Abstract
Transitioning to the nursing home setting is a complex process for family caregivers of older adults with dementia. While nursing home placement (NHP) can alleviate certain caregiving responsibilities, new stressors can also emerge. In the present study, the researchers examined how care-related factors can change leading up to NHP and how these factors influence caregiver outcomes following NHP. A sample of 634 family dementia caregivers (N = 634) were surveyed at three six-month intervals prior to NHP and once during the 12 month period following institutionalization. Growth curve modeling revealed dynamic changes in certain factors leading up to NHP (e.g., caregivers’ perceived health), while other factors remained stable (e.g., caregiver burden). Several factors emerged as significant predictors of caregiver burden following NHP, including pre-placement burden and adult day service utilization. For geriatric social workers, these findings may be useful in assessing family caregivers, and in the development and utilization of appropriate interventions.
Keywords: caregiver burden, nursing home placement, dementia, trajectories
The long-term nature of many dementia-related illnesses has led to the characterization of family caregiving as a ‘career,’ with transitions that occur as diseases progress, needs and capabilities change, and shifts occur in care settings (Aneshensel, et al., 1995; Gaugler, Anderson, Zarit, & Pearlin, 2004; Schulz et al., 2004). Nursing home placement (NHP) represents one key shift in the caregiving career as family members relinquish certain responsibilities, such as bathing and feeding, continue on with other duties, such as providing social support, and adopt new activities and roles, such as interacting with staff and advocating for the care recipient (Aneshensel, et al., 1995; Gaugler et al., 2007a; Schulz et al., 2004). These changes, however, do not necessarily result in the alleviation of stress and burden for caregivers. Former burdens may be reduced (e.g., physical care duties), while new sources of stress may arise (e.g., conflict with staff; Aneshensel et al., 1995). The present study utilizes longitudinal data in order to examine how pre-placement factors influence the burden that dementia caregivers experience following NHP. Understanding this key transition and how pre-placement factors impact post-placement caregiver adaptation is critical for social work professionals assisting families prior to, during, and following NHP.
Transitions in Caregiving
Transitions in caregiving have been conceptualized within the literature as complex and multidimensional processes. Meleis and colleagues (2000), in their conceptual model of health transitions, have identified five properties of the health transition experience, thus elucidating the complex nature in which transitions are experienced. These properties include awareness (i.e., the perception and recognition of a transition); engagement (i.e., the level of involvement in the processes within the transition); change and difference (i.e., while all transitions involve change, not all change involves a transition); time span (i.e., the transition may have an identifiable end point); and critical points and events (i.e., turning points associated with the transition which may lead to more active engagement with the transition). This complexity is reflected in the growing body of research that has examined transitions in caregiving, most notably the transitions that occur during the NHP process for dementia caregivers. Once again, these studies confirm that family caregivers do in fact stay involved in various forms of care following NHP (Gaugler, Zarit, & Pearlin, 2003a; Rowles & High, 1996; Smith & Bengston, 1979; York & Calsyn, 1977; Zarit & Whitlatch, 1992). How caregivers respond to this transition is much less clear. Some studies have shown that caregivers can experience declines in depression and burden following NHP (Gaugler, Roth, Haley, & Mittelman, 2008; Gaugler, Mittelman, Hepburn, & Newcomer, 2009). This may be due to the relinquishing of certain stressful responsibilities, such as constant monitoring and physical care. However, other investigations have shown that caregivers can experience negative outcomes (e.g., burden, depression) following NHP (Aneshensel, 1995; Schulz et al., 2004). This may be attributed to feelings of guilt for institutionalizing a family member or the often reported stress that is associated with interactions with staff and lack of satisfaction with institutional care.
Questions remain as to which factors predict caregiver outcomes following the transition to institutional care. Prior studies of predictors of caregiver adaptation to NHP have produced mixed results. Several studies have suggested that behavioral problems exhibited by care recipients prior to NHP are correlated with negative emotional outcomes for caregivers after NHP (Almberg et al., 2000; Gaugler et al., 2000; Majerovitz, 2007, 2009; Whitlatch et al., 2001). Other studies suggest that behavioral problems have less of an effect on caregiver outcomes following NHP (Gaugler, Anderson, Zarit, & Pearlin, 2004; Tornatore & Grant, 2002). Familial relationship to the care recipient has also been linked to caregiver adaptation to NHP. Findings from these studies maintain that spouses experience more symptoms of depression and more dissatisfaction with the NH setting during the post-placement transition (Gaugler et al., 2000; Schulz et al., 2004). Earlier research suggests no difference in adaptation to NHP among spouses or adult children (Zarit & Whitlatch, 1992). Many of these studies, however, do not examine trajectories of care provided within the home, and how the experiences of long-term home care influence post NHP burden and stress. This is important, as dementia care is a long-term process for families. On average, families spend over five years providing at-home care to functionally and/or cognitively impaired relatives (Alzheimer’s Association, 2009). Again, the complexity of the NHP process and the multitude of factors shown to be associated with emotional distress for caregivers during this transition preclude researchers from reaching a consensus on precisely which caregivers are at greatest risk of experiencing deleterious outcomes during and after NHP.
There are a number of limitations that should be noted in reviewing these past attempts to elucidate the experiences of caregivers during this complex transition in care. Although most researchers used longitudinal methods, many of these studies also relied on small sample sizes, thus impacting the ability to detect changes during NHP. Furthermore, past studies have largely relied upon static measures rather than looking at change (e.g., cross-sectional correlates of stress among caregivers at some point after NHP). For instance, changes in caregiver resources (e.g., use of outside assistance) may be a more appropriate measure in understanding stress and burden rather than a simple measure of caregiver resources at one point in time. In the current study, these limitations are addressed through the use of a large, diverse sample and through the implementation of multiple measures over time, thereby providing measures at discrete points of time as well as measures of change over the trajectory of the caregiving career. These multiple measures allow for the development of a better understanding of the experiences of caregivers during this important transition in caregiving.
