limitation problems at high acoustic frequencies (> 3MHz) are discussed along with potential solutions. Next, the feasibility of simultaneous SURLAS hyperthermia and IMRT/IGRT is established based on published and newly presented studies. Finally, based on the encouraging clinical results thus far, it is concluded that new trials employing the latest technologies are warranted along with further developments in treatment planning.
Keywords: breast, cancer, chest wall, heat, hyperthermia, radiation therapy, radiotherapy, radiosensitization, recurrence, thermoradiotherapy, simultaneous, ultrasound, intensity modulated
Hyperthermia and Cancer
Conventional hyperthermia in cancer therapy can be defined as the elevation of tissue temperatures to 41~43°C for more than 30 minutes. Hyperthermia is typically used as an adjunct therapy to radiotherapy and/or chemotherapy [1–5]. Many well-conducted clinical trials, including phase III multi-institutional trials following quality assurance guidelines, have shown that hyperthermia can significantly increase both local tumor control rates and duration of local control in tumors that recur or persist after surgery, radiotherapy and/or chemotherapy [6–9]. Furthermore, hyperthermia has been shown beneficial in the treatment of residual microscopic disease in the management of local-regional breast cancer [10], in the treatment of soft tissue sarcomas preoperatively with radiation [11], and in the treatment of deep pelvic tumors [12, 13]. A significant survival benefit was also reported when hyperthermia was combined with brachytherapy in the treatment of glioblastoma multiforme [14] and with external beam radiotherapy in the treatment of recurrent head and neck cancer [15].
In fact, when clinical trials have been conducted under widely accepted quality assurance guidelines—which implies matching the heating technology to the target site along with the implementation of a reasonable thermometry strategy—radiotherapy plus hyperthermia has always resulted in statistically better outcomes than radiotherapy alone [16].
Thermoradiotherapy of Breast Cancer
Patients with persistent and/or recurrent breast cancer and chest wall tumors have significantly benefited when hyperthermia has been added to their radiotherapy and/or chemotherapy regimens [17–26]. One of the physical reasons for the success of hyperthermia in this group of patients is the superficial location of the local disease. Superficial lesions are the least difficult to heat adequately because of their accessibility and proximity to external energy sources. The composition of the local anatomy may also contribute to better heating [27, 28]. Another possible reason may be that superficial lesions are more amenable to invasive thermometry and thermal mapping of temperature sensors, thus providing more temperature feedback data during treatment, which can be used to improve heat delivery and ensure treatment quality [29, 30].
Clinical research efforts have demonstrated that the response of cancerous tumors to sequential thermoradiotherapy (i.e., sequentially combined radiotherapy and hyperthermia) is well correlated with power deposition coverage and/or thermal dose coverage [24, 30–40]. These studies have also point to the challenge of achieving consistently biologically meaningful thermal doses in 100% of the target volume in routine clinical practice. Therefore, it is widely accepted that the benefits of hyperthermia as an adjunct to radiotherapy can be significantly augmented with improvements in treatment delivery techniques, better heating technology, advances in treatment planning and implementation of quality assurance guidelines [6, 13, 30, 41, 42]. Moreover, in vitro and animal studies have shown that when hyperthermia and radiation are administered simultaneously —rather than sequentially as it is conventionally done—heat-induced radiosensitization (HIR) is increased at thermal doses achievable in the clinic [43–47]. For instance, mild hyperthermia—41°C maintained for ~60 minutes—produces HIR if radiation and heat are delivered simultaneously, but not sequentially. This is significant because a minimum target temperature of 41°C is more clinically achievable than the > 42°C needed to produce HIR with sequential treatment [44, 47, 48]. The above facts support the development of clinical hyperthermia devices that permit simultaneous delivery of heat and ionizing radiation.
Clinically Implemented Approaches for Simultaneous Thermoradiotherapy of Breast Cancer
In this section, a review is given of the systems and techniques clinically implemented for the delivery of simultaneous thermoradiotherapy at Washington University in St. Louis. This research group has been the only one to complete several simultaneous thermoradiotherapy clinical trials with breast cancer being the site treated the most.
Microwave Hyperthermia and Co-60 Teletherapy
Although it had been known from in vitro and in vivo experiments that simultaneous delivery resulted in larger thermal enhancement ratios than sequential delivery, simultaneous treatments had not been tried with human patients mainly due to formidable logistical problems [46]. The research group set out to overcome these problems and embark in a long-term clinical research effort. The first approach consisted of heating with 915 MHz microwave applicators and irradiating with a Co-60 teletherapy unit [49]. Both technologies enjoyed extensive clinical experience, were well-understood and had been used in sequential thermoradiotherapy [39, 40]. Therefore, any unusual response to the new therapy approach could be attributed to the simultaneous delivery of heat and gamma radiation. Hyperthermia waveguide applicators were used, one at the time. Two clinical setups were characterized. In one a microwave applicator was attached to a blocking tray and inserted into the tray slot in the head of the gantry of the teletherapy unit. Thus the gamma beam traveled through a mostly hollowed waveguide and into a treatment volume after transversing a mineral oil coupling bolus. This was called the en face setup. The other setup was with the microwave propagation vector perpendicular to the gamma beam central axis. This was called the orthogonal setup. Using these setups a 400 cGy radiation fraction of 4 to 7 minutes duration could be delivered in the middle of a 60 minute hyperthermia treatment without interruptions. Temperatures and power level were remotely monitored and recorded outside the teletherapy room. The microwave applicator was not mounted or in contact with the teletherapy unit in the orthogonal setup, so it did not affected the radiation dose distributions. However, for the en face setup the dose distributions were affected by the microwave applicator. Film measurements in a solid water phantom showed uniform dose within the radiation field, except for 10–18% attenuation under the metal tuning electrodes inside the waveguide. This dose defect was clinically smoothed using feathering techniques. This approach was used successfully without technical problems in a phase I/II clinical trial. Importantly, an analysis showed that the temperature distributions achieved during simultaneous delivery had the same general characteristics as those achieved during sequential delivery, and that the steady state distributions were maintained during the time of simultaneous irradiation. This first experience demonstrated that simultaneous superficial microwave hyperthermia and external beam radiation was technically feasible and safe [49].