In the current study, we attempt to identify and understand which factors affect the experiences of caregivers in the months leading up to and following NHP. Based upon the literature and an understanding of the stress process of dementia caregiving, the following hypothesis was developed and tested: Caregivers who experience decreases in key stress variables (e.g., behavioral problems exhibited by the care recipient, caregiver health impairment) and increases in the availability and use of resources (e.g., assistance with care) prior to NHP will report lower caregiver burden following NHP. It should be noted that caregiver depression was not included as an outcome measure. A recent analysis of the same data used in the present study did not find significant clinical changes in caregiver depression following NHP (Gaugler, Mittelman, Hepburn, & Newcomer, 2009). For this reason, the authors chose to focus specifically on caregiver burden.
In order to gain a better understanding of the trajectory of care, we will examine these stress variables and caregiver resources at multiple points in time prior to NHP and then assess these same variables again following NHP. Growth curve modeling will provide an illustrative understanding of precisely which factors play significant roles in the experiences of caregivers during the NHP process.
Methods
Sample
The sample for the present study was drawn from the Medicare Alzheimer’s Disease Demonstration Evaluation (MADDE) study. MADDE was a large-scale, longitudinal study of a caregiver intervention conducted across eight diverse regions in the United States between 1989 and 1994 (for additional details, see Newcomer, Spitnaly, Fox, & Yordi, 1999). Caregivers were defined in this study as the relative who provided the most assistance to the person with dementia throughout the course of the study. As the goal of the current analysis is to examine the impact of pre-placement factors on post-placement caregiver burden, “synthetic” placement cohorts were constructed that included only those caregivers with 3 waves of pre-placement data and one wave of post-placement data. Caregivers in the MADDE data set who did not have a complete set of four waves of data due to premature NHP or to attrition (e.g., relinquishing caregiver role, drop-out, death) were excluded from the current analysis. Three waves of pre-placement data were selected because this allowed for a more in-depth, empirical analysis of caregiving trajectories prior to NHP via growth curve modeling (see Collins & Sayer, 1997; Raudenbush & Bryk, 2002 and Data Analysis section below) than the analysis of 1 or 2 points of data would have allowed. This resulted in a final sample of 634 (N = 634) dementia caregivers from the original 5,831 dementia caregivers who initially enrolled in MADDE. Caregivers were predominantly female (71.8%), older (M = 64.04 years), spouses (53.0%) of care recipients. Additional sample demographics are presented in Table 1.
Table 1.
Sample characteristics (at baseline)
| Variable | M/% | SD | Range |
|---|---|---|---|
| CG age | 64.04 | 14.11 | 25–96 |
| CG gender (female) | 71.8% | ||
| CG relationship to CR | |||
| Spouse/Partner | 53.0% | ||
| Adult child | |||
| Other | |||
| CG education | |||
| No formal schooling | 0.2% | ||
| Elementary school | 7.4% | ||
| Some high school | 14.2% | ||
| High school or equivalent | 30.8% | ||
| Some college | 24.3% | ||
| College graduate | 13.9% | ||
| Post-graduate | 9.3% | ||
| CG income | |||
| Under $4,999 | 2.1% | ||
| $5,000–$9,999 | 4.7% | ||
| $10,000–$14,999 | 17.2% | ||
| $15,000–$19,999 | 14.4% | ||
| $20,000–$24,999 | 13.0% | ||
| $25,000–$29,999 | 12.8% | ||
| $30,000–$34,999 | 10.3% | ||
| $35,000–$39,999 | 4.1% | ||
| $40,000–$44,999 | 5.5% | ||
| $45,000–$49,999 | 3.6% | ||
| $50,000 and above | 12.5% | ||
| CG employment status (employed) | 33.0% | ||
| CR age | 78.67 | 9.22 | 30–102 |
| CR gender (female) | 58.7% | ||
| CR race/ethnicity | |||
| Caucasian | 92.0% | ||
| African-American | 6.0% | ||
| Hispanic (White) | 1.4 | ||
| Other | 0.6% | ||
| 75.4% | |||
| CR lived with CG | |||
Notes: CG = caregiver; CR = care recipient
Measures
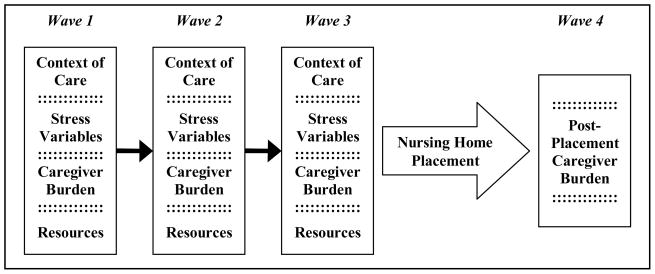
The measures consisted of a series of quantitative scales designed to assess the following: context of care (e.g., demographic and care demand variables), caregiving stress (e.g., unmet need, behavior problems); caregiver burden; and caregiver resources (e.g., assistance with care). Surveys were administered to caregivers by trained nurses and social workers three times at six-month intervals prior to NHP and one time during the 12 months following NHP (see Figure 1 for the sampling framework). Initial interviews were conducted in-person and subsequent interviews were conducted via telephone.
Figure 1.
Sampling framework
Context of Care
A number of contextual variables were measured at baseline, such as gender, caregiver relationship to care recipient, age, income, employment status, education, and duration of care. Additional contextual variables were measured at pre-placement intervals, including caregivers’ self-reported health status and caregivers’ functional dependency as measured by 5 activities of daily living (ADLs: α = .63; Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963) and 8 instrumental activities of daily living (IADLs: α = .80; Lawton & Brody, 1969).