Ultrasound Hyperthermia and Co-60 Teletherapy
The waveguide microwave applicators limited the size of the lesions we could treat with hyperthermia simultaneously with gamma rays [39, 40]. In order to be able to treat larger lesions, we decided to adapt a commercial planar ultrasound system to deliver simultaneous treatments. This task was much more challenging because the ultrasound applicators were not hollowed like the microwave waveguides and degassed water was needed to couple the sound waves into the treatment volume. The ultrasound applicators of the Labthermics 1000 system were also bulkier and heavier than the microwave applicators. An orthogonal setup similar to the one used with microwaves was relatively simple to mimic, but many tumor sites would require an en face setup for proper treatment. Since ultrasound is reflected efficiently and specularly from metal surfaces, we devised a reflecting system in which the ultrasound beam, initially directed perpendicularly to the gamma beam, was deflected 90° so that both beams travel through the same window of entry into the tumor while the ultrasound source remained outside the radiation beam [50]. The reflecting system, which was mounted on the blocking tray, was filled with degassed water and made of water-equivalent materials, except for a 1 mm sheet of polished brass used as the reflector. With this en face approach the absorbed power patterns generated with and without the reflecting system at the same extended distance from the transducer demonstrated that the hyperthermia system remained able to control heating pattern s. The effect of the reflecting system on the gamma beam was minimal except for uniform attenuation, and the Co-60 beam had no effect on the performance of the thermocouples. Extensive testing followed by clinical treatments of patients on protocol demonstrated that the modifications made did not impair the ability to deliver ultrasound hyperthermia or teletherapy effectively. Again, this work showed that the implementation of ultrasound hyperthermia simultaneous with gamma irradiation was technically and clinically feasible without complications or hazards to patients.
Superficial (Microwave or Ultrasound) Hyperthermia and Mega voltage Photon Beam Radiation using a Medical Linear Accelerator (Linac)
In 1995 the Co-60 teletherapy unit at the Mallinckrodt Institute of Radiology was decommissioned. The only option for external beam radiation was to develop the devices and techniques to allow the use of a medical linear accelerator. Although excited about the use of modern radiation technology, the transfer to megavoltage photon beam necessitated additional developments and measurements. Both the orthogonal and the en face setups were successfully transferred, but had to be adapted to the different geometry and dimensions of the linear accelerator. Straube et al. (2001) reported on devices, techniques and dosimetry for simultaneous thermoradiotherapy delivered with a linear accelerator including detailed day-to-day simulation and treatment procedures [51].
Summary of Simultaneous Thermoradiotherapy Clinical Trials
The above described developments have made possible the conduct of clinical trials since 1992. The first phase I trial was ended successfully in 1995, a second phase I/II dose escalation trial closed in 2001, and a third trial was initiated 1999. These clinical results have been summarized previously by Myerson et al. (1999, 2004) [44, 47]. Up-to-date, 119 patients have been enrolled on these three consecutive trials. The first two trials (60 cases) were for patients with macroscopic disease, usually recurrent after prior therapies, including radiotherapy, and escalated the number of simultaneous treatments from 3 to 8 in a course of 30–32 Gy. The third trial was to evaluate the short-and long -term effects and local control of simultaneous thermoradiotherapy in the treatment of high risk, but curative, subclinical (no visible disease after surgery and/or chemotherapy) breast carcinoma in patients with no prior radiotherapy. The simultaneous administration of radiotherapy and hyperthermia is of particular potential value for this patient population because tumor cells share normal tissue physiology. Fifty nine patients were accrued in this trial. The number of simultaneous treatments was escalated from 4 to 8 in a course of 60 Gy; most patients receiving 400 cGy per hyperthermia treatment—approximately 26% to 53% of the radiation dose was given under hyperthermic conditions. Elective hyperthermia was given to the primary tumor bed site plus an adjacent 6×12cm strip randomized to lie medial or lateral to the primary site. The adjacent strip served as an unheated but irradiated control. The first two studies demonstrated that the per treatment average thermal dose progressively improved with the number of hyperthermia treatments. In addition the product of radiation dose and total thermal dose was highly correlated with complete response [47]. In the third trial the overall local control was 97% with no significant morbidity difference between heated and control sectors and no increase in morbidity between 4 and 8 simultaneous treatments.
Finally, the data clearly shows that chest wall lesions (recurrent breast cancer) have been the most responsive to simultaneous thermoradiotherapy with highly significant statistical correlation with radio-thermal dose factors (p < 0.05) [47]. This exciting finding points to the importance of developing thermoradiotherapy treatment planning systems and continuing efforts to improve clinical thermal dosimetry techniques.
The SURLAS: A Device Developed for Simultaneous Thermoradiotherapy
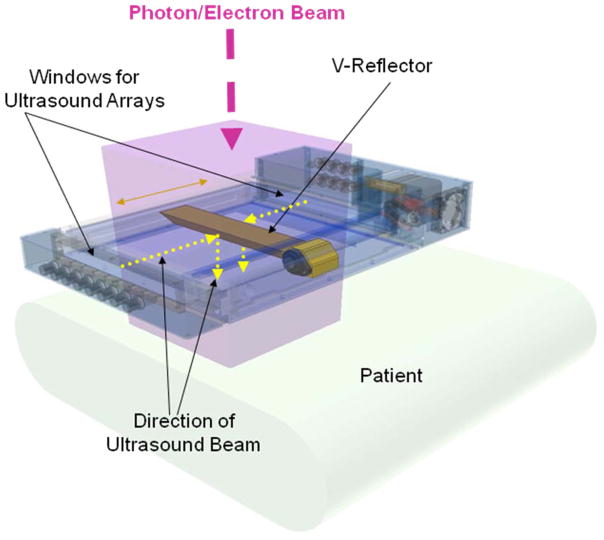
In parallel with the efforts to adapt existing commercially available hyperthermia technology to deliver simultaneous hyperthermia and external photon beam radiation, ideas were being discussed for the development of a system specifically designed for this purpose. During the decade of the nineties, electron beams were used commonly in the treatment of superficial lesions due to their limited depth of penetration, which meant sparing of underlying normal tissues. However, the existing hyperthermia devices were too bulky/dense to permit the use of electron beams. This was the main reason only high energy photon beams had been used when delivering simultaneous thermoradiotherapy. Eventually, the concept of the Scanning Ultrasound Reflector Linear Arrays System, or SURLAS, was born [52, 53]. By combining ultrasound linear arrays and scanning ultrasound reflectors, an applicator thin enough to permit the passage of high energy electron beams could be made to work using an en face approach. Obviously, photon beams would also work as in the past. The device concept is illustrated in Figure 1, which shows a computer-aided solid model of the clinical grade applicator that was developed [54, 55]. Figure 1 shows the basic components of a dual-frequency SURLAS applicator. The reflecting surfaces of a scanning double-faced V-shaped reflector make 45° angles with respect to the sound propagation coming from the (high and low frequency) arrays at the side ends of the applicator head (Figure 1 shows the windows for the arrays, not the arrays), thus both sound beams are deflected in parallel toward the treatment volume. As the reflector scans back and forth, the sound energy is distributed over the treatment volume producing therapeutic time-averaged temperature distributions with acceptable temperature fluctuations [56, 57]. Each array has several individually powered elements. Modulation of power input to the array elements as the reflector scans between the arrays provides control of the two-dimensional surface energy fluence pattern [55, 58]. This capability is referred to as Lateral Power Conformability or LPC. One of the arrays operates at a low frequency (1 ~ 2 MHz) while the other operates at a high frequency (3 ~ 5 MHz). This arrangement allows concomitant dual-frequency insonation. Penetration depth control, or PDC, is thus achieved by varying the power input to one array relative to the other’s, i.e., frequency mixing [59, 60]. For example, for areas where the target volume is deeper, the low frequency can be weighted more heavily than the high frequency. LPC plus PDC means that the SURLAS has 3D power deposition control, which can eventually be fully exploited with the implementation of temperature feedback control strategies based on temperatures measured during treatment [61].
Figure 1.
Three dimensional model of the SURLAS applicator showing basic components.
Several laboratory prototypes of the SURLAS were developed over the years in order to demonstrate feasibility of the overall concept and of particular features such as LPC and PDC. Finally, a clinical grade system was developed that could be used under approval of the Federal Food and Drug Administration (FDA) via the Investigational Device Exemption (IDE). However, manufacturing a clinical device proved to be a much more rigorous process than assembling prototypes for laboratory studies. Important requirements concerning reliability, patient and operator safety, and quality control/assurance presented great challenges to there search group. In addition to these rigorous requirements, the following were specific design criteria for the clinical SURLAS applicator:
Capable of heating superficial tumors extending up to 3 cm deep and up to 15 cm × 15 cm of lateral dimensions.
Capable of controlling power deposition in three dimensions.
No operational interference with radiotherapy linear accelerators.
Suitable for delivery of an external photon (en face or orthogonal setups) or electron (en face setup only) beam radiation during a hyperthermia treatment.
Significantly more compact and lighter than existing commercial ultrasound applicators.
These design criteria were met for the most part as reported in a paper published in early 2005 that focused mainly on the hardware components of the clinical grade SURLAS [54]. A second paper published later that same year reported on the design, development, and testing of the personal computer based treatment delivery software that coordinated the interactions between the operator, the SURLAS applicator and several peripheral devices [55]. There were two important tasks in software development worth mentioning here. The first was the coordination of the input power sequences to the elements of the high (4.9 MHz) and the low (1.9 MHz) frequency arrays (eight 1.5 cm × 2.0 cm elements/array) with the position of the dual-face scanning reflector. This was achieved by dividing the treatment window in up to 64 sectors (minimum size of 2cm × 2 cm) and controlling the power delivery to each sector independently by adjusting the output power from the 16 channels of a programmable radio-frequency generator. Upon completion of the software development process, it was integrated with the hardware followed by extensive testing. The second important task was safety, which was a paramount concern and design criterion. To ensure safety, a failure mode and effects analysis, or FMEA, was applied to the entire system in order to identify safety issues and rank their relative importance. The FMEA analysis led to the implementation of a software structure where each peripheral device communicated independently and directly with the controlling personal computer, so that in case of a malfunction in any component of the system or any violation of a pre-defined safety criterion, the software can terminate treatment immediately.
Performance of the SURLAS
As mentioned before the original motivation and goal was to develop an ultrasound hyperthermia device that would enable simultaneous hyperthermia and electron beam radiation [52]. Consequently, we tried to make the profile (height) of the SURLAS as small as possible in order that a high energy electron beam could travel through it and still be energetic enough to penetrate into superficial lesions as deep as 3 cm (electron beams are attenuated in water about 2 MeV/cm and the 80 to 90% isodose cloud is commonly used for tumor coverage). This meant that we implemented the smallest arrays possible that our previous studies indicated suitable in terms of the required emittance (W/cm2) to induce adequate hyperthermia. Note that the smaller the array the higher the required continuous wave (CW) emittance. This choice and other factors discussed below, however, created problems in practice that required time to figure out and resolve and de railed the clinical translation of the SURLAS.
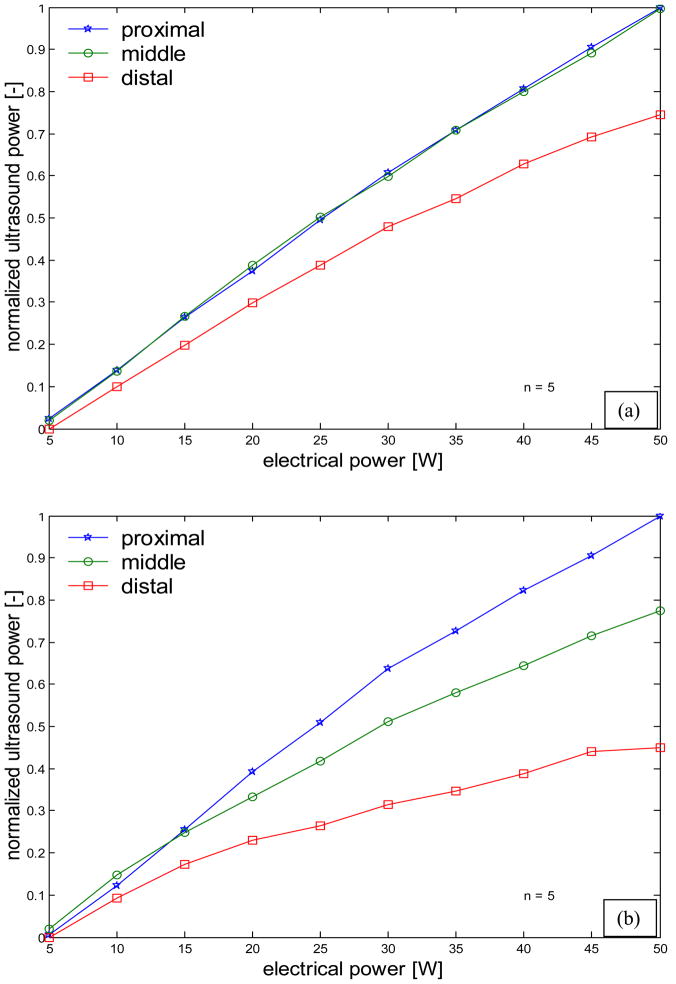
The major problem was a decrease in electrical-to-acoustic efficiency with increasing transducer-to-reflector distance [54]. This was particularly obvious for the high frequency array as shown in Figure 2, which presents radiation force balance measurements for the low (2a) and high (2b) linear arrays. This loss of ultrasonic power with distance was determined to be non -linear propagation, a subject of much research in recent years. Essentially, nonlinear propagation is the conversion of ultrasonic energy from the fundamental frequency to higher frequency harmonics as the waves are distorted while propagating from sinusoidal-like to sawtooth-like [62]. The wave distortion increases with the acoustic intensity, increasing distance from the source and increasing frequency. It also depends on the characteristics of the medium. This phenomenon has been described by the shock parameter σ [63],
Figure 2.