Stress Variables
Several measures assessed care recipient functional, behavioral, and memory impairments at each pre-placement study interval. Care recipient functional variables include dependence on 10 ADLs (α = .90) and 8 IADLs (α = .86). Care recipient cognitive status was measures using the Mini-Mental Status Examination (MMSE) administered at baseline (α = .93; Folstein, Folstein, & McHugh, 1975). Care recipient behavior problems such as asking repetitive questions, being suspicious or accusative, or wandering/getting lost were measured with a 19-item measure (α = .75; Zarit, Orr, & Zarit, 1985). The hours caregivers spent on providing care during a typical week was also included (primary informal caregiving hours). Caregivers’ perceptions of unmet need providing care for ADL and IADL limitations of the care recipient (e.g., more help was needed providing a specific ADL or IADL) were summed (α = .86).
Caregiver Burden
Caregiver burden was measured with a 9-item short form of the Zarit Burden Interview (ZBI; α = .90; Zarit, Reever, & Bach-Peterson, 1980). The ZBI assesses the social, emotional, financial, and psychological distress related to family care provision. The ZBI was administered at all pre-placement and post-placement study interviews.
Resources
In this study, resources were defined as the various services that caregivers used to augment their caregiving capabilities. These services included assistance with chores, personal care services, adult day services, overnight hospital respite, and assistance from family and friends. Service use was assessed using a fixed list of options at each pre-placement interval and at the post-placement interval.
Descriptive data on the measures are presented in Table 2.
Table 2.
Descriptive data
| Variable | M | SD | Range |
|---|---|---|---|
| CG pre-placement health | 1.98 | 0.80 | 1–4 |
| CG pre-placement ADLs | 0.26 | 0.70 | 0–5 |
| CG pre-placement IADLs | 0.75 | 1.41 | 0–8 |
| CG pre-placement unmet needs | 2.85 | 3.73 | 0–18 |
| CG pre-placement caregiving hours (weekly) | 78.48 | 55.30 | 0–168 |
| CG pre-placement burden | 12.74 | 6.22 | 0–28 |
| CG post-placement burden | 13.52 | 7.56 | 0–28 |
| CR pre-placement ADLs | 3.19 | 2.44 | 0–10 |
| CR pre-placement IADLs | 6.40 | 1.67 | 0–8 |
| CR MMSE at initial interview | 15.80 | 7.55 | 0–30 |
| CR pre-placement behavior problems | 9.23 | 3.88 | 0–19 |
| Chore service use (times) | 30.34 | 116.57 | 0–1,456 |
| Personal care use (times) | 50.55 | 191.49 | 0–1,456 |
| Adult day service use (days) | 12.59 | 30.12 | 0–120 |
| Overnight hospital use (times) | 1.84 | 6.07 | 0–58 |
| Secondary caregiving hours (weekly) | 9.97 | 23.42 | 0–168 |
| Duration of Care (months) | 44.44 | 42.78 | 0–384 |
| Time to NHP from pre-placement (days) | 93.47 | 50.13 | 0–265 |
Notes: Measured at baseline except where noted.
M = mean; SD = standard deviation; CR = care recipient; CG = caregiver; NHP = nursing home placement; ADL = activities of daily living; IADLs = instrumental activities of daily living; MMSE = Mini-Mental State Examination
Data Analysis
The first objective of this analysis was to determine whether significant change occurred in the predictor variables prior to NHP. Since 3 waves of data were available prior to NHP, a complex descriptive model was possible. Specifically, a Level 1 growth curve model was “fit” to describe trajectories of change in stress process variables prior to NHP. A growth curve model includes two levels. Level 1 is an initial within-subjects model that describes intra-individual change in a variable (i.e., a random effects model where the intercept and rate of change parameters are estimated for a given sample; see Gaugler, Pot, & Zarit, 2007a). The within-subjects model examines each individual’s growth as a function of time. To describe trajectories of change in stress process variables measured at each pre-placement interval, a Level 1 model using LISREL was conducted (Joreskog & Sorbom, 1993). LISREL provides a number of “goodness of fit” indicators as well as parameter estimates and mean level change values. As only two parameters can be estimated with the three pre-placement waves of data, our Level 1 models focused on initial status (e.g., estimates of pre-placement stress process variables) and rate of change (estimates of linear change in each stress process variable) parameters.
The main research question (change in key stress process variables will predict post-placement burden) was addressed in the empirical analysis. A level 2 growth curve model was conducted using LISTAT. This model is a between-subjects model (e.g., also known as the fixed effects model; Collins & Sayer, 1997; Raudenbush & Bryk, 2002). Initial status and rate of change in stress process model variables served as the predictors in this growth curve model; the dependent variable was post-placement burden. Stress process variables that were measured at baseline only (e.g., MMSE, various context of care variables were also included in the model.
Results
For those variables measured at multiple time points prior to NHP, Level 1 growth curve models were fit to determine trajectories of linear change. Each of the Level 1 models was an excellent fit to the observed data; “excellent” fit is demonstrated in structural equation/growth curve models where p > .05, Root Mean Square Error Approximation (RMSEA) < .05, Non-Normed Fit Index (NNFI) >.95, Comparative Fit Index (CFI) > .95, and Goodness of Fit Index (GFI) >.92 (see Schumacker & Lomax, 1996).
Predictors varied as to whether they increased, decreased, or remained relatively stable in the pre-placement measurement period. Specifically, several variables indicated significant and considerable increases prior to institutionalization, including ADLs (Mrate of change = .49; p < .001; Mrate of change refers to the average point increase or decrease at each of the three pre-placement measurement intervals), IADLs (Mrate of change = .36; p < .001), caregivers’ negative perceptions of health (Mrate of change = .06; p < .05), adult day service use (Mrate of change = 5.04; p < .01), and personal care use (Mrate of change = 13.78; p < .05). Other predictor variables demonstrated significant decreases, such as behavior problems (Mrate of change = −.22; p < .05), caregiving hours (Mrate of change = −6.39; p < .01), and unmet need (Mrate of change = −.24; p < .05). On average, caregiver ADLs (Mrate of change = .00; p > .05), caregiver IADLs (Mrate of change = .05; p > .05), chore service use (Mrate of change = 1.26; p > .05), overnight hospital use (Mrate of change = −.07; p > .05), caregiver burden (Mrate of change = .06; p > .05), and secondary hours (Mrate of change = −.59; p > .05) showed relative stability in the months leading up to the NH transition.