Force balance results for the low (a) and high (b) frequency arrays. The three curves in each plot are for measurements for three different positions of the reflector with respect to an array. Distal was when the reflector was the furthest from then array in question and thus the ultrasound traveled the longest before reaching the force balance detector. Each data value was the average of five measurements. Standard deviations were too small to plot as error bars.
| (1) |
where β is the coefficient of nonlinearity of the medium, ε is the mach number, k is the wave number, and x the travel distance. Based on calculations using the shock parameter we determined that the high frequency array was suffering significant power loss due to non-linear propagation. For the clinical SURLAS, the maximum travel distance of the waves from the array to the distal water bolus membrane (including reflection) was about 23 cm. For the high frequency waves(~ 4.9 MHz), nonlinear propagation was calculated to occur at acoustic intensities as low as 0.7 W/cm 2at the maximum distance for σ =1 (onset of nonlinear propagation). The acoustic intensities required for hyperthermia are higher than this value [53]. Moreover, note that scanning of the ultrasound energy over the treatment window requires higher CW intensities in comparison to a single transducer of comparable size to the treatment window [53, 64]. When σ = 3, the waveforms become sawtooth causing intensity losses of 6 dB with respect to the fundamental frequency. Assuming plane wave behavior, a series of simulations were generated to determine 1) the CW intensity required for the clinical SURLAS to induce and maintain hyperthermic temperatures, and 2) the maximum deliverable CW intensity for a shock parameter equal to3 (σ = 3). The frequency, the treatment widow length (~ scanning distance), and height of the linear array were variables. Selected results are presented in Table 1, which shows the maximum fundamental frequency (fmax) for four treatment window lengths (WL) and three array heights (AH). The AH for the clinical SURLAS is 1.5 cm and the thickness of the water coupling bolus is approximately2 cm. The developed clinical SURLAS has a maximum window length of 16 cm. Table 1 indicates that to utilize a window this size fmax could not be higher than 1.89 MHz. The frequency of the high frequency array is ~ 4.9 MHz, hence significant nonlinear propagation effects are to be expected per equation (1) and as shown in Figure 2. We had seen this effect before with our commercial ultrasound system for the en face setup at the frequency of ~3.5 MHz [50], but the source to skin distance there was over 50 cm, and despite the ~40% reduction of power adequate hyperthermia treatments were possible. This indicated that other factors were contributing to low efficiencies. These were:
Table 1.
Maximum fundamental frequency (fmax) for four treatment window lengths (WL) and three array heights (AH).
| WL (cm) | AH = 1.5 cm | AH = 2.5 cm | AH = 5 cm |
|---|---|---|---|
| fmax (MHz) | fmax (MHz) | fmax (MHz) | |
| 10 | 4.5 | > 5.0 | > 5.0 |
| 12 | 3.03 | 3.8 | 4.29 |
| 14 | 2.32 | 2.85 | 3.27 |
| 16 | 1.89 | 2.29 | 2.67 |
Reflectivity of a Styrofoam reflector relative to a brass reflector was estimated to be as 0.76 at 5.0 MHz [52].
The first radio frequency generator used had a drop in electrical power output for frequencies > 3.5 MHz.
The array element size in the current arrays is 1.5 cm × 2 cm (the smallest ever used). This turned out to be too small due to: a) influence of the soldered spot and b) damping by the mount at the edges.
Beam divergence at large reflector-to-source distance due to small misalignment between the arrays and the reflector. Computer models had ruled out this possibility [53], but beam plot measurements of the clinical SURLAS suggested otherwise [54].
The message from Table 1 and the above listed factors is clear, to avoid nonlinear propagation and improve electrical-to-acoustic efficiency, a new SURLAS must be constructed considering the following: lower frequency for the high frequency array, larger surface areas arrays (larger AH), shorter treatment window length (smaller WL), reflecting areas > array projected areas, and a more powerful radiofrequency generator with flat frequency response. The lower frequency for the high frequency array means some reduction in PDC. The smaller treatment window implies a proportional reduction in the size of the treatment area. A larger array height means a higher profile applicator—less or not suitable for electron beams. And larger scanning (possibly metallic) reflector precludes electron beams. That leaves only photon beams for the delivery of simultaneous thermoradiotherapy with the SURLAS. As discussed in the next section, this was actually welcome news due to advances in modern radiotherapy, especially intensity modulated radiation therapy or IMRT, as it is commonly called.
SURLAS and IMRT/IGRT
Intensity modulated radiation therapy (IMRT) has become clinically widespread worldwide in the last decade [65]. IMRT’s appeal is its ability to focus dose to the targeted volume (commonly called the planning treatment volume or PTV) while minimizing dose to surrounding normal tissues. Our first working hypothesis was that IMRT can produce clinically acceptable dose distributions on a recurrent breast cancer tumor while that same tumor receives ultrasound hyperthermia using the SURLAS. To test this hypothesis two research projects were initiated: a radiation treatment planning study to compute dose distributions in recurrent breast cancer PTVs with the SURLAS applicator in place [66]; and an experimental study, where a radiation treatment plan was computed and delivered to a phantom with the SURLAS applicator on top of the phantom simulating a clinical setup, to evaluate the effects of the presence and potential misplacement of the SURLAS applicator on measured dose distributions [67].
The above studies were carried out using the treatment planning station and treatment unit of a Helical Tomotherapy (HT) system (Tomotherapy Inc., Madison, WI). This technology was chosen over conventional gantry-based medical linear accelerators (both available at our institution), because we thought that the multiplicity of beam angles and the helical motion would greatly minimize the perturbing effects of the SURLAS applicator on dose distributions. In addition, the mega voltage computed tomography (MVCT) feature of Tomotherapy, which is used for image-guided radiotherapy (IGRT) to verify the patient’s position right before treatment delivery, could also be used for treatment planning purposes without major image distortions or artifacts due to the metallic parts of the SURLAS applicator[68]. Moreover, the MVCT images could be also used to verify the position of the SURLAS applicator with respect to the patient and from treatment to treatment. All these ideas were tested successfully [66, 67].
The main conclusion from the treatment planning study was that simultaneous treatment with the SURLAS and HT IMRT/IGRT is feasible as demonstrated by the clinically acceptable radiation treatment plans generated [66]. Likewise, the main conclusion of the experimental study was that the delivered (measured) and planned radiation dose distributions were in excellent agreement when the SURLAS applicator was positioned as it was planned. Misplacement of the applicator from its planned position was found to have small effects on the measured dose distributions [67]. Potentially large discrepancies between planned and delivered doses due to gross misplacement of the SURLAS can be further minimized by the implementation of routine quality assurance procedures using a position-and-orientation magnetic tracking device which was successful in precisely and reproducibly positioning of the applicator. Moreover, it was shown that there is great potential for the use of this tracking device for monitoring of the SURLAS applicator position and orientation during simultaneous treatments, and not just for patient/SURLAS set-up prior to daily treatment using MVCT [67].
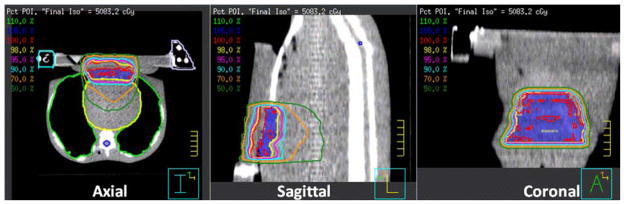
Do the above findings apply if a conventional medical linear accelerator is used? This is important question to answer because gantry-based linacs remain the most commonly used technology in radiation therapy departments. Here we present new treatment planning results that indicate that Linac-based IMRT can also deliver clinically acceptable radiation dose distributions with the SURLAS applicator on the patient’s chest wall. The clinical setup and planning MVCT can be seen on the axial plane of Figure 3. The PTV was the superficial case in Penagaricano et al. 2008, with maximum dimensions of 1 cm deep by 11.5 cm wide (lateral) by 11 cm long (superior-inferior) on the lower chest/upper abdominal wall mimicking a chest wall recurrence from breast cancer[66]. The results of Figures 3 and 4 were generated using the Pinnacle3 inverse IMRT treatment planning system (P3IMRT, Philips, Andover, MA) to model megavoltage photon beam dose deposition delivered by a Varian 2100 EX linear accelerator with 120-leaf dynamic multi-leaf collimator (Varian Medical Systems, Palo Alto, CA). A 12 beam plan was used, 8 beams were coplanar (linac central axis on the axial plane) and 4 beams were non-coplanar (linac central axis on the sagittal plane). Of the 8 coplanar beams, 6 were aimed from above the SURLAS applicator and 2 were aimed laterally and tangentially to the chest wall. The noncoplanar beams were all aimed from above. The prescription was 50 Gy in 25 fractions to 95% of the PTV using 6 MV photons. It was assumed that every fraction was given under hyperthermic conditions for the purpose of illustration. Cardiac toxicity would be solely dependent on radiation dose because none of the existing or forth coming devices would be able to induce significant hyperthermia in heart tissue due to 1) the depth of heart tissue and 2) the very high cardiac perfusion rates.
Figure 3.
Twelve-beam IMRT plan dose distributions on the axial, sagittal and coronal planes through the PTV and SURLAS applicator. An MVCT of the RANDO phantom with the SURLAS on top simulating a typical clinical setup for the treatment of chest wall recurrence of breast cancer was used as the planning CT.
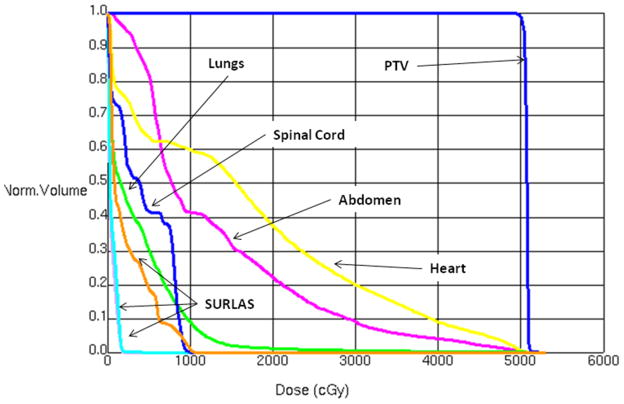
Figure 4.
Dose volume histograms for the PTV and organs at risks for the treatment plan shown in Figure 3.
Figure 3 shows computed dose distributions on the axial, sagittal and coronal planes through the PTV and SURLAS applicator. It can be readily seen that the mass was nicely covered by the prescription dose with low doses to surrounding normal tissues. Dose volume histograms (DVH) for the PTV and organs at risk are shown in Figure 4. These DVHs are clinically acceptable for the PTV and surrounding organs and are comparable to the ones obtained using the Tomotherapy system [66]. The PTV mean dose, the PTV D95%, the heart, lung and abdomen mean doses, and the spinal cord maximum dose were 50.7, 50.4, 16.7, 3.7, 12.9 and 10.0 Gy, respectively. These metrics are in good agreement with those reported by Penagaricano et al. 2008 for the Tomotherapy system (Table IV in [66]). In short, IMRT with either radiation therapy system is suitable for simultaneous thermoradiotherapy using the SURLAS.
Besides more conformal radiation doses, there are other advantages of using IMRT with the SURLAS. First, IMRT is expected to be highly forgiving of the modifications needed to the SURLAS applicator to minimize non-linear propagation and improve electrical-to-acoustical efficiencies. Second, the clinical experience thus far has only used one radiation beam concomitantly with hyperthermia; consequently the time of simultaneous delivery is short compared to the heating time. With IMRT and the SURLAS, the simultaneous time is expected to be longer for hyperthermia can be given during an entire multi-beam IMRT fraction. Third, the application of IGRT and magnetic position-orientation tracking technologies, to ensure reproducible applicator positioning prior and during the treatments, may encourage physicians to prescribe hyperthermia simultaneously with more if not every IMRT fraction. Finally, more simultaneous fractions should maximize the radiosensitizing and physiological effects of hyperthermia even if IMRT is delivered in shorter times using the emerging arc therapy paradigm [69].
Final Remarks
The clinical implementation of simultaneous thermoradiotherapy has been challenging but proven to be feasible and safe. Clinical trial results have been encouraging and breast cancers are thus far the most responsive, with statistically significant correlations (p < 0.05) with radio-thermal dosimetric factors [47]. Therefore, new technological developments such as combining the SURLAS and IMRT/IGRT with thermo-radio dose treatment planning should translate into improvements in radiothermal dose coverage and consequently in better treatment outcomes. Furthermore, several research groups have been developing advanced simultaneous heat and irradiation technologies that are moving toward clinical deployment while others have attempted different clinical approaches using existing hyperthermia devices [70–76]. In conclusion, new clinical protocols combining hypethermia and radiotherapy simultaneously are now possible and warranted.
Acknowledgments
The work reviewed in this paper was supported by NIH Grants CA 63121 and CA 71638, and by a grant from the Whitaker Foundation. We gratefully acknowledge partial support from the Central Arkansas Radiation Therapy Institute (CARTI) and a Medical Research Endowment pilot award from College of Medicine of the University of Arkansas for Medical Sciences, Little Rock. We thank our cancer patients for their courage and participation in the clinical research. Finally, we gratefully acknowledge the contributions of many collaborators over the years as reflected in the authorship of previously published papers and abstracts.