The growth curve model tested the hypothesis that change in key stress process variables prior to NHP would lead to greater burden after institutionalization. The model explained a considerable amount of variance in post-placement burden (R2 = .65). However, the model provided only a moderate fit to the observed data (df = 255; χ2 = 1030.59; p = .00; RMSEA = .06; NNFI = .87; CFI = .94; GFI = .93). Only one variable emerged as a significant predictor of post-placement burden; baseline burden was a strong, significant predictor of post-placement burden (β = .82, p < .01)
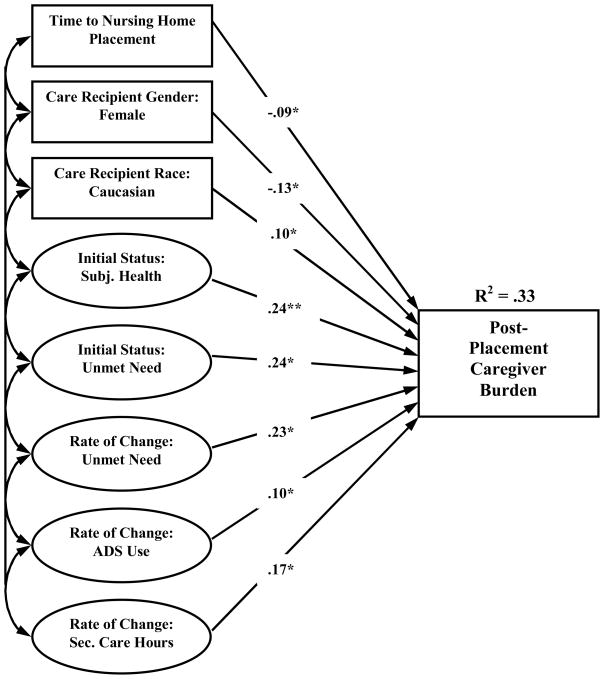
A second model was conducted that excluded pre-placement burden. The model is presented in Figure 2. The model again provided a moderate fit to the data (df = 207; χ2 =799.91; p = .00; RMSEA = .07; NNFI = .85; CFI = .94; GFI = .94) and accounted for a moderate amount of variance in post-placement burden (R2 = .33).
Figure 2.
Predictors of post-placement burden
Notes: Subj. = subjective health; ADS = adult day services; Sec. = secondary caregiving hours Only significant, standardized regression coefficients shown (* p < .05; ** p < .01) df = 207; χ2 = 799.91; p = .00; RMSEA - .07; NNFI = .85; CFI = .94; GFI = .94
Several contextual variables were predictive of post-placement burden. Caregivers who were interviewed at a date more proximal to NHP were more likely to report post-placement burden (β = −.09, p < .05), while care recipients who were male or Caucasian (compared to non-Caucasian) had caregivers indicate greater burden after institutionalization (β = −.13, p < .05; β = .10, p < .05). Caregivers who reported greater health impairment at baseline also perceived greater burden after NHP (β = .24, p < .01).
One stressor and two resource variables appeared to predict feelings of burden after NH entry. Greater unmet need at baseline and increases in unmet need prior to NHP were predictive of greater burden at post-placement (β = .24, p < .05; β = .23, p < .05). Increases in adult day service use appeared to lead to a more difficult emotional transition for caregivers following NHP (β = .10, p < .05). Caregivers who reported reductions in hourly help from other family members or friends in the months leading up to NHP indicated greater burden after institutionalization (β = −.17, p < .05).
Discussion
Providing care to a family member with dementia is a role marked by considerable stress and burden, particularly as the troubling symptoms of the dementia increase and caregivers transition care recipients out of the home care setting (Aneshensel et al., 1995; Dellasega & Nolan, 1997; Schulz et al., 2004). While researchers have considered predictors of NHP across a wide range of samples (for reviews, see Gaugler et al., 2007b; Luppa et al., 2008), this study moves beyond a discrete analysis of predictors of NHP. We examined changes in the caregiving stress process over a 12-month period prior to NHP and followed these caregivers for up to 6 months after NHP to examine factors related to post-placement burden. Our findings indicated that significant change occurs in a number of caregiving variables prior to NHP, such as the functional dependency of caregivers (significant increases) and the hours spent on caregiving (significant decrease). Following NHP, we found that caregiver burden remained stable. More importantly we were able to identify certain contextual variables (e.g., gender and race of care recipient), and resource variables (e.g., adult day service use) that influenced post-placement caregiver burden. In this manner, we believe the findings can help guide NH-based social workers and other NH staff when designing and targeting clinical interventions to assist caregiving families during the placement transition. In the following section, these results will be discussed in detail, as will the practice implications for social work professionals who serve caregivers and care recipients before, during, and after NHP.
The first objective of this study was to investigate whether changes occurred in caregiving variables prior to NHP. Analysis of three waves of data in the 18-month period prior to NHP revealed that there was dynamic change in certain covariates, while others remained stable. Covariates such as care recipients’ functional dependency with ADLs and IADLs, caregivers’ negative perceptions of health, and resource variables such as adult day service use and personal care use all increased significantly prior to NHP. These findings help to describe dementia caregiving conditions that often precede NHP. As the functional abilities of care recipients deteriorate over time, their increased level of dependency can negatively impact the health and well-being of caregivers (see Pinquart & Sorensen, 2007). At the same time, caregivers may increasingly seek outside sources for assistance (e.g., adult day services). However, past research on adult day services and other such interventions has yet to definitively determine whether they are effective in reducing burden or delaying NHP (Pinquart & Sorensen, 2006; Torti et al., 2004). As some have speculated, it may be the case that such efforts to seek assistance are too little, too late (e.g., Chappell & Reid, 2002).
Other caregiving-related factors decreased over the 18-month period prior to NHP, including care recipient behavior problems, caregiving hours, and caregivers’ unmet need. Interpreting these findings is somewhat more complicated. In past research, behavior problems associated with dementia, such as aggression or wandering, have consistently been found to predict NHP, and one might assume that these behavior problems might escalate prior to NHP (Gaugler et al., 2007b). It may be the case that behavior problems in the current sample were perceived as decreasing by caregivers as they increasingly used outside assistance, such as adult day services. Another interpretation is that as dementia progresses, behavior problems such agitation and wandering give way to more functional dependency, such as increased ADLs. While exacerbated behavior problems could pose “crisis” events that trigger institutionalization, the sample and findings here suggest a more gradual placement process based on this functional decline. Eventually, functional decline led to the need for 24-hour skilled nursing care. It should be noted that the cases analyzed in this study are more representative of relatively stable trajectories rather than crisis trajectories or shortened observed time within the community. This operationalization of crisis events vs. more gradual functional decline is an important issue to be addressed in future research.
Finally, several variables remained stable across the period leading to NHP, including care recipient dependency with ADLs and IADLs, use of assistance with chores, overnight hospital use, caregiver burden, and hours of caregiving assistance from family and friends. Again, one might expect each of these factors to increase during the period leading to NHP, most notably caregiver burden. Past studies and the findings from initial analyses of institutionalization using MADDE data have found caregiver burden to be a significant predictor of NHP (for a review, see Gaugler, Mittelman, Hepburn, & Newcomer, 2009). These findings suggest that the consistency and persistency of caregiver burden may be a better predictor of NHP than simply the presence of burden measured at one point in time. It is also important to note that the reasons underlying burden may change over time. Earlier in the caregiving process behavior problems and similar at-home care demands trigger burden. As the decision to place a relative becomes imminent other issues may emerge, such as selection of nursing home, payment issues, or similar concerns which account for changes in burden leading up to and following institutionalization.
Our second objective in this study was to test the hypothesis that changes in key caregiving variables would predict post-placement burden. In our first model, we found that baseline pre-placement burden was the sole significant predictor of post-placement burden. Past research has shown that pre-placement burden is strongly related to post-placement burden (Gaugler et al., 2007a; Schulz et al., 2004). It is also becoming apparent that reductions in caregiver burden occur following NHP (Gaugler, Yu, Krichbaum, & Wyman, 2009). Caregivers should anticipate that while certain stressors may be alleviated by NHP, other stressors may arise to supplant previous burdens, such as problematic interactions with nursing home staff and increased financial burdens, (Gaugler, 2005; Gaugler et al., 2004b; Zarit & Whitlatch, 1992).
We excluded pre-placement burden in our second model to help clarify whether other factors played a role in this process. Three contextual variables emerged as significant predictors of higher levels of post-placement burden, including the gender of the care recipient (male), the race of the care recipient (Caucasian), and the level of caregiver health impairment at baseline. Findings from a number of past studies on caregiver burden, both in the home setting and following NHP, have also found that burden is higher when care recipients are male (Bedard et al., 2005; Nagatomo et al., 1999; Young, 2003) and Caucasian (Buhr, Kuchibhatla, & Clipp, 2006; Friedman, Steinwachs, Temkin-Greener, & Mukamel, 2006; Stevens et al., 2004; Yaffe et al., 2002). This finding is important for practitioners as it identifies a discrete group of care recipients and caregivers who may be at highest risk of burden following NHP, thereby facilitating interventions. Our finding that post-placement burden was greater for those caregivers who had higher levels of health impairment at baseline was not unforeseen, as caregivers with greater health impairment may experience more difficulty adjusting to NHP. Caregivers’ own health problems may be compounded by the changing stressors imposed during this difficult transition period (Gaugler et al., 2007a; Schulz et al., 2004).
Two caregiving resource variables, adult day service usage and hourly help with caregiving from family and friends, were also found to be significant predictors of post-placement burden. Somewhat reflective of past research, we found that increased utilization of adult day service predicted higher levels of post-placement burden. As previously discussed, adult day service use has not been found to delay NHP. Increased use of adult day services may actually be indicative of caregivers who are at the end stage of home care and are struggling to keep their care recipients in the home setting. NHP may not reduce the burden experienced by these caregivers and, as these findings and past findings reveal, burden may be exacerbated by new stressors (Garity, 2006; Gaugler et al., 2007a; Schulz et al., 2004). Caregivers with diminishing assistance from family or friends may also find themselves at greatest risk of burden and stress when NHP finally occurs. Again, there seems to be a misperception that NHP alleviates the need for assistance and support, when in reality the time leading up to NHP and immediately following NHP may be a period during which caregivers need increased guidance, information, and perhaps case management (Garity, 2006; Gaugler, Roth, Haley, & Mittelman, 2008).
The second model also identified two stressors variables as predictive of higher levels of post-placement burden in caregivers: higher levels of unmet caregiver need at baseline and increases in unmet need in the period leading up to NHP. Unmet need is a condition or set of conditions in which the burden of providing care either exceeds the resources of the caregiver or creates deficits in the life of the caregiver (Branch, 2000). Unmet need can be comprised of several areas related to caregiving, such as assistance with ADLs and IADLs, social support, or financial support. While past research has identified post-placement unmet need as a predictor of post-placement burden (Anderson & Gaugler, 2006; Gaugler et al., 2004a), our findings indicate that the rate at which unmet need grows prior to NHP may be equally important as an indicator of post-placement burden. Unmet need is not static, nor is the burden created by unmet need. These findings confirm the dynamic nature of the caregiving process.