References
- 1.Kampinga HH. Cell biological effects of hyperthermia alone or combined with radiation or drugs: a short introduction to newcomers in the field. Int J Hyperthermia. 2006;22:191–6. doi: 10.1080/02656730500532028. [DOI] [PubMed] [Google Scholar]
- 2.Moyer HR, Delman KA. The role of hyperthermia in optimizing tumor response to regional therapy. Int J Hyperthermia. 2008;24:251–61. doi: 10.1080/02656730701772480. [DOI] [PubMed] [Google Scholar]
- 3.Hildebrandt B, Wust P. The biologic rationale of hyperthermia. Cancer Treat Res. 2007;134:171–84. doi: 10.1007/978-0-387-48993-3_10. [DOI] [PubMed] [Google Scholar]
- 4.Dewhirst MW, Vujaskovic Z, Jones E, et al. Re-setting the biologic rationale for thermal therapy. Int J Hyperthermia. 2005;21:779–90. doi: 10.1080/02656730500271668. [DOI] [PubMed] [Google Scholar]
- 5.Bergs JW, Franken NA, Haveman J, et al. Hyperthermia, cisplatin and radiation trimodality treatment: a promising cancer treatment? A review from preclinical studies to clinical application. Int J Hyperthermia. 2007;23:329–41. doi: 10.1080/02656730701378684. [DOI] [PubMed] [Google Scholar]
- 6.Dewhirst MW, Prosnitz L, Thrall D, et al. Hyperthermic treatment of malignant diseases: current status and a view toward the future. Semin Oncol. 1997;24:616–25. [PubMed] [Google Scholar]
- 7.Falk MH, Issels RD. Hyperthermia in oncology. Int J Hyperthermia. 2001;17:1–18. doi: 10.1080/02656730150201552. [DOI] [PubMed] [Google Scholar]
- 8.Hehr T, Wust P, Bamberg M, et al. Current and potential role of thermoradiotherapy for solid tumours. Onkologie. 2003;26:295–302. doi: 10.1159/000071628. [DOI] [PubMed] [Google Scholar]
- 9.Issels RD. Regional hyperthermia in high-risk soft tissue sarcomas. Curr Opin Oncol. 2008;20:438–43. doi: 10.1097/CCO.0b013e3283025e50. [DOI] [PubMed] [Google Scholar]
- 10.Kapp DS, Cox RS, Barnett TA, et al. Thermoradiotherapy for residual microscopic cancer: elective or post-excisional hyperthermia and radiation therapy in the management of local-regional recurrent breast cancer. Int J Radiat Oncol Biol Phys. 1992;24:261–77. doi: 10.1016/0360-3016(92)90681-7. [DOI] [PubMed] [Google Scholar]
- 11.Prosnitz LR, Maguire P, Anderson JM, et al. The treatment of high-grade soft tissue sarcomas with preoperative thermoradiotherapy. Int J Radiat Oncol Biol Phys. 1999;45:941–9. doi: 10.1016/s0360-3016(99)00272-2. [DOI] [PubMed] [Google Scholar]
- 12.van der Zee J, Gonzalez GD. The Dutch Deep Hyperthermia Trial: results in cervical cancer. Int J Hyperthermia. 2002;18:1–12. doi: 10.1080/02656730110091919. [DOI] [PubMed] [Google Scholar]
- 13.van der Zee J. Heating the patient: a promising approach? Ann Oncol. 2002;13:1173–84. doi: 10.1093/annonc/mdf280. [DOI] [PubMed] [Google Scholar]
- 14.Sneed PK, Stauffer PR, McDermott MW, et al. Survival benefit of hyperthermia in a prospective randomized trial of brachytherapy boost +/− hyperthermia for gliobla stoma multiforme. Int J Radiat Oncol Biol Phys. 1998;40:287–95. doi: 10.1016/s0360-3016(97)00731-1. [DOI] [PubMed] [Google Scholar]
- 15.Valdagni R, Amichetti M. Report of long-term follow-up in a randomized trial comparing radiation therapy and radiation therapy plus hyperthermia to metastatic lymph nodes in stage IV head and neck patients. Int J Radiat Oncol Biol Phys. 1994;28:163–9. doi: 10.1016/0360-3016(94)90154-6. [DOI] [PubMed] [Google Scholar]
- 16.Dewhirst MW, Sneed PK. Those in gene therapy should pay closer attention to lessons from hyperthermia. Int J Radiat Oncol Biol Phys. 2003;57:597–9. doi: 10.1016/s0360-3016(03)00421-8. author reply 599–600. [DOI] [PubMed] [Google Scholar]
- 17.Jones EL, Oleson JR, Prosnitz LR, et al. Randomized trial of hyperthermia and radiation for superficial tumors. J Clin Oncol. 2005;23:3079–85. doi: 10.1200/JCO.2005.05.520. [DOI] [PubMed] [Google Scholar]
- 18.Jones EL, Prosnitz LR, Dewhirst MW, et al. Thermochemoradiotherapy improves oxygenation in locally advanced breast cancer. Clin Cancer Res. 2004;10:4287–93. doi: 10.1158/1078-0432.CCR-04-0133. [DOI] [PubMed] [Google Scholar]
- 19.Feyerabend T, Wiedemann GJ, Jager B, et al. Local hyperthermia, radiation, and chemotherapy in recurrent breast cancer is feasible and effective except for inflammatory disease. Int J Radiat Oncol Biol Phys. 2001;49:1317–25. doi: 10.1016/s0360-3016(00)01514-5. [DOI] [PubMed] [Google Scholar]
- 20.Hehr T, Lamprecht U, Glocker S, et al. Thermoradiotherapy for locally recurrent breast cancer with skin involvement. Int J Hyperthermia. 2001;17:291–301. doi: 10.1080/02656730110049538. [DOI] [PubMed] [Google Scholar]
- 21.Jones EL, Marks LB, Prosnitz LR. Point: Hyperthermia with radiation for chest wall recurrences. J Natl Compr Canc Netw. 2007;5:339–44. doi: 10.6004/jnccn.2007.0029. [DOI] [PubMed] [Google Scholar]
- 22.Wahl AO, Rademaker A, Kiel KD, et al. Multi-institutional review of repeat irradiation of chest wall and breast for recurrent breast cancer. Int J Radiat Oncol Biol Phys. 2008;70:477–84. doi: 10.1016/j.ijrobp.2007.06.035. [DOI] [PubMed] [Google Scholar]
- 23.Welz S, Hehr T, Lamprecht U, et al. Thermoradiotherapy of the chest wall in locally advanced or recurrent breast cancer with marginal resection. Int J Hyperthermia. 2005;21:159–67. doi: 10.1080/02656730400003393. [DOI] [PubMed] [Google Scholar]
- 24.Lee HK, Antell AG, Perez CA, et al. Superficial hyperthermia and irradiation for recurrent breast carcinoma of the chest wall: prognostic factors in 196 tumors. Int J Radiat Oncol Biol Phys. 1998;40:365–75. doi: 10.1016/s0360-3016(97)00740-2. [DOI] [PubMed] [Google Scholar]
- 25.Kapp DS, Barnett TA, Cox RS, et al. Hyperthermia and radiation therapy of local-regional recurrent breast cancer: prognostic factors for response and local control of diffuse or nodular tumors. Int J Radiat Oncol Biol Phys. 1991;20:1147–64. doi: 10.1016/0360-3016(91)90220-x. [DOI] [PubMed] [Google Scholar]
- 26.Vernon CC, Hand JW, Field SB, et al. Radiotherapy with or without hyperthermia in the treatment of superficial localized breast cancer: results from five randomized controlled trials. International Collaborative Hyperthermia Group. Int J Radiat Oncol Biol Phys. 1996;35:731–44. doi: 10.1016/0360-3016(96)00154-x. [DOI] [PubMed] [Google Scholar]