Limitations
There are several limitations to consider in interpreting the findings from this study. First, the data set for the MADDE study is approximately 14–19 years old which makes our findings somewhat dated. Despite this apparent limitation, there is little evidence to suggest that the experience of dementia caregivers has changed significantly over this time period, particularly the burden associated with this role (see Gaugler et al., 2008). Nonetheless, the emerging development and availability of care alternatives (e.g., extended use of home care services, assisted living) may influence the experiences of the current cohort of dementia caregivers and care recipients. While the sample in this study was relatively large, it should be noted that participants were not randomly selected. The sample, therefore, may not be representative of the overall population of dementia caregivers and care recipients, which limits our ability to generalize the findings to the overall population. Caregiver/care recipient dyads were also excluded if they were unable to complete the three waves of pre-placement and the one wave of post-placement data collection. While a necessary step for this analysis of caregiving trajectories, we are not able to shed light on the experiences of caregivers with truncated trajectories. This exclusion may have resulted in some selection bias. In actuality, burden may have been a contributing factor in the failure of these caregivers to complete the three waves of data collection. Future analyses using this data set should focus on this specific group of caregivers and care recipients. Finally, the exclusion of the pre-placement burden variable in our second model may have resulted in an over-emphasis on other factors related to post-placement burden. While a limitation, this step provided a richer understanding of the complexity of dementia caregiving and for the illumination of factors that may have been overlooked in past models due to the strength of pre-placement burden in predicting post-placement burden in dementia caregivers.
Implications for Practice
For social workers who provide important clinical support to family caregivers, each transition point within the caregiving career presents opportunities for interventions that may be effective in addressing caregiver stress and burden (Meleis et al., 2000). As reflected in the findings from the present study, there may be warning signs prior to NHP that certain caregivers are at a higher risk of suffering increased burden following NHP. It is imperative for social workers and other health care professionals to identify these “at-risk” caregivers and tailor interventions to address their specific challenges and needs. This process should, and typically does, take place during interventions across the care spectrum. In the home care setting, these interventions may consist of care consultation provided by The Alzheimer’s Association; counseling/caregiving “coaching” provided by Area Agencies on Aging; and multi-component programs that include education, support, therapy, and respite. These interventions have been found to have small but significant impacts on caregiver stress, burden, and well-being. Researchers have found mixed results in terms of the ability of home-based interventions in delaying NHP. It appears that interventions tailored to the specific needs (and unmet needs) of each caregiving situation and that use multiple approaches to addressing caregiver stress and burden may be the most effective for practitioners working with family caregivers in the community (for a review, see Pinquart & Sörensen, 2006). In our study, we found that the variables that predict post-placement caregiver burden often increase or decrease. This reinforces the notion that assessment must be an ongoing process and that interventions should be flexible to meet changing needs. Assessment and intervention procedures should also be sensitive to differences seen within gradual versus crisis caregiving situations, in which stressors may vary considerably in each circumstance.
The present study further confirmed that caregiver burden can be an especially acute problem during the transitions leading to and following NHP. Again, social workers should be particularly alert to factors that might predict burden and stress for caregivers during transition periods. For instance, we found that caregivers who rely increasingly on adult day services have more difficulty during the transition to NHP. Following NHP, caregivers may also continue to experience burden that is related to a new set of factors, including adjusting to the care recipient no longer living at home, financial stressors, and working with NH staff. Nursing home social workers should be cognizant of such predictors and outcomes, and understand that such caregivers may require additional support and services during this time period. A number of innovative programs have been developed to help caregivers during this difficult time and may be especially appropriate for at-risk caregivers. One program specifically designed to assist families with adjustment to NHP has been found to be particularly effective. The Family Involvement in Care (FIC) intervention consists of four components administered by trained senior NH staff (such as the social worker or unit nurse) upon NHP: (1) orienting the caregiver to the NH and to their role in the facility; (2) providing education to the caregiver about the NH environment; (3) negotiating a partnership between the caregiver and the staff; and, (4) remaining in contact with the caregiver and renegotiating the partnership as the caregiving situation evolves. An evaluation of this intervention found that it had significant effects in increasing satisfaction with care, improving family-staff relationships (often a considerable source of stress for both caregivers and staff), and reducing caregivers’ feelings of role loss and role captivity (Specht, Reed, & Maas, 2005). This intervention presents a simple and cost-effective method for social workers and other professionals to help caregivers adapt to and thrive in the NH setting.
Conclusion
It has long been established that transitions in life can be difficult for families and individuals. Researchers have confirmed that transitions from community settings to the nursing home setting are no exception to the notion of “stress in transition” for family caregivers. In the current study, it was found that this transition period is marked by both change and stability in certain caregiving variables prior to NHP and that these variables can help geriatric social workers in identifying and assisting family caregivers in need. Understanding the dynamic nature of caregiving during this transition period is critical for practitioners and dictates ongoing assessment and reflective adjustment to interventions in the months leading to and following NHP. Social work researchers should continue to focus efforts on disentangling the different predictors of caregiver stress during NHP and work with practicing social workers in a translational process to develop feasible and effective interventions.
Acknowledgments
This research was supported by grant R21 AG025625 from the National Institute on Aging/National Institutes of Health.
Contributor Information
Katherina A. Nikzad-Terhune, Email: kanikz2@uky.edu.
Keith A. Anderson, Email: anderson.1630@osu.edu.
Robert Newcomer, Email: robert.newcomer@ucsf.edu.
Joseph E. Gaugler, Email: gaug0015@umn.edu.
References
- Almberg B, Grafstrom M, Krichbaum K, Winblad B. The interplay of institution and family caregiving: relations between patient hassles, nursing home hassles and caregivers’ burnout. Int J Geriatr Psychiatry. 2000;15(10):931–9. doi: 10.1002/1099-1166(200010)15:10<931::aid-gps219>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Alzheimer’s Association. 2009 Retrieved 27 June, 2009 from http://www.alz.org/national/documents/report_alzfactsfigures2009.pdf.
- Anderson KA, Gaugler JE. Unmet need in dementia caregiving: Current research and future directions. In: Welsh EM, editor. Topics in Alzheimer’s disease. Hauppauge, NY: Nova Science Publishers; 2006. pp. 69–88. [Google Scholar]
- Aneshensel CS, Pearlin LI, Mullan JT, Zarit SH, Whitlatch CJ. Profiles in caregiving: The unexpected career. San Diego, CA: Academic Press; 1995. [Google Scholar]
- Bedard M, Kuzik R, Chambers L, Molloy WD, DuBois S, Lever JA. Understanding burden differences between men and women caregivers: The contribution of care-recipient problem behaviors. International Psychogeriatrics. 2005;17(1):99–118. doi: 10.1017/s1041610204000857. [DOI] [PubMed] [Google Scholar]
- Belle SH, Burgio L, Burns R, Coon D, Czaja SJ, Gallagher-Thompson D, et al. ENHPncing the quality of life of dementia caregivers from different ethnic and racial groups. Annals of Internal Medicine. 2006;145:727–738. doi: 10.7326/0003-4819-145-10-200611210-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branch LG. Assessment of chronic care need and use. Gerontologist. 2000;40:390–396. doi: 10.1093/geront/40.4.390. [DOI] [PubMed] [Google Scholar]
- Buhr GT, Kuchibhatla M, Clipp EC. Caregivers’ reasons for nursing home placement: Clues for improving discussions with families prior to transition. Gerontologist. 2006;46:52–61. doi: 10.1093/geront/46.1.52. [DOI] [PubMed] [Google Scholar]
- Chappell NL, Reid RC. Burden and well-being among caregivers: Examining the distinction. Gerontologist. 2002;42(6):772–780. doi: 10.1093/geront/42.6.772. [DOI] [PubMed] [Google Scholar]
- Collins LM, Sayer AG. Modeling growth and change processes: Design, measurement, and analysis for research in social psychology. In: Reiss H, Judd C, editors. Handbook of research methods in social psychology. New York: Cambridge University Press; 1997. pp. 478–495. [Google Scholar]
- Dellasega C, Nolan M. Admission to care: Facilitating role transition amongst family carers. Journal of Clinical Nursing. 1997;6(6):443–451. [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Friedman SM, Steinwachs DM, Temkin-Greener H, Mukamel DB. Informal caregivers and the risk of nursing home admission among individuals enrolled in the Program of All-Inclusive Care for the Elderly. Gerontologist. 2006;46(4):456–463. doi: 10.1093/geront/46.4.456. [DOI] [PubMed] [Google Scholar]
- Garity J. Caring for a family member with Alzheimer’s disease: Coping with caregiver burden post-nursing home placement. Journal of Gerontological Nursing. 2006;32(6):39–48. doi: 10.3928/00989134-20060601-07. [DOI] [PubMed] [Google Scholar]
- Gaugler JE. Family involvement in residential long-term care: A synthesis and critical review. Aging & Mental Health. 2005;9:105–188. doi: 10.1080/13607860412331310245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Anderson KA, Leach CR, Smith CD, Schmitt FA, Mendiondo M. The emotional ramifications of unmet need in dementia caregiving. American Journal of Alzheimer’s Disease and Other Dementias. 2004a;19(6):369–379. doi: 10.1177/153331750401900605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Anderson KA, Zarit SH, Pearlin LI. Family involvement in the nursing home: Effects on stress and well-being. Aging & Mental Health. 2004;8:65–75. doi: 10.1080/13607860310001613356. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Duval S, Anderson KA, Kane RL. Predicting nursing home admission: A meta-analysis. BMC Geriatrics. 2007b doi: 10.1186/1471-2318-7-13. Retrieved July 29, 2008, from http://www.biomedcentral.com/1471-2318/7/13. [DOI] [PMC free article] [PubMed]
- Gaugler JE, Kane RA, Langlois J. Assessment of family caregivers of older adults. In: Kane RL, Kane RA, editors. Assessing the well-being of older people: Measures, meaning, and practical applications. New York: Oxford University Press; 2000. pp. 320–359. [Google Scholar]
- Gaugler JE, Mittelman MS, Hepburn K, Newcomer R. Predictors of change in caregiver burden and depressive symptoms following nursing home admission. Psychology and Aging. 2009;24(2):385–396. doi: 10.1037/a0016052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Pot AM, Zarit SH. Long-term adaptation to institutionalization in dementia caregivers. The Gerontologist. 2007a;47(6):730–740. doi: 10.1093/geront/47.6.730. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Roth DL, Haley WE, Mittelman MS. Can counseling and support reduce burden and depressive symptoms in caregivers of people with Alzheimer’s disease during the transition to institutionalization? Results from the New York University Caregiver Intervention Study. Journal of the American Geriatrics Society. 2008;56:421–428. doi: 10.1111/j.1532-5415.2007.01593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaugler JE, Yu F, Krichbaum K, Wyman JF. Predictors of nursing home admission for persons with dementia. Medical Care. 2009;47:191–198. doi: 10.1097/MLR.0b013e31818457ce. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Zarit SH, Pearlin LI. The onset of dementia caregiving and its longitudinal implications. Psychology and Aging. 2003;18(2):171–80. doi: 10.1037/0882-7974.18.2.171. [DOI] [PubMed] [Google Scholar]