- 27.Leon SA, Asbell SO, Edelstein G, et al. Effects of hyperthermia on bone. I. Heating rate patterns induced by microwave irradiation in bone and muscle phantoms. Int J Hyperthermia. 1993;9:69–75. doi: 10.3109/02656739309061479. [DOI] [PubMed] [Google Scholar]
- 28.Moros EG, Novak P, Straube WL, et al. Thermal contribution of compact bone to intervening tissue-like media exposed to planar ultrasound. Phys Med Biol. 2004;49:869–86. doi: 10.1088/0031-9155/49/6/001. [DOI] [PubMed] [Google Scholar]
- 29.Hand JW. Guidelines for thermometry in clinical hyperthermia. Front Med Biol Eng. 1992;4:99–104. [PubMed] [Google Scholar]
- 30.Dewhirst MW, Phillips TL, Samulski TV, et al. RTOG quality assurance guidelines for clinical trials using hyperthermia. Int J Radiat Oncol Biol Phys. 1990;18:1249–59. doi: 10.1016/0360-3016(90)90466-w. [DOI] [PubMed] [Google Scholar]
- 31.Cox RS, Kapp DS. Correlation of thermal parameters with outcome in combined radiation therapy-hyperthermia trials. Int J Hyperthermia. 1992;8:719–32. doi: 10.3109/02656739209005020. [DOI] [PubMed] [Google Scholar]
- 32.Hand JW, Machin D, Vernon CC, et al. Analysis of thermal parameters obtained during phase III trials of hyperthermia as an adjunct to radiotherapy in the treatment of breast carcinoma. Int J Hyperthermia. 1997;13:343–64. doi: 10.3109/02656739709046538. [DOI] [PubMed] [Google Scholar]
- 33.Sherar M, Liu FF, Pintilie M, et al. Relationship between thermal dose and outcome in thermoradiotherapy treatments for superficial recurrences of breast cancer: data from a phase III trial. Int J Radiat Oncol Biol Phys. 1997;39:371–80. doi: 10.1016/s0360-3016(97)00333-7. [DOI] [PubMed] [Google Scholar]
- 34.Kapp DS, Cox RS. Thermal treatment parameters are most predictive of outcome in patients with single tumor nodules per treatment field in recurrent adenocarcinoma of the breast. Int J Radiat Oncol Biol Phys. 1995;33:887–99. doi: 10.1016/0360-3016(95)00212-4. [DOI] [PubMed] [Google Scholar]
- 35.Leopold KA, Dewhirst M, Samulski T, et al. Relationships among tumor temperature, treatment time, and histopathological outcome using preoperative hyperthermia with radiation in soft tissue sarcomas. Int J Radiat Oncol Biol Phys. 1992;22:989–98. doi: 10.1016/0360-3016(92)90798-m. [DOI] [PubMed] [Google Scholar]
- 36.Leopold KA, Dewhirst MW, Samulski TV, et al. Cumulative minutes with T90 greater than Tempindex is predictive of response of superficial malignancies to hyperthermia and radiation. Int J Radiat Oncol Biol Phys. 1993;25:841–7. doi: 10.1016/0360-3016(93)90314-l. [DOI] [PubMed] [Google Scholar]
- 37.Oleson JR, Samulski TV, Leopold KA, et al. Sensitivity of hyperthermia trial outcomes to temperature and time: implications for thermal goals of treatment. Int J Radiat Oncol Biol Phys. 1993;25:289–97. doi: 10.1016/0360-3016(93)90351-u. [DOI] [PubMed] [Google Scholar]
- 38.Oleson JR, Dewhirst MW, Harrelson JM, et al. Tumor temperature distributions predict hyperthermia effect. Int J Radiat Oncol Biol Phys. 1989;16:559–70. doi: 10.1016/0360-3016(89)90472-0. [DOI] [PubMed] [Google Scholar]
- 39.Myerson RJ, Perez CA, Emami B, et al. Tumor control in long-term survivors following superficial hyperthermia. Int J Radiat Oncol Biol Phys. 1990;18:1123–9. doi: 10.1016/0360-3016(90)90448-s. [DOI] [PubMed] [Google Scholar]
- 40.Myerson RJ, Emami BN, Perez CA, et al. Equilibrium temperature distributions in uniform phantoms for superficial microwave applicators: implications for temperature-based standards of applicator adequacy. Int J Hyperthermia. 1992;8:11–21. doi: 10.3109/02656739209052875. [DOI] [PubMed] [Google Scholar]
- 41.Wust P, Hildebrandt B, Sreenivasa G, et al. Hyperthermia in combined treatment of cancer. Lancet Oncol. 2002;3:487–97. doi: 10.1016/s1470-2045(02)00818-5. [DOI] [PubMed] [Google Scholar]
- 42.Roemer RB. Engineering aspects of hyperthermia therapy. Annu Rev Biomed Eng. 1999;1:347–76. doi: 10.1146/annurev.bioeng.1.1.347. [DOI] [PubMed] [Google Scholar]
- 43.Dewey WC. Arrhenius relationships from the molecule and cell to the clinic. Int J Hyperthermia. 1994;10:457–83. doi: 10.3109/02656739409009351. [DOI] [PubMed] [Google Scholar]
- 44.Myerson RJ, Straube WL, Moros EG, et al. Simultaneous superficial hyperthermia and external radiotherapy: report of thermal dosimetry and tolerance to treatment. Int J Hyperthermia. 1999;15:251–66. doi: 10.1080/026567399285639. [DOI] [PubMed] [Google Scholar]
- 45.Steeves RA, Tompkins DT, Nash RN, et al. Thermoradiotherapy of intraocular tumors in an animal model: concurrent vs. sequential brachytherapy and ferromagnetic hyperthermia. Int J Radiat Oncol Biol Phys. 1995;33:659–62. doi: 10.1016/0360-3016(95)00206-E. [DOI] [PubMed] [Google Scholar]
- 46.Overgaard J. The current and potential role of hyperthermia in radiotherapy. Int J Radiat Oncol Biol Phys. 1989;16:535–49. doi: 10.1016/0360-3016(89)90470-7. [DOI] [PubMed] [Google Scholar]
- 47.Myerson RJ, Roti Roti JL, Moros EG, et al. Modeling heat-induced radiosensitization: clinical implications. Int J Hyperthermia. 2004;20:201–12. doi: 10.1080/02656730310001609353. [DOI] [PubMed] [Google Scholar]
- 48.Xu M, Myerson RJ, Straube WL, et al. Radiosensitization of heat resistant human tumour cells by 1 hour at 41.1 degrees C and its effect on DNA repair. Int J Hyperthermia. 2002;18:385–403. doi: 10.1080/02656730210146908. [DOI] [PubMed] [Google Scholar]
- 49.Moros EG, Straube WL, Klein EE, et al. Clinical system for simultaneous external superficial microwave hyperthermia and cobalt-60 radiation. Int J Hyperthermia. 1995;11:11–26. doi: 10.3109/02656739509004944. [DOI] [PubMed] [Google Scholar]
- 50.Straube WL, Moros EG, Low DA, et al. An ultrasound system for simultaneous ultrasound hyperthermia and photon beam irradiation. Int J Radiat Oncol Biol Phys. 1996;36:1189–200. doi: 10.1016/s0360-3016(96)00369-0. [DOI] [PubMed] [Google Scholar]