- Joreskog KG, Sorbom D. LISREL 8: Structural equation modeling with the SIMPLIS command language. Chicago, IL: Scientific Software International; 1993. [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. the index of ADL: A standardized measure of biological and psychosocial function. JAMA: The Journal of the American Medical Association. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- Luppa M, Luck T, Brahler E, Konig H, Riedel-Heller SG. Prediction of institutionalization in dementia. Dementia and Geriatric Cognitive Disorders. 2008;26:65–78. doi: 10.1159/000144027. [DOI] [PubMed] [Google Scholar]
- Majerovitz SD. Predictors of burden and depression among nursing home family caregivers. Aging and Mental Health. 2007;11(3):323–329. doi: 10.1080/13607860600963380. [DOI] [PubMed] [Google Scholar]
- Majerovitz SD, Mollott RJ, Rudder C. We’re on the same side: Improving communication between nursing home and family. Health Commun. 2009;24(1):12–20. doi: 10.1080/10410230802606950. [DOI] [PubMed] [Google Scholar]
- Meleis AI, Sawyer LM, Im EO, Hilfinger Messias DK, Schumacher K. Experiencing transitions: an emerging middle-range theory. Adv Nurs Sci. 2000;23(1):12–28. doi: 10.1097/00012272-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Nagatomo I, Akasaki Y, Uchida M, Tominaga M, Hashiguchi W, Takigawa M, et al. Gender of demented patients and specific family relationship on caregiver to patients influence mental fatigue and burdens on relatives as caregivers. International Journal of Geriatric Psychiatry. 1999;14(8):618–625. doi: 10.1002/(sici)1099-1166(199908)14:8<618::aid-gps989>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Newcomer R, Spitalny M, Fox P, Yordi C. Effects of the Medicare Alzheimer’s disease demonstration evaluation on the use of community-based services. Health Services Research. 1999;34:645–667. [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Helping caregivers of persons with dementia: Which interventions work and how large are their effects? International Psychogeriatrics. 2006;18(4):577–595. doi: 10.1017/S1041610206003462. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Correlates of physical health of informal caregivers: A meta-analysis. Journals of Gerontology: Psychological and Social Sciences. 2007;62B(2):126–137. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Application and data analysis methods. 2. Sage Publications; 2002. [Google Scholar]
- Rowles GD, High DM. Individualizing care: Family roles in nursing home decision-making. Journal of Gerontological Nursing. 1996;22(3):20–5. doi: 10.3928/0098-9134-19960301-08. [DOI] [PubMed] [Google Scholar]
- Schulz R, Belle SH, Czaja SJ, McGinnis KA, Stevens A, Zhang S. Long-term care placement of dementia patients and caregiver health and well-being. JAMA: The Journal of the American Medical Association. 2004;292(8):961–967. doi: 10.1001/jama.292.8.961. [DOI] [PubMed] [Google Scholar]
- Schumacker R, Lomax RG. A beginner’s guide to structural equation modeling. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. [Google Scholar]
- Smith KF, Bengston VL. Positive consequences of institutionalization: solidarity between elderly parents and their middle-aged children. The Gerontologist. 1979;19(5 Pt 1):438–47. doi: 10.1093/geront/19.5_part_1.438. [DOI] [PubMed] [Google Scholar]
- Specht JKP, Reed D, Maas ML. Family involvement in care of residents with dementia: An important resource for quality of life and care. In: Gaugler JE, editor. Promoting family involvement in long-term care settings: A guide to programs that work. Baltimore, MD: Health Professions Press; 2005. pp. 163–200. [Google Scholar]
- Stevens A, Owen J, Roth D, Clay O, Bartolucci A, Haley W. Predictors of time to nursing home placement in white and African American individuals with dementia. Journal of Aging and Health. 2004;16(3):375–397. doi: 10.1177/0898264304264206. [DOI] [PubMed] [Google Scholar]
- Tornatore JB, Grant LA. Burden among family caregivers of persons with Alzheimer’s disease in nursing homes. The Gerontologist. 2002;42(4):497–506. doi: 10.1093/geront/42.4.497. [DOI] [PubMed] [Google Scholar]
- Torti FM, Gwyther LP, Reed SD, Friedman JY, Schulman KA. A multinational review of recent trends and reports in dementia caregiver burden. American Journal of Alzheimer’s Disease and Associated Disorders. 2004;18(2):99–109. doi: 10.1097/01.wad.0000126902.37908.b2. [DOI] [PubMed] [Google Scholar]
- Whitlatch CJ, Schur D, Noelker LS, Ejaz FK, Looman WJ. The stress process of family caregiving in institutional settings. The Gerontologist. 2001;41(4):462–73. doi: 10.1093/geront/41.4.462. [DOI] [PubMed] [Google Scholar]
- Yaffe K, Fox P, Newcomer R, Sands L, Linquist K, Dane K, et al. Patient and caregiver characteristics and nursing home placement in patients with dementia. JAMA: The Journal of the American Medical Association. 2002;287(16):2090–2097. doi: 10.1001/jama.287.16.2090. [DOI] [PubMed] [Google Scholar]
- York JL, Calsyn RJ. Family involvement in nursing homes. The Gerontologist. 1977;17(6):500–5. doi: 10.1093/geront/17.6.500. [DOI] [PubMed] [Google Scholar]
- Young RF. Nursing home admission of female Alzheimer’s patients: Family care aspects. Womens Health Issues. 2003;13:2–7. doi: 10.1016/s1049-3867(03)00002-1. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Orr N, Zarit J. Understanding the stress of caregivers: Planning an intervention. In: Zarit SH, Orr N, Zarit J, editors. Hidden victims of Alzheimer’s disease: Families under stress. New York: NYU Press; 1985. pp. 69–86. [Google Scholar]
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20(6):649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Whitlatch CJ. Institutional placement: Phase of transition. Gerontologist. 1992;32:665–672. doi: 10.1093/geront/32.5.665. [DOI] [PubMed] [Google Scholar]