- 51.Straube WL, Klein EE, Moros EG, et al. Dosimetry and techniques for simultaneous hyperthermia and external beam radiation therapy. Int J Hyperthermia. 2001;17:48–62. doi: 10.1080/02656730150201598. [DOI] [PubMed] [Google Scholar]
- 52.Moros EG, Straube WL, Klein EE, et al. Simultaneous delivery of electron beam therapy and ultrasound hyperthermia using scanning reflectors: a feasibility study. Int J Radiat Oncol Biol Phys. 1995;31:893–904. doi: 10.1016/0360-3016(94)00469-2. [DOI] [PubMed] [Google Scholar]
- 53.Moros EG, Straube WL, Myerson RJ. A reflected-scanned ultrasound system for external simultaneous thermoradiotherapy. Ieee T Ultrason Ferr. 1996;43:441–449. [Google Scholar]
- 54.Novak P, Moros EG, Straube WL, et al. SURLAS: a new clinical grade ultrasound system for sequential or concomitant thermoradiotherapy of superficial tumors: applicator description. Med Phys. 2005;32:230–40. doi: 10.1118/1.1835572. [DOI] [PubMed] [Google Scholar]
- 55.Novak P, Moros EG, Straube WL, et al. Treatment delivery software for a new clinical grade ultrasound system for thermoradiotherapy. Med Phys. 2005;32:3246–56. doi: 10.1118/1.2064848. [DOI] [PubMed] [Google Scholar]
- 56.Moros EG, Fan X, Straube WL, et al. Numerical and in vitro evaluation of temperature fluctuations during reflected-scanned planar ultrasound hyperthermia. Int J Hyperthermia. 1998;14:367–82. doi: 10.3109/02656739809018239. [DOI] [PubMed] [Google Scholar]
- 57.Moros EG, Fan X, Straube WL. Ultrasound power deposition model for the chest wall. Ultrasound Med Biol. 1999;25:1275–87. doi: 10.1016/s0301-5629(99)00087-3. [DOI] [PubMed] [Google Scholar]
- 58.Moros EG, Straube WL, Myerson RJ. Potential for power deposition conformability using reflected-scanned planar ultrasound. Int J Hyperthermia. 1996;12:723–36. doi: 10.3109/02656739609027679. [DOI] [PubMed] [Google Scholar]
- 59.Moros EG, Fan X, Straube WL. An investigation of penetration depth control using parallel opposed ultrasound arrays and a scanning reflector. J Acoust Soc Am. 1997;101:1734–41. doi: 10.1121/1.418154. [DOI] [PubMed] [Google Scholar]
- 60.Moros EG, Fan X, Straube WL. Experimental assessment of power and temperature penetration depth control with a dual frequency ultrasonic system. Med Phys. 1999;26:810–7. doi: 10.1118/1.598589. [DOI] [PubMed] [Google Scholar]
- 61.Moros EG, Straube WL, Myerson RJ, et al. The impact of ultrasonic parameters on chest wall hyperthermia. Int J Hyperthermia. 2000;16:523–38. doi: 10.1080/02656730050199368. [DOI] [PubMed] [Google Scholar]
- 62.Harpen MD. Basic nonlinear acoustics: an introduction for radiological physicists. Med Phys. 2006;33:3241–7. doi: 10.1118/1.2207128. [DOI] [PubMed] [Google Scholar]
- 63.Hamilton MF, Blackstock DT. Nonlinear Acoustics. Academic Press; 1997. [Google Scholar]
- 64.Moros EG, Myerson RJ, Straube WL. Aperture size to therapeutic volume relation for a multielement ultrasound system: determination of applicator adequacy for superficial hyperthermia. Med Phys. 1993;20:1399–409. doi: 10.1118/1.597125. [DOI] [PubMed] [Google Scholar]
- 65.Veldeman L, Madani I, Hulstaert F, et al. Evidence behind use of intensity-modulated radiotherapy: a systematic review of comparative clinical studies. Lancet Oncology. 2008;9:367–375. doi: 10.1016/S1470-2045(08)70098-6. [DOI] [PubMed] [Google Scholar]
- 66.Penagaricano JA, Moros E, Novak P, et al. Feasibility of concurrent treatment with the scanning ultrasound reflector linear array system (SURLAS) and the helical tomotherapy system. Int J Hyperthermia. 2008;24:377–88. doi: 10.1080/02656730801929923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Novak P, Penagaricano JA, Nahirnyak V, et al. Influence of the SURLAS applicator on radiation dose distributions during simultaneous thermoradiotherapy with helical tomotherapy. Phys Med Biol. 2008;53:2509–22. doi: 10.1088/0031-9155/53/10/004. [DOI] [PubMed] [Google Scholar]
- 68.Meeks SL, Harmon JF, Jr, Langen KM, et al. Performance characterization of megavoltage computed tomography imaging on a helical tomotherapy unit. Med Phys. 2005;32:2673–81. doi: 10.1118/1.1990289. [DOI] [PubMed] [Google Scholar]
- 69.Palma DA, Verbakel WF, Otto K, et al. New developments in arc radiation therapy: A review. Cancer Treat Rev. doi: 10.1016/j.ctrv.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 70.Armour EP, Raaphorst GP. Long duration mild temperature hyperthermia and brachytherapy. Int J Hyperthermia. 2004;20:175–89. doi: 10.1080/02656730310001609335. [DOI] [PubMed] [Google Scholar]
- 71.Fuwa N, Nomoto Y, Shouji K, et al. Therapeutic effects of simultaneous intraluminal irradiation and intraluminal hyperthermia on oesophageal carcinoma. Br J Radiol. 2001;74:709–14. doi: 10.1259/bjr.74.884.740709. [DOI] [PubMed] [Google Scholar]
- 72.Geiger M, Strnad V, Lotter M, et al. Pulsed-dose rate brachytherapy with concomitant chemotherapy and interstitial hyperthermia in patients with recurrent head-and-neck cancer. Brachytherapy. 2002;1:149–53. doi: 10.1016/s1538-4721(02)00056-9. [DOI] [PubMed] [Google Scholar]
- 73.Gelvich EA, Klimanov VA, Kramer-Ageev EA, et al. Computational evaluation of changes in ionizing radiation dose distribution in tissues caused by EM applicators when external radiation and hyperthermia act simultaneously. Int J Hyperthermia. 2006;22:343–52. doi: 10.1080/02656730600661750. [DOI] [PubMed] [Google Scholar]
- 74.Juang T, Stauffer PR, Neuman DG, et al. Multilayer conformal applicator for microwave heating and brachytherapy treatment of superficial tissue disease. Int J Hyperthermia. 2006;22:527–44. doi: 10.1080/02656730600931815. [DOI] [PubMed] [Google Scholar]
- 75.Sakurai H, Mitsuhashi N, Tamaki Y, et al. Clinical application of low dose-rate brachytherapy combined with simultaneous mild temperature hyperthermia. Anticancer Res. 2001;21:679–84. [PubMed] [Google Scholar]
- 76.Diederich CJ, Khalil IS, Stauffer PR, et al. Direct-coupled interstitial ultrasound applicators for simultaneous thermobrachytherapy: a feasibility study. Int J Hyperthermia. 1996;12:401–19. doi: 10.3109/02656739609022527. [DOI] [PubMed] [Google Scholar